Abstract
Introduction: Mushroom poisoning was the leading cause of foodborne disease outbreaks and outbreak-associated deaths in China. Mushroom poisoning outbreak surveillance can provide insight into the epidemiological characteristics of mushroom poisonings and guide policymaking and health education to reduce illnesses and deaths.
Methods: Foodborne Disease Outbreak Surveillance System was upgraded in 2011 to collect foodborne disease outbreaks in China. Mushroom poisoning outbreaks during 2010–2020 were selected to analyze geographical distribution, seasonal distribution, and setting of food preparation.
Results: A total of 10,036 outbreaks, which resulted in 38,676 illnesses and 788 deaths, were reported in this period. Mushroom poisonings occurred all over the country, but with highest incidence in the southwest and central China. Overall, 84.6% outbreaks were associated with food prepared in households, followed by 8.7% in street stalls, and 2.5% in canteens. Mushroom poisoning outbreaks clearly exhibited seasonality, and the peak season was summer through autumn. Outbreaks occurring between May and October accounted for 94.1% of total outbreaks, 92.4% illnesses, and 97.2% deaths.
Conclusions: Mushroom poisoning is a food safety issue of higher concern in China. Targeted health education is essential to reduce mushroom poisoning, especially in southwest China. Citizens are advised to not collect or eat wild mushrooms.
Keywords: Mushroom Poisoning, Outbreaks, China
INTRODUCTION
Wild mushroom consumption is widespread throughout the world, due to the nutritional value and medicinal properties (1-2). However, mushroom poisoning is a cause of major mortality and morbidity throughout the world (3-4). Toxic mushrooms are distributed across the globe with over 5,000 species. Among them, 100 species are responsible for most of the cases of mushroom poisoning (5). A total of 1,020 edible, 692 medicinal, and 480 poisonous species have been identified in China (6). Mushrooms are more abundant in warm and rainy summer and autumn, and mushroom pickers, especially if inexperienced, may not fully perceive the risks associated with ingesting potentially toxic mushroom species. Most mushroom poisonings reported were accidental oral ingestion of poisonous mushrooms misidentified for edible species. Morphological characteristics and appearance of many edible species were like those of poisonous mushrooms. Poisonous mushrooms cause the most deaths in remote districts in southwest regions in China (7). Mushroom poisonings often occur in other countries (8-9), but outbreaks were rarely reported (10).
Different levels of CDCs in China investigate and report foodborne disease outbreaks according to the requirements of the Food Safety Law. The China National Center for Food Safety Risk Assessment (CFSA) maintains and manages the Foodborne Disease Outbreaks Surveillance System for data collection and analysis. This study aimed to summarize and analyze the epidemiological characteristics of mushroom poisoning outbreaks from 2010 to 2020 in China.
METHODS
A foodborne disease outbreak is defined as an incident in which two or more cases involve a similar illness resulting from the consumption of a common food (11). A standard form was used to report the foodborne disease outbreaks investigated by CDCs at provincial, municipal, and county levels. All approved mushroom poisoning outbreak reports from 2010 through 2020 were collected through Foodborne Disease Outbreaks Surveillance System. Data collected in each outbreak report included the reporting CDC, the date of occurrence, the number of illnesses, hospitalizations, deaths, the etiologic agents, implicated food vehicle, setting of food preparation, and contributing factors.
All reported outbreaks were audited and checked, then stored and managed using Microsoft Excel (version 2016, Microsoft, USA). All variable values were reported as counts or proportions (%).
RESULTS
During 2010–2020, a total of 10,036 mushroom poisoning outbreaks were reported to Foodborne Disease Outbreaks Surveillance System, resulting in 38,676 illnesses, 21,967 hospitalizations, and 788 deaths. The annual number of reported outbreaks increased each year, from 37 reported in 2010 to 2,705 in 2020 (Figure 1). The average number of illnesses per outbreak was 3.9, and average hospitalization and fatality rates were 56.8% and 2.0%, respectively.
Figure 1.
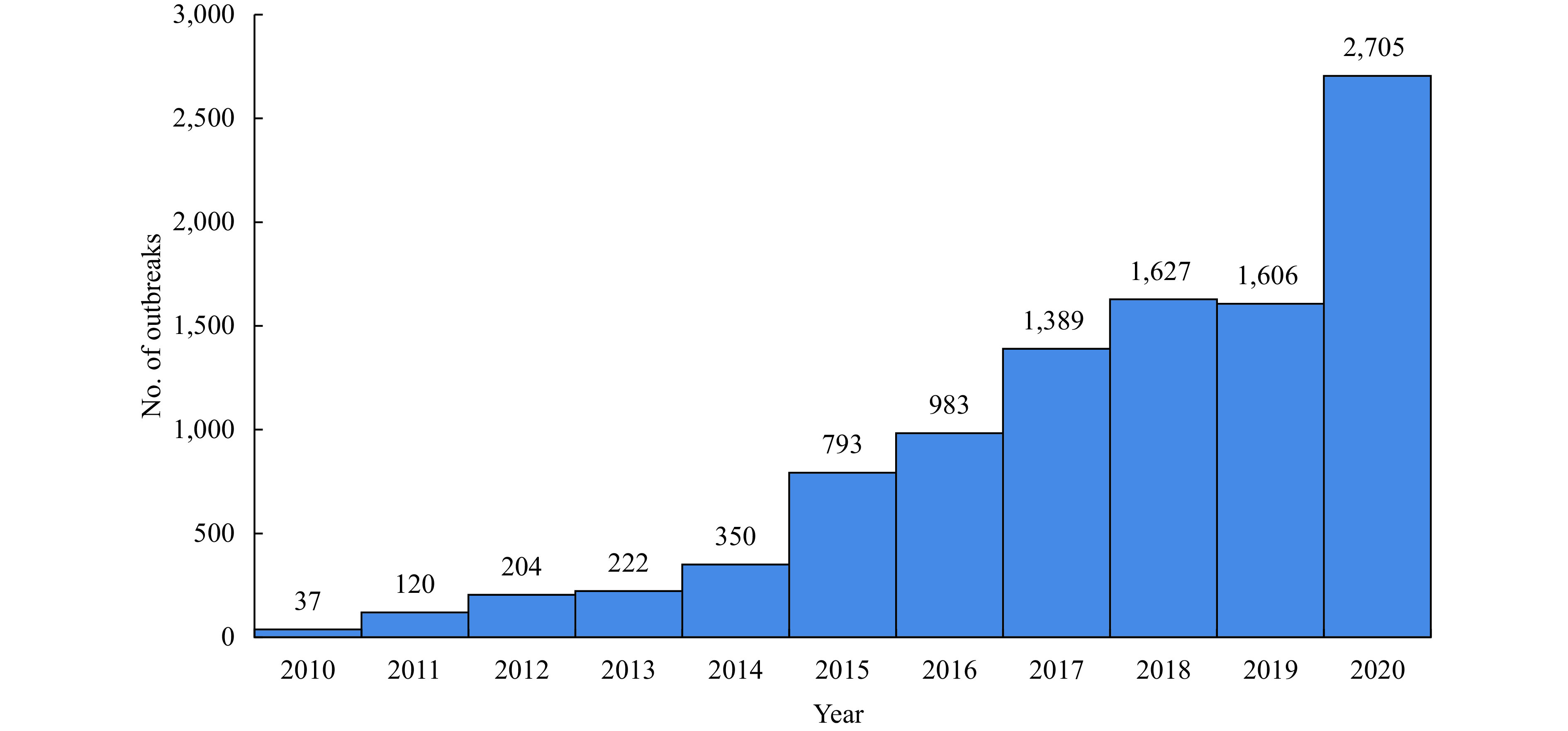
Number of reported mushroom poisoning outbreaks by year, Foodborne Disease Outbreak Surveillance System, China, 2010–2020.
Except for Xizang (Tibet) Autonomous Region, the other 30 provincial-level administrative divisions (PLADs) in China reported outbreaks (Figure 2). Southwest China was the region with highest number of outbreaks (6,062), illnesses (24,444), and deaths (454); 1,900 outbreaks occurred in central China, leading to 6,559 illnesses and 137 deaths; 1,132 outbreaks occurred in east China, leading to 4,094 illnesses and 112 deaths; 423 outbreaks occurred in south China, leading to 1,663 illnesses and 30 deaths; and followed by northwest China (213 outbreaks, 749 illnesses, and 20 deaths), north China (153 outbreaks, 621 illnesses, and 25 deaths), and northeast China (153 outbreaks, 546 illnesses, and 10 deaths). The total number of outbreaks reported by each PLAD varied from as low as 1 in Tianjin and Shanghai to as high as 4,010 in Yunnan. The overall national reporting rate during 2010–2020 was 0.3 outbreaks/million population. The top 5 PLADs, including Yunnan, Hunan, Guizhou, Sichuan, and Jiangxi, comprised 79.7% (8,002/10,036) of total outbreaks, 80.3% (31,058/38,676) of total illnesses, and 74.6% (588/788) of total deaths. Yunnan reported the most outbreaks, illnesses, and deaths, accounting for 40.0%, 43.6%, and 41.0%, respectively.
Figure 2.
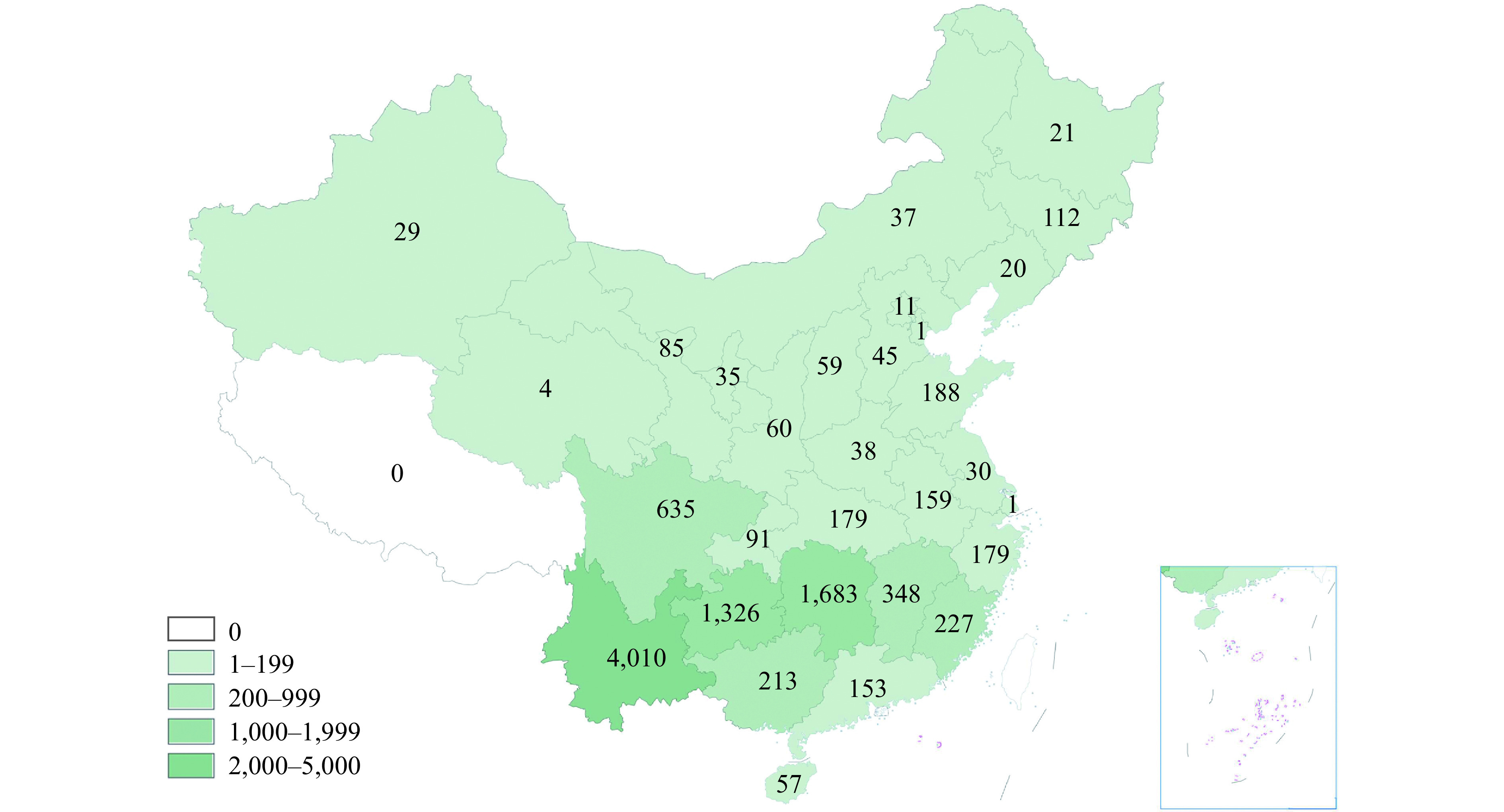
Number of reported mushroom poisoning outbreaks by PLADs in China, 2010–2020.
Abbreviation: PLADs=provincial-level administrative divisions.
The locations of food preparation were divided into 2 main categories: household and catering service places (Table 1). Among the 10,036 reported outbreaks, 84.7% were associated with food prepared in private homes (leading to 77.8% illnesses and 92.8% deaths), followed by 8.8% related with food prepared in street stalls (leading to 8.6% illnesses and 2.0% deaths), and 2.5% in canteens (leading to 4.6% illnesses and 1.9% deaths). The major cause of private-home outbreaks was self-harvest of wild mushrooms, which led to 98.1% of all private home outbreaks, 98.2% of illnesses, and 99.6% of deaths. Purchase of wild mushroom was the most common cause of catering service outbreaks, accounting for 63.5% of all catering service outbreaks, 49.0% illnesses, and 28.3% deaths.
Table 1. Number and percentage of mushroom poisoning outbreaks, illnesses, hospitalizations, and deaths by settings in China, 2010–2020.
| Setting | Outbreaks | Illnesses | Hospitalizations | Deaths | |||||||
| Number | % | Number | % | Number | % | Number | % | ||||
| Household | 8,495 | 84.6 | 30,098 | 77.8 | 17,456 | 79.5 | 731 | 92.8 | |||
| Catering Service Places | 1,463 | 14.6 | 8,083 | 20.9 | 4,196 | 19.1 | 46 | 5.8 | |||
| Street stall | 878 | 8.7 | 3,317 | 8.6 | 1,677 | 7.6 | 16 | 2.0 | |||
| Staff canteen | 249 | 2.5 | 1,783 | 4.6 | 899 | 4.1 | 15 | 1.9 | |||
| Restaurant | 175 | 1.7 | 1,107 | 2.9 | 550 | 2.5 | 0 | 0.0 | |||
| Rural banquet | 58 | 0.6 | 1,240 | 3.2 | 789 | 3.6 | 9 | 1.1 | |||
| Cafe | 50 | 0.5 | 276 | 0.7 | 131 | 0.6 | 3 | 0.4 | |||
| Fast food store | 32 | 0.3 | 144 | 0.4 | 83 | 0.4 | 3 | 0.4 | |||
| School canteen | 7 | 0.1 | 71 | 0.2 | 30 | 0.1 | 0 | 0.0 | |||
| Home delivery of meal | 5 | 0.0 | 109 | 0.3 | 12 | 0.1 | 0 | 0.0 | |||
| Other | 9 | 0.1 | 36 | 0.1 | 25 | 0.1 | 0 | 0.0 | |||
| Campus | 6 | 0.1 | 27 | 0.1 | 14 | 0.1 | 0 | 0.0 | |||
| Other location | 72 | 0.7 | 468 | 1.2 | 301 | 1.4 | 11 | 1.4 | |||
| Total | 10,036 | 100.0 | 38,676 | 100.0 | 21,967 | 100.0 | 788 | 100.0 | |||
From 2010 to 2020, mushroom poisoning outbreaks annually clearly exhibited seasonality (Figure 3). A large proportion of outbreaks occurred between May and October, accounting for 94.1% of total outbreaks, 92.4% of total illnesses, and 97.2% of total deaths. In Yunnan, there was a clear peak of outbreaks in July, while 2 peaks appearing in June and September were observed in Hunan and Guizhou.
Figure 3.
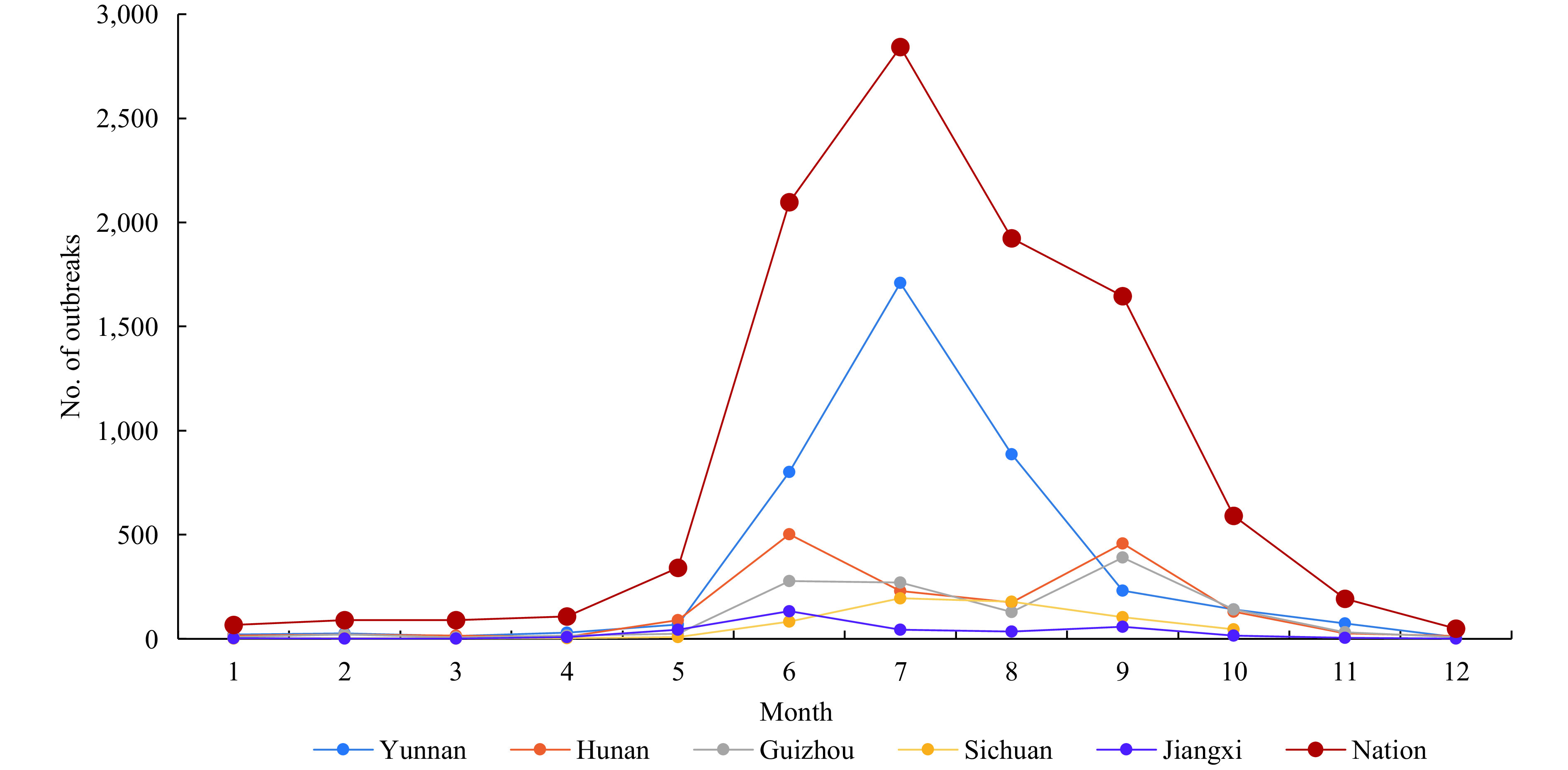
Monthly distribution of reported mushroom poisoning outbreaks in China, 2010–2020.
For all the reported outbreaks, 96.8% involved fewer than 10 cases per outbreak, leading to 95.7% of the total deaths. In addition, 12 outbreaks had more than 30 cases, met the limits of the public health emergency incidents of China, and led to 943 illnesses and no reported deaths.
DISSCUSSION
Mushroom poisoning was the leading cause of foodborne disease outbreaks and outbreak-associated deaths in China. Surveillance data showed that mushroom poisonings accounted for 31.8% of the total outbreaks and 47.4% of the total associated deaths from 2003–2017 (12). The annual number of mushroom poisoning outbreaks reported in China gradually increased between 2010 and 2020. The increase is expected to be associated with the implementation of compulsory surveillance in 2011, increasingly strict requirements for outbreak reporting, and enhancement of reporting awareness. Therefore, the increase owed a great deal to the improvement of surveillance sensitivity. Even though 2,075 mushroom outbreaks were reported in 2020, underreporting is still likely.
Mushroom poisonings were reported throughout the country, but the incidence was highest in the southwest and central, likely due to the warm and damp climate conditions. Most outbreaks occurred in private home settings, especially in rural areas, mainly because of the self-harvesting of wild mushroom. Non-expert wild mushroom picking and consumption increases the risk of poisoning due to the difficulties of identifying poisonous mushrooms and distinguishing them from non-poisonous mushrooms. Although citizens are advised not to collect and eat wild mushrooms, mushroom poisoning continues to occur every year.
Mushroom poisoning occurred every month, with peaks in summer and autumn. The seasonality suggests that, albeit always important, health education is especially crucial in this period. Since mushroom picking is more frequent in rural environments, health education targeted for specific groups in rural areas is also essential to reduce mushroom poisonings.
Only 3,872 outbreaks (38.6%) were reported with mushroom names, involving 15,475 illnesses (40.0%) and 275 deaths (34.9%); 65.1% deaths were reported in 6,164 outbreaks involving unidentified mushrooms. Absence of relevant mushroom samples and ingestion of multiple mushrooms increased the difficulty of identifying causative species. Over 180 mushroom names were reported, but most of the outbreaks were reported with trivial, non-scientific names. Accurate and prompt species identification is crucial in the diagnosis and treatment process. More effort and cooperation is needed from administrative agencies, epidemiologists, doctors, and mycologists to increase the identification rate (13).
It is not possible to evaluate if the increase in reporting of mushroom poisoning outbreaks in investigations is only due to changes in surveillance practices or reflecting a true increase in incidence. Evaluating trends will be possible when surveillance and reporting practices are well-established and stable throughout the country. Currently, some degree of underreporting still exists, which is also a challenge for all foodborne illnesses globally (14). In addition to challenges in surveillance, underreporting is also related to failures in any other step between the occurrence of an illness and the reporting of the outbreak, i.e., patients seeking medical care, the cause of the illness being investigated, and the illness being registered (15).
Despite important improvements in surveillance of mushroom poisoning outbreaks, some of the results in the analysis were still subject to some limitations. Some of the epidemiological information is still not complete and accurate, such as mushroom species identification. Efforts should be made to improve investigative procedures, reporting practices, and data collection. Because of different surveillance systems and reporting standards, the results might be different from the other published results earlier or later (13).
Identifying and prioritizing interventions to reduce diseases, including mushroom poisoning, requires data on the public health impact of these diseases. The results of this study showed that targeted interventions to reduce mushroom poising in China are crucial. Policy efforts should be focused on citizen campaigns to raise awareness of the risks, and are particularly important in summer and autumn months, rural areas, and specific regions of China.
Conflicts of interest: No conflicts of interest.
Acknowledgments
All members in all participating CDCs.
Funding Statement
The National Key Research and Development Program of China (Grant number 2017YFC1601503)
Contributor Information
Ping Fu, Email: fuping@cfsa.net.cn.
Yunchang Guo, Email: gych@cfsa.net.cn.
References
- 1.Svanberg I, Lindh H Mushroom hunting and consumption in twenty-first century post-industrial Sweden. J Ethnobiol Ethnomed. 2019;15(1):42. doi: 10.1186/s13002-019-0318-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feeney MJ, Miller AM, Roupas P Mushrooms-biologically distinct and nutritionally unique: exploring a “third food kingdom”. Nutr Today. 2014;49(6):301–7. doi: 10.1097/NT.0000000000000063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan CK, Lam HC, Chiu SW, Tse ML, Lau FL Mushroom poisoning in Hong Kong: a ten-year review. Hong Kong Med J. 2016;22(2):124–30. doi: 10.12809/hkmj154706. [DOI] [PubMed] [Google Scholar]
- 4.Trakulsrichai S, Jeeratheepatanont P, Sriapha C, Tongpoo A, Wananukul W Myotoxic mushroom poisoning in Thailand: clinical characteristics and outcomes. Int J Gen Med. 2020;13:1139–46. doi: 10.2147/IJGM.S271914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dadpour B, Tajoddini S, Rajabi M, Afshari R Mushroom poisoning in the northeast of iran; a retrospective 6-year epidemiologic study. Emerg (Tehran) 2017;5(1):e23. doi: 10.22037/emergency.v5i1.13607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu F, Zhou LW, Yang ZL, Bau T, Li TH, Dai YC Resource diversity of Chinese macrofungi: edible, medicinal and poisonous species. Fungal Divers. 2019;98(1):1–76. doi: 10.1007/s13225-019-00432-7. [DOI] [Google Scholar]
- 7.Liu JK, Bai L, Li WW, Han HH, Fu P, Ma XC, et al Trends of foodborne diseases in China: lessons from laboratory-based surveillance since 2011. Front Med. 2018;12(1):48–57. doi: 10.1007/s11684-017-0608-6. [DOI] [PubMed] [Google Scholar]
- 8.Brandenburg WE, Ward KJ Mushroom poisoning epidemiology in the United States. Mycologia. 2018;110(4):637–41. doi: 10.1080/00275514.2018.1479561. [DOI] [PubMed] [Google Scholar]
- 9.Cervellin G, Comelli I, Rastelli G, Sanchis-Gomar F, Negri F, De Luca C, et al Epidemiology and clinics of mushroom poisoning in Northern Italy: a 21-year retrospective analysis. Hum Exp Toxicol. 2018;37(7):697–703. doi: 10.1177/0960327117730882. [DOI] [PubMed] [Google Scholar]
- 10.Dalton CB, Gregory J, Kirk MD, Stafford RJ, Givney R, Kraa E, et al Foodborne disease outbreaks in Australia, 1995 to 2000. Commun Dis Intell Q Rep. 2004;28(2):211–24. [PubMed] [Google Scholar]
- 11.Gould LH, Walsh KA, Vieira AR, Herman K, Williams IT, Hall AJ, et al Surveillance for foodborne disease outbreaks—United States, 1998–2008. MMWR Surveill Summ. 2013;62(2):1–34. [PubMed] [Google Scholar]
- 12.Li WW, Liu ZT, Ma XC, Liang JJ, Jiang YY, Chen J, et al Surveillance of foodborne disease outbreaks in China, 2003–2017. Food Control. 2020;118:107359. doi: 10.1016/j.foodcont.2020.107359. [DOI] [Google Scholar]
- 13.Li HJ, Zhang HS, Zhang YZ, Zhou J, Yin Y, He Q, et al Mushroom poisoning outbreaks — China, 2020. China CDC Wkly. 2021;3(3):41–5. doi: 10.46234/ccdcw2021.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Havelaar AH, Kirk MD, Torgerson PR, Gibb HJ, Hald T, Lake RJ, et al World Health Organization global estimates and regional comparisons of the burden of foodborne disease in 2010. PLoS Med. 2015;12(12):e1001923. doi: 10.1371/journal.pmed.1001923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haagsma JA, Geenen PL, Ethelberg S, Fetsch A, Hansdotter F, Jansen A, et al Community incidence of pathogen-specific gastroenteritis: reconstructing the surveillance pyramid for seven pathogens in seven European Union member states. Epidemiol Infect. 2012;141(8):1625–39. doi: 10.1017/S0950268812002166. [DOI] [PMC free article] [PubMed] [Google Scholar]


