Abstract
Background:
Controversy remains regarding the optimal technique for tibial fixation of soft tissue grafts in anterior cruciate ligament (ACL) reconstruction.
Purpose/Hypothesis:
To compare the biomechanical outcomes of a novel transtibial tubercle fixation technique with those of a commonly utilized interference screw fixation at the tibial site. Our hypothesis was that transtibial tubercle fixation achieves higher ultimate failure loads than interference screw fixation.
Study Design:
Controlled laboratory study.
Methods:
We used 24 matched porcine tibias and digital extensor tendons, from which 12 grafts and tibial tunnels were prepared using the novel transtibial tubercle fixation technique and 12 were prepared using the interference screw fixation technique. The specimens underwent a cyclic loading test (50-250 N applied for 1000 cycles at a frequency of 1 Hz), followed by a load-to-failure test. The slippage, stiffness, and ultimate failure loads were compared between the techniques.
Results:
No differences in slippage were found during the cyclic loading test, and no graft fixation or tibial complex failures occurred during cyclic testing in either group. The transtibial tubercle fixation technique had higher ultimate failure loads (mean ± SD, 756.28 ± 123.43 N) as compared with interference screw fixation (602.15 ± 81.62 N; P < .05). The grafts in the transtibial tubercle fixation group were less stiff than those in the interference screw fixation group (84.43 vs 101.23 N/mm; P < .05).
Conclusion:
Transtibial tubercle fixation achieved higher ultimate failure loads than interference screw fixation in the load-to-failure test.
Clinical Relevance:
The novel transtibial tubercle fixation technique compared favorably with interference screw fixation during ACL reconstruction. This technique does not require hardware, has a low cost, theoretically eliminates the risk of complications associated with hardware implantation (eg, graft damage and pain attributed to retained hardware requiring removal), and is relatively easy to perform.
Keywords: biomechanical study, anterior cruciate ligament reconstruction, tibial fixation, interference screw, transtibial tubercle fixation
The anterior cruciate ligament (ACL) is one of the most commonly injured ligamentous structures of the knee and often requires reconstruction when torn.20 Grafts selected for use in ACL reconstruction include autografts, allografts, bone–patellar tendon–bone grafts, and hamstring grafts, among others. The outcomes of ACL reconstruction are good to excellent in approximately 90% of patients.8,19,24,31,32,34,42 Despite these results, the optimal graft fixation technique remains controversial, particularly for soft tissue grafts.§ The fixation construct must be sufficiently strong and stiff to resist slippage and avoid failure during early accelerated postoperative rehabilitation. The tibia comprises softer bone than the femur; therefore, the weakest point in the construct during the initial postoperative phase after ACL reconstruction is at the tibial fixation site.4,17
There are many options available for tibial fixation in ACL reconstruction using soft tissue grafts, such as interference screws,2,3,7,17,22,23,38,39 cross pins,38 suspensory devices,2,9,21,22,39 WasherLoc systems,13 and IntraFix expansion systems.6,14 Interference screws are widely used for graft fixation to the tibia, with good to excellent results reported in most patients6,13,16; however, many doctors have concerns related to interference screw fixation, including concerns regarding graft damage during screw insertion and a small tendon-to-bone contact area for biological graft incorporation.2,21 The transosseous suture technique was introduced for the repair of quadriceps tendon ruptures or medial patellofemoral ligament reconstruction,43 and we applied this fixation technique in ACL reconstruction.
The purpose of this study was to compare the biomechanical outcomes of a novel transtibial tubercle fixation technique for soft tissue graft fixation with those of commonly utilized interference screw fixation at the tibial site. Our hypothesis was that transtibial tubercle fixation achieves higher ultimate failure loads than interference screw fixation.
Methods
This study was conducted in May 2019 at the materials testing laboratory of China Medical University. We used 24 fresh-frozen porcine tibias and digital extensor tendons (12 matched pairs) from healthy male pigs aged 12 months and weighing 90 kg. The porcine model was similar to that used by Mayr et al.21,22 The digital extensor tendons of the pigs were used for the grafts because the structural properties of these tendons are similar to those of the human hamstring tendon2,5,10,18,21,36; in addition, the bone density of porcine tibias is approximately the same as that of young human bone.21 The study protocol was approved by an institutional review board.
Specimen Preparation
The methods for preparing the graft and tibial tunnel were similar for the 2 fixation methods. All specimens were stored at –80°C. Before testing, the specimens were thawed at room temperature for 12 hours. All of the specimens underwent 1 freeze-thaw cycle before experimental testing. A double-looped porcine tendon graft was prepared on a table; the graft was folded in half (the folded graft length was approximately 70 mm) and thinned to 8 mm in diameter. Three No. 2 UltraBraid sutures (Smith & Nephew) were used to sew 30 mm of each tendon together on both ends using a criss-cross stitch. For all porcine tibias, a tunnel with a diameter of 8 mm and length of 4 cm was prepared in the anteromedial tibia. The specimens were randomly assigned to 2 groups, each of which included 12 specimens: the interference screw fixation group and the new transtibial tubercle fixation group (Figure 1).
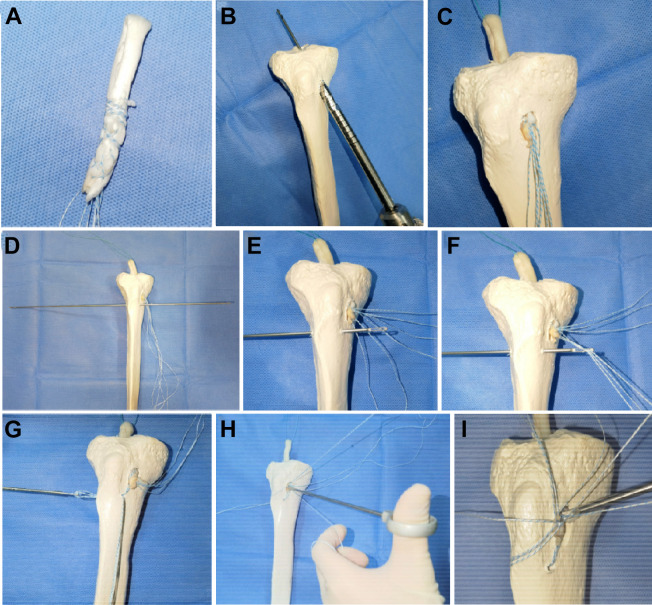
Figure 1.
Computer drawing of each type of fixation.
Transtibial Tubercle Fixation
The tendon was whipstitched with 3 No. 2 UltraBraid sutures approximately 30 mm distal to the graft whipstitches. Figure 2 demonstrates this new tibial fixation technique. The tendinous portion of the graft was pulled into the tibial tunnel. An eyelet-passing pin was drilled 1 cm distal to the tibial tunnel and 1 cm posterior to the anterior tibial cortex. The musculature of the anterior compartment was then cleared off to retrieve the pin. Half of these sutures (3 sutures on 1 side) were passed to the lateral side with the eyelet-passing pin; then, the sutures on the medial side and the lateral transosseous ends of the sutures were tied at the proximal tibia with a surgeon’s knot, followed by 5 alternating half-hitch knots made with a shoulder knot pusher.
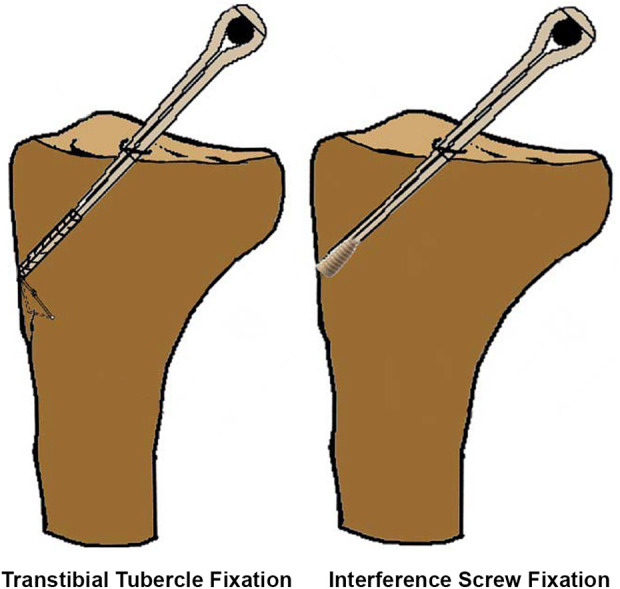
Figure 2.
(A) The tendons were whipstitched with 3 high-strength sutures. (B) The tibial tunnel was created with an 8-mm reamer, and a tibial tunnel that was 8 mm in diameter and 40 mm in length was drilled. (C) The tendinous portion of the graft was pulled into the tibial tunnel. (D) An eyelet-passing pin was drilled transversely 1 cm distal to the tibial tunnel (parallel to the tibial joint line) and 1 cm posterior to the anterior tibial cortex. (E-G) The sutures were passed to the lateral side with the eyelet-passing pin. (H, I) The transosseous sutures were tied at the tibia.
Interference Screw Fixation
The diameter of the tibial tunnel was drilled to be 8 mm, which was consistent with the diameter of the graft. An 8 × 25–mm interference screw (BioScrew; ConMed Linvatec) was inserted between the graft and the posterior wall of the tibial tunnel until it was contained within the tibial tunnel (Figure 1).
Biomechanical Testing Using Animal Tissue
The 2 graft fixation techniques were tested biomechanically using cyclic loading and a load-to-failure test. The biomechanical test protocols were similar to those described in previous studies.21,36 All tensile strength tests were performed using an ElectroPuls E3000 unit (Instron). The tibias were fixed in a custom jig (Figure 3). The looped end of the double-looped porcine tendon graft was fixed to a bar attached to the base of the materials testing machine. The distance between the bar and tibial articulating surface was fixed at the length of the graft (3 cm), as if it were implanted in a reconstructed knee (Figure 4). The tibial bone tunnel was parallel to the axis of the testing machine. The tensile force applied to the graft was in line with the tibial tunnel, in accordance with the worst-case scenario for graft testing.21
Figure 3.
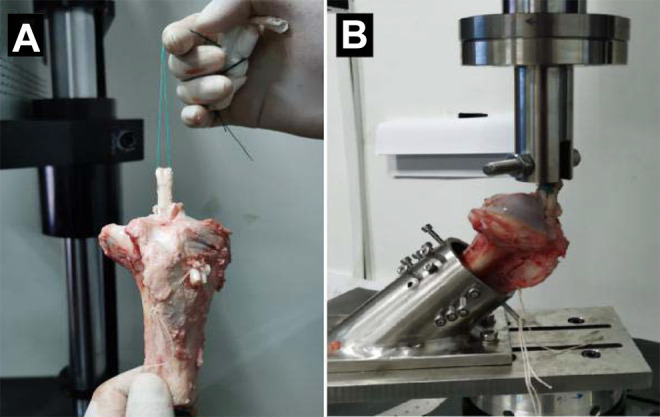
Testing setup. (A) The graft was fixed by transosseous sutures. (B) Then the tibia was fixed by a custom-made jig.
Figure 4.
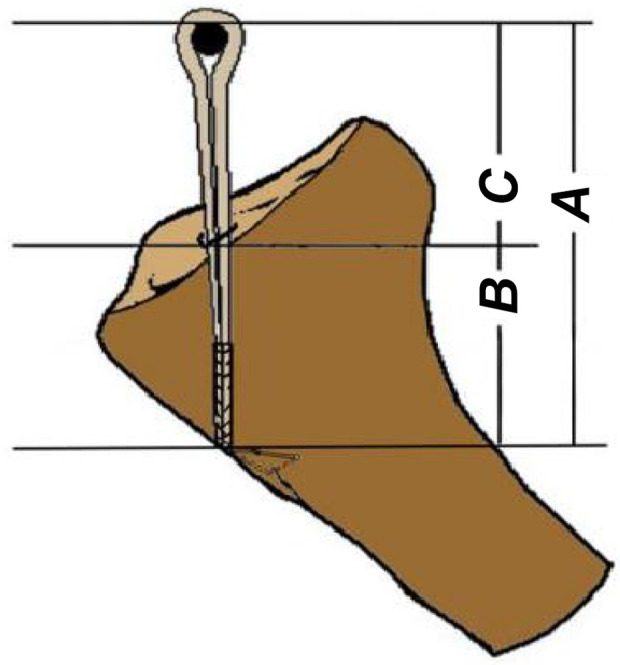
Diagram depicting the method used for this study. The double-looped graft was attached to the material-testing machine. A = total graft length, B = length of the graft in the tibial tunnel, and C = length of the intra-articular portion of the graft. A length of 30 mm was chosen, as the length of the intra-articular portion of the graft was 30 mm. The mean length of the free graft between the edge of the tibia and the clamp was 3 cm, which was similar to the normal mean distance of 31 to 35 mm of the anterior cruciate ligament in vivo.
Each tibial complex treated by graft fixation was preconditioned at 50 N for 5 minutes; then, cyclic loads between 50 and 250 N were applied for 1000 cycles at a frequency of 1 Hz.6,21,36,39 This protocol mimicked the ACL loads incurred during normal walking. The graft slippage of each tibial complex treated by graft fixation was measured continuously. The magnitude of graft slippage (in mm) was defined as the distance between the lines: the grafts were marked with ink at the tunnel exit points and again after cyclic tensile loading, and the distance was measured with digital calipers. Afterward, the tibial complexes treated by graft fixation that did not fail the cyclic loading test were loaded to failure at 50 mm/min after the cyclic tensile loading test was completed17,21; the ultimate failure load (N) was determined. The pullout stiffness (in N/mm) was calculated as the slope of the linear portion of the load-elongation curve. The failure modes were noted. The extent of graft elongation (in mm) after the cyclic loading test was recorded. The tendons were moistened with a saline spray during preparation and testing.
Statistical Analysis
The initial data of 12 matched pairs of specimens were used for primary analysis. The data analysis was performed by the same experienced examiner and biostatistician (T.S.). Statistical analysis was performed using SPSS Version 21.0 (IBM). Continuous variables are expressed as mean and standard deviation. The Kolmogorov-Smirnov test was used to determine whether the data were normally distributed within the groups. The chi-square test was used in the case of nonparametric variance. The Student t test was used to compare the stiffness, elongation, and ultimate failure loads between groups. The significance level was set at P < .05.
Results
After the cyclic loading test, the mean magnitude of graft slippage was 2.98 ± 0.57 mm in the transtibial tubercle fixation group and 2.82 ± 0.46 mm in the interference screw fixation group (P = .48) after 1000 cycles (Table 1). No significant difference in graft slippage was observed between the groups. No graft fixation or tibial complex failures occurred during cyclic testing in either group.
TABLE 1.
Comparison of the Structural Properties of the Transtibial Tubercle Fixation Group and Interference Screw Fixation Groupa
| Structural Property | Transtibial Tubercle Fixation | Interference Screw Fixation | t Value | P Value |
|---|---|---|---|---|
| Slippage, mm | 2.98 ± 0.57 | 2.82 ± 0.46 | 0.719 | .48 |
| Stiffness, N/mm | 84.43 ± 14.07 | 101.23 ± 17.36 | –2.604 | .016 |
| Ultimate load, N | 756.28 ± 123.43 | 602.15 ± 81.62 | 3.608 | .02 |
aData are reported as mean ± SD. Bold P values indicate statistically significant difference between groups (P < .05).
Grafts with transtibial tubercle fixation showed higher ultimate failure loads than grafts with screw fixation (756.28 ± 123.43 vs 602.15 ± 81.62 N; P = .02). Nevertheless, in both groups, the fixation strength (>450 N) was suitable for early rehabilitation after ACL reconstruction.
The median stiffness was 84.43 ± 14.07 N/mm in the transtibial tubercle fixation group and 101.23 ± 17.36 N/mm in the interference screw fixation group, and the difference was statistically significant (P = .016).
All tibial complexes treated by graft fixation underwent the cyclic loading test. No tibial complexes treated by graft fixation failed after the cyclic loads were applied. The failure mechanism in the transtibial tubercle fixation group was suture breakage in 6 cases, tendon graft rupture near the tibial side in 3 cases and near the custom jig side in 2 cases, and tibial fracture on the tibial side in 1 case (1/12; 8%). The mechanism of failure for the grafts in the interference screw fixation group was graft slippage outside of the tibial tunnel in 9 cases and graft rupture in 3 cases.
Discussion
For ACL reconstruction, the ideal soft tissue fixation technique remains controversial. In the present study, we compared the biomechanical outcomes of a new tibial fixation technique performed with transosseous sutures (No. 2 high-strength sutures) and conventional graft fixation using tibial interference screws during ACL reconstruction. The initial hypothesis was confirmed. The most important finding of this study was that the ultimate failure load for the new transtibial tubercle fixation technique was 756.28 ± 123.43 N, greater than that of interference screw fixation (602.15 ± 81.62 N). Therefore, this transosseous suture fixation technique may be a very effective and useful method for ACL reconstruction in clinical practice.
Graft fixation is important for ACL reconstruction. The method of graft fixation should provide sufficient strength for patients to perform early range of motion exercises, thereby reducing postoperative stiffness, allow weightbearing on the knee joint in the early postoperative period, and maintain the stability of the knee joint as the graft heals. The estimated daily load on ACL grafts during intensive rehabilitation is 450 to 500 N.26,27,33 In both groups, the fixation strength far exceeded 500 N. Therefore, both techniques appear to suitable for soft tissue graft tibial fixation.
Several biomechanical studies have examined the strength provided by different types of soft tissue tibial fixation techniques.∥ In these biomechanical studies, the mean reported ultimate failure loads for interference screw fixation ranged from 537 to 937 N.2,17,21,34 Pasque and de la Garza29 published a technical note on transtibial tubercle fixation without hardware for ACL and posterior cruciate ligament reconstruction. Our technique differs from that in the Pasque et al study. In their technique, the sutures were passed through the 2 transverse drill holes below the tibial tunnel, and both ends of the graft sutures from the medial and lateral sides were fixed at the tibia. Furthermore, no biomechanical tests comparing this technique with the standard fixation technique were reported in the Pasque et al study. In this study, the new transtibial tubercle fixation technique yielded a higher ultimate tensile load than interference screw fixation (756 vs 602 N). The transosseous suture and interference screw techniques both achieved safe fixation of the graft to the tibial attachment. In our study, there was no significant difference between the fixation techniques with regard to slippage during the cyclic loading test. The median stiffness in the transtibial tubercle fixation group was lower than that in the interference screw fixation group. However, because of the lack of clinical results, it is difficult to conclude that the new method is better than that involving conventional interference screws. Decreased overall graft stiffness may lead to decreased total graft deformation. In the future, studies on knee ligament reconstruction techniques with the new fixation technique should assess mid- to long-term stability.
The novel “no-hardware” technique for ACL reconstruction at the tibial site offers several potential advantages over fixation involving conventional interference screws. (1) The ultimate load is higher. (2) When no fixation materials are used, the tendon-bone contact area is larger than that with the use of interference screws. (3) The overall cost is lower. At our institution, the cost for interference screws is approximately $800, plus the cost of 2 No. 2 FiberWire sutures (approximately $50 per suture; Arthrex). The transtibial tubercle fixation technique requires only 5 No. 2 FiberWire sutures. This technique may be used instead of techniques involving interference screws or suspensory devices with adjustable or fixed loops at the tibial site. (4) Theoretically, this novel fixation technique may be preferable for use in skeletally immature patients because there are no implants in the bone tunnel. (5) This technique can theoretically also be used for ACL revision surgery with tibial tunnel widening at the tibial site or for hybrid fixation on the tibial side in addition to tibial interference screw fixation in clinical practice.
This study has some limitations. (1) We assessed the slippage, stiffness, and maximum failure force in 1 direction only. This in vitro study is not similar to an in vivo study because the tibial tunnel does not exhibit pure axial alignment. (2) The porcine bone specimens used in the present study do not exactly mimic young human bone or the human hamstring tendon in biomechanical tests. However, they are commonly used because their structural and material properties are similar to those of human hamstring tendons and have a homogeneous graft diameter and length.2,5,10,18,21,36 The bone mineral density of the porcine proximal tibia (1.42 g/cm2) is more similar to that of a young human proximal tibia (1.30 g/cm2) than to an older cadaveric tibia (0.30 g/cm2).21,25,29 In fact, we use this method for secondary fixation in ACL revision with tunnel widening in clinical practice. This fixation method does not require extensive soft tissue dissection of the anterolateral tibia in the clinic (using an eyelet-passing pin, the surgeon passes high-strength sutures subcutaneously through the tibial tubercle as closely as possible to the bone, using surgical curved forceps, to exit via the lateral patellar skin incision). (3) This technique requires an additional incision lateral to the tibial tubercle. (4) The patients may experience some discomfort with the sutures or knot passing over the front of the tibial tubercle. (5) More high-quality trials and randomized controlled trials with clinical outcomes, such as anterior stability, the subjective International Knee Documentation Committee score, and range of motion, are needed.
Conclusion
The results of this biomechanical study suggest that this novel transosseous suture fixation technique yields higher ultimate failure loads than conventional interference screw fixation. We believe that our technique is a potential and useful alternative method for ACL reconstruction using soft tissue grafts.
Footnotes
Final revision submitted December 26, 2020; accepted February 9, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from China Medical University (protocol No. KT2020120).
References
- 1.Aga C, Rasmussen MT, Smith SD, et al. Biomechanical comparison of interference screws and combination screw and sheath devices for soft tissue anterior cruciate ligament reconstruction on the tibial side. Am J Sports Med. 2013;41(4):841–848. [DOI] [PubMed] [Google Scholar]
- 2.Ahmad CS, Gardner TR, Groh M, et al. Mechanical properties of soft tissue femoral fixation devices for anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(3):635–640. [DOI] [PubMed] [Google Scholar]
- 3.Bartz RL, Mossoni K, Tyber J, et al. A biomechanical comparison of initial fixation strength of 3 different methods of anterior cruciate ligament soft tissue graft tibial fixation: resistance to monotonic and cyclic loading. Am J Sports Med. 2007;35(6):949–954. [DOI] [PubMed] [Google Scholar]
- 4.Brand JC, Jr, Pienkowski D, Steenlage E, et al. Interference screw fixation strength of a quadrupled hamstring tendon graft is directly related to bone mineral density and insertion torque. Am J Sports Med. 2000;28(5):705–710. [DOI] [PubMed] [Google Scholar]
- 5.Brown GA, Pena F, Grontvedt T, et al. Fixation strength of interference screw fixation in bovine, young human, and elderly human cadaver knees: influence of insertion torque, tunnelbone block gap, and interference. Knee Surg Sports Traumatol Arthrosc. 1996;3(4):238–244. [DOI] [PubMed] [Google Scholar]
- 6.Caborn DN, Brand JC, Jr, Nyland J, et al. A biomechanical comparison of initial soft tissue tibial fixation devices: the Intrafix versus a tapered 35-mm bioabsorbable interference screw. Am J Sports Med. 2004;32(4):956–961. [DOI] [PubMed] [Google Scholar]
- 7.Carulli C, Matassi F, Soderi S, et al. Resorbable screw and sheath versus resorbable interference screw and staples for ACL reconstruction: a comparison of two tibial fixation methods. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1264–1271. [DOI] [PubMed] [Google Scholar]
- 8.Chen L, Cooley V, Rosenberg T. ACL reconstruction with hamstring tendon. Orthop Clin North Am. 2003;34(1):9–18. [DOI] [PubMed] [Google Scholar]
- 9.Chiang ER, Chen KH, Chih-Chang Lin A, et al. Comparison of tunnel enlargement and clinical outcome between bioabsorbable interference screws and cortical button-post fixation in arthroscopic double-bundle anterior cruciate ligament reconstruction: a prospective, randomized study with a minimum follow-up of 2 Years. Arthroscopy. 2019;35(2):544–551. [DOI] [PubMed] [Google Scholar]
- 10.Donahue TL, Gregersen C, Hull ML, et al. Comparison of viscoelastic, structural, and material properties of double-looped anterior cruciate ligament grafts made from bovine digital extensor and human hamstring tendons. J Biomech Eng. 2001;123(2):162–169. [DOI] [PubMed] [Google Scholar]
- 11.Emond CE, Woelber EB, Kurd SK, et al. A comparison of the results of anterior cruciate ligament reconstruction using bioabsorbable versus metal interference screws: a meta-analysis. J Bone Joint Surg Am. 2011;93(6):572–580. [DOI] [PubMed] [Google Scholar]
- 12.Fauno P, Kaalund S. Tunnel widening after hamstring anterior cruciate ligament reconstruction is influenced by the type of graft fixation used: a prospective randomized study. Arthroscopy. 2005;21(11):1337–1341. [DOI] [PubMed] [Google Scholar]
- 13.Hapa O, Barber FA. ACL fixation devices. Sports Med Arthrosc Rev. 2009;17(4):217–223. [DOI] [PubMed] [Google Scholar]
- 14.Harilainen A, Sandelin J. A prospective comparison of 3 hamstring ACL fixation devices—Rigidfix, BioScrew, and Intrafix—randomized into 4 groups with 2 years of follow-up. Am J Sports Med. 2009;37(4):699–706. [DOI] [PubMed] [Google Scholar]
- 15.Jagodzinski M, Geiges B, von Falck C, et al. Biodegradable screw versus a press-fit bone plug fixation for hamstring anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med. 2010;38(3):501–508. [DOI] [PubMed] [Google Scholar]
- 16.Kim HS, Seon JK, Jo AR. Current trends in anterior cruciate ligament reconstruction. Knee Surg Relat Res. 2013;25(4):165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kousa P, Järvinen TL, Vihavainen M, et al. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part II: tibial site. Am J Sports Med. 2003;31(2):182–188. [DOI] [PubMed] [Google Scholar]
- 18.Lee CH, Huang GS, Chao KH, et al. Differential pretensions of a flexor tendon graft for anterior cruciate ligament reconstruction: a biomechanical comparison in a porcine knee model. Arthroscopy. 2005;21(5):540–546. [DOI] [PubMed] [Google Scholar]
- 19.Leiter JR, Gourlay R, McRae S, et al. Long-term follow-up of ACL reconstruction with hamstring autograft. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1061–1069. [DOI] [PubMed] [Google Scholar]
- 20.Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. [DOI] [PubMed] [Google Scholar]
- 21.Mayr R, Heinrichs CH, Eichinger M, et al. Biomechanical comparison of 2 anterior cruciate ligament graft preparation techniques for tibial fixation: adjustable-length loop cortical button or interference screw. Am J Sports Med. 2015;43(6):1380–1385. [DOI] [PubMed] [Google Scholar]
- 22.Mayr R, Smekal V, Koidl C, et al. ACL reconstruction with adjustable-length loop cortical button fixation results in less tibial tunnel widening compared with interference screw fixation. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1036–1044. [DOI] [PubMed] [Google Scholar]
- 23.Milano G, Mulas PD, Ziranu F, et al. Comparison between different femoral fixation devices for ACL reconstruction with doubled hamstring tendon graft: a biomechanical analysis. Arthroscopy. 2006;22(6):660–668. [DOI] [PubMed] [Google Scholar]
- 24.Mouarbes D, Menetrey J, Marot V, et al. Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone–patellar tendon–bone and hamstring-tendon autografts. Am J Sports Med. 2019;47(14):3531–3540. [DOI] [PubMed] [Google Scholar]
- 25.Nagarkatti DG, McKeon BP, Donahue BS, et al. Mechanical evaluation of a soft tissue interference screw in free tendon anterior cruciate ligament graft fixation. Am J Sports Med. 2001;29(1):67–71. [DOI] [PubMed] [Google Scholar]
- 26.Noyes FR, Butler DL, Paulos LE, et al. Intra-articular cruciate reconstruction. I: perspectives on graft strength, vascularization, and immediate motion after replacement. Clin Orthop Relat Res. 1983;(172):71–77. [PubMed] [Google Scholar]
- 27.Noyes FR, Keller CS, Grood ES, et al. Advances in the understanding of knee ligament injury, repair, and rehabilitation. Med Sci Sports Exerc. 1984;16(5):427–43. [DOI] [PubMed] [Google Scholar]
- 28.Paessler HH, Mastrokalos DS. Anterior cruciate ligament reconstruction using semitendinosus and gracilis tendons, bone patellar tendon, or quadriceps tendon-graft with press-fit fixation without hardware: a new and innovative procedure. Orthop Clin North Am. 2003;34(1):49–64. [DOI] [PubMed] [Google Scholar]
- 29.Pasque CB, de la Garza S. Transtibial tubercle fixation without hardware for anterior cruciate ligament and posterior cruciate ligament reconstruction A new technique. Arthroscopy. 2004;20(suppl 2):164–170. [DOI] [PubMed] [Google Scholar]
- 30.Robert H, Bowen M, Odry G, et al. A comparison of four tibial-fixation systems in hamstring-graft anterior ligament reconstruction. Eur J Orthop Surg Traumatol. 2015;25(2):339–347. [DOI] [PubMed] [Google Scholar]
- 31.Sajovic M, Strahovnik A, Dernovsek MZ, et al. Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: an 11-year follow-up of a randomized controlled trial. Am J Sports Med. 2011;39(10):2161–2169. [DOI] [PubMed] [Google Scholar]
- 32.Sajovic M, Stropnik D, Skaza K. Long-term comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: a 17-year follow-up of a randomized controlled trial. Am J Sports Med. 2018;46(8):1800–1808. [DOI] [PubMed] [Google Scholar]
- 33.Salmon L, Pinczewski L, Roe J. The science of rehabilitation of the ACL injured and reconstructed knee. J Sci Med Sport. 2009;12:S59–S60. [Google Scholar]
- 34.Shaieb MD, Kan DM, Chang SK, et al. A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30(2):214–220. [DOI] [PubMed] [Google Scholar]
- 35.Sharp JW, Kani KK, Gee A, et al. Anterior cruciate ligament fixation devices: expected imaging appearance and common complications. Eur J Radiol. 2018;99:17–27. [DOI] [PubMed] [Google Scholar]
- 36.Smith PA, DeBerardino TM. Tibial fixation properties of a continuous-loop ACL hamstring graft construct with suspensory fixation in porcine bone. J Knee Surg. 2015;28(6):506–512. [DOI] [PubMed] [Google Scholar]
- 37.Tetsumura S, Fujita A, Nakajima M, et al. Biomechanical comparison of different fixation methods on the tibial side in anterior cruciate ligament reconstruction: a biomechanical study in porcine tibial bone. J Orthop Sci. 2006;11(3):278–282. [DOI] [PubMed] [Google Scholar]
- 38.Volpi P, Marinoni L, Bait C, et al. Tibial fixation in anterior cruciate ligament reconstruction with bone–patellar tendon–bone and semitendinosus-gracilis autografts: a comparison between bioabsorbable screws and bioabsorbable cross-pin fixation. Am J Sports Med. 2009;37(4):808–812. [DOI] [PubMed] [Google Scholar]
- 39.Walsh MP, Wijdicks CA, Parker JB, et al. A comparison between a retrograde interference screw, suture button, and combined fixation on the tibial side in an all-inside anterior cruciate ligament reconstruction: a biomechanical study in a porcine model. Am J Sports Med. 2009;37:160–167. [DOI] [PubMed] [Google Scholar]
- 40.Weiss FP, Possoli FAA, Costa IZ, et al. Fixation of the anterior ligament graft at the tibial pole: biomechanical analysis of three methods. Rev Bras Ortop (Sao Paulo). 2019;54(6):697–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yoo JS, Lee SJ, Jang JE, et al. Biomechanical comparison of different tendon suturing techniques for three-stranded all-inside anterior cruciate ligament grafts. Orthop Traumatol Surg Res. 2019;105(6):1101–1106. [DOI] [PubMed] [Google Scholar]
- 42.Yoo SH, Song EK, Shin YR, et al. Comparison of clinical outcomes and second-look arthroscopic findings after ACL reconstruction using a hamstring autograft or a tibialis allograft. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1290–1297. [DOI] [PubMed] [Google Scholar]
- 43.Zhang H, Ye M, Liang Q. Clinical outcomes after medial patellofemoral ligament reconstruction with suture fixation of the gracilis tendon via transosseous tunnels. Orthop J Sports Med. 2020;8(2):2325967119900373. [DOI] [PMC free article] [PubMed] [Google Scholar]