Abstract
Although neighborhood environmental factors have been found to be associated with cognitive decline, few longitudinal studies have focused on their effect on older adults living in rural areas. This longitudinal study aimed to investigate the role of neighborhood environmental factors in cognitive decline among rural older adults. The data of 485 older adults aged ≥60 years who were living in Unnan City in Japan and had participated in two surveys conducted between 2014 and 2018 were analyzed. Cognitive function was assessed using the Cognitive Assessment for Dementia, iPad version 2. Elevation, hilliness, residential density, and proximity to a community center were determined using geographic information system. We applied a generalized estimating equation with odds ratios (OR) and 95% confidence intervals (CIs) of cognitive decline in the quartiles of neighborhood environmental factors. A total of 56 (11.6%) participants demonstrated a decrease in cognitive function at follow up. Elevation (adjusted OR 2.58, 95% CI (1.39, 4.77) for Q4 vs. Q1) and hilliness (adjusted OR 1.93, 95% CI (1.03, 3.63) for Q4 vs. Q1) were associated with a higher likelihood of cognitive decline. The second quartiles of residential density showed significantly lower likelihoods of cognitive decline compared with the first quartiles (adjusted OR 0.36, 95% CI (0.19, 0.71) for Q2 vs. Q1). Thus, an elevated hilly environment and residential density predicted cognitive decline among rural older adults.
Keywords: cognitive function, rural mountainous area, older adults
1. Introduction
Dementia is a significant public health issue in aging societies worldwide. Not only does it disrupt the lives of affected individuals and their caregivers and families, but it also imposes a significant economic burden on society [1]. Dementia affects approximately 50 million people worldwide, and this number is expected to rise to 82 million by 2030 [2].
Previous reviews have focused on the relationship between cognitive decline and personal factors such as lifestyle and health status [3,4]. In addition, air pollution, occupational exposure, and stress have been reported as physical environmental factors relevant to cognitive function [3]. Therefore, to intervene in high-risk communities for primary prevention, it is important to understand the environmental factors that predict cognitive decline.
In recent years, studies have examined the relationship between neighborhood environmental factors and health-related outcomes using a geographic information system (GIS), which has proven useful in the field of public health [5,6]. As a result, it has become clear that social cohesion, the neighborhood sidewalk environment, and proximity to nearby facilities affect cognitive function [7,8,9]. Several cross-sectional studies have also examined the relationship between various physical environmental factors and cognitive function [10,11,12]. However, there has been insufficient research on how physical environmental factors, which are unique to rural areas, affect long-term cognitive decline.
In this study, we examined the factors that contribute to cognitive decline among older adults, with the aim of developing effective measures against its progression. We focused on physical environmental factors in a rural area in Japan with a substantial aging population.
2. Materials and Methods
2.1. Design, Setting, and Sample
This longitudinal four-year follow-up study was conducted using data collected as part of the Shimane CoHRE Study in Shimane Prefecture. It targeted lifestyle-related diseases through the collection of data concerning medical history, lifestyle, and cognitive function during annual municipal health examinations [13,14,15,16].
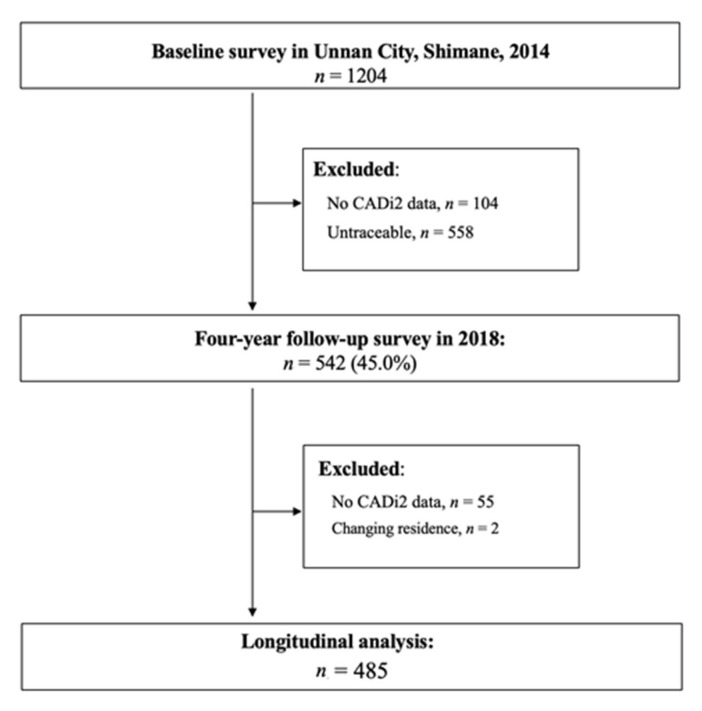
The research team collected longitudinal data between August and October in 2014 and in 2018, in collaboration with the annual health examination program that involved the population of Unnan City, Shimane Prefecture, Japan. Annual health examinations are available once a year for residents in this municipality who are covered by the National Health Insurance. We provided information regarding this study at least once to potential participants through a document prior to conducting the health examinations. The participants were older adults aged 60 years and above who were residing in Unnan City, which has an aging population of more than 35%. The study included those who had participated in both the baseline survey in 2014 and the follow-up survey in 2018. After excluding those with missing data (n = 55) and those who did not reside at the same address as in 2014 (n = 2), the total sample size was 485 (218 males and 267 females) (Figure 1).
Figure 1.
Flowchart of the study. CADi2: Cognitive Assessment for Dementia, iPad version 2.
2.2. Outcome Variable
The research team assessed cognitive function using the Cognitive Assessment for Dementia, iPad version 2 (CADi2), which has been evaluated for validity and reliability [17]. The CADi2 consists of 10 items: immediate recognition, long-term memory, digits backward, orientation (month), orientation (day of the week), calculation, cube rotation, sequence making A, sequence making B, and delayed recognition. Scores ranged from 0 to 10, with higher scores indicating better cognitive function. Cognitive decline was defined using a cutoff score (<7 points) determined based on past findings; accordingly, the scores were divided into two categories. The participants used an iPad (https://apps.apple.com/jp/app/cadi2/id808586504 (accessed on 5 July 2021); currently available only in Japanese) to answer questions during an audio presentation. CADi2 data from 2014 and 2018 were used.
2.3. Exposure Variables
Using a GIS, we measured elevation, hilliness, residential density, and proximity to the nearest community center. We calculated hilliness and residential density within a network buffer of 1000 m from each participant’s residential address based on the actual road network [18]. Elevation was measured when the residential point fell within the 5th mesh polygon data where mean elevation value is assigned, based on the data administered and published by the Geospatial Information Authority of Japan under the Ministry of Land, Infrastructure, Transport, and Tourism. Hilliness for each individual’s network buffer was measured based on the mean land slope degree in angular units using the 5th mesh data that intersected with the network buffers. We calculated the residential density by aggregating the number of households stored by the minimum census unit as point data within the network buffer. We measured proximity to the community center based on the road network from each residential point to the nearest community center. In Japan, a community center is a public facility that can be freely used by local groups and to hold regular meetings. We categorized each calculated value into four groups using quartiles and analyzed its effect on the change in cognitive function. We conducted all spatial analyses using ArcGIS Pro.2.0 (Esri Japan). We used the most recent data available, as of 2009 for elevation and hilliness, as of 2010 for residential density, and as of 2016 for proximity to the nearest community center.
2.4. Covariates
Using questionnaires and empirical measurements, we recorded the following covariates: sex (male or female), age (in years), body mass index (BMI; measured height and weight data in kg/m2), hypertension (categorized as hypertension if any of the following conditions were met: medication for hypertension, systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg), and depression (categorized using a cutoff score of ≥40 on the Zung Self-Rating Depression Scale) [19]. We used data of these covariates collected in 2014.
2.5. Statistical Analysis
We calculated descriptive statistics for all the variables for each cognitive function group (normal, declining) and examined group differences using the χ2 test for categorical variables.
Further, we used a generalized estimating equation with an unadjusted model (Model 1) and a model adjusted for sex, age, BMI, hypertension, depressive symptoms, and cognitive function at baseline as potential confounders (Model 2), while environmental variables were grouped by quartiles (reference group: Q1). We examined the correlations among the environmental variables and multicollinearity before applying the generalized estimating equation. Subsequently, we observed multicollinearity between each environmental variable (r ≥ 0.32, p < 0.001); therefore, all the environmental factors were independently included in the model for analysis.
We conducted statistical analysis using SPSS version 26.0 for Windows (IBM Corp., Armonk, NY, USA); p-values less than 0.05 were considered statistically significant.
2.6. Ethical Considerations
Data were collected after obtaining written informed consent from all participants prior to enrollment. The study received approval from the Ethics Committee of Shimane University School of Medicine (#20180420-2) and the Ethical Review Committee of the Shimane Rehabilitation Institute (#73).
3. Results
Table 1 presents the characteristics of the participants. There were 485 participants in this study (44.9% males and 55.1% females). Their median (interquartile range; IQR) age was 70.0 (66.0–75.0) years. Their median (IQR) BMI was 21.6 (19.9–23.8) kg/m2. Of all the participants, 55 (11.3%) had cognitive decline at baseline, 240 (49.5%) met the criteria for hypertension, and 91 (18.8%) had depression. As of 2018, the number of participants who demonstrated cognitive decline was 56 (11.5%).
Table 1.
Participant characteristics at baseline.
| Variables | Total | Cognitive Function at Follow-Up a | p | |
|---|---|---|---|---|
| Low | High | |||
| n(%) | 485 | 56 (11.5) | 429(88.5) | |
| Sex | ||||
| Males | 218 (44.9) | 37 (66.1) | 181 (42.2) | 0.001 |
| Females | 267 (55.1) | 19 (33.9) | 248 (57.8) | |
| Age, years, median (IQR) | 70.0 (66.0–75.0) | 74.0 (70.0–78.0) | 70.0 (66.0–74.0) | <0.001 |
| Body mass index, kg/m2, median (IQR) | 21.6 (19.9–23.8) | 21.2 (19.9–22.8) | 21.7 (19.9–23.9) | 0.168 |
| Cognitive function at baseline a | ||||
| High | 430 (88.7) | 40 (71.4) | 390 (90.9) | < 0.001 |
| Low | 55 (11.3) | 16 (28.6) | 39 (9.1) | |
| Hypertension b | ||||
| No | 245 (50.5) | 21 (37.5) | 224 (52.2) | 0.038 |
| Yes | 240 (49.5) | 35 (62.5) | 205 (47.8) | |
| Depressive symptoms c | ||||
| No | 394 (81.2) | 46 (82.1) | 348 (81.1) | 0.854 |
| Yes | 91 (18.8) | 10 (17.9) | 81 (18.9) | |
a Cognitive function was assessed using the Cognitive Assessment for Dementia, iPad version 2 and defined using a cutoff score of <7 points. b Hypertension was defined as follows: taking antihypertensive medication or systolic/diastolic blood pressure ≥140/90 mm Hg. c Depressive symptoms were assessed using the Zung Self-Rating Depression Scale and defined using a cutoff score of ≥40 points. IQR: interquartile range.
Table 2 presents the results of the generalized estimating equation of cognitive function. In Model 2 (adjusted model), which shows the relationship between elevation and cognitive decline, there was no significant increase in cognitive decline from the first to the third quartile, but there was a significant increase in the fourth quartile (adjusted odds ratio (OR) 2.58, 95% confidence interval (CI) (1.39, 4.77)). With regard to hilliness, although there was no significant increase in cognitive decline in the second and third quartiles, it increased significantly in the fourth quartile in relation to the first quartile (adjusted OR 1.93, 95% CI (1.03, 3.63)). In terms of residential density, there was a significant decrease in the second quartile (adjusted OR 0.36, 95% CI (0.19, 0.71)). In terms of distance to the community center, there was no significant increase in cognitive decline from the second to the fourth quartile.
Table 2.
Longitudinal associations between environmental factors and cognitive decline among older adults in rural areas.
| Environmental Factors | Case/n (%) | Model 1 a | Model 2 b | ||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | ||||
| Elevation | Low | Q1 | 6/121 (5.0) | 1.00 | (reference) | 1.00 | (reference) |
| Q2 | 9/124 (7.3) | 1.35 | (0.68, 2.69) | 1.31 | (0.67, 2.56) | ||
| Q3 | 15/119 (12.6) | 1.69 | (0.88, 3.28) | 1.42 | (0.73, 2.75) | ||
| High | Q4 | 26/121 (21.5) | 2.94 | (1.57, 5.50) | 2.58 | (1.39, 4.77) | |
| Hilliness | Low | Q1 | 9/121 (7.4) | 1.00 | (reference) | 1.00 | (reference) |
| Q2 | 10/122 (8.2) | 1.10 | (0.57, 2.11) | 1.32 | (0.69, 2.54) | ||
| Q3 | 10/121 (8.3) | 1.21 | (0.62, 2.36) | 1.48 | (0.76, 2.87) | ||
| High | Q4 | 27/121 (22.3) | 2.21 | (1.19, 4.12) | 1.93 | (1.03, 3.63) | |
| Residential density | Low | Q1 | 25/119 (21.0) | 1.00 | (reference) | 1.00 | (reference) |
| Q2 | 6/123 (4.9) | 0.30 | (0.16, 0.57) | 0.36 | (0.19, 0.71) | ||
| Q3 | 13/122 (10.7) | 0.65 | (0.37, 1.15) | 0.65 | (0.37, 1.15) | ||
| High | Q4 | 12/121 (9.9) | 0.51 | (0.28, 0.93) | 0.55 | (0.30, 1.04) | |
| Distance to community center | Near | Q1 | 16/121 (13.2) | 1.00 | (reference) | 1.00 | (reference) |
| Q2 | 10/122 (8.2) | 0.83 | (0.44, 1.58) | 0.86 | (0.45, 1.64) | ||
| Q3 | 9/121 (7.4) | 0.80 | (0.43, 1.47) | 0.93 | (0.51, 1.71) | ||
| Far | Q4 | 21/121 (17.4) | 1.53 | (0.86, 2.72) | 1.72 | (0.96, 3.08) | |
a Model 1: Crude model. b Model 2: Adjustments were made for sex, age, body mass index, hypertension, and depressive symptoms. Each environmental factor based on network buffer was analyzed separately. OR: odds ratio; CI: confidence interval.
4. Discussion
In this study, we aimed to examine the effects of neighborhood environmental factors on cognitive health in order to help develop preventive strategies against cognitive decline among older adults in the community. This is the longitudinal study to focus on the hilly nature of neighborhood environmental factors that influence cognitive decline among older adults in rural Japan. The results indicate that neighborhood environment has an effect on cognitive decline. In particular, the risk of cognitive decline was higher in more hilly environments (increased elevation and hilliness). This finding is consistent with the results of a cross-sectional study conducted by Hamano et al. in a similar area [20]. It also supports the results of a longitudinal study of land slope and cognitive function by Tani et al. [9]. Moreover, we found that the second quartiles of residential density were associated with significantly lower likelihoods of cognitive decline compared with the first quartile. High residential density positively affected cognitive health; this finding is slightly different from the results of the cross-sectional study conducted by Ng et al. [11]. In that study, higher residential density tended to be associated with a lower likelihood of cognitive decline, although the results were not statistically significant.
Several studies have investigated the relationship between cognitive function and neighborhood environment. However, most of them were cross-sectional and did not yield sufficient evidence because of the complexity of regional characteristics [21]. Our longitudinal study found the hilly nature of neighborhood environmental factors that influence cognitive decline among older adults in rural Japan. In the study by Tanaka et al., older women living in the sloped area engaged in less physical activity and had more depressive symptoms compared with their counterparts in the flat area [22]. It is possible that these personal factors cause cognitive decline in the long term [4]. Thus, the hilly environment may be one of the barriers to engagement in daily physical activity in older adults. In addition, plains tend to have a low elevation and be more densely populated because of their proximity to various living centers. Thus, we can deduce that the accessibility and availability of living centers, where people can interact with others, are more strongly related to the results as secondary psychosocial influences than the hilly environment and housing density themselves. Indeed, our study found a negative relationship between residential density and cognitive decline. Several studies have demonstrated support for the relationship between the accessibility and availability of living centers and cognitive function. A one-year follow-up study conducted in Japan found that the availability of grocery stores reduced cognitive decline [23]. In Hong Kong, a large cross-sectional study reported that library availability reduced cognitive decline [24]. Reinforcing these findings, a recent study showed that the condition of roads that affect access to living centers also affects the development of dementia [9]. In addition, populated areas may have higher social engagement than less populated areas. According to a systematic review of the literature on community and cognitive functioning, 11 out of 15 studies reported significant correlations between community engagement and various measures of cognitive functioning [21]. It has also been shown that social capital and availability of community resources have a positive impact on cognitive function [25,26]. Complementing these findings, our results suggest that there is a negative association between poor accessibility and availability of community and leisure activity centers and cognitive decline among older adults.
We focused on community centers, which are the local hubs of activity in Japan. The distance from the home to the community center can be seen as a proxy variable for social environmental factors. When we examined the relationship between cognitive function and the distance between local residences and their respective community centers, we found that participants in the second and third quartiles tended to have a lower likelihood of cognitive decline, even though the results were not statistically significant. In Japan, people can participate in cultural and educational activities at the nearest community center. Hikichi et al. [27] found that participation in a community center prevented cognitive decline, while Iwasa et al. [28] found a longitudinal inverse association between participation in hobbies and cognitive decline among community-dwelling older adults. Hence, people who live near community centers may find it easier to participate in these activities than those who live far away. In addition, walking may have affected the accessibility of community centers, since the culture in Japan is to walk rather than drive to community centers when they are relatively close by. Several studies have shown a positive relationship between residential density and walking [29,30], and it is possible that the method of travel to the community center is involved in the relationship between residential density and cognitive function.
A few study limitations should be noted. First, some participants demonstrated improved cognitive function at follow-up. This may be attributable to preventive measures (improved diet, social interaction, etc.) taken by the participants after they were diagnosed with cognitive decline within the framework of the medical checkup. Alternatively, it may be because of the implementation of activities focused on dementia prevention in certain areas. Our study could not examine this dimension. Second, the sampling technique posed certain limitations. In contrast to past large-scale epidemiological studies, our longitudinal four-year study targeted older adults who live in mountainous regions by convenient sampling. These limit the generalization of this study within older adults who are relatively healthy enough to participate in health examinations and living in mountainous regions. Future studies need to collect larger samples from different regions by random sampling in order to improve practical and political implications. Third, we used GIS to examine the relationship between objective environmental factors and dementia, but we were not able to examine the effects of subjectively measured environmental factors (e.g., perceptions to unfavorable and disadvantaged neighborhood conditions), which have been examined in past studies [31,32]. In addition, all the environment variables were measured at one time point. Thus, we cannot discount the measurement bias related to possible longitudinal changes in neighborhood environments, such as local development, or changes in road conditions. There might have been maturation effect of repeated measurements of cognitive function (i.e., participants learn to respond on the cognitive test) as another measurement bias. Finally, we could not account for the influence of any unmeasured variables that could affect the relationship between environmental variables and cognitive decline, such as physical activity, nutritional status, educational attainment, and low-income population rate [33,34,35,36].
5. Conclusions
The findings of this longitudinal study suggest that elevated hilly environments increased the risk of cognitive decline among older adults in rural Japan. Moreover, residential density was negatively associated with cognitive decline. Hence, the geography surrounding residential spaces may influence cognitive function among older residents of rural areas.
Acknowledgments
We greatly appreciate the cooperation of the participants, and we thank the Shimane CoHRE study members for their skillful assistance.
Author Contributions
Conceptualization, A.M., K.O. (Kenta Okuyama) and T.A.; methodology, A.M., K.O. (Kenta Okuyama) and T.A.; formal analysis, A.M. and K.O. (Kenta Okuyama); investigation, M.I., K.O. (Keiichi Onoda), T.A. and K.O. (Kenta Okuyama); data curation, T.A. and K.O. (Kenta Okuyama); writing—original draft preparation, A.M., T.A. and K.O. (Kenta Okuyama); writing—review and editing, T.I., T.N. and S.K.; supervision, M.I., T.N. and S.K.; funding acquisition, T.I. and T.A. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the Japan Society for the Promotion of Science (KAKENHI Grant Number 19K02335).
Institutional Review Board Statement
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of Shimane University School of Medicine (#20180420-2) and the Ethical Review Committee of Shimane Rehabilitation Institute (#73).
Informed Consent Statement
Written informed consent was obtained from all participants.
Data Availability Statement
This study used data from the Shimane CoHRE study. Some data are available at the Center for Community-Based Healthcare Research and Education (CoHRE), Organization for Research and Academic Information, Shimane University, 223-8 Enya-cho, Izumo-shi, Shimane 693-8501, Japan.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Alzheimer’s Disease International. Dementia: A Public Health Priority. World Health Organization; Geneva, Switzerland: 2012. [(accessed on 18 March 2021)]. Available online: http://www.who.int/mental_health/publications/dementia_report_2012/en/13-15. [Google Scholar]
- 2.World Health Organization . Risk Reduction of Cognitive Decline and Dementia: WHO Guidelines. World Health Organization; Geneva, Switzerland: 2019. [(accessed on 18 March 2021)]. Available online: https://www.ncbi.nlm.nih.gov/books/NBK542796/1-5. [PubMed] [Google Scholar]
- 3.Committee on the Public Health Dimensions of Cognitive Aging. Board on Health Sciences Policy. Institute of Medicine . Cognitive Aging: Progress in Understanding and Opportunities for Action. National Academies Press; Washington, DC, USA: 2015. [PubMed] [Google Scholar]
- 4.Livingston G., Sommerlad A., Orgeta V., Costafreda S.G., Huntley J., Ames D., Ballard C., Banerjee M.D., Burns A., Cohen-Mansfield J., et al. Dementia prevention, intervention, and care. Lancet. 2020;390:2673–2734. doi: 10.1016/S0140-6736(17)31363-6. [DOI] [PubMed] [Google Scholar]
- 5.Shaw N., McGuire S. Understanding the use of geographical information systems (GIS) in health informatics research: A review. J. Innov. Health Inform. 2017;24:228–233. doi: 10.14236/jhi.v24i2.940. [DOI] [PubMed] [Google Scholar]
- 6.Fletcher-Lartey S., Caprarelli G. Application of GIS technology in public health: Successes and challenges. Parasitology. 2016;143:401–415. doi: 10.1017/S0031182015001869. [DOI] [PubMed] [Google Scholar]
- 7.Wu Y.T., Brayne C., Liu Z., Huang Y., Sosa A.L., Acosta D., Prina M. Neighborhood environment and dementia in older people from high-, middle- and low-income countries: Results from two population-based cohort studies. BMC Public Health. 2020;20:1330. doi: 10.1186/s12889-020-09435-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Estrella M., Durazo-Arvizu R.A., Gallo L.C., Isasi C.R., Perreira K.M., Vu T.T., Vasquez E., Sachdeva S., Zeng D., Llabre M.M., et al. Associations between perceived neighborhood environment and cognitive function among middle-aged and older women and men: Hispanic community health study/Study of Latinos sociocultural ancillary study. Soc. Psychiatry Psychiatr. Epidemiol. 2020;55:685–696. doi: 10.1007/s00127-019-01829-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tani Y., Hanazato M., Fujiwara T., Suzuki N., Kondo K. Neighborhood sidewalk environment and incidence of dementia in older Japanese adults: The Japan Gerontological Evaluation Study Cohort. Am. J. Epidemiol. 2021;190:1270–1280. doi: 10.1093/aje/kwab043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu Y.T., Prina A.M., Jones A., Matthews F.E., Brayne C. Medical Research Council Cognitive Function and Ageing Study Collaboration. The built environment and cognitive disorders: Results from the cognitive function and ageing study II. Am. J. Prev. Med. 2017;53:25–32. doi: 10.1016/j.amepre.2016.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng T.P., Nyunt M.S.Z., Shuvo F.K., Eng J.Y., Yap K.B., Hee L.M., Chan S.P., Scherer S. The neighborhood built environment and cognitive function of older persons: Results from the Singapore longitudinal ageing study. Gerontology. 2018;64:149–156. doi: 10.1159/000480080. [DOI] [PubMed] [Google Scholar]
- 12.Besser L.M., McDonald N., Song Y., Kukull W.A., Rodriguez D.A. Neighborhood environment and cognition in older adults: A systematic review. Am. J. Prev. Med. 2017;53:241–251. doi: 10.1016/j.amepre.2017.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okuyama K., Abe T., Hamano T., Takeda M., Sundquist K., Sundquist J., Nabika T. Hilly neighborhoods are associated with increased risk of weight gain among older adults in rural Japan: A 3-years follow-up study. Int. J. Health Geogr. 2019;18:10. doi: 10.1186/s12942-019-0174-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fukuoka R., Takeda M., Abe T., Yamasaki M., Kimura S., Okuyama K., Isomura M., Nabika T. Inconvenience of living place affects individual HbA1c level in a rural area in Japan: Shimane CoHRE study. Int. J. Environ. Res. Public Health. 2021;18:1147. doi: 10.3390/ijerph18031147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abe T., Okuyama K., Hamano T., Takeda M., Isomura M., Nabika T. Hilly environment and physical activity among community-dwelling older adults in Japan: A cross-sectional study. BMJ Open. 2020;10:e033338. doi: 10.1136/bmjopen-2019-033338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abe T., Okuyama K., Hamano T., Takeda M., Yamasaki M., Isomura M., Nakano K., Sundquist K., Nabika T. As sessing the Impact of a Hilly Environment on Depressive Symptoms among Community-Dwelling Older Adults in Japan: A Cross-Sectional Study. Int. J. Environ. Res. Public Health. 2021;18:4520. doi: 10.3390/ijerph18094520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Onoda K., Yamaguchi S. Revision of the cognitive assessment for dementia, IPad version (CADi2) PLoS ONE. 2014;9:e109931. doi: 10.1371/journal.pone.0109931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mavoa S., Bagheri N., Koohsari M.J., Kaczynski A.T., Lamb K.E., Oka K., O’Sullivan D., Witten K. How do neighborhood definitions influence the associations between the built environment and physical activity? Int. J. Environ. Res. Public Health. 2019;16:1501. doi: 10.3390/ijerph16091501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zung W.K. A Self-Rating Depression Scale. Arch. Gen. Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 20.Hamano T., Onoda K., Takeda M., Sundquist K., Yamaguchi S., Nabika T. Geographic elevation and cognitive function among elderly residents in rural mountainous areas: Shimane CoHRE Study. Int. J. Environ. Res. Public Health. 2015;12:13365–13371. doi: 10.3390/ijerph121013365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Y.T., Prina A.M., Brayne C. The association between community environment and cognitive function: A systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 2015;50:351–362. doi: 10.1007/s00127-014-0945-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tanaka T., Tanaka K., Suyama K., Honda S., Senjyu H., Kozu R. A comparison of objective physical activity, muscle strength, and depression among community-dwelling older women living in sloped versus non-sloped environments. J. Nutr. Health Aging. 2016;20:520–524. doi: 10.1007/s12603-015-0602-0. [DOI] [PubMed] [Google Scholar]
- 23.Tani Y., Suzuki N., Fujiwara T., Hanazato M., Kondo K. Neighborhood food environment and dementia incidence: The Japan Gerontological Evaluation Study cohort survey. Am. J. Prev. Med. 2019;56:383–392. doi: 10.1016/j.amepre.2018.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo Y., Chan C.H., Chang Q., Liu T., Yip P.S.F. Neighborhood environment and cognitive function in older adults: A multilevel analysis in Hong Kong. Health Place. 2019;58:102146. doi: 10.1016/j.healthplace.2019.102146. [DOI] [PubMed] [Google Scholar]
- 25.Clarke P.J., Weuve J., Barnes L., Evans D.A., Mendes de Leon C.F. Cognitive decline and the neighborhood environment. Ann. Epidemiol. 2015;25:849–854. doi: 10.1016/j.annepidem.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ito T., Okuyama K., Abe T., Takeda M., Hamano T., Nakano K., Nabika T. Relationship between Individual Social Capital and Cognitive Function among Older Adults by Gender: A Cross-Sectional Study. Int. J. Environ. Res. Public Health. 2019;16:2142. doi: 10.3390/ijerph16122142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hikichi H., Kondo K., Takeda T., Kawachi I. Social interaction and cognitive decline: Results of a 7-year community intervention. Alzheimer’s Dement. 2016;3:23–32. doi: 10.1016/j.trci.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iwasa H., Yoshida Y., Kai I., Suzuki T., Kim H., Yoshida H. Leisure activities and cognitive function in elderly community-dwelling individuals in Japan: A 5-year prospective cohort study. J. Psychosom. Res. 2012;72:159–164. doi: 10.1016/j.jpsychores.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 29.Barnett D.W. Build environment correlates of older adults’ total physical activity and walking: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017;14:103. doi: 10.1186/s12966-017-0558-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yen I.H., Michael Y.L., Perdue L. Neighborhood environment in studies of health of older adults. A systematic review. Am. J. Prev. Med. 2009;37:455–463. doi: 10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muñoz E., Scott S.B., Corley R., Wadsworth S.J., Sliwinski M.J., Reynolds C.A. The role of neighborhood stressors on cognitive function: A coordinated analysis. Health Place. 2020;66:102442. doi: 10.1016/j.healthplace.2020.102442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thierry A.D., Sherman-Wilkins K., Armendariz M., Sullivan A., Farmer H.R. Perceived Neighborhood Characteristics and Cognitive Functioning among Diverse Older Adults: An Intersectional Approach. Int. J. Environ. Res. Public Health. 2021;18:2661. doi: 10.3390/ijerph18052661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luo Y., Zhang l., Pan X. Neighborhood environments and cognitive decline among middle-aged and older people in China. J. Gerontol. B. 2019;74:e60–e71. doi: 10.1093/geronb/gbz016. [DOI] [PubMed] [Google Scholar]
- 34.Senger J., Bruscato N.M., Werle B., Moriguchi E.H., Pattussi M.P. Nutritional status and cognitive impairment among the very old in a community sample from southern Brazil. J. Nutr. Health Aging. 2019;23:923–929. doi: 10.1007/s12603-019-1230-x. [DOI] [PubMed] [Google Scholar]
- 35.Wang J., Xiao L.D., Wang K., Luo Y., Li X. Cognitive impairment and associated factors in rural elderly in north China. J. Alzheimer’s Dis. 2020;77:1241–1253. doi: 10.3233/JAD-200404. [DOI] [PubMed] [Google Scholar]
- 36.Hsu H.C., Bai C.H. Social and Built Environments Related to Cognitive Function of Older Adults: A Multi-Level Analysis Study in Taiwan. Int. J. Environ. Res. Public Health. 2021;18:2820. doi: 10.3390/ijerph18062820. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This study used data from the Shimane CoHRE study. Some data are available at the Center for Community-Based Healthcare Research and Education (CoHRE), Organization for Research and Academic Information, Shimane University, 223-8 Enya-cho, Izumo-shi, Shimane 693-8501, Japan.