Abstract
Background
This review was carried out to synthesize the evidence of the effectiveness of community health worker (CHW) navigation in primary care chronic disease management.
Methods
We searched the English language literature between January 1990 and March 2020 in Medline, Embase, Emcare, PubMed, Psych Info, CINAHL, Scopus, and Medline Epub ahead of print. Data extraction, quality rating, and assessment of the reporting of interventions were performed by two reviewers independently and the findings were synthesized narratively.
Results
Twenty-nine articles met the inclusion criteria. All but two were carried out in the USA and half were randomized controlled trials. Six of the 29 studies were of strong methodological quality while 12 were moderate and 11 weak. Overall, CHW navigation interventions were effective in increasing adherence to cancer screening and improving use of primary care for chronic disease management. There was insufficient evidence that they improved clinical outcomes or risk factors and reduced use of secondary or tertiary care or that they were cost-effective. However, criteria for recruitment, duration, and mode of training and supervision arrangements varied greatly between studies.
Discussion
CHW navigation interventions improved aspects of chronic disease management. However, there is insufficient evidence of the impact on patient experience, clinical outcomes, or cost-effectiveness of the interventions. Future research should focus on standardizing organizational components of the CHW navigation interventions and evaluating their cost-effectiveness.
Protocol Registration
The review protocol was published in PROSPERO (CRD42020153921).
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-06667-y.
INTRODUCTION
Worldwide, non-communicable diseases account for more than 70% of the 41 million annual deaths1 and 80% of total disabilities,2 and pose a huge demand for health systems.3
Due to fragmentation in health system and complex needs of the patients, many patients find difficulties navigating the increasingly complex health system.4, 5 This is particularly true for patients from culturally and linguistically diverse backgrounds including immigrants and refugees with poor health literacy which often results from culture and language barriers.6, 7
Primary care is the first level of contact into the health system and often the principal avenue of care for chronic disease management.8 A strong primary care system which provides coordinated, comprehensive, affordable, community-focused, and family-oriented care results in better management of chronic disease.9, 10 Alongside the treatment and long-term care for the patients with chronic diseases, primary care also carries out activities such as health promotion, community education, patient advocacy, and illness prevention.11, 12 Furthermore, primary care is also responsible for the coordination of specialist services.9
While there is increasing recognition of the importance of primary care in management of chronic illnesses, there is often lack of coordination among different health providers.13 Studies carried out in different countries point out that lack of time during the clinical visit is one of the most important barriers to the provision of quality primary care for chronic diseases.14 In a recent study carried out in Australian general practice, Song and colleagues15 reported that a major barrier to access care among patients with chronic conditions was providers’ inability to tailor care to patients’ expectations and preferences. Culturally and linguistically diverse patients also experience barriers due to inadequate English language proficiency, lack of understanding of health system, poor health literacy, and inability to pay high out-of-pocket costs for referral services.16–18
Globally, community health workers (CHWs) are considered an integral part of the primary care.19–21 CHWs are defined as “frontline public health workers who serve as a liaison/link/intermediary between health/social services and the community to facilitate access to services and improve the quality and cultural competence of service delivery”.22 Community health workers can serve several roles, including care coordination, health assessments,23, 24 health education,25–27 and psychosocial support.28–30
Meanwhile, patient navigation is an important health service delivery tool to promote timely movement of an individual patient across the complex healthcare continuum.31 The concept of patient navigation was first developed by Professor Harold Freeman, in 1990. Freeman introduced the term “patient navigator” whose role was to address the barriers in breast cancer diagnosis and treatment among poor, uninsured, and underserved women in Harlem.31, 32 In recent years, the patient navigation role has been expanded to different aspects of healthcare.33
However, there is a lack of systematic reviews focusing on the role of CHWs as navigators. Therefore, the present systematic review aimed to evaluate the effectiveness of the CHW role as navigator in the context of chronic disease management in primary care.
METHODS
We followed PRISMA (preferred reporting items for systematic reviews and meta-analyses) guidelines34 in conducting this systematic review and the review protocol was registered in PROSPERO (CRD42020153921).
Search Strategy
We systematically searched the electronic databases Medline, Embase, Emcare, PubMed, Psych Info, CINAHL, Scopus, and Medline Epub ahead of print to identify potential research studies. We used Google and Google scholar in scoping the review and searching for possible gray literature. A combination of Medical Subject Headings (MeSH) and free-text keywords categorized into three groups (CHW, navigation, and primary care) was used to search for relevant articles in selected databases which are published in English between January 1990 and March 2020. Detailed search strategy is presented in Annex 1.
Study Selection
The articles identified through electronic database searches were assessed against predefined inclusion and exclusion criteria (Box 1) by two independent reviewers. First, we screened the title and abstract of the articles and full text was obtained for articles passing this screen. More in-depth assessment was carried among the full-text articles. The study selection was performed using Covidence (https://www.covidence.org/)35 in which reviewers could vote independently. Differences were resolved by discussion.
Box 1 Inclusion and exclusion criteria
| Inclusion criteria | |
| • Published in English | |
| • Published between 1990 and March 2020 | |
| • Studies evaluating navigation intervention | |
| • Carried out in primary care setting or in other community settings | |
| • Navigation services provided by CHWs | |
| • Navigation services provided for chronic disease management | |
| • Primary studies | |
| Exclusion criteria | |
| • Published in language other than English | |
| • Published before 1990 and March 2020 | |
| • Studies not evaluating navigation intervention | |
| • Carried out in secondary and tertiary care setting | |
| • Navigation services provided by professionals other than CHWs | |
| • Navigation services provided for infectious disease management | |
| • Article is review/commentary/protocol |
Data Extraction and Quality Assessment
Relevant data were extracted using a template developed by the authors. Two of the authors assessed the methodological quality of each of the selected studies using Effective Public Health Practice Project (EPHPP) quality assessment tool.36 Each study was scored (weak, moderate, or strong) against six methodological criteria: selection bias, study design, confounders, blinding, data collection methods, withdrawals, and drops. A study was categorized as weak if it had two or more weak rating, moderate if had one weak rating, and strong if had no weak rating. Differences were resolved by discussion. We also assessed the quality of reporting of the intervention in the selected studies using TIDieR checklist.37
Data Analysis
Descriptive analysis was performed to summarize the interventions, roles, training, and outcomes of the studies in relation to the objectives of the research. Considering the heterogeneous design and outcomes, we did not perform meta-analysis.
RESULTS
Search Result
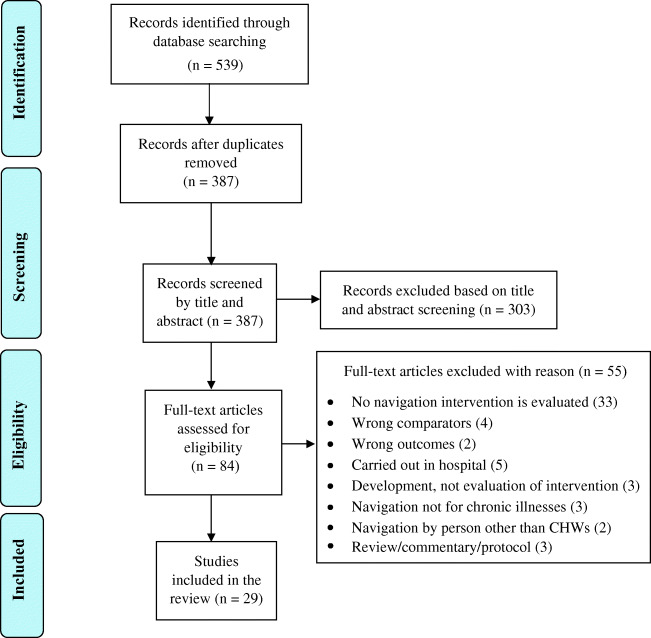
A total of 539 articles were identified through initial searching. After screening, we included 29 articles in the final analysis (Fig. 1). Study characteristics are summarized in Table 1. Six of the 29 studies had strong methodological quality,38–44 12 moderate, and 11 weak 45–55 (Annex 2). When assessed according to the TIDieR checklist, 24 studies reported procedures, who provided, how, where, and when.37 Few studies11 reported the frequency and time period of the intervention sessions and only one study55 reported how the intervention had been tailored to local needs. No studies reported on modifications to the intervention or fidelity of its implementation (Annex 3).
Figure 1.
PRISMA diagram of study selection.
Table 1.
Characteristics of Included Studies
| Study | Country | Study setting | Study design | Study population/subject/participants | Characteristics of the navigators | Recruitment, training, supervision and integration in healthcare team | Mode of navigation delivery |
|---|---|---|---|---|---|---|---|
| Allen et al., 201445 | Boston, USA | Latino Baptist Church | One-group pre-/post-evaluation | Female Hispanic or Latino Church members aged 18 years or above (n=155). | Navigators were Peer Health Advisors (PHAs). Three PHAs were recruited aged 18 years and above Hispanic/Latina/English/Spanish speaking women who were long-time church members | Navigators were recruited two months prior to the intervention and were selected by the pastor based on their leadership, communication, and interpersonal skills. PHAs completed two full days of training that covered cancer risk factors and prevention, screening, guidelines, and techniques for conducting community outreach and education. | Navigators delivered the intervention in-person, via phone and using the online media as well |
| Battaglia et al., 201246 | Boston, USA | Urban safety net primary care practice | Feasibility study, using mixed methods | A total of 109 female low-income African American patients aged 51–70 years with at least one prior mammogram and more than 18 months since their most recent documented mammogram was participated | Five primary care-based breast health patient navigators | Navigators had clinical experience and completed CHW core competencies offered by a regional education center for 2 weeks. Training covered general discharge information, screening guidelines, motivational interview. They received a booster training after 1 month of study enrolment. | Navigation services provided via phone |
| Braun et al., 201538 | Hawaii, USA | Moloka’i General Hospital | Randomized controlled trial (RCT) | Asian and Pacific Islander Medicare beneficiaries (n=488). | Two lay navigators from the community—one native Hawaiian and one Filipino | Navigators were not certified healthcare providers, but they completed a 48-h evidence-based navigator training program and took part in a quarterly education session. Initially they were supervised by a nurse but later they were supervised by a woman having a business degree and two physicians. | Navigators contacted the participants on the telephone or made home visits |
| Christie et al., 200847 | New York, USA | A local community health center (Settlement Health) | Randomized controlled trial (RCT) | Low-income minorities both men and women aged >50 years who had a referral for screening colonoscopy. A total of 21 patients were included. | One patient navigator | Patient navigator was a health educator who received training on navigation. | Navigation services were provided via phone |
| Chukwudozie et al., 201857 | Chicago, USA | Primary care setting | Before–after repeated measures | Eligible patients were either English- or Spanish-speaking adults (≥18 years) receiving chronic hemodialysis recruited from one of the two sites (n=173). | Two CHWs served as health promoters or navigators | CHW was included as part of a team which included a primary care provider, a nurse coordinator, a pharmacist and a CHW. | CHW had an initial visit with the patients and then monthly check-in visits |
| Cole et al., 201748 | New York, USA | Community setting | 3-parallel-arm, randomized trial | Black men aged 50 years or older, not be up to date on CRC screening and have uncontrolled high blood pressure, recruited at barbershops between 2010 and 2013 in New York City (n=740). | CHWs | Patient navigators were community health workers. | Navigation services provided via phone |
| Dudley et al., 201249 | San Antonio, Texas, USA | University Health Systems (UHS), the county safety net hospital system | Quasi-experimental design comparing unmatched control and intervention participants | Mentally competent 18 years of age and older Hispanic women residing in south Texas who had abnormal breast screening testing were eligible to participate in the study and were recruited from November 2006 to May 2010 (intervention=200, control=200). | Combination of patient navigators and promotoras. 4 PNs and 4 promotoras were involved | Of the 4 PNs, one was nurse, one dental hygienist, one social worker, and one with master’s in business administration. All promotoras had a background of community health education. | PN/promotora meet the patients, prepare the care plan, and began actively navigating the patient |
| Enard and Ganelin, 201358 | Houston, Texas, USA | Primary care setting | Quasi-experimental study design | Participants are the patients who discharged from the ED of Memorial Hermann Texas Medical Center (MH-TMC) (intervention=1905, control=11737). They were low-income uninsured or publicly ensured ethnic minorities. | Bilingual community health workers | Navigators were state-certified community health workers and were trained in peer-to-peer counselling. | Both in-person and telephone navigation services |
| Enard et al., 201559 | Texas, USA | University of Texas MD Anderson Cancer Center | Randomized controlled trial (RCT) | Latino Medicare enrollees aged ≥40 years who have not been diagnosed with any type of cancer within the last 5 years (intervention=135, control=168) | Patient navigators | Navigators had a bachelor’s degree in public health or relevant discipline and field experience of 2 years or more. They also received 80 h training on PN core competencies and attended in at least one 3-day continuing education conference. Navigators were trained on communication, service coordination and advocacy. | Navigation service was provided via telephone and email |
| Fedder et al., 200360 | West Baltimore, Maryland, USA | Community based and primary care setting | Retrospective comparison design | Medicaid patients with diabetes, with or without hypertension recruited between March 1992 and June 1993 (n=117). Patients were African American and aged between 14 and 90 years. | A total of 38 CHWs with a mean age of 59 years were involved in providing services to the patients. All but one CHW were female. | CHWs were recruited from the target neighborhoods and provided a minimum of 60 h training over 6 months. They received training on chronic illnesses, resource identification, outreach, and case management. Bi-weekly supervision meeting were arranged with case allocation, forms distribution and problem solving. Trainers were recruited from University of Maryland in Baltimore and Department of Health and Mental Hygiene Diabetes Control Program. | Patients were contacted at least once weekly, alternating in-home visits with phone calls |
| Felix et al., 201965 | Arkansas, USA | The study used Community Connector Program (CCP) records and the Arkansas Medicaid claims records | A quasi-experimental design was followed | All Medicaid-eligible adults ≥ 18 years of age who resided in the CCP’s service area (a 15-county region of eastern Arkansas) with at least one HCBS claim and at least one month of Medicaid enrolment during the SFY of their home and community-based long-term services and supports (HCBS) claim were included as study subjects (n = 20,551). | CHWs | CHWs were recruited from the same communities from where participants were recruited. | Services were provided in-person by setting up booths at local events and going door-to-door |
| Fiscella et al., 201240 | Rochester and Denver, USA | Participating oncology practices from both Rochester and Denver site | Randomized controlled trial (RCT) | Participants were eligible to be referred for the trials if they had newly diagnosed breast (female) or colorectal (female or male) cancer and received care from any participating practice. The Rochester site contributed 319 participants and Denver 119. | Navigators were lay person from the community | Navigators had a minimum of high-school degree, strong communication skills, fluent in Spanish and English, demonstrated ability to learn and current driver’s license. They were equipped with intensive training and were supervised with experienced managers who met them regularly. | Contact was established between navigators and patients through face-to face meeting, telephone, and email |
| Griswold et al., 201050 | New York, USA | Primary care setting | Randomized controlled trial (RCT) | Participants were adults aged 18 and over, not having any emergency medical condition and presented at an urban Comprehensive Psychiatric Emergency Program (CPEP) (n=175). | Care navigators | All care navigators received an initial and ongoing training focusing on patient interviewing, case assessment and management of patients in a psychiatric emergency. | Regular contact was maintained by the navigators through face-to-face visit and by phone. |
| Guillaume et al., 201739 | France | Study area consisted of three French departments collectively comprising 2360 small geographical units for which census data are available (around 2000 inhabitants per unit) | Cluster randomized controlled trial | Participants were 50–74 years low-income people who were asked by their general practitioners for CRC screening (intervention=14,373; control=14,556) | Screening navigators (SN) | SN were specifically trained for a week by several professionals such as gastroenterologist, public health researchers and psychologist. They were accustomed to work with disadvantaged population. | Navigation was done by phone, letter, and home visit. |
| Honeycutt et al., 201361 | Georgia, USA | Community health center (CHC) clinics in southwest Georgia | Quasi-experimental research study | Participants were aged 50–64 years, poor, underinsured/uninsured, and visited the clinic at least once during the study period (n=809). | Health navigators | Trained professional health navigators worked with health centers, hospital, and gastroenterology practices to facilitate program activities. | Navigation was delivered in-person and over phone. |
| Horne et al., 201541 | Baltimore City, Maryland, USA | Community-based and clinical setting (senior center) | Randomized controlled trial (RCT) | Participants were urban African American adults and deemed eligible for the study if they were a Baltimore City resident, aged 65 and older, and enrolled in Medicare Parts A and B (n=1220). | Patient navigators | Patient navigators are health coordinator trained by Johns Hopkins. | Navigators communicated with the participants in-person. |
| Jandorf et al., 201342 | New York, USA | Mount Sinai’s primary care clinic | Randomized controlled trial (RCT) | Participants were African American patients aged 50 years and above, without active gastrointestinal symptoms, significant comorbidities, or a history of inflammatory bowel disease or colorectal cancer (CRC) (n=532). | Both peer patient navigator (Peer-PN) and professional patient navigator (Pro-PN) was involved who were African American aged above 50 years | Both peer and professional PN received 19 h of training and a series of one-to-one structured role plays. | Navigation services were delivered via telephone. |
| Lasser et al., 200953 | MA, USA | Community health centers in Cambridge, Somerville, and Everett, MA | Feasibility and effectiveness study using mixed method design | Study participants were patients aged 52–80 years who appeared to be unscreened for colorectal cancer (n=183). | Navigators were CHWs speaking English and Spanish, Portuguese, and Haitian Creole. All of them were women and were age 47, 42, and 37 years respectively. | Navigators attended a two-day training program which involves lecture and interactive role plays on disease information, screening information, motivational interviewing, logistics, communication, and prevention. The project manager supervised the activities of the navigators sit with the navigators on weekly basis to discuss any challenges and review the intervention process. | Navigation services was provided via phone. |
| Lasser et al., 201362 | Boston, USA | Four different primary care practices at Boston Medical Center | Pilot randomized controlled trial | Patients were aged ≥ 18 who smoked cigarettes in the past week and had a scheduled visit with a primary care provider (PCP) in the next six months (n=47). | Navigator is nurse’s assistant aged 52 years | The navigator had 20 years’ experience in patient navigation and community health outreach. The navigator previously received training on motivational interviewing and patient navigation. For this study, she also received 3 additional training sessions delivered by motivational interviewing trainer. Training includes lecture and role plays on motivational interviews, health risk associated with smoking, logistics, use of reflective listening, sensitization, patient readiness, and communication. Navigators are supervised on bi-weekly basis by study investigator and provided feedback from audit of transcript, discussed challenges, and review of motivational training. | Navigators make the contact both in-person and by phone. |
| Lui and Perkins, 201551 | AL, USA | An urban, university-based Family Medicine residency | One-group pre-/post-evaluation | Eligible patients included patients aged 50 to 74 years seen in the clinic within the past 3 years who were not at high risk for colorectal cancer, did not have a terminal disease, and were not part of special populations requiring an individualized approach. There were 1394 eligible patients. | A lay health worker was navigator | The paper did not provide any detail of the training or supervision of the navigator. | Navigation services were delivered via phone. |
| Loskutova et al., 201652 | AL, USA | 6 primary care practices in Birmingham, Alabama | Before/after cohort study | Study participants were English-speaking adult patients residing within the Birmingham city limits and receiving services at one of the enrolled practices and if they1 were diagnosed with type 2 diabetes and2 were at risk for type 2 diabetes (n=179). | Patient navigators |
Navigators were recruited from 2 of the Cities for Life partner community organizations. They lived and worked in the communities they served and received two 1.5-h webinar-based training sessions on patient centeredness, individualized care plans, motivational interviewing techniques, and communication delivered by the project manager. The project manager carried out ongoing review and feedback sessions, and supervised patient navigation activities. |
Navigation service was provided over telephone |
| Marshall et al., 201654 | Baltimore City, Maryland, USA | Community-based and clinical setting | Randomized controlled trial (RCT) | Participants were African American Medicare enrollees in Baltimore City. Participants were eligible if they were age ≥65 years, self-reported African American, enrolled in fee-for-service Medicare Parts A and B, and a Baltimore City resident (n=2593). | Patient navigators | Navigators received training included classroom training, role playing, and use of electronic database designed to support navigators’ patient education. | Navigators made both in-person and phone-based contact. |
| McDermott et al., 201556 | Queensland, Australia | The study setting was 12 small remote communities in far north Queensland where most of the population was Aboriginal or Torres Strait Islander | A pragmatic cluster randomized controlled trial | Two hundred and thirteen aboriginal adults with poorly controlled diabetes (HbA1c > 8.5%) and significant comorbidities in 12 remote communities were selected for the study. | Indigenous health worker as navigator | Indigenous health workers are the residents of the community selected by the health services to work as part of the primary care team. They received an intensive 3-week training on clinical aspects of diabetes and other chronic condition care including how to support patients in self-management skills, advice on medication, routine foot care, nutrition, smoking cessation, follow up referrals to other providers and schedule test before the intervention being implemented. | Services were provided in-person in home and out of clinic. |
| Mojica et al., 201666 | San Antonio, Texas, USA | Community based; participants recruited from the west and south sides of San Antonio, Texas | A single-arm, nonrandomized, pre-post design | Eligible participants were Latino women1 aged 40 to 74 years who had never had a mammogram or not had one in the past 2 years,2 aged 18 to 65 years who had never had a Pap test or not had one in the past 3 years, or3 aged 50 to 75 years who had never had a stool blood test or not had one in the past 2 years (n=1612). | Bilingual, bicultural CHWs |
CHWs received an initial 2-week training on breast, cervical, and colon cancer risk factors, screening tests and screening guidelines as well as on data collection and entry. Booster training session was delivered once per year. CHWs were supervised on a weekly basis by project coordinator to discuss weekly goal and activities |
Both in-person and telephone navigation services |
| Percac-Lima et al., 201363 | Chelsea, Massachusetts, USA | The Massachusetts General Hospital (MGH) colposcopy clinic the MGH Chelsea HealthCare Center (MGH Chelsea), an urban community health center | Quasi-experimental design | 533 Latina women with an abnormal Pap smear requiring colposcopy screening. | Patient navigators |
Navigator was a Latina-immigrant woman and native Spanish speaker from the Chelsea community. Navigator was trained in patient navigation, cervical health, and cervical cancer. Navigator was supervised by a social worker and nurse practitioners with expertise in women’s health issues |
Navigation services were provided both in-person and via phone. |
| Percac-Lima et al., 200964 | Chelsea, Massachusetts, USA | The Massachusetts General Hospital (MGH) Chelsea HealthCare Center (MGH Chelsea), an urban community health center | Randomized controlled trial (RCT) | Patients were low-income immigrants aged between 52–79 years and had not undergone colorectal cancer screening in the last 10 years, sigmoidoscopy/barium enema in the past 5 years, or home fecal occult blood testing in the past year (n=1223). | Navigators were CHWs | They were health center outreach workers and interpreters who took part in 6-h training course run by the study PI and center’s community health director which involves training on different aspects of patient navigation and CRC screening. | Participants were contacted via phone or in-person |
| Phillips et al., 201144 | Boston, USA | Primary care of an academic safety net hospital in Boston | Randomized controlled trial (RCT) | A total of 3895 ethnic minority women aged 51 to 70 who were assigned a primary care provider and had a documented visit with that provider in the previous 2 years were included in the study. | Patient navigators | Navigators received national and local navigation training programs that emphasize barriers-focused culturally tailored services based upon the care management model. | Navigation services provided via phone |
| Raich et al., 201243 | Denver, USA | Denver Health (DH), the safety net healthcare system serving Denver | Randomized controlled trial (RCT) | 993 ethnic minority adults aged 18 years above were eligible with abnormal screening tests, 628 had abnormal breast screens, while 235 had abnormal colorectal and 130 had abnormal prostate screens. | Patient navigators |
Navigators attended an annual training conference designed and delivered by the American society. In addition, frequent institution-based training sessions were conducted on clinical and psychosocial topics. The program manager met the navigators on a weekly basis at the initial stage and continued to meet monthly thereafter. |
Navigators contacted the patients in-person, via phone and email. |
| Shlay et al., 201155 | Denver, USA | Community health centers in the Denver Health and Hospital Authority (DHHA), an urban safety net healthcare system | Quasi-experimental pre-post (baseline and 12-month follow-up) design | A total of 919 participants were included who had a Framingham risk score (FRS) greater or equal to 10%, being aged 30 to 64 years, and having an active status at 1 of the 3 intervention community health centers. | Bilingual patient navigators |
Navigators were English- and Spanish-speaking peer counsellor and certified in core competencies of community health through a 12-week course offered at local community college. They also received training on the use of FRS and CVD risk reduction strategies by intervention staffs. They were also trained to identify participants readiness to change behaviors and to use motivational techniques. Additional training was also provided on human subject research, privacy practices, smoking cessation, medication adherence, cultural competency, and aggression management. Navigators were supervised by the intervention manager through periodic audits. |
Intervention was provided in-person and via phone. |
Study Settings
All but two studies were carried out in the USA. One study was carried out in France39 and one in Australia.56 All included studies were carried out in primary care38, 40–44, 46, 47, 49–55, 57–64 or in other community settings.39, 45, 48, 56, 65, 66 A range of primary care settings were reported including primary care practices, community health centers, and primary care units of hospitals. Community settings included rural community areas as well as civic organizations such as senior centers, churches, and a barbershop.
Study Designs
A variety of research designs were reported. Fifteen of the included studies were randomized controlled trials (RCT),38–44, 47, 48, 50, 54, 56, 59, 62, 64 six were quasi-experimental studies,49, 55, 58, 61, 63, 65 four were pre-post,45, 51, 57, 66 one was an interventional prospective cohort study,52 one was a retrospective comparative study,60 and two were mixed method studies.46, 53
Type of Participants
The interventions predominantly focused on the medically underserved populations such as racial/ethnic minorities or immigrants40, 43, 44, 46, 47, 52, 56–58, 64 including African Americans,41, 42, 48, 50, 54, 60, 65 Hispanic/Latinos,45, 49, 55, 59, 63, 66 and Asian and Pacific Islanders.38 In eight studies, participants were economically disadvantaged,39, 43, 46, 47, 58, 61, 62, 64 and in four, they were underinsured or uninsured.43, 44, 58, 61
Role Titles of CHWs
Healthcare navigation roles of CHWs were described through different role titles based on the activities they performed, including patient navigators,41, 43, 44, 46, 47, 52, 54, 55, 59, 62, 63 CHWs,48, 53, 57, 60, 64, 65 lay health workers,40, 51 bilingual CHWs,58, 66 Promotoras,49 care navigators,50 health navigators,38, 61 screening navigators,39 indigenous health workers,56 and peer navigators.42, 45
Recruitment, Training, and Supervision of CHWs
In most studies, CHWs were recruited from the communities they served with or without having any previous healthcare experience. CHWs were mostly female lay community members who spoke English in addition to their own community languages.
There was considerable variability in the breadth and extent of the description of training. Twenty-two studies38–45, 50–56, 58–60, 62–64, 66 documented the training of CHWs as navigators. In 16 studies,39, 40, 42, 43, 45, 50–54, 56, 59, 60, 63, 64, 66 CHWs received training as part of the intervention while six studies38, 41, 44, 55, 58, 62 reported that CHWs were trained before their recruitment. The most commonly reported components of the training included clinical education on specific diseases,42, 43, 45, 46, 53, 56, 60 screening related information,42, 45, 46, 53, 64, 66 motivational interviewing,50, 52, 53, 62 and communication skills.42, 52, 53, 59, 62 Other training addressed the navigation processes and responsibilities,42, 64 case management,50, 60 conducting community education,45, 59 patient centeredness,52, 56 risk factors of specific diseases,45, 66 patients readiness to change,55, 62 and identification and use of local resources.60
In most cases, training was provided face-to-face using both didactic classroom lectures and interactive role play. The length of the training period varied considerably, ranging from 3 h52 to 3 weeks.56 However, only a few studies reported details of the trainers and/or the institution or programs through which CHWs were trained. No studies evaluated the skills and competencies gained through CHW training. Supervision of the CHWs was reported in only 5 studies53, 55, 60, 62, 66 mostly by the program managers, in weekly or bi-weekly supervision meetings where case allocation,60 problem solving60,53,62 and CHW audit53, 55, 62, 66 were performed.
Types of CHW Roles as Navigator
The CHWs provided navigation assistance to the participants through a wide range of activities involving the prevention and management of different chronic illnesses (Table 3). The most frequently reported roles were education and counselling, addressing barriers to accessing screening or health services, and supporting patients to attend appointments (through scheduling, reminders, assistance with transport, or accompanying patients) and provide patient follow-up.
Table 3.
Roles of CHW as Navigators in Primary Care
| Outcome** | Education and counselling | Addressing barriers to screen or access | Scheduling appointments | Reminders for appointments | Transportation to appointments | Accompany to appointments | Communicate/coordinate with health providers | Helping with paperwork | Patient follow-up | Social support/community resources | Promoting self-management | Motivation interviewing | Monitoring disease status | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cancer screening and diagnosis | ||||||||||||||
| Braun 201538 | x | x | x | x | x | x | ||||||||
| Guillaume 201739 | + | x | x | |||||||||||
| Horne 201541 | + | x | ||||||||||||
| Jandorf 201342 | x | x | x | |||||||||||
| Phillips 201144 | + | x | x | |||||||||||
| Raich 201243 | x | x | x | x | ||||||||||
| Enard 201559 | + | x | x | x | ||||||||||
| Honeycutt 201361 | + | x | x | x | x | |||||||||
| Mojica 201666 | + | x | x | x | x | |||||||||
| Percac-Lima 201363 | + | x | x | x | ||||||||||
| Percac-Lima 200964 | + | x | x | x | x | |||||||||
| Allen 201445 | x | x | x | x | ||||||||||
| Battaglia 201246 | + | x | x | x | x | |||||||||
| Christie 200847 | + | x | x | x | x | x | ||||||||
| Cole 201748 | + | x | x | x | ||||||||||
| Dudley 201249 | + | x | ||||||||||||
| Lasser 200953 | x | x | ||||||||||||
| Marshall 201654 | x | x | ||||||||||||
| Access to primary care | ||||||||||||||
| Chukwudozie 201857 | + | x | x | x | ||||||||||
| Enard 201358 | x | x | x | |||||||||||
| Fedder 200360 | x | x | x | x | ||||||||||
| Felix 201965 | + | x | ||||||||||||
| McDermott 201556 | x | x | x | |||||||||||
| Griswold 201050 | + | x | x | |||||||||||
| Loskutova 201652 | x | x | x | |||||||||||
| Risk factors management | ||||||||||||||
| Lasser 201362 | x | |||||||||||||
| Shlay 201155 | x | |||||||||||||
| Total | 15 | 7 | 18 | 10 | 6 | 4 | 3 | 2 | 7 | 2 | 2 | 1 | 1 | |
**Outcome: positive for either increased screening or appropriate use of primary care
CHWs communicated with the participants both in-person and via telephone in 15 studies.38–40, 43, 45, 50, 54, 55, 58, 60–64, 66 However, in some studies, navigation consultations were provided either via telephone42, 44, 46–48, 51–53, 59 or in-person.41, 49, 56, 57, 65 Online media was also used in some studies40, 43, 45, 59 to complement in-person and telephone communication.
In 26 studies, CHWs were solely responsible for carrying out the intervention and the effect of the CHW role was evaluated independently. In three studies,42, 49, 57 CHWs were engaged as part of a team with other trained staff and CHW role was assessed as part of the team’s achievements.
Effects of CHW Navigation Intervention (Table 2)
Table 2.
Impact/Outcome of Healthcare Navigation Delivered by CHWs
| Impact on health behaviors, other underlying risk factors | Use of primary care, reducing barriers to access primary care | Use of secondary and tertiary services (e.g., Emergency Dept presentation, hospitalizations) | Impact on health screening, reducing barriers to screening | Intermediate outcomes or patient reported outcomes | Impact on patient satisfaction | Economic evaluation | |
|---|---|---|---|---|---|---|---|
| Allen et al., 201445 | ↑ | ↑ | |||||
| Battaglia et al., 201246 | ↑ | ↑ | ↑ | ||||
| Braun et al., 201538 | ↑ | ↑ | |||||
| Christie et al., 200847 | ↑ | ↑ | |||||
| Chukwudozie et al., 201857 | ↑ | ||||||
| Cole et al., 201748 | ↑ | ||||||
| Dudley et al., 201249 | ↑ | ||||||
| Enard and Ganelin, 201358 | ↑ | ↑ | |||||
| Enard et al., 201559 | ↑ | ||||||
| Fedder et al., 200360 | ↑ | ↑ | |||||
| Felix et al., 201965 | ↑ | ↑ | ↑ | ||||
| Fiscella et al., 201240 | ↔ | ↔ | |||||
| Griswold et al., 201050 | ↑ | ||||||
| Guillaume et al., 201739 | ↑ | ||||||
| Honeycutt et al., 201361 | ↑ | ||||||
| Horne et al., 201541 | ↑ | ||||||
| Jandorf et al., 201342 | ↔ | ||||||
| Lasser et al., 200953 | ↑ | ||||||
| Lasser et al., 201362 | ↑ | ↑ | |||||
| Lui and Perkins, 201551 | ↑ | ||||||
| Loskutova et al., 201652 | ↑ | ↑ | |||||
| Marshall et al., 201654 | ↑ | ||||||
| McDermott et al., 201556 | ↑ | ||||||
| Mojica et al., 201666 | ↑ | ||||||
| Percac-Lima et al., 201363 | ↑ | ↑ | |||||
| Percac-Lima et al., 200964 | ↑ | ||||||
| Phillips et al., 201144 | ↑ | ||||||
| Raich et al., 201243 | ↑ | ||||||
| Shlay et al., 201155 | ↑ |
Cancer Prevention and Treatment
Among the 17 studies38, 39, 41, 42, 44–48, 51, 53, 54, 59, 61, 63, 64, 66 that investigated the effect of CHWs in improving cancer screening outcomes through providing navigation supports, increase in cancer screening rates was noted in 15 studies38, 39, 41, 44, 46–48, 51, 53, 54, 59, 61, 63, 64, 66 (3 of them were of strong methodological quality, 6 moderate, and 6 weak). Significant positive changes in adherence to breast cancer screening were reported in 5 studies38, 44, 46, 54, 66 of the 6 that targeted breast cancer. Of the 13 studies that focused on colorectal cancer, 12 studies noted significant increase in adherence to colorectal cancer screening.38, 39, 41, 47, 48, 51, 53, 59, 61, 63, 64, 66 Positive outcomes in screening for multiple cancers such as breast, colorectal, cervical, and prostate were also noted in all the three studies38, 45, 66 (with varied mythological qualities) that focused on multiple cancers. Two interventions, one with strong methodological quality43 and other weak,49 focused on the time for cancer diagnostic resolution following an abnormal screening result and both reported a significantly shorter time among the navigated participants compared to those without navigation. Another study with strong methodological quality40 reported no significant improvement in the time to completion of primary cancer treatment among the navigated participants compared to the non-navigated.
Effective Primary Care Services
Effective primary care services included improved access and continuity of care through regular visits, appropriate follow-up, and linking to long-term resources for care. Of the five studies40, 46, 50, 57, 65 that focused on primary care, all but one study40 noted a significant improvement in use of primary care services among the navigated patients. In two of the four studies with positive outcomes, the methods were of moderate quality,57, 65 and in others, the methods were weak.46, 50 Battaglia et al.46 found that 71% of the participants scheduled primary care visit to follow-up on their health priorities, and after 30 days, 54% of participants visited their primary care provider. Chukwudozie and colleagues57 noted that CHWs were effective in increasing the use of patient-centered medical home for kidney disease primary care physician (PCMH-KD PCP) among the patients. A moderate--quality study65 that focused on identifying the patients with long-term health needs and linking them to local resources found that CHWs were effective in identifying and helping patients access long-term care services (HCBS). However, Fiscella et al.,40 in a study of strong methodological quality, did not find any significant effect of navigators in time to completion of cancer treatment or psychological distress in primary care.
Reducing Use of Secondary and Tertiary Care
Three moderate quality studies58, 60, 65 investigated the effect of CHWs as navigators in reducing the use of secondary and tertiary services and all reported positive outcomes. Of the two studies that focused on reducing use of emergency department, one study58 noted that navigated patients had significantly fewer primary care-related emergency department visits during the intervention period. The other study60 also reported that emergency room visits decreased by 38% among the navigated patients and hospital admissions were reduced by 53% in 1 year post-intervention. One study65 tested the effect of CHWs as navigators in use of nursing homes and found that visits by navigated participants to nursing homes were five times fewer than those who were not navigated.
Intermediate Outcomes
All four studies that focused on assessing the effect of CHWs as navigators on patient reported outcomes or intermediate outcomes52, 55, 56, 63 reported significant positive outcomes. However, their methodological quality varied from weak52, 55 to moderate.56, 63 Two studies52, 56 reported significant reductions in HBA1c level (p<0.05) and another55 a reduction in total cholesterol (183 mg/dL vs 197 mg/dL). Another study63 found a reduction in the severity of cervical abnormalities in Pap smears among intervention compared control patients.
Addressing Risk Factors for Chronic Disease
Two moderate62 to weak55 methodological quality studies tested the effect of a CHW navigation intervention on how effectively the risk factors of chronic disease were addressed. One62 found no difference in adherence to smoking cessation (47.4% vs 42.9%, p=0.80). Another found that CHW navigation had a greater impact on reducing cardiovascular risk68 after 12 months of follow-up.
Patient Satisfaction
Patient levels of satisfaction with the navigation services were assessed in six studies38, 40, 46, 47, 52, 62 and all but one study reported that majority of the navigated participants were satisfied with the navigation services. For example, Loskutova et al.52 reported that levels of satisfaction were high among the participants receiving the navigation services and they would recommend the services to their friend and family, and 90% of the patients reported that they would use the program in future. A study by Lasser et al.62 found that most of the patients were satisfied with the navigation services and they did not feel any pressure to make changes. However, Fiscella et al.40 found no significant difference between navigated and non-navigated participants in terms of satisfaction with cancer-related primary care. However, they noted that socially disadvantaged patients who received patient navigation services were more satisfied than those who received usual care (p<0.05). Three of the studies with positive outcomes were of weak,46, 47, 52 one moderate62, and two strong 38, 40 methodological quality.
Cost Outcomes
Three moderate methodological quality studies58, 60, 65 measured cost outcomes of the CHW navigation intervention. In one study,58 it was found that the total savings associated with reduction of emergency room visit among the navigated participants was higher than the cost of implementing the intervention. Fedder et al.60 also noted that their CHW program resulted in an annual average savings of $2245 per year. The other study65 found that mean annual spending per beneficiary was significantly higher among the navigated participants than non-navigated ($6769 vs $3687, p<0.0001), but this was not assessed in terms of the benefit of the intervention.
DISCUSSION
This review identified that CHW navigation interventions were effective in increasing adherence to cancer screening, particularly for breast, cervical, and colorectal cancers, and improving use of primary care for effective chronic disease management. However, there was insufficient evidence of their impact on use of secondary and tertiary care, risk factors or intermediary outcomes in chronic disease management, or cost-effectiveness. The impact on patient satisfaction was uncertain due to lack of high-quality studies. These findings are consistent with other reviews evaluating CHW interventions, although in these reviews, navigation was only one component of a more complicated intervention33, 67, 68 or navigation was performed by other providers other than CHWs.5, 68, 69 Kim et al.67 reported in a systematic review that CHWs were effective in improving access to cancer screening. They also commented on the lack of strong evidence for the cost-effectiveness of CHW interventions. In another review,68 it was also reported that CHWs and patient navigators were effective in improving adherence to and timely completion of breast, cervical, and colorectal cancer screening in medically underserved populations.
The most frequently reported functional roles for community health navigators are listed in Table 3. Most interventions with these roles reported positive outcomes in terms of either increased cancer screening and diagnosis or more appropriate use of primary care. These roles also map against the patient education and care coordination roles defined in the CHW Core Consensus (C3) project70 and similar roles for CHW in primary care were defined in a review by Hartzler et al..71 Based on these findings, we have suggested four core functional roles for CHW as navigators for patients with chronic disease in primary care (Box 2). There was limited evidence for other roles such as social support and self-management.
Box 2 Functional roles for CHW as navigators in primary care
| Domain | Sub-roles | ||
| Core | 1 | Health Education | Provision of education and counselling about health care |
| 2 | Addressing barriers | Identification and addressing of barriers to health care | |
| 3 | Care navigation | Helping schedule appointments, reminders, assisting with transport and accompanying patients to appointments | |
| 4 | Patients follow up | Following patients up after healthcare | |
| Other potential | Coordination with other providers | Communication and coordination with other healthcare providers | |
| Community resources/social support | Linking patients with community resources | ||
| Monitoring | Supporting patients to monitor their condition | ||
| Self-management | Motivation and support for self-management | ||
Similar to another study,67 most of the studies in our review reported that CHWs were recruited from the communities they served and this has been previously noted to help ensure cultural sensitivity and wider community acceptance.33 The settings in which the CHW was based were primary care or the community. However, neither of these settings was more likely to be associated with positive screening or access outcomes.
There was a wide variability in terms of the criteria for recruitment of the CHWs, duration, frequency and mode of training, qualification of the trainers, and supervision arrangements in the included studies. Many of the studies provided insufficient information on these critical aspects of CHW programs and we were unable to assess their effectiveness. Other systematic reviews have also reported variability in recruitment, training, and supervision of navigators.67, 68 Previous reviews33, 72, 73 pointed out the importance of rigorous training and optimum level of competencies gained through the training to successfully complete the assigned tasks. Yet, no study in the present review reported the competencies gained through the training. In the future, studies should clearly describe the training including training materials, frequency, and duration of training as well as competencies gained through the training.
Policy Implications
Previous research has highlight the important contribution which system navigation can make to healthcare access and care coordination.4 The findings of the present review have significant implications for incorporating CHWs as part of the patient-centered primary care team. Carter and colleagues4 also mentioned that while navigator roles can add an additional complexity to the health system, they can substantially contribute to improve care coordination and facilitation of care and services. While discussing the navigation role, McBrien et al.5 recommended that patient navigators should focus on identification and addressing barriers to receipt of care rather than providing any clinical support. It is also very important to develop clear selection criteria for navigators, a well-developed training procedure, competency assessment, and proper supervision arrangements before recommending that CHWs as navigator become integrated into the healthcare team.68 The level of reimbursement for the CHWs is also important. While we did not find any information pertaining to this, previous studies74, 75 have pointed out that CHWs were more flexible and productive when they were adequately reimbursed.
As in previous studies,67, 68 we found a lack of sufficient information on the cost-effectiveness of CHW interventions. This can be challenging, as it is often difficult to separate out the cost-effectiveness of CHW interventions themselves from the medical interventions that they support (e.g., cancer screening). Future research should focus on rigorous cost-effectiveness analysis of CHW navigation interventions before integrating them into the healthcare system.
Limitations
Our review had several limitations. As there are several role titles for CHWs in the literature, it is possible that some, with titles outside those used in our search, may have been missed. To address this, we exploded both MeSH terms and keywords in our database searches. We restricted our searches to peer-reviewed articles only, and therefore, we might have missed some non-peer-reviewed gray literature published outside of academic journals.
There are also methodological issues that need to be considered when interpreting the study results as only 6 of the included studies were of strong methodological quality. Several of those with a strong research design (RCT)40, 47, 50, 59 were of weak to moderate methodological quality. There was also significant variability in the reporting of the intervention characteristics (Annex 3) that need to be considered when interpreting the impact of specific roles for CHW as navigators.
We restricted our searches to English papers and thus may have missed publications written in non-English languages. In some of the included studies, the intervention involved CHWs as part of a team and the effect of CHWs was not assessed separately. Also, we could not conduct a meta-analysis due to heterogeneity in the study designs and outcomes of the included studies.
CONCLUSION
Our review suggests that CHW navigation interventions were effective in supporting screening for cancer and access to primary care. Our findings suggest that core roles include health education, addressing barriers to care, providing navigation to care, and patient follow-up. However, there was insufficient evidence of cost-effectiveness, clinical outcomes, and patient experience resulting from the CHW navigation roles. Future research needs to be of strong methodological quality and should focus on determining the relative effectiveness of elements of CHW navigation roles in improving health outcomes and patient experience in primary care.
Supplementary Information
(DOCX 15 kb)
(DOCX 18 kb)
(DOCX 19 kb)
(DOCX 23 kb)
(DOC 64 kb)
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Noncommunicable diseases: key fact. 2018. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases. Accessed 03/09/2020.
- 2.Roser M, Ritchie H. Burden of disease. Our World in Data. 2016. https://ourworldindata.org/burden-of-disease. Accessed 03/09/2020.
- 3.Dennis SM, Zwar N, Griffiths R, Roland M, Hasan I, Powell Davies G, et al. Chronic disease management in primary care: from evidence to policy. Med J Aust. 2008;188:S53–S6. doi: 10.5694/j.1326-5377.2008.tb01745.x. [DOI] [PubMed] [Google Scholar]
- 4.Carter N, Valaitis RK, Lam A, Feather J, Nicholl J, Cleghorn L. Navigation delivery models and roles of navigators in primary care: a scoping literature review. BMC Health Serv Res. 2018;18(1):96. doi: 10.1186/s12913-018-2889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McBrien KA, Ivers N, Barnieh L, Bailey JJ, Lorenzetti DL, Nicholas D, et al. Patient navigators for people with chronic disease: a systematic review. PLoS One. 2018;13(2):e0191980. doi: 10.1371/journal.pone.0191980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Victoria ECC. An investment not an expense: Enhancing the health literacy in culturally and linguistically diverse communities. 2012. https://apo.org.au/node/30745. Accessed 03/09/2020.
- 7.Chiarenza A, Dauvrin M, Chiesa V, Baatout S, Verrept H. Supporting access to healthcare for refugees and migrants in European countries under particular migratory pressure. BMC Health Serv Res. 2019;19(1):513. doi: 10.1186/s12913-019-4353-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin CM, Peterson C. Improving chronic illness care: revisiting the role of care planning. Aust Fam Physician. 2008;37(3):161. [PubMed] [Google Scholar]
- 9.Rothman AA, Wagner EH. Chronic illness management: what is the role of primary care? Ann Intern Med. 2003;138(3):256–61. doi: 10.7326/0003-4819-138-3-200302040-00034. [DOI] [PubMed] [Google Scholar]
- 10.Reynolds R, Dennis S, Hasan I, Slewa J, Chen W, Tian D, et al. A systematic review of chronic disease management interventions in primary care. BMC Fam Pract. 2018;19(1):11. doi: 10.1186/s12875-017-0692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levesque J-F, Breton M, Senn N, Levesque P, Bergeron P, Roy DA. The interaction of public health and primary care: functional roles and organizational models that bridge individual and population perspectives. Public Health Rev. 2013;35(1):14. [Google Scholar]
- 12.Pati S, Chauhan AS, Mahapatra S, Sinha R, Pati S. Practicing health promotion in primary care–a reflective enquiry. J Prev Med Hyg. 2017;58(4):E288. doi: 10.15167/2421-4248/jpmh2017.58.4.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kadu MK, Stolee P. Facilitators and barriers of implementing the chronic care model in primary care: a systematic review. BMC Fam Pract. 2015;16(1):12. doi: 10.1186/s12875-014-0219-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foo KM, Sundram M, Legido-Quigley H. Facilitators and barriers of managing patients with multiple chronic conditions in the community: a qualitative study. BMC Public Health. 2020;20(1):1–15. doi: 10.1186/s12889-020-8375-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Song HJ, Dennis S, Levesque J-F, Harris MF. What matters to people with chronic conditions when accessing care in Australian general practice? A qualitative study of patient, carer, and provider perspectives. BMC Fam Pract. 2019;20(1):79. doi: 10.1186/s12875-019-0973-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Correa-Velez I, Sundararajan V, Brown K, Gifford SM. Hospital utilisation among people born in refugee-source countries: an analysis of hospital admissions, Victoria, 1998–2004. Med J Aust. 2007;186(11):577–80. doi: 10.5694/j.1326-5377.2007.tb01058.x. [DOI] [PubMed] [Google Scholar]
- 17.Spike EA, Smith MM, Harris MF. Access to primary health care services by community-based asylum seekers. Med J Aust. 2011;195(4):188–91. doi: 10.5694/j.1326-5377.2011.tb03277.x. [DOI] [PubMed] [Google Scholar]
- 18.Keleher H, Thomacos N. Health literacy and CALD populations in Australia. Aust Mosaic. 2009;22:27–8. [Google Scholar]
- 19.Alaofè H, Asaolu I, Ehiri J, Moretz H, Asuzu C, Balogun M, et al. Community health Workers in Diabetes Prevention and Management in developing countries. Ann Glob Health. 2017;83(3-4):661–75. doi: 10.1016/j.aogh.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 20.Mishra SR, Neupane D, Preen D, Kallestrup P, Perry HB. Mitigation of non-communicable diseases in developing countries with community health workers. Glob Health. 2015;11(1):43. doi: 10.1186/s12992-015-0129-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schaaf M, Fox J, Topp SM, Warthin C, Freedman LP, Robinson RS, et al. Community health workers and accountability: reflections from an international “think-in”. International Journal for Equity in Health 2018;17(1):1-5. [DOI] [PMC free article] [PubMed]
- 22.American Public Health A. Support for community health worker leadership in determining workforce standards for training and credentialing. 2014. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2015/01/28/14/15/support-forcommunity-health-worker-leadership. Accessed 03/09/2020.
- 23.Bemelmans M, Baert S, Negussie E, Bygrave H, Biot M, Jamet C, et al. Sustaining the future of HIV counselling to reach 90-90-90: a regional country analysis. J Int AIDS Soc. 2016;19(1):20751. doi: 10.7448/IAS.19.1.20751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruizendaal E, Dierickx S, Grietens KP, Schallig HD, Pagnoni F, Mens PF. Success or failure of critical steps in community case management of malaria with rapid diagnostic tests: a systematic review. Malar J. 2014;13(1):229. doi: 10.1186/1475-2875-13-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pérez-Escamilla R, Damio G, Chhabra J, Fernandez ML, Segura-Pérez S, Vega-López S, et al. Impact of a community health workers–led structured program on blood glucose control among Latinos with type 2 diabetes: the DIALBEST trial. Diabetes Care 2015;38(2):197-205. [DOI] [PMC free article] [PubMed]
- 26.Matiz LA, Peretz PJ, Jacotin PG, Cruz C, Ramirez-Diaz E, Nieto AR, et al. The impact of integrating community health workers into the patient-centered medical home. Journal of Primary Care & Community health 2014;5(4):271-4. [DOI] [PubMed]
- 27.Kangovi S, Mitra N, Grande D, White ML, McCollum S, Sellman J, et al. Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA Internal Medicine 2014;174(4):535-43. [DOI] [PubMed]
- 28.Rahman A, Fisher J, Bower P, Luchters S, Tran T, Yasamy MT, et al. Interventions for common perinatal mental disorders in women in low-and middle-income countries: a systematic review and meta-analysis. Bulletin of the World Health Organization 2013;91:593-601I. [DOI] [PMC free article] [PubMed]
- 29.Lassi ZS, Bhutta ZA. Community‐based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database of Systematic Reviews 2015(3). [DOI] [PMC free article] [PubMed]
- 30.Hoeft TJ, Fortney JC, Patel V, Unützer J. Task-sharing approaches to improve mental health care in rural and other low-resource settings: a systematic review. J Rural Health. 2018;34(1):48–62. doi: 10.1111/jrh.12229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Freeman HP. The origin, evolution, and principles of patient navigation. 2012. https://cebp.aacrjournals.org/content/21/10/1614. Accessed 03/09/2020. [DOI] [PubMed]
- 32.Freeman HP. The history, principles, and future of patient navigation: commentary. Semin Oncol Nurs 2013;29(2):72-5. [DOI] [PubMed]
- 33.Shommu NS, Ahmed S, Rumana N, Barron GRS, McBrien KA, Turin TC. What is the scope of improving immigrant and ethnic minority healthcare using community navigators: A systematic scoping review. Int J Equity Health. 2016;15(1):6. doi: 10.1186/s12939-016-0298-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Bmj. 2009;339:b2700-b. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Covidence. https://www.covidence.org/. Accessed 25/05/2020.
- 36.Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid-Based Nurs. 2004;1(3):176–84. doi: 10.1111/j.1524-475X.2004.04006.x. [DOI] [PubMed] [Google Scholar]
- 37.Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. Bmj 2014;348:g1687. [DOI] [PubMed]
- 38.Braun KL, Thomas WL, Jr, Domingo JL, Allison AL, Ponce A, Haunani Kamakana P, et al. Reducing cancer screening disparities in medicare beneficiaries through cancer patient navigation. J Am Geriatr Soc. 2015;63(2):365–70. doi: 10.1111/jgs.13192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guillaume E, Dejardin O, Bouvier V, De Mil R, Berchi C, Pornet C, et al. Patient navigation to reduce social inequalities in colorectal cancer screening participation: A cluster randomized controlled trial. Prev Med. 2017;103:76–83. doi: 10.1016/j.ypmed.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 40.Fiscella K, Whitley E, Hendren S, Raich P, Humiston S, Winters P, et al. Patient navigation for breast and colorectal cancer treatment: a randomized trial. 2012. https://cebp.aacrjournals.org/content/21/10/1673. Accessed 03/09/2020. [DOI] [PMC free article] [PubMed]
- 41.Horne HN, Phelan-Emrick DF, Pollack CE, Markakis D, Wenzel J, Ahmed S, et al. Effect of patient navigation on colorectal cancer screening in a community-based randomized controlled trial of urban African American adults. Cancer Causes Control. 2015;26(2):239–46. doi: 10.1007/s10552-014-0505-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jandorf L, Braschi C, Ernstoff E, Wong CR, Thelemaque L, Winkel G, et al. Culturally targeted patient navigation for increasing African Americans’ adherence to screening colonoscopy: a randomized clinical trial. Cancer Epidemiol Biomark Prev. 2013;22(9):1577–87. doi: 10.1158/1055-9965.EPI-12-1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Raich PC, Whitley EM, Thorland W, Valverde P, Fairclough D. Patient navigation improves cancer diagnostic resolution: an individually randomized clinical trial in an underserved population. 2012. https://cebp.aacrjournals.org/content/21/10/1629. Accessed 03/09/2020. [DOI] [PMC free article] [PubMed]
- 44.Phillips CE, Rothstein JD, Beaver K, Sherman BJ, Freund KM, Battaglia TA. Patient navigation to increase mammography screening among inner city women. J Gen Intern Med. 2011;26(2):123–9. doi: 10.1007/s11606-010-1527-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Allen JD, Perez JE, Tom L, Leyva B, Diaz D, Idali TM. A pilot test of a church-based intervention to promote multiple cancer-screening behaviors among Latinas. J Cancer Educ. 2014;29(1):136–43. doi: 10.1007/s13187-013-0560-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Battaglia TA, McCloskey L, Caron SE, Murrell SS, Bernstein E, Childs A, et al. Feasibility of chronic disease patient navigation in an urban primary care practice. J Ambul Care Manage. 2012;35(1):38–49. doi: 10.1097/JAC.0b013e31822cbd7c. [DOI] [PubMed] [Google Scholar]
- 47.Christie J, Itzkowitz S, Lihau-Nkanza I, Castillo A, Redd W, Jandorf L. A randomized controlled trial using patient navigation to increase colonoscopy screening among low-income minorities. J Natl Med Assoc. 2008;100(3):278–84. doi: 10.1016/s0027-9684(15)31240-2. [DOI] [PubMed] [Google Scholar]
- 48.Cole H, Thompson HS, White M, Browne R, Trinh-Shevrin C, Braithwaite S, et al. Community-based, preclinical patient navigation for colorectal cancer screening among older black men recruited from barbershops: The MISTER B Trial. Am J Public Health. 2017;107(9):1433–40. doi: 10.2105/AJPH.2017.303885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dudley DJ, Drake J, Quinlan J, Holden A, Saegert P, Karnad A, et al. Beneficial effects of a combined navigator/promotora approach for Hispanic women diagnosed with breast abnormalities. Cancer Epidemiol Biomark Prev. 2012;21(10):1639–44. doi: 10.1158/1055-9965.EPI-12-0538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Griswold KS, Homish GG, Pastore PA, Leonard KE. A randomized trial: are care navigators effective in connecting patients to primary care after psychiatric crisis? Community Ment Health J. 2010;46(4):398–402. doi: 10.1007/s10597-010-9300-x. [DOI] [PubMed] [Google Scholar]
- 51.Liu G, Perkins A. Using a lay cancer screening navigator to increase colorectal cancer screening rates. J Am Board Fam Med. 2015;28(2):280–2. doi: 10.3122/jabfm.2015.02.140209. [DOI] [PubMed] [Google Scholar]
- 52.Loskutova NY, Tsai AG, Fisher EB, LaCruz DM, Cherrington AL, Harrington TM, et al. Patient navigators connecting patients to community resources to improve diabetes outcomes. J Am Board Fam Med. 2016;29(1):78–89. doi: 10.3122/jabfm.2016.01.150048. [DOI] [PubMed] [Google Scholar]
- 53.Lasser KE, Murillo J, Medlin E, Lisboa S, Valley-Shah L, Fletcher RH, et al. A multilevel intervention to promote colorectal cancer screening among community health center patients: Results of a pilot study. BMC Fam Pract. 2009;10. doi:10.1186/1471-2296-10-37 [DOI] [PMC free article] [PubMed]
- 54.Marshall JK, Mbah OM, Ford JG, Phelan-Emrick D, Ahmed S, Bone L, et al. Effect of patient navigation on breast cancer screening among African American Medicare beneficiaries: a randomized controlled trial. J Gen Intern Med. 2016;31(1):68–76. doi: 10.1007/s11606-015-3484-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shlay JC, Barber B, Mickiewicz T, Maravi M, Drisko J, Estacio R, et al. Peer Reviewed: Reducing Cardiovascular Disease Risk Using Patient Navigators, Denver, Colorado, 2007-2009. Prev Chronic Dis 2011;8(6):A143. [PMC free article] [PubMed]
- 56.McDermott RA, Schmidt B, Preece C, Owens V, Taylor S, Li M, et al. Community health workers improve diabetes care in remote Australian indigenous communities: Results of a pragmatic cluster randomized controlled trial. BMC Health Serv Res. 2015; 15(1). doi:10.1186/s12913-015-0695-5 [DOI] [PMC free article] [PubMed]
- 57.Chukwudozie IB, Fitzgibbon ML, Schiffer L, Berbaum M, Gilmartin C, David P, et al. Facilitating primary care provider use in a patient-centered medical home intervention study for chronic hemodialysis patients. Transl Behav Med. 2018;8(3):341–50. doi: 10.1093/tbm/iby021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Enard KR, Ganelin DM. Reducing preventable emergency department utilization and costs by using community health workers as patient navigators. J Healthc Manag. 2013;58(6):412–27. [PMC free article] [PubMed] [Google Scholar]
- 59.Enard KR, Nevarez L, Hernandez M, Hovick SR, Moguel MR, Hajek RA, et al. Patient navigation to increase colorectal cancer screening among Latino Medicare enrollees: a randomized controlled trial. Cancer Causes Control. 2015;26(9):1351–9. doi: 10.1007/s10552-015-0620-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fedder DO, Chang RJ, Curry S, Nichols G. The effectiveness of a community health worker outreach program on healthcare utilization of West Baltimore City medicaid patients with diabetes, with or without hypertension. Ethn Dis. 2003;13(1):22–7. [PubMed] [Google Scholar]
- 61.Honeycutt S, Green R, Ballard D, Hermstad A, Brueder A, Haardorfer R, et al. Evaluation of a patient navigation program to promote colorectal cancer screening in rural Georgia, USA. Cancer. 2013;119(16):3059–66. doi: 10.1002/cncr.28033. [DOI] [PubMed] [Google Scholar]
- 62.Lasser KE, Kenst KS, Quintiliani LM, Wiener RS, Murillo J, Pbert L, et al. Patient navigation to promote smoking cessation among low-income primary care patients: a pilot randomized controlled trial. J Ethn Subst Abus. 2013;12(4):374–90. doi: 10.1080/15332640.2013.819311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Percac-Lima S, Benner CS, Lui R, Aldrich LS, Oo SA, Regan N, et al. The impact of a culturally tailored patient navigator program on cervical cancer prevention in Latina women. J Women's Health. 2013;22(5):426–31. doi: 10.1089/jwh.2012.3900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Percac-Lima S, Grant RW, Green AR, Ashburner JM, Gamba G, Oo S, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009;24(2):211–7. doi: 10.1007/s11606-008-0864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Felix HC, Ali M, Bird TM, Cottoms N, Stewart MK. Are community health workers more effective in identifying persons in need of home and community-based long-term services than standard-passive approaches. Home Health Care Serv Q. 2019;38(3):194–208. doi: 10.1080/01621424.2019.1604461. [DOI] [PubMed] [Google Scholar]
- 66.Mojica CM, Morales-Campos DY, Carmona CM, Ouyang Y, Liang Y. Breast, Cervical, and Colorectal Cancer Education and Navigation: Results of a Community Health Worker Intervention. Health Promot Pract. 2016;17(3):353–63. doi: 10.1177/1524839915603362. [DOI] [PubMed] [Google Scholar]
- 67.Kim K, Choi JS, Choi E, Nieman CL, Joo JH, Lin FR, et al. Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: a systematic review. Am J Public Health. 2016;106(4):e3–e28. doi: 10.2105/AJPH.2015.302987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Roland KB, Milliken EL, Rohan EA, DeGroff A, White S, Melillo S. Use of Community Health Workers and Patient Navigators to Improve Cancer Outcomes Among Patients Served by Federally Qualified Health Centers: A Systematic Literature Review. Health Equity. 2017;1(1):61–76. doi: 10.1089/heq.2017.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ali-Faisal SF, Colella TJF, Medina-Jaudes N, Scott LB. The effectiveness of patient navigation to improve healthcare utilization outcomes: A meta-analysis of randomized controlled trials. Patient Educ Couns. 2017;100(3):436–48. doi: 10.1016/j.pec.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 70.C3 Project. CHW Core Consensus Project. 2018. https://www.c3project.org/. Accessed 29/12/2020.
- 71.Hartzler AL, Tuzzio L, Hsu C, Wagner EH. Roles and functions of community health workers in primary care. Ann Fam Med. 2018;16(3):240–5. doi: 10.1370/afm.2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Norris SL, Chowdhury FM, Van Le K, Horsley T, Brownstein JN, Zhang X, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006;23(5):544–56. doi: 10.1111/j.1464-5491.2006.01845.x. [DOI] [PubMed] [Google Scholar]
- 73.Brownstein JN, Chowdhury FM, Norris SL, Horsley T, Jack L, Jr, Zhang X, et al. Effectiveness of community health workers in the care of people with hypertension. Am J Prev Med. 2007;32(5):435–47. doi: 10.1016/j.amepre.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 74.Kasteng F, Settumba S, Källander K, Vassall A, in SSG Valuing the work of unpaid community health workers and exploring the incentives to volunteering in rural Africa. Health Policy Plan. 2016;31(2):205–16. doi: 10.1093/heapol/czv042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cherrington A, Ayala GX, Elder JP, Arredondo EM, Fouad M, Scarinci I. Recognizing the diverse roles of community health workers in the elimination of health disparities: from paid staff to volunteers. Ethn Dis. 2010;20(2):189. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 15 kb)
(DOCX 18 kb)
(DOCX 19 kb)
(DOCX 23 kb)
(DOC 64 kb)