Abstract
BACKGROUND
Association between tea consumption and incident hypertension remains uncertain. This study conducted to examine the health effects of tea consumption on blood pressure progression and hypertension incidence.
METHODS
A population-based cohort of 38,913 Chinese participants without hypertension at baseline were included in the current study. Information on tea consumption was collected through standardized questionnaires. Associations of tea consumption with blood pressure progression and incident hypertension were analyzed using logistic regression models and Cox proportional hazards regression models, respectively.
RESULTS
During a median follow-up of 5.9 years, 17,657 individuals had experienced progression to a higher blood pressure stage and 5,935 individuals had developed hypertension. In multivariate analyses, habitual tea drinkers (≥ 3 times/week for at least six months) had a 17% lower risk for blood pressure progression [odds ratio (OR) = 0.83, 95% CI: 0.79–0.88] and a 14% decreased risk for incident hypertension [hazard ratio (HR) = 0.86, 95% CI: 0.80–0.91] compared with non-habitual tea drinkers. Individuals in different baseline blood pressure groups could obtain similar benefit from habitual tea drinking. In terms of tea consumption amount, an inverse, linear dose-response relation between monthly consumption of tea leaves and risk of blood pressure progression was observed, while the risk of incident hypertension did not reduce further after consuming around 100 g of tea leaves per month.
CONCLUSIONS
Our study demonstrated that habitual tea consumption could provide preventive effect against blood pressure progression and hypertension incidence.
Cardiovascular disease (CVD) is the leading cause of death in China. Hypertension is the most important risk factor for CVD that affects 23.2% of Chinese adults.[1] According to the Global Burden of Disease Study, high systolic blood pressure (SBP) was consistently responsible for the largest number of all-cause deaths, which accounted for 10.8 million deaths in 2019.[2] Furthermore, 29.2% of global adult population were predicted to have hypertension and the number of adults with hypertension was predicted to be 1.56 billion in 2025.[3] Thus, it is essential to place high priority for hypertension prevention and control.
Tea is produced from hot water infusion of dried Camellia sinensis to create a flavonoid-rich beverage. As the second most frequently consumed beverage worldwide, tea has been regularly consumed for centuries in China. Given the high consumption of tea, it is important to understand its potential health effects in diverse populations. Over the past few decades, exploratory research has reported that tea may influence the risks of numerous diseases, including CVD, type 2 diabetes mellitus, and cancer.[4–6] Many epidemiological studies have shown that tea consumption was related to lower risk of CVD.[4,7,8] One potential mechanism is that tea consumption might lower blood pressure (BP), thereby mediating the protective effect of tea on CVD. However, existing evidence remains inconclusive as to the association between tea consumption and hypertension risk.[9–13] Relatively small sample sizes, cross-sectional design, and the absence of important covariates might have led to the varying results. Evidence related to this association from prospective investigations is still lacking. Therefore, large-scale prospective cohort studies are essential to investigate the associations of tea consumption with BP progression and hypertension incidence.
In the current study, we aimed to assess the longitudinal relationship of tea consumption with BP progression and incident hypertension among a prospective cohort of 38,913 Chinese adults.
METHODS
Study Population
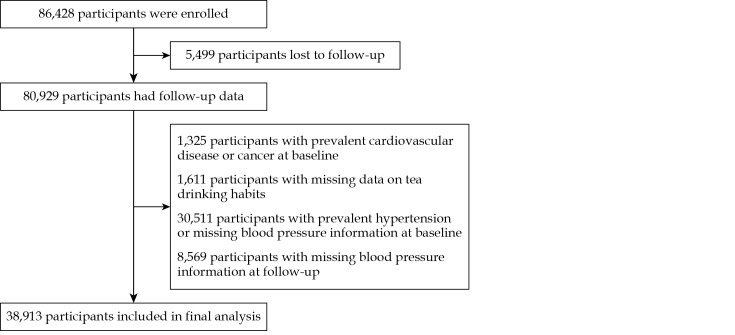
Participants for the current study were from the Community Intervention of Metabolic Syndrome in China & Chinese Family Health Study (CIMIC). Details of study design and inclusion criteria for this study have been described elsewhere. [14] In brief, the CIMIC study was a large, community-based cohort established from 2007 to 2008. A cluster random sampling method was applied to select participants aged ≥ 18 years in Shandong, Henan, and Jiangsu provinces. A total of 86,428 participants were enrolled at baseline and invited to participate in the follow-up survey from 2012 to 2015. Of the original participants in the CIMIC study, 80,929 participants were followed-up successfully (93.6%). We subsequently excluded 1,325 participants who reported a history of CVD or cancer at baseline, 1,611 participants with missing data on tea drinking habits, 30,511 participants with prevalent hypertension or missing BP information at baseline, and 8,569 participants with missing BP information at follow-up. Finally, 38,913 participants were available for the current analyses (Figure 1).
Figure 1.
Flowchart of study population inclusion and exclusion.
This study was approved by the Institutional Review Board at Fuwai Hospital in Beijing (No.2012-399). Informed consent was obtained from each participant prior to data collection.
Assessment of Tea Consumption and Covariates
At the baseline survey, all participants were asked to report their tea consumption habit during the past year through standardized questionnaires by trained and certificated staff. Tea drinking frequency was measured via the times of replacement of tea leaves or tea bags. Participants were asked whether they were habitual tea drinkers (≥ 3 times/week for at least six months) or not. We further collected information on monthly tea leaves consumption amount [dry weight, in Chinese liang (unit of weight equal to 50 g)] for habitual tea drinkers.
Information on socio-demographic characteristics, lifestyle risk factors, and family and personal medical history via standardized questionnaires were also collected at baseline. Body weight and height were measured with participants wearing only light clothes without shoes. Body mass index (BMI) was defined as the body weight divided by the square of the body height (kg/m2). A smoker was defined as someone who had consumed at least one cigarette daily for one year or more. An alcohol drinker was defined as someone who drank at least once weekly during the past year. Ideal physical activity was defined as at least 150 min of moderate physical activity or at least 75 min of vigorous physical activity per week. Family history of hypertension was considered positive if his/her parent or sibling were reported with hypertension. Blood samples were drawn from participants after fasting for at least ten hours to determine blood glucose and lipid levels.
Outcome Measures
We measured BP and collected data on antihypertensive drugs at baseline and follow-up visit. Trained investigators measured BP using an electronic BP monitor during the clinic or home visits generally in the morning, according to a common protocol recommended by the American Heart Association.[15] Participants were advised to avoid alcohol, cigarette smoking, coffee/tea, and exercise for at least 30 min before their BP measurement. BP was measured with the participant in the sitting position after at least 5 min of rest. An appropriate arm-cuff (pediatric, regular adult, large, or thigh) was chosen based on the circumference of participant’s arm and was placed on the right arm. BP measurements were repeated three times with a thirty-second interval between each measurement. The average of the three BP measurements was used in the analysis.
At baseline, three BP categories were defined as follows: (1) below 120 mmHg for SBP and 75 mmHg for diastolic blood pressure (DBP); (2) 120−129 mmHg for SBP or 75−84 mmHg for DBP; and (3) 130−139 mmHg for SBP or 85–89 mmHg for DBP.[16] To assess BP progression, we created categories of BP at follow-up identical to those at baseline. BP progression was defined by progressing at least one BP category compared with baseline or by a new diagnosis of hypertension during follow-up. Hypertension was defined as SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg and/or use of antihypertensive medication within the past two weeks.
Statistical Analysis
Baseline characteristics were described as mean ± SD for continuous variables or percentages for categorical variables. We constructed logistic regression models to examine the relationship between tea consumption and BP progression. Cox proportional hazards models were fitted to assess these relationships for incident hypertension. Person-years of follow-up were calculated from the date of baseline survey until the date of first hypertension diagnosis, or initial use of antihypertensive medication, or the date of last follow-up. Two separate models were constructed for these analyses: model 1 was adjusted for age, gender, BMI, region (north/south), and baseline SBP; model 2 was additionally adjusted for smoking (yes or no), drinking (yes or no), physical activity (ideal or not), education level (≥ 12 years or not), fasting blood glucose, total cholesterol, and family history of hypertension (yes or no). Trend tests were conducted by modeling the median of tea consumption amount of each category as a continuous variable. Dose-response relationships were assessed by restricted cubic spline analyses with 0 g/month consumption of tea leaves serving as the reference level. Nonlinear associations were checked firstly by using the likelihood ratio test. If tests for nonlinearity were significant, spline models were used to describe the overall association, otherwise, linear models were used.
Subgroup analyses by age, sex, BMI, and baseline BP levels were conducted, and an interaction term with tea consumption was tested to investigate the potential effect modification. Sensitivity analyses were conducted by excluding all participants suffering hypertension within the first year of follow-up. Data were analyzed using R software (version 3.6.0, R Foundation for Statistical Computing, Vienna, Austria) or SAS 9.4 (SAS Institute Inc, Cary, North Carolina, USA). All statistical tests were two-sided, with P-value < 0.05 considered statistically significant.
RESULTS
Table 1 presented the baseline characteristics of the study participants, overall and according to tea drinking frequency. At baseline, the mean age of participants was 49.2 years, 35.6% of participants were males and 22.1% of participants were smokers. Overall, 25.6% of all participants reported drank tea ≥ 3 times/week for at least six months. Habitual tea drinkers were more likely to be males, smokers, habitual alcohol drinkers and well-educated.
Table 1. Baseline characteristics of the study participants overall and according to tea drinking frequency.
| Characteristics | All participants
(n = 38,913) |
Non-habitual tea drinkers
(n = 28,933) |
Habitual tea drinkers
(n = 9,980)* |
| Data are presented as means ± SD or n (%). *Refers to someone who had drank tea ≥ 3 times/week for at least six months. | |||
| Age, yrs | 49.2 ± 12.3 | 49.6 ± 12.5 | 47.9 ± 11.8 |
| Male | 13,846 (35.6%) | 8,158 (28.2%) | 5,688 (57.0%) |
| Northern | 18,896 (48.6%) | 13,238 (45.8%) | 5,658 (56.7%) |
| Education ≥ 12 yrs | 4,049 (10.4%) | 2,772 (9.6%) | 1,277 (12.8%) |
| Smokers | 8,579 (22.1%) | 4,652 (16.1%) | 3,927 (39.5%) |
| Habitual alcohol drinkers | 5,798 (14.9%) | 3,204 (11.1%) | 2,594 (26.0%) |
| Physical active | 28,864 (74.2%) | 21,722 (75.1%) | 7,142 (71.6%) |
| Family history of hypertension | 9,680 (24.9%) | 6,883 (23.8%) | 2,797 (28.0%) |
| Body mass index, kg/m2 | 23.2 ± 3.3 | 23.1 ± 3.3 | 23.4 ± 3.3 |
| Systolic blood pressure, mmHg | 117.5 ± 11.3 | 117.0 ± 11.5 | 119.2 ± 10.9 |
| Diastolic blood pressure, mmHg | 73.3 ± 7.9 | 72.8 ± 8.0 | 74.9 ± 7.6 |
| Fasting blood glucose, mg/dL | 88.8 ± 24.8 | 88.7 ± 24.2 | 88.9 ± 26.4 |
| Total serum cholesterol, mg/dL | 167.2 ± 32.9 | 167.2 ± 33.1 | 167.3 ± 32.3 |
During a median follow-up of 5.9 years, 17,657 individuals had experienced progression to a higher BP stage and 5,935 individuals developed incident hypertension. The associations of tea consumption with BP progression were illustrated in Table 2. Habitual tea consumption was associated with a 17% decreased risk of BP progression [odds ratio (OR) = 0.83, 95% CI: 0.79−0.88] in the fully adjusted model. We also observed that monthly tea consumption amount was inversely associated with BP progression. Compared with non-habitual tea drinkers, those who consumed 50 g, 100 g, and ≥ 150 g tea leaves per month were associated with 10%, 13%, and 23% lower risk of BP progression (Ptrend < 0.001), respectively.
Table 2. Odds ratios for risk of blood pressure progression associated with tea consumption.
| Tea consumption | Total number | Number of cases | OR (95% CI)* | OR (95% CI)** |
| *Refers to ORs (95% CIs) were adjusted for age, sex, body mass index, region, and baseline systolic blood pressure. **Refers to ORs (95% CIs) were further adjusted for smoking, drinking, physical activity, education level, fasting blood glucose, total cholesterol, and family history of hypertension. ***Refers to someone who had drank tea ≥ 3 times/week for at least six months. CI: confidence interval; OR: odds ratio. | ||||
| Tea drinking frequency | ||||
| Non-habitual tea drinkers | 28,933 | 13,646 | Reference | Reference |
| Habitual tea drinkers*** | 9,980 | 4,011 | 0.84 (0.80–0.88) | 0.83 (0.79–0.88) |
| Tea consumption amount | ||||
| Non-habitual tea drinkers | 28,933 | 13,646 | Reference | Reference |
| 50 g/month | 2,208 | 952 | 0.92 (0.84–1.00) | 0.90 (0.82–0.99) |
| 100 g/month | 3,287 | 1,325 | 0.89 (0.82–0.96) | 0.87 (0.81–0.95) |
| ≥ 150 g/month | 4,485 | 1,734 | 0.76 (0.71–0.82) | 0.77 (0.72–0.83) |
| Ptrend | — | — | < 0.001 | < 0.001 |
Tea consumption also provided preventive effect against incident hypertension. Habitual tea consumption was associated with a 14% lower risk of incident hypertension [hazard ratio (HR) = 0.86, 95% CI: 0.80−0.91] (Table 3). Compared with non-habitual tea drinkers, the estimated HRs of incident hypertension were 0.95 (95% CI: 0.85−1.07) for those who consumed 50 g/month of tea leaves, 0.83 (95% CI: 0.75−0.92) for those who consumed 100 g/month, and 0.83 (95% CI: 0.76−0.91) for those who consumed ≥ 150 g/month.
Table 3. Hazard ratios for incident hypertension associated with tea consumption.
| Tea consumption | Total number | Person-years | Number of cases | Incidence rate
(per 1,000 person-years) |
HR (95% CI)* | HR (95% CI)** |
| *Refers to HRs (95% CIs) were adjusted for age, sex, body mass index, region, and baseline systolic blood pressure. **Refers to HRs (95% CIs) were further adjusted for smoking, drinking, physical activity, education level, fasting blood glucose, total cholesterol, and family history of hypertension. ***Refers to someone who had drank tea ≥ 3 times/week for at least six months. CI: confidence interval; HR: hazard ratio. | ||||||
| Tea drinking frequency | ||||||
| Non-habitual tea drinkers | 28,933 | 163,254 | 4,491 | 27.5 | Reference | Reference |
| Habitual tea drinkers*** | 9,980 | 54,078 | 1,444 | 26.7 | 0.89 (0.84–0.95) | 0.86 (0.80–0.91) |
| Tea consumption amount | ||||||
| Non-habitual tea drinkers | 28,933 | 163,254 | 4,491 | 27.5 | Reference | Reference |
| 50 g/month | 2,208 | 12,372 | 326 | 26.3 | 0.96 (0.86–1.08) | 0.95 (0.85–1.07) |
| 100 g/month | 3,287 | 18,005 | 459 | 25.5 | 0.86 (0.78–0.94) | 0.83 (0.75–0.92) |
| ≥ 150 g/month | 4,485 | 23,699 | 659 | 27.8 | 0.88 (0.81–0.96) | 0.83 (0.76–0.91) |
| Ptrend | — | — | — | — | < 0.001 | < 0.001 |
We further plotted the dose-response curves for BP progression and hypertension incidence associated with monthly tea consumption amount. There was an inverse, and almost linear association between tea consumption amount and BP progression (Pnonlinear = 0.438), whereas the decreasing risk for incident hypertension reached a flattening after consuming approximately 100 g/month of tea leaves (Pnonlinear = 0.002) (Figure 2).
Figure 2.
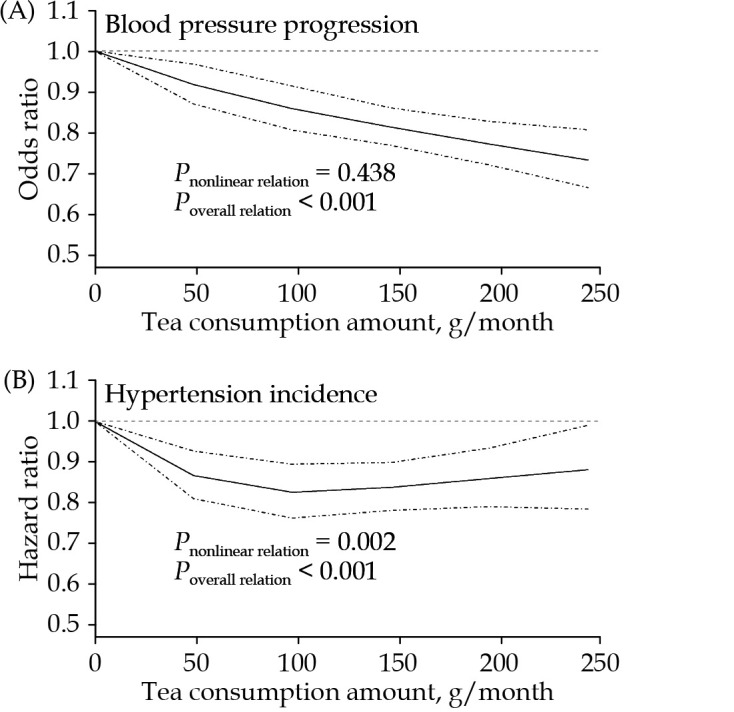
Dose-response relations of monthly tea leaves consumption with blood pressure progression and hypertension incidence.
Odds ratios of blood pressure progression (A) and hazard ratios of incident hypertension (B) were estimated using a restrict cubic spline function by comparing to a reference value of 0 g/month. Solid line represents point estimate and dashed lines represent 95% confidence intervals.
The relationships of habitual tea consumption with BP progression and incident hypertension remained stable after excluding those with incident hypertension occurring within the first year of follow-up (Tables 4 & 5). Analyses stratified by age, baseline BMI, and BP levels revealed similar effects of habitual tea consumption on BP progression and incident hypertension. We observed potential effect modifications by sex related to tea consumption, which presented a more pronounced association for BP progression among males and a stronger association for hypertension incidence among females (Table 6).
Table 4. Associations of tea consumption with blood pressure progression after excluding hypertension cases within the first year of follow-up.
| Tea consumption | Total number | Number of cases | OR (95% CI)* | OR (95% CI)** |
| *Refers to ORs (95% CIs) were adjusted for age, sex, body mass index, region, and baseline systolic blood pressure. **Refers to ORs (95% CIs) were further adjusted for smoking, drinking, physical activity, education level, fasting blood glucose, total cholesterol, and family history of hypertension. ***Refers to someone who had drank tea ≥ 3 times/week for at least six months. CI: confidence interval; OR: odds ratio. | ||||
| Tea drinking frequency | ||||
| Non-habitual tea drinkers | 28,799 | 13,512 | Reference | Reference |
| Habitual tea drinkers*** | 9,931 | 3,962 | 0.84 (0.79–0.88) | 0.83 (0.79–0.88) |
| Tea consumption amount | ||||
| Non-habitual tea drinkers | 28,799 | 13,512 | Reference | Reference |
| 50 g/month | 2,199 | 943 | 0.92 (0.84–1.00) | 0.90 (0.82–0.99) |
| 100 g/month | 3,267 | 1,305 | 0.88 (0.82–0.95) | 0.87 (0.80–0.94) |
| ≥ 150 g/month | 4,465 | 1,714 | 0.76 (0.71–0.82) | 0.77 (0.72–0.83) |
| Ptrend | — | — | < 0.001 | < 0.001 |
Table 5. Associations of tea consumption with incident hypertension after excluding hypertension cases within the first year of follow-up.
| Tea consumption | Total number | Person-years | Number of cases | Incidence rate
(per 1,000 person-years) |
HR (95% CI)* | HR (95% CI)** |
| *Refers to HRs (95% CIs) were adjusted for age, sex, body mass index, region, and baseline systolic blood pressure. **Refers to HRs (95% CIs) were further adjusted for smoking, drinking, physical activity, education level, fasting blood glucose, total cholesterol, and family history of hypertension. ***Refers to someone who had drank tea ≥ 3 times/week for at least six months. CI: confidence interval; HR: hazard ratio. | ||||||
| Tea drinking frequency | ||||||
| Non-habitual tea drinkers | 28,799 | 163,186 | 4,357 | 26.7 | Reference | Reference |
| Habitual tea drinkers*** | 9,931 | 54,056 | 1,395 | 25.8 | 0.89 (0.83–0.94) | 0.85 (0.80–0.91) |
| Tea consumption amount | ||||||
| Non-habitual tea drinkers | 28,799 | 163,186 | 4,357 | 26.7 | Reference | Reference |
| 50 g/month | 2,199 | 12,369 | 317 | 25.6 | 0.96 (0.86–1.08) | 0.95 (0.85–1.07) |
| 100 g/month | 3,267 | 17,996 | 439 | 24.4 | 0.84 (0.76–0.93) | 0.82 (0.74–0.90) |
| ≥ 150 g/month | 4,465 | 23,691 | 639 | 27.0 | 0.88 (0.81–0.96) | 0.83 (0.76–0.91) |
| Ptrend | — | — | — | — | < 0.001 | < 0.001 |
Table 6. Subgroup analyses for blood pressure progression and incident hypertension associated with habitual tea drinking by specific characteristics.
| Subgroup | Blood pressure progression | Hypertension incidence | |||||
| Number of
cases/Total number |
OR
(95% CI)* |
Pinteraction-value | Number of
cases/Total number |
HR
(95% CI)** |
Pinteraction-value | ||
| *Refers to ORs were derived from multivariable logistic regression analysis adjusting for age, sex, body mass index, baseline systolic blood pressure, region, smoking, drinking, physical activity, education level, fasting blood glucose, total cholesterol, and family history of hypertension. **Refers to HRs were derived from multivariable Cox regression analysis adjusting for age, sex, body mass index, baseline systolic blood pressure, region, smoking, drinking, physical activity, education level, fasting blood glucose, total cholesterol, and family history of hypertension. CI: confidence interval; HR: hazard ratio; OR: odds ratio. | |||||||
| Age, yrs | 0.053 | 0.312 | |||||
| < 50 | 7,536/19,605 | 0.85 (0.79−0.91) | 2,092/19,605 | 0.88 (0.80−0.97) | |||
| 50–60 | 5,583/11,403 | 0.82 (0.74−0.90) | 1,955/11,403 | 0.87 (0.77−0.97) | |||
| ≥ 60 | 4,538/7,905 | 0.87 (0.77−0.98) | 1,888/7,905 | 0.83 (0.73−0.94) | |||
| Sex | 0.004 | 0.001 | |||||
| Male | 6,317/13,846 | 0.77 (0.71−0.83) | 2,308/13,846 | 0.96 (0.88−1.05) | |||
| Female | 11,340/25,067 | 0.90 (0.84−0.97) | 3,627/25,067 | 0.76 (0.69−0.84) | |||
| Body mass index, kg/m2 | 0.102 | 0.437 | |||||
| < 24 | 10,864/24,377 | 0.86 (0.81−0.92) | 3,177/24,377 | 0.88 (0.81−0.96) | |||
| ≥ 24 | 6,793/14,536 | 0.81 (0.74−0.88) | 2,758/14,536 | 0.84 (0.77−0.92) | |||
| Baseline blood pressure, mmHg | 0.943 | 0.560 | |||||
| < 120/75 | 9,396/17,027 | 0.87 (0.80−0.94) | 1,092/17,027 | 0.90 (0.76−1.06) | |||
| 120−129/75−84 | 5,744/14,119 | 0.86 (0.79−0.94) | 2,326/14,119 | 0.80 (0.72−0.89) | |||
| 130–139/85–89 | 2,517/7,767 | 0.84 (0.74−0.94) | 2,517/7,767 | 0.89 (0.81−0.98) | |||
DISCUSSION
In this large prospective cohort study of 38,913 participants in China, we found that habitual tea drinkers had 17% and 14% lower risk of BP progression and hypertension incidence, compared with non-habitual tea drinkers. The health benefits of habitual tea consumption on BP progression and hypertension were similar across different baseline BP categories. There was a progressive reduction in risk of BP progression associated with higher amount of monthly tea consumption. The current study suggests that tea might be a healthy beverage for primary prevention against BP progression and hypertension.
The available epidemiologic evidence on tea intake related to hypertension is inconclusive. Several cross-sectional studies have assessed the relationship between tea consumption, BP, and hypertension. For example, the Observation of Cardiovascular Risk Factors study in Luxembourg (ORISCAV-LUX) with 1,352 individuals showed daily consumption of 1 dL of tea was associated with a significant reduction of SBP by 0.6 mmHg and pulse pressure by 0.5 mmHg.[10] Another cross-sectional study observed that habitual green or oolong tea consumption (120 mL/day or more) for at least one year was associated with decreased risk of hypertension prevalence in a population of 1,507 subjects in Taiwan, China.[9] Additionally, one study conducted in Jiangsu, China with 4,579 older adults also found that habitual tea drinking was inversely associated with SBP values and prevalence of hypertension.[11] Although many of these studies report a significant inverse association of tea with BP or hypertension, evidences from prospective cohort studies remain scarce. A cohort study of 1,878 Iran adult with six-year follow-up observed no significant association between tea intake and the risk of hypertension.[13] The Singapore Chinese Health Study with 9.5 years of follow-up among 38,592 participants found that daily consumption of black tea or green tea might cause higher risk of hypertension, and this association was attenuated and became non-significant after adjusting for caffeine intake.[12] This study used the number of cups of tea as the measure of exposure and self-reported hypertension as the measure of outcome, which may lead to misclassifications due to the high unawareness rate of hypertension in Singapore (43.1%).[17] In contrast, our study provided substantial evidence about health benefits of tea consumption on both BP progression and hypertension incidence through standardized clinical measurements of BP.
In the current prospective cohort study with a duration of 5.9-year follow-up in China, we observed that habitual tea consumption was associated with a reduced risk of both BP progression and hypertension. It was notable that individuals with prehypertension could obtain the similar benefits as those with ideal BP. Several prior cohort studies supported the protective effects of tea consumption on cardiometabolic diseases. Our recent study showed that habitual tea drinkers had 20%, 22%, and 15% lower risk of CVD incidence, CVD mortality, and all-cause mortality, respectively, compared with non-habitual tea drinkers.[4] The Dongfeng-Tongji cohort study found that green tea consumption could reduce the risk of coronary heart disease incidence (HR = 0.89, 95% CI: 0.81−0.98) and improve blood lipid and uric acid levels.[18] A meta-analysis of nine cohort studies revealed that tea consumption ≥ 4 cups per day (relative risk = 0.80, 95% CI: 0.70−0.93) might play a role in the prevention of type 2 diabetes mellitus.[19] Besides habitual tea drinking frequency these studies focused on, we further examined the linear dose-response relation between tea consumption amount and BP progression. We found that individuals who consumed ≥ 50 g tea leaves per month could achieve benefit for both BP progression and hypertension incidence, whereas the risk of incident hypertension did not reduce further after around 100 g/month of tea consumption. The threshold of monthly tea consumption amount benefitting cardiovascular health was similar to that in the China Kadoorie Biobank, which demonstrated that daily consumption of ≥ 2 g tea (being equivalent to 60 g/month) could reduce the risk of stroke incidence.[20] Further studies in large prospective cohorts are needed to confirm the dose-response relation.
The findings that tea consumption was associated with lower risk of BP progression and incident hypertension are biologically reasonable. Tea contains a variety of antioxidants and other chemicals (flavonoids, theaflavins, thearubigins, and polyphenols, etc.) that have endothelial protection and anti-inflammatory effects.[21] Tea flavonoids can act as modulators of enzymes involved in oxidative and inflammatory stress, enhance nitric oxide status, and improve endothelial function, which may contribute to potential benefits on cardiovascular health.[22] During last decades, in vitro and animal studies indicated that potentially beneficial effects of tea polyphenols mainly due to its antioxidant properties and bioactivity on scavenging free radicals, promoting lipid metabolism and maintaining stability of vascular endothelium.[23–26] There were also some randomized controlled trials in humans which observed an inverse association between tea and BP. A meta-analysis of twenty-one randomized trials showed that after long-term tea intake (≥ 1 week), the pooled mean SBP and DBP were lower by 1.8 mmHg (95% CI: 1.1−2.4) and 1.4 mmHg (95% CI: 0.6−2.2), respectively.[27]
STRENGTHS AND LIMITATION
To our knowledge, this is the first longitudinal study to evaluate the effects of tea consumption on the risk of BP progression and hypertension incidence in China. The strengths of our study included the prospective study design, large sample size, and the collection of a broad range of covariates at individual level. Furthermore, we also measured tea consumption in grams of dry tea leaves which may better reflect the actual ingested tea components. In addition, we assessed outcome by standardized clinical measurements of BP, which could be more precise than self-reported hypertension. Several limitations of the current study should also be noted. On the one hand, since information on tea consumption and the covariates, such as physical activity, were self-reported, inevitable recall bias might result in misclassification. However, possible measurement errors would have most likely been non-differential and biased the results towards the null. On the other hand, tea drinking habit may change over time and lead to underestimation of the true association.
CONCLUSIONS
In conclusion, habitual tea consumption could reduce the risk for both BP progression and hypertension in China. These results gave us a further insight into the role of tea consumption in cardiovascular health and indicated that tea might be a healthy beverage worth of popularizing.
ACKNOWLEDGMENTS
This study was supported by the National Nature Science Foundation of China (No.91643208), the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2017-I2M-1-004 & 2019-I2M-2-003), and the National Key Research & Development Program of China (2017YFC0211700 & 2018YFE0115300). All authors had no conflicts of interest to disclose.
References
- 1.Wang Z, Chen Z, Zhang L, et al Status of hypertension in China: results from the China Hypertension Survey, 2012–2015. Circulation. 2018;137:2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 2.GBD 2019 Risk Factors Collaborators Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kearney PM, Whelton M, Reynolds K, et al Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 4.Wang X, Liu F, Li J, et al Tea consumption and the risk of atherosclerotic cardiovascular disease and all-cause mortality: the China-PAR project. Eur J Prev Cardiol. 2020;27:1956–1963. doi: 10.1177/2047487319894685. [DOI] [PubMed] [Google Scholar]
- 5.Liu X, Xu W, Cai H, et al Green tea consumption and risk of type 2 diabetes in Chinese adults: the Shanghai Women’s Health Study and the Shanghai Men’s Health Study. Int J Epidemiol. 2018;47:1887–1896. doi: 10.1093/ije/dyy173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li X, Yu C, Guo Y, et al Association between tea consumption and risk of cancer: a prospective cohort study of 0.5 million Chinese adults. Eur J Epidemiol. 2019;34:753–763. doi: 10.1007/s10654-019-00530-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li X, Yu C, Guo Y, et al Tea consumption and risk of ischaemic heart disease. Heart. 2017;103:783–789. doi: 10.1136/heartjnl-2016-310462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang C, Qin YY, Wei X, et al Tea consumption and risk of cardiovascular outcomes and total mortality: a systematic review and meta-analysis of prospective observational studies. Eur J Epidemiol. 2015;30:103–113. doi: 10.1007/s10654-014-9960-x. [DOI] [PubMed] [Google Scholar]
- 9.Yang YC, Lu FH, Wu JS, et al The protective effect of habitual tea consumption on hypertension. Arch Intern Med. 2004;164:1534–1540. doi: 10.1001/archinte.164.14.1534. [DOI] [PubMed] [Google Scholar]
- 10.Alkerwi A, Sauvageot N, Crichton GE, et al Tea, but not coffee consumption, is associated with components of arterial pressure. The Observation of Cardiovascular Risk Factors study in Luxembourg. Nutr Res. 2015;35:557–565. doi: 10.1016/j.nutres.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Yin JY, Duan SY, Liu FC, et al Blood pressure is associated with tea consumption: a cross-sectional study in a rural, elderly population of Jiangsu China. J Nutr Health Aging. 2017;21:1151–1159. doi: 10.1007/s12603-016-0829-4. [DOI] [PubMed] [Google Scholar]
- 12.Chei CL, Loh JK, Soh A, et al Coffee, tea, caffeine, and risk of hypertension: the Singapore Chinese Health Study. Eur J Nutr. 2018;57:1333–1342. doi: 10.1007/s00394-017-1412-4. [DOI] [PubMed] [Google Scholar]
- 13.Gaeini Z, Bahadoran Z, Mirmiran P, et al Tea, coffee, caffeine intake and the risk of cardio-metabolic outcomes: findings from a population with low coffee and high tea consumption. Nutr Metab (Lond) 2019;16:28. doi: 10.1186/s12986-019-0355-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang X, Li J, Hu D, et al Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: the China-PAR project (Prediction for ASCVD Risk in China) Circulation. 2016;134:1430–1440. doi: 10.1161/CIRCULATIONAHA.116.022367. [DOI] [PubMed] [Google Scholar]
- 15.Perloff D, Grim C, Flack J, et al Human blood pressure determination by sphygmomanometry. Circulation. 1993;88:2460–2470. doi: 10.1161/01.CIR.88.5.2460. [DOI] [PubMed] [Google Scholar]
- 16.Conen D, Glynn RJ, Ridker PM, et al Socioeconomic status, blood pressure progression, and incident hypertension in a prospective cohort of female health professionals. Eur Heart J. 2009;30:1378–1384. doi: 10.1093/eurheartj/ehp072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Man REK, Gan AHW, Fenwick EK, et al Prevalence, determinants and association of unawareness of diabetes, hypertension and hypercholesterolemia with poor disease control in a multi-ethnic Asian population without cardiovascular disease. Popul Health Metr. 2019;17:17. doi: 10.1186/s12963-019-0197-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tian C, Huang Q, Yang L, et al Green tea consumption is associated with reduced incident CHD and improved CHD-related biomarkers in the Dongfeng-Tongji cohort. Sci Rep. 2016;6:24353. doi: 10.1038/srep24353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jing Y, Han G, Hu Y, et al Tea consumption and risk of type 2 diabetes: a meta-analysis of cohort studies. J Gen Intern Med. 2009;24:557–562. doi: 10.1007/s11606-009-0929-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tian T, Lv J, Jin G, et al Tea consumption and risk of stroke in Chinese adults: a prospective cohort study of 0.5 million men and women. Am J Clin Nutr. 2020;111:197–206. doi: 10.1093/ajcn/nqz274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Balentine DA, Wiseman SA, Bouwens LC The chemistry of tea flavonoids. Crit Rev Food Sci Nutr. 1997;37:693–704. doi: 10.1080/10408399709527797. [DOI] [PubMed] [Google Scholar]
- 22.Grassi D, Desideri G, Di Giosia P, et al Tea, flavonoids, and cardiovascular health: endothelial protection. Am J Clin Nutr. 2013;98:1660S–1666S. doi: 10.3945/ajcn.113.058313. [DOI] [PubMed] [Google Scholar]
- 23.Ihm SH, Jang SW, Kim OR, et al Decaffeinated green tea extract improves hypertension and insulin resistance in a rat model of metabolic syndrome. Atherosclerosis. 2012;224:377–383. doi: 10.1016/j.atherosclerosis.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 24.Chyu KY, Babbidge SM, Zhao X, et al Differential effects of green tea-derived catechin on developing versus established atherosclerosis in apolipoprotein E-null mice. Circulation. 2004;109:2448–2453. doi: 10.1161/01.CIR.0000128034.70732.C2. [DOI] [PubMed] [Google Scholar]
- 25.Negishi H, Xu JW, Ikeda K, et al Black and green tea polyphenols attenuate blood pressure increases in stroke-prone spontaneously hypertensive rats. J Nutr. 2004;134:38–42. doi: 10.1093/jn/134.1.38. [DOI] [PubMed] [Google Scholar]
- 26.Li D, Wang R, Huang J, et al Effects and mechanisms of tea regulating blood pressure: evidences and promises. Nutrients. 2019;11:1115. doi: 10.3390/nu11051115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu G, Mi XN, Zheng XX, et al Effects of tea intake on blood pressure: a meta-analysis of randomised controlled trials. Br J Nutr. 2014;112:1043–1054. doi: 10.1017/S0007114514001731. [DOI] [PubMed] [Google Scholar]