Abstract
Background
Little is known about the risk of admission for emergency department (ED) visits for ambulatory care sensitive conditions (ACSCs) by limited English proficient (LEP) patients.
Objective
Estimate admission rates from ED for ACSCs comparing LEP and English proficient (EP) patients and examine how these rates vary at hospitals with a high versus low proportion of LEP patients.
Design
Retrospective cohort study of California’s 2017 inpatient and ED administrative data
Participants
Community-dwelling individuals ≥ 18 years without a primary diagnosis of pregnancy or childbirth. LEP patients had a principal language other than English.
Main Measures
We used a series of linear probability models with incremental sets of covariates, including patient demographics, primary diagnosis, and Elixhauser comorbidities, to examine admission rate for visits of LEP versus EP patients. We then added an interaction covariate for high versus low LEP-serving hospital. We estimated models with and without hospital-level random effects.
Key Results
These analyses included 9,641,689 ED visits; 14.7% were for LEP patients. . Observed rate of admission for all ACSC ED visits was higher for LEP than for EP patients (26.2% vs. 25.2; p value < .001). Adjusted rate of admission was not statistically significant (27.3% [95% CI 25.4–29.3%] vs. 26.2% [95% CI 24.3–28.1%]). For COPD, the difference was significant (36.8% [95% CI 35.0–38.6%] vs. 33.3% [95% CI 31.7–34.9%]). Difference in adjusted admission rate for LEP versus EP visits did not differ in high versus low LEP-serving hospitals.
Conclusions
In adjusted analyses, LEP was not a risk factor for admission for most ACSCs. This finding was observed in both high and low LEP-serving hospitals.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-020-06523-5.
KEY WORDS: limited English proficiency, health disparities, ambulatory care sensitive conditions
INTRODUCTION
Twenty-five million people—8% of the US population—has limited English proficiency (LEP). Patients with LEP are more likely to be uninsured and are less likely to have access to regular primary care.1,2 The lack of an adequate healthcare workforce with language skills to meet the needs of patients and underutilization of professional interpreters despite federal mandates likely contribute to compromise in communication between clinicians and patients.3–5 Patients with LEP are more likely to report poor understanding of their medical care, lower satisfaction with care, and difficulty getting health information and advice over the phone.6–9 Consequently, patients with LEP may experience worse care.
LEP patients may have higher emergency department (ED) utilization even when empaneled in a primary care practice.10 They are more likely to be admitted than English proficient (EP) patients presenting with similar conditions.10–13 Much of this evidence comes from single-center studies. Additionally, few studies have examined if LEP patients have more preventable hospitalizations than EP patients.14
Admission for an ambulatory care sensitive condition (ACSC) is a quality metric used to identify potentially preventable admissions.15 Although this metric has been examined in regard to race/ethnicity and insurance status, few studies have examined if LEP patients are at increased risk for admission for ACSCs compared to English proficient patients.14 One study using 2013–2014 data from New Jersey found that LEP patients were less likely to be admitted for ACSCs as compared to English proficient patients.14 The extent to which this pattern generalizes to other states is unknown. Previous studies have not examined the impact of hospital factors on admission. The quality of services to support the needs of LEP patients, such as robust interpreter services, may impact admission rates. The availability of these services may be related to the volume of LEP patients at a hospital.
California has the highest proportion of residents with LEP of any state (19%).16,17 We used data from California to examine if the hospital admission rate for LEP patients differed from that for EP patients overall and for ACSCs. We additionally sought to examine if the disparity in admission rate between LEP and EP patients varied between hospitals that serve a higher versus lower percentage of LEP patients.
METHODS
Data source
Our primary data sources were California’s 2017 ED and inpatient discharge databases.18,19 We included data on hospital characteristics from the American Hospital Association (AHA) Annual Survey.
Study Sample
Our primary unit of analysis was an ED visit resulting in admission or discharge. We included ED visits to AHA-identified community hospitals for people aged ≥ 18 years whose presentation to an ED resulted in either a hospital admission or discharge. ED visits or admissions with a primary diagnosis of “pregnancy or childbirth or diseases occurring in the perinatal period” were also excluded as these patients are not included in analyses of potentially preventable hospitalizations. We also excluded individuals for whom key variables (e.g., principal diagnosis, preferred language) were missing. Hospitals with fewer than 100 ED visits, admission rate > 50%, less than 1% of an LEP population, or fewer than 200 LEP patient visits were also excluded to improve generalizability and model stability (Fig. 1).
Figure 1.
Analytic dataset and sensitivity analyses.
Primary Exposure of Interest
Any individual who selected a language other than English as the principal language used in communicating with healthcare providers was considered LEP.14,20,21 Those who selected English were considered English proficient. We further categorized LEP based on the most frequent languages in the dataset: Spanish, Chinese (Mandarin and Cantonese), Tagalog, Vietnamese, and other.
Outcomes of Interest
Our primary outcome was the proportion of ED visits resulting in admission. Our secondary outcome was the rate of admission for ACSCs.15 We used discharge diagnosis codes (ICD-10-CM) and the Agency for Healthcare Research and Quality (AHRQ)’s Prevention Quality Indicators algorithm to identify ACSCs.15 Specifically, we included admissions for ten conditions: diabetes with short-term complications, diabetes with long-term complications, uncontrolled diabetes without complications, chronic obstructive pulmonary disease, asthma, hypertension, heart failure, dehydration, bacterial pneumonia, or urinary tract infection. We did not include the admissions for amputation as this would always require inpatient admission. We categorized ACSCs into the following: (a) any ACSC; (b) acute ACSCs (dehydration, bacterial pneumonia, and urinary tract infection); and (c) chronic ACSCs (short-term and long-term complications of diabetes, chronic obstructive lung disease or asthma in older adults, hypertension, heart failure, uncontrolled diabetes, and asthma in younger adults).15 We also examined admission rates for each individual ACSC.
Covariates
Covariates included individual sex, age (18–30, 21–40, 41–50, 51–64, and ≥ 65), and race/ethnicity (Latino, non-Latino white, non-Latino Black, non-Latino Asian, and other). Those with unknown or missing race/ethnicity were categorized as “other.” As socioeconomic indicators, we used patient’s primary payor (commercial, Medicare, Medicaid, or other public insurance, self-pay, and other) and zip code median income for patient’s zip code of residence.22 We additionally included clinical characteristics that may influence admission decision: primary diagnosis, classified using ICD-10-CM Clinical Classification Software (CCS), and Elixhauser comorbidities.23,24
We included hospital-level characteristics: teaching status (yes/no), ownership (public, private for-profit, and private non-profit), hospital bed size (6–199 beds, 200–399, ≥ 400 beds), and safety net hospital (yes/no), which we defined as the top quartile of hospitals in California by proportion of patients covered by Medicaid. We grouped all hospitals into deciles by the proportion of LEP ED visits and defined the hospitals in the 60th percentile or greater as “high LEP-serving.”
Statistical Analyses
We performed chi-square and Student’s t tests for unadjusted analyses comparing visits for LEP and EP patients. We clustered patients at the hospital level and calculated the difference in admission rate overall and for ACSCs for LEP and EP patient visits. To obtain adjusted admission rates for LEP and EP patient visits, we estimated linear probability regression models with individual ED visit as the unit of observation and dichotomous indicator of admission as the outcome. We estimated a series of models, incrementally adding covariates, to enable better interpretation of the role of different covariate domains. First, we adjusted for age, sex, race/ethnicity, primary discharge diagnosis, and Elixhauser comorbidities. We then added insurance type, zip code income quartile, and patient county-level fixed effects. Finally, we included hospital characteristics, and to adjust for clustering at specific hospitals, we used random effects. For all models, we obtained standard errors clustered at the hospital level.25 These models were estimated separately for all ED visits and subgroups of ACSCs. Adding interaction terms for high and low LEP-serving hospitals to the linear probability regression models, we estimated the difference in adjusted admission rates between LEP and EP patients in high LEP-serving versus low LEP-serving hospitals.
Sensitivity Analyses
We examined if repeated ED visits across individuals affected our estimates. For this, we selected the subgroup of observations with a valid patient ID (n = 8,615,842, 89.4 %). Among the subgroup of patients with two or more ED visits, we randomly selected one visit per patient. We estimated the linear probability models for this subgroup of observations. We also examined sensitivity of our estimates to the choice of cutoff in defining high and low LEP-serving hospitals; we examined alternative cutoffs of 70th percentile and 50th percentile. Analyses were performed using SAS (version 9.4) and Stata (version 15.1). This study was approved by the IRB at Boston University School of Medicine.
RESULTS
There were 9,641,689 ED visits included in our sample, of which14.7% were for patients with LEP (Table 1). LEP patients were more likely to be female (58.8% vs. 53.9%, p < .0001), older (mean age 54.7 vs. 48.7, p < .0001), and more likely to identify as Latino (76.0% vs. 27.6%, p < .0001). Those with LEP were more likely to have Medicaid insurance (47.6% vs. 35.7%, p value < .0001). They were also more likely to reside in a zip code in the lowest income quartile (13.8% vs. 26.6%, p value < .0001), and more likely to have a visit at a safety net hospital (29.9% vs. 22.8%, p < .0001).
Table 1.
Sample Characteristics by LEP and English Proficiency
| Variable | LEP n = 1,421,385 |
EP n = 8,220,304 |
p value |
|---|---|---|---|
| Female | 58.8% | 53.% | < .0001 |
| Age category | < .0001 | ||
| 18–30 | 9.28% | 23.09% | |
| 31–40 | 14.22% | 16.45% | |
| 41–50 | 18.30% | 13.99% | |
| 51–64 | 26.86% | 22.52% | |
| ≥ 65 | 31.34% | 23.95% | |
| Age mean (ST) | 54.7 (18.7) | 48.7 (20.5) | < .0001 |
| Race/ethnicity | < .0001 | ||
| White | 6.0% | 46.4% | |
| African-American | 0.3% | 13.2% | |
| Latino | 76.0% | 27.6% | |
| Asian | 10.8% | 5.1% | |
| Other/unknown/missing | 6.9% | 7.8% | |
| Language | N/A | ||
| English | N/A | 100% | |
| Spanish | 80.2% | N/A | |
| Vietnamese | 2.7% | N/A | |
| Mandarin/Cantonese | 2.0% | N/A | |
| Tagalog | 1.4% | N/A | |
| Other | 13.6% | N/A | |
| Insurance | < .0001 | ||
| Commercial | 13.8% | 26.6% | |
| Medicaid | 47.6% | 35.7% | |
| Medicare | 27.5% | 28.1% | |
| Other | 2.8% | 3.4% | |
| Self-pay | 8.4% | 6.1% | |
| Zip code income quartiles (lowest to highest) | < .0001 | ||
| 1st | 33.9% | 24.3% | |
| 2nd | 28.7% | 24.0% | |
| 3rd | 22.7% | 25.4% | |
| 4th | 14.8% | 26.4% | |
| Hospital ownership | < .0001 | ||
| Government non-federal | 26.7% | 17.5% | |
| Non-government not for profit | 60.6% | 69.2% | |
| Investor owned (for profit) | 12.7% | 13.3% | |
| Teaching hospital | < .0001 | ||
| Yes | 12.2% | 8.1% | |
| Safety net hospital | < .0001 | ||
| Yes | 29.9% | 22.8% | < .0001 |
| Hospital size | < .0001 | ||
| 6–199 beds | 34.3% | 34.1% | |
| 200–399 beds | 44.0% | 45.8% | |
| ≥ 400 beds | 21.8% | 20.1% | |
| Admission rate | 26.2% | 25.2% | < .0001 |
| Admission rate by ACSC | |||
| Overall | 18.9% | 16.1% | < .0001 |
| Acute condition | 18.7% | 18.1% | < .0001 |
| Chronic condition | 34.5% | 32.2% | < .0001 |
| Diabetes short-term complications | 54.0% | 70.9% | < .0001 |
| Diabetes long-term complications | 54.4% | 54.0% | 0.46 |
| COPD or asthma in older adults | 37.8% | 31.8% | < .0001 |
| Hypertension | 13.9% | 11.7% | < .0001 |
| Heart failure | 72.1% | 66.2% | < .0001 |
| Dehydration | 48.7% | 39.7% | < .0001 |
| Community-acquired pneumonia | 34.1% | 30.1% | < .0001 |
| Urinary tract infection | 8.9% | 8.3% | < .0001 |
| Uncontrolled diabetes | 16.4% | 16.1% | 0.39 |
| Asthma in younger adult | 33.7% | 17.9% | < .0001 |
LEP, limited English proficient; EP, English proficient; ACSC, ambulatory care sensitive condition
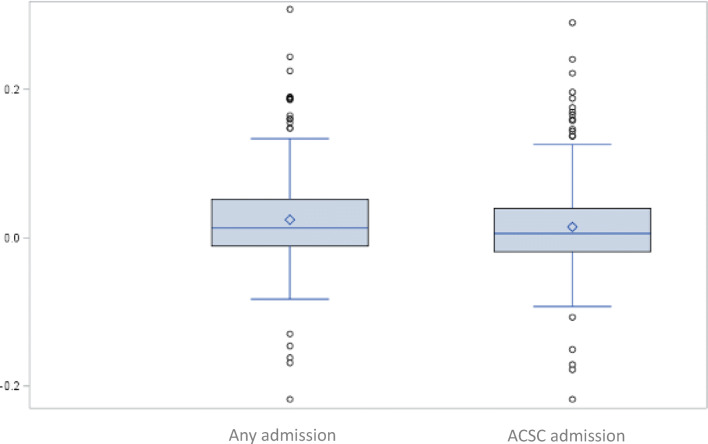
In unadjusted analyses, visits for LEP patients were more likely to result in an admission overall, for any ACSC, for any acute ACSC, and for any chronic ACSC (26.2% vs. 25.2; 18.9% vs. 16.1%; 18.7% vs. 18.1%; 34.5% vs. 32.2%, all p values < .0001) (Table 1). LEP patients were more likely to be admitted for COPD or asthma in an older adult and hypertension, heart failure, dehydration, community-acquired pneumonia, urinary tract infections, and asthma in a younger adult. LEP patients were less likely to be admitted for diabetes with short-term complications (54.0% vs. 70.9%, p < .0001) (Table 1). Hospitals varied in their disparity in admission rates for LEP and EP patient visits. The median difference in hospital-level admission rate was 1.3% (i.e., more LEP patients were admitted than EP patients) with an inter-quartile range (IQR) of − 1.1 to 5.1%. For ACSCs, the median difference was − 1.1% (i.e., fewer LEP patients were admitted than EP patients) with an IQR of − 4.6 to 3.3% (Fig. 2).
Figure 2.
Distribution of difference in admission rate at each hospital, between limited English proficient patient visits and English proficient patient visits: any admission and ACSC admissions.
Table 2 reports the adjusted rate of admission for LEP and EP patients. LEP patients were more likely to be admitted for any condition (17.8% [95% CI 17.1–18.6%] vs. 16.3% [95% CI 15.6–17.0%]), but this difference was no longer statistically significant when adjusted for hospital-level clustering (model 3). LEP patients were also more likely to be admitted for any ACSC (27.4% [95% CI 26.2–28.7%] vs. 25.0% [95% CI 23.9–26.1%]) but this difference was no longer significant when insurance type, visit quarter, patient county fixed effects, and zip code income quartile were added to the model (model 2). There was no significant difference in admission for acute ACSCs (models 1–3). LEP patients were more likely to be admitted for chronic ACSCs (35.6% [95% CI 34.1–37.0%] vs. 32.0% [95% CI 30.7–33.3%]), but this difference was no longer statistically significant when hospital-level factors were added to the model (model 3).
Table 2.
Adjusted Emergency Department Encounter Admission Rates for Visits of Limited English Proficient Patients Versus English Proficient Patient Visits, Overall and for Ambulatory Care Sensitive Conditions
| Model 1* | Model 2‡ | Model 3§ | |
|---|---|---|---|
| Adjusted percentage 95% CI |
Adjusted percentage 95% CI |
Adjusted percentage 95% CI |
|
| Admission | |||
| LEP |
17.8% 17.1%, 18.6% |
17.8% 17.1%, 18.6% |
17.8% 14.5%, 19.2% |
| EP |
16.3% 15.6%, 17.0% |
16.3% 15.6%, 17.0% |
16.9% 15.4%, 20.2% |
| ACSC admission | |||
| LEP |
27.4% 26.2%, 28.7% |
27.1% 25.9%, 28.2% |
27.3% 25.4%, 29.3% |
| EP |
25.0% 23.9%, 26.1% |
25.0% 24.0%, 26.1% |
26.2% 24.3%, 28.1% |
| Acute ACSC admission | |||
| LEP |
19.7% 18.7%, 20.8% |
19.6% 18.5%, 20.6% |
19.7% 18.4%, 21.1% |
| EP |
17.9% 17.0%, 18.7% |
17.9% 17.1%, 18.7% |
18.6% 17.4%, 19.9% |
| Chronic ACSC admission | |||
| LEP |
35.6% 34.1%, 37.0% |
35.1% 33.8%, 36.4% |
35.4% 31.6%, 35.5% |
| EP |
32.0% 30.7%, 33.3% |
32.1% 30.9%, 33.3% |
33.6% 33.4%, 37.5% |
Bold indicates statistically significant at a level of p < .05
LEP, limited English proficient; EP, English proficient; ACSC, ambulatory care sensitive condition
*Model 1: age, sex, race, primary diagnosis, Elixhauser comorbidities, with standard errors clustered at hospital level. In models of ACSCs, primary diagnosis was not included
‡Model 2: Model 1 and insurance type, quarter, zip code income quartile, patient county of residence, with standard errors clustered at the hospital level. In models of ACSCs, primary diagnosis was not included
§Model 3: Model 2 and hospital teaching status, hospital ownership, hospital random effects, and with standard errors clustered at the hospital level. In models of ACSCs, primary diagnosis was not included
Evaluated for individual ACSCs, LEP patients were more likely to be admitted for COPD or asthma in older adults and this finding was significant in all models (36.8% [95% CI 35.0–38.6%] vs. 33.3% [95% CI 31.7–34.9%]). For none of the other ACSCs was the estimated difference in likelihood of admission between LEP and EP patients statistically significant in the fully adjusted models (Table 3).
Table 3.
Adjusted Emergency Department Encounter Admission Rates for Visits of Limited English Proficient Patients Versus English Proficient Patient Visits for Specific Ambulatory Care Sensitive Conditions
| ACSC | Model 3* |
|---|---|
| Adjusted percentage 95% CI | |
| Diabetes short-term complication | |
| LEP |
69.7% 68.9%, 72.4% |
| EP |
70.6% 67.1%, 72.3% |
| Diabetes long-term complication | |
| LEP |
55.8% 54.0%, 57.6% |
| EP |
54.5% 52.8%, 56.3% |
| COPD or asthma in older adults | |
| LEP |
36.8% 35.0%, 38.6% |
| EP |
33.3% 31.7%, 34.9% |
| Hypertension | |
| LEP |
13.7% 12.8%, 14.7% |
| EP |
12.2% 11.5%, 13.0% |
| Heart failure | |
| LEP |
69.8% 67.6%, 72.0% |
| EP |
67.1% 65.1%, 69.0% |
| Dehydration | |
| LEP |
42.6% 40.8%, 44.3% |
| EP |
41.6% 40.0%, 43.1% |
| Community-acquired pneumonia | |
| LEP |
33.2% 31.5%, 35.0% |
| EP |
31.2% 29.7%, 32.6% |
| Urinary tract infection | |
| LEP |
9.5% 8.6%, 10.4% |
| EP |
8.9% 8.0%, 9.7% |
| Uncontrolled diabetes | |
| LEP |
18.8% 17.4%, 20.2% |
| EP |
17.5% 16.3%, 18.7% |
| Asthma in younger adult | |
| LEP |
19.4% 18.3%, 20.5% |
| EP |
19.4% 18.9%, 19.9% |
Bold indicates statistically significant at a level of p < .05.
LEP, limited English proficient; EP, English proficient; ACSC, ambulatory care sensitive condition
*Model 3: Model 2 and hospital teaching status, hospital ownership, hospital random effects, and with standard errors clustered at the hospital level. Primary diagnosis not included in models with ACSCs
Table 4 gives estimated difference in the admission rate for LEP versus EP patients across hospitals grouped as high and low LEP-serving. The estimated difference in admission rate in low LEP-serving hospitals was 1.3% (95% CI 1.0–1.7%) versus 0.7% (95% CI 0.3–1.2%) in high LEP-serving hospitals. For ACSCs, the differences in admission rates for low and high LEP-serving hospitals were similar.
Table 4.
Differences in Emergency Department Encounter Admission Rates for Limited English Proficient Versus English Proficient Patients in High Versus Low Limited English Proficient-Serving Hospitals
| Model 4* | |
|---|---|
| Adjusted percentage 95% CI | |
| Admission | |
| Difference in admission rate: low LEP-serving hospital† |
1.3% 1.0%, 1.7% |
| Difference in admission rate: high LEP-serving hospital‡ |
0.7% 0.3%, 1.2% |
| ASCS admission | |
| Difference in admission rate: low LEP-serving hospital† |
1.3% 0.8%, 1.9% |
| Difference in admission rate: high LEP-serving hospital‡ |
1.1% 0.5%, 1.8% |
| Acute ACSC | |
| Difference in admission rate: low LEP-serving hospital† |
1.3% 0.7%, 1.8% |
| Difference in admission rate: high LEP-serving hospital‡ |
1.0% 0.4%, 1.6% |
| Chronic ACSC | |
| Difference in admission rate: low LEP-serving hospital† |
1.8% 1.0%, 2.5% |
| Difference in admission rate: high LEP-serving hospital‡ |
2.0% 1.1%, 2.8% |
LEP, limited English proficient; ACSC, ambulatory care sensitive condition
*Adjusting for age, sex, race, insurance type, quarter, zip code income quartile, clinical classification software primary diagnosis, Elixhauser comorbidities, hospital teaching status, hospital ownership. LEP patient at low LEP-serving hospital is referent. Standard errors are clustered at the hospital level. In models with ACSCs, primary diagnosis not included
†A low LEP-serving hospital is one in which fewer than 20% of visits are for LEP patients, which is also hospitals below the 6th decile for proportion of visits where the patient has LEP
‡A high LEP-serving hospital is one in which 20% or greater of visits are for LEP patients, which is also hospitals in the 6th decile or above for proportion of visits where the patient has LEP
Analyses of specific languages demonstrated variable admission rates for chronic ACSCs, short-term complications for diabetes, long-term complications for diabetes, COPD, hypertension, urinary tract infections, and uncontrolled diabetes. Admission rates for those who spoke Mandarin/Cantonese, those who spoke Vietnamese, and those whose language was categorized as “other” were the language groups for which there was a significant difference in admission rate compared to English (Appendix Table 1). Adjusting the cutoff for LEP-serving hospital did not alter results in any meaningful way (Appendix Tables 2 and 3). Sensitivity analyses among those with a valid patient ID and at the individual patient level were consistent with the overall analysis (Appendix Tables 4 and 5).
DISCUSSION
Using California statewide data, we found that older adult LEP patients presenting with COPD or asthma were more likely to be admitted than EP patients presenting with the same diagnosis codes even after accounting for patient and hospital factors. Patients with LEP were more likely to be admitted to the hospital than EP patients for any admission, for any ACSC, and for chronic ACSCs. However, the difference in admission rate for acute ACSCs was not significant when adjusted for socioeconomic factors. The difference between LEP and EP patients in overall admission rates and admission for most chronic ACSCs was not significant when adjusted for hospital factors, indicating that differences in the hospitals where LEP and EP patients received care may be associated with the unadjusted (observed) differences in admission rates.
Counter to our hypothesis, there was no significant difference in admission rates in the fully adjusted models for most ACSCs, and in cases where there was a difference, the difference was quite small. It is possible that data on principal language did not adequately capture those who experience language barriers in healthcare. An individual may be proficient in English but report another principal language and this would bias the results towards the null. Alternatively, compared to other states, California may be providing more effective care to their LEP population than other states with a high proportion of LEP residents. California has made concerted efforts at the state level to address the care of LEP patients. In 2005, California developed the healthcare interpreter network to provide video and voice interpretation to public hospitals and clinics that serve the California Medicaid population.26 The Health Care Language Assistance Act which went into full effect in 2009 holds health plans accountable for the provision of language services and requires health plans and health insurers to provide their enrollees with interpreter services and translated material.27
Accordingly, state-specific policies may explain why our results differed from those of Anderson et al. who evaluated the impact of language and admission for ACSCs in New Jersey and found a lower admission rate for those with LEP.14 They hypothesized LEP patients may be more likely to turn to the ED for non-urgent primary care issues while EP patients would first seek outpatient care and only present to the ED for more severe issues. While both studies controlled for insurance, it is possible that Californians with LEP have, on average, more established connections in primary care than those in New Jersey and that this resulted in minimal difference in admission for acute ACSCs between LEP and EP patients in California but persistent differences for some chronic ACSCs.14 Although these differences were quite small in percentage terms, they represent large spending given the high volumes and high cost of an ED visit ($1106) and inpatient stay ($14,892). 28 The differences in admission rates for chronic ACSCs are consistent with prior literature demonstrating poorer chronic disease management for those with LEP even with access to primary care.29–31 This finding may reflect factors beyond access to care such as health literacy, ability to afford medications, or difficulty understanding provider’s instructions around disease management due to language barriers. Our findings may also differ from those of Anderson et al. because the predominant languages in New Jersey differ from those in California; distinct sociolinguistic contexts may influence cultural differences in how people interact with the healthcare system.
Contrary to our hypothesis, hospitals serving a higher portion of LEP patients did not do better than hospitals serving a lower portion of LEP patients. One explanation for this finding may be that having a high proportion of LEP patients does not necessarily result in improved care for this population. These hospitals may not be overcoming language barriers possibly due to a shortage of interpreters for the high demand or underutilization of interpreters for other reasons.5,32–34 The range in disparity in admission between hospitals warrants further research to understand what other hospital characteristics contribute to disparities in admission rates between LEP and EP patients. Our study also demonstrates that a major driver of difference in admission rates relates to which hospital LEP and EP patients present. Further research is needed to understand what factors lead LEP and EP patients to different hospitals.
We also found that admission rates for some ACSCs varied by specific language. One reason for this difference may be the linguistic capabilities of providers, as language-concordant care has been shown to improve outcomes.35–39 About 30% of physicians in California speak Spanish while only 3% speak Cantonese, 6% Mandarin, 6% Tagalog, and 4% Vietnamese.3 Some of the variability by language may be a reflection of sociocultural differences in conception of illness and self-care; such factors can influence when patients present to emergency departments, how they describe their symptoms, and the likelihood of admission.40,41
Our study has several limitations. First, it may be inappropriate to extrapolate our findings to other states where the predominant languages may differ from those of California and where state policies may differ. Second, although we were able to control for comorbidities, which may influence risk of admission, we were unable to control for acuity at presentation. Additionally, we were not able to measure characteristics of patients’ primary care environments. Third, because of the high proportion of LEP patients without a person-level indicator, we are unable to adjust for person-level clustering of ED visits. However, our subgroup analysis for people with person-level indicators exhibited consistent results. Fourth, our indicators for income were area level and therefore may not accurately represent the socioeconomic status of the individual patient. Additionally, we were not able to identify dual enrolled (Medicare/Medicaid) individuals. Finally, principal language as captured by these data cannot be confirmed; it is possible that some individuals who were identified as LEP in fact spoke English and some who identified as English speaking were in fact LEP.42
Using data from California, we found that patients with LEP are at a small but significant increased risk for admission from the emergency department for COPD or asthma in older adults but no other ACSCs in fully adjusted models. The disparity in admission rate between LEP and EP patients was not different between hospitals that serve higher versus lower proportions of LEP patients. More research is needed to understand what factors impact differences in admission rates for ACSCs between LEP and EP patients.
Supplementary Information
(DOCX 34 kb)
Acknowledgments
The authors would like to acknowledge Lisa Marks for her technical support.
Funding
This work was supported in part by a Health Resources and Services Administration’s National Research Service Award (T32HP10028) (Dr. Schulson), Agency for Healthcare Research and Quality Award (T32HS022242) (Dr. Lin), and National Institute on Minority Health and Health Disparities Grant R01MD011594 (Dr. Hanchate).
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lu T, Myerson R. Disparities in Health Insurance Coverage and Access to Care by English Language Proficiency in the USA, 2006–2016. J Gen Intern Med. 2020. 10.1007/s11606-019-05609-z [DOI] [PMC free article] [PubMed]
- 2.DuBard CA, Gizlice Z. Language spoken and differences in health status, access to care, and receipt of preventive services among US Hispanics. Am J Public Health. 2008;98(11):2021–2028. doi: 10.2105/AJPH.2007.119008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garcia ME, Bindman AB, Coffman J. Language-Concordant Primary Care Physicians for a Diverse Population: The View from California. Health Equity. 2019;3(1):343–349. doi: 10.1089/heq.2019.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diamond LC, Tuot DS, Karliner LS. The Use of Spanish Language Skills by Physicians and Nurses: Policy Implications for Teaching and Testing. J Gen Intern Med. 2012;27(1):117–123. doi: 10.1007/s11606-011-1779-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schenker Y, Pérez-Stable EJ, Nickleach D, Karliner LS. Patterns of interpreter use for hospitalized patients with limited English proficiency. J Gen Intern Med. 2011;26(7):712–717. doi: 10.1007/s11606-010-1619-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calo WA, Cubillos L, Breen J, et al. Experiences of Latinos with limited English proficiency with patient registration systems and their interactions with clinic front office staff: an exploratory study to inform community-based translational research in North Carolina. BMC Health Serv Res. 2015;15(1). 10.1186/s12913-015-1235-z [DOI] [PMC free article] [PubMed]
- 7.Regan FR. Primary care for limited English-speaking patients and parents. J Am Assoc Nurse Pract. 2015;27(3):167–176. doi: 10.1002/2327-6924.12148. [DOI] [PubMed] [Google Scholar]
- 8.Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. Are Latinos less satisfied with communication by health care providers? J Gen Intern Med. 1999;14(7):409–417. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pippins JR, Alegría M, Haas JS. Association between language proficiency and the quality of primary care among a national sample of insured Latinos. Med Care. 2007;45(11):1020–1025. doi: 10.1097/MLR.0b013e31814847be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Njeru JW, St Sauver JL, Jacobson DJ, et al. Emergency department and inpatient health care utilization among patients who require interpreter services. BMC Health Serv Res. 2015;15:214. doi: 10.1186/s12913-015-0874-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schulson L, Novack V, Smulowitz PB, Dechen T, Landon BE. Emergency Department Care for Patients with Limited English Proficiency: a Retrospective Cohort Study. J Gen Intern Med Published online September 5, 2018. 10.1007/s11606-018-4493-8 [DOI] [PMC free article] [PubMed]
- 12.Gallagher RA, Porter S, Monuteaux MC, Stack AM. Unscheduled return visits to the emergency department: the impact of language. Pediatr Emerg Care. 2013;29(5):579–583. doi: 10.1097/PEC.0b013e31828e62f4. [DOI] [PubMed] [Google Scholar]
- 13.Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language barriers and resource utilization in a pediatric emergency department. Pediatrics. 1999;103(6 Pt 1):1253–1256. doi: 10.1542/peds.103.6.1253. [DOI] [PubMed] [Google Scholar]
- 14.Anderson TS, Karliner LS, Lin GA. Association of Primary Language and Hospitalization for Ambulatory Care Sensitive Conditions. Med Care. 2020;58(1):45–51. doi: 10.1097/MLR.0000000000001245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agency for Healthcare Research and Quality. Prevention quality indicators overview. 2018. https://www.qualityindicators.ahrq.gov/modules/pqi_resources.aspx
- 16.Zong J, Batalova J. The Limited English Proficient Population in the United States. Migr Policy Inst Published online July 8, 2015. https://www.migrationpolicy.org/article/limited-english-proficient-population-united-states
- 17.American Community Survey. California Department of Finance Estimates and Projections; US Census Bureau Estimates; Decennial Censuses.; 2017.
- 18.California Emergency Department & Ambulatory Surgery Data Reporting Manual. 5th ed. Office of Statewide Health Planning and Development; 2020. https://oshpd.ca.gov/data-and-reports/submit-data/patient-data/edas-reporting/
- 19.Inpatient Discharge Reporting. Office of Statewide Health Planning and Development; 2020. https://oshpd.ca.gov/data-and-reports/submit-data/patient-data/inpatient-reporting/
- 20.Biswas S, Dinh D, Lucas M, et al. Impact of limited English proficiency on presentation and clinical outcomes of patients undergoing primary percutaneous coronary intervention. Eur Heart J - Qual Care Clin Outcomes. Published online November 29, 2019:qcz061. 10.1093/ehjqcco/qcz061 [DOI] [PubMed]
- 21.Hines A, Andrews R, Moy E, Barrett M, Coffey R. Disparities in Rates of Inpatient Mortality and Adverse Events: Race/Ethnicity and Language as Independent Contributors. Int J Environ Res Public Health. 2014;11(12):13017–13034. doi: 10.3390/ijerph111213017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Community Survery 2012-2016. United States Census Bureau
- 23.Centers for Disease Control and Prevention. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Published online 2017. Accessed March 5, 2018. http://www.cdc.gov/nchs/icd/icd9cm. htm.
- 24.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Colin Cameron A, Miller DL. A Practitioner’s Guide to Cluster-Robust Inference. J Hum Resour. 2015;50(2):317–372. doi: 10.3368/jhr.50.2.317. [DOI] [Google Scholar]
- 26.Health Care Interpreter Network. Healthcare Interpreter Network: About Us. . http://www.hcin.org/
- 27.Escutia, Perata. The Health Care Language Access Act (SB 853).; 2003.
- 28.Access and Cost Trends, Medical Expenditure Panel Survey, 2017. Agency for Healthcare Research and Quality; 2017.
- 29.Wisnivesky JP, Krauskopf K, Wolf MS, et al. The association between language proficiency and outcomes of elderly patients with asthma. Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol. 2012;109(3):179–184. doi: 10.1016/j.anai.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 30.Kim EJ, Kim T, Paasche-Orlow MK, Rose AJ, Hanchate AD. Disparities in Hypertension Associated with Limited English Proficiency. J Gen Intern Med. 2017;32(6):632–639. doi: 10.1007/s11606-017-3999-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seman M, Karanatsios B, Simons K, et al. The impact of cultural and linguistic diversity on hospital readmission in patients hospitalized with acute heart failure. Eur Heart J - Qual Care Clin Outcomes. Published online July 23, 2019:qcz034. 10.1093/ehjqcco/qcz034 [DOI] [PubMed]
- 32.Mayo R, Parker VG, Sherrill WW, et al. Cutting Corners: Provider Perceptions of Interpretation Services and Factors Related to Use of an Ad Hoc Interpreter. Hisp Health Care Int. 2016;14(2):73–80. doi: 10.1177/1540415316646097. [DOI] [PubMed] [Google Scholar]
- 33.Hsieh E. Not just “getting by”: factors influencing providers’ choice of interpreters. J Gen Intern Med. 2015;30(1):75–82. doi: 10.1007/s11606-014-3066-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ramirez D, Engel KG, Tang TS. Language interpreter utilization in the emergency department setting: a clinical review. J Health Care Poor Underserved. 2008;19(2):352–362. doi: 10.1353/hpu.0.0019. [DOI] [PubMed] [Google Scholar]
- 35.Fernandez A, Schillinger D, Warton EM, et al. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE) J Gen Intern Med. 2011;26(2):170–176. doi: 10.1007/s11606-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ngo-Metzger Q, Sorkin DH, Phillips RS, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007;22(Suppl 2):324–330. doi: 10.1007/s11606-007-0340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Villalobos BT, Bridges AJ, Anastasia EA, Ojeda CA, Rodriguez JH, Gomez D. Effects of language concordance and interpreter use on therapeutic alliance in Spanish-speaking integrated behavioral health care patients. Psychol Serv. 2016;13(1):49–59. doi: 10.1037/ser0000051. [DOI] [PubMed] [Google Scholar]
- 38.Green AR, Ngo-Metzger Q, Legedza ATR, Massagli MP, Phillips RS, Iezzoni LI. Interpreter services, language concordance, and health care quality. Experiences of Asian Americans with limited English proficiency. J Gen Intern Med. 2005;20(11):1050–1056. doi: 10.1111/j.1525-1497.2005.0223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Diamond L, Izquierdo K, Canfield D, Matsoukas K, Gany F. A Systematic Review of the Impact of Patient-Physician Non-English Language Concordance on Quality of Care and Outcomes. J Gen Intern Med. 2019;34(8):1591–1606. doi: 10.1007/s11606-019-04847-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yeheskel A, Rawal S. Exploring the “Patient Experience” of Individuals with Limited English Proficiency: A Scoping Review. J Immigr Minor Health. 2019;21(4):853–878. doi: 10.1007/s10903-018-0816-4. [DOI] [PubMed] [Google Scholar]
- 41.Shaw SJ, Huebner C, Armin J, Orzech K, Orzech K, Vivian J. The role of culture in health literacy and chronic disease screening and management. J Immigr Minor Health. 2009;11(6):460–467. doi: 10.1007/s10903-008-9135-5. [DOI] [PubMed] [Google Scholar]
- 42.Klinger EV, Carlini SV, Gonzalez I, et al. Accuracy of race, ethnicity, and language preference in an electronic health record. J Gen Intern Med. 2015;30(6):719–723. doi: 10.1007/s11606-014-3102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 34 kb)