Abstract
Background
Despite the success of childhood immunization in reducing vaccine-preventable diseases, vaccine hesitancy is now a global health threat to this achievement. The current COVID-19 pandemic may change the picture of vaccine hesitancy toward childhood immunizations, which could influence the mothers’ intention to vaccinate their children against COVID-19.
Aim
To measure the prevalence and related factors of vaccine hesitancy towards childhood immunization during the era of COVID-19 along with the prevalence of mothers’ intention to vaccinate their children the future COVID-19 and its association with childhood vaccine hesitancy.
Methods
Cross sectional study was conducted among 270 Saudi mothers attending outpatient clinics at King Abdullah University Hospital (KAAUH) in Riyadh by purposive sampling technique. Data were collected from January to February 2021 using SAGE Group standardized questionnaire.
Results
Although most mothers strongly agree on the importance of the vaccine (79%), almost one-fourth of mothers were hesitant towards childhood immunization (24.31%). Similar percentage of mothers’ intended to vaccinate their children against COVID-19 in the next 6 months was reported (24%). Vaccine hesitancy was found to be a significant predictor of mothers’ intention. Mothers’ education level was significantly associated with being hesitant towards childhood immunization as well as the intention to accept the future COVID-19 vaccine (p < 0.05). Main reason that was highly significantly associated with being hesitant is the concerns about the side effect (50%).
Conclusion
The present study reported a considerable percentage of mothers who are hesitant towards childhood immunization which predicts their intension to vaccinate towards COVID19 and is associated with the level of education.
Keywords: Vaccine hesitancy, Childhood immunization, Mother’s intention, COVID-19, Riyadh
Introduction
Childhood vaccinations are considered one of the most significant achievements of public health interventions, resulting in a clear reduction in morbidity and mortality rates for vaccine-preventable diseases (VPDs) [1]. The World Health Organization (WHO) has stated that improved public vaccination coverage of vaccination is considered a cost-effective strategy that could prevent up to 1.5 million deaths yearly [2]. In 1979, the Kingdom of Saudi Arabia (KSA) adopted the Expanded Programme on Immunization (EPI) that had previously been launched by the WHO [3]. In 2019, the programme succeeded in improving measles immunisation coverage by 96% [4]. Moreover, a marked reduction of more than 90% was observed in the incidence of VPDs [5]. In spite of the programme’s success, vaccine hesitancy is now considered a global challenge to the effectiveness of vaccination programmes in all developed and developing countries [1,3]. Vaccine mistrust is one of the main factors that affects vaccine hesitancy, which is defined by the WHO’s Strategic Advisory Group of Experts (SAGE) on Immunization Working Group as a ‘delay in acceptance or refusal of vaccines despite availability of vaccination services’ [6]. Generally, vaccine hesitancy is complex, varies across time and geographical region and is affected by numerous factors, such as complacency, convenience and lack of confidence [6]. Vaccine hesitancy has contributed to a reduction in vaccine uptake worldwide, causing a resurgence of measles and other VPDs [2,7]. A study conducted by Benecke and DeYoung titled Anti-Vaccine Decision-Making and Measles Resurgence in the United States stated that a 5% reduction in the mumps, measles and rubella (MMR) vaccine uptake has resulted in a 3-fold increase in measles cases [8]. Napolitano et al. investigating Italian parents’ vaccine hesitancy estimated prevalence of vaccine hesitancy in Italy to be 35% [9]. This was similar also in KSA, as demonstrated by a study conducted by Alsubaie et al. at King Khalid University Hospital, which found that 20% of Saudi parents were hesitant with respect to availing of childhood immunisations [3]. In 2019, a new outbreak of respiratory illnesses caused by a novel coronavirus (COVID-19) has emerged in Wuhan, China [10]. The resulting pandemic may alter current vaccine hesitancy trends [11]. Global efforts to accelerate the development of the COVID-19 vaccine were applied in a bid to bring the pandemic under control, and the developed vaccines’ efficacy and effectiveness were trialled and proven among adults [12,13], and clinical trials are currently underway with the aim of developing a vaccine that is safe for use in younger age groups [13]. To achieve herd immunity against COVID-19, a future coverage of 55%–82% is required [14]. Therefore, parents’ positive intentions to vaccinate their children are essential to achieving higher levels of immunity [15]. To date, no studies have investigated the association between Saudi Arabian mothers’ intentions to avail of any future COVID-19 vaccines for their children and vaccine hesitancy with respect to childhood immunisation. This phenomenon may influence mothers’ intentions to vaccinate their children against COVID-19. Therefore, the present study aims to measure the prevalence of vaccine hesitancy towards childhood immunisation and its associated factors during the era of COVID-19. In addition to the prevalence of mothers’ intentions to vaccinate their children against the future COVID-19 vaccine and its association with childhood vaccine hesitancy.
Methods
Study design, setting and population
A descriptive cross-sectional study was conducted among Saudi mothers of children aged 7 years and under attending outpatient clinics at King Abdullah University Hospital (KAAUH) in Riyadh, Saudi Arabia. Mothers of children with immunodeficiency problems, allergic encephalopathy and coma following previous immunisations were excluded. The sample size was 246, following calculations using the formula: n’ based on a prevalence of 20% from a previous study [4]. Z = 1.96 and = 0.05. A further 10% were added to the sample in anticipation of the non-response rate, giving a sample size of 270. A non-probability purposive sampling technique. The recruitment of the study population took place in the outpatient clinic’s female waiting area. The participants were questioned to ensure that they met the inclusion criteria and that they were willing to participate.
Data collection tools
Data collection occurred between 1 January and 28 February 2021, using the validated standard questionnaire designed by WHO SAGE Group. The questionnaire contains two sections. The first section includes three domains: the first domain targets demographic characteristics, including age, educational level, employment status, number of children, and age of youngest child. The second domain measures vaccine hesitancy using a ten-item Likert-type scale (vaccine importance, effectiveness, beneficence, protection, source of information, side effects, and risks). The third domain includes 11 items that aim to identify the underlying factors of vaccine hesitancy, along with an extra open-ended question. Qualitative information was extracted from the written answers [6]. The second section comprises a three-item Likert-type scale aimed at measuring mothers’ intentions to vaccinate their children against COVID-19 extracted from a previous study and adapted to the study topic [16]. The questionnaire was translated into Arabic by researchers who are native Arabic speakers. The Arabic version of the questionnaire was translated again into English by an expert as an evaluation of the preliminary translation. A bilingual expert was enlisted to answer both versions for the purpose of checking the cross-language equivalence. The participants completed the final Arabic version of the questionnaire, which took approximately five minutes to complete, under the researchers’ supervision. The questionnaire’s validity was measured by the average congruency percentage completed by three experts, and the average was 100%. The questionnaire was pilot tested among 20 participants to assess reliability and face validity. The Cronbach’s alphas for the scales measuring vaccine hesitancy and mothers’ intentions were 0.843 and 0.964, respectively. The vaccine hesitancy scale was scored as 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree and 5 = strongly agree, and items 5, 9 and 10 were coded in reverse and given a total score varying from 10 to 50. Items regarding the underlying factors of vaccine hesitancy were scored as 2 = yes, 1 = no and 0 = not sure. The scale measuring mothers’ intentions to vaccinate their children against COVID-19 was scored as 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree and 5 = strongly agree, with a total score varying from 3 to 15.
Statistical analysis
The data were analysed using the statistical software JMP 16.0.0. Frequency tables were used to describe categorical data, and continuous variables were summarised using means and standard deviations. Continuous variables (mother’s age, number of children, age of youngest child) were converted into categorical variables. Vaccine hesitancy and mothers’ intentions total scores were computed by summing the respondent’s answers using the formula function in JMP. To calculate vaccine hesitancy prevalence, total scores were categorised into three groups: hesitant, neutral and non-hesitant, using the lower and upper quartiles as cutoff points. The first 25% of the data with a score of 21–38 were identified as hesitant, 75% of the data and below with a score of 39–44 were identified as neutral, and more than 75% of the data with a score of 45–50 were identified as non-hesitant. The same cutoff points were used to calculate the prevalence of mothers’ intentions to avail of the future COVID-19 vaccine for their children. Graphs were used to illustrate the prevalence of vaccine hesitancy and mothers’ intentions. Associations between categorical data were assessed using the Chi-square test and Fisher’s exact test where applicable. Multivariate analysis was performed using simple linear regression to find the predictor of vaccine hesitancy. Pearson’s correlation was performed before the simple linear regression.
Ethical considerations
Ethical approval was obtained from the Princess Nourah University Institutional Review Board (IRB) (IRB Log Number: 20-0516). Data collection permission was obtained from the KAAUH (RO2021-P-001). Participation was on a voluntary basis, and we obtained informed consent from the participants after explaining the study’s objectives to them. The confidentiality of the collected data was assured as only the researchers had access to the data, and all participants’ identities remained anonymous.
Results
Between January and February 2021, a total of 270 Saudi mothers attending outpatient clinics at King Abdullah University Hospital (KAAUH) in Riyadh, Saudi Arabia participated in this study. Table 1 shows the distribution of the sample’s sociodemographic characteristics. The mean age of the mothers was 33 ± 5.5. Most mothers (61.71%) had completed bachelor’s degrees, while a small proportion of them had not completed high school (2.23%). The majority of participants (61.63%) were employed. More than eighty percent (85%) had four children or fewer, and more than sixty percent of the mothers (69.39%) had children aged 18 months and over.
Table 1.
Sociodemographic characteristics of studied sample. N = 270.
| Variables | N | % |
|---|---|---|
| Age of mother, mean ± SD | 33 ± 5.5 | |
| Level of mother education | ||
| Less than high school | 6 | 2.23 |
| High school | 32 | 11.65 |
| Diploma | 19 | 4.96 |
| Bachelor’s degree | 157 | 61.71 |
| Post graduate degree | 56 | 19.45 |
| Employment status | ||
| Unemployed | 101 | 38.37 |
| Employed | 169 | 61.63 |
| Number of children | ||
| 1–2 children | 130 | 46.13 |
| 3–4 children | 103 | 38.97 |
| 5 or more children | 36 | 14.62 |
| Age of the youngest child | ||
| Less than 6 months | 39 | 12.40 |
| 6 — less than 9 months | 14 | 6.23 |
| 9 — less than 18 months | 32 | 11.97 |
| 18 and above | 185 | 69.39 |
Table 2 details the vaccine hesitancy prevalence and the mothers’ attitudes towards childhood immunisation. Vaccine hesitancy prevalence towards childhood immunisation was (24.31%) and (22.10%) of the mothers were non-hesitant, while more than half of the studied sample had a neutral attitude towards childhood immunisation (53.59%). Almost eighty percent of the mothers strongly agreed on the importance of the vaccines for their children (79.91%). Moreover, 75.27% strongly agreed that vaccines offered by the government are beneficial for their children. Nearly 37% of mothers neither agreed nor disagreed that new vaccines, such as the vaccines against COVID-19, carry more risks than older vaccines.
Table 2.
Attitude of mothers toward vaccinations using SAGE Group vaccine hesitancy 10 item scale. N = 270.
| Strongly agree | Agree | Neutral | Disagree | Strongly disagree | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |
| Childhood vaccines important for my child's health | 211 | 79.91 | 45 | 15.49 | 10 | 3.48 | 3 | 0.93 | 1 | 0.19 |
| Childhood vaccines are effective | 192 | 71.78 | 65 | 23.42 | 9 | 3.46 | 3 | 1.32 | 1 | 0.03 |
| Having my child vaccinated is important for the health of others in my community. | 193 | 69.66 | 60 | 23.49 | 10 | 4.36 | 7 | 2.49 | 0 | 0 |
| All childhood vaccines offered by the government programme in my community are beneficial. | 204 | 75.27 | 53 | 19.37 | 13 | 5.37 | 0 | 0 | 0 | 0 |
| New vaccines carry more risks than older vaccines | 28 | 10.56 | 28 | 10.56 | 110 | 36.59 | 85 | 34.66 | 19 | 7.47 |
| The information I receive about vaccines from the vaccine programme is reliable and trustworthy. | 101 | 36.35 | 105 | 40.38 | 50 | 17.26 | 13 | 5.66 | 1 | 0.03 |
| Getting vaccines is a good way to protect my child/children from disease. | 190 | 72.61 | 61 | 21.03 | 17 | 5.99 | 2 | 0.38 | 0 | 0 |
| Generally, I do what my doctor or health care provider recommends about vaccines for my child/children. | 190 | 72.79 | 65 | 22.93 | 10 | 2.60 | 4 | 1.36 | 1 | 0.32 |
| I am concerned about serious adverse effects of vaccines. | 73 | 26.25 | 90 | 35.54 | 57 | 18.06 | 35 | 13.65 | 15 | 6.51 |
| My child/children do or do not need vaccines for diseases that are not common anymore. | 40 | 12.64 | 39 | 15.61 | 58 | 20.39 | 67 | 24.48 | 66 | 26.88 |
Table 3 represents mothers’ intentions to vaccinate their children against COVID-19. Almost 25.61% strongly agreed that they were most likely to vaccinate their children against COVID-19 within the next six months, while 14.10% of mothers reported that they were unlikely to avail of any future COVID-19 vaccine for their children. The percentage of mothers who reported that they intended to avail of a future COVID-19 vaccine for their children was 24%, while 44% reported that they had no intention of vaccinating their children.
Table 3.
Mothers’ intention to vaccinate their children against COVID-19. N = 270.
| Strongly agree |
Agree |
Neutral |
Disagree |
Strongly disagree |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |
| I intend to vaccinate my child/children against COVID-19 when the vaccine is available in the next 6 months | 68 | 23.31 | 59 | 20.46 | 84 | 32.72 | 34 | 14.10 | 25 | 9.40 |
| I plan to vaccinate my child/children against COVID-19 when the vaccine is available in the next 6 months | 69 | 24.02 | 62 | 22.77 | 89 | 33.91 | 27 | 9.91 | 23 | 9.39 |
| It is likely that I will vaccinate my child/children against COVID-19 in the next 6 months | 74 | 25.61 | 73 | 25.88 | 78 | 30.41 | 25 | 10.36 | 20 | 7.74 |
Table 4 demonstrates the association between demographic characteristics and childhood vaccine hesitancy and mothers’ intentions. A significant association was observed between mothers’ education levels and both vaccine hesitancy towards childhood immunisation and their intentions to vaccinate their children against COVID-19 (p-value = 0.0045 and 0.0288, respectively).
Table 4.
Association of sociodemographic characteristics with vaccine hesitancy and mothers’ intention among studied sample. N = 270.
| Vaccine hesitancy |
Mothers’ intention |
|||
|---|---|---|---|---|
| Test value | p-Value | Test value | p-Value | |
| Age of mothers | 5.389⍖ | 0.2496 | 2.183⍖ | 0.7022 |
| 20 — less than 30 years | ||||
| 30 — less than 40 years | ||||
| 40–50 years | ||||
| Level of mother education | ||||
| Less than high school | 22.216 ☍ | 0.0045 | 17.128 ☍ | 0.0288 |
| High school | ||||
| Diploma | ||||
| Bachelor’s degree | ||||
| Post graduate degree | ||||
| Employment status | 3.134⍖ | 0.2087 | 4.681⍖ | 0.0963 |
| Unemployed | ||||
| Employed | ||||
| Number of children^ | 3.035⍖ | 0.5520 | 5.105⍖ | 0.2767 |
| 1−2 children | ||||
| 3−4 children | ||||
| 5 or more children | ||||
| Age of the youngest child | ||||
| 0 — less than 6 months | 8.296⍖ | 0.2172 | 2.886⍖ | 0.8230 |
| 6 — less than 9 months | ||||
| 9 — less than 18months | ||||
| 18 months and above | ||||
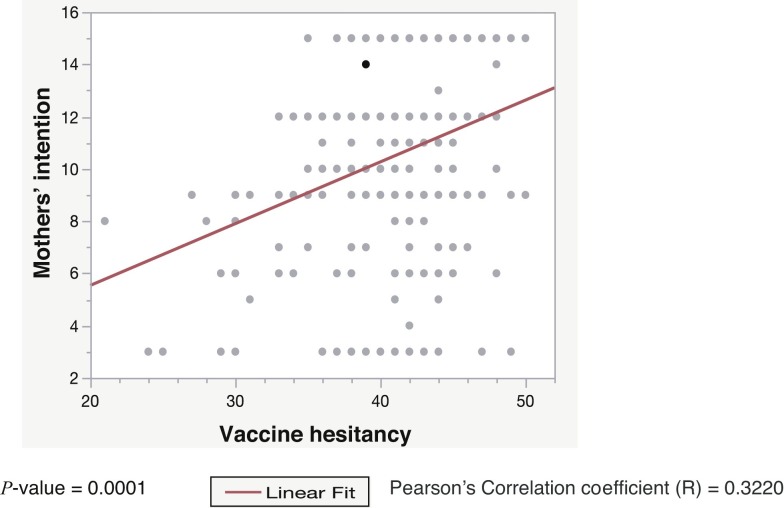
Table 5 details a simple linear regression that was performed to test whether vaccine hesitancy predicts mothers’ intentions to vaccinate their children against COVID-19 in the future. The regression results indicated that the model explained 10.3% of the mothers’ intentions and that vaccine hesitancy significantly predicts mothers’ intentions to avail of a future COVID-19 vaccine for their children (F (31.0032), p-value <0.0001). The equation used to predict the mothers’ intentions is y = a + bx, where y = mothers’ intention score, a = intercept estimate, b = vaccine hesitancy total score estimate and x = vaccine hesitancy score.
Table 5.
Simple linear regression between vaccine hesitancy and mothers’ intention to vaccinate their children against COVID-19. N = 270.
| Summary of fit | |
|---|---|
| R square | 0.103689 |
| R square adj | 0.100344 |
| Root mean square error | 3.367668 |
| Mean of response | 10.45926 |
| Observations | 270 |
| Parameter estimates | ||||
|---|---|---|---|---|
| Term | Estimate | Std error | t Ratio | Prob>|t| |
| Intercept | 0.812 | 1.744 | 0.47 | 0.6420 |
| Vaccine hesitancy total score | 0.236 | 0.042 | 5.57 | <0.0001* |
The final predictive model mother’s intention score = 0.8120604 + 0.2362794*vaccine hesitancy score.
The final predictive model was the mother’s intention score = 0.8120604 + 0.2362794*vaccine hesitancy score.
Table 6 details the association between the underlying factors and vaccine hesitancy towards childhood immunisation using a Chi-Square test. The following factors were identified: Did not know where to get vaccination; Did not know where to access good/reliable information; Did not think vaccine was effective; Did not think vaccine was necessary; Did not think the vaccine was safe/concerned about side effects; Someone else told me theytheir child had a bad reaction; Someone else told me that vaccine was not safe; Heard or read negative media that were significantly associated with vaccine hesitancy towards childhood immunisations (p-value < 0.05).
Table 6.
Association of underlying factors of childhood vaccine hesitancy according to mothers’ hesitancy status. N = 270.
| Underlying factors | Hesitant mothers | Neutral | Non-hesitant mothers | Test value | p-Value |
|---|---|---|---|---|---|
| n = 70 | n = 144 | n = 56 | |||
| Did not know where to get vaccination | 11.943 | 0.0178 | |||
| No | 52 (74.29%) | 117 (81.25%) | 54 (96.43%) | ||
| Not sure | 9 (12.86%) | 16 (11.11%) | 2 (3.57%) | ||
| Yes | 9 (12.86%) | 11 (7.64%) | 0 (0%) | ||
| Did not know where to get good/reliable information | 19.161 | 0.0007 | |||
| No | 44 (62.86%) | 105 (72.92%) | 52 (92.86%) | ||
| Not sure | 5 (7.14%) | 10 (6.94%) | 2 (3.75%) | ||
| Yes | 21 (30%) | 29 (20.14%) | 2 (3.57%) | ||
| Did not think vaccine was effective | 28.710 | <0.0001 | |||
| No | 41 (58.57%) | 117 (81.25%) | 54 (96.43%) | ||
| Not sure | 10 (14.29%) | 12 (8.33%) | 0 (0%) | ||
| Yes | 19 (27.14%) | 15 (10.42%) | 2 (3.57%) | ||
| Did not think it was needed | 30.113 | <0.0001 | |||
| No | 45 (64.29%) | 121 (84.03%) | 55 (98.21%) | ||
| Not sure | 7 (10%) | 10 (6.94%) | 0 (0%) | ||
| Yes | 18 (25.71%) | 13 (9.03%) | 1 (1.79%) | ||
| Did not think the vaccine was safe/concerned about side effects | 50.099 | <0.0001 | |||
| No | 26 (37.14%) | 105 (72.92%) | 52 (92.86%) | ||
| Not sure | 9 (12.86%) | 12 (8.33%) | 2 (3.57%) | ||
| Yes | 35 (50%) | 27 (18.75%) | 2 (3.57%) | ||
| Had a bad experience with a vaccinator/health clinic | 4.573 | 0.3340 | |||
| No | 61 (87.14%) | 134 (93.06%) | 54 (96.43%) | ||
| Not sure | 3 (4.29%) | 5 (3.47%) | 1 (1.79%) | ||
| Yes | 6 (8.57%) | 5 (3.47%) | 1 (1.79%) | ||
| Had a bad experience or reaction with previous vaccination | 0.912 | 0.9229 | |||
| No | 65 (92.86%) | 137 (95.14%) | 54 (96.43%) | ||
| Not sure | 2 (2.86%) | 3 (2.08%) | 1 (1.79%) | ||
| Yes | 3 (4.29%) | 4 (2.78%) | 1 (1.79%) | ||
| Fear of needles | 3.919 | 0.4170 | |||
| No | 48 (68.57%) | 109 (75.69%) | 46 (82.14%) | ||
| Not sure | 1 (1.43%) | 1 (0.69%) | 1 (1.79%) | ||
| Yes | 21 (30%) | 34 (23.61%) | 9 (16.07%) | ||
| Someone else told me theytheir child had a bad reaction | 18.484 | 0.0010 | |||
| No | 43 (61.43%) | 115 (79.86%) | 49 (87.50%) | ||
| Not sure | 4 (5.71%) | 9 (6.25%) | 4 (7.14%) | ||
| Yes | 23 (32.86%) | 20 (13.89%) | 3 (5.36%) | ||
| Someone else told me that vaccine was not safe | 20.140 | 0.0005 | |||
| No | 40 (57.14%) | 103 (71.53%) | 50 (89.29%) | ||
| Not sure | 6 (8.57%) | 10 (6.94%) | 0 (0%) | ||
| Yes | 24 (34.29%) | 31 (21.53%) | 6 (10.71%) | ||
| Heard or read negative media | 14.644 | 0.0055 | |||
| No | 40 (57.14%) | 97 (67.36%) | 48 (85.71%) | ||
| Not sure | 5 (7.14%) | 8 (5.56%) | 3 (5.36%) | ||
| Yes | 25 (35.71%) | 39 (27.08%) | 5 (8.93%) | ||
Fig. 1 illustrates a positive weak relationship between vaccine hesitancy and mothers’ intentions to vaccinate their children against COVID-19. A statistically significant correlation is evident between vaccine hesitancy and mothers’ intentions.
Fig. 1.
The correlation between vaccine hesitancy and mothers’ intention to vaccinate their children COVID-19 among 270 mothers.
Explanation of causes of vaccine hesitancy using content analysis for qualitative data approach
Some hesitant parents reported extra factors that contributed to their hesitation, such as autism, which was mentioned by two respondents. Participant 179 said, ‘I noticed the occurrence of autism in my family among children after the vaccinations for children aged four months and 18 months’ while Participant 264 cited ‘the experiences of two of my nephews with autism after vaccinations’. Another participant mentioned vaccine safety as a cause of her hesitancy: she said, ‘I am afraid that it is not safe and that my child is a victim of a clinical trial, and I reject this principle’ (Participant 236). Two further participants mentioned the lack of studies regarding vaccination: the first said, ‘the long-term studies are insufficient, especially for those with allergy symptoms’ (Participant 133). The other one said, “The vaccine was not subjected to a sufficient trial” (Participant 87). Vaccines’ side effects were also among the stated causes of hesitancy for three participants, along with the concern that the vaccines will cause diseases: Participant 40 said, ‘the long-term side effects are not yet known’. Participant 97 stated, ‘The vaccine has side effects that were experienced by people close to me, and there are people who got the vaccine and got the disease.’ The third said, ‘I am afraid that my children will catch diseases’ (Participant 91).
Other reasons for hesitancy include rejection of the new vaccine and the health care provider’s attitude. Participant 77 stated, ‘I reject the new vaccines for children’. Participant 41 said that they would reject the vaccine ‘due to the fatigue that follows vaccination’ as well as doctors’ doubts about the vaccines’ future side effects.
Discussion
Vaccine hesitancy is a worldwide phenomenon that may impede the efforts of childhood vaccination programmes, which have contributed to a major reduction in the prevalence of VPDs. Overcoming this challenge and increasing the uptake of vaccines is essential, particularly during the ongoing COVID-19 pandemic, in which this hesitancy might influence mothers’ intentions in vaccinating their children. The present study aimed to measure the prevalence of vaccine hesitancy towards childhood immunisation and its associated factors during the era of the COVID-19 pandemic, along with measuring the prevalence of mothers’ intentions to vaccinate their children against COVID-19 in the future and its association with childhood VPD vaccine hesitancy.
The present study found that almost one-quarter of mothers in KAAUH were hesitant towards childhood immunisations. This may be explained by the fact that almost half of the mothers are new to the motherhood experience with only one or two children; thus, they may have more concerns about the vaccines than mothers with more than two children who had more experience of childhood immunisation. These findings were similar to those of a study conducted in Riyadh by Alsubaie et al., which stated that twenty percent of the parents studied were hesitant towards children’s routine vaccinations [3]. Current study showed that more than half of the mothers expressed a neutral attitude towards childhood immunisation. This may be attributed to the high percentage of neutral responses (i.e., neither agree nor disagree) to the statements ‘new vaccines carry more risks than old ones’ and ‘children do not need vaccines for uncommon diseases’. The observed neutral attitudes might be due to the mothers’ lack of knowledge regarding vaccine risks or the mothers’ misunderstanding of the statement making it impossible for them to confirm their agreement or disagreement. This finding coincides with a previous study conducted in China by Ren et al., which concluded that the majority of the studied sample exhibited a neutral attitude towards the statement that ‘new vaccines carry more risk than old ones’ [17]. The results also indicated a statistically significant association between vaccine hesitancy and low education levels. This may be due to the fact that the group with low education were more likely to believe and share misleading information, and this is supported by the fact that the second factor chosen by hesitant mothers was ‘heard or read negative media’. This association was also observed in previous studies conducted in Pakistan and China [18,19].
This study also revealed that the source of vaccine information was significantly more influential in hesitant mothers, as almost one-third of them did not know where to access good or reliable information about childhood immunisations and nearly a quarter of them had previously heard or read negative media. This may be explained by the influence of social media in recent years and the multiplicity of sources available, which makes it difficult to distinguish between true and false information. These findings are similar to those of a study conducted in China by Du et al., which demonstrated that more than half of the hesitant respondents had heard or read negative information about the vaccine in the media, which was considered the primary contributing factor in their hesitancy [18]. The results of this study also demonstrated that factors pertaining to lack of vaccine confidence are highly significant among hesitant mothers; half of the hesitant mothers reported concerns about the vaccine’s safety and its side effects, and almost one-third believed that the vaccine was not effective. This was confirmed by the qualitative data expressed in the open-ended question by hesitant mothers about their concerns that vaccines might cause autism in their children and the unknown side effects that might emerge in the long term. One mother stated that the vaccines might not be subjected to sufficient trials. These findings are consistent with a study that Khattak et al. conducted in Pakistan to determine the vaccination refusal rate using the SAGE Group tool, which found that hesitant people have greater concerns about vaccine effectiveness and side effects with a p-value <0.005 [19]. In this study peer influence was significantly associated with hesitancy, as about one-third of hesitant mothers reported that someone else had told them that the vaccine was not safe and that their child had experienced a bad reaction. This may be due to the fact that people usually influence one another and that as most of the hesitant mothers were younger, they may have been more easily influenced. These findings corroborate those of a study conducted in Canada by Dube et al., which demonstrated that social influence was a significant factor in parents’ decisions to not vaccinate their children [20].
In assessing the mothers’ intentions to vaccinate their children against COVID-19, it was found that almost one-quarter intended to vaccinate their children. A possible explanation for this result is the fact that mothers may be uncertain or anxious about the vaccine’s long-term effects, which they mentioned when asked about the reasons for their hesitancy. These findings disagree with those of a study conducted by Bell et al. in England, which reported higher levels of intention to vaccinate children against COVID-19 in the future [21]. These differences may be due to the escalated pandemic situation in the UK and the higher perceived risk compared to the Saudi context. Moreover, education level is significantly associated with mothers’ intentions to vaccinate their children against COVID-19; as the level of education increased, the mother’s intention also increased. This may indicate that more highly educated mothers know where to access reliable information and have greater awareness of the benefits that vaccines offer with respect to controlling the pandemic. The findings were also consistent with Akarsu et al.’s study in Turkey, which identified a significant association between education level and willingness to vaccinate children against COVID-19 [22]. Analysis using linear regression in this study confirmed that vaccine hesitancy towards childhood immunisation is a predictor of mothers’ intentions to vaccinate their children against COVID-19 in the future, whereby hesitant mothers have lower intentions to avail of any future COVID-19 vaccine. This may be due to the fact that peoples’ attitudes are difficult to influence, and therefore, mothers’ existing attitudes towards childhood immunisation will influence their decisions or willingness to avail of new vaccines for their children. Similarly, Goldman et al.’s study conducted across six different countries found that those who were committed to the childhood immunisation schedule were more willing to accept the COVID-19 vaccine for their children and that this was a significant predictor of their intention [23].
Conclusion and recommendations
The present study reported a considerable percentage of mothers who were hesitant to avail of childhood immunisation; moreover, a lower percentage reported any intention to vaccinate their children in the future against COVID-19 once a vaccine becomes available. Education level was found to be significantly associated with vaccine hesitancy towards childhood immunisation and mothers’ intentions to vaccinate their children against COVID-19. Factors that may explain the mothers’ hesitancy include lack of confidence and low risk perception with respect to VPDs, which were also found to be highly significant factors in hesitancy towards children’s routine vaccinations. In addition, the regression model used in this study confirmed that vaccine hesitancy significantly predicts mothers’ intentions to vaccinate their children against COVID-19 in the future. Authors suggest that public health officials, such as those at the Ministry of Health (MOH), should engage in routine childhood vaccination community campaigns on a regular basis and use World Immunization Week to inform and clarify how these vaccines have contributed significantly to controlling many life-threatening diseases. In recent years, media influence has become a powerful tool, either changing of reinforcing collective or individual beliefs and making it easier for hesitant people to connect and influence one another. Therefore, it is recommended that health authorities take advantage of the media to increase awareness in the community by promoting credible information about vaccines. We recommend that health facilities deliver appropriate educational programmes on COVID-19 in their respective communities to enhance mothers’ intentions and overall knowledge regarding the importance of vaccinating their children and increase their willingness and acceptance once a children’s COVID-19 vaccine becomes available. We recommend that future studies further investigate the determinants of the mothers’ intentions to vaccinate their children against COVID-19 to proactively address the low intention rate.
Limitations and acknowledgment
We would like to acknowledge the study population for their time in contribution in the study. Although sample size was small but is representative for the population which it resamples as it is calculated using sample size calculator using specific parameters.
Limitation was non-generalizability as the sample was recruited by a non-probability sampling technique.
Authors’ contribution
All authors contribute in preparation of the work starting from writing the proposal, collecting and analyzing data, and writing the report.
Funding
This research was funded by the Deanship of Scientific Research at Princess Nourah Bint Abdulrahman University through the Fast-Track Research Funding Program.
Competing interests
None declared.
Ethical approval
Not required.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jiph.2021.08.028.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Dubé E., Laberge C., Guay M., Bramadat P., Roy R., Bettinger J. Vaccine hesitancy: an overview. Hum Vaccines Immunother. 2013;9:1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . World Health Organization; 2019. Ten threats to global health in 2019; pp. 1–18.https://www.WHO.int/news-room/spotlight/ten-threats-to-global-health-in-2019 . [Accessed 10 April 2021] [Google Scholar]
- 3.Alsubaie S.S., Gosadi I.M., Alsaadi B.M., Albacker N.B., Bawazir M.A., Bin-Daud N. Vaccine hesitancy among Saudi parents and its determinants. Saudi Med J. 2018;40:1242–1250. doi: 10.15537/smj.2019.12.24653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO, UNICEF . 2019. India: WHO and UNICEF estimates of immunization coverage: 2015. [Google Scholar]
- 5.Tufenkeji H., Kattan H. Childhood immunization in the Kingdom of Saudi Arabia. Ann Saudi Med. 1994;14:91–93. doi: 10.5144/0256-4947.1994.91. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organisation SAGE . 2014. Report of the SAGE Working Group on vaccine hesitancy. [Google Scholar]
- 7.Benecke O., DeYoung S.E. Anti-vaccine decision-making and measles resurgence in the United States. Global Pediatr Health. 2019;6:1–5. doi: 10.1177/2333794X19862949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lo N.C., Hotez P.J. Public health and economic consequences of vaccine hesitancy for measles in the United States. JAMA Pediatr. 2017;171:887–892. doi: 10.1001/jamapediatrics.2017.1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Napolitano F., D’Alessandro A., Angelillo I.F. Investigating Italian parents’ vaccine hesitancy: a cross-sectional survey. Hum Vaccines Immunother. 2018;14:1558–1565. doi: 10.1080/21645515.2018.1463943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abebe E.C., Dejenie T.A., Shiferaw M.Y., Malik T. The newly emerged COVID-19 disease: a systemic review. Virol J. 2020;17:1–8. doi: 10.1186/s12985-020-01363-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chandir S., Siddiqi D.A., Mehmood M., Setayesh H., Siddique M., Mirza A. Impact of COVID-19 pandemic response on uptake of routine immunizations in Sindh, Pakistan: an analysis of provincial electronic immunization registry data. Vaccine. 2020;38:7146–7155. doi: 10.1016/j.vaccine.2020.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saudi Press Agency . The Official Saudi Press Agency; 2020. SFDA approves registration of Pfizer-BioNTech COVID-19 vaccine.https://www.spa.gov.sa/viewfullstory.php?lang=en&newsid=2166947 [Google Scholar]
- 13.Salazar J. Connect Child Spec Gr; 2021. When will the COVID-19 vaccine be available for kids, and will it be safe for your family?https://www.connecticutchildrens.org/coronavirus/when-will-the-covid-19-vaccine-be-available-for-kids-and-will-it-be-safe-for-your-family/ [Google Scholar]
- 14.Schaffer Deroo S., Pudalov N.J., Fu L.Y. Planning for a COVID-19 vaccination program. JAMA J Am Med Assoc. 2020;323:2458–2459. doi: 10.1001/jama.2020.8711. [DOI] [PubMed] [Google Scholar]
- 15.Velavan T.P., Pollard A.J., Kremsner P.G. Herd immunity and vaccination of children for COVID-19. Int J Infect Dis. 2020;98:14–15. doi: 10.1016/j.ijid.2020.06.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kowitt S.D., Cornacchione Ross J., Jarman K.L., Kistler C.E., Lazard A.J., Ranney L.M. Tobacco quit intentions and behaviors among cigar smokers in the United States in response to COVID-19. Int J Environ Res Public Health. 2020;17:5368. doi: 10.3390/ijerph17155368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ren J., Wagner A.L., Zheng A., Sun X., Boulton M.L., Huang Z. The demographics of vaccine hesitancy in Shanghai, China. PLoS One. 2018;13 doi: 10.1371/journal.pone.0209117. e0209117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Du F., Chantler T., Francis M.R., Sun F.Y., Zhang X., Han K. The determinants of vaccine hesitancy in China: a cross-sectional study following the Changchun Changsheng vaccine incident. Vaccine. 2020;38:7464–7471. doi: 10.1016/j.vaccine.2020.09.075. [DOI] [PubMed] [Google Scholar]
- 19.Khattak F.A., Rehman K., Shahzad M., Arif N., Ullah N., Kibria Z. Prevalence of Parental refusal rate and its associated factors in routine immunization by using WHO vaccine hesitancy tool: a cross sectional study at district Bannu, KP, Pakistan. Int J Infect Dis. 2021;104:117–124. doi: 10.1016/j.ijid.2020.12.029. [DOI] [PubMed] [Google Scholar]
- 20.Dube E., Bettinger J.A., Halperin B., Bradet R., Lavoie F., Sauvageau C. Determinants of parents’ decision to vaccinate their children against rotavirus: results of a longitudinal study. Health Educ Res. 2012;27:1069–1080. doi: 10.1093/her/cys088. [DOI] [PubMed] [Google Scholar]
- 21.Bell S., Clarke R., Mounier-Jack S., Walker J.L., Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. 2020;38:7789–7798. doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Akarsu B., Canbay Özdemir D., Ayhan Baser D., Aksoy H., Fidancı İ., Cankurtaran M. While studies on COVID-19 vaccine is ongoing, the public’s thoughts and attitudes to the future COVID-19 vaccine. Int J Clin Pract. 2020;67:1–10. doi: 10.1111/ijcp.13891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldman R.D., Yan T.D., Seiler M., Parra Cotanda C., Brown J.C., Klein E.J. Caregiver willingness to vaccinate their children against COVID-19: cross sectional survey. Vaccine. 2020;38:7668–7673. doi: 10.1016/j.vaccine.2020.09.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.