Abstract
What is already known about this topic?
Tuberculosis (TB) notification data and the underreporting rate are major sources used in estimating TB incidence. China’s TB Information Management System (TBIMS) was launched in 2005 but has not yet been evaluated for sensitivity.
What is added by this report?
The average underreporting rate of pulmonary TB to TBIMS in selected facilities was 8.23%. However, provincial TB or infectious disease-specific health facilities, or general health facilities had higher underreporting rates. Children, migrants, and drug resistant TB patients had higher chances to be underreported than other populations.
What are the implications for public health practice?
Underreporting surveys should be routinely implemented in the future. This will be vital for enhancing TB reporting and the transfer mechanisms in TB or infectious disease-specific hospitals, or general hospitals and improving the case information registration procedures in designated health facilities (DHFs).
The number of pulmonary tuberculosis (PTB) reported cases in the National Notifiable Disease Reporting System (NNDRS) was used to indicate TB incidence data in China. While globally, notification data based on confirmed cases were more often used to estimate or model TB incidence with quantified underreporting levels (1-2). China’s Tuberculosis Information Management System (TBIMS) was launched in 2005 to collect diagnosis, treatment, and management information of TB cases enrolled in the National Tuberculosis Program (NTP) by designated health facilities (DHFs), but its sensitivity has never been evaluated at a national level. A retrospective cross-sectional survey was carried out by the National Center for Tuberculosis Control and Prevention (NCTB) to evaluate the underreporting level of TBIMS in 2015.
The average underreporting rate of PTB to TBIMS in selected facilities was 8.23%. Among the different levels and types of health facilities, provincial facilities had the highest underreporting rate, and general TB or infectious disease-specific health facilities or general health facilities had higher underreporting rate than DHFs in same level. Children, migrants and drug resistant patients had a higher likelihood to be underreported than other populations. Enhancing TB reporting and transfer mechanisms in TB or infectious disease-specific hospitals or general hospitals are recommended to reduce underreporting and lost follow-ups among patients referred to TB DHFs. Meanwhile, the registration procedure for patient information in DHFs also needs to be improved, especially to target patients that are children, drug resistant, or migrants.
Furthermore, reporting PTB cases is a mandatory requirement enforced by law (3). As part of the National Disease Control Information System, TBIMS can exchange information on TB cases with the NNDRS. When a case was considered PTB, either presumptive or confirmed, the case must be reported to the NNDRS first and then transferred to TB DHFs where the patient will undergo further diagnosis verification. With the information exchanged between NNDRS and TBIMS, DHFs can easily trace patients diagnosed by every hospital/clinic/primary health center all over the country and enroll them into NTP. TBIMS is a web-based, real-time PTB notification system for describing TB epidemic and long-term trends, which has helped improve China’s TB control strategies.
The survey design and procedures have referred to the World Health Organization (WHO) guideline: Assessing tuberculosis underreporting through inventory studies (4). The study population was defined as patients whose current address was in selected areas and eventually confirmed as PTB (clinical or laboratory confirmed) in sampled health facilities during selected months of 2015; tuberculous pleurisy didn't include.
Sampling was performed as follows: 30% of prefectures were randomly selected throughout 32 provincial-level administration divisions (PLADs); then 30% of counties or districts were also randomly selected from previously selected prefectures; a TB DHF and a general hospital were selected in each county/district and all PTB cases diagnosed in these two types of facilities were accounted for. At the prefectural and provincial level, a TB DHF, a general hospital, and a TB or infectious disease-specific hospital (if existing) were selected. The enrolled facilities must also fulfill following criteria: 1) county- level or above-county-level facilities; 2) TB diagnostic ability, which includes the ability to conduct chest x-ray examinations and/or sputum smear examinations of mycobacterium; and 3) has reported at least 1 PTB case (presumptive or confirmed) in the NNDRS in 2015. The description of final enrolled facilities is in Table 1.
Table 1. Number of sites and health facilities selected in the 2015 nationwide Tuberculosis Information Management System (TBIMS) underreporting survey in China.
| Administrative level | Total regions | Total No. of health facilities | Sampled regions | No. of sampled health facilities | ||||
| TB DHF | TB or infectious disease-specific hospitals | General health facilities | TB DHF | TB or infectious disease-specific hospitals | General health facilities | |||
| Abbreviation: DHF=designated health facility, TB=tuberculosis.
*Generally there should be at least one DHF in each county or district, while in reality plural counties/districts may share the same DHF and upper-level DHF could also represent the role of lower DHF in its location area. Hence, there were less selected county-level DHFs than selected number of counties/districts. | ||||||||
| Province | 32 | 58 | 11 | 764 | 32 | 18 | 7 | 40 |
| Prefecture | 348 | 304 | 59 | 1,834 | 116 | 88 | 12 | 137 |
| County/district | 3,093 | 2,812 | 0 | 6,825 | 436 | 348* | 0 | 335 |
The data was collected and processed as follows: record reviewing work was carried out by local NTP health workers. All medical records which contained “结核” (tuberculosis in Chinese) during designated periods were collected in enrolled health facilities’ outpatient, inpatient, and laboratory departments. For the data processing procedure, see Figure 1.
Figure 1.
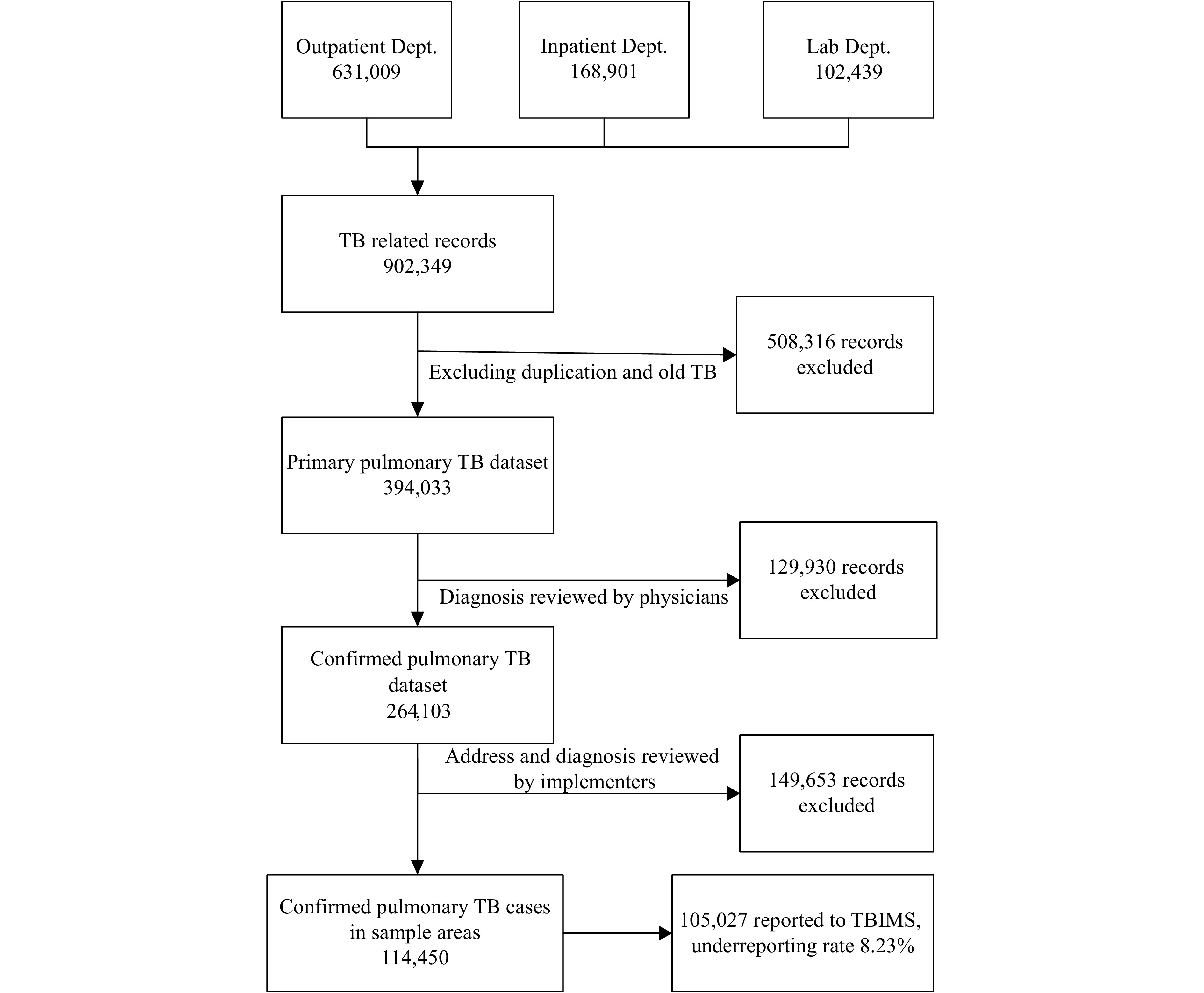
Flowchart of the 2015 nationwide Tuberculosis Information Management System (TBIMS) underreporting survey in China. Dept.=Department.
Data analysis was conducted using a specific “multisystem TB records matching and linking software” that was predesigned for data matching between health facility medical records and the TBIMS notification database. SPSS Software (version 17.0, SPSS Inc., Chicago, Il, USA) was used for analysis of final dataset. Chi square tests were used for testing relationships between categorical variables. P<0.05 was considered statistically significant. The underreporting rate was defined as follow:
 |
A total of 902,349 cases with TB related diagnosis were collected in this survey including 631,009 (69.93%) outpatient records, 168,901 (18.72%) inpatient records, and 102,439 (11.35%) laboratory records. Among 902,349 records, 508,316 duplicated or old TB cases were excluded after preliminary data cleaning. Then another 279,583 cases were excluded by physicians and implementers due to living outside of the sampled sites or exclusion of TB. Finally, 114,450 confirmed cases from 985 health facilities in 32 PLADs were included in the survey (Table 2).
Table 2. The number and underreporting rate of pulmonary tuberculosis (PTB) cases enrolled in the 2015 nationwide Tuberculosis Information Management System (TBIMS) underreporting survey in China.
| Categories | Number | Proportion (%) | Underreporting cases | Underreporting rate (%) | p | χ2 |
| Abbreviation: ID=Infectious Disease, DHF=designated health facility, MDR/RR=multi-drug resistant/rifampin resistant, TB=tuberculosis.
* The chi square and p-value are the result of testing between laboratory-confirmed cases and clinically-diagnosed cases. | ||||||
| Gender | <0.0001 | 30.23 | ||||
| Male | 79,463 | 69.43 | 6,362 | 8.01 | ||
| Female | 34,800 | 30.41 | 3,028 | 8.70 | ||
| Not recorded | 187 | 0.16 | 33 | 17.65 | ||
| Age groups (years) | <0.0001 | 381.36 | ||||
| 0–14 | 609 | 0.53 | 135 | 22.17 | ||
| 15–64 | 87,689 | 76.62 | 6,462 | 7.37 | ||
| ≥65 | 26,152 | 22.85 | 2,826 | 10.81 | ||
| Diagnosis categories | <0.0001* | 127.27* | ||||
| Laboratory confirmed | 33,037 | 28.87 | 2,206 | 6.68 | ||
| - MDR/RR | 978 | 0.85 | 317 | 32.41 | ||
| Clinically diagnosed | 81,413 | 71.13 | 7,217 | 8.86 | ||
| Data sources | <0.0001 | 30.23 | ||||
| Outpatient | 91,427 | 79.88 | 4,507 | 4.93 | ||
| Inpatient | 14,485 | 12.66 | 3,939 | 27.19 | ||
| Laboratory | 8,538 | 7.46 | 977 | 11.44 | ||
| Reporting area | <0.0001 | 1218.90 | ||||
| Within living provinces | 113,755 | 99.39 | 9,038 | 7.95 | ||
| Out of living provinces | 695 | 0.61 | 385 | 55.40 | ||
| Classification of health facilities | <0.0001 | 19971.59 | ||||
| Provincial DHFs | 4351 | 3.80 | 1,090 | 25.05 | ||
| Provincial TB/ID-specific hospitals | 1,375 | 1.20 | 468 | 34.04 | ||
| Provincial general health facilities | 746 | 0.65 | 301 | 40.35 | ||
| Prefectural DHFs | 8,234 | 7.19 | 1,348 | 16.37 | ||
| Prefectural TB/ID-specific hospitals | 1,016 | 0.89 | 282 | 27.76 | ||
| Prefectural general health facilities | 2,110 | 1.84 | 545 | 25.83 | ||
| County-level DHFs | 87,102 | 76.10 | 1,943 | 2.23 | ||
| County-level general health facilities | 9,516 | 8.31 | 3,446 | 36.21 | ||
| Total | 114,450 | 100.00 | 9,423 | 8.23 | ||
The average underreporting rate of PTB in TBIMS in selected facilities was 8.23% (9,423/114,450). The underreporting rates of cases collected from outpatient, inpatient, and laboratory records were 4.93% (4,507/91,427), 27.19% (3,939/14,485), and 11.44% (977/8,538), respectively. The underreporting rate was 22.17% (135/609) among children under 15 years old, while it was 7.37% (6,462/87,689) among those aged 15–64 years and 10.81% (2,826/26,152) among elders aged over 64 years. Among laboratory confirmed cases, 6.68% (2,206/33,037) cases were not reported to TBIMS, among which the underreporting rate of multi-drug resistant/rifampin resistant (MDR/RR) TB cases was 32.41% (317/978). Correspondingly, the underreporting rate among clinically diagnosed cases was 8.86% (7,217/81,413). When a patient was diagnosed within his or her PLAD of residence, the likelihood of not being reported to TBIMS was 7.95% (9,038/113,755). However, if a case was diagnosed out of his or her PLAD of residence, the likelihood of not being reported was 55.40% (385/695). Among different types of health facilities, provincial general health facilities had the highest underreporting rate at 40.35% (301/746) and county level DHFs had the lowest underreporting rate at 2.23% (1,943/87,102) (Table 2).
Discussion
In 2015, about 92% (105,027/114,450) of PTB cases diagnosed in 985 sampled health facilities were reported to national TBIMS, which was higher than the WHO estimated case finding rate of 87% (notified/estimated incidence) (5) and could indicate China’s NTP surveillance system had relatively good coverage and sensitivity. However, many challenges and barriers were also revealed in this survey.
Among different levels and types of health facilities, provincial facilities had the highest underreporting rate, and general TB or infectious disease-specific or general health facilities had higher underreporting rates than DHFs at the same regional level. This showed that quality control work should be carried out in every health facility and TB diagnostic capacity especially needs to be improved in higher level, non-designated units. Children are a vulnerable population facing TB infections, and our global society is risking a silent epidemic of childhood TB. (6) The much higher underreporting rate among children under 15 years revealed the urgency of involving diagnosed childhood TB into NTP management. Currently, reporting work is mostly conducted by outpatient departments. PTB cases diagnosed in outpatient departments had a smaller likelihood to be underreported in this survey, while inpatient and laboratory departments need to improve their internal information transfer work. Less than half the patients diagnosed out of their PLAD of residence have been reported in TBIMS, which was quite low comparing to patients diagnosed within their PLAD of residence. This indicated great barriers in cross-area patient management. Compared to local residents, migrant PTB cases may not be appropriately reported based on many reasons such as social insurance, changing residential addresses, and stigma, etc.
China has the second highest MDR/RR TB burden in the world. There was still a big gap between notified cases and estimated MDR/RR TB incidence in recent years (1). In this survey, nearly one third of diagnosed MDR/RR TB cases have not been correctly reported to TBIMS. Further investigation and analysis must be done to clarify the underlying reasons in the near future.
This is the first nationwide underreporting survey that may help improve the national TB incidence estimation. Furthermore, routine surveys (e.g. every five years) are suggested in the future for evaluating the quality and progress of TBIMS. Enhancing TB surveillance work is a major request in the national “Stop TB Action Plan (2019–2022)”. All relevant stakeholders, including health authorities, CDCs, and health facilities, need to enhance their roles by following national regulations and guidelines. Enhancing TB reporting and transfer mechanisms in TB or infectious disease-specific hospitals or general hospitals are recommended to reduce underreporting and lost follow-ups among patients referred to TB DHFs. Meanwhile, the registration procedures for patient information in DHFs also needs to be improved, especially those targeting patients that are children, drug resistant, or migrant.
Acknowledgement
We thank our colleagues and healthcare workers who contributed to the survey from all levels of CDCs, hospitals, and health facilities for data collection and review.
Contributor Information
Xin Du, Email: duxin@chinacdc.cn.
Hui Zhang, Email: zhanghui@chinacdc.cn.
References
- 1.World Health Organization. Global tuberculosis report 2019. Geneva, Switzerland: WHO. 2019. https://www.who.int/tb/publications/global_report/en/.[2020-03-10].
- 2.Kyu HH, Maddison ER, Henry NJ, Ledesma JR, Wiens KE, Reiner Jr R, et al Global, regional, and national burden of tuberculosis, 1990-2016: results from the global burden of diseases, injuries, and risk factors 2016 study. Lancet Infect Dis. 2018;18(12):1329–49. doi: 10.1016/S1473-3099(18)30625-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National People’s Congress. Law of infectious disease control. 2005. http://www.gov.cn/banshi/2005-08/01/content_19023.htm. [2019-12-27]. (In Chinese).
- 4.World Health Organization. Assessing tuberculosis underreporting through inventory studies. Geneva: WHO. 2012. https://www.tandfonline.com/doi/ref/10.1080/17476348.2016.1199278?scroll=top. [2020-03-10].
- 5.World Health Organization. Global tuberculosis report 2016. Geneva, Switzerland: WHO. 2016. https://apps.who.int/iris/bitstream/handle/10665/250441/9789241565394-eng.pdf?sequence=1&isAllowed=y. [2020-03-10].
- 6.International Union Against Tuberculosis and Lung Disease[Internet]. Silent epidemic: a call to action against child tuberculosis. c2018. https://childtb.theunion.org/wp-content/uploads/2018/08/Silent-Epidemic.pdf. [2020-03-10].


