Abstract
Simple Summary
Biliary tract cancer is a rare malignancy with poor overall survival. The majority of patients are faced with advanced disease stage. Cisplatin-based treatment schedules represent the mainstay of first-line therapeutic strategy, yet only a small portion of patients develop a treatment response. One of the main reasons is acquired drug resistance. Previous studies correlated certain microRNAs (miRNAs), including miR-200c-3p, with drug resistance in various cancer types. However, limited knowledge exists about miR-200c-3p expression and cisplatin resistance in biliary tract cancer. Thus, the main aim of this study was to investigate the influence of miR-200c-3p on the cisplatin resistance in this cancer entity. We demonstrated that miR-200c-3p contributes to cisplatin resistance independently of its known influence on ZEB1 expression.
Abstract
Biliary tract cancer is a major global health issue in cancer-related mortality. Therapeutic options are limited, and cisplatin-based treatment schedules represent the mainstay of first-line therapeutic strategies. Although the gain of survival by the addition of cisplatin to gemcitabine is moderate, acquired cisplatin resistance frequently leads to treatment failures with mechanisms that are still poorly understood. Epithelial–mesenchymal transition (EMT) is a dynamic process that changes the shape, function, and gene expression pattern of biliary tract cancer cells. In this study, we explored the influence of the EMT-regulating miR-200c-3p on cisplatin sensitivity in biliary tract cancer cells. Using gain of function experiments, we demonstrated that miR-200c-3p regulates epithelial cell markers through the downregulation of the transcription factor ZEB1. MiR-200c-3p upregulation led to a decreased sensitivity against cisplatin, as observed in transient overexpression models as well as in cell lines stably overexpressing miR-200c-3p. The underlying mechanism seems to be independent of miR-200c-3p’s influence on ZEB1 expression, as ZEB1 knockdown resulted in the opposite effect on cisplatin resistance, which was abolished when ZEB1 knockdown and miR-200c-3p overexpression occurred in parallel. Using a gene panel of 40 genes that were previously associated with cisplatin resistance, two (Dual Specificity Phosphatase 16 (DUSP16) and Stratifin (SFN)) were identified as significantly (>2 fold, p-value < 0.05) up-regulated in miR-200c-3p overexpressing cells. In conclusion, miR-200c-3p might be an important contributor to cisplatin resistance in biliary tract cancer, independently of its interaction with ZEB1.
Keywords: biliary tract cancer, chemoresistance, cisplatin resistance, epithelial–mesenchymal transition, miR-200c-3p, ZEB1
1. Introduction
Biliary tract cancer (BTC) is a rare malignancy arising from the epithelium of intrahepatic or extrahepatic bile ducts or the gallbladder [1]. Despite the low incidence in most developed countries, BTC is turning into a major global health issue as the number of new intrahepatic cases is constantly rising [2]. BTC is an aggressive cancer type with poor overall survival. Surgery is the only potential curative treatment, but most patients are diagnosed with locally advanced or metastatic disease [3,4]. Therapeutic options in these situations are limited. Gemcitabine plus cisplatin treatment schedules represent the mainstay of first-line therapy. While this combination, chemotherapy shows superiority and improved survival over gemcitabine alone, and acquired drug resistance leads to a modest 3-month increase in median survival time [5,6,7].
Mechanisms underlying cisplatin resistance in cancer are poorly understood. Previous studies reported the involvement of DNA repair mechanisms, altered cellular accumulation, and drug metabolism [8,9]. In addition, deregulated microRNA (miRNA) expression has been associated with cisplatin resistance in various cancers, including BTC [10,11,12]. miRNAs are a class of small, single-stranded, non-coding, regulatory RNAs with a length of 17–25 nucleotides. Their main role is the post-transcriptional regulation of target mRNAs by binding to their 3′-untranslated region (3′-UTR), leading to their degradation [13,14]. miR-200c-3p is a member of the miR-200 family, which has been reported to be involved in crucial processes such as cell proliferation, invasion, metastasis, apoptosis, and drug resistance [15]. In addition to resistance to paclitaxel and doxorubicin in breast cancer, epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors and radiotherapy in non-small cell lung cancer (NSCLC), and etoposide and topotecan in small cell lung cancer (SCLC) [16,17,18,19,20], alterations in miR-200c-3p expression levels have been reported to be responsible for the resistance to cisplatin in gastric cancer, esophageal cancer, and ovarian cancer [21,22,23].
Multiple studies proved that common molecular mechanisms of miR-200c-3p-related drug resistance are mediated via upregulation of zinc finger E-box binding homeobox (ZEB) family genes [24,25,26,27]. ZEB proteins downregulate E-cadherin, a transmembrane glycoprotein important in the maintenance of cell–cell interactions [28]. Thus, the loss of E-cadherin leads to weakened cell–cell interactions and eventual induction of epithelial–mesenchymal transition (EMT) in cancers [29,30]. EMT has been demonstrated to contribute to cancer cell plasticity by switching between continuous states of cell fate [31], and miRNAs regulating this process might be contributors to cisplatin resistance.
Limited knowledge exists about miR-200c-3p expression and cisplatin resistance in BTC. Therefore, the present study investigated the role of miR-200c-3p in the cisplatin resistance of BTC cells.
2. Materials and Methods
2.1. Cell Culture
A panel of ten BTC cell lines was used in this study: EGI-1 (ACC 385 [32]) and TFK-1 (ACC 344 [33]) cells were purchased from the German Collection of Microorganisms and Cell Cultures (DSMZ; https://www.dsmz.de, last accessed on 1 August 2021); HuCCT1 (JCRB0425 [34]), HuH28 (JCRB0426 [35]), KKU-055 (JCRB1551), KKU-100 (JCRB1568 [36]), KKU-213 (JCRB1557 [37]), NOZ (JCRB1033 [38]), OCUG-1 (JCRB0191 [39]) and OZ (JCRB1032 [40]) were purchased from the Japanese Collection of Research Bioresources Cell Bank (JCRB; https://cellbank.nibiohn.go.jp, last accessed on 1 August 2021). The immortalized human cholangiocyte cell line MMNK-1 (JCRB1554 [41]) was purchased from JCRB. All cell lines were cultured in L-glutamine-free Dulbecco’s Modified Eagle Medium (DMEM) containing 4.5 g/L glucose (Gibco, Thermo Fisher Scientific, Waltham, MA, USA). Medium was supplemented with 10% fetal bovine serum (FBS; Serana Europe GmbH, Pessin, Germany) and 1% penicillin/streptomycin (Gibco, Thermo Fisher Scientific, Waltham, MA, USA). Cells were cultured at standard conditions (37 °C, 21% O2, 5% CO2, and 98% humidity).
2.2. Transient Transfection
For transient miR-200c-3p overexpression, MMNK-1, OCUG-1, and HuCCT1 cells were seeded in 6-well plates or 96-well plates and transfected with 10 nM mirVana miR-200c-3p mimic (Cat. #: 4464066, Thermo Fisher Scientific, Waltham, MA, USA) or 10 nM mirVana miRNA mimic Negative Control #1 (Cat. #: 4464058, Thermo Fisher Scientific, Waltham, MA, USA). For transient ZEB1 knockdown, cells were seeded in 6-well plates or 96-well plates and transfected with 50 nM siRNA directed against ZEB1 (Hs_ZEB1_2, Cat. #: SI04272492, QIAGEN, Hilden, Germany) or 50 nM AllStars Negative Control siRNA (Cat. #: 1027280, QIAGEN, Hilden, Germany). The transfection procedure was carried out according to the fast-forward protocol of the HiPerFect Transfection Reagent (Cat. #: 301707, QIAGEN, Hilden, Germany). For co-transfection experiments, MMNK-1 cells were seeded into 96-well plates at a density of 1500 cells per well, and transfected with 10 nM mirVana miR-200c-3p mimic (Cat. #: 4464066, Thermo Fisher Scientific, Waltham, Massachusetts, USA) and 50 nM siRNA directed against ZEB1 (Hs_ZEB1_2, Cat. #: SI04272492, QIAGEN, Hilden, Germany), or 10 nM mirVana miRNA mimic Negative Control #1 (Cat. #: 4464058, Thermo Fisher Scientific, Waltham, MA, USA) and 50 nM AllStars Negative Control siRNA (Cat. #: 1027280, QIAGEN, Hilden, Germany) according to the fast-forward protocol of the HiPerFect Transfection Reagent (Cat. #: 301707, QIAGEN, Hilden, Germany).
2.3. Generation of Stable miRNA Overexpression Cell Lines
OCUG-1 cells were seeded into 12-well plates at a density of 100,000 cells per well. After a twenty-four-hour incubation under standard conditions, growth medium was replaced with medium containing 10 μg/mL Polybrene (Cat #: sc-134220, Santa Cruz Biotechnology, Inc., Dallas, TX, USA), 0.5% ViralPlus Transduction Enhancer (Applied Biological Materials Inc., Vancouver, BC, Canada), and either LentimiRa-GFP-hsa-miR-200c-3p Virus (mh15263, Applied Biological Materials Inc., Vancouver, British Columbia, Canada) or Lenti-III-mir-GFP Control Virus (m002, Applied Biological Materials Inc., Vancouver, BC, Canada). Transduced cells were selected with growth medium containing a sublethal concentration of puromycin (Gibco, Thermo Fisher Scientific, Waltham, MA, USA) for up to eight weeks. To further increase miR-200c-3p overexpression levels, transduced cells were sorted according to their GFP expression via flow cytometry using the FACSARia IIIu (BD Biosciences, Franklin Lakes, NJ, USA). Cells with the highest GFP intensity (top 20% GFP signal) were cultured and used for subsequent experiments.
2.4. Reverse Transcription Quantitative PCR (RT-qPCR)
Total RNA was isolated from 70 to 90% confluent cells using QIAzol Lysis Reagent (Cat. #: 79306, QIAGEN, Hilden, Germany) according to the manufacturer’s recommendations. Subsequently, 1 μg of total RNA was reversely transcribed with the miScript II RT Kit (Cat. #: 218161, QIAGEN, Hilden, Germany) using the miScript HiFlex buffer to enable quantification of both miRNA and mRNA. qPCR was performed on the LightCycler 480 (Roche, Basel, Switzerland) using the QuantiTect SYBR Green PCR Kit (Cat. #: 204145, QIAGEN, Hilden, Germany). For the quantification of miR-200c-3p, the Hs_miR-200c_1 miScript Primer Assay (Cat. #: MS00003752, QIAGEN, Hilden, Germany) and Hs_RNU6-2_11 miScript Primer Assay (Cat. #: MS00033740, QIAGEN, Hilden, Germany) were used, with RNU6-2 serving as a reference gene. For mRNA quantification, expression levels of Keratin 8 (KRT8), E-cadherin (CDH1), N-cadherin (CDH2), Collagen Type III Alpha 1 Chain (COL3A1), Vimentin (VIM), zinc finger E-box binding homeobox 1 (ZEB1), zinc finger E-box binding homeobox 2 (ZEB2), and genes that have previously been associated with cisplatin resistance (see Table S1) were normalized to the mean expression of GAPDH and U6. Primer sequences are listed in Table S2. Differences in gene expression were evaluated by the ΔΔCt method.
2.5. Immunoblot Analysis
Cells were lysed in radioimmunoprecipitation assay (RIPA) buffer supplemented with 2% Protease Inhibitor Cocktail (Thermo Fisher Scientific, Waltham, Massachusetts, USA). Thirty micrograms of total protein was mixed with 4x Laemmli buffer containing 10% β-mercaptoethanol and denaturized at 95 °C for 10 min. Proteins were separated on 4–15% Mini-PROTEAN® TGX Stain-free™ Gels (Bio-Rad Laboratories, Inc., Hercules, CA, USA) and transferred to a 0.45 µm nitrocellulose membrane (Bio-Rad Laboratories, Inc., Hercules, CA, USA). Membranes were blocked with 5% milk powder in Tris-buffered saline (TBS) containing 0.1% Tween® 20 (5% M-TBS-T) for 1–5 h before incubation with primary antibody targeted at ZEB1 (TCF8/ZEB1 (D80D3) Rabbit mAb, #702743, Cell Signaling Technology®, Danvers, Massachusetts, USA; diluted 1:1000 in 2.5% M-TBS-T) at 4 °C for 16 h. Subsequently, membranes were incubated with the corresponding secondary horseradish peroxidase (HRP)-conjugated antibody (Peroxidase AffiniPure Goat Anti-Rabbit IgG antibody, 111-035-144, Jackson ImmunoResearch Laboratories, Inc., West Grove, PA, USA; diluted 1:10,000 in 2.5% M-TBS-T) for 1 h at room temperature (RT). Membranes were incubated with SuperSignal® West Femto PLUS Chemiluminescent Substrate (Bio-Rad Laboratories, Inc., Hercules, CA, USA) and imaged on a ChemiDoc™ Touch (Bio-Rad Laboratories, Inc., Hercules, CA, USA). To verify equal protein loading, membranes were stripped and re-probed for Cofilin (Anti-Cofilin antibody, ab42824, Abcam, Cambridge, UK; diluted 1:5000 in 2.5% M-TBS-T). Uncropped Western blot images can be found at Figure S5.
2.6. Cisplatin Sensitivity Assay
MMNK-1, OCUG-1, and HuCCT1 cells were seeded into 96-well plates at densities of 1500, 500, and 3500 cells per well, respectively, and transfected according to the HiPerFect fast-forward protocol (QIAGEN, Hilden, Germany). Twenty-four hours later, standard growth medium was exchanged with fresh growth medium containing cisplatin in various concentrations (0–50 µM). Forty-eight hours after the addition of cisplatin, 100 µL of medium was removed and 10 µL Cell Proliferation Reagent WST-1 (Cat. #: 11644807001, Roche, Basel, Switzerland) was added to each well. After a 180 min incubation at standard conditions, absorbances at 450 nm and 620 nm (reference wavelength) were measured on the SPECTROstar Omega (BMG LABTECH GmbH, Ortenberg, Germany). Results were used for the IC50 calculations via ordinary least-squares regression with outlier removal following the ROUT method [42].
2.7. Statistical Analysis
All experiments were performed at least three independent times. Data are presented as mean ± standard deviation (SD). Statistical analyses were performed using the GraphPad Prism 5.0 software (GraphPad Software, San Diego, CA, USA). The unpaired two-tailed t-test and one-way ANOVA with Tukey’s Post Hoc test were used when applicable. A p value of less than 0.05 was regarded as statistically significant. * p < 0.05, ** p < 0.01, *** p < 0.001.
3. Results
3.1. MiR-200c-3p and Its Influence on EMT Markers in Immortalized Cholangiocytes, Biliary Tract Cancer Cell Lines, and Human Tissue
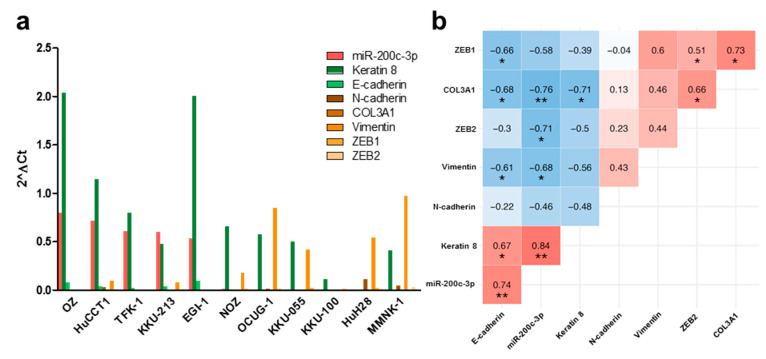
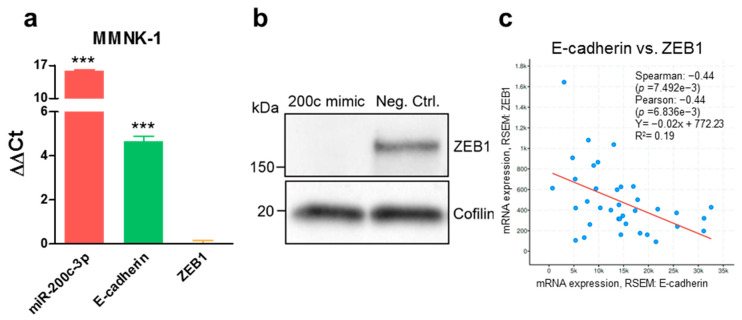
In an attempt to better understand the relationship between miR-200c-3p and the epithelial–mesenchymal transition status in BTC, we analyzed the endogenous expression levels of miR-200c-3p and several epithelial (Keratin 8 (KRT8), E-cadherin (CDH1)) and mesenchymal (N-cadherin (CDH2), Collagen Type III Alpha 1 Chain (COL3A1), Vimentin (VIM), ZEB1, ZEB2) gene expression markers in immortalized cholangiocytes and BTC cell lines. Based on these endogenous expression levels, cell lines with a predominantly epithelial expression profile (high miR-200c-3p, high CDH1, and low ZEB1) or a predominantly mesenchymal expression profile (low miR-200c-3p, low CDH1, and high ZEB1) were determined (Figure 1a). A significant correlation between miR-200c-3p and epithelial gene expression markers was confirmed (Figure 1b). Additionally, we functionally confirmed the relationship between ZEB1, CDH1, and miR-200c-3p expression in MMNK-1 cells by gain of function experiments. After ectopic overexpression of miR-200c-3p, an increased expression of CDH1 on RNA level (Figure 2a) and a decreased expression of ZEB1 on protein level (Figure 2b) were observed. The negative correlation between ZEB1 and CDH1 was further validated in 36 human BTC tissue samples of The Cancer Genome Atlas datasets (Figure 2c).
Figure 1.
Endogenous expression levels of miR-200c-3p correlates with the expression of EMT markers in immortalized cholangiocytes and biliary tract cancer cell lines. (a) Expression levels of miR-200c-3p and various EMT markers were analyzed in immortalized cholangiocytes (MMNK-1 cells) and 10 BTC cell lines via RT-qPCR. (b) Spearman rank correlation matrix of endogenously expressed miR-200c-3p and EMT markers in MMNK-1 cells and BTC cell lines. Positive correlations are depicted in shades of red, negative correlations in shades of blue. Correlation coefficient and statistical significance indicators are shown in the respective tiles. * p < 0.05, ** p < 0.01.
Figure 2.
Transient miR-200c-3p overexpression induces an epithelial phenotype through the interaction with E-cadherin and ZEB1. (a) MMNK-1 cells were transiently transfected with 10 nM mirVana miR-200c-3p mimic, and the expression levels of miR-200c-3p, E-cadherin (CDH1), and ZEB1 were compared to those of respective cells transfected with 10 nM mirVana mimic negative control. Positive values represent an overexpression. A value of 0 indicates that there was no difference between cells transfected with miR-200c-3p mimic and mimic negative control. Unpaired two-tailed t-test was used to evaluate statistical significance. *** p < 0.001. (b) ZEB1 protein levels were compared between miR-200c-3p mimic-transfected MMNK-1 cells and Neg. Ctrl.-transfected MMNK-1 cells. Cofilin was used as loading control. (c) In silico correlation analysis of E-cadherin (CDH1) and ZEB1 expression levels in 36 human BTC tissue samples from The Cancer Genome Atlas.
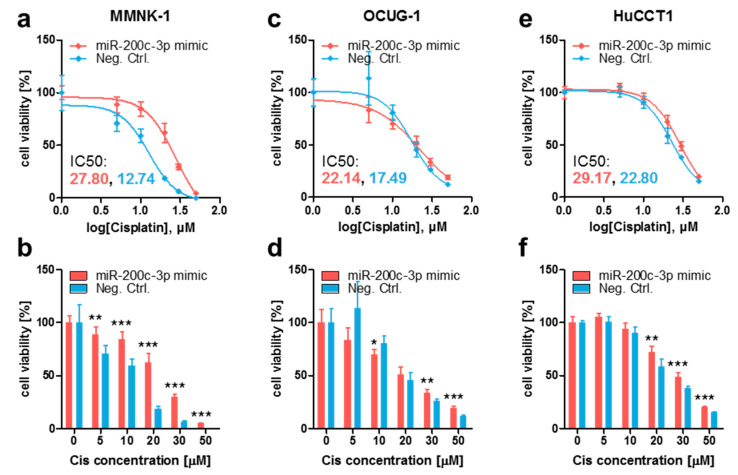
3.2. Ectopic MiR-200c-3p Overexpression Increases Cisplatin Resistance in Immortalized Cholangiocytes and Biliary Tract Cancer Cells
Cisplatin is a mainstay of therapeutic strategies and has significantly improved the survival of metastatic BTC patients in recent years [5]. Since there seems to be a link between the EMT status of cancer cells and their sensitivity to cisplatin, and because miR-200c-3p expression shows a tendency to influence overall survival in patients suffering from cholangiocarcinoma (Figure S1), we sought to determine if the EMT-regulating miR-200c-3p affects the cisplatin sensitivity of BTC cells. Therefore, we ectopically overexpressed miR-200c-3p by transfecting MMNK-1, OCUG-1, and HuCCT1 cells with miR-200c-3p mimic and mimic Negative Control (Neg. Ctrl.). After confirming a dose-dependent and time-dependent effect of cisplatin (Figure S2), cisplatin sensitivity was compared between miR-200c-3p mimic-transfected and Neg. Ctrl.-transfected cells. In all three cell lines, miR-200c-3p overexpression rendered cells more resistant to cisplatin when compared to their control counterparts, which was made apparent by the increased inhibitory concentration 50% (IC50) values (Figure 3a,c,e) and in the direct viability comparison (Figure 3b,d,f).
Figure 3.
Transient miR-200c-3p overexpression renders immortalized cholangiocytes and BTC cells more resistant to cisplatin. (a,b) MMNK-1, (c,d) OCUG-1, and (e,f) HuCCT1 cells were transfected with 10 nM mirVana miR-200c-3p mimic (miR-200c-3p mimic) or mirVana mimic Negative Control (Neg. Ctrl.) for 24 h and subsequently treated with various concentrations of cisplatin (Cis). After 48 h, cell viability was assessed by adding WST-1 reagent and measuring absorbances at 450 nm and 620 nm (reference wavelength). Cells treated with cisplatin were normalized to untreated (0 μM) cells (set to 100%). (a,c,e) Ordinary least-squares regression with outlier removal following the ROUT method was used to determine the inhibitory concentration 50% (IC50) values. (b,d,f) Unpaired two-tailed t-test was used to evaluate statistical significance. * p < 0.05, ** p < 0.01, *** p < 0.001.
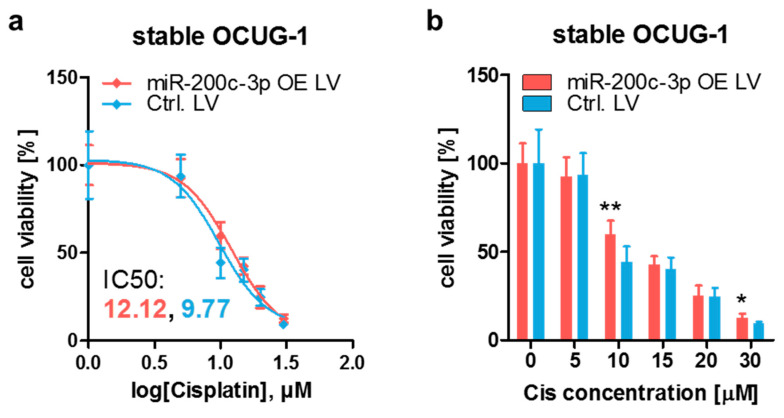
3.3. Stable Endogenous MiR-200c-3p Overexpression Increases Cisplatin Resistance in Biliary Tract Cancer Cells
To corroborate the results of the transient overexpression setting, stable endogenous miR-200c-3p overexpression OCUG-1 cells were generated by lentiviral transduction (Figure S3). In comparison to Control cells (Ctrl. LV), miR-200c-3p overexpression cells (miR-200c-3p OE LV) were less sensitive to cisplatin, confirming the results from the transient overexpression models (Figure 4).
Figure 4.
Stable miR-200c-3p overexpression results in an increased cisplatin resistance in OCUG-1 cells. (a) IC50 determination and (b) direct comparison of stable miR-200c-3p overexpression OCUG-1 cells (miR-200c-3p OE LV) and OCUG-1 control cells (Ctrl. LV). Cells were treated with various concentrations of cisplatin (Cis). After 48 h, cell viability was assessed by adding WST-1 reagent and measuring the absorbance at 450 nm and 620 nm (reference wavelength). Cells treated with cisplatin were normalized to untreated (0 μM) cells (set to 100%). (a) Ordinary least-squares regression with outlier removal following the ROUT method was used to determine the IC50 values of the respective cells. (b) Unpaired two-tailed t-test was used to evaluate statistical significance. * p < 0.05, ** p < 0.01.
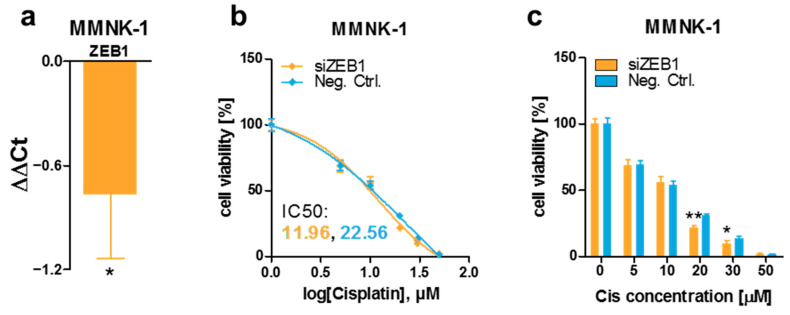
3.4. ZEB1 Knockdown Decreases Cisplatin Resistance of MMNK-1 Cells, Rescue Experiments and Cisplatin-Resistance Associated Gene Expression Pattern
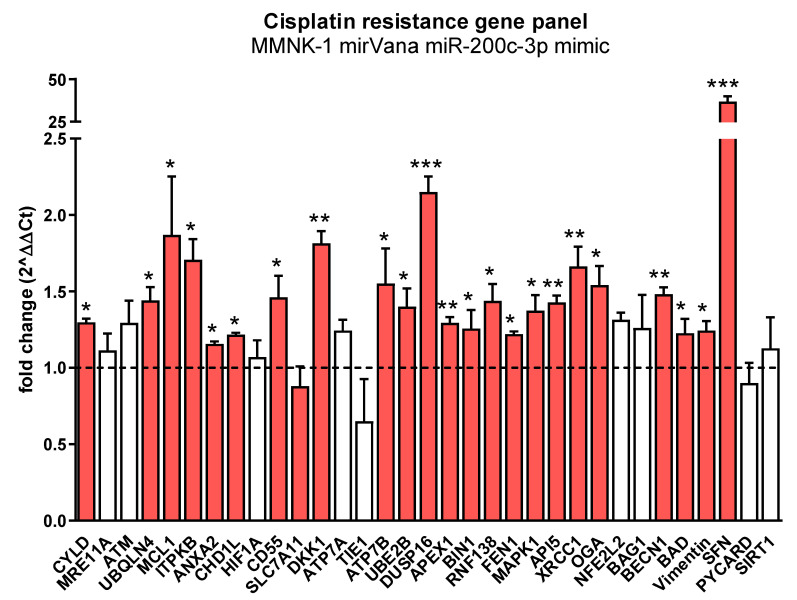
In order to explore if miR-200c-3p exerts its effect on cisplatin sensitivity by downregulating ZEB1, or in a ZEB1-independent manner, we decreased ZEB1 expression levels in MMNK-1 cells by siRNA-mediated knockdown (Figure 5a) and evaluated the changes in cisplatin sensitivity. In contrast to miR-200c-3p-mediated effects, ZEB1 knockdown resulted in a decreased cisplatin resistance in MMNK-1 cells, indicating that different miR-200c-3p-regulated mechanisms are responsible for the observed alterations in cisplatin sensitivity (Figure 5b,c). In order to explore whether the effect of ZEB1 knockdown can be reversed by miR-200c-3p overexpression, we performed a co-transfection experiment with simultaneous transfection of siRNA against ZEB1 and miR-200c-3p mimics. As shown in Figure S4, the effect of ZEB1 knockdown was rescued by co-transfection of miR-200c (IC50 10.6 versus 11.6, p = 0.38). In order to identify some possible mechanisms of the miR-200c-3p effects, we measured the expression of about 40 genes that were previously associated with cisplatin resistance. As shown in Figure 6, several genes were significantly differentially expressed, including two with greater than two-fold up-regulation (DUSP16 and SFN).
Figure 5.
Transient ZEB1 knockdown leads to a decreased cisplatin resistance in MMNK-1 cells. (a) MMNK-1 cells were transfected with 50 nM ZEB1 siRNA (siZEB1) or Allstars Neg. Ctrl. (Neg. Ctrl.), and the ZEB1 expression level was compared via the ΔΔCt method. A negative value represents a downregulation; a value of 0 indicates that there was no difference between siZEB1-transfected cells and Neg. Ctrl.-transfected cells. Unpaired two-tailed t-test was used to evaluate statistical significance. (b) IC50 determination via ordinary least-squares regression with outlier removal following the ROUT method and (c) direct comparison of transient ZEB1 knockdown and control conditions in MMNK-1 cells. Cells were transfected with 50 nM ZEB1 siRNA (siZEB1) or AllStars Neg. Ctrl. (Neg. Ctrl.) and subsequently treated with various concentrations of cisplatin (Cis). After 48 h, cell viability was assessed by adding WST-1 reagent and measuring absorbance at 450 nm and 620 nm (reference wavelength). Cells treated with cisplatin were normalized to untreated (0 μM) cells (set to 100%). Unpaired two-tailed t-test was used to evaluate statistical significance. * p < 0.05, ** p < 0.01.
Figure 6.
The cisplatin conferring genes DUSP16 and SFN are significantly (>2 fold, p-value < 0.05) up-regulated in miR-200c-3p overexpressing cells. MMNK-1 cells were transfected with 10 nM mirVana miR-200c-3p mimic or 10 nM mirVana miRNA mimic Negative Control. After 48 h, total RNA was isolated from 70 to 90% confluent cells using QIAzol Lysis Reagent. Reverse Transcription Quantitative PCR (RT-qPCR) of cisplatin-resistance-conferring genes was performed, and gene expression was normalized to GAPDH and U6. Differences in gene expression were evaluated by the ΔΔCt method. Unpaired two-tailed t-test was used to evaluate statistical significance. * p < 0.05, ** p < 0.01, *** p < 0.001.
4. Discussion
BTC continues to be an aggressive cancer type with poor outcome and exhibits a low response rate to the cisplatin-based first-line treatment standard. Therefore, understanding the underlying mechanism behind cisplatin-based resistance is of utmost importance for the improvement of current treatment schedules. Emerging evidence suggests that alterations in miRNA expression levels significantly contribute to this resistance issue. For instance, miR-1249 drives cisplatin resistance via the expansion of cancer stem cell populations through Wnt pathway deregulation [12]. Downregulated miR-145 and miR-199a-3p diminish the cisplatin-induced expression of multidrug resistance associated protein 1 (MRP1) and multidrug resistant protein 1 (MDR1) in gallbladder cancer [43,44]. miR-31 contributes to cisplatin resistance in gallbladder cancer via the anti-apoptotic Src/Akt/Bax/Bcl-2 signaling pathway [45]. Similarly, reduced expression of miR-125b-5p contributes to cisplatin resistance through upregulated Bcl-2 expression [46].
In our study, we focused on miR-200c-3p, a previously described factor that is centrally involved in EMT. Furthermore, miR-200c-3p is a member of the miR-200 family and has been reported to be abnormally expressed in various cancers. It is significantly downregulated in prostate cancer, nephroblastoma, breast cancer, and gastric cancer [16,47,48,49,50]. On the other hand, miR-200c-3p is upregulated and leads to worse clinicopathological features in several other cancer entities, such as nasopharyngeal carcinoma, oral squamous cell carcinoma (OSCC), colorectal cancer (CRC), ovarian cancer, small cell lung cancer (SCLC), and endometrial cancer [20,51,52,53,54,55]. Involvement of this miRNA in the development of drug resistance in different cancers has been reported [16,17,18,19,20]. A common molecular mechanism of miR-200c-3p-induced general drug resistance is mediated via the induction of EMT. One study has shown an interaction between long-noncoding RNA ATB (lncATB) and miR-200c in breast cancer cells. LncATB acts as a competing endogenous RNA (ceRNA) sponging miR-200c. The resulting downregulation of miR-200c leads to restored expression of the transcription factor TWIST1, which further results in EMT-mediated trastuzumab resistance [26,56]. Similarly, an interaction between long-noncoding RNA metastasis-associated lung adenocarcinoma transcript 1 (MALAT-1) and miR-200c-3p was reported in pancreatic cancer. MALAT-1 functions as a ceRNA to suppress miR-200c-3p, leading to the upregulation of ZEB1 expression [27]. Circular RNA hsa_circ_001783 sponges miR-200c-3p in breast cancer, which leads to the upregulation of miR-200c-3p target genes ZEB1, ZEB2, and ETS1 [24]. ZEB2 is a direct target of miR-200c-3p that is downregulated in prostate cancer, which results in EMT [25]. Alternatively, miR-200c-3p modulates the expression of metabolic enzyme cytochrome P450 1B1 (CYP1B1) and transcription factor SOX2 in renal cell carcinoma and breast cancer, respectively. These effects contribute to the resistance to taxanes [16,57].
However, limited knowledge exists about miR-200c-3p expression and cisplatin-resistance in BTC. Two studies documented lower expression in intrahepatic BTC and gallbladder cancer compared to normal tissue [58,59]. Shen et al. have shown that miR-200c-3p could be an efficient biomarker for BTC as serum levels of exosomal miR-200c-3p positively correlate with the rate of BTC progression [60]. Li et al. found that long intergenic non-protein coding RNA 667 (LINC00667) functions as a ceRNA for miR-200c-3p in BTC. As a consequence of this miR-200c-3p downregulation, overexpressed LINC00667 upregulates pyruvate dehydrogenase kinase 1 (PDK1) to promote the development of BTC through the enhanced proliferation, migration, invasion and EMT of BTC cells [61]. Nevertheless, no study has yet investigated the role of miR-200c-3p in cisplatin resistance in BTC. Due to the well-established association between miR-200c-3p and EMT-mediated chemoresistance in various cancers, the connection between the miR-200 family and EMT in BTC [62], as well as the link between EMT and overall cisplatin resistance [63], we investigated this pathway in BTC.
First of all, our study was conducted to confirm the relationship between miR-200c-3p and the EMT status in BTC. EMT is the process during which cancer cells lose epithelial features, and reorganize their cytoskeletal architecture and cell shape to acquire a mesenchymal phenotype. This process leads to enhanced cell motility and eventual dissemination [64]. Based on the endogenous expression levels of miR-200c-3p and several epithelial and mesenchymal genes, we could ascribe either a predominantly epithelial expression profile (high miR-200c-3p, high E-cadherin, and low ZEB1) or a predominantly mesenchymal expression profile (low miR-200c-3p, low E-cadherin, and high ZEB1) to different BTC cell lines and found a correlation between the expression of miR-200c-3p and EMT marker genes. Furthermore, miR-200c-3p overexpression experiments resulted in an increased expression of E-cadherin (CDH1) on RNA level and a decreased ZEB1 protein level. Thus, our results are in accordance with the already well-described relationship between miR-200c-3p and EMT-associated genes such as ZEB1.
ZEB1 is a transcriptional factor involved in the regulation of embryonic development and cancer progression. It plays an important role in the regulation of DNA damage repair, cancer cell differentiation, and metastasis. ZEB1 directly binds to the CDH1 promoter, thereby suppressing transcription of the CDH1 gene, which encodes for E-cadherin. E-cadherin is a transmembrane glycoprotein whose main function is to form structures that establish and maintain cell–cell interactions. With the loss of E-cadherin, cell–cell interactions are attenuated or completely lost, leading to EMT [28]. In addition, increasing evidence suggests that ZEB1-mediated EMT is an important process affecting the cancer sensitivity to chemotherapeutics [65,66]. Interestingly, we found that miR-200c-3p mediates cisplatin resistance in BTC, and this apparently occurs independently of its suppressive effect on ZEB1, as knockdown of ZEB1 could not recapitulate the increased cisplatin sensitivity seen after miR-200c-3p overexpression. Our gene expression panel of previously reported cisplatin-resistance-conferring genes included DUSP16 and SFN; both proteins have previously been reported to contribute to cisplatin resistance when upregulated [67,68]. Thus, though not comprehensively characterized in our study, these genes may contribute to the effects described herein in this manuscript.
5. Conclusions
In conclusion, the present study is the first report that miR-200c-3p contributes to cisplatin resistance in BTC. Moreover, we found that this cisplatin resistance is mediated via ZEB1-independent mechanisms. Further studies are necessary to elucidate detailed molecular mechanisms.
Acknowledgments
The authors acknowledge the efforts of Banchob Spira (Khon Kaen University) for depositing the KKU-055 (JCRB1551) cell line and of Seishi Nagamori (National Institute of Infectious Diseases, Tokyo) for depositing the NOZ (JCRB1033) and OZ (JCRB1032) cell lines. Open Access Funding by the Austrian Science Fund (FWF).
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/cancers13163996/s1, Figure S1: Overall survival based on miR-200c-3p expression in cholangiocarcinoma patients, Figure S2: Cisplatin inhibits cell proliferation in a time- and dose-dependent manner, Figure S3: Stable miR-200c-3p overexpression OCUG-1, Figure S4: miR-200c-3p reverses the effect of ZEB1 knockdown, Figure S5: Uncropped Figure 2B, Table S1: Cisplatin resistance gene panel with references, Table S2: Primer sequences for RT-qPCR analysis of mRNA expression.
Author Contributions
Conceptualization, F.P. (Florian Posch), F.P. (Felix Prinz), A.G. and M.P.; writing—original draft preparation, F.P. (Florian Posch), F.P. (Felix Prinz), A.B., C.M., T.K., K.J., C.K., D.A.B., J.M.R., A.G. and M.P.; writing—review and editing, F.P. (Florian Posch), F.P. (Felix Prinz), A.B., C.M., T.K., K.J., C.K., D.A.B., J.M.R., A.G. and M.P.; visualization, F.P. (Florian Posch), F.P. (Felix Prinz), A.B., C.M., T.K., K.J., C.K., D.A.B., J.M.R., A.G. and M.P.; supervision, F.P. (Florian Posch) and M.P.; funding acquisition, F.P. (Florian Posch), A.B. and M.P. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by an institutional START grant of the Medical University of Graz (to F.P. (Florian Posch)) and by BioTechMed-Graz (Lab Rotation Program 2020, to A.B.). The research of M.P. was supported by the Austrian Science Fund FWF (DK-MCD, W 1226). Open Access Funding was provided by the Austrian Science Fund (FWF).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Moeini A., Haber P.K., Sia D. Cell of origin in biliary tract cancers and clinical implications. JHEP Rep. Innov. Hepatol. 2021;3:100226. doi: 10.1016/j.jhepr.2021.100226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang H., Sun P., Baria K. The world-wide incidence of biliary tract cancer (BTC) J. Clin. Oncol. 2020;38:585. doi: 10.1200/JCO.2020.38.4_suppl.585. [DOI] [Google Scholar]
- 3.Ghouri Y., Mian I., Blechacz B. Cancer review: Cholangiocarcinoma. J. Carcinog. 2015;14 doi: 10.4103/1477-3163.151940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Valle J.W., Kelley R.K., Nervi B., Oh D.Y., Zhu A.X. Biliary tract cancer. Lancet. 2021;397:428–444. doi: 10.1016/S0140-6736(21)00153-7. [DOI] [PubMed] [Google Scholar]
- 5.Valle J., Wasan H., Palmer D.H., Cunningham D., Anthoney A., Maraveyas A., Madhusudan S., Iveson T., Hughes S., Pereira S.P., et al. Cisplatin plus Gemcitabine versus Gemcitabine for Biliary Tract Cancer. N. Engl. J. Med. 2010;362:1273–1281. doi: 10.1056/NEJMoa0908721. [DOI] [PubMed] [Google Scholar]
- 6.Morizane C., Ueno M., Ikeda M., Okusaka T., Ishii H., Furuse J. New developments in systemic therapy for advanced biliary tract cancer. Jpn. J. Clin. Oncol. 2018;48:703–711. doi: 10.1093/jjco/hyy082. [DOI] [PubMed] [Google Scholar]
- 7.Nara S., Esaki M., Ban D., Takamoto T., Shimada K., Ioka T., Okusaka T., Ishii H., Furuse J. Adjuvant and neoadjuvant therapy for biliary tract cancer: A review of clinical trials. Jpn. J. Clin. Oncol. 2020;50:1353–1363. doi: 10.1093/jjco/hyaa170. [DOI] [PubMed] [Google Scholar]
- 8.Basourakos S.P., Li L., Aparicio A.M., Corn P.G., Kim J., Thompson T.C. Combination Platinum-based and DNA Damage Response-targeting Cancer Therapy: Evolution and Future Directions. Curr. Med. Chem. 2016;24:1586. doi: 10.2174/0929867323666161214114948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amable L. Cisplatin resistance and opportunities for precision medicine. Pharmacol. Res. 2016;106:27–36. doi: 10.1016/j.phrs.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Chen Y., Gao Y., Zhang K., Li C., Pan Y., Chen J., Wang R., Chen L. MicroRNAs as Regulators of Cisplatin Resistance in Lung Cancer. Cell. Physiol. Biochem. 2015;37:1869–1880. doi: 10.1159/000438548. [DOI] [PubMed] [Google Scholar]
- 11.Chen X., Lu P., Wu Y., Wang D.D., Zhou S., Yang S.J., Shen H.Y., Zhang X.-H., Zhao J.-H., Tang J.-H. MiRNAs-mediated cisplatin resistance in breast cancer. Tumor Biol. 2016;37:12905–12913. doi: 10.1007/s13277-016-5216-6. [DOI] [PubMed] [Google Scholar]
- 12.Carotenuto P., Hedayat S., Fassan M., Cardinale V., Lampis A., Guzzardo V., Vicentini C., Scarpa A., Cascione L., Costantini D., et al. Modulation of Biliary Cancer Chemo-Resistance Through MicroRNA-Mediated Rewiring of the Expansion of CD133+ Cells. Hepatology. 2020;72:982–996. doi: 10.1002/hep.31094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Acunzo M., Romano G., Wernicke D., Croce C.M. MicroRNA and cancer—A brief overview. Adv. Biol. Regul. 2015;57:1–9. doi: 10.1016/j.jbior.2014.09.013. [DOI] [PubMed] [Google Scholar]
- 14.Condrat C.E., Thompson D.C., Barbu M.G., Bugnar O.L., Boboc A., Cretoiu D., Suciu N., Cretoiu S.M., Voinea S.C. miRNAs as Biomarkers in Disease: Latest Findings Regarding Their Role in Diagnosis and Prognosis. Cells. 2020;9:276. doi: 10.3390/cells9020276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mutlu M., Raza U., Saatci Ö., Eyüpoğlu E., Yurdusev E., Şahin Ö. miR-200c: A versatile watchdog in cancer progression, EMT, and drug resistance. J. Mol. Med. 2016;94:629–644. doi: 10.1007/s00109-016-1420-5. [DOI] [PubMed] [Google Scholar]
- 16.Chen J., Tian W., He H., Chen F., Huang J., Wang X., Chen Z. Downregulation of miR-200c-3p contributes to the resistance of breast cancer cells to paclitaxel by targeting SOX2. Oncol. Rep. 2018;40:3821–3829. doi: 10.3892/or.2018.6735. [DOI] [PubMed] [Google Scholar]
- 17.Zhang M., Wang F., Xiang Z., Huang T., Zhou W.B. LncRNA XIST promotes chemoresistance of breast cancer cells to doxorubicin by sponging miR-200c-3p to upregulate ANLN. Clin. Exp. Pharmacol. Physiol. 2020;47:1464–1472. doi: 10.1111/1440-1681.13307. [DOI] [PubMed] [Google Scholar]
- 18.Wang H.Y., Liu Y.N., Wu S.G., Hsu C.L., Chang T.H., Tsai M.F., Lin Y.T., Shih J.Y. MiR-200c-3p suppression is associated with development of acquired resistance to epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors in EGFR mutant non-small cell lung cancer via a mediating epithelial-to-mesenchymal transition (EMT) process. Cancer Biomark. 2020;28:351–363. doi: 10.3233/CBM-191119. [DOI] [PubMed] [Google Scholar]
- 19.Ma Q., Niu R., Huang W., Da L., Tang Y., Jiang D., Xi Y., Zhang C. Long Noncoding RNA PTPRG Antisense RNA 1 Reduces Radiosensitivity of Nonsmall Cell Lung Cancer Cells Via Regulating MiR-200c-3p/TCF4. Technol. Cancer Res. Treat. 2020;19:1533033820942615. doi: 10.1177/1533033820942615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polley E., Kunkel M., Evans D., Silvers T., Delosh R., Laudeman J., Ogle C., Reinhart R., Selby M., Connelly J., et al. Small Cell Lung Cancer Screen of Oncology Drugs, Investigational Agents, and Gene and microRNA Expression. J. Natl. Cancer Inst. 2016;108 doi: 10.1093/jnci/djw122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li M., Gao M., Xie X., Zhang Y., Ning J., Liu P., Gu K. MicroRNA-200c reverses drug resistance of human gastric cancer cells by targeting regulation of the NER-ERCC3/4 pathway. Oncol. Lett. 2019;18:145–152. doi: 10.3892/ol.2019.10304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hamano R., Miyata H., Yamasaki M., Kurokawa Y., Hara J., Moon J.H., Nakajima K., Takiguchi S., Fujiwara Y., Mori M., et al. Overexpression of miR-200c induces chemoresistance in esophageal cancers mediated through activation of the Akt signaling pathway. Clin. Cancer Res. 2011;17:3029–3038. doi: 10.1158/1078-0432.CCR-10-2532. [DOI] [PubMed] [Google Scholar]
- 23.Liu J., Zhang X., Huang Y., Zhang Q., Zhou J., Zhang X., Wang X. mir-200b and mir-200c co-contribute to the cisplatin sensitivity of ovarian cancer cells by targeting DNA methyltransferases. Oncol. Lett. 2019;17:1453–1460. doi: 10.3892/ol.2018.9745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu Z., Zhou Y., Liang G., Ling Y., Tan W., Tan L., Andrews R., Zhong W., Zhang X., Song E., et al. Circular RNA hsa_circ_001783 regulates breast cancer progression via sponging miR-200c-3p. Cell Death Dis. 2019;10:55. doi: 10.1038/s41419-018-1287-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang J., Zhang H., Qin Y., Chen C., Yang J., Song N., Gu M. MicroRNA-200c-3p/ZEB2 loop plays a crucial role in the tumor progression of prostate carcinoma. Ann. Transl. Med. 2019;7:141. doi: 10.21037/atm.2019.02.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li R.-H., Chen M., Liu J., Shao C.-C., Guo C.-P., Wei X.-L., Li Y.-C., Huang W.-H., Zhang G.-J. Long noncoding RNA ATB promotes the epithelial−mesenchymal transition by upregulating the miR-200c/Twist1 axe and predicts poor prognosis in breast cancer. Cell Death Dis. 2018;9:1171. doi: 10.1038/s41419-018-1210-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhuo M., Yuan C., Han T., Cui J., Jiao F., Wang L. A novel feedback loop between high MALAT-1 and low miR-200c-3p promotes cell migration and invasion in pancreatic ductal adenocarcinoma and is predictive of poor prognosis. BMC Cancer. 2018;18:1032. doi: 10.1186/s12885-018-4954-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bure I.V., Nemtsova M.V., Zaletaev D.V. Roles of e-cadherin and noncoding rnas in the epithelial–mesenchymal transition and progression in gastric cancer. Int. J. Mol. Sci. 2019;20:2870. doi: 10.3390/ijms20122870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Díaz-López A., Moreno-Bueno G., Cano A. Role of microRNA in epithelial to mesenchymal transition and metastasis and clinical perspectives. Cancer Manag. Res. 2014;6:205–216. doi: 10.2147/CMAR.S38156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee J.Y., Kong G. Roles and epigenetic regulation of epithelial–mesenchymal transition and its transcription factors in cancer initiation and progression. Cell. Mol. Life Sci. 2016;73:4643–4660. doi: 10.1007/s00018-016-2313-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kiesslich T., Pichler M., Neureiter D. Epigenetic control of epithelial-mesenchymal-transition in human cancer. Mol. Clin. Oncol. 2013;1:3–11. doi: 10.3892/mco.2012.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scherdin G., Garbrecht K.M. In vitro interaction of α-difluoromethylornithine (DFMO) and human recombinant interferon-a (rIFN-a) on human cancer cell lines. Immunobiology. 1987;175:1–143. [Google Scholar]
- 33.Saijyo S., Kudo T., Suzuki M., Katayose Y., Shinoda M., Muto T., Fukuhara K., Suzuki T., Matsuno S. Establishment of a New Extrahepatic Bile Duct Carcinoma Cell Line, TFK-1. Tohoku J. Exp. Med. 1995;177:61–71. doi: 10.1620/tjem.177.61. [DOI] [PubMed] [Google Scholar]
- 34.Miyagiwa M., Ichida T., Tokiwa T., Sato J., Sasaki H. A new human cholangiocellular carcinoma cell line (HuCC-T1) producing carbohydrate antigen 19/9 in serum-free medium. Vitr. Cell. Dev. Biol. 1989;25:503–510. doi: 10.1007/BF02623562. [DOI] [PubMed] [Google Scholar]
- 35.Kusaka Y., Tokiwa T., Sato J. Establishment and characterization of a cell line from a human cholangiocellular carcinoma. Res. Exp. Med. 1988;188:367–375. doi: 10.1007/BF01851205. [DOI] [PubMed] [Google Scholar]
- 36.Sripa B., Leungwattanawanit S., Nitta T., Wongkham C., Bhudhisawasdi V., Puapairoj A., Sripa C., Miwa M. Establishment and characterization of an opisthorchiasis-associated cholangiocarcinoma cell line (KKU-100) World J. Gastroenterol. 2005;11:3392–3397. doi: 10.3748/wjg.v11.i22.3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sripa B., Seubwai W., Vaeteewoottacharn K., Sawanyawisuth K., Silsirivanit A., Kaewkong W., Muisuk K., Dana P., Phoomak C., Lert-itthiporn W., et al. Functional and genetic characterization of three cell lines derived from a single tumor of an Opisthorchis viverrini-associated cholangiocarcinoma patient. Hum. Cell. 2020;33:695–708. doi: 10.1007/s13577-020-00334-w. [DOI] [PubMed] [Google Scholar]
- 38.Homma S., Hasumura S., Nagamori S., Kameda H. Establishment and characterization of a human gall bladder carcinoma cell line NOZ. Hum. Cell Off. J. Hum. Cell Res. Soc. 1988;1:95–97. [PubMed] [Google Scholar]
- 39.Yamada N., Chung Y.S., Ohtani H., Ikeda T., Onoda N., Sawada T., Nishiguchi Y., Hasuma T., Sowa M. Establishment and characterization of a new human gallbladder carcinoma cell line (OCUG-1) producing TA-4. Int. J. Oncol. 1997;10:1251–1255. doi: 10.3892/ijo.10.6.1251. [DOI] [PubMed] [Google Scholar]
- 40.Homma S., Nagamori S., Fujise K., Yamazaki K., Hasumura S., Sujino H., Matsuura T., Shimizu K., Kameda H., Takaki K. Human bile duct carcinoma cell line producing abundant mucin in vitro. Gastroenterol. Jpn. 1987;22:474–479. doi: 10.1007/BF02773816. [DOI] [PubMed] [Google Scholar]
- 41.Maruyama M., Kobayashi N., Westerman K.A., Sakaguchi M., Allain J.E., Totsugawa T., Okitsu T., Fukazawa T., Weber A., Stolz D.B., et al. Establishment of a highly differentiated immortalized human cholangiocyte cell line with SV40T and hTERT. Transplantation. 2004;77:446–451. doi: 10.1097/01.TP.0000110292.73873.25. [DOI] [PubMed] [Google Scholar]
- 42.Motulsky H.J., Brown R.E. Detecting outliers when fitting data with nonlinear regression—A new method based on robust nonlinear regression and the false discovery rate. BMC Bioinform. 2006;7:123. doi: 10.1186/1471-2105-7-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhan M., Zhao X., Wang H., Chen W., Xu S., Wang W., Shen H., Huang S., Wang J. miR-145 sensitizes gallbladder cancer to cisplatin by regulating multidrug resistance associated protein 1. Tumor Biol. 2016;37:10553–10562. doi: 10.1007/s13277-016-4957-6. [DOI] [PubMed] [Google Scholar]
- 44.Li Q., Xia X., Ji J., Ma J., Tao L., Mo L., Chen W. MiR-199a-3p enhances cisplatin sensitivity of cholangiocarcinoma cells by inhibiting mTOR signaling pathway and expression of MDR1. Oncotarget. 2017;8:33621–33630. doi: 10.18632/oncotarget.16834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li M., Chen W., Zhang H., Zhang Y., Ke F., Wu X., Zhang Y., Weng M., Liu Y., Gong W. MiR-31 regulates the cisplatin resistance by targeting Src in gallbladder cancer. Oncotarget. 2016;7:83060–83070. doi: 10.18632/oncotarget.13067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang D., Zhan M., Chen T., Chen W., Zhang Y., Xu S., Yan J., Huang Q., Wang J. MIR-125b-5p enhances chemotherapy sensitivity to cisplatin by down-regulating Bcl2 in gallbladder cancer. Sci. Rep. 2017;7:1–9. doi: 10.1038/srep43109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Danarto R., Astuti I., Umbas R., Haryana S.M. Urine miR-21-5p and miR-200c-3p as potential non-invasive biomarkers in patients with prostate cancer. Turk. J. Urol. 2020;46:26–30. doi: 10.5152/tud.2019.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xia L., Han Q., Chi C., Zhu Y., Pan J., Dong B., Huang Y., Xia W., Xue W., Sha J. Transcriptional regulation of PRKAR2B by miR-200b-3p/200c-3p and XBP1 in human prostate cancer. Biomed. Pharmacother. 2020;124:109863. doi: 10.1016/j.biopha.2020.109863. [DOI] [PubMed] [Google Scholar]
- 49.Li T., Zhao P., Li Z., Wang C.C., Wang Y.L., Gu Q. MIR-200c-3p suppresses the proliferative, migratory, and invasive capacities of nephroblastoma cells via targeting FRS2. Biopreserv. Biobank. 2019;17:444–451. doi: 10.1089/bio.2019.0009. [DOI] [PubMed] [Google Scholar]
- 50.Li M., Gu K., Liu W., Xie X., Huang X. MicroRNA-200c as a prognostic and sensitivity marker for platinum chemotherapy in advanced gastric cancer. Oncotarget. 2017;8:51190–51199. doi: 10.18632/oncotarget.17087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cao W., Suna J. MicroRNA-200c promotes tumor cell proliferation and migration by directly targeting dachshund family transcription factor 1 by the Wnt/β-catenin signaling pathway in nasopharyngeal carcinoma. Anticancer. Drugs. 2019;30:218–224. doi: 10.1097/CAD.0000000000000713. [DOI] [PubMed] [Google Scholar]
- 52.Kawakubo-Yasukochi T., Morioka M., Hazekawa M., Yasukochi A., Nishinakagawa T., Ono K., Kawano S., Nakamura S., Nakashima M. miR-200c-3p spreads invasive capacity in human oral squamous cell carcinoma microenvironment. Mol. Carcinog. 2018;57:295–302. doi: 10.1002/mc.22744. [DOI] [PubMed] [Google Scholar]
- 53.Ardila H.J., Sanabria-Salas M.C., Meneses X., Rios R., Huertas-Salgado A., Serrano M.L. Circulating miR-141-3p, miR-143-3p and miR-200c-3p are differentially expressed in colorectal cancer and advanced adenomas. Mol. Clin. Oncol. 2019;11:201–207. doi: 10.3892/mco.2019.1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang W., Wu L.-r., Li C., Zhou X., Liu P., Jia X., Chen Y., Zhu W. Five serum microRNAs for detection and predicting of ovarian cancer. Eur. J. Obstet. Gynecol. Reprod. Biol. X. 2019;3:100017. doi: 10.1016/j.eurox.2019.100017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Srivastava A., Moxley K., Ruskin R., Dhanasekaran D.N., Zhao Y.D., Ramesh R. A Non-invasive Liquid Biopsy Screening of Urine-Derived Exosomes for miRNAs as Biomarkers in Endometrial Cancer Patients. AAPS J. 2018;20:1–11. doi: 10.1208/s12248-018-0220-y. [DOI] [PubMed] [Google Scholar]
- 56.Shi S.J., Wang L.J., Yu B., Li Y.H., Jin Y., Bai X.Z. LncRNA-ATB promotes trastuzumab resistance and invasionmetastasis cascade in breast cancer. Oncotarget. 2015;6:11652–11663. doi: 10.18632/oncotarget.3457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chang I., Mitsui Y., Fukuhara S., Gill A., Wong D.K., Yamamura S., Shahryari V., Laura Tabatabai Z., Dahiya R., Shin D.M., et al. Loss of miR-200c up-regulates CYP1B1 and confers docetaxel resistance in renal cell carcinoma. Oncotarget. 2015;6:7774–7787. doi: 10.18632/oncotarget.3484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li Z., Shen J., Chan M.T.V., Wu W.K.K. The role of microRNAs in intrahepatic cholangiocarcinoma. J. Cell. Mol. Med. 2017;21:177–184. doi: 10.1111/jcmm.12951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang J., Jin Y., Li S., Song Q., Tang P. Identification of microRNAs associated with the survival of patients with gallbladder carcinoma. J. Int. Med. Res. 2020;48:1–8. doi: 10.1177/0300060520918061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shen L., Chen G., Xia Q., Shao S., Fang H. Exosomal miR-200 family as serum biomarkers for early detection and prognostic prediction of cholangiocarcinoma. Int. J. Clin. Exp. Pathol. 2019;12:3870–3876. [PMC free article] [PubMed] [Google Scholar]
- 61.Li J., Guan C., Hu Z., Liu L., Su Z., Kang P., Jiang X., Cui Y. Yin Yang 1-induced LINC00667 up-regulates pyruvate dehydrogenase kinase 1 to promote proliferation, migration and invasion of cholangiocarcinoma cells by sponging miR-200c-3p. Hum. Cell. 2021;34:187–200. doi: 10.1007/s13577-020-00448-1. [DOI] [PubMed] [Google Scholar]
- 62.Urbas R., Mayr C., Klieser E., Fuereder J., Bach D., Stättner S., Primavesi F., Jaeger T., Stanzer S., Ress A.L., et al. Relevance of microRNA200 family and microRNA205 for epithelial to mesenchymal transition and clinical outcome in biliary tract cancer patients. Int. J. Mol. Sci. 2016;17:2053. doi: 10.3390/ijms17122053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ashrafizadeh M., Zarrabi A., Hushmandi K., Kalantari M., Mohammadinejad R., Javaheri T., Sethi G. Association of the Epithelial–Mesenchymal Transition (EMT) with Cisplatin Resistance. Int. J. Mol. Sci. 2020;21:4002. doi: 10.3390/ijms21114002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nieszporek A., Skrzypek K., Adamek G., Majka M. Molecular mechanisms of epithelial to mesenchymal transition in tumor metastasis. Acta Biochim. Pol. 2019;66:509–520. doi: 10.18388/abp.2019_2899. [DOI] [PubMed] [Google Scholar]
- 65.Zhang Y., Xu L., Li A., Han X. The roles of ZEB1 in tumorigenic progression and epigenetic modifications. Biomed. Pharmacother. 2019;110:400–408. doi: 10.1016/j.biopha.2018.11.112. [DOI] [PubMed] [Google Scholar]
- 66.Drápela S., Bouchal J., Jolly M.K., Culig Z., Souček K. ZEB1: A Critical Regulator of Cell Plasticity, DNA Damage Response, and Therapy Resistance. Front. Mol. Biosci. 2020;7:36. doi: 10.3389/fmolb.2020.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Low H.B., Wong Z.L., Wu B., Kong L.R., Png C.W., Cho Y.-L., Li C.-W., Xiao F., Xin X., Yang H., et al. DUSP16 promotes cancer chemoresistance through regulation of mitochondria-mediated cell death. Nat. Commun. 2021;12:1–16. doi: 10.1038/s41467-021-22638-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.KK L., KT C., MY C., HK W., EY F., HY L., W T., LN T., DK T., RW S., et al. 14-3-3σ confers cisplatin resistance in esophageal squamous cell carcinoma cells via regulating DNA repair molecules. Tumour Biol. 2016;37:2127–2136. doi: 10.1007/S13277-015-4018-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.