Abstract
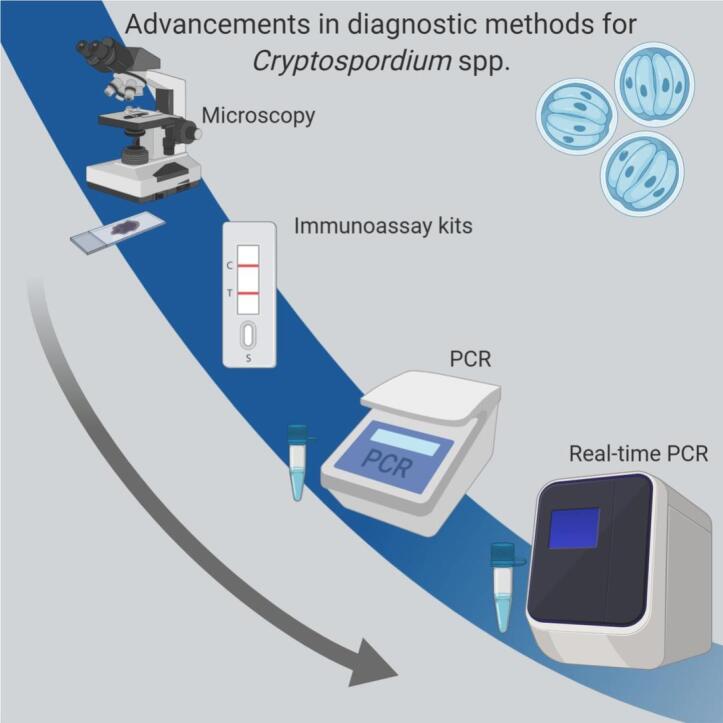
The protozoan parasite Cryptosporidium has emerged as a leading cause of diarrhoeal illness worldwide, posing a significant threat to young children and immunocompromised patients. While endemic in the vast majority of developing countries, Cryptosporidium also has the potential to cause waterborne epidemics and large scale outbreaks in both developing and developed nations. Anthroponontic and zoonotic transmission routes are well defined, with the ingestion of faecally contaminated food and water supplies a common source of infection. Microscopy, the current diagnostic mainstay, is considered by many to be suboptimal. This has prompted a shift towards alternative diagnostic techniques in the advent of the molecular era. Molecular methods, particularly PCR, are gaining traction in a diagnostic capacity over microscopy in the diagnosis of cryptosporidiosis, given the laborious and often tedious nature of the latter. Until now, developments in the field of Cryptosporidium detection and research have been somewhat hampered by the intractable nature of this parasite. However, recent advances in the field have taken the tentative first steps towards bringing Cryptosporidium research into the 21st century. Herein, we provide a review of these advances.
Keywords: Cryptosporidium, Cryptosporidium parvum, Cryptosporidium hominis, Infectious disease, Clinical diagnosis, CRISPR/Cas
Graphical abstract
Highlights
-
•
Cryptosporidium, a protozoan parasite, is a leading cause of gastroenteritis worldwide.
-
•
Despite its prevalence and impact, it is underreported, with no vaccine and few treatment options.
-
•
While molecular diagnosis options are increasing, microscopy remains the gold standard.
-
•
Many areas of research have also been limited by the intractable nature of this pathogen.
-
•
Advances in molecular biology, e.g. NGS and CRISPR/Cas, stand to advance research in this field.
1. Introduction
Cryptosporidium is an obligate enteric protozoan parasite and a well-established pathogen of the gastrointestinal tract (Tzipori and Widmer, 2008). Originally described from histological preparations of murine gastric mucosa in 1907 (Tyzzer, 1910), Cryptosporidium was not linked with human infection until 1976 (Nime et al., 1976). Sentinel alert of the clinical significance of cryptosporidial infection was established after reports of fatal cryptosporidiosis in AIDS patients during the 1980s (Soave et al., 1984), and a large waterborne outbreak affecting approximately 400,000 Milwaukee residents in 1993 (D’Antonio et al., 1985; MacKenzie et al., 1995; Soave et al., 1984). Cryptosporidium is environmentally and geographically ubiquitous, comprising many species spanning a wide host range. To date over 40 species have been described, with at least 20 species having been reported in human infection (Feng et al., 2018; Xiao and Feng, 2017). However, C. hominis and C. parvum have been reported to account for the vast majority of infections in humans (Feng et al., 2018).
Cryptosporidium has now emerged as a leading cause of diarrhoeal illness worldwide, posing a significant threat to young children and immunocompromised patients. It has been reported to be a leading cause of moderate-to-severe gastrointestinal morbidity in children younger than 5 years in developing countries (Kotloff et al., 2013). A recent study into the global burden of gastrointestinal disease found that Cryptosporidium spp. accounted for in excess of 1 million deaths, almost half a million of which were in children under the age of five, and over 71 million disability-adjusted life years (DALYs) between 2005 and 2015; the highest mortality rates were observed in developing countries, particularly those in sub-Saharan Africa (Troeger et al., 2017).
While endemic in the vast majority of developing countries, Cryptosporidium also has the potential to cause waterborne epidemics and large scale outbreaks in both developing and developed nations (Efstratiou et al., 2017). Anthroponontic and zoonotic transmission routes are well defined, with the ingestion of faecally contaminated food and water supplies a common source of infection (King et al., 2019; McKerr et al., 2019; Ryan et al., 2018).
Microscopy, the current diagnostic mainstay, is considered by many to be suboptimal. This has prompted a shift towards alternative diagnostic techniques in the advent of the molecular era. Molecular methods, particularly PCR, are gaining traction in a diagnostic capacity over microscopy in the detection of Cryptosporidium spp., given the laborious and tedious nature of the latter. The supersession of microscopy by molecular techniques, which offer rapid diagnosis and improved sensitivity, may also be attributed to diminishing microscopy skills in modern clinical laboratories (Meurs et al., 2017). Until now, developments in the field of Cryptosporidium detection and research have been somewhat hampered by the intractable nature of this parasite. However, recent advances, particularly in the application of the CRISPR/Cas system to produce genetically modified, tractable Cryptosporidium oocysts (Vinayak et al., 2015), have allowed the field to take tentative steps towards bringing Cryptosporidium research into the 21st century.
2. Diagnosis
Given the broad spectrum of susceptibility and the significant morbidity and mortality rates associated with Cryptosporidium in immunosuppressed patient populations, the development of efficient and effective screening criteria and robust testing algorithms is vital in clinical laboratories (Bruijnesteijn van Coppenraet et al., 2009; Garcia et al., 2003; Hawash, 2014). However, there remains no international standard methods for the diagnosis of cryptosporidiosis. In some countries Cryptosporidium testing is limited to known HIV/AIDS patients, however, testing of adult samples is usually reliant upon stipulating factors such as watery or persistent diarrhoea, and when clinically suspected (Chalmers, 2008). Current UK microbiological standards recommend that all symptomatic cases of acute diarrhoea are investigated based on guidelines for faecal screening for Cryptosporidium, published in 1993 (Casemore and Roberts, 1993). These guidelines are the culmination of a two year prospective survey conducted in 16 clinical laboratories on some 62,000 patients, which provided data pertaining to the absolute and relative frequency of Cryptosporidium infection across all age groups and consequently allowed for meaningful age-based selection criteria to be determined (Casemore and Roberts, 1993; Palmer and Biffin, 1990; Public Health England, 2014). Compliance with these guidelines is not absolute, several UK-based studies determined that routine screening of all diagnostic stool specimens for Cryptosporidium in participating clinical laboratories ranged from 33 to 72.5% (Chalmers and Thomas, 2002; Chalmers et al., 2015). The more recent of these studies found that 27.5% of surveyed laboratories conducted for Cryptosporidium spp. testing on samples based on one or more selection criteria, including stool consistency (19% [16 of 85]), patient age (21 % [18 of 85]), history or clinical details (47 % [40 of 85]), duration of hospitalization (21% [18 of 85]), or clinician requests (29 % [25 of 85]), prompting further revision of UK national standards to encourage testing of all submitted samples (Chalmers et al., 2015).
Owing to higher prevalence of Cryptosporidium in children, patient age is currently used as the primary selection criterion for Cryptosporidium testing within the UK and Ireland (Chalmers and Davies, 2010). It is widely acknowledged that age bias impacts on the reported age distribution rates of a variety of pathogens, including Cryptosporidium. Adding to this bias are parental and health care professional behaviours towards gastrointestinal symptoms and stool samples collection, respectively, leading to higher reporting of Cryptosporidium cases in children than in adults (Garvey and McKeown, 2009). There also remains a wide-scale lack of standardisation in clinical Cryptosporidium detection practices both within and between nations, and comparative information is particularly limited (Manser et al., 2014).
In Ireland, a 2004 report by the Health Protection Surveillance Centre in Ireland (HPSC) recommended the testing of all stool samples from patients exhibiting clinical symptoms associated with cryptosporidiosis (Health Protection Surveillance Centre, 2004). However, should resource and logistical constraints prohibit this, it is recommended that all patients under the age of 10 be screened as an alternative, with a comparable age threshold of 15 advised in a similar UK report (Crook et al., 2002). It is important to note, however, that should such an age threshold be employed, it should only be applied for the investigation of sporadic cases rather than in outbreak situations. A study of a 2007 outbreak in Galway, in the Republic of Ireland concluded that 40% of all infections occurred in patients over the age of 15. Thus, it appears likely that laboratories using such thresholds also fail to detect a large proportion of sporadic cases (Pelly et al., 2007).
In many countries, such as the United States and France, Cryptosporidium screening is not a routine component of standard “ova plus parasite” examinations carried out in clinical laboratories regardless of patient age, clinical and epidemiological evidence, unless specifically requesting by a clinician or recommended by the laboratory directorate. Thus, further contributing to the under reporting of cases (ANOFEL Cryptosporidium National Network, 2010; Chen et al., 2002). Meanwhile, a recent European survey of 18 laboratories found noteworthy variety between detection methods with almost all laboratories relying upon microscopic methods either alone or in combination with other detection methods. Half of all laboratories surveyed used at least two methods of detection, only two of which employed molecular diagnostics (Manser et al., 2014).
Expertise in the field of stool microscopy is declining among the modern clinical laboratory workforce, particularly in areas of decreasing prevalence of faecal parasites (McHardy et al., 2014). While a number of studies have reported that molecular methods are employed by only a minority of routine clinical microbiology laboratories in Europe and the US (Chalmers and Davies, 2010; Fournet et al., 2013; Jones et al., 2004; Manser et al., 2014; ten Hove et al., 2007), the growing acceptance of molecular methods and increasing throughput of samples has prompted the necessity for automated, walk-away technology in these laboratories.
Additionally, given the low prevalence of Cryptosporidium within the population in developed countries at least, certain laboratories may not receive adequate levels of positive samples to establish and maintain expertise in this area (McHardy et al., 2014). Consequently, although microscopy is currently regarded as the gold standard in the diagnosis of cryptosporidiosis, it seems likely that molecular methods will eventually replace microscopy altogether.
A summary of the advantages and disadvantages associated with the various diagnostic methods discussed herein are outlined in Table 1.
Table 1.
Advantages and disadvantages of microscopic, immunological and molecular diagnostic methods for Cryptosporidium spp.
| Diagnostic Test | Advantages | Disadvantages |
|---|---|---|
| Microscopy |
|
|
| Immunoassay based methods |
|
|
| Molecular/Nucleic acid amplification methods |
|
|
2.1. Brightfield and fluorescent microscopy
Faecal investigation for the presence of shed oocysts or antigens is the diagnostic mainstay in Cryptosporidium detection (Manser et al., 2014). Conventional clinical diagnosis has largely relied on microscopic examination of tinctorially or fluorescently stained faecal smears. The acid-fast properties of Cryptosporidium were demonstrated in 1981, with the development of a modified Ziehl-Neelson (mZN) stain for differential staining (Henricksen and Pohlenz, 1981). Prior to this Cryptosporidium was largely identified through Giemsa staining of histological preparation of intestinal biopsy samples, with iodine, trichrome and iron haematoxylin stained faecal specimens yielding poor results (Kissinger, 2008; McNabb et al., 1985).
A variety of stains including the acid-fast Kinyoun’s stain and differential stains such as the hot safrinin-methylene blue stain have also been employed by clinical laboratories (Baxby et al., 1984; Kageruka et al., 1984). In addition, a variety of negative and fluorescent stains have been developed. Both staining techniques provide a rapid, inexpensive, sensitive alternative to the acid-fast techniques (Casemore et al., 1985; Garcia et al., 1983; Hanscheid et al., 2008; Khurana et al., 2012; Vohra et al., 2012). Despite this, acid-fast staining, particularly the mZN technique, predominates in clinical laboratories (Manser et al., 2014). However, although there is a marked contrast between the red stained oocyst against the green background counterstain of the mZN, yeasts, fungal and bacterial spores may be erroneously identified as oocysts (Casemore, 1991). Intermittent oocyst shedding is inherent to the Cryptosporidium life cycle. Thus, in order to improve diagnostic sensitivity, faecal specimens are often collected over three different days, adding to the laboratory workload (Goñi et al., 2012; van Gool et al., 2003). Overall, this time consuming and tedious staining technique demands an experienced microscopist, but exhibits poor sensitivity (37-100%) (Abou El-Naga and Gaafar, 2014; Chalmers et al., 2011; Kaushik et al., 2008; Tuli et al., 2010; Zaglool et al., 2013).
Unsurprisingly, given the variable levels of sensitivity associated with brightfield and fluorescent staining techniques, a number of oocyst concentration methods have been developed in order to maximise oocyst yields from faecal samples (Garcia et al., 1983; Weber et al., 1991). These techniques are most useful when preserved stool specimens are received in epidemiological cases, asymptomatic cases, and in immunocompromised patients with a clinical history of unexplained diarrhoea, as this patient population is susceptible to recrudescence following periods of remission (Casemore, 1991; Omoruyi et al., 2014).
Although faecal staining methods remain the cornerstone of parasitological investigations in both American and European clinical laboratories, these methods were previously surpassed by a variety of immunological and most significantly, molecular identification methods (Jones et al., 2004; Manser et al., 2014). Cryptosporidium targeting, immunofluorescent monoclonal antibodies (MAb) were initially introduced almost three decades ago following the advent of hybridoma technology, which allowed for the generation of highly specific antibodies (Milstein, 1999; Sterling and Arrowood, 1986). Monoclonal oocyst wall antibodies have been conjugated with fluorescent labels such as fluorescein isothiocyanate (FITC) and biotin hydrazide, which imparts a distinct apple green-to-yellow fluorescence to the oocysts against a dark background, allowing visualisation of intact parasites (Arrowood and Sterling, 1989; Garcia et al., 1987; Sterling and Arrowood, 1986). Comparative studies have found the sensitivity and specificity of immunofluorescent techniques to outweigh the sensitivity and specificity exhibited by conventional brightfield staining techniques (Alles et al., 1995; Arrowood and Sterling, 1989; Current and Garcia, 1991; Elsafi et al., 2014; Garcia et al., 1992; Kamal et al., 2008). Additionally, indirect immunofluorescent techniques, although requiring an additional incubation step, have been reported to possess similar levels of sensitivity and specificity to those of their direct counterparts (Rusnak et al., 1989; Stibbs and Ongerth, 1986).
While immunofluorescent detection of Cryptosporidium spp. necessitates the use of a fluorescent microscope, which has prevented widespread utilisation of this method and may preclude the use of this technique in developing countries, the marked distinction of oocysts from the non-fluorescent background conveniently reduces the amount of time required for microscopic investigation (Vohra et al., 2012). In addition, faecal concentration is not a prerequisite when faecal samples contain a paucity of oocysts, given the sensitivity of this method (Elsafi et al., 2014). Immunofluorescence enhances the ease with which less experienced microscopists can definitively identify the presence of oocysts (Alles et al., 1995; Garcia et al., 1987).
2.2. Enzyme immunoassays (EIA), ELISA and immunochromatographic methods
Faecal-antigen diagnostic techniques have been developed in order to obviate the need for skilled microscopists, laborious methodologies and specialised equipment, such as fluorescent microscopes, while also accommodating batch testing requirements (Helmy et al., 2014; Rosenblatt and Sloan, 1993; Ungar, 1990). Indeed, the colorimetric principles underlying quantitative enzyme immunoassays (EIA) and enzyme linked immuno-sorbent assays (ELISA) eliminate the requirement for extensive microscopy training of lab personnel and subjectivity associated with conventional microscopy (Goñi et al., 2012; Newman et al., 1993). Comparative studies investigating the diagnostic utility of EIA and ELISA kits have found that they provide significantly improved sensitivity (94 - 100%) and specificity (93 -100%) over conventional acid-fast staining methods (Kehl et al., 1995; Parghi et al., 2014; Siddons et al., 1992). However, comparisons between fluorescent and immunofluorescent staining methods have indicated enzyme-based immunological detection of Cryptosporidium to be inferior, with reduced capabilities of detecting low oocyst densities (Johnston et al., 2003; Kehl et al., 1995; Newman et al., 1993; Weitzel et al., 2006). In addition, several cases detailing the generation of false positive results by the ProSpect Cryptosporidium immunoassay (Alexon, Inc., Mountain View, California) have been reported, perhaps owing to faecal antigen shedding often persisting after intact oocyst shedding has abated (Doing et al., 1999; Johnston et al., 2003; Miller and Mojica, 1999).
Immunochromatographic kits provide a detection system that surpasses enzyme-based methods in terms of rapidity by eliminating the need for additional reagent additions, washing steps and incubations (Current and Garcia, 1991; Garcia et al., 2003). Antigen migration via capillary action allows detection of Cryptosporidium antigens by a discrete, colloidal dye labelled antibody impregnated in a line assay, permitting objective antigen detection (Llorente et al., 2002). Sensitivities and specificities of these qualitative faecal-antigen kits vary considerably, with one study which investigated four kits reporting ranges of 47 - 71 % and 98 - 100%, respectively, when compared to microscopy (Agnamey et al., 2011). Meanwhile three independent studies reported sensitivities and specificities of 98% and 100%, 98% and 100%, 100% and 99%, respectively, in immunochromatographic kits. In each study the immunochromatographic kits in question were compared to microscopy, EIA and ELISA, respectively (Chan et al., 2000; Garcia and Shimizu, 2000; Youn et al., 2009).
Like their enzyme-based counterparts, immunochromatographic kits have been found to generate false positive results, resulting in one case, for example, in a lot recall of the CoulorPACTM Cryptosporidium/Giardia rapid assay kit (Haupst and Davis, 2002). Immunoassay based kits also offer a reduced diagnostic spectrum, as many are tailored solely for the detection of C. parvum and C. hominis. Therefore the clinical utility of such kits is limited in regions where alternative Cryptosporidium species are attributable to a significant number of cryptosporidiosis cases (Agnamey et al., 2011; Llorente et al., 2002). Consequently, despite the logistical and economical improvements in assay methodology over conventional staining methods, enzyme and non-enzyme based immunoassays are not deemed to be a suitable substitution for such techniques in the modern clinical laboratory, even though they may be used as a confirmatory adjunct to conventional methods in clinical laboratories with limited experience in Cryptosporidium detection, or for epidemiological studies (Checkley et al., 1997; Goñi et al., 2012; Hanson and Cartwright, 2001; Weitzel et al., 2006).
2.3. Molecular approaches
Following its inception in 1983, the polymerase chain reaction (PCR) has vastly improved molecular diagnostic approaches in many fields, including clinical microbiology (Espy et al., 2006; Tong and Giffard, 2012). PCR detection of Cryptosporidium has been proven to be more sensitive than conventional microscopic and immunological methods, while also permitting batch testing, species and sub-species identification of detected organisms (Chalmers et al., 2011; Elsafi et al., 2013; Aghamolaie et al., 2016; Uppal et al., 2014).
A sequence survey identifying >250 kb of the C. parvum genome heralded the beginning of the genomic era of Cryptosporidium research in the late 1990s (Liu et al., 1999). Given the clinical significance and the dearth of epidemiological and molecular Cryptosporidium data at the time, the National Institute of Allergy and Infectious Diseases (NIAID) subsequently allocated funding to a consortium of three American universities, which were tasked with sequencing both C. parvum and C. hominis genomes (Widmer and Sullivan, 2012). Two separate studies, undertaking whole genome shotgun sequencing strategies, subsequently yielded the fully sequenced genomes of C. parvum IOWA and C. hominis TU502 isolates (Abrahamsen et al., 2004; Xu et al., 2004).This research ultimately led to the establishment of CryptoDB in 2003, an online database of known Cryptosporidium genomes (Heiges et al., 2006; Puiu et al., 2004). This collaborative effort integrates all genomic and functional genomic data pertaining to Cryptosporidium spp. in a single online, bioinformatics resource. At present, CryptoDB houses 15 genome sequences encompassing nine different species/genotypes, while 52 genome assemblies are available for the Cryptosporidium genus in the NCBI GenBank (Baptista et al., 2021). These genomic advances have paved the way for current epidemiological studies, functional analyses, protein and metabolic pathway predictions and genome annotation (Isaza et al., 2015; Mazurie et al., 2013).
In the initial advent of molecular techniques, characterisation of Cryptosporidium genotypes was largely achieved through PCR-mediated amplification of specific genetic regions, followed by enzymatic cleavage or sequencing (Cheun et al., 2013; Ibrahim et al., 2021; Insulander et al., 2013; Sulaiman et al., 2005). Prior to the C. hominis and C. parvum whole genome sequencing projects and the widespread availability of DNA sequencing techniques, RFLP was the primary means by which to conduct inter-species genotyping on Cryptosporidium spp. (Awad-el-Kariem et al., 1994; Leng et al., 1996). This technique utilises a number of key molecular markers amenable to PCR amplification and restriction digestion to produce unique banding patterns that are visualised via gel electrophoresis (Roellig and Xiao, 2020). However, RFLP based genotyping is limited in that it cannot resolve differences between isolates of the same genotype, particularly C. hominis and C. parvum, necessitating an alternative sub-genotyping technique (Roellig and Xiao, 2020).
The C. parvum and C. hominis genome sequencing projects enabled the identification of a number of highly polymorphic micro- and minisatellite loci and conserved loci flanking sequences (Aiello et al., 1999; Cacciò et al., 2000; Feng et al., 2000). These sequences permitted the development of microsatellite and minisatellite locus-specific PCR assays for both species regions, thereby permitting genotyping superior to that of RFLP, and ultimately the development of a technique that is also capable of identifying the subtleties of intra-species differentiation (Ramo et al., 2015; Xiao and Feng, 2017).
Key molecular markers for species identification include the small sub-unit rRNA (SSU rRNA), Cryptosporidium outer wall protein (COWP), 70-kDa heat shock protein (HSP70), thrombospondin-related adhesive protein (TRAP-C2) and actin genes (Roellig and Xiao, 2020; Elwin et al., 2013; Hadfield et al., 2011). These regions contain large numbers of interspecific polymorphisms, which make them ideal for basic species identification. Owing to low levels of intraspecific variation, the SSU rRNA gene is the most widely used of these genetic targets in genotypic differentiation between an array of human and animal infecting species (de Lucio et al., 2016; Roellig and Xiao, 2020). Highly variable regions, such as the tandem repeat containing 60-kDa glycoprotein (gp60) gene and the microsatellite loci, ML1 and ML2, are predominantly used for this purpose given the marked amount of intra-species sequence heterogeneity expressed in these regions (Robinson and Chalmers, 2012). These regions have been pivotal in the determination of the extensive number of C. parvum and C. hominis sub-species. Extensive panels including these markers, among many others, are commonly employed in multi-locus sequence typing (MLST) based epidemiological studies to identify population structures, and inter- and intra-species genetic diversity (De Waele et al., 2013; Feng et al., 2014; Garcia-R et al., 2020; Wang et al., 2015; Xiao, 2010).
Within the Cryptosporidium genus and more specifically among the predominant human-pathogenic species, C. parvum and C. hominis, asexual and sexual life cycle stages, genetic recombination and selective pressures, such as parasite-host coevolution, host adaptation and geographic segregation, have led to generation of new subtype families and diverse genetic populations (Abal-Fabeiro et al., 2013; Feng et al., 2002; Garcia-R and Hayman, 2017). gp60, which is firmly established as a key marker of genetic variation within Cryptosporidium spp (Abal-Fabeiro et al., 2013), is subject to selective pressure which has resulted in a lack of global sub-structuring, with the same gp60 alleles emerging in different locations globally (Abal-Fabeiro et al., 2013; Widmer, 2009). Thus, gp60 is not a sufficient descriptor of population structure to enable single locus typing (Robinson and Chalmers, 2012). Multi-locus genotyping (MLG) is necessary to adequately assess genetic variation and population structures within Cryptosporidium spp.
Research is ongoing into the identification of novel genetic markers, and refining known markers into an internationally standardised MLG scheme (Chalmers et al., 2018). Population-level analyses (nucleotide diversity (θπ) and Watterson’s theta (θW), Tajima’s D statistic etc.) have been used in several studies seeking to assess genetic diversity and evolutionary processes at multiple loci within Cryptosporidium spp. in order to aid understanding of host-parasite adaptation and evolution (Garcia-R et al., 2020; Garcia-R and Hayman, 2017). MLG, accomplished via DNA sequencing of PCR amplified amplicons from specific loci, or real-time PCR based high resolution melting analysis of loci amplicons, is also being evaluated for epidemiological surveillance and outbreak investigations in clinical laboratories (Chalmers et al., 2017; O'Leary et al., 2021a, O'Leary et al., 2021b).
Overall, several studies have recommended the incorporation of PCR techniques into routine clinical Cryptosporidium diagnosis methods (Rubio et al., 2014; Stensvold et al., 2011; Uppal et al., 2014). Indeed, PCR has been reported as having improved sensitivity over current detection methods, with reported limits of detection ranging from 1 × 105 to 1 oocyst/Gram of faeces (Costa et al., 2021). This is a significant improvement in detection when compared to the limit of detection associated microscopy based detection, which requires between 1 × 104 – 5 × 104 oocysts per mL of faeces (Khurana and Chaudhary, 2018). Although promising results have been reported, standard PCR techniques, particularly nested PCR, are not ideally suited to routine human diagnostics as they have been associated with considerable contamination risks, owing to multiple rounds of DNA amplification and concomitant DNA manipulation steps.
The development of real-time PCR (or quantitative PCR, qPCR) offers a convenient alternative to conventional techniques. Completed within an hour or less, qPCR reaction times are superior to those seen in conventional PCR methods (Espy et al., 2006). Fluorescent probes are used to detect DNA amplification, while the closed reaction vessel ensures that contamination is comparably negligible to that associated with conventional PCR (Espy et al., 2006; Minarovičová et al., 2009). In addition, sensitivity and specificity levels equal to, or surpassing, those observed in conventional PCR have been reported (Elsafi et al., 2013; Hadfield et al., 2011; Liu et al., 2013). Table 2 provides a comparison between reported sensitivities and specificities of common microscopic methods versus currently available commercial immunological and DNA-based diagnostic panels.
Table 2.
Sensitivities and specificities of microscopic methods, and currently available immunological and DNA-based diagnostic tests for Cryptosporidium spp.
| Microscopic Staining Techniques | |||
|---|---|---|---|
| Test Name | Sensitivity | Specificity | Reference |
| mZiehl-Neelsen stain | 37–79.1% | 100% | Chalmers et al. (2011); Kaushik et al. (2008); Khurana et al. (2012) |
| Fluorescent – auramine phenol stain | 92.1 –100% | 99.6–100% | Abou El-Naga and Gaafar (2014); Chalmers et al. (2011); Khurana et al. (2012) |
| Kinyoun’s acid fast stain | 66.7–91.6% | 88.2–100% | Abou El-Naga and Gaafar (2014); Elsafi et al. (2014) |
| Commercial Immunological Diagnostic Tests for Cryptosporidium spp. | |||||
|---|---|---|---|---|---|
| Test Name | Sensitivitya | Specificitya | Additional Pathogens Detected | Supplier | Reference |
| Crypto-Strip | 47.2% | 100% | N/A | Coris BioConcept, Gembloux, Belgium | Agnamey et al. (2011) |
| Cryptosporidium and Giardia Duo-Strip | 91.7% | 100% | Giardia duodenalis | Coris BioConcept, Gembloux, Belgium | Van den Bossche et al. (2015) |
| Cryptosporidium EZ VUE lateral-flow test strips | 89% | 99% | N/A | TechLab Inc., Blacksburg, Virginia, United States | Johansen et al. (2021) |
| Cryptosporidium II test | 71.8% | 94.3% | N/A | TechLab Inc., Blacksburg, Virginia, United States | Kabir et al. (2018) |
| Giardia/Cryptosporidium Quik Chek | 92.3–100% | 97.1–100% | G. duodenalis | TechLab Inc., Blacksburg, Virginia, United States | Chalmers et al. (2011); Van den Bossche et al. (2015); Kabir et al. (2018); Minak et al. (2012) |
| ImmunocardSTAT® C/ G | 5.5–96% | 96.6–100% | G. duodenalis | Meridian Bioscience Inc., Cincinnati, Ohio, United States | Agnamey et al. (2011); El-Moamly and El-Sweify (2012); Bouyou-Akotet et al. (2016) |
| ImmunoCard STAT!® CGE | 100% | 45.6–100% | G. duodenalis, and Entamoeba histolytica | Meridian Bioscience Inc., Cincinnati, Ohio, United States | Van den Bossche et al. (2015) |
| RIDA®QUICK | 62.4–84.9% | 98% | N/A | R-Biopharm Diagnostic, Darmstadt, Germany | Agnamey et al. (2011); Chalmers et al. (2011) |
| RIDA®QUICK Combi | 60.4–100% | 100% | G. duodenalis, and E. histolytica /dispar | R-Biopharm Diagnostic, Darmstadt, Germany | Van den Bossche et al. (2015); Helmy et al. (2014) |
| Remel ProSpecT | 91.4% | 100% | G. duodenalis | ThermoScientific, Waltham, Massachusetts, United States | Chalmers et al. (2011) |
| Remel-Xpect | 68.8% | 100% | N/A | ThermoScientific, Waltham, Massachusetts, United States | Agnamey et al. (2011) |
| Commercial Molecular Diagnostic Tests for Cryptosporidium spp, | |||||
|---|---|---|---|---|---|
| Test Name | Sensitivitya | Specificitya | Additional Pathogens Detected | Supplier | Reference |
| AllplexTM Gastrointestinal Panel-Parasite Assay (GIPPA) | 100% | Up to 100% – further testing needed. | G. duodenalis, E. histolytica, Dientamoeba fragilis, B. hominis, and Cyclospora cayetanensis | Seegene Inc, Seoul, Korea | Autier et al. (2020); Paulos et al. (2019) |
| Amplidiag® Stool Parasites | 103 oocysts/g | Not specified | G. duodenalis, E. histolytica, and D. fragilis | Mobidiag, Espoo, Finland | Costa et al. (2021) |
| BD Max parasitic panel (EPP) | 95.5% | 99.6% | G. duodenalis, and E. histolytica | BD Diagnostics, Sparks, Maryland, United States | Madison-Antenucci et al. (2016); Mölling et al. (2016) |
| Biofire FilmArrayTM Gastrointestinal Panel | 100% | 99.6–100% | 14 bacterial and 5 viral targets. 3 further parasites: G. duodenalis, E. histolytica, and C. cayetanensis | BioFire Diagnostics, Salt Lake City, Utah, United States | Murphy et al. (2017); Binnicker (2015); Khare et al. (2014); Zhang et al. (2015) |
| EasyScreenTM Enteric Parasite Detection Kit | 100% | 100% | G. duodenalis, Entamoeba complex; D. fragilis, and Blastocystis spp. | Genetic Signatures, Sydney, Australia | Stark et al. (2014) |
| EntericBio GastroPanel II | 100% | 100% | 4 bacterial targets and G. duodenalis | Serosep. Limerick, Ireland | McAuliffe et al. (2017) |
| FTD Stool Parasites | 53.1% | Up to 100% – further testing needed. | Giardia spp, and E. histolytica | Fast Track Diagnostics, Esch-sur-Alzette, Luxembourg | Paulos et al. (2019) |
| Gastroenteritis/Parasite Panel I | 92–100% | Up to 100% – further testing needed. | G. duodenalis, and E. histolytica | Diagnode, Seraing, Belgium | Paulos et al. (2019) |
| Luminex xTAG® Gastrointestinal Pathogen Panel | 95–100% | 100% | 12 bacterial and viral targets and 2 further parasites: G. duodenalis and E. histolytica | Luminex Corporation, Austin, Texas, United States | Patel et al. (2014); Wessels et al. (2014); Claas et al. (2013); Navidad et al. (2013); Perry et al. (2014); Zhang et al. (2015) |
| NanoCHIP® Gastrointestinal Panel (GIP) |
Detection limit of 5 x 103 oocysts | Up to 100% – further testing needed. | 3 bacterial targets and G. duodenalis, E. histolytica, E. dispar, D. fragilis, and Blastocystis hominis | Savyon Diagnostics, Ashdod, Israel | Dror et al. (2016) |
| ParaGENIE Crypto-Micro PCR | 91.7% | 100% | Also differentiates between Enterocytozoon bieneusi and Encephalitozoon intestinalis | Ademtech, Pessac, France | Morio et al. (2019) |
| RIDA®GENE Parasitic Stool Panel | 87.5% | Up to 100% – further testing needed. | G. duodenalis, E. histolytica, and D. fragilis | R-Biopharm Diagnostic, Darmstadt, Germany | Paulos et al. (2019) |
| QIAStat Dx® GIP | Not specified | Not specified | 14 bacterial targets, 6 viral targets and 3 further parasites: G. lamblia, E. histolytica, and C. cayetanensis |
Qiagen, Hilden, Germany | Boers et al. (2020) |
aSensitivity and specificity for Cryptosporidium spp. only are given here. Variable sensitivities and specificities reported for other pathogens detection by these panels.
Multiplex PCR has become a popular means by which to investigate the presence of multiple enteric parasites in a single sample. Initial studies found multiplex qPCR assays to be both 100% sensitive and specific when compared to the monoplex qPCR assays, with superior sensitivity and specificity over conventional microscopic methods for each of the protozoan parasites tested (Stark et al., 2011). This technology continues to increase in popularity for use in clinical laboratories, with in excess of 10 enteric pathogen-targeting commercial multiplex qPCR kits currently available, including Allplex, Amplidia, BD Max, Biofire FilmArray, FTD Stool Parasites, Gastro Panel EntericBio Panel II, Gastroenteritis/Parasite Panel I, Luminex, NanoChip, PARAGenie, RIDAGENE, and QIAstat (Table 2) (Autier et al., 2020; Boers et al., 2020; Morio et al., 2019; Hannet et al., 2019; O'Leary et al., 2018; Ryan et al., 2017; Paulos et al., 2019). In addition, multiplex assays significantly reduce reagent and labour costs, and outperform the majority of alternative methods currently in use (Haque et al., 2007; Stark et al., 2011; ten Hove et al., 2007; Verweij and Van Lieshout, 2011). qPCR also readily accommodates genotyping via melting curve analysis, and more recently high resolution melting (HRM) curve analysis (Chelbi et al., 2018; Lalonde et al., 2013; O'Leary et al., 2021a, O'Leary et al., 2021b).
While appearing to offer a myriad of diagnostic and logistical advantages, conventional PCR and qPCR have not yet been widely incorporated into routine Cryptosporidium detection procedures. This is likely to be due, at least in part, to the requirement for significant investment in reagents and analysers, coupled with extensive personnel training (Burnet et al., 2013; Checkley et al., 2014). However, a future molecular shift in the field of diagnostic parasitology would appear to be inevitable in order to provide essential improvement to current diagnostic services. Thus, the potential benefits must be carefully weighed against the perceived disadvantages associated with molecular methods in the context of current diagnostic limitations.
2.4. Future trends in molecular platforms
In recent years a third-generation implementation of conventional PCR that obfuscates the need for calibration curves in the quantification of nucleic acid targets, digital PCR (dPCR), has been gaining traction for its utility in pathogen detection. The method, which is based on the principle of amplifying a single DNA template from maximally diluted samples, therefore generating amplicons that are exclusively derived from one template, based on Poisson statistics, remains a relatively new concept in the field of medical parasitology (Pomari et al., 2019). Unlike qPCR, which produces an exponential signal, dPCR generates linear, digital signals, allowing quantitative analysis of the PCR product, detecting very rare mutations with unprecedented precision and sensitivity (Pohl and Shih, 2004). As of yet, application of dPCR to the detection and quantification of Cryptosporidium in human faecal samples is limited to a single study (Yang et al., 2014). However, despite this, the reported precision of dPCR is consistently superior to that of qPCR, and the quantitative detection less affected by the presence of inhibitors. Thus, the initial application of dPCR to the detection and quantification of Cryptosporidium oocysts by Yang et al. (2014) may herald its incorporation into mainstream clinical diagnostic methodologies over the coming years.
The emergence and increasing prevalence of next generation sequencing (NGS) technologies is also likely to shape the field of protozoan parasitology over the course of the coming decade, (DeMone et al., 2020). Evaluations of Cryptosporidium isolates with NGS techniques have revealed unprecedented within-isolate genetic diversity to a degree that is not possible to discern through current conventional PCR and Sanger sequencing-based subtyping methodologies, given their inability to resolve complex DNA mixtures and detect low-abundance intra-isolate variants (Grinberg et al., 2013; Grinberg and Widmer, 2016; Zahedi et al., 2017). Consequently, NGS-based studies have already advanced current knowledge on the taxonomic distribution and transmission dynamics of Cryptosporidium spp., and may also play a future role in outbreak identification and surveillance of new and virulent subtypes (Zahedi et al., 2018; Zahedi et al., 2017).
Despite difficulties in extracting high quality pure DNA from clinical samples, issues with uneven depth of read coverage that leads to gaps in the assembled genome sequence, all of which impact cost and may preclude the widespread use of NGS platforms in clinical laboratories and Public Health agencies; NGS remains likely to exert an important, indirect impact on clinical diagnostics through informing the development of much needed multi-locus sequence typing (MLST) schemes (Cacciò and Chalmers, 2016; Morris et al., 2019). Furthermore, NGS will also undoubtedly play an increasingly pivotal role in epidemiological analyses of Cryptosporidium spp., in addition to vaccine and drug development, over the coming decade (Morris et al., 2019; Zahedi et al., 2017).
It would be imprudent to ignore the role of the rapidly-developing fields of bioinformatics and proteomics in this post-genomic era. Efforts to integrate biochemical and genomic data have led to the development of predictive computational models, known as GEMs (genome scale models), for a number of microorganisms in recent years. These models utilise genomic and environmentally based parameters to predict phenotypic outcomes and growth based on biochemical mechanisms (Monk and Palsson, 2014). This is a concept that has already been put into practice for well characterised microorganisms, such as E. coli (Carrera et al., 2014), while attempts to develop a genome scale metabolic model of C. hominis have already been reported (Vanee et al., 2010). Given the fact that the genomes of both C. parvum and C. hominis have been fully sequenced, and in light of the studies carried out by Vanee et al. (2010), it is conceivable that GEMs may soon be employed to predict the phenotypic outcome of genetic variations in Cryptosporidium species (Vanee et al., 2010; Vinayak et al., 2015).
3. Treatment limitations, propagation via cell culture, and implications for future advancements
To date, Cryptosporidium has remained a largely enigmatic pathogen, owing to its limited tractability and the difficultly encountered in successfully propagating the parasite in vitro in cell lines (Karanis and Aldeyarbi, 2011). In vitro culture efforts generally result in low yields of mature parasites, as current Cryptosporidium cell culture methods generally suffer from rapid host cell overgrowth and ageing, resulting in premature termination of the Cryptosporidium lifecycle (Hijjawi, 2010). Normal intestinal epithelial cell (IEC) models fail to adequately recapitulate human intestinal structure and function. Support of parasitic infection by these and immortalised adenocarcinoma derived human IEC models is generally limited to only a few days, precluding parasitic life-cycle completion or continuous propagation (Bhalchandra et al., 2018).
Lack of suitably facile animal models, and molecular tools have also hampered progress in key areas such as developmental biology, the elucidation of host-parasite interactions, biochemical, immunological and molecular studies development, and, perhaps most significantly, evaluation and development of effective anti-cryptosporidial drug therapies (Di Cristina and Carruthers, 2018; Hijjawi et al., 2001). Nitazoxanide, a broad spectrum antimicrobial agent, is currently the only FDA approved treatment for cryptosporidiosis in patients 1 year and older (Sparks et al., 2015). Three double-blind placebo controlled studies suggest the efficacy of nitazoxanide in immunocompetent patients (Amadi et al., 2002; Rossignol et al., 2001, Rossignol et al., 2006). Nitazoxanide, however, is not without considerable limitations in its utility among patient populations that are most vulnerable to Cryptosporidium infection. A study conducted on malnourished children found nitazoxanide to improve diarrhoea and morality rates, but the response rate was limited to 56% of studied patients (Amadi et al., 2002). Nitazoxanide has also been found to be ineffective in AIDS patients (Amadi et al., 2009), while various other drugs such as paromomycin, azithromycin, rifamycin, and HIV protease inhibitors have also been unsuccessful in the treatment of cryptosporidiosis in AIDS patients (Checkley et al., 2014; Sparks et al., 2015).
The pursuit of an optimal in vitro culture system for Cryptosporidium has spanned four decades, with the first complete development of C. parvum reported in human, and porcine cell line models in 1984 (Current and Haynes, 1984). In recent years a variety of both cell-free and axenic culture-based systems have yielded promising results. Key milestones in the drive to develop a suitable cell culture-based in vitro model have also been published in the past decade (Alcantara Warren et al., 2008; Castellanos-Gonzalez et al., 2008). More recent advancements have sought to extend periods of culture survival (Castellanos-Gonzalez et al., 2013; Jossé et al., 2019; Karanis, 2018; Miller et al., 2018; Varughese et al., 2014). Hollow fibre technologies and stem-cell derived organoids, have also provided a basis for sustained in-vitro oocyst propagation (Morada et al., 2016). The development of a system employing stem-cell derived small intestinal, and lung organoids, capable of recapitulating the in vivo physiology of their original tissues, to model Cryptosporidium infection has been described. These organoids support propagation and completion of the parasitic life-cycle, generating infectious oocysts equivalent to those derived from animal models (Dutta et al., 2019; Heo et al., 2018).
Advancements in cell culturing methodologies have enabled several compound screening studies to be conducted. These screening studies have yielded promising potential anti-cryptosporidial compounds. A HCT-8 cell-based, high-throughput screen (HTS) of the Medicines for Malaria (MMV) Open Access Malaria box, a collection of 400 compounds selected from 19,000 structurally unique molecules that were shown to have activity against the Plasmodium falciparum, was conducted by Bessoff et al. (2014) and identified several scaffold structures with activity against C. parvum. Another study screened a bank of over 6,000 compounds known to exhibit anti-protozoan activity via a high-content imaging infection assay in HCT-8 cells resulting in the identification of the Cryptosporidium orthologue to Plasmodium lipid kinase PI(4)K, Cryptosporidium lipid kinase PI(4)K, as a potential target for pyrazolopyridines based therapeutic candidates (Manjunatha et al., 2017).
Most significantly, however, is the recent application of the CRISPR/Cas system genome editing technology to Cryptosporidium. In a major breakthrough for Cryptosporidium in vitro research, Vinayak et al. (2015) harnessed the CRISPR/Cas system, to successfully transfect C. parvum sprozoites in tissue culture and subsequently isolate genetically modified C. parvum sporozoites. Such a demonstration of genetically modified Cryptosporidium sporozoites was the first of its kind, paving the way for the development of subsequent parasite survival assays that are furthering contemporary understanding of the basic biology and virulence of this pathogen, and tractable in vivo models (Pawlowic et al., 2019; Sateriale et al., 2019; Vinayak et al., 2015).
Similar to the advances made in NGS technologies, future applications of CRISPR/Cas systems may result in far reaching implications and advancements in diverse areas of Cryptosporidium research. For example, given the severe limitations associated with current treatment options, the recent advancements employing the aforementioned CRISPR/Cas9 genetic modification of C. parvum may prove critical in the development of vaccines and more effective drug therapies, particularly given the utility of gene ablation in identifying alternative treatment strategies (Doudna and Charpentier, 2014; Vinayak et al., 2015). Additionally, the recent incorporation of the CRISPR/Cas12a system within a fluorescent lateral flow strip biosensor tailored for on-site diagnosis of Cryptosporidium parvum subtype family IId demonstrates the clinical potential and diagnostic utility of CRISPR/Cas system in Cryptosporidium detection (Yu et al., 2021).
4. Concluding remarks
The 2015 Nobel Prize in Physiology or Medicine is a pertinent reminder of the importance and necessity for continued research in the field of parasitology. The work of Tu Youyou and the combined efforts of William C. Campbell and Satoshi Ōmura were recognised for the discoveries made concerning the development of novel therapies for malaria, a parasite also of the apicomplexan phylum, and roundworm, respectively (Długońska, 2015). Such high profile recognition in the field of parasitology is arguably suggestive of a resurgence of interest in the field, which has stagnated somewhat in terms of clinical, therapeutic and molecular diagnostic advances. The renaissance of Cryptosporidium research is already underway; the major breakthrough in producing CRISPR/Cas modified, tractable C. parvum oocysts signifies a reinvigoration of the field. This advancement is likely aid the advancement of knowledge in areas such as host-parasite interactions, and the biochemical and immunological pathways at play within Cryptosporidium spp. It will also facilitate the identification and validation of much needed drug targets.
It is also crucial to note that the causative agent remains undetected in 70% of gastroenteritis cases. Advances in diagnostic approaches for Cryptosporidium spp., and parasitic species in general, may play a significant role in further elucidating the nature of this unknown, and potentially diverse, pathogenic conglomerate (Freedman et al., 2015). This is particularly relevant in light of the human and economic toll exerted by gastrointestinal infection on a global scale, which according to a recent WHO study affected 2 billion people, caused 1 billion deaths and 78.7 million disability adjusted life years in 2010 (Kirk et al., 2015). As a consequence, Cryptosporidium research has perhaps never been more pertinent than it is today.
Funding
This work was supported by the Irish Research Council [GOIPG/2014/918].
Declaration of Competing Interest
There are no conflicts of interest, of which we are aware, relating to this body of work.
Acknowledgements
The authors wish to extend our thanks to the staff of the Medical Microbiology Department of Cork University Hospital for their continued support and expertise.
References
- Abal-Fabeiro J.L., Maside X., Bello X., Llovo J., Bartolomé C. Multilocus patterns of genetic variation across Cryptosporidium species suggest balancing selection at the gp60 locus. Mol. Ecol. 2013;22:4723–4732. doi: 10.1111/mec.12425. [DOI] [PubMed] [Google Scholar]
- Abou El-Naga I.F., Gaafar M.R. Auramine-Phenol vs. modified kinyoun’s acid-fast stains for detection of coccidia parasites. Lab. Med. 2014;45:65–73. doi: 10.1309/LMS0WN7K7UKZCPMI. [DOI] [PubMed] [Google Scholar]
- Abrahamsen M.S., Templeton T.J., Enomoto S., Abrahante J.E., Zhu G., Lancto C.A., Deng M., Liu C., Widmer G., Tzipori S., Buck G.A., Xu P., Bankier A.T., Dear P.H., Konfortov B.A., Spriggs H.F., Iyer L., Anantharaman V., Aravind L., Kapur V. Complete genome sequence of the apicomplexan, Cryptosporidium parvum. Science. 2004;304:441–445. doi: 10.1126/science.1094786. [DOI] [PubMed] [Google Scholar]
- Aghamolaie S., Rostami A., Fallahi S., Tahvildar Biderouni F., Haghighi A., Salehi N. Evaluation of modified Ziehl-Neelsen, direct fluorescent-antibody and PCR assay for detection of Cryptosporidium spp. in children faecal specimens. J. Parasit. Dis. 2016;40:958–963. doi: 10.1007/S12639-014-0614-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agnamey P., Sarfati C., Pinel C., Rabodoniriina M., Kapel N., Dutoit E., Garnaud C., Diouf M., Garin J.F., Totet A., Derouin F. Evaluation of four commercial rapid immunochromatographic assays for detection of Cryptosporidium antigens in stool samples: A blind multicenter trial. J. Clin. Microbiol. 2011;49:1605–1607. doi: 10.1128/JCM.02074-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiello A.E., Xiao L., Limor J.R., Liu C., Abrahamsen M.S., Lal A.A. Microsatellite analysis of the human and bovine genotypes of Cryptosporidium parvum. J. Eukaryot. Microbiol. 1999;46:46S–47S. [PubMed] [Google Scholar]
- Alcantara Warren C., Destura R.V., Sevilleja J.E.A.D., Barroso L.F., Carvalho H., Barrett L.J., O’Brien A.D., Guerrant R.L. Detection of epithelial-cell injury, and quantification of infection, in the HCT-8 organoid model of cryptosporidiosis. J. Infect. Dis. 2008;198:143–149. doi: 10.1086/588819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alles A., Waldron M., Sierra L., Mattia A. Prospective comparison of direct immunofluorescence and conventional staining methods for detection of Giardia and Cryptosporidium spp. in human fecal Prospective Comparison of Direct Immunofluorescence and Conventional Staining Methods for Detection of. Prospect. Comp. Direct Immunofluoresc. Conv. Stain. Methods Detect. Giardia Cryptosporidium spp. Hum. Fecal Specimens. 1995;33:1632–1634. doi: 10.1128/jcm.33.6.1632-1634.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amadi B., Mwiya M., Musuku J., Watuka A., Sianongo S., Ayoub A., Kelly P. Effect of nitazoxanide on morbidity and mortality in Zambian children with cryptosporidiosis: a randomised controlled trial. Lancet. 2002;360:1375–1380. doi: 10.1016/S0140-6736(02)11401-2. [DOI] [PubMed] [Google Scholar]
- Amadi B., Mwiya M., Sianongo S., Payne L., Watuka A., Katubulushi M., Kelly P. High dose prolonged treatment with nitazoxanide is not effective for cryptosporidiosis in HIV positive Zambian children: a randomised controlled trial. BMC Infect. Dis. 2009;9:195. doi: 10.1186/1471-2334-9-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ANOFEL Cryptosporidium National Network Laboratory-based surveillance for Cryptosporidium in France, 2006-2009. Euro Surveill. 2010;15:19642. [PubMed] [Google Scholar]
- Arrowood M.J., Sterling C.R. Comparison of conventional staining methods and monoclonal antibody-based methods for Cryptosporidium oocyst detection. J. Clin. Microbiol. 1989;27:1490–1495. doi: 10.1128/jcm.27.7.1490-1495.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Autier B., Gangneux J.-P., Robert-Gangneux F. Evaluation of the AllplexTM gastrointestinal panel—parasite assay for protozoa detection in stool samples: a retrospective and prospective study. Microorganisms. 2020;8 doi: 10.3390/MICROORGANISMS8040569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awad-el-Kariem F.M., Warhurst D.C., McDonald V. Detection and species identification of Cryptosporidium oocysts using a system based on PCR and endonuclease restriction. Parasitology. 1994;109(Pt 1):19–22. doi: 10.1017/s0031182000077714. [DOI] [PubMed] [Google Scholar]
- Baptista R.P., Cooper G.W., Kissinger J.C. Challenges for Cryptosporidium population studies. Genes (Basel) 2021;12:894. doi: 10.3390/GENES12060894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxby D., Blundell N., Hart C.A. The development and performance of a simple, sensitive method for the detection of Cryptosporidium oocysts in faeces. J. Hyg. (Lond). 1984;93:317–323. doi: 10.1017/s0022172400064858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bessoff K., Spangenberg T., Foderaro J.E., Jumani R.S., Ward G.E., Hustona C.D. Identification of Cryptosporidium parvum active chemical series by repurposing the open access malaria box. Antimicrob. Agents Chemother. 2014;58:2731–2739. doi: 10.1128/AAC.02641-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhalchandra S., Cardenas D., Ward H.D. Recent breakthroughs and ongoing limitations in Cryptosporidium research. F1000Research. 2018;7:1380. doi: 10.12688/f1000research.15333.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binnicker M.J. Multiplex molecular panels for diagnosis of gastrointestinal infection: performance, result interpretation, and cost-effectiveness. J. Clin. Microbiol. 2015;53:3723–3728. doi: 10.1128/JCM.02103-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boers S.A., Peters C.J.A., Wessels E., Melchers W.J.G., Claas E.C.J. Performance of the QIAstat-Dx gastrointestinal panel for diagnosing infectious gastroenteritis. J. Clin. Microbiol. 2020;58 doi: 10.1128/JCM.01737-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouyou-Akotet M.K., Owono-Medang M., Moussavou-Boussougou M.N., Mabika Mamfoumbi M., Mintsa-Nguema R., Mawili-Mboumba D.P., Kombila M. Low sensitivity of the IMMUNOCARDSTAT® Crypto/Giardia Rapid Assay test for the detection of Giardia and cryptosporidium in fecal samples from children living in libreville, Central Africa. J. Parasit.Dis. 2016;40:1179–1183. doi: 10.1007/s12639-015-0645-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruijnesteijn van Coppenraet L.E.S., Wallinga J.A., Ruijs G.J.H.M., Bruins M.J., Verweij J.J. Parasitological diagnosis combining an internally controlled real-time PCR assay for the detection of four protozoa in stool samples with a testing algorithm for microscopy. Clin. Microbiol. Infect. 2009;15:869–874. doi: 10.1111/j.1469-0691.2009.02894.x. [DOI] [PubMed] [Google Scholar]
- Burnet J.B., Ogorzaly L., Tissier A., Penny C., Cauchie H.M. Novel quantitative TaqMan real-time PCR assays for detection of Cryptosporidium at the genus level and genotyping of major human and cattle-infecting species. J. Appl. Microbiol. 2013;114:1211–1222. doi: 10.1111/jam.12103. [DOI] [PubMed] [Google Scholar]
- Cacciò S., Homan W., Camilli R., Traldi G., Kortbeek T., Pozio E. A microsatellite marker reveals population heterogeneity within human and animal genotypes of Cryptosporidium parvum. Parasitology. 2000;120(Pt 3):237–244. doi: 10.1017/s0031182099005508. [DOI] [PubMed] [Google Scholar]
- Cacciò S.M., Chalmers R.M. Human cryptosporidiosis in Europe. Clin. Microbiol. Infect. 2016;22:471–480. doi: 10.1016/j.cmi.2016.04.021. [DOI] [PubMed] [Google Scholar]
- Carrera J., Estrela R., Luo J., Rai N., Tsoukalas A., Tagkopoulos I. An integrative, multi-scale, genome-wide model reveals the phenotypic landscape of Escherichia coli. Mol. Syst. Biol. 2014;10:735. doi: 10.15252/msb.20145108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casemore D.P. ACP Broadsheet 128: June 1991. Laboratory methods for diagnosing cryptosporidiosis. J. Clin. Pathol. 1991;44:445–451. doi: 10.1136/jcp.44.6.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casemore D.P., Roberts C. Guidelines for screening for Cryptosporidium in stools: report of a joint working group. J. Clin. Pathol. 1993;46:2–4. doi: 10.1136/jcp.46.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casemore D.P., Armstrong M., Sands R.L. Laboratory diagnosis of cryptosporidiosis. J. Clin. Pathol. 1985;38:1337–1341. doi: 10.1136/jcp.38.12.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos-Gonzalez A., Yancey L.S., Wang H.-C., Pantenburg B., Liscum K.R., Lewis D.E., White A.C. Cryptosporidium infection of human intestinal epithelial cells increases expression of osteoprotegerin: a novel mechanism for evasion of host defenses. J. Infect. Dis. 2008;197:916–923. doi: 10.1086/528374. [DOI] [PubMed] [Google Scholar]
- Castellanos-Gonzalez A., Cabada M.M., Nichols J., Gomez G., White A.C. Human primary intestinal epithelial cells as an improved in vitro model for Cryptosporidium parvum infection. Infect. Immun. 2013;81:1996–2001. doi: 10.1128/IAI.01131-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalmers R.M. Cryptosporidium: from laboratory diagnosis to surveillance and outbreaks. Parasite. 2008;15:372–378. doi: 10.1051/parasite/2008153372. [DOI] [PubMed] [Google Scholar]
- Chalmers R.M., Davies A.P. Minireview: clinical cryptosporidiosis. Exp. Parasitol. 2010;124:138–146. doi: 10.1016/j.exppara.2009.02.003. [DOI] [PubMed] [Google Scholar]
- Chalmers R.M., Thomas P.D. Laboratory ascertainment of Cryptosporidium and local authority policies for investigating sporadic cases of cryptosporidiosis in two regions of the United Kingdom. Commun. Dis. Public Health. 2002;5:114–118. [PubMed] [Google Scholar]
- Chalmers R.M., Campbell B.M., Crouch N., Charlett A., Davies A.P. Comparison of diagnostic sensitivity and specificity of seven Cryptosporidium assays used in the UK. J. Med. Microbiol. 2011;60:1598–1604. doi: 10.1099/jmm.0.034181-0. [DOI] [PubMed] [Google Scholar]
- Chalmers R.M., Atchison C., Barlow K., Young Y., Roche A., Manuel R. An audit of the laboratory diagnosis of cryptosporidiosis in England and Wales. J. Med. Microbiol. 2015;64:688–693. doi: 10.1099/JMM.0.000089. [DOI] [PubMed] [Google Scholar]
- Chalmers R.M., Robinson G., Hotchkiss E., Alexander C., May S., Gilray J., Connelly L., Hadfield S.J. Suitability of loci for multiple-locus variable-number of tandem-repeats analysis of Cryptosporidium parvum for inter-laboratory surveillance and outbreak investigations. Parasitology. 2017;144:37–47. doi: 10.1017/S0031182015001766. [DOI] [PubMed] [Google Scholar]
- Chalmers R.M., Pérez-Cordón G., Cacció S.M., Klotz C., Robertson L.J., participants of the Cryptosporidium genotyping workshop (EURO-FBP) Cryptosporidium genotyping in Europe: the current status and processes for a harmonised multi-locus genotyping scheme. Exp. Parasitol. 2018;191:25–30. doi: 10.1016/j.exppara.2018.06.004. [DOI] [PubMed] [Google Scholar]
- Chan R., Chen J., York M.K., Setijono N., Kaplan R.L., Graham F., Tanowitz H.B. Evaluation of a combination rapid immunoassay for detection of Giardia and Cryptosporidium antigens. J. Clin. Microbiol. 2000;38:393–394. doi: 10.1128/jcm.38.1.393-394.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Checkley W., Gilman R.H., Epstein L.D., Suarez M., Diaz J.F., Cabrera L., Black R.E., Sterling C.R. Asymptomatic and symptomatic cryptosporidiosis: their acute effect on weight gain in Peruvian children. Am. J. Epidemiol. 1997;145:156–163. doi: 10.1093/oxfordjournals.aje.a009086. [DOI] [PubMed] [Google Scholar]
- Checkley W., White A.C., Jaganath D., Arrowood M.J., Chalmers R.M., Chen X.-M., Fayer R., Griffiths J.K., Guerrant R.L., Hedstrom L., Huston C.D., Kotloff K.L., Kang G., Mead J.R., Miller M., Petri W.A., Priest J.W., Roos D.S., Striepen B., Thompson R.C.A., Ward H.D., Van Voorhis W.A., Xiao L., Zhu G., Houpt E.R. A review of the global burden, novel diagnostics, therapeutics, and vaccine targets for Cryptosporidium. Lancet Infect. Dis. 2014;3099:1–10. doi: 10.1016/S1473-3099(14)70772-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chelbi H., Essid R., Jelassi R., Bouzekri N., Zidi I., Ben Salah H., Mrad I., Ben Sghaier I., Abdelmalek R., Aissa S., Bouratbine A., Aoun K. High-resolution melting-curve (HRM) analysis for C. meleagridis identification in stool samples. Microb. Pathog. 2018;115:332–337. doi: 10.1016/j.micpath.2017.12.070. [DOI] [PubMed] [Google Scholar]
- Chen X.M., Keithly J., Paya C., LaRusso N. Cryptosporid- ium parvum. N. Engl. J. Med. 2002;346:1723–1732. doi: 10.1056/NEJMra013170. [DOI] [PubMed] [Google Scholar]
- Cheun H., Kim K., Yoon S., Lee W., Park W., Sim S., Yu J. Cryptosporidium hominis Infection Diagnosed by. Korean J. Parasitol. 2013;51:353–355. doi: 10.3347/kjp.2013.51.3.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claas E.C.J., Burnham C.D., Mazzulli T., Templeton K., Topin F. Performance of the xTAG® gastrointestinal pathogen panel, a multiplex molecular assay for simultaneous detection of bacterial, viral, and parasitic causes of infectious gastroenteritis. J. Microbiol. Biotechnol. 2013;23:1041–1045. doi: 10.4014/JMB.1212.12042. [DOI] [PubMed] [Google Scholar]
- Costa D., Soulieux L., Razakandrainibe R., Basmaciyan L., Gargala G., Valot S., Dalle F., Favennec L. Comparative Performance of Eight PCR Methods to Detect Cryptosporidium Species. Pathog. (Basel, Switzerland) 2021;10 doi: 10.3390/PATHOGENS10060647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crook P., Mayon-White R., Reacher M. Enhancing surveillance of cryptosporidiosis: test all faecal specimens from children. Commun. Dis. Public Health. 2002;5:112–113. [PubMed] [Google Scholar]
- Current W.L., Garcia L.S. Cryptosporidiosis. Clin. Microbiol. Rev. 1991;4:325–358. doi: 10.1128/cmr.4.3.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Current W.L., Haynes T.B. Complete development of Cryptosporidium in cell culture. Science (80) 1984;224:603–605. doi: 10.1126/science.6710159. [DOI] [PubMed] [Google Scholar]
- D’Antonio R.G., Winn R.E., Taylor J.P., Gustafson T.L., Current W.L., Rhodes M.M., Gary G.W., Zajac R.A. A waterborne outbreak of cryptosporidiosis in normal hosts. Ann. Intern. Med. 1985;103:886–888. doi: 10.7326/0003-4819-103-6-886. [DOI] [PubMed] [Google Scholar]
- De Waele V., Van den Broeck F., Huyse T., McGrath G., Higgins I., Speybroeck N., Berzano M., Raleigh P., Mulcahy G.M., Murphy T.M. Panmictic structure of the Cryptosporidium parvum population in Irish Calves: influence of prevalence and host movement. Appl. Environ. Microbiol. 2013;79:2534–2541. doi: 10.1128/AEM.03613-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMone C., Hwang M.H., Feng Z., McClure J.T., Greenwood S.J., Fung R., Kim M., Weese J.S., Shapiro K. Application of next generation sequencing for detection of protozoan pathogens in shellfish. Food Waterborne Parasitol. 2020;21 doi: 10.1016/J.FAWPAR.2020.E00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Cristina M., Carruthers V.B. New and emerging uses of CRISPR/Cas9 to genetically manipulate apicomplexan parasites. Parasitology. 2018;145:1119–1126. doi: 10.1017/S003118201800001X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Długońska H. The Nobel Prize 2015 in physiology or medicine for highly effective antiparasitic drugs. Ann. Parasitol. 2015;61:299–301. doi: 10.17420/ap6104.23. [DOI] [PubMed] [Google Scholar]
- Doing K.M., Hamm J.L., Jellison J.A., Marquis J.A., Kingsbury C. False-positive results obtained with the Alexon ProSpecT Cryptosporidium enzyme immunoassay. J. Clin. Microbiol. 1999;37:1582–1583. doi: 10.1128/jcm.37.5.1582-1583.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doudna J.A., Charpentier E. Genome editing. The new frontier of genome engineering with CRISPR-Cas9. Science. 2014;346 doi: 10.1126/science.1258096. [DOI] [PubMed] [Google Scholar]
- Dror S.K., Pavlotzky E., Barak M. Evaluation of the NanoCHIP® Gastrointestinal Panel (GIP) test for simultaneous detection of parasitic and bacterial enteric pathogens in fecal specimens. PLoS One. 2016;11 doi: 10.1371/JOURNAL.PONE.0159440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta D., Heo I., O’connor R. Studying Cryptosporidium infection in 3D tissue-derived human organoid culture systems by microinjection. J. Vis. Exp. 2019;2019 doi: 10.3791/59610. [DOI] [PubMed] [Google Scholar]
- Efstratiou A., Ongerth J.E., Karanis P. Waterborne transmission of protozoan parasites: review of worldwide outbreaks - An update 2011–2016. Water Res. 2017;114:14–22. doi: 10.1016/j.watres.2017.01.036. [DOI] [PubMed] [Google Scholar]
- El-Moamly A.A.R., El-Sweify M.A. ImmunoCard STAT! cartridge antigen detection assay compared to microplate enzyme immunoassay and modified Kinyoun’s acid-fast staining technique for detection of Cryptosporidium in fecal specimens. Parasitol. Res. 2012;110:1037–1041. doi: 10.1007/S00436-011-2585-Z. [DOI] [PubMed] [Google Scholar]
- Elsafi S.H., Al-Sheban S.S., Al-Jubran K.M., Abu Hassan M.M., Al Zahrani E.M. Comparison of Kinyoun’s acid-fast and immunofluorescent methods detected an unprecedented occurrence of Cryptosporidium in the Eastern Region of Saudi Arabia. J. Taibah Univ. Med. Sci. 2014;9:263–267. doi: 10.1016/j.jtumed.2014.03.008. [DOI] [Google Scholar]
- Elsafi Salah H., Al-Maqati T.N., Hussein M.I., Adam A.A., Hassan M.M.A., Al Zahrani E.M. Comparison of microscopy, rapid immunoassay, and molecular techniques for the detection of Giardia lamblia and Cryptosporidium parvum. Parasitol. Res. 2013;112:1641–1646. doi: 10.1007/s00436-013-3319-1. [DOI] [PubMed] [Google Scholar]
- Elwin K., Fairclough H.V., Hadfield S.J., Chalmers R.M. Giardia duodenalis typing from stools: a comparison of three approaches to extracting DNA, and validation of a probe-based real-time PCR typing assay. J. Med. Microbiol. 2013;63:38–44. doi: 10.1099/jmm.0.066050-0. [DOI] [PubMed] [Google Scholar]
- Espy M.J., Uhl J.R., Sloan L.M., Buckwalter S.P., Jones M.F., Vetter E.A., Yao J.D.C., Wengenack N.L., Rosenblatt J.E., Cockerill F.R., Smith T.F. Real-time PCR in clinical microbiology: applications for routine laboratory testing. Clin. Microbiol. Rev. 2006;19:165–256. doi: 10.1128/CMR.19.1.165-256.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng X., Rich S.M., Akiyoshi D., Tumwine J.K., Kekitiinwa A., Nabukeera N., Tzipori S., Widmer G. Extensive polymorphism in Cryptosporidium parvum identified by multilocus microsatellite analysis. Appl. Environ. Microbiol. 2000;66:3344–3349. doi: 10.1128/aem.66.8.3344-3349.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng X., Rich S.M., Tzipori S., Widmer G. Experimental evidence for genetic recombination in the opportunistic pathogen Cryptosporidium parvum. Mol. Biochem. Parasitol. 2002;119:55–62. doi: 10.1016/s0166-6851(01)00393-0. [DOI] [PubMed] [Google Scholar]
- Feng Y., Tiao N., Li N., Hlavsa M., Xiao L., Doern G.V. Multilocus sequence typing of an emerging Cryptosporidium hominis subtype in the united states. J. Clin. Microbiol. 2014;52:524–530. doi: 10.1128/JCM.02973-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y., Ryan U.M., Xiao L. Genetic diversity and population structure of Cryptosporidium. Trends Parasitol. 2018;34:997–1011. doi: 10.1016/j.pt.2018.07.009. [DOI] [PubMed] [Google Scholar]
- Fournet N., Deege M.P., Urbanus A.T., Nichols G., Rosner B.M., Chalmers R.M., Gorton R., Pollock K.G., van der Giessen J.W.B., Wever P.C., Dorigo-Zetsma J.W., Mulder B., Mank T.G., Overdevest I., Kusters J.G., van Pelt W., Kortbeek L.M. Simultaneous increase of Cryptosporidium infections in the Netherlands, the United Kingdom and Germany in late summer season, 2012. Eurosurveillance. 2013:18. [PubMed] [Google Scholar]
- Freedman S.B., Lee B.E., Louie M., Pang X.-L., Ali S., Chuck A., Chui L., Currie G.R., Dickinson J., Drews S.J., Eltorki M., Graham T., Jiang X., Johnson D.W., Kellner J., Lavoie M., MacDonald J., MacDonald S., Svenson L.W., Talbot J., Tarr P., Tellier R., Vanderkooi O.G. Alberta Provincial Pediatric EnTeric Infection TEam (APPETITE): epidemiology, emerging organisms, and economics. BMC Pediatr. 2015;15:89. doi: 10.1186/s12887-015-0407-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L.S., Shimizu R.Y. Detection of Giardia lamblia and Cryptosporidium parvum antigens in human fecal specimens using the ColorPAC Combination Rapid Solid-Phase qualitative Immunochromatographic assay antigens in human fecal specimens using the ColorPAC combination rapid solid. J. Clin. Microbiol. 2000;38:1267–1269. doi: 10.1128/jcm.38.3.1267-1268.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L.S., Bruckner D.A., Brewer T.C., Shimizu R.Y. Techniques for the recovery and identification of Cryptosporidium oocysts from stool specimens. J. Clin. Microbiol. 1983;18:185–190. doi: 10.1128/jcm.18.1.185-190.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L.S., Brewer T.C., Bruckner D.A. Fluorescence detection of Cryptosporidium oocysts in human fecal specimens by using monoclonal antibodies. J. Clin. Microbiol. 1987;25:119–121. doi: 10.1128/jcm.25.1.119-121.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L.S., Shum A.C., Bruckner D.A. Evaluation of a new monoclonal antibody combination reagent for direct fluorescence detection of Giardia cysts and Cryptosporidium oocysts in human fecal specimens. J. Clin. Microbiol. 1992;30:3255–3257. doi: 10.1128/jcm.30.12.3255-3257.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L.S., Shimizu R.Y., Novak S., Carroll M., Chan F. Commercial assay for detection of Giardia lamblia and Cryptosporidium parvum antigens in human fecal specimens by rapid solid-phase qualitative immunochromatography. J. Clin. Microbiol. 2003;41:209–212. doi: 10.1128/JCM.41.1.209-212.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-R J.C., Hayman D.T.S. Evolutionary processes in populations of Cryptosporidium inferred from gp60 sequence data. Parasitol. Res. 2017;116:1855–1861. doi: 10.1007/s00436-017-5459-1. [DOI] [PubMed] [Google Scholar]
- Garcia-R J.C., Cox M.P., Hayman D.T.S. Comparative genetic diversity of Cryptosporidium species causing human infections. Parasitology. 2020;147:1532–1537. doi: 10.1017/S0031182020001493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garvey P., McKeown P. Epidemiology of human cryptosporidiosis in Ireland, 2004-2006: analysis of national notification data. Eurosurveillance. 2009;14 [PubMed] [Google Scholar]
- Goñi P., Martín B., Villacampa M., García A., Seral C., Castillo F.J., Clavel A. Evaluation of an immunochromatographic dip strip test for simultaneous detection of Cryptosporidium spp, Giardia duodenalis, and Entamoeba histolytica antigens in human faecal samples. Eur. J. Clin. Microbiol. Infect. Dis. 2012;31:2077–2082. doi: 10.1007/s10096-012-1544-77. [DOI] [PubMed] [Google Scholar]
- van Gool T., Weijts R., Lommerse E., Mank T.G. Triple faeces test: an effective tool for detection of intestinal parasites in routine clinical practice. Eur. J. Clin. Microbiol. Infect. Dis. 2003;22:284–290. doi: 10.1007/s10096-003-0919-1. [DOI] [PubMed] [Google Scholar]
- Grinberg A., Widmer G. Cryptosporidium within-host genetic diversity: systematic bibliographical search and narrative overview. Int. J. Parasitol. 2016;46:465–471. doi: 10.1016/j.ijpara.2016.03.002. [DOI] [PubMed] [Google Scholar]
- Grinberg A., Biggs P.J., Dukkipati V.S.R., George T.T. Extensive intra-host genetic diversity uncovered in Cryptosporidium parvum using Next Generation Sequencing. Infect. Genet. Evol. 2013;15:18–24. doi: 10.1016/J.MEEGID.2012.08. [DOI] [PubMed] [Google Scholar]
- Hadfield S.J., Robinson G., Elwin K., Chalmers R.M. Detection and differentiation of Cryptosporidium spp. in human clinical samples by use of real-time PCR. J. Clin. Microbiol. 2011;49:918–924. doi: 10.1128/JCM.01733-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannet I., Engsbro A.L., Pareja J., Schneider U.V., Lisby J.G., Pružinec-Popović B., Hoerauf A., Parčina M. Multicenter evaluation of the new QIAstat gastrointestinal panel for the rapid syndromic testing of acute gastroenteritis. Eur. J. Clin. Microbiol. Infect. Dis. 2019;38:2103–2112. doi: 10.1007/S10096-019-03646-4. [DOI] [PubMed] [Google Scholar]
- Hanscheid T., Cristino J.M., Salgado M.J. Screening of auramine-stained smears of all fecal samples is a rapid and inexpensive way to increase the detection of coccidial infections. Int. J. Infect. Dis. 2008;12:47–50. doi: 10.1016/j.ijid.2007.04.008. [DOI] [PubMed] [Google Scholar]
- Hanson K.L., Cartwright C.P. Use of an enzyme immunoassay does not eliminate the need to analyze multiple stool specimens for sensitive detection of Giardia lamblia. J. Clin. Microbiol. 2001;39:474–477. doi: 10.1128/JCM.39.2.474-477.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haque R., Roy S., Siddique A., Mondal U., Rahman S.M.M., Mondal D., Houpt E., Petri W.A. Multiplex real-time PCR assay for detection of Entamoeba histolytica, Giardia intestinalis, and Cryptosporidium spp. Am. J. Trop. Med. Hyg. 2007;76:713–717. [PubMed] [Google Scholar]
- Haupst T., Davis J. Manufacturer’s recall of Rapid assay kits based on false positive Cryptosporidium Anitgen tests - Wisconsin 2001-2002. JAMA. 2002:287. [PubMed] [Google Scholar]
- Hawash Y. Evaluation of an immunoassay-based algorithm for screening and identification of giardia and Cryptosporidium antigens in human faecal specimens from saudi arabia. J. Parasitol. Res. 2014;2014:213745. doi: 10.1155/2014/213745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Protection Surveillance Centre . 2004. Report of Waterborne Cryptosporidiosis Subcommittee of the Scientific Advisory Committee. [Google Scholar]
- Heiges M., Wang H., Robinson E., Aurrecoechea C., Gao X., Kaluskar N., Rhodes P., Wang S., He C.-Z., Su Y., Miller J., Kraemer E., Kissinger J.C. CryptoDB: a Cryptosporidium bioinformatics resource update. Nucleic Acids Res. 2006;34:D419–D422. doi: 10.1093/nar/gkj078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmy Y.A., Krücken J., Nöckler K., von Samson-Himmelstjerna G., Zessin K.-H. Comparison between two commercially available serological tests and polymerase chain reaction in the diagnosis of Cryptosporidium in animals and diarrhoeic children. Parasitol. Res. 2014;113:211–216. doi: 10.1007/s00436-013-3645-3. [DOI] [PubMed] [Google Scholar]
- Henricksen S.A., Pohlenz J.F.L. Staining of cryptosporidia by a modified Ziehl-Neelsen technique. Acta Vet. Scand. 1981;22:594–596. doi: 10.1186/BF03548684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heo I., Dutta D., Schaefer D.A., Iakobachvili N., Artegiani B., Sachs N., Boonekamp K.E., Bowden G., Hendrickx A.P.A., Willems R.J.L., Peters P.J., Riggs M.W., O’Connor R., Clevers H. Modelling Cryptosporidium infection in human small intestinal and lung organoids. Nat. Microbiol. 2018;3:814–823. doi: 10.1038/s41564-018-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hijjawi N. Cryptosporidium: new developments in cell culture. Exp. Parasitol. 2010;124:54–60. doi: 10.1016/j.exppara.2009.05.015. [DOI] [PubMed] [Google Scholar]
- Hijjawi N., Meloni B., Morgan U., Thompson R.C. Complete development and long-term maintenance of Cryptosporidium parvum human and cattle genotypes in cell culture. Int. J. Parasitol. 2001;31:1048–1055. doi: 10.1016/S0020-7519(01)00212-0. [DOI] [PubMed] [Google Scholar]
- ten Hove R., Schuurman T., Kooistra M., Möller L., Van Lieshout L., Verweij J.J. Detection of diarrhoea-causing protozoa in general practice patients in The Netherlands by multiplex real-time PCR. Clin. Microbiol. Infect. 2007;13:1001–1007. doi: 10.1111/j.1469-0691.2007.01788.x. [DOI] [PubMed] [Google Scholar]
- Ibrahim H.S., Shehab A.Y., Allam A.F., Mohamed M.A., Farag H.F., Tolba M.M. Detection and molecular identification of Cryptosporidium species among children with malignancies. Acta Parasitol. 2021;66:377–383. doi: 10.1007/S11686-020-00250-X. [DOI] [PubMed] [Google Scholar]
- Insulander M., Silverlås C., Lebbad M., Karlsson L., Mattsson J.G., Svenungsson B. Molecular epidemiology and clinical manifestations of human cryptosporidiosis in Sweden. Epidemiol. Infect. 2013;141:1009–1020. doi: 10.1017/S0950268812001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaza J.P., Galván A.L., Polanco V., Huang B., Matveyev A.V., Serrano M.G., Manque P., Buck G.A., Alzate J.F. Revisiting the reference genomes of human pathogenic Cryptosporidium species: reannotation of C. parvum Iowa and a new C. hominis reference. Sci. Rep. 2015;5:16324. doi: 10.1038/srep16324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansen Ø.H., Abdissa A., Zangenberg M., Mekonnen Z., Eshetu B., Bjørang O., Alemu Y., Sharew B., Langeland N., Robertson L.J., Hanevik K. Performance and operational feasibility of two diagnostic tests for cryptosporidiosis in children (CRYPTO-POC): a clinical, prospective, diagnostic accuracy study. Lancet Infect. Dis. 2021;21:722–730. doi: 10.1016/S1473-3099(20)30556-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston S.P., Ballard M.M., Beach M.J., Causer L., Wilkins P.P. Evaluation of three commercial assays for detection of Giardia and Cryptosporidium organisms in fecal specimens. J. Clin. Microbiol. 2003;41:623–626. doi: 10.1128/JCM.41.2.623-626.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones J.L., Lopez A., Wahlquist S.P., Nadle J., Wilson M. Survey of clinical laboratory practices for parasitic diseases. Clin. Infect. Dis. 2004;38(Suppl. 3):S198–S202. doi: 10.1086/381587. [DOI] [PubMed] [Google Scholar]
- Jossé L., Bones A.J., Purton T., Michaelis M., Tsaousis A.D. A cell culture platform for the cultivation of Cryptosporidium parvum. Curr. Protoc. Microbiol. 2019;53 doi: 10.1002/cpmc.80. [DOI] [PubMed] [Google Scholar]
- Kabir M., Ahmed E., Hossain B., Alam M., Ahmed S., Taniuchi M., Gilchrist C.A., Houpt E.R., Faruque A.S.G., Petri W.A., Jr., Haque R. Giardia/Cryptosporidium QUIK CHEK assay is more specific than quantitative polymerase chain reaction for rapid point-of-care diagnosis of cryptosporidiosis in infants in Bangladesh. Clin. Infect. Dis. An Off. Publ. Infect. Dis. Soc. Am. 2018;67:1897. doi: 10.1093/CID/CIY372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kageruka P., Brandt J.R., Taelman H. Modified Köster staining method for the diagnosis of cryptosporidiosis. Ann. Soc. Belg. Med. Trop. 1984;1920(64):171–175. [PubMed] [Google Scholar]
- Kamal K., Ei-dib N., Hassanin F. Evaluation of immunoflourescent antibody (IFA) kit for the detection of Cryptosporidium parvum Oocyst s and Giardia latublia Cysts in stool specimens. Parasitol. United J. 2008;1:145–148. [Google Scholar]
- Karanis P. The truth about in vitro culture of Cryptosporidium species. Parasitology. 2018 doi: 10.1017/S0031182017001937. [DOI] [PubMed] [Google Scholar]
- Karanis P., Aldeyarbi H.M. Evolution of Cryptosporidium in vitro culture. Int. J. Parasitol. 2011 doi: 10.1016/j.ijpara.2011.08.001. [DOI] [PubMed] [Google Scholar]
- Kaushik K., Khurana S., Wanchu A., Malla N. Evaluation of staining techniques, antigen detection and nested PCR for the diagnosis of cryptosporidiosis in HIV seropositive and seronegative patients. Acta Trop. 2008;107:1–7. doi: 10.1016/j.actatropica.2008.02.007. [DOI] [PubMed] [Google Scholar]
- Kehl K.S., Cicirello H., Havens P.L. Comparison of four different methods for detection of Cryptosporidium species. J. Clin. Microbiol. 1995;33:416–418. doi: 10.1128/jcm.33.2.416-418.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khare R., EspY M.J., Cebelinski E., Boxrud D., Sloan L.M., Cunningham S.A., Pritt B.S., Patel R., Binnicker M.J. Comparative evaluation of two commercial multiplex panels for detection of gastrointestinal pathogens by use of clinical stool specimens. J. Clin. Microbiol. 2014;52:3667–3673. doi: 10.1128/JCM.01637-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurana S., Chaudhary P. Laboratory diagnosis of cryptosporidiosis. Trop. Parasitol. 2018;8:2. doi: 10.4103/TP.TP_34_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurana S., Sharma P., Sharma A., Malla N. Evaluation of Ziehl-Neelsen staining, auramine phenol staining, antigen detection enzyme linked immunosorbent assay and polymerase chain reaction, for the diagnosis of intestinal cryptosporidiosis. Trop. Parasitol. 2012;2:20–23. doi: 10.4103/2229-5070.97234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King P., Tyler K.M., Hunter P.R. Anthroponotic transmission of Cryptosporidium parvum predominates in countries with poorer sanitation: a systematic review and meta-analysis. Parasit. Vectors. 2019;12:16. doi: 10.1186/s13071-018-3263-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk M.D., Pires S.M., Black R.E., Caipo M., Crump J.A., Devleesschauwer B., Döpfer D., Fazil A., Fischer-Walker C.L., Hald T., Hall A.J., Keddy K.H., Lake R.J., Lanata C.F., Torgerson P.R., Havelaar A.H., Angulo F.J. World Health organization estimates of the global and regional disease burden of 22 foodborne bacterial, protozoal, and viral diseases, 2010: a data synthesis. PLoS Med. 2015;12 doi: 10.1371/journal.pmed.1001921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissinger J.C. In: Cryptosporidium and Cryptosporidiosis. Fayer R., Xiao L., editors. CRC Press; Boca Raton, United States: 2008. Genomics; pp. 43–56. [Google Scholar]
- Kotloff K.L., Nataro J.P., Blackwelder W.C., Nasrin D., Farag T.H., Panchalingam S., Wu Y., Sow S.O., Sur D., Breiman R.F., Faruque A.S.G., Zaidi A.K.M., Saha D., Alonso P.L., Tamboura B., Sanogo D., Onwuchekwa U., Manna B., Ramamurthy T., Kanungo S., Ochieng J.B., Omore R., Oundo J.O., Hossain A., Das S.K., Ahmed S., Qureshi S., Quadri F., Adegbola R.A., Antonio M., Hossain M.J., Akinsola A., Mandomando I., Nhampossa T., Acácio S., Biswas K., O’Reilly C.E., Mintz E.D., Berkeley L.Y., Muhsen K., Sommerfelt H., Robins-Browne R.M., Levine M.M. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): A prospective, case-control study. Lancet. 2013;382:209–222. doi: 10.1016/S0140-6736(13)60844-2. [DOI] [PubMed] [Google Scholar]
- Lalonde L.F., Reyes J., Gajadhar A.A. Application of a qPCR assay with melting curve analysis for detection and differentiation of protozoan oocysts in human fecal samples from Dominican Republic. Am. J. Trop. Med. Hyg. 2013;89:892–898. doi: 10.4269/ajtmh.13-0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leng X., Mosier D.A., Oberst R.D. Differentiation of Cryptosporidium parvum, C. muris, and C. baileyi by PCR-RFLP analysis of the 18s rRNA gene. Vet. Parasitol. 1996;62:1–7. doi: 10.1016/0304-4017(95)00863-2. [DOI] [PubMed] [Google Scholar]
- Liu C., Vigdorovich V., Kapur V., Abrahamsen M.S. A random survey of the Cryptosporidium parrum genome. Infect. Immun. 1999;67:3960–3969. doi: 10.1128/iai.67.8.3960-3969.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Gratz J., Amour C., Kibiki G., Becker S., Janaki L., Verweij J.J., Taniuchi M., Sobuz S.U., Haque R., Haverstick D.M., Houpt E.R. A laboratory-developed taqman array card for simultaneous detection of 19 enteropathogens. J. Clin. Microbiol. 2013;51:472–480. doi: 10.1128/JCM.02658-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llorente M.T., Clavel A., Varea M., Olivera S., Castillo F.J., Sahagún J., Rubio M.C., Gómez-Lus R. Evaluation of an immunochromatographic dip-strip test for the detection of Cryptosporidium oocysts in stool specimens. Eur. J. Clin. Microbiol. Infect. Dis. 2002;21:624–625. doi: 10.1007/s10096-002-0778-1. [DOI] [PubMed] [Google Scholar]
- de Lucio A., Merino F.J., Martínez-Ruiz R., Bailo B., Aguilera M., Fuentes I., Carmena D. Molecular genotyping and sub-genotyping of Cryptosporidium spp. isolates from symptomatic individuals attending two major public hospitals in Madrid. Spain. Infect. Genet. Evol. 2016;37:49–56. doi: 10.1016/j.meegid.2015.10.026. [DOI] [PubMed] [Google Scholar]
- MacKenzie W.R., Schell W.L., Blair K.A., Addiss D.G., Peterson D.E., Hoxie N.J., Kazmierczak J.J., Davis J.P. Massive outbreak of waterborne Cryptosporidium infection in Milwaukee, Wisconsin: recurrence of illness and risk of secondary transmission. Clin. Infect. Dis. 1995;21:57–62. doi: 10.1093/clinids/21.1.57. [DOI] [PubMed] [Google Scholar]
- Madison-Antenucci S., Relich R.F., Doyle L., Espina N., Fuller D., Karchmer T., Lainesse A., Mortensen J.E., Pancholi P., Veros W., Harrington S.M. Multicenter evaluation of BD Max Enteric Parasite Real-Time PCR Assay for detection of Giardia duodenalis, Cryptosporidium hominis, Cryptosporidium parvum, and Entamoeba histolytica. J. Clin. Microbiol. 2016;54:2681–2688. doi: 10.1128/JCM.00765-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manjunatha U.H., Vinayak S., Zambriski J.A., Chao A.T., Sy T., Noble C.G., Bonamy G.M.C., Kondreddi R.R., Zou B., Gedeck P., Brooks C.F., Herbert G.T., Sateriale A., Tandel J., Noh S., Lakshminarayana S.B., Lim S.H., Goodman L.B., Bodenreider C., Feng G., Zhang L., Blasco F., Wagner J., Leong F.J., Striepen B., Diagana T.T. A Cryptosporidium PI(4)K inhibitor is a drug candidate for cryptosporidiosis. Nature. 2017;546:376–380. doi: 10.1038/nature22337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manser M., Granlund M., Edwards H., Saez A., Petersen E., Evengard B., Chiodini P. Detection of Cryptosporidium and Giardia in clinical laboratories in Europe--a comparative study. Clin. Microbiol. Infect. 2014;20:O65–O71. doi: 10.1111/1469-0691.12297. [DOI] [PubMed] [Google Scholar]
- Mazurie A.J., Alves J.M., Ozaki L.S., Zhou S., Schwartz D.C., Buck G.A. Comparative genomics of Cryptosporidium. Int. J. Genomics. 2013;2013 doi: 10.1155/2013/832756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuliffe G., Bissessor L., Williamson D., Moore S., Wilson J., Dufour M., Taylor S., Upton A. Use of the EntericBio Gastro Panel II in a diagnostic microbiology laboratory: challenges and opportunities. Pathology. 2017;49:419–422. doi: 10.1016/j.pathol.2017.02.003. [DOI] [PubMed] [Google Scholar]
- McHardy I.H., Wu M., Shimizu-Cohen R., Couturier M.R., Humphries R.M. Detection of intestinal protozoa in the clinical laboratory. J. Clin. Microbiol. 2014;52:712–720. doi: 10.1128/JCM.02877-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKerr C., Chalmers R.M., Vivancos R., O’Brien S.J., Mugarza J., Christley R.M. Cross-sectional investigation of household transmission of Cryptosporidium in England and Wales: the epiCrypt study protocol. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-026116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNabb S.J.N., Hensel D.M., Welch D.F., Heijbel H., McKee G.L., Istre G.R. Comparison of sedimentation and flotation techniques for identification of Cryptosporidium sp. oocysts in a large outbreak of human diarrhea. J. Clin. Microbiol. 1985;22:587–589. doi: 10.1128/jcm.22.4.587-589.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meurs L., Polderman A.M., Vinkeles Melchers N.V.S., Brienen E.A.T., Verweij J.J., Groosjohan B., Mendes F., Mechendura M., Hepp D.H., Langenberg M.C.C., Edelenbosch R., Polman K., van Lieshout L. diagnosing polyparasitism in a high-prevalence setting in Beira, Mozambique: detection of intestinal parasites in fecal samples by microscopy and real-time PCR. PLoS Negl. Trop. Dis. 2017:11. doi: 10.1371/journal.pntd.0005310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller C.N., Jossé L., Brown I., Blakeman B., Povey J., Yiangou L., Price M., Cinatl J., Xue W.F., Michaelis M., Tsaousis A.D. A cell culture platform for Cryptosporidium that enables long-term cultivation and new tools for the systematic investigation of its biology. Int. J. Parasitol. 2018;48:197–201. doi: 10.1016/j.ijpara.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller J., Mojica B. False positive laboratory tests for Cryptosporidium involving enzye linked immunosorbent Assay - United States, November 1997- March 1998. JAMA. 1999;281:5. [Google Scholar]
- Milstein C. The hybridoma revolution: An offshoot of basic research. BioEssays. 1999;21:966–973. doi: 10.1002/(SICI)1521-1878(199911)21:11<966::AID-BIES9>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- Minak J., Kabir M., Mahmud I., Liu Y., Liu L., Haque R., Petri W.A., Jr. Evaluation of rapid antigen point-of-care tests for detection of Giardia and Cryptosporidium species in human fecal specimens. J. Clin. Microbiol. 2012;50:154. doi: 10.1128/JCM.01194-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minarovičová J., Kaclíková E., Krascsenicsová K., Siekel P., Kuchta T. A single-tube nested real-time polymerase chain reaction for sensitive contained detection of Cryptosporidium parvum. Lett. Appl. Microbiol. 2009;49:568–572. doi: 10.1111/j.1472-765X.2009.02708.x. [DOI] [PubMed] [Google Scholar]
- Mölling P., Nilsson P., Ennefors T., Ögren J., Florén K., Hedberg S.T., Sundqvist M. Evaluation of the BD max enteric parasite panel for clinical diagnostics. J. Clin. Microbiol. 2016;54:443–444. doi: 10.1128/JCM.02100-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk J., Palsson B.O. Genetics. Predicting microbial growth. Science. 2014;344:1448–1449. doi: 10.1126/science.1253388. [DOI] [PubMed] [Google Scholar]
- Morada M., Lee S., Gunther-Cummins L., Weiss L.M., Widmer G., Tzipori S., Yarlett N. Continuous culture of Cryptosporidium parvum using hollow fiber technology. Int. J. Parasitol. 2016 doi: 10.1016/j.ijpara.2015.07.006. [DOI] [PubMed] [Google Scholar]
- Morio F., Poirier P., Le Govic Y., Laude A., Valot S., Desoubeaux G., Argy N., Nourrisson C., Pomares C., Machouart M., Dalle F., Botterel F., Bourgeois N., Cateau E., Leterrier M., Beser J., Lavergne R., Le Pape P. Assessment of the first commercial multiplex PCR kit (ParaGENIE Crypto-Micro Real-Time PCR) for the detection of Cryptosporidium spp., Enterocytozoon bieneusi, and Encephalitozoon intestinalis from fecal samples. Diagn. Microbiol. Infect. Dis. 2019;95:34–37. doi: 10.1016/J.DIAGMICROBIO.2019.04.004. [DOI] [PubMed] [Google Scholar]
- Morris A., Robinson G., Swain M.T., Chalmers R.M. Direct sequencing of Cryptosporidium in stool samples for public health. Front. Public Health. 2019;7:360. doi: 10.3389/FPUBH.2019.00360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy C.N., Fowler R.C., Iwen P.C., Fey P.D. Evaluation of the BioFire FilmArray® GastrointestinalPanel in a Midwestern Academic Hospital. Eur. J. Clin. Microbiol. Infect. Dis. 2017;36:747–754. doi: 10.1007/S10096-016-2858-7. [DOI] [PubMed] [Google Scholar]
- Navidad J.F., Griswold D.J., Gradus M., Bhattacharyya S. Evaluation of Luminex xTAG gastrointestinal pathogen analyte-specific reagents for high-throughput, simultaneous detection of bacteria, viruses, and parasites of clinical and public health importance. J. Clin. Microbiol. 2013;51:3018–3024. doi: 10.1128/JCM.00896-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman R.D., Jaeger K.L., Wuhib T., Lima A.A., Guerrant R.L., Sears C.L. Evaluation of an antigen capture enzyme-linked immunosorbent assay for detection of Cryptosporidium oocysts. J. Clin. Microbiol. 1993;31:2080–2084. doi: 10.1128/jcm.31.8.2080-2084.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nime F.A., Burek J.D., Page D.L., Holscher M.A., Yardley J.H. Acute enterocolitis in a human being infected with the protozoan Cryptosporidium. Gastroenterology. 1976;70:592–598. [PubMed] [Google Scholar]
- O'Leary J.K., Blake L., Corcoran D., Sleator R.D., Lucey B. Trials and tribulations of enteric parasitology in the molecular era. J. Med. Microbiol. 2018;67:145–147. doi: 10.1099/jmm.0.000670. [DOI] [PubMed] [Google Scholar]
- O'Leary J.K., Blake L., Corcoran G.D., Sleator R.D., Lucey B. A novel genotyping method for Cryptosporidium hominis. Exp. Parasitol. 2021;225:108113. doi: 10.1016/J.EXPPARA.2021.108113. [DOI] [PubMed] [Google Scholar]
- O'Leary J.K., Blake L., Corcoran G.D., Sleator R.D., Lucey B. Development of a novel, high resolution melting analysis based genotyping method for Cryptosporidium parvum. Eur. J. Protistol. 2021;79:125799. doi: 10.1016/J.EJOP.2021.125799. [DOI] [PubMed] [Google Scholar]
- Omoruyi B.E., Nwodo U.U., Udem C.S., Okonkwo F.O. Comparative diagnostic techniques for Cryptosporidium infection. Molecules. 2014;19:2674–2683. doi: 10.3390/molecules19022674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer S.R., Biffin A.H. Cryptosporidiosis in England and Wales: prevalence and clinical and epidemiological features. Br. Med. J. (Clin. Res. Ed.) 1990;300:774–777. doi: 10.1136/bmj.300.6727.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parghi E., Dash L., Shastri J. Evaluation of different modifications of acid-fast staining techniques and stool enzyme-linked immunosorbent assay in detecting fecal Cryptosporidium in diarrheic HIV seropositive and seronegative patients. Trop. Parasitol. 2014;4:99–104. doi: 10.4103/2229-5070.138537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel A., Navidad J., Bhattacharyya S. Site-specific clinical evaluation of the Luminex xTAG gastrointestinal pathogen panel for detection of infectious gastroenteritis in fecal specimens. J. Clin. Microbiol. 2014;52:3068–3071. doi: 10.1128/JCM.01393-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulos S., Saugar J.M., de Lucio A., Fuentes I., Mateo M., Carmena D. Comparative performance evaluation of four commercial multiplex real-time PCR assays for the detection of the diarrhoea-causing protozoa Cryptosporidium hominis/parvum, Giardia duodenalis and Entamoeba histolytica. PLoS One. 2019;14 doi: 10.1371/JOURNAL.PONE.0215068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawlowic M.C., Somepalli M., Sateriale A., Herbert G.T., Gibson A.R., Cuny G.D., Hedstrom L., Striepen B. Genetic ablation of purine salvage in Cryptosporidium parvum reveals nucleotide uptake from the host cell. Proc. Natl. Acad. Sci. 2019;116:21160–21165. doi: 10.1073/PNAS.1908239116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelly H., Cormican M., O’Donovan D., Chalmers R., Hanahoe B., Cloughley R., McKeown P., Corbett-Feeney G. A large outbreak of cryptosporidiosis in western Ireland linked to public water supply: a preliminary report. Eurosurveillance. 2007;12(5) doi: 10.2807/esw.12.18.03187-en. [DOI] [PubMed] [Google Scholar]
- Perry M.D., Corden S.A., Howe R.A. Evaluation of the Luminex xTAG gastrointestinal pathogen panel and the savyon diagnostics gastrointestinal infection panel for the detection of enteric pathogens in clinical samples. J. Med. Microbiol. 2014;63:1419–1426. doi: 10.1099/JMM.0.074773-0. [DOI] [PubMed] [Google Scholar]
- Pohl G., Shih L.M. Principle and applications of digital PCR, in: expert review of molecular diagnostics. Expert. Rev. Mol. Diagn. 2004:41–47. doi: 10.1586/14737159.4.1.41. [DOI] [PubMed] [Google Scholar]
- Pomari E., Piubelli C., Perandin F., Bisoffi Z. Digital PCR: a new technology for diagnosis of parasitic infections. Clin. Microbiol. Infect. 2019 doi: 10.1016/j.cmi.2019.06.009. [DOI] [PubMed] [Google Scholar]
- Public Health England . 2014. UK Standards for Microbiology Investigations B 31: Investigation of Specimens Other than Blood for Parasites. [Google Scholar]
- Puiu D., Enomoto S., Buck G.A., Abrahamsen M.S., Kissinger J.C. CryptoDB: the Cryptosporidium genome resource. Nucleic Acids Res. 2004;32:D329–D331. doi: 10.1093/nar/gkh050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo A., Quílez J., Vergara-Castiblanco C., Monteagudo L., Del Cacho E., Clavel A. Multilocus typing and population structure of Cryptosporidium from children in Zaragoza, Spain. Infect. Genet. Evol. 2015;31:190–197. doi: 10.1016/j.meegid.2015.01.023. [DOI] [PubMed] [Google Scholar]
- Robinson G., Chalmers R.M. Assessment of polymorphic genetic markers for multi-locus typing of Cryptosporidium parvum and Cryptosporidium hominis. Exp. Parasitol. 2012;132:200–215. doi: 10.1016/j.exppara.2012.06.016. [DOI] [PubMed] [Google Scholar]
- Roellig D.M., Xiao L. Cryptosporidium genotyping for epidemiology tracking. Methods Mol. Biol. 2020;2052:103–116. doi: 10.1007/978-1-4939-9748-0_7. [DOI] [PubMed] [Google Scholar]
- Rosenblatt J.E., Sloan L.M. Evaluation of an enzyme-linked immunosorbent assay for detection of Cryptosporidium spp. in stool specimens. J. Clin. Microbiol. 1993;31:1468–1471. doi: 10.1128/jcm.31.6.1468-1471.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossignol J.F., Ayoub A., Ayers M.S. Treatment of diarrhea caused by Cryptosporidium parvum: a prospective randomized, double-blind, placebo-controlled study of Nitazoxanide. J. Infect. Dis. 2001;184:103–106. doi: 10.1086/321008. [DOI] [PubMed] [Google Scholar]
- Rossignol J.-F., Kabil S.M., El-Gohary Y., Younis A.M. Effect of nitazoxanide in diarrhea and enteritis caused by Cryptosporidium species. Clin. Gastroenterol. Hepatol. 2006;4:320–324. doi: 10.1016/j.cgh.2005.12.020. [DOI] [PubMed] [Google Scholar]
- Rubio J.M., Lanza M., Fuentes I., Soliman R.H. A novel nested multiplex PCR for the simultaneous detection and differentiation of Cryptosporidium spp., Enterocytozoon bieneusi and Encephalitozoon intestinalis. Parasitol. Int. 2014;63:664–669. doi: 10.1016/j.parint.2014.05.002. [DOI] [PubMed] [Google Scholar]
- Rusnak J., Hadfield T.L., Rhodes M.M., Gaines J.K. Detection of Cryptosporidium oocysts in human fecal specimens by an indirect immunofluorescence assay with monoclonal antibodies. J. Clin. Microbiol. 1989;27:1135–1136. doi: 10.1128/jcm.27.5.1135-1136.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan U., Paparini A., Oskam C. New Technologies for Detection of Enteric Parasites. Trends Parasitol. 2017;33:532–546. doi: 10.1016/j.pt.2017.03.005. [DOI] [PubMed] [Google Scholar]
- Ryan U., Hijjawi N., Xiao L. Foodborne cryptosporidiosis. Int. J. Parasitol. 2018 doi: 10.1016/j.ijpara.2017.09.004. [DOI] [PubMed] [Google Scholar]
- Sateriale A., Slapeta J., Baptista R., Kissinger J.C., Hunter C.A., Correspondence B.S. A genetically tractable, natural mouse model of cryptosporidiosis offers insights into host protective immunity. Cell Host Microbe. 2019;26 doi: 10.1016/j.chom.2019.05.006. 135-146.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddons C.A., Chapman P.A., Rush B.A. Evaluation of an enzyme immunoassay kit for detecting Cryptosporidium in faeces and environmental samples. J. Clin. Pathol. 1992;45:479–482. doi: 10.1136/jcp.45.6.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soave R., Danner R.L., Honig C.L., Ma P., Hart C.C., Nash T., Roberts R.B. Cryptosporidiosis in homosexual men. Ann. Intern. Med. 1984;100:504–511. doi: 10.7326/0003-4819-100-4-504. [DOI] [PubMed] [Google Scholar]
- Sparks H., Nair G., Castellanos-Gonzalez A., White A.C. Treatment of Cryptosporidium: what we know, gaps, and the way forward. Curr. Trop. Med. Reports. 2015 doi: 10.1007/s40475-015-0056-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark D., Al-Qassab S.E., Barratt J.L.N., Stanley K., Roberts T., Marriott D., Harkness J., Ellis J.T. Evaluation of multiplex tandem real-time PCR for Detection of Cryptosporidium spp., Dientamoeba fragilis, Entamoeba histolytica, and Giardia intestinalis in clinical stool samples. J. Clin. Microbiol. 2011;49:257–262. doi: 10.1128/JCM.01796-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark D., Roberts T., Ellis J.T., Marriott D., Harkness J. Evaluation of the EasyScreenTM enteric parasite detection kit for the detection of Blastocystis spp., Cryptosporidium spp., Dientamoeba fragilis, Entamoeba complex, and Giardia intestinalis from clinical stool samples. Diagn. Microbiol. Infect. Dis. 2014;78:149–152. doi: 10.1016/j.diagmicrobio.2013.10.013. [DOI] [PubMed] [Google Scholar]
- Stensvold C.R., Lebbad M., Verweij J.J. The impact of genetic diversity in protozoa on molecular diagnostics. Trends Parasitol. 2011;27:53–58. doi: 10.1016/j.pt.2010.11.005. [DOI] [PubMed] [Google Scholar]
- Sterling C., Arrowood M. Detection of Cryptosporidium sp. infctions using a direct imunofluorescent assay. Paediatr. Infect. Dis. 1986;5:139–142. doi: 10.1097/00006454-198601001-00022. [DOI] [PubMed] [Google Scholar]
- Stibbs H.H., Ongerth J.E. Immunofluorescence detection of Cryptosporidium oocysts in fecal smears. J. Clin. Microbiol. 1986;24:517–521. doi: 10.1128/jcm.24.4.517-521.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sulaiman I.M., Hira P.R., Zhou L., Faiza M., Al-shelahi F.A., Shweiki H.M., Al-ali F.M., Iqbal J. 2005. Unique Endemicity of Cryptosporidiosis in Children in Kuwait Unique Endemicity of Cryptosporidiosis in Children in Kuwait. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong S.Y.C., Giffard P.M. Microbiological applications of high-resolution melting analysis. J. Clin. Microbiol. 2012 doi: 10.1128/JCM.01709-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troeger C., Forouzanfar M., Rao P.C., Khalil I., Brown A., Reiner R.C., Fullman N., Thompson R.L., Abajobir A., Ahmed M., Alemayohu M.A., Alvis-Guzman N., Amare A.T., Antonio C.A., Asayesh H., Avokpaho E., Awasthi A., Bacha U., Barac A., Betsue B.D., Beyene A.S., Boneya D.J., Malta D.C., Dandona L., Dandona R., Dubey M., Eshrati B., Fitchett J.R.A., Gebrehiwot T.T., Hailu G.B., Horino M., Hotez P.J., Jibat T., Jonas J.B., Kasaeian A., Kissoon N., Kotloff K., Koyanagi A., Kumar G.A., Rai R.K., Lal A., El Razek H.M.A., Mengistie M.A., Moe C., Patton G., Platts-Mills J.A., Qorbani M., Ram U., Roba H.S., Sanabria J., Sartorius B., Sawhney M., Shigematsu M., Sreeramareddy C., Swaminathan S., Tedla B.A., Jagiellonian R.T.M., Ukwaja K., Werdecker A., Widdowson M.A., Yonemoto N., El Sayed Zaki M., Lim S.S., Naghavi M., Vos T., Hay S.I., Murray C.J.L., Mokdad A.H. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect. Dis. 2017 doi: 10.1016/S1473-3099(17)30276-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuli L., Singh D.K., Gulati A.K., Sundar S., Mohapatra T.M. A multiattribute utility evaluation of different methods for the detection of enteric protozoa causing diarrhea in AIDS patients. BMC Microbiol. 2010;10:11. doi: 10.1186/1471-2180-10-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyzzer E. An extracellular Coccidium, Cryptosporidium Muris (Gen. Et Sp. Nov.), of the gastric Glands of the Common Mouse. J. Med. Res. 1910;23:487–510.3. [PMC free article] [PubMed] [Google Scholar]
- Tzipori S., Widmer G. A hundred-year retrospective on cryptosporidiosis. Trends Parasitol. 2008;24:184–189. doi: 10.1016/j.pt.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungar B.L.P. Enzyme-linked immunoassay for detection of Cryptosporidium antigens in fecal specimens. J. Clin. Microbiol. 1990;28:2491–2495. doi: 10.1128/jcm.28.11.2491-2495.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uppal B., Singh O., Chadha S., Jha A.K. A comparison of nested PCR assay with conventional techniques for diagnosis of intestinal cryptosporidiosis in AIDS cases from northern India. J. Parasitol. Res. 2014;2014:706105. doi: 10.1155/2014/706105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Bossche D., Cnops L., Verschueren J., Van Esbroeck M. Comparison of four rapid diagnostic tests, ELISA, microscopy and PCR for the detection of Giardia lamblia, Cryptosporidium spp. and Entamoeba histolytica in feces. J. Microbiol. Methods. 2015;110:78–84. doi: 10.1016/J.MIMET.2015.01.016. [DOI] [PubMed] [Google Scholar]
- Vanee N., Roberts S.B., Fong S.S., Manque P., Buck G.A. A genome-scale metabolic model of Cryptosporidium hominis. Chem. Biodivers. 2010;7:1026–1039. doi: 10.1002/cbdv.200900323. [DOI] [PubMed] [Google Scholar]
- Varughese E.A., Bennett-Stamper C.L., Wymer L.J., Yadav J.S. A new in vitro model using small intestinal epithelial cells to enhance infection of Cryptosporidium parvum. J. Microbiol. Methods. 2014;106:47–54. doi: 10.1016/j.mimet.2014.07.017. [DOI] [PubMed] [Google Scholar]
- Verweij J.J., Van Lieshout L. Intestinal parasitic infections in an industrialized country; a new focus on children with better DNA-based diagnostics. Parasitology. 2011;138:1492–1498. doi: 10.1017/S0031182011001211. [DOI] [PubMed] [Google Scholar]
- Vinayak S., Pawlowic M.C., Sateriale A., Brooks C.F., Studstill C.J., Bar-Peled Y., Cipriano M.J., Striepen B. Genetic modification of the diarrhoeal pathogen Cryptosporidium parvum. Nature. 2015;523:477–480. doi: 10.1038/nature14651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vohra P., Sharma M., Chaudhary U. A comprehensive review of diagnostic techniques for detection of Cryptosporidium parvum in stool samples. IOSR J. Pharm. 2012;2:15–26. [Google Scholar]
- Wang R., Zhang L., Axén C., Bjorkman C., Jian F., Amer S., Liu A., Feng Y., Li G., Lv C., Zhao Z., Qi M., Dong H., Wang H., Sun Y., Ning C., Xiao L. Cryptosporidium parvum IId family: clonal population and dispersal from Western Asia to other geographical regions. Sci. Rep. 2015;4:4208. doi: 10.1038/srep04208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber R., Bryan R.T., Bishop H.S., Wahlquist S.P., Sullivan J.J., Juranek D.D. Threshold of detection of Cryptosporidium oocysts in human stool specimens: Evidence for low sensitivity of current diagnostic methods. J. Clin. Microbiol. 1991;29:1323–1327. doi: 10.1128/jcm.29.7.1323-1327.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzel T., Dittrich S., Möhl I., Adusu E., Jelinek T. Evaluation of seven commercial antigen detection tests for Giardia and Cryptosporidium in stool samples. Clin. Microbiol. Infect. 2006;12:656–659. doi: 10.1111/j.1469-0691.2006.01457.x. [DOI] [PubMed] [Google Scholar]
- Wessels E., Rusman L.G., van Bussel M.J.A.W.M., Claas E.C.J. Added value of multiplex Luminex Gastrointestinal Pathogen Panel (xTAG® GPP) testing in the diagnosis of infectious gastroenteritis. Clin. Microbiol. Infect. 2014;20 doi: 10.1111/1469-0691.12364. [DOI] [PubMed] [Google Scholar]
- Widmer G. Meta-analysis of a polymorphic surface glycoprotein of the parasitic protozoa Cryptosporidium parvum and Cryptosporidium hominis. Epidemiol. Infect. 2009;137:1800–1808. doi: 10.1017/S0950268809990215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widmer G., Sullivan S. Genomics and population biology of Cryptosporidium species. Parasite Immunol. 2012;34:61–71. doi: 10.1111/j.1365-3024.2011.01301.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao L. Molecular epidemiology of cryptosporidiosis: an update. Exp. Parasitol. 2010;124:80–89. doi: 10.1016/j.exppara.2009.03.018. [DOI] [PubMed] [Google Scholar]
- Xiao L., Feng Y. Molecular epidemiologic tools for waterborne pathogens Cryptosporidium spp. and Giardia duodenalis. Food Waterborne Parasitol. 2017;8–9:14–32. doi: 10.1016/J.FAWPAR.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu P., Widmer G., Wang Y., Ozaki L.S., Alves J.M., Serrano M.G., Puiu D., Manque P., Akiyoshi D., Mackey A.J., Pearson W.R., Dear P.H., Bankier A.T., Peterson D.L., Abrahamsen M.S., Kapur V., Tzipori S., Buck G.A. The genome of Cryptosporidium hominis. Nature. 2004;431:1107–1112. doi: 10.1038/nature02977. [DOI] [PubMed] [Google Scholar]
- Yang R., Paparini A., Monis P., Ryan U. Comparison of next-generation droplet digital PCR (ddPCR) with quantitative PCR (qPCR) for enumeration of Cryptosporidium oocysts in faecal samples. Int. J. Parasitol. 2014;44:1105–1113. doi: 10.1016/j.ijpara.2014.08.004. [DOI] [PubMed] [Google Scholar]
- Youn S., Kabir M., Haque R., Petri W.A. Evaluation of a screening test for detection of Giardia and Cryptosporidium parasites. J. Clin. Microbiol. 2009;47:451–452. doi: 10.1128/JCM.01736-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu F., Zhang K., Wang Y., Li D., Cui Z., Huang J., Zhang S., Li X., Zhang L. CRISPR/Cas12a-based on-site diagnostics of Cryptosporidium parvum IId-subtype-family from human and cattle fecal samples. Parasit. Vectors. 2021;14 doi: 10.1186/S13071-021-04709-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaglool D.A.M., Mohamed A., Khodari Y.A.W., Farooq M.U. Crypto-Giardia antigen rapid test versus conventional modified Ziehl-Neelsen acid fast staining method for diagnosis of cryptosporidiosis. Asian Pac J Trop Med. 2013;6:212–215. doi: 10.1016/S1995-7645(13)60025-5. [DOI] [PubMed] [Google Scholar]
- Zahedi A., Gofton A.W., Jian F., Paparini A., Oskam C., Ball A., Robertson I., Ryan U. Next Generation Sequencing uncovers within-host differences in the genetic diversity of Cryptosporidium gp60 subtypes. Int. J. Parasitol. 2017;47:601–607. doi: 10.1016/j.ijpara.2017.03.003. [DOI] [PubMed] [Google Scholar]
- Zahedi A., Gofton A.W., Greay T., Monis P., Oskam C., Ball A., Bath A., Watkinson A., Robertson I., Ryan U.M. Profiling the diversity of Cryptosporidium species and genotypes in wastewater treatment plants in Australia using next generation sequencing. Sci. Total Environ. 2018;644:635–648. doi: 10.1016/J.SCITOTENV.2018.07.024. [DOI] [PubMed] [Google Scholar]
- Zhang H., Morrison S., Tang Y.-W. Multiplex PCR tests for detection of pathogens associated with gastroenteritis. Clin. Lab. Med. 2015;35:461. doi: 10.1016/J.CLL.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]


