Abstract
Purpose of Review
Proximal femur fractures are common traumatic injuries treated by orthopedic surgeons. Preparation and positioning for surgical intervention are critical in the proper management of proximal femur fractures. The purpose of this study was to review the current evidence on the various positioning options for patients and to highlight the principles and emerging techniques to help orthopedic surgeons treat this common injury.
Recent Findings
Strategic patient positioning is key to the reduction and fixation of proximal femur fractures without complications. The use of intramedullary devices for the fixation of proximal femur fractures has led to an increased use of the modern fracture table. The fracture table should be used when surgeons are facile with its use to avoid significant complications. Recent best available evidence has suggested increased risk of malrotation associated with the use of the fracture table. The use of the radiolucent table offers the most flexibility, but limits surgeons as multiple assistants are needed to maintain reduction during fixation.
Summary
Positioning for proximal femur fractures is an important technique for general and trauma orthopedic surgeons. Surgeons need to be aware of the various techniques for positioning of proximal femur fractures due to the diversity of injury patterns and patient characteristics. Each positioning technique has it benefits and potential complications that every orthopaedic surgeon should be familiar with while treating these injuries.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12178-021-09710-x.
Keywords: Hip fracture, Proximal femur fracture, Patient positioning
Introduction
Fractures of the proximal femur are among the most common traumatic injuries addressed by orthopedic surgeons [1]. These fractures include fractures of the femoral neck through the trochanteric region to the proximal shaft and demonstrate a continuum from nondisplaced simple fractures to highly comminuted fracture patterns caused by osteoporosis or high-energy trauma. Proximal femoral fractures can be treated with a variety of treatment modalities including internal fixation with an intramedullary or extramedullary device, hemiarthroplasty, or total hip arthroplasty. This review addresses the principles of patient positioning: the pearls, the pitfalls, and the emerging techniques to help the orthopedic surgeon stabilize the proximal femur.
Significant morbidity and mortality are associated with hip fractures, and this has led to an emphasis on prompt fixation and early ambulation, especially for elderly patients [2]. Lengthy immobilization is known to increase risk of pneumonia, delirium, DVTs, cardiac failure, muscular decompensation, and perioperative mortality [3]. While planning for early fixation, the surgeon must consider coexisting goals of operative time, predicted blood loss, and minimization of soft tissue trauma. This is especially true for polytrauma patients with either multiple extremity injuries or trauma to the head, chest, or abdomen. Safe management of polytrauma patients involves active coordination with all involved services in order to ensure preoperative stabilization and postoperative resuscitative management [4].
Options for fixation of proximal femur fractures have changed dramatically over the past century. The dynamic hip screw was one of the early devices designed to treat intertrochanteric hip or valgus impacted femoral neck fractures [5]. Fixation of proximal femur fractures with a dynamic hip screw is still a viable and cost-effective method particularly for stable fracture patterns. Initial femoral intramedullary fixation began with straight rods, before contoured intramedullary devices and cephalomedullary devices were introduced [6].
Intramedullary nailing is now considered the standard of care for most femoral shaft fractures, while most peritrochanteric hip fractures are treated with a dynamic hip screw or an intramedullary hip screw, depending on stability and integrity of the lateral femoral cortex [7]. Intramedullary fixation is associated with efficient operative time and immediate return to weight bearing in most patients [8•]. The modern fracture table and the development of mobile fluoroscopy have greatly aided efficient and accurate fixation with intramedullary devices. For fractures that are not amenable to intramedullary fixation, plate fixation remains a viable option. While intramedullary fixation remains the gold standard for most fractures, these principles may need to be modified in the setting of severe fracture comminution, unstable polytrauma, intracranial injuries, or severely open fractures [9].
The Orthopedic Fracture Table
The fracture table, also known as a traction table, was described as early as 1913, as a means to “afford reliable support and traction of the lower limbs in the treatment of fractures [10].” Modern fracture tables consist of a central body with a perineal post to hold the patient’s upper body against axial traction, and articulating arms that allow for the manipulation of the lower extremities. These tables have become popular not only for lower extremity orthopedic trauma, but also for a variety of procedures including hip arthroscopy and arthroplasty [11]. This often enables a single surgeon to complete an operation with fewer assistants [12]. Once a patient has been positioned on the table, the injured leg may be taken through a common series of maneuvers to aid in fracture reduction and locked into position.
A patient may be placed in a variety of positions on a fracture table, including supine in hemilithotomy position, supine with both legs extended, lateral with the operative leg elevated, or prone. For most hip and femur fractures, the first two positions are used; these are described below. Table 1
Table 1.
Advantages and disadvantages of each common intraoperative patient position
| Position | Advantages | Disadvantages |
|---|---|---|
| Fracture table, hemilithotomy |
No need for assistant to pull traction Efficient if well-versed with table Imaging easy to obtain |
Risk of perineal injury, compartment syndrome, or nerve injury Table is expensive Cannot compare leg rotation Unsuitable for obese patients |
| Fracture table, well leg straight |
No need for assistant to pull traction Efficient if well-versed with table Imaging easy to obtain Can compare leg rotation/alignment |
Risk of perineal injury Unsuitable for obese patients Table is expensive |
| Supine on radiolucent table |
Table universally available Protect unstable spine, pelvis Address multiple orthopedic injuries Facilitate simultaneous procedures with other surgical services Good for obese patients Allows mobilization of open fractures Can compare leg rotation/alignment |
Requires assistant to pull traction |
| Lateral on radiolucent table |
Table universally available Improves exposure for obese patients Allows mobilization of open fractures May result in improved reduction |
Imaging more challenging Requires assistant to pull traction Cannot compare leg rotation |
Supine in Hemilithotomy
A standard fracture table with two articulating arms for the lower extremities is used. A boot is placed on the injured leg, and the patient is transferred to the fracture table. A well-padded perineal post is placed, and the patient is seated firmly against the post with care to prevent genitalia entrapment. The patient’s upper body should be abducted above the pelvis away from the fractured side; this will facilitate passage of instruments at the fracture site. Excess pannus may be taped at this time. A folded sheet is used to both pad a seatbelt strap and to immobilize the ipsilateral arm across the body. The contralateral well leg is placed in a padded leg holder, then elevated, externally rotated, and abducted into a hemilithotomy position. External rotation of the well leg allows the image intensifier to be brought between the legs for an anterior to posterior view of the hip and then the beam rotated to horizontal for a lateral view (Fig. 1).
Fig. 1.
Supine hemilithotomy position with injured extremity in traction, adducted, and well-leg abducted and externally rotated to allow space for the image intensifier
Once a patient is positioned, the image intensifier may be brought into position prior to draping, and the fracture may be reduced through manipulation of the extremity. Valgus impacted femoral neck fractures may not need a reduction or may be addressed with judicious application of traction and hip adduction to correct an exaggerated valgus head-neck angle. For intertrochanteric hip fractures, reduction is typically obtained via traction, internal rotation, and adduction of the leg. Comminuted peritrochanteric femur fractures may present a greater challenge, with translation of the distal femur anterior or posterior to the proximal fragments. In this case, a small accessory portal may be made lateral to the fracture line, and a Cobb elevator, bone reduction forceps, or similar instrument used to directly reduce these fragments. Once the surgeon is satisfied with the reduction, the extremity is locked in place, the image intensifier is withdrawn, and a sterile drape may then be placed across the well leg to avoid contaminating the image intensifier during the case. The patient is then draped either with a single large plastic sheet or with split extremity drapes in standard fashion. Supplementary S1, S2, S3.
Supine with Well Leg Extended
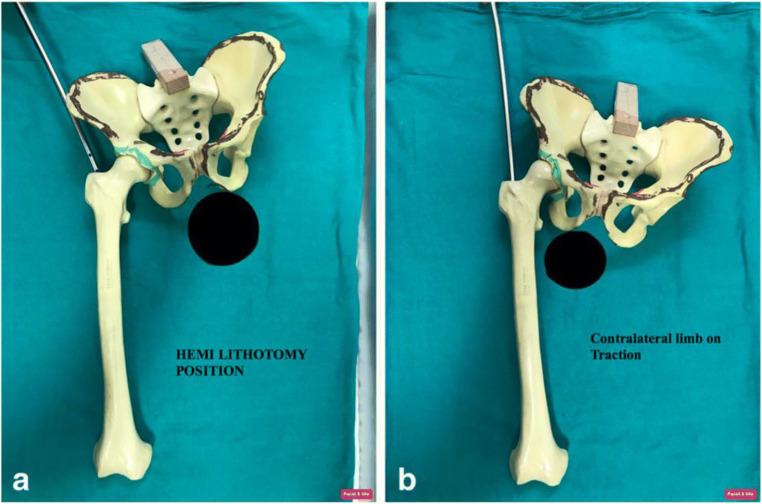
Initial setup is identical to the supine hemilithotomy position (see Fig. 1). The patient is transferred to the fracture table with boots on both feet. The patient’s upper body is positioned as above, with the arm ipsilateral to the injury adducted and secured. Once positioning is satisfactory, the well leg is either kept neutral at the hip or is extended 15–20 degrees below the level of the injured leg to allow for orthogonal views of the distal and mid-femur (Fig. 2). Tension is taken off the well leg, and the leg may be locked at this point or left free to move. As with the hemilithotomy position, fracture reduction may be obtained at this point, followed by draping in standard fashion. This patient position has the advantage of appropriately positioning the pelvis against the perineal post allowing for appropriate access to intramedullary nail insertion which is highlighted in Fig. 3 adopted from Kasha et al.
Fig. 2.
Supine position with well-leg extended still giving space for the image intensifier
Fig. 3.
Adopted from Kasha et al.’s “Management of Subtrochanteric fracture by nail osteosynthesis: a review of tips and tricks” (International orthopaedics 44.4 (2020): 645–653). (A) demonstrates the pelvic tilt with the contralateral limb in the hemilithotomy position compared to (B) with the pelvic tilt achieved with the contralateral limb extended in the traction boot, which allows for intramedullary nail insertion [6]
Complications from the Fracture Table
Fracture tables are associated with significant known complications [11]. Perineal complications, including pudendal nerve palsy and skin sloughing, are well described in the orthopedic literature [11, 13–16]. Brumback et al. reviewed the outcomes of 106 patients who were treated for femoral fractures via a fracture table and found a linear relationship between the force of applied traction and the incidence of pudendal nerve palsy [17]. Total time in traction is likewise related to nerve palsy and soft tissue breakdown [11]. Erectile dysfunction, testicular trauma, and genital hematoma have also been observed [18–20]. Fortunately, most perineal injuries including neural compromise are transient and resolve within weeks to months [16, 18].
Compartment syndrome is a real and potentially devastating complication unique to the hemilithotomy position. In this position, both the hip and the knee are flexed to roughly 90 degrees. Excessive knee flexion has been shown to dramatically increase intracompartmental pressures within the leg [21, 22]. The effects are worse in obese patients, when full flexion of the knee causes increased soft tissue pressures due to interposed fatty tissue posterior to the knee [21, 22]. Excessive hip and knee flexion is unnecessary to obtain necessary imaging, as judicious external rotation of the well leg will allow passage of the image intensifier between the legs. Given the risk of compartment syndrome, the hip and knee should be flexed to the minimal degree necessary to allow for appropriate imaging. The biggest risk factor for developing compartment syndrome is excessive surgical time, a relationship that has been widely reported across multiple surgical specialties using the lithotomy position, including urology, gynecology, and colorectal surgery [23–25]. Some authors have suggested that during extended surgeries, the well leg may be fully extended periodically to allow for decrease in pressures along with improved perfusion [11].
Sciatic and peroneal nerve palsies are also noted complications of the hemilithotomy position [26•, 27]. This may be due to flexion of the well hip to 90 degrees, without compensatory knee flexion past 90 degrees, thereby tensioning the sciatic nerve and giving rise to traction related nerve injury. Attention should be paid to positioning such that the knee is compensatorily flexed to account for hip flexion and neurovascular tension.
The fracture table may involve increased operative time compared to a standard radiolucent table. Sonmez et al. randomized 82 patients with unstable intertrochanteric hip fractures to a fracture table versus lateral decubitus position on a standard table. All patients were treated with a semi-open approach to the fracture. The authors found that both operative and fluoroscopic time were increased in the cases done using a fracture table [28]. This delay may be due in part to the learning curve associated with both the surgeon and room staff gaining familiarity with how to use this equipment.
Use of a fracture table is also associated with malrotation. This frequently occurs when internally rotating the hip while finding the starting point, with subsequent failure to adequately externally rotate the distal leg to neutral, or when rotating the leg to place distal interlocking screws [12]. The risk of malrotation is higher with the well leg in hemilithotomy position, as gross rotation of bilateral lower extremities cannot be assessed. Accurate femoral rotation may be achieved via obtaining preoperative imaging of the well leg lesser trochanter profile relative to a true anterior-posterior film of the distal femoral condyles. These films are compared to the operative leg intraoperatively prior to distal interlocking screw placement to ensure symmetric rotation with the well leg.
Patient Selection for the Fracture Table
Use of a fracture table is best suited to a patient with a relatively straightforward, closed intertrochanteric fracture pattern, with no injuries of the trunk or extremities that would preclude fracture table use. The patient should be non-obese, allowing for adequate imaging and preventing injury to the perineum or suspended extremities due to excessive weight-related traction. It can be obtained with no injuries of the ipsilateral or contralateral extremity that would preclude fracture table use. The surgeon should elect to use the fracture table for cases where a shorter operative time is anticipated. This is especially true for the hemilithotomy position, where prolonged knee flexion should be avoided due to risks of compartment syndrome or nerve palsy. The well leg should be examined to ensure adequate abduction, flexion, and external rotation at the hip. If the well leg cannot be brought into satisfactory elevation, the well leg should be kept extended as previously described.
Importantly, the surgeon should be comfortable with using the fracture table. The surgeon may request the table if minimal assistance is available to hold traction. In such a case, the surgeon may obtain fracture reduction under fluoroscopic guidance preoperatively, then lock the leg in place, prepare and drape the operative site, and complete the operation singlehandedly. If the surgeon anticipates rotational malalignment, such as in a femoral shaft fracture with circumferential cortical comminution, both legs should be kept straight and a clear plastic drape used, thereby allowing gross visual examination of symmetrical alignment and rotation.
Supine on a Radiolucent Table
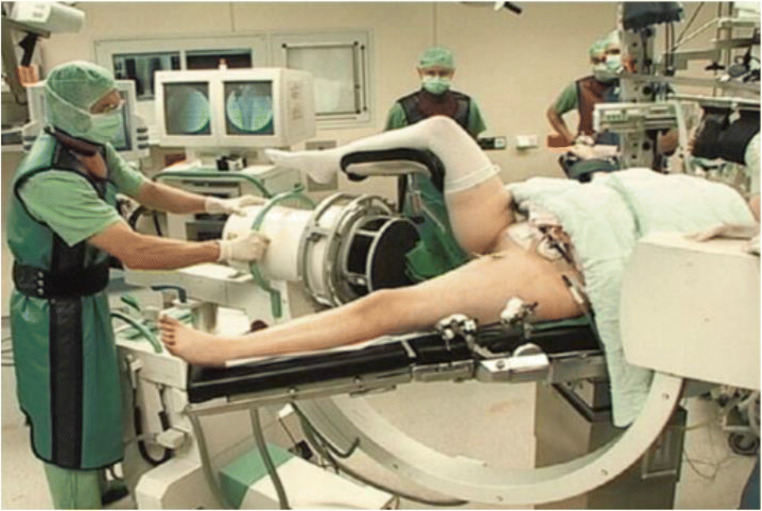
When treating a patient with a proximal femur fracture on a radiolucent table, the patient will be first transferred to the radiolucent table. In our institution, we prefer the use of a Flat Jackson Table. A rolled sheet will be placed underneath the ipsilateral sacrum and lumbar spine to elevate the ipsilateral hip. The image intensifier will be brought in from the contralateral side. The entire lower extremity will then be prepared and draped in the usual sterile fashion (Fig. 4). If the patient has multiple injuries, the contralateral or ipsilateral extremity may be draped accordingly to allow a single preparation for the treatment of multiple injuries.
Fig. 4.
Polytraumatized patient positioned supine on a radiolucent table with the contralateral limb flexed at the hip with slight external rotation in a leg-holding device in order to allow for adequate space for the image intensifier to obtain orthogonal imaging of the entire femur. Images reprinted with permission from Gösling and Krettek [29]
Proponents of proximal femur fixation supine on a radiolucent table state that the use of this technique allows the treatment of multiply injured patients without transfer [12, 30]. In the case of a polytrauma patient, multiple surgical specialists may be involved, and the use of a fracture table can be problematic [30]. The radiolucent table allows the preparation of multiple orthopedic injuries in one setting. The use of a fracture table would necessitate the transfer of the patient to a table between operations and repeat preparation and draping [12, 30]. Other advantages of the radiolucent table include avoiding the risk of a pudendal nerve palsy, well leg compartment syndromes, skin sloughing over the peroneal region, and in a polytrauma patient avoiding continuous traction in a patient with an unstable spine or pelvic ring injury [12, 30]. These complications are particularly relevant in the morbidly obese trauma population. Given an epidemic of obesity faced by many hospitals, the standard radiolucent table may be a preferred or necessary option for the management of these patients [11].
The use of manual traction for fracture reduction has been a long debated topic. The use of manual traction has required the use of an additional assistant. Other investigators have clearly defined the use of a femoral distractor for fracture reduction with intramedullary nailing [31, 32•]. However, reports have shown that the use of the femoral distractor although successful requires significantly longer operative times and is technically more demanding [32•]. The use of manual traction has been proven to have shorter operative times when compared to the use of a fracture table. In a randomized controlled trial, Stephen et al. demonstrated that the use of manual traction on a radiolucent table when compared to use of a fracture table decreased operative time by approximately 20 min and improved the quality of reduction in femoral shaft fractures [12].
In proximal femoral shaft fractures or subtrochanteric fractures, the use of the radiolucent table allows the entire injured limb to be available, and this affords the surgeon access to assess limb alignment and rotation. The image intensifier can be used to image the contralateral extremity and compare rotational profiles. If the fracture table is used and the patient has the contralateral extremity flexed, the position of the two limbs cannot be compared [12]. Evidence has demonstrated that quality of fracture reduction is improved with the use of the radiolucent table when compared to the fracture table [12].
Finally, standard radiolucent tables are both versatile and ubiquitous. In a resource limited environment, an orthopedic surgeon may not have access to a designated fracture table for the treatment of proximal femur fractures. Similarly, small community hospitals may be unable or unwilling to afford a fracture table for a limited case volume. While new technology such as dedicated fracture tables may decrease the need for assistants or aid in the management of particular fracture patterns, we believe that it is important for every orthopedic surgeon to be fluent in the use of a standard radiolucent table for the treatment of proximal femur fractures.
Patient Selection
The use of the radiolucent table can be used for a wide variety of patients and is not limited by many of the constraints of the fracture table. The radiolucent table can be used for obese patients, in situations where a fracture table may not be available, for polytrauma patients with either multiple orthopaedic or non-orthopaedic related injuries, open or complex fractures that need mobilization of the lower extremity for reduction and for severely comminuted fractures in which assessing alignment and rotation may be difficult. The general orthopedic surgeon should be well versed and trained to use the radiolucent table for fixation of proximal femur fractures.
Lateral Decubitus on a Radiolucent Table
While the popularity of supine patient positioning has led to the gradual decline in intramedullary nailing of the proximal femur in the lateral position, there are instances in which lateral patient positioning may be preferable.
At our institution, once general or neuraxial anesthesia has been administered, the patient is transferred to a radiolucent flat-top table without a central pedestal, such as a Flat Jackson Table. The fractured extremity is positioned superiorly, and patient positioning is maintained with a bean bag, pegs on a peg board, or other appropriate positioning aids. Care is taken to ensure that the operative extremity can be fully ranged to allow for unimpeded fracture reduction maneuvers. All bony prominences are well padded, a safety strap is applied, and the operative leg is prepped and draped in the usual sterile fashion from the iliac crest to the distal knee. The image intensifier may be brought in from either side of the patient; however, it is our preference that the intensifier be placed on the side opposite the surgeon. An assistant can be utilized to pull manual traction by standing at the foot of the bed, grasping the ankle with both hands, and using his or her body weight to apply longitudinal traction utilizing a “water ski maneuver” [33].
Challenges inherent in obtaining intraoperative fluoroscopy are a known potential disadvantage of lateral positioning. The lateral view is obtained by shooting downward through the table, while the anteroposterior view is obtained by rotating the C-arm under the table. When obtaining lateral images, Carr and colleagues recommend adjusting the tilt of the intensifier to be parallel to the femoral neck axis, approximately 10° to 20° off of vertical [33]. If lateral views remain obstructed due to overlap of the contralateral leg, the operative extremity may be repositioned anteriorly until adequate imaging is obtained. Ozkan and colleagues highlight the advantages of intramedullary nailing in the lateral decubitus position shown in Fig. 5.
Fig. 5.
mages adopted from Ozkan et al.’s “Proximal femoral nailing without a fracture table” (European Journal of Orthopaedic Surgery & Traumatology 20.3 (2010): 229–231). (A) demonstrates the lateral positioning with padded posts to maintain a lateral decubitus position. (B) and (C) demonstrate the image intensifier appropriately positioned with the operative extremity positioned anteriorly for adequate lateral imaging [34]
There are several advantages to performing intramedullary nailing of proximal femur fractures in the lateral position. First, the starting point can be easily obtained, even in overweight and obese patients, as the excess soft tissue displaces away anteriorly and posteriorly from the starting point due to the force of gravity. If open reduction is necessary, most open approaches to the hip and proximal femur are not impeded [35]. Additionally, because the hip is flexed during the procedure, iatrogenic damage to the abductors can be minimized or negated by placing the intramedullary nail posterior to the gluteus medius [33, 36]. Furthermore, it is easier to counteract the deforming forces causing flexion and abduction of the proximal fracture fragment when the patient is positioned laterally, as the hip can be flexed as much as is required to overcome the force of the iliopsoas [33]. Some evidence suggests that neutralizing deforming forces and utilizing manual traction in the lateral decubitus position may result in more accurate fracture reduction and femoral rotation [37]. Similar to placing a patient supine on a fracture table, lateral positioning avoids the costs inherent in obtaining and becoming facile with a fracture table. Lateral positioning may be utilized even in profoundly resource-limited settings.
Patient Selection
Lateral intramedullary nailing of proximal femur fractures may be preferred in obese patients without contraindications to lateral positioning. In one study comparing antegrade nailing of obese (BMI ≥ 30) versus non-obese (BMI < 30) patients, Tucker et al. demonstrated a 52% increase in operative time and a 79% greater average radiation exposure time in the obese patient cohort, likely due in part to difficulty with obtaining an appropriate starting point [38]. Sonmez et al. similarly reported a statistically significant decrease in mean operative and fluoroscopic time when comparing patients treated with proximal femoral nailing in the lateral decubitus position with those patients treated supine on a fracture table [28]. Overall, the ability to treat proximal femur fractures in the lateral position is an important addition to the armamentarium of the orthopedic surgeon and may contribute to improved patient outcomes if utilized in appropriate patient populations.
Lateral patient positioning should not be used in multiply injured patients or those patients with unstable spine injuries [33]. Care must be taken to ensure that all bony prominences are well padded to avoid possible peroneal nerve palsy of the down leg. Proper rotation of the nail upon entry should be closely scrutinized, as the nail can oftentimes be rotated posteriorly if the anterior displacement done to facilitate reduction is not accounted for [33]. The majority of reports on proximal femoral nailing in the lateral position demonstrate satisfactory reduction; however, reports of increased rotational malalignment do exist [39].
Recommendations
Strategic patient positioning is key to the reduction and fixation of proximal femur fractures and is the focus of this review. At our institution, proximal femur fractures comprise a significant proportion of traumatic orthopedic injuries and are managed by several trauma and general orthopedic surgeons. Patients are initially evaluated for isolated injuries versus polytraumas. The presence of significant other extremity orthopedic injuries often precludes use of a fracture table, as does the need for simultaneous operative management by additional surgical services. Additional factors including the presence of open injuries, comminution, patient obesity, lengthy anticipated surgery, and need for symmetric evaluation of both legs further dictate choice of patient positioning (see Fig. 2).
We recommend that the fracture table is employed when the surgeon is facile with its use and the patient is non-obese with an isolated, simple, closed fracture. Ideal candidates are valgus femoral neck fractures, intertrochanteric femur fractures, or closed, minimally comminuted subtrochanteric femur fractures. Care should be taken to avoid excessive flexion of the well hip or knee to avoid risks of compartment syndrome and sciatic or femoral nerve injury. Excessive traction should be avoided, and surgery should be conducted efficiently. If surgical delay occurs, the well leg may be extended periodically. Should the surgeon wish to compare lower extremity symmetry, the fracture table may be used with both legs supine and a clear drape system used with bilateral knees and feet visible.
For the multiply injured patient, we recommend principles of damage control orthopedics and initial resuscitation, as well as close coordination with other surgical services. Supine on a standard radiolucent table offers the most flexibility for abdominal and thoracic exposure, as well as for treatment of multiple ipsilateral or bilateral lower extremity injuries. The surgeon must have the assistance of one and often two operative assistants to hold traction distally as well as assist at the fracture site. The supine position allows for protection of unstable spine and pelvis fractures and potential simultaneous percutaneous instrumentation of the latter. Adequate imaging may be obtained with an image intensifier as previously discussed. To aid in both fracture fixation and imaging, the patient may be bumped with a roll of linen beneath the ipsilateral hip. The standard radiolucent table is our table of choice for the morbidly obese patient and for open or extensively comminuted fractures where mobilization of the operative leg is essential. On a standard table, morbidly obese patients may be addressed in the lateral decubitus position, allowing excess soft tissue to fall away from the surgical site.
Conclusion
Proximal femur fractures represent a large portion of traumatic injuries treated by the general and trauma orthopedic surgeon. There are multiple historic and common techniques for patient positioning. These techniques are variable based on injury pattern, concomitant injuries, and patient BMI to name a few factors. Each positioning technique has potential complications as well as an ideal patient and injury population. The treating orthopedic surgeon should have familiarity with multiple methods of operative positioning and thus have a broad armamentarium with which to address proximal femur fractures in any patient.
Supplementary Information
(PDF 72 kb)
(PDF 72 kb)
(PDF 72 kb)
Declaration
Conflict of Interest
KSV certifies that he had nothing of value related to this study.
CA certifies that he had nothing of value related to this study.
JRY certifies that he had nothing of value related to this study.
EP certifies that he had nothing of value related to this study.
CO certifies that he had nothing of value related to this study.
CC certifies that he had nothing of value related to this study.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects. Informed consent was not required for this study as it did not study human subjects.
Ethical review committee statement:
The study has been performed in accordance with the ethical standards in the 1964 Declaration of Helsinki and has been carried out in accordance with relevant regulations of the US Health Insurance Portability and Accountability Act (HIPAA). This work was performed at The Albany Medical Center, Albany, NY.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Khushdeep S. Vig, Joseph R. Young, Eric Perloff and Cory M. Czajka contributed equally to this work.
Contributor Information
Khushdeep S. Vig, Email: vigk23@gmail.com
Curtis Adams, Email: docadamsortho@gmail.com.
Joseph R. Young, Email: joseph.russell.young@gmail.com
Eric Perloff, Email: eric.perloff@gmail.com.
Casey M. O’Connor, Email: oconnoc1@mail.amc.edu
Cory M. Czajka, Email: cczajka@caportho.com
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Mittal R, Banerjee S. Proximal femoral fractures: principles of management and review of literature. Journal of clinical orthopaedics and trauma. 2012;3(1):15–23. doi: 10.1016/j.jcot.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2005;16(Suppl 2):S3–S7. doi: 10.1007/s00198-004-1702-6. [DOI] [PubMed] [Google Scholar]
- 3.Singer BR, McLauchlan GJ, Robinson CM, Christie J. Epidemiology of fractures in 15,000 adults: the influence of age and gender. The Journal of bone and joint surgery British volume. 1998;80(2):243–248. doi: 10.1302/0301-620X.80B2.0800243. [DOI] [PubMed] [Google Scholar]
- 4.Stevens JA, Rudd RA. The impact of decreasing U.S. hip fracture rates on future hip fracture estimates. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2013;24(10):2725–2728. doi: 10.1007/s00198-013-2375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friedman SM, Mendelson DA, Bingham KW, Kates SL. Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Arch Intern Med. 2009;169(18):1712–1717. doi: 10.1001/archinternmed.2009.321. [DOI] [PubMed] [Google Scholar]
- 6.Kasha S, Yalamanchili RK. Management of subtrochanteric fractures by nail osteosynthesis: a review of tips and tricks. International Orthopaedics (SICOT) 2020;44:645–653. doi: 10.1007/s00264-019-04404-z. [DOI] [PubMed] [Google Scholar]
- 7.Siu AL, Penrod JD, Boockvar KS, Koval K, Strauss E, Morrison RS. Early ambulation after hip fracture: effects on function and mortality. Arch Intern Med. 2006;166(7):766–771. doi: 10.1001/archinte.166.7.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.• Testa G, Vescio A, Aloj DC, et al. Definitive treatment of femoral shaft fractures: comparison between anterograde intramedullary nailing and monoaxial external fixation. J Clin Med. 2019;8(8) Safe management of polytrauma patients involves active coordination with all involved services in order to ensure preoperative stabilization and postoperative resuscitative management. While planning for early fixation, the surgeon must consider coexisting goals of operative time, predicted blood loss, and minimization of soft tissue trauma. [DOI] [PMC free article] [PubMed]
- 9.Bartonicek J, Rammelt S. The history of internal fixation of proximal femur fractures Ernst Pohl-the genius behind. Int Orthop. 2014;38(11):2421–2426. doi: 10.1007/s00264-014-2320-3. [DOI] [PubMed] [Google Scholar]
- 10.Riehl JT, Widmaier JC. Techniques of obtaining and maintaining reduction during nailing of femur fractures. Orthopedics. 2009;32(8):581. doi: 10.3928/01477447-20090624-17. [DOI] [PubMed] [Google Scholar]
- 11.Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res. 1998;348:87–94. doi: 10.1097/00003086-199803000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Pape HC, Grimme K, Van Griensven M, et al. Impact of intramedullary instrumentation versus damage control for femoral fractures on immunoinflammatory parameters: prospective randomized analysis by the EPOFF Study Group. J Trauma. 2003;55(1):7–13. doi: 10.1097/01.TA.0000075787.69695.4E. [DOI] [PubMed] [Google Scholar]
- 13.Hawley G. Fracture orthopedic table. J Am Med Assoc. 1913;60(24):1850–1851. doi: 10.1001/jama.1913.04340240006004. [DOI] [Google Scholar]
- 14.Flierl MA, Stahel PF, Hak DJ, Morgan SJ, Smith WR. Traction table-related complications in orthopaedic surgery. The Journal of the American Academy of Orthopaedic Surgeons. 2010;18(11):668–675. doi: 10.5435/00124635-201011000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Stephen DJ, Kreder HJ, Schemitsch EH, Conlan LB, Wild L, McKee MD. Femoral intramedullary nailing: comparison of fracture-table and manual traction. a prospective, randomized study. J Bone Joint Surg Am. 2002;84(9):1514–1521. doi: 10.2106/00004623-200209000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Coelho RF, Gomes CM, Sakaki MH, Montag E, Guglielmetti GB, de Barros Filho TE, Srougi M. Genitoperineal injuries associated with the use of an orthopedic table with a perineal posttraction. J Trauma. 2008;65(4):820–823. doi: 10.1097/TA.0b013e31811eaa66. [DOI] [PubMed] [Google Scholar]
- 17.Hammit MD, Cole PA, Kregor PJ. Massive perineal wound slough after treatment of complex pelvic and acetabular fractures using a traction table. J Orthop Trauma. 2002;16(8):601–605. doi: 10.1097/00005131-200209000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Kao JT, Burton D, Comstock C, McClellan RT, Carragee E. Pudendal nerve palsy after femoral intramedullary nailing. J Orthop Trauma. 1993;7(1):58–63. doi: 10.1097/00005131-199302000-00011. [DOI] [PubMed] [Google Scholar]
- 19.France MP, Aurori BF. Pudendal nerve palsy following fracture table traction. Clin Orthop Relat Res. 1992;276:272–276. [PubMed] [Google Scholar]
- 20.Brumback RJ, Ellison TS, Molligan H, Molligan DJ, Mahaffey S, Schmidhauser C. Pudendal nerve palsy complicating intramedullary nailing of the femur. J Bone Joint Surg Am. 1992;74(10):1450–1455. doi: 10.2106/00004623-199274100-00003. [DOI] [PubMed] [Google Scholar]
- 21.Rajbabu K, Brown C, Poulsen J. Erectile dysfunction after perineal compression in young men undergoing internal fixation of femur fractures. Int J Impot Res. 2007;19(3):336–338. doi: 10.1038/sj.ijir.3901529. [DOI] [PubMed] [Google Scholar]
- 22.Mallet R, Tricoire JL, Rischmann P, Sarramon JP, Puget J, Malavaud B. High prevalence of erectile dysfunction in young male patients after intramedullary femoral nailing. Urology. 2005;65(3):559–563. doi: 10.1016/j.urology.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 23.Choudhuri AH, Sharma H, Dharmani P, Goyal N. Vulval injury due to perineal post on fracture table: Concern for anaesthesiologist. The Internet Journal of Anesthesiology. 2006;11(2).
- 24.Meyer RS, White KK, Smith JM, Groppo ER, Mubarak SJ, Hargens AR. Intramuscular and blood pressures in legs positioned in the hemilithotomy position : clarification of risk factors for well-leg acute compartment syndrome. J Bone Joint Surg Am. 2002;84(10):1829–1835. doi: 10.2106/00004623-200210000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Tan V, Pepe MD, Glaser DL, Seldes RM, Heppenstall RB, Esterhai JL., Jr Well-leg compartment pressures during hemilithotomy position for fracture fixation. J Orthop Trauma. 2000;14(3):157–161. doi: 10.1097/00005131-200003000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Dos Reis JMC, Queiroz LJM, Mello PF, Teixeira RKC, Goncalves FA. Bilateral compartment syndrome of the lower limbs after urological surgery in the lithotomy position: a clinical case. Jornal vascular brasileiro. 2019;18:e20180117. doi: 10.1590/1677-5449.180117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stornelli N, Wydra FB, Mitchell JJ, Stahel PF, Fabbri S. The dangers of lithotomy positioning in the operating room: case report of bilateral lower extremity compartment syndrome after a 90-minutes surgical procedure. Patient safety in surgery. 2016;10:18. doi: 10.1186/s13037-016-0106-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beraldo S, Dodds SR. Lower limb acute compartment syndrome after colorectal surgery in prolonged lithotomy position. Dis Colon Rectum. 2006;49(11):1772–1780. doi: 10.1007/s10350-006-0712-1. [DOI] [PubMed] [Google Scholar]
- 29.Krettek C, Gösling T. Femur diaphysis. In: Rommens P, Hessmann M, editors. Intramedullary Nailing. London: Springer; 2015. 10.1007/978-1-4471-6612-2_19.
- 30.Tait GR, Danton M. Contralateral sciatic nerve palsy following femoral nailing. The Journal of bone and joint surgery British volume. 1991;73(4):689–690. doi: 10.1302/0301-620X.73B4.2071664. [DOI] [PubMed] [Google Scholar]
- 31.Lhowe DW, Hansen ST. Immediate nailing of open fractures of the femoral shaft. J Bone Joint Surg Am. 1988;70(6):812–820. doi: 10.2106/00004623-198870060-00003. [DOI] [PubMed] [Google Scholar]
- 32.Sonmez MM, Camur S, Erturer E, Ugurlar M, Kara A, Ozturk I. Strategies for proximal femoral nailing of unstable intertrochanteric fractures: lateral decubitus position or traction table. The Journal of the American Academy of Orthopaedic Surgeons. 2017;25(3):e37–e44. doi: 10.5435/JAAOS-D-15-00691. [DOI] [PubMed] [Google Scholar]
- 33.Karpos PA, McFerran MA, Johnson KD. Intramedullary nailing of acute femoral shaft fractures using manual traction without a fracture table. J Orthop Trauma. 1995;9(1):57–62. doi: 10.1097/00005131-199502000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Ozkan K, Cift H, Akan K, Sahin A, Eceviz E, Ugutmen E. Proximal femoral nailing without a fracture table. Eur J Orthop Surg Traumatol. 2010;20:229–231. doi: 10.1007/s00590-009-0550-7. [DOI] [Google Scholar]
- 35.Baumgaertel F, Dahlen C, Stiletto R, Gotzen L. Technique of using the AO-femoral distractor for femoral intramedullary nailing. J Orthop Trauma. 1994;8(4):315–321. doi: 10.1097/00005131-199408000-00007. [DOI] [PubMed] [Google Scholar]
- 36.McFerran MA, Johnson KD. Intramedullary nailing of acute femoral shaft fractures without a fracture table: technique of using a femoral distractor. J Orthop Trauma. 1992;6(3):271–278. doi: 10.1097/00005131-199209000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Carr JB, Williams D, Richards M. Lateral decubitus positioning for intramedullary nailing of the femur without the use of a fracture table. Orthopedics. 2009;32(10). [DOI] [PubMed]
- 38.Bishop JA, Rodriguez EK. Closed intramedullary nailing of the femur in the lateral decubitus position. J Trauma. 2010;68(1):231–235. doi: 10.1097/TA.0b013e3181c488d8. [DOI] [PubMed] [Google Scholar]
- 39.Ozsoy MH, Basarir K, Bayramoglu A, Erdemli B, Tuccar E, Eksioglu MF. Risk of superior gluteal nerve and gluteus medius muscle injury during femoral nail insertion. J Bone Joint Surg Am. 2007;89(4):829–834. doi: 10.2106/00004623-200704000-00019. [DOI] [PubMed] [Google Scholar]
- 40.Delgado JM. Intramedullary nailing of subtrochanteric femur fractures in the lateral position. Tech Orthop. 2014;29(3):133–139. doi: 10.1097/BTO.0000000000000066. [DOI] [Google Scholar]
- 41.Tucker MC, Schwappach JR, Leighton RK, Coupe K, Ricci WM. Results of femoral intramedullary nailing in patients who are obese versus those who are not obese: a prospective multicenter comparison study. J Orthop Trauma. 2007;21(8):523–529. doi: 10.1097/BOT.0b013e31813347ac. [DOI] [PubMed] [Google Scholar]
- 42.Abubeih HMA, Farouk O, Abdelnasser MK, Eisa AA, Said GZ, El-Adly W. Femoral malalignment after gamma nail insertion in the lateral decubitus position. Sicot-j. 2018;4:34. doi: 10.1051/sicotj/2018033. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 72 kb)
(PDF 72 kb)
(PDF 72 kb)