Abstract
The Africanized honey bee commonly referred to as the "killer bee," is a hybrid of the East African lowland honey bee with various European honey bees. These bees tend to be more hostile as compared to other bee species. Their stings may have devastating clinical sequelae, including cardiovascular, cerebrovascular events, and fatalities. We report the first-in-Caribbean case of a middle-aged woman who experienced stress-related, Takotsubo cardiomyopathy (also known as stress-related cardiomyopathy [SRC]) after being afflicted with innumerable Africanized honey bee stings.
Key clinical message: The clinician should be cognizant of Takotsubo's cardiomyopathy as a potential sequela of Hymenoptera envenomation and anaphylaxis.
Keywords: africanized honey bee, envenomation, hymenoptera, stress-related cardiomyopathy, stress-induced cardiomyopathy, takotsubo's syndrome
Introduction
The Africanized honey bee is rapidly looming as an environmental health care issue in the Caribbean [1]. These crossbred honey bees are generally hostile and intrusive, often inflicting a more painful sting and higher risk of envenomation [2].
These bee swarm invasions can precipitate cardiovascular and cerebrovascular events, even culminating in death [1]. The literature is not replete describing anaphylaxis-associated, stress-induced Takotsubo syndrome with only a paucity of case reports [3-5]. Herein, we report the first-in-Caribbean case of a middle-aged woman who experienced stress-related cardiomyopathy (SRC) after being afflicted with innumerable Africanized honey bee stings.
Case presentation
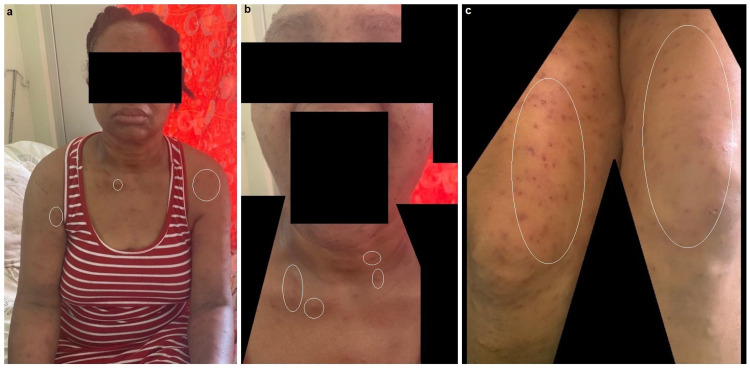
A 48-year-old Caribbean-Black female with no significant medical history presented to the emergency department via family members en extremis, obtunded and somnolent. Her vital signs indicated systolic blood pressures of 98 mm Hg, heart rate of 105 beats/min, respiratory rate of 26 breaths/min, and oxygen saturation of 94% on supplemental oxygen. Her physical examination revealed hundreds of stings throughout her body, including her face, upper chest, and lower extremities (see Figures 1a-1c). The emergency medicine team reported that the patient was attacked by a swarm of Africanized honey bees at home, circa 3-4 hours prior, and did not receive epinephrine en route.
Figure 1. Patient's stings throughout her body during her recovery.
(a) Frontal view aspect of the patient's stings involving the entirety of her body (some lesions encircled in white). (b) Close-up view of patient's face and upper neck displaying healing lesions with mild induration and erythema. (c) Multiple bee stings on upper thigh regions through various stages of healing.
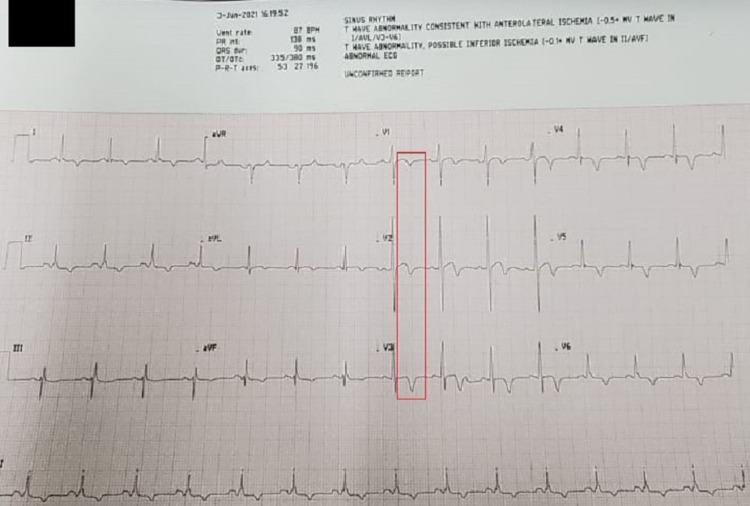
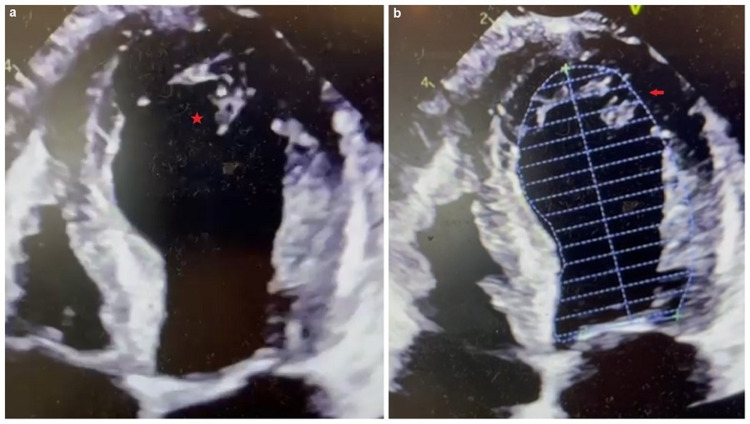
A 12-lead electrocardiogram (ECG) revealed sinus rhythm with subtle 1-2 mm ST-segment myocardial elevation in V1-V3 with diffuse T-wave inversions (Figure 2). A portable chest radiograph indicated mild interstitial edema without cardiomegaly or pleural effusions. Pertinent diagnostic laboratory investigations included a d-dimer 2,583 ng/dL (normal ≤ 500 ng/mL), N-terminal-pro-brain natriuretic peptide 3,674 pg/mL (normal ≤ 300 pg/mL), troponin I 1.49 ng/mL (normal < 0.15 ng/mL). Her complete blood count revealed a mild leukocytosis with normal hemoglobin and platelet count. Renal function tests, including random blood glucose and hepatic function panel, were relatively normal. A bedside two-dimensional transthoracic echocardiogram (2D-TTE) demonstrated severe apical "ballooning" with an estimated ejection fraction of 20%-25% (Figures 3a, 3b). SARS-CoV-2 IgM and IgM antibody serologies (Abbott Laboratories, Chicago, IL, USA) were negative.
Figure 2. Patient's 12-lead electrocardiogram.
The red box illustrates the subtle 1-2 mm ST-segment elevation with T-wave inversions in the precordial leads, a common electrocardiographic finding in Takotsubo's cardiomyopathy.
Figure 3. Patient's transthoracic echocardiogram.
(a) Apical four-chamber view demonstrating the severe apical akinesis with left ventricular dilatation as depicted by the red star (apical ballooning). (b) Apical four-chamber view with endocardial tracing outline illustrating the similarity to the Japanese octopus trap as depicted by the red arrow.
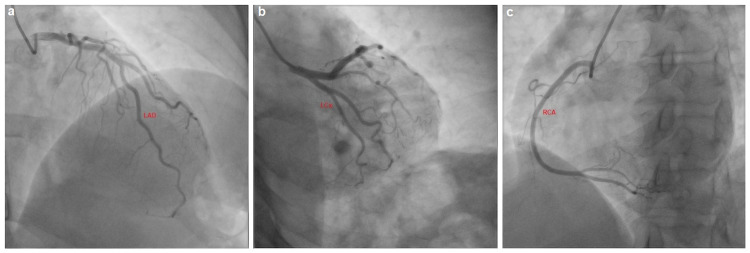
The patient was subsequently admitted to the cardiac care unit and initiated on a norepinephrine infusion, where her mental state improved to being oriented and fully conversant. She was immediately administered intravenous antihistamines (diphenhydramine 50 mg every six hours) and glucocorticoids (hydrocortisone 200 mg every eight hours). Her blood pressures stabilized hemodynamically within the ensuing hour, and she then proceeded to urgent coronary angiography, which revealed angiographically normal coronary arteries (Figures 4a-4c). Additionally, she was transitioned to comprehensive, guideline-directed medical therapy for the tentative diagnosis of SRC and Takotsubo's syndrome as she gradually became normotensive. This included low-dose valsartan/sacubitril 50 mg, eplerenone 25 mg, bisoprolol 2.5 mg, and dapagliflozin 5 mg. Her antihistaminergic and steroid therapies were subsequently weaned to an oral regimen during her inpatient one-week hospitalization. She was eventually discharged with the aforementioned neurohormonal inhibition. On her scheduled follow-up appointment two weeks later, her interval surveillance echocardiogram revealed normalization of the left ventricular ejection fraction to 60%.
Figure 4. Patient's coronary angiogram.
(a) Angiographically normal left anterior descending (LAD) coronary artery. (b) Angiographically normal left circumflex (LCx) coronary artery. (c) Angiographically normal right coronary artery (RCA).
Discussion
Africanized honey bees belong to the Apoidea winged Hymenoptera family [6]. Envenomation may ensue in a “cytokine storm,” resulting in multisystemic inflammatory syndrome. Typically, anaphylaxis has a prevalence of less than 5% and usually manifests in excess of 50-100 stings [7]. Adolescence ( age < 20 years) and male gender are negatively associated with increased mortality [8]. Our patient's clinical trajectory was consistent with Takotsubo's syndrome, aptly named due to the left ventricle's morphologic similarity to a Japanese octopus trap [9,10]. Kounis syndrome, which has been implicated in SRC, was also considered a differential diagnosis; however, no coronary vasospasm was apparent on coronary angiography [11].
The patient's pathophysiology may have resulted from either a direct envenomation effect, anaphylaxis, excessive exogenous or endogenous epinephrine. SRC has been observed with hymenopterous-induced anaphylaxis, but central to these reports has been the administration of exogenous epinephrine (0.2-5 mg) during the emergent resuscitation [12-14]. It is worthwhile to note that various phenotypes of SRC do clinically manifest, including "reverse Takotsubo syndrome" with mid-basal akinesis [14]. Our patient's classical left ventricular apical ballooning was echocardiographically diagnosed before she was initiated on the norepinephrine infusion, thus refuting the rationale for excessive exogenous epinephrine. We postulate that the patient experienced more than 200 stings which stimulated an endogenous catecholamine storm with an estimated envenomation toxin volume of 60 mg (0.3 mg per sting) [8]. Murine studies revealed a marked decrease in tissue noradrenaline concentration when injected with Africanized honey bee venom, suggesting its intracellular release [5]. It is also biologically plausible that the SRC may have resulted from a direct toxic effect of the bee venom, which may precipitate vascular thromboembolic phenomenon, refractory hypotension, malignant hypertension, arrhythmias, and hypercoagulability. Its constituents comprise histamine, serotonin, thromboxanes, leukotrienes, polypeptide toxins, hyaluronidase, phospholipase enzymes which can induce vasoconstriction and disrupt cell integrity [1,15].
The patient was treated with supportive measures, including norepinephrine, histamine receptor blockade, and parenteral glucocorticoids before being tapered and transitioned to an oral regimen. However, there are no specific evidence-based guidelines to define an optimal medical regimen for SRC [16]. Preemptively, the patient is treated with standard heart failure therapies until there is a recovery of systolic function, which usually occurs in 1-4 weeks. As such, our patient was treated with the "fantastic four" combination of an angiotensin-receptor, neprilysin inhibitor, beta-blocker, mineralocorticoid receptor antagonist, and sodium-glucose-like type cotransporter inhibitor to derive cardiovascular benefit with respect to mortality and morbidity, including heart failure hospitalizations [17].
Conclusions
We report the first-in-Caribbean case of a middle-aged woman who experienced stress-related, Takotsubo cardiomyopathy after being afflicted with a cluster of Africanized honey bee stings which was successfully managed with emergency resuscitative and supportive measures followed by the gradual introduction of neurohormonal therapies. The clinician should be cognizant of Takotsubo's cardiomyopathy as a potential sequela of Hymenoptera envenomation and anaphylaxis.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Africanised honey bee sting-induced ischaemic stroke. Ramlackhansingh AF, Seecheran N. BMJ Case Rep. 2020;13:0. doi: 10.1136/bcr-2020-234877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Historical perspective and human consequences of Africanized bee stings in the Americas. Ferreira RS Jr, Almeida RAMB, Barraviera SRCS, Barraviera B. J Toxicol Environ Health B Crit Rev. 2012;15:97–108. doi: 10.1080/10937404.2012.645141. [DOI] [PubMed] [Google Scholar]
- 3.Multiple bee sting-induced life-threatening Takotsubo cardiomyopathy. Aono J, Saito M, Inaba S, et al. Circ J. 2019;83:489. doi: 10.1253/circj.CJ-18-0047. [DOI] [PubMed] [Google Scholar]
- 4.Bee sting: a rare cause of Takotsubo cardiomyopathy. Mishra S, Mishra A, Mishra JP. Int J Cardiol. 2016;223:787–789. doi: 10.1016/j.ijcard.2016.08.312. [DOI] [PubMed] [Google Scholar]
- 5.Takotsubo cardiomyopathy caused by epinephrine-treated bee sting anaphylaxis: a case report. Ghanim D, Adler Z, Qarawani D, et al. J Med Case Rep. 2015;9:247. doi: 10.1186/s13256-015-0722-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fan HW, Kalil J. Critical Care Toxicology. Cham: Springer; 2016. Massive bee envenomation; pp. 1–10. [Google Scholar]
- 7.Massive poisoning by African bee stings. Bourgain C, Pauti MD, Fillastre JP, et al. Presse Med. 1998;27:1099–1101. [PubMed] [Google Scholar]
- 8.Bee and wasp venom allergy in Turkey. Kalyoncu AF, Fuat Kalyoncu A, Uğur Demir A, et al. Ann Allergy Asthma Immunol . 1997;78:408–412. doi: 10.1016/S1081-1206(10)63203-6. [DOI] [PubMed] [Google Scholar]
- 9.Stress cardiomyopathy. Akashi YJ, Nef HM, Möllmann H, et al. Annu Rev Med. 2010;61:271–286. doi: 10.1146/annurev.med.041908.191750. [DOI] [PubMed] [Google Scholar]
- 10.Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Tsuchihashi K, Ueshima K, Uchida T, et al. J Am Coll Cardiol. 2001;38:11–18. doi: 10.1016/s0735-1097(01)01316-x. [DOI] [PubMed] [Google Scholar]
- 11.A case of takotsubo cardiomyopathy associated with Kounis syndrome. Yanagawa Y, Nishi K, Tomiharu N, et al. Int J Cardiol. 2009;132:65–67. doi: 10.1016/j.ijcard.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 12.Apical ballooning syndrome after administration of intravenous epinephrine during an anaphylactic reaction. Manivannan V, Li JTC, Prasad A, et al. Mayo Clinic Proc. 2009;84:845–846. doi: 10.4065/84.9.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Midventricular hypokinesis as a cardiac manifestation of anaphylaxis: a case report. Han Y, Yeon S. J Am Soc Echocardiogr. 2006;19:1529. doi: 10.1016/j.echo.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 14.Stress cardiomyopathy after intravenous administration of catecholamines and beta-receptor agonists. Abraham J, Mudd JO, Kapur NK, et al. J Am Coll Cardiol. 2009;53:1320–1325. doi: 10.1016/j.jacc.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 15.Cerebral infarction: a rare complication of wasp sting. Crawley F, Schon F, Brown MM. J Neurol Neurosurg. 1999;66:550–551. doi: 10.1136/jnnp.66.4.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Bybee KA, Kara T, Prasad A, et al. Ann Intern Med. 2004;141:858–865. doi: 10.7326/0003-4819-141-11-200412070-00010. [DOI] [PubMed] [Google Scholar]
- 17.Heart failure drug treatment: the fantastic four. Bauersachs J. Eur Heart J. 2021;pp.:681–683. doi: 10.1093/eurheartj/ehaa1012. [DOI] [PMC free article] [PubMed] [Google Scholar]