Abstract
Aim: Many governments in East and Southeast Asia responded promptly and effectively at the onset of the COVID-19 pandemic. Synthesizing and analyzing these responses is vital for disease control evidence-based policymaking. Methods: An extensive review of COVID-19 control measures was conducted in selected Asian countries and subregions, including Mainland China, Hong Kong, Taiwan, South Korea, Singapore, Japan, and Vietnam from 1 January to 30 May 2020. Control measures were categorized into administrative, public health, and health system measures. To evaluate the stringency and timeliness of responses, we developed two indices: the Initial Response Index (IRI) and the Modified Stringency Index (MSI), which builds on the Oxford COVID-19 Government Response Tracker (OxCGRT). Results: Comprehensive administrative, public health, and health system control measures were implemented at the onset of the outbreak. Despite variations in package components, the stringency of control measures across the study sites increased with the acceleration of the outbreak, with public health control measures implemented the most stringently. Variations in daily average MSI scores are observed, with Mainland China scoring the highest (74.2), followed by Singapore (67.4), Vietnam (66.8), Hong Kong (66.2), South Korea (62.3), Taiwan (52.1), and Japan (50.3). Variations in IRI scores depicting timeliness were higher: Hong Kong, Taiwan, Vietnam, and Singapore acted faster (IRI > 50.0), while Japan (42.4) and Mainland China (4.2) followed. Conclusions: Timely setting of stringency of the control measures, especially public health measures, at dynamically high levels is key to optimally controlling outbreaks.
Keywords: COVID-19 control, government response, Asia, stringency, timeliness
1. Introduction
Since the onset of the COVID-19 pandemic in 2019 up to 1 August 2021, more than 198.3 million confirmed cases and 4.2 million deaths have been reported globally [1]. Governments have been responding with unprecedented policy responses, aiming to control the spread and mitigate consequences as much as possible. Upon discovering the virus, Mainland China had the highest number of cases and fatalities. However, starting in March 2020, the global epicenter started shifting from Mainland China to Europe and North America. Shortly afterward, in May 2020, significant declines in new cases were observed in several countries; these can be attributed to effective control measures.
Despite more control, new waves of infections have been observed as countries started reducing the stringency of measures and reopening their economies. These waves of infections have been much worse, especially in European countries and the United States since November 2020 [2], which may be the result of lower outdoor temperatures, more indoor activities, holiday gatherings, and the mutations of the coronavirus that have been discovered. In November 2020, a new variant of COVID-19 was discovered in South Africa [3], which requires even more stringent measures because of its more infectious nature. As of July 2021, four major variants are being discovered globally, among which the B.1.617.2 (Delta) has been driving a new surge of COVID-19 cases worldwide [4]. Meanwhile, reduced effectiveness of current vaccines has been found against the widespread Delta variant [5], which highlights the importance of evidence-based effective control measures.
Significant differences across regions in new cases and case fatality rates are observed at the early phases of the pandemic. The daily new confirmed cases per million people were 349.3, 277.8, and 20.7 in Europe, North America, and Asia, respectively, on 15 November, and the case fatality rate was 1.8% in Asia compared with 2.3% and 2.9% in Europe and North America [2]. These differences can be attributed to the variations in government responses. Therefore, it is important to examine common control measures taken by Asian countries in response to the pandemic and to analyze the difference in implementation that may have produced different effects.
Since the outbreak of the COVID-19 pandemic, countries have been adopting various approaches in combating the pandemic based on their different political, socio-economic, cultural, and health system contexts. This has resulted in variations in the ability to effectively control new cases and mortality attributed to COVID-19. Overall, Asian countries and subregions, most of which had prior experience in combating epidemics of novel infectious diseases such as SARS, MERS, and H1N1, have outperformed their counterparts in Europe and North America in controlling the COVID-19 pandemic with timely and effective government responses.
Many studies have been conducted to summarize the control measures implemented globally, including those in Asian countries [6,7,8,9], though few have systematically and comprehensively summarized and analyzed these measures. The Oxford COVID-19 Government Response Tracker (OxCGRT) [10] was developed to evaluate the implementation of the control measures, specifically focusing on variation in the stringency of government response. The most up-to-date OxCGRT contains 19 indicators covering dimensions of containment and closure, economic, health system, and miscellaneous policies [11]. Though informative and widely used, the OxCGRT fails to comprehensively capture several key control measures—for example, establishing coordinated governance has not been included in the OxCGRT. Governance, leadership, and macro-management of the pandemic at the national level is likely to be critically important to the success of its effective control, and therefore should be accounted for when considering the effectiveness of government responses. Furthermore, the OxCGRT evaluates only stringency but ignores timeliness, another essential factor associated with effective control.
This paper aims to examine and compare the timeliness and stringency of control measures implemented during the early phase of the COVID-19 pandemic in selected Asian countries and subregions. The paper focuses on Asian countries and subregions with quality data availability and epidemic control experiences and practices. This was done by extensively reviewing high-quality literature available from 1 January to 30 May 2020. Control measures upon collection were grouped into three categories: administrative, public health, and health system measures. We develop two indices to evaluate and compare the stringency and timeliness of countries’ COVID-19 responses: the Modified Stringency Index (MSI), adapted from the OxCGRT, and the Initial Response Index (IRI). We then propose policy recommendations for future pandemics preparedness.
2. Methods
2.1. Country/Subregion Selection
China (including Mainland China, Hong Kong SAR/China (hereafter referred to as Hong Kong), and Taiwan/China (hereafter referred to as Taiwan)), South Korea, Singapore, Japan, and Vietnam (hereafter all referred to as the “study sites”), were purposively selected in this review because of the generally good or unique practices manifested in response to the COVID-19 pandemic; their previous epidemic control experiences with SARS, MERS and H1N1; and the availability of comprehensive and comparable data.
2.2. Data
Data on the control strategies, policies, and measures taken by the governments of the study sites between 1 January and 30 May 2020 when most of the COVID-19 cases were reported before the current new wave, were collected from various sources. While peer-reviewed publications were prioritized, reliance on gray literature was inevitable because of the limited number of publications available as a result of the short time period. PubMed was first searched using the following key search terms: “COVID-19” (AND), “response” (OR) “experience” (OR) “intervention” (OR) “policy” (AND), the name of specific geographic locations. Gray literature, including articles from reputable magazines and media reports that presented reliable and robustly vetted information, were also utilized. In addition, we collected data from preprints on MedRxiv and unpublished internal reports, which were attained through our collaborations with international and national organizations working in Asia.
Data on the stringency of measures were collected from the University of Oxford for existing indicators. Data on novel indicators that are not part of the OxCGRT were collected from the review results. In addition to policy measures, epidemiological data were also collected to measure the effectiveness of control. These data were collected from authoritative sources including the European Centre for Disease Prevention and Control (ECDC), which has synthesized data from government websites of countries; and the Center for Systems Sciences and Engineering (CSSE) at Johns Hopkins University (JHU) if data on ECDC were not available.
2.3. Indicators and Dimensions to Assess COVID-19 Responses
To measure and evaluate governments’ responses, we created key indicators based on the review results. To create the indicators, we first developed an analytical framework to summarize the control measures used across the study sites, grouped into (i) administrative, (ii) public health, and (iii) health system measures. The analytical framework included important indicators, including the location, intervention, implementation date, specific practices, implementation enablers, and barriers.
We then evaluated these key indicators within each category based on the review result and compared them with those included in the OxCGRT. In cases where an indicator was included to measure the same intervention as that in the OxCGRT, the indicator was kept as-is for consistency. If the indicator was included in our framework but was not already part of the OxCGRT, it was added accordingly.
The final set of indicators includes 11 administrative indicators (A), five public health indicators (P), and two health system indicators (H) (Table 1). Seven out of the 18 indicators are novel and are not part of the OxCGRT. These include coordinated governance (A1), legislation and regulations (A2), transparent communications (A11), quarantine (P3), mask-wearing (P5), increasing the supply of personal protective equipment (PPE) (H1), and building/strengthening health facilities (H2).
Table 1.
List of the indicators included in the evaluation/measurement indices.
| Indicator ID | Included in OxCGRT | Indicator Name | Description |
|---|---|---|---|
| Administrative | |||
| A1 | No | Coordinated governance | Recorded establishing a national task force/committee consisting of leaders from different ministries/sectors |
| A2 | No | Legislation and regulations | Recorded developing or amending existing legislation and regulations for COVID-19 control |
| A3 | Yes | Border control | Recorded border control for COVID-19 control |
| A4 | Yes | Canceling public events | Recorded canceling public events |
| A5 | Yes | Restrictions on gatherings | Recorded the cut-off size for bans on private gatherings |
| A6 | Yes | School closures | Recorded school and university closures |
| A7 | Yes | Workplace closures | Recorded workplace closures |
| A8 | Yes | Stay-at-home requirements | Recorded “shelter-in-place” and otherwise confine to the home |
| A9 | Yes | Closing public transportation | Recorded public transportation closures |
| A10 | Yes | Restrictions on internal movement | Recorded restrictions on moving between regions/cities |
| A11 | No | Transparent communications | Recorded establishing transparent communications working mechanism |
| Public health | |||
| P1 | Yes | Contact tracing | Recorded government policy on contact tracing after a positive diagnosis |
| P2 | Yes | Testing policy | Recorded government policy on who has access to testing |
| P3 | No | Quarantine | Recorded government policy on quarantine |
| P4 | Yes | Public information campaigns | Recorded presence of public information campaigns on COVID-19 |
| P5 | No | Mask-wearing | Recorded mask-wearing policy for COVID-19 control |
| Health system | |||
| H1 | No | Increasing the supply of PPE | Recorded actions on increasing the supply of PPE for health professionals |
| H2 | No | Building/strengthening health facilities | Recorded actions to build or strengthen health facilities |
PPE = Personal Protective Equipment.
2.4. Development of the MSI and the IRI
To evaluate the stringency of the control measures, we used the scaling methodology of OxCGRT [11] to develop the MSI (see Appendix A Table A1 for the codebook). This consisted of assigning an ordinal value (0, 1, 2, 3, 4) to each indicator based on its stringency level. If an indicator contained a range of information, the ordinal value for measures with a targeted population (instead of the general public) would be deducted by 0.5 to reflect its limited effects. A rescaled score between 0 and 100 was then created based on the ordinal value of each indicator, with missing values given a score of 0. The rescaling process was based on its proportion to the maximum ordinal value of this indicator (see Appendix A). These scores were then averaged among all indicators to get the composite index, MSI. To examine heterogeneity across control measure categories, separate scores for the sub-MSI of administrative and public health indicators were calculated. We did not calculate the sub-MSI score of health system measures as the category consists of only two indicators.
To evaluate and compare the timeliness of responses at the early stage of the pandemic, which is crucial for infectious disease control, we developed the Initial Response Index (IRI). The IRI incorporates timeliness into the stringency index through weighting. Each indicator’s stringency index was assigned a time-based weight, which was calculated using 100 confirmed COVID-19 cases [12] as the threshold and the weight of calculated as:
| (1) |
where is the day a control measure was implemented and is the number of confirmed cases for the day before . We took only positive values, and the weighted stringency index of each indicator was averaged to get the IRI value.
2.5. Data Analysis
The developed analytical framework was used to examine and compare control measures across the study sites. In addition, we compared and analyzed the change of MSI and the sub-MSI values using average daily MSI scores, and how they changed relative to the disease outbreak by comparing daily new cases. The IRI was also calculated and compared to evaluate variations in governments’ initial responses.
3. Results
Summary of the Government Response among the Study Sites
This analysis highlighted how the study sites have actively been implementing a package of control measures since the onset of the outbreak, covering administrative, public health, and health system dimensions (Table 2). Administrative measures included effective leadership, legislation, and communication in addition to restricting people’s mobility. One common leadership measure taken across most of the study sites is the establishment of coordinated governance. This entailed setting up a national committee or task force consisting of leaders from different ministries/sectors with high-level political leadership at the early stage of the outbreak [13]. Taiwan and Singapore are particularly noteworthy as they commenced these administrative measure–related efforts and achieved this coordination prior to having any confirmed cases [14,15]. With regard to legislation, the key strategies implemented are either to strengthen or issue new legislation and regulations as well as to provide strong enforcement [16,17,18,19]. Governments of the study sites also emphasized transparent information sharing with the public on the epidemic situation [20,21,22,23,24,25]. The key administrative interventions to restrict or limit people’s mobility included border control, lockdown [26,27], and social distancing. To achieve better implementation of lockdown and social distancing policies, governments have taken actions to control traffic, close non-essential businesses, encourage people to stay at home and work from home, and suspend in-person schooling [28,29].
Table 2.
Summary of government responses to COVID-19 in the study sites, 1 January to 30 May 2020.
| Key Control Measures | Geographic Coverage | Common Practice | Variation in Implementation |
|---|---|---|---|
| Administrative | |||
| Establishing coordinated governance [13,14,15,30,31,32,33,34] | All but JP | Established at the very early stage of the outbreak, with high-level political leadership and commitment, and multi-sectoral or multi-ministerial coordination. | Governments differ in the timeliness of establishing this coordinated high-level leadership (e.g., HK, TW, SG, and VN did so even before there were ≤5 confirmed cases) |
| Amending/adding legislations or regulations [14,16,17,18,19,35,36] | CHN, TW, SG, SK and VN | Governments usually add new regulations or pass new acts related to COVID-19 control, and impose severe penalties to violators for enforcement. | New rules differ in legislative nature (Act, Regulations, etc.), regulated thematic areas and enforcement stringency (e.g., SG and SK have issued strict penalty rules for violation). |
| Transparently sharing epidemiological status [20,22,23,24,25,32] | All | Press conferences were held across the study sites and media tools were used to present timely updates to the public. | Governments differ in the timeliness of establishing these transparent sharing mechanisms. Variations also exist in format and frequency. |
| Implementing mobility restrictions interventions [26,27,28,29,37,38,39,40] | All | Governments have used their executive power to implement administrative interventions to restrict people’s mobility, including border control, lockdowns, and social distancing. Lockdowns and social distancing were achieved through interventions such as traffic control, non-essential business closures, shelter-in-place policies, in-person school closures, etc. | Study sites differ in the package of interventions implemented and the stringency of their implementation. |
| Public Health | |||
| Aggressive contact tracing aided by digital tools [41,42,43,44] | All but JP | Contact tracing is done through massive and careful epidemiological investigations among close contacts of people who test positive. Given its labor-intensive nature, most countries mobilized human resources and adopted digital tools to assist with the process. | All are similar except for Japan, which uses a different cluster-based approach to trace contacts and did not implement aggressive measures, to protect personal privacy. |
| Extensive testing [45,46,47,48,49,50,51,52] | All but JP | Governments focused on conducting nucleic acid amplification tests to detect the virus in suspected cases and in close contacts of confirmed cases. | All are similar except for Japan, which had adopted a restrictive testing approach aiming to not overwhelm its healthcare system. |
| Strict quarantine [48,53,54,55,56,57,58,59,60,61] | All but JP | Quarantine has been implemented among people with infection risk, including close contacts, suspected cases, travelers, and recovered COVID-19 patients. | All are similar except for Japan, in which quarantine policies are comparatively loose and target only travelers. |
| Mask-wearing (compulsory and voluntary) [43,62,63,64,65,66,67] | All | Both healthy and infected people are encouraged to wear masks in public places. | Compulsory mask-wearing was observed in some study sites from the very beginning (e.g., CHN, VN), while voluntary mask-wearing was observed in others (HK, SK and JP). Some adjusted their policy to make mask-wearing compulsory for all, including for healthy people (SG and TW). |
| Disinfecting public places [68] | All | Regular and thorough disinfection of public places, especially those with large population mobility and density. | No variations |
| Widespread temperature screening | All | Wide thermal equipment was set up in public places such as subway entries and airports and manual temperature checks were given to people before entering a residential area or closed building | No variations |
| Health education/awareness campaigns [45] | All | Health education and awareness campaigns were usually implemented on TV, social media, and phones and in public places, etc. | No variations |
| Health system | |||
| Improving health service delivery [45,62,69,70,71] | All | Governments focused on increasing testing capacity, building new health facilities, increasing the supply of PPE, and improving the triage of patients to improve health service delivery. | Governments differ in the timeliness of initiating these actions, and in the resources utilized for implementation. |
| Mobilizing the health workforce [45] | CHN, SG, and SK | Human resources for health were mobilized from other regions to support the most heavily affected places. | Study sites differ in the scale of health workforce mobilization and the types of health workers mobilized. |
| Increasing health financing [24] | All | Effective financing strategies were implemented to cover the majority, if not all, of the testing and treatment costs through health insurance plus special subsidies. | Study sites differ in the costs and population coverage (eg. SK had everything covered). |
| Enhancing health information systems [45] | CHN | Careful monitoring, review, and timely publication of cases and a strong oversight and accountability mechanism | Data unavailable |
CHN = Mainland China; JP = Japan; SG = Singapore; SK = South Korea; TW = Taiwan; VN = Vietnam.
Key public health interventions taken by governments of the study sites concern contact tracing, testing, quarantine, mask-wearing, disinfecting public places, widespread temperature checks, and health education or awareness campaigns. Governments of all the study sites analyzed have taken measures to implement a package of public health interventions, though the components and stringency levels vary. Several similarities in implementation techniques were observed. Most governments within the study sites actively utilized digital and smart tools to achieve more effective implementation with variation [41,42,43,44]. For example, in Japan, a less intrusive method of monitoring was adopted to protect personal privacy. Digital tools have been used for six main purposes: regular documentation and analysis, real-time tracking and alerting, contact tracing, online health consultations and diagnosis, non-human-contact delivery and management, and peer and community reporting (Table 3).
Table 3.
Summary of key digital and smart tools used for controlling COVID-19 in the study sites, 1 January to 30 May 2020.
| Purpose | Data Collected | Intrusiveness | Examples |
|---|---|---|---|
| Regular documentation and analysis | Health, travel history, drug purchase behaviors, etc. | High | CHN, TW, HK—border control health declaration by scanning a QR code [72] CHN—“Health code” [73], drug purchase direct reporting system [34], health self-reporting system, online registration system for employees to contain risk, etc. TW [74]—big data system to integrate health insurance and customs and immigration database; a digital platform to operate a nationalized system of mask distribution, and the “NHI Express App” for users to check mask availability SK—big data system to collect people’s credit card transaction data, CCTV footage, and mobile phone locations etc. |
| Real-time tracking and alert system | Health, travel history, GPS location, CCTV footage, etc. | High | TW [14]—electronic security monitoring system and SMS notifications; social distancing alert app HK [75]—wristbands and mobile app SK [24]—cell phones vibrate with emergency alerts when cases are nearby |
| Contact tracing | Health, basic socio-economic status, travel history, credit card, CCTV footage, etc. | High | CHN [76], TW [14], SK [77], VN [78]—using big data to trace contacts SG [42]—TraceTogether (mobile app) VN [41]—Bluezone (mobile app) |
| Online health consultation and diagnosis | Health, travel history, and other relevant information per request | Medium | CHN [79]—remote consultation with doctors online; AI-assisted diagnosis JP [80], VN [81]—remote consultation SK [82]—self-diagnosis app |
| Non-human-contact delivery and management | N/A | Low | CHN [79,83]— Drones: delivery of goods and medical samples; disinfection; crowd management Robots: meals delivery and disinfection |
| Peer and community support | N/A | Low | CHN [84]—WeChat group to coordinate needs for living essential goods for collective order and delivery SG [85]—“Stay Home for Singapore” portal |
CHN = Mainland China; JP = Japan; SG = Singapore; SK = South Korea; TW = Taiwan; VN = Vietnam; N/A = not available.
Finally, the last category of health system strengthening included measures taken to facilitate the system with the needed capacity to ensure that it continues functioning. Actions have been taken targeting health service delivery, human resources, health financing, and information systems [45,62,69,70,71]. Despite measures being taken, some systems still suffered significantly, especially at the early stage of the outbreak. With no vaccines or known treatment protocols at the time, governments of the study sites focused on increasing testing capacity for fast and accurate diagnosis, building new health facilities or strengthening the capacity of existing health facilities, increasing the supply of PPE, and improving patient triage to facilitate health service delivery. Actively mobilizing human resources has been key to overcoming shortages of health personnel in response to the outbreak. Active mobilization has been implemented in Mainland China, Singapore, and South Korea [45]. The increase of health funds to relieve the financial burden of seeking care was fundamental to be able to expand testing and treatment coverage. Effective health financing strategies have been implemented by governments of the study sites to cover nearly all costs related to testing and treatment. Strengthening health information systems is also observed as a common measure to ensure data quality. This was especially critical for countries with less-developed systems prior to the outbreak.
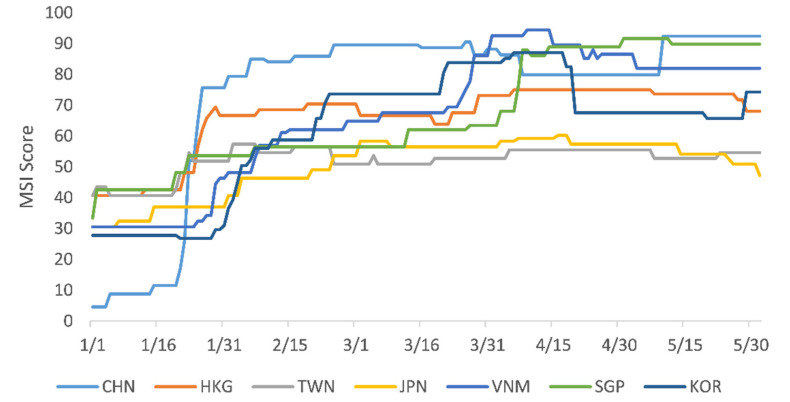
While variations existed among the study sites, generally they have all kept a high stringency level and adjusted it over time (Figure 1). From 1 January to 30 May 2020, the daily average MSI score was 62.8 among the Asian countries. It was highest in Mainland China (74.2), followed by Singapore (67.4), Vietnam (66.8), Hong Kong (66.2), South Korea (62.3), Taiwan (52.1), and Japan (50.3). Observing variations over time, four clear phases with distinct characteristics are evident. The first period is from 1 January to 23 January 2020, when Mainland China fell far behind others—especially Singapore and Hong Kong, which had MSI scores above 40. The second time period is from 23 January to mid-March and is characterized by Mainland China significantly increasing its stringency level to become the highest among the study sites (with mean MSI scores above 85) and others gradually increasing their stringency levels. The third period runs from mid-March to 15 April, when Vietnam, South Korea, and Singapore dramatically increased stringency level while others’ MSI scores remained steady. Finally, the period from 15 April to 30 May can be characterized by reopening, where some countries started to ease stringency levels for economic reasons.
Figure 1.
Change in the MSI score in the study sites, 1 January to 30 May 2020. CHN = China, HKG = Hong Kong; JPN = Japan; KOR = South Korea; SGP = Singapore; TWN = Taiwan; VNM = Vietnam. Data sources: ECDC (https://www.ecdc.europa.eu/en/COVID-19/situation-updates (accessed on 1 July 2020)), CSSE at JHU (https://github.com/CSSEGISandData/COVID-19/blob/master/README.md (accessed on 1 July 2020)).
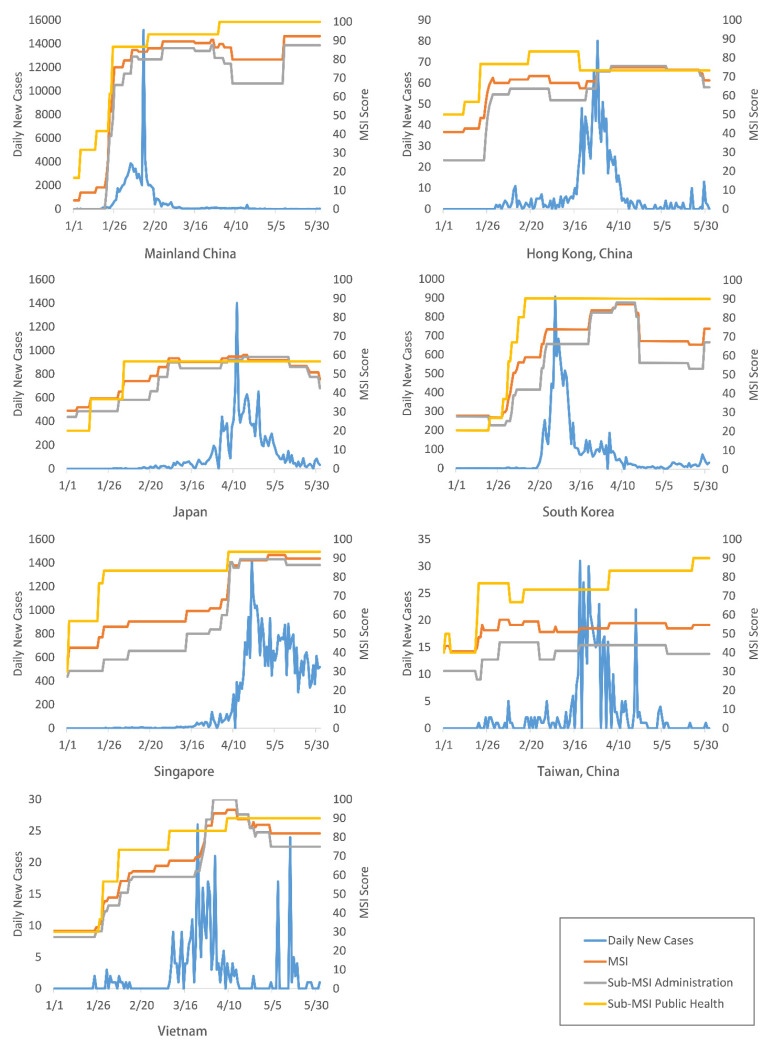
Comparing the change in the MSI and the sub-MSI scores with the number of new daily COVID-19 cases (Figure 2), a common trend can be observed: governments increased stringency levels with the acceleration of the outbreak, and stringency was usually highest at the peak outbreak period. Another common feature across the study sites was the central dependency on public health measures. When increasing stringency levels, public health measures were usually prioritized with higher stringency levels than that of administrative measures. On the other hand, when decreasing stringency levels with outbreak decelerations, governments focused on reducing the stringency of administrative measures only, while keeping or even increasing the stringency levels of public health measures.
Figure 2.
Change of the MSI and sub-MSI relative to disease outbreak in the study sites, 1 January to 30 May 2020. Data sources: ECDC (https://www.ecdc.europa.eu/en/COVID-19/situation-updates (accessed on 1 July 2020)), SSE at JHU (https://github.com/CSSEGISandData/COVID-19/blob/master/README.md (accessed on 1 July 2020)).
Results of the IRI show that there are significant variations among the study sites in terms of the timeliness of initial responses. Hong Kong and Taiwan, which are closest to Mainland China and have learned lessons from the SARS outbreak, acted significantly more expeditiously. IRI scores vary, with Hong Kong (62.4), Taiwan (55.9), Vietnam (53.9), and Singapore (50.1) being the highest, while Japan (42.4), and Mainland China (4.2) follow behind.
4. Discussion
Incident and fatality rates of COVID-19 are generally much lower in the study sites than in other areas at the early phases of the pandemic. Through an extensive review, we find that governments of the study sites have actively undertaken a series of administrative, public health, and health system–related measures to control the COVID-19 pandemic.
Though variations in control measures exist, the main measures are consistent across the study sites, providing lessons for disease control. The MSI scores showed variation in the stringency of the implemented control measures across the study sites and within each site over time. The common trends are they usually increased the stringency with the acceleration of the outbreak and prioritized the public health measures. This can be attributed to the flexibility and ease of adaption of public health measures compared to other measures. Results of the IRI provide new insights on the importance of the timeliness of government response and how expeditiously the governments of the study sites acted at the onset of the outbreak. Variations in the timeliness of the initial response were observed: Hong Kong, Taiwan, Vietnam, and Singapore acted much more expeditiously at the onset of the outbreak to implement control measures. Results emphasize the importance of early and timely catchup of implementing control measures, emphasized by the case of Mainland China, which fell behind initially but was able to catch up and surpass others in the study sites.
To our knowledge, this is the first study that has systematically examined control measures by category within the study sites and quantified the timeliness of the initial response. These findings and distilled experiences become especially important to governments globally at the current timing, considering the wide-spread transmission of the Delta variant globally and the reduced effectiveness of the vaccines against it [4,5]. Due to the early identification of COVID-19 cases and overall good performance of the governments of the study sites in responding to the pandemic, previous studies have focused on summarizing the control measures and evaluating their effectiveness, usually done in a single Asian country or subregion such as Mainland China [6,7,9,86], Taiwan [49,87], Singapore [8,88], or South Korea [77,82,89]. Additionally, the OxCGRT, which included 19 indicators to evaluate and compare the stringency level of the control measures across countries, has been used in a few studies to analyze the variation of government response [90] and link the stringency of the OxGGRT with the change of epidemiological indicators [91,92,93].
A distinctive feature of the governments of the study sites is their experience dealing with previous epidemics, thus being prepared with a stock of evidence-based policies. Their experience gave these sites the advantage and ability to react in a timely and effective manner to control the COVID-19 pandemic. Mainland China [94], Hong Kong [95], Taiwan [49,96], and Singapore [8] were severely hit by SARS in 2003. Japan [97] and Taiwan [49] experienced the outbreak of H1N1 in 2009, and South Korea [98] was hit by MERS in 2015. Based on their previous experiences, governments of the study sites took five key actions to improve their response before the COVID-19 pandemic: (i) develop new or amend existing legislation on infectious disease prevention and control [24,94,95,99,100,101]; (ii) set up a government-led organizational structure and mechanism to fight against the emerging infectious diseases [8,74,94,96]; (iii) strengthen infectious disease diagnosis and treatment capacity and reporting system [8,49,94,102]; (iv) improve communication to ensure effective, rapid, and transparent communication between the government and the public [49,94,102]; and (v) strengthen social norms toward controlling infectious diseases among the general population, such as voluntary mask-wearing among the general public.
Based on the results discussed above, we propose several key policy recommendations for COVID-19 pandemic control and pandemic preparedness. First, establishing a well-functioning legislative and organizational structure to guide the response is vital. Second, timely activation of the response mechanism and undertaking evidence-based control measures promptly and dynamically is critical. Public health control measures are particularly important and should febe prioritized and not eased, even with outbreak deceleration. Third, timely and transparent communications with the public and other key stakeholders are highly imperative to reduce panic and boost people’s trust in government. Fourth, ensuring universal access to testing and treatment for all people is critical. Fifth, strengthening the health system is an on-going process and has to be prioritized for effective emergency preparedness response. Last, strengthening surveillance and reporting systems of infectious diseases cannot be ignored, especially in countries where information systems are less developed. In addition, all central governments should develop a realistic and practical roadmap for reopening their economy and businesses.
The current study has several limitations. Firstly, this study is not representative, since a purposive selection of sites was conducted. Additionally, the information collected is not balanced across the study sites, largely because of language barriers and data availability. For example, we find Japan has published significant amounts of COVID-19-related information in Japanese, and evidence related to Vietnam is less rich. Also, though the evaluation indices add indicators to previously used indices, they contain only 18 indicators. These have not captured all the important control measures found based on the review, especially in the health system group, because of limited data availability. We also rely on the number of cases to assess the timeliness of the response in the IRI; this is potentially biased, as the number of confirmed cases is highly dependent on the testing capacity. However, these are the best data available. In addition, the 100-case threshold used for early response is arbitrary and based on literature, given that there is no universal standard. Finally, the data was collected from January to May 2020, failing to include the recent response changes due to the COVID-19 variants (e.g., Delta variant). However, the control measures do not change much except for that some governments tightened them up, such as prolonging the quarantine days, expanding the definition on close contacts et al. We believe lessons drawn from the current study apply to the control of the Delta variant and future pandemics. Future studies can improve on the methodology as more data and information become available and can expand the range of countries to explore how the MSI and IRI correlate with the change of COVID-19 epidemiological indicators to provide feasible policy implications.
5. Conclusions
Governments of the study sites in Asia have implemented a series of similar administrative, public health, and health system measures to control the COVID-19 pandemic, though with variations in components, stringency, and timeliness of the initial response. Results based on extensive literature review and in-depth analysis reveal that setting and adapting the stringency of control measures, especially public health measures, according to outbreak accelerations, and reacting expeditiously are key to controlling outbreaks. Such results imply that governments can enhance their response to better control COVID-19 through strengthening its legislative and organizational structure, timely activating the response mechanism and undertaking evidence-based control measures, establishing timely and transparent communications with the public and other key stakeholders, ensuring universal access to testing and treatment for all, and improving the surveillance system.
Acknowledgments
We acknowledge Joao Ricardo N. Vissoci from DGHI for his constructive comments, Michelle Pender from DGHI for her language polish, and Jiawen Wu, a master’s student from DGHI for her excellent research assistance on data collection. The authors are grateful for continued support from Sameh El-Saharty, World Bank Human Development Program Lead, GCC countries, Rekha Menon, World Bank Practice Manager, Health Nutrition and Population, Middle East and North Africa region and Katelyn Jison Yoo, World Bank Asia Team.
Appendix A
Table A1.
Indicator codebook.
| ID | Indicators Name | Meaurment | Coding Instructions |
|---|---|---|---|
| A1 | Coordinated governance | Ordinal | 0—No measures 1—Health sector coordination 2—Established multi-sector coordinated leading/governance team Blank—No data |
| A2 | Legislation and regulations | Binary | 0—No measures 1—Amended existing or developed new legisltions or regulations for COVID-19 Blank—No data |
| A3 | Border control | Ordinal | 0—No measures 1—Open to all countries with travelers * screening 2—Border closure with targeted countries 3—Border closure with all countries Blank—No data |
| A4 | Canceling public events | Ordinal scale + binary for geographic scope | 0—No measures 1—Recommended cancellation 2—Required cancellation Blank—No data 0—Targeted 1—General Blank—No data |
| A5 | Restrictions on gatherings | Ordinal scale + binary for geographic scope | 0—No restrictions 1—Restrictions on very large gatherings (the limit is above 1000 people) 2—Restrictions on gatherings between 101 and 1000 people 3—Restrictions on gatherings between 11 and 100 people 4—Restrictions on gatherings of 10 people or less Blank—No data 0—Targeted 1—General Blank—No data |
| A6 | In-person school closures | Ordinal scale + binary for geographic scope | 0—No measures 1—Recommended closing 2—Required closing at some levels 3—Required closing at all levels Blank—No data 0—Targeted 1—General Blank—No data |
| A7 | In-person workplace closures | Ordinal scale + binary for geographic scope | 0—No measures 1—Recommended closing (or recommend work from home) 2—Required closing (or work from home) for some sectors or categories of workers 3—Required closing (or work from home) for all-but-essential workplaces (e.g., grocery stores, doctors) Blank—No data 0—Targeted 1—General Blank—No data |
| A8 | Stay-at-home requirements | Ordinal scale + binary for geographic scope | 0—No measures 1—Recommended not leaving the house 2—Required not leaving the house with exceptions for daily exercise, grocery shopping, and “essential” trips 3—Required not leaving the house with minimal exceptions (e.g., allowed to leave once a week, or only one person can leave at a time, etc.) Blank- No data 0—Targeted 1—General Blank—No data |
| A9 | Closing public transportation | Ordinal scale + binary for geographic scope | 0—No measures 1—Recommended closing (or significantly reduced volume/route/means of transport available) 2—Required closing (or prohibited most citizens from using it) Blank—No data 0—Targeted 1—General Blank—No data |
| A10 | Restrictions on internal movement | Ordinal | 0—no measures 1—Recommended not to travel between regions/cities 2—Internal movement restrictions in place Blank—Bo data 0—Targeted 1—General Blank—No data |
| A11 | Transparent communications | Ordinal | 0—No measures 1—Establishing a transparent communications mechanism by the government though with pauses 2—Establishing nonstop transparent communications by the government on COVID-19 Blank—No data |
| P1 | Contact tracing | Ordinal | 0—No contact tracing 1—Limited contact tracing; not done for all cases 2—Comprehensive contact tracing; done for all identified cases Blank—No data |
| P2T | Testing policy | Ordinal | 0—No testing policy 1—Only those who both (a) have symptoms AND (b) meet specific criteria (e.g., key workers, admitted to hospital, came into contact with a known case, returned from overseas) 2—Testing of anyone showing COVID-19 symptoms 3—Open public testing (e.g., “drive through” testing available to asymptomatic people) Blank—No data |
| P3 | Quarantine | Ordinal | 0—No quarantine policy 1—Only targeted to international travelers 2—Quarantining all persons with infection risks, including travelers, close contacts, suspected cases and recovered patients Blank—No data |
| P4 | Public information campaigns | Ordinal | 0—No COVID-19 public information campaign 1—Public officials urging caution about COVID-19 2—Coordinated public information campaigns (e.g., across traditional and social media) Blank—No data |
| P5 | Mask-wearing | Ordinal | 0—No measures 1—Recommended mask-wearing in public places 2—Compulsory mask-wearing in public places Blank—No data |
| H1 | Increasing the supply of PPE | Ordinal | 0—No measures 1—Some action to increase the supply of PPE 2—Used all-societal resources to the increase supply of PPE Blank—No data |
| H2 | Building/strengthening health facilities | Ordinal | 0—No measures 1—Renovated health facilities or strengthen infection control in health facilities 2—Built new health facilities for COVID-19 patients only Blank—No data |
* Different from OxCGRT’s coding: code 1 (Screening) and 2 (Quarantine arrivals from high-risk regions) in the OxCGRT were merged into code 1 in our codebook.
Author Contributions
S.C.; T.A.; M.A.; D.D.; C.H.H. and S.T. conceived and designed the study. S.C.; X.Z. and G.C.A.T. collected data. S.C. and L.G. conducted data analysis. S.C. and S.T. drafted the manuscript with input from all authors. D.D.; T.A.; M.A.; M.M.H.; R.A.; Y.Z.; N.A.; R.S. and C.H.H. provided critical inputs and comments on the manuscript. All authors contributed to revising the manuscript and approved the version to be submitted and published. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the Health, Nutrition and Population Reimbursable Advisory Services Program (P172148) between the World Bank and the Ministry of Finance in Saudi Arabia. Duke Global Health Institute (DGHI) has supported research assistantships for the literature review of the study. Research members from the funding institutions participated in the study design, data analysis, interpretation, preparation, writing and submission of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data used for analysis are all available in the manuscript and appendix.
Conflicts of Interest
The authors declare no conflict of interests.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Roser M., Ritchie H., Ortiz-Ospina E., Hasell J. Coronavirus Pandemic (COVID-19). Our World Data. Published Online 4 March 2020. [(accessed on 2 August 2021)]; Available online: https://ourworldindata.org/coronavirus.
- 2.COVID-19 Situation Update Worldwide, As of Week 50 2020. European Centre for Disease Prevention and Control. [(accessed on 18 December 2020)]; Available online: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases.
- 3.SARS-CoV-2 Variants. World Health Organization. [(accessed on 25 January 2021)]; Available online: http://www.who.int/csr/don/31-december-2020-sars-cov2-variants/en/
- 4.World Health Organization Tracking SARS-CoV-2 Variants. [(accessed on 4 August 2021)]; Available online: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/
- 5.Lopez Bernal J., Andrews N., Gower C., Gallagher E., Simmons R., Thelwall S., Stowe J., Tessier E., Groves N., Dabrera G., et al. Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. N. Engl. J. Med. 2021 doi: 10.1056/NEJMoa2108891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prem K., Liu Y., Russell T.W., Kucharski A.J., Eggo R.M., Davies N. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: A modelling study. Lancet Public Health. 2020;5:e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leung K., Wu J.T., Liu D., Leung G.M. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: A modelling impact assessment. Lancet. 2020;395:1382–1393. doi: 10.1016/S0140-6736(20)30746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong J.E.L., Leo Y.S., Tan C.C. COVID-19 in Singapore—Current Experience: Critical Global Issues That Require Attention and Action. JAMA. 2020;323:1243. doi: 10.1001/jama.2020.2467. [DOI] [PubMed] [Google Scholar]
- 9.Pan A., Liu L., Wang C., Guo H., Hao X., Wang Q., Huang J., He N., Yu H., Lin X., et al. Association of Public Health Interventions With the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA. 2020;323:1–9. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas H., Webster S., Petherick A., Phillips T., Kira B. Oxford COVID-19 Government Response Tracker. Blavatnik School of Government. [(accessed on 20 December 2020)]; Available online: https://www.bsg.ox.ac.uk/research/research-projects/coronavirus-government-response-tracker.
- 11.OxCGRT/Covid-Policy-Tracker. GitHub. [(accessed on 20 December 2020)]; Available online: https://github.com/OxCGRT/covid-policy-tracker.
- 12.Hartfield M., Alizon S. Introducing the outbreak threshold in epidemiology. PLOS Pathog. 2013;9:e1003277. doi: 10.1371/journal.ppat.1003277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Party Central Committee Sets Up a Leading Group for Epidemic Response. The Paper. [(accessed on 1 July 2020)]; Available online: https://www.thepaper.cn/newsDetail_forward_5639081.
- 14.Prevention and Control of COVID-19 in Taiwan. [(accessed on 1 July 2020)]; Available online: https://www.cdc.gov.tw/En/Category/Page/0vq8rsAob_9HCi5GQ5jH1Q.
- 15.Low J. COVID-19 Crisis Management: An Early Look. Ethos. [(accessed on 3 June 2020)]; Available online: https://www.csc.gov.sg/articles/covid-19-crisis-management-an-early-look.
- 16.Law to Cope with Coronavirus Impact Clears Legislative Floor—Focus Taiwan. [(accessed on 1 July 2020)]; Available online: https://focustaiwan.tw/politics/202002250010.
- 17.Shanghai, Tianjin, Chongqing, and ANHUI Launch a First-Level Response Mechanism for Major Public Health Emergencies. Chinese Government Website. [(accessed on 1 July 2020)]; Available online: http://www.gov.cn/xinwen/2020-01/24/content_5472050.htm.
- 18.Protection from Online Falsehoods and Manipulation Act. POFMA Office. [(accessed on 1 July 2020)]; Available online: https://www.pofmaoffice.gov.sg/regulations/protection-from-online-falsehoods-and-manipulation-act/
- 19.Umeda S. South Korea: Parliament Responded Quickly to COVID-19 by Amending Three Acts. Global Legal Monitor. Published 4 June 2020. [(accessed on 1 July 2020)]; Available online: http://www.loc.gov/law/foreign-news/article/south-korea-parliament-responded-quickly-to-covid-19-by-amending-three-acts/
- 20.Q68: How Did the Chinese Government Address Misinformation Amid the COVID-19 Outbreak? Center for International Knowledge on Development, China (CIKD) [(accessed on 1 July 2020)]; Available online: http://www.cikd.org/english/detail?leafId=213&docId=1420.
- 21.Department of Health—Press Release. [(accessed on 1 July 2020)]; Available online: https://www.dh.gov.hk/textonly/english/press/2020/press_2020.html.
- 22.Lessons from Taiwan’s Experience with COVID-19. Atlantic Council. Published 7 April 2020. [(accessed on 1 July 2020)]; Available online: https://www.atlanticcouncil.org/blogs/new-atlanticist/lessons-from-taiwans-experience-with-covid-19/
- 23.Legal News. SingaporeLegalAdvice.com. [(accessed on 1 July 2020)]; Available online: https://singaporelegaladvice.com/legal-news/
- 24.How South Korea Flattened the Curve. ProQuest. [(accessed on 1 July 2020)]; Available online: http://search.proquest.com/docview/2381936994/C3AECB690C424A35PQ/1?accountid=10598.
- 25.Information on the Novel Coronavirus Diseases (COVID-19). Ministry of Foreign Affairs of Japan. [(accessed on 1 July 2020)]; Available online: https://www.mofa.go.jp/p_pd/pds/page22e_000910.html.
- 26.China ends 76-Day Lockdown of Wuhan City, Where the Virus Outbreak Started. CNBC. Published 8 April 2020. [(accessed on 1 July 2020)]; Available online: https://www.cnbc.com/2020/04/08/coronavirus-china-ends-lockdown-of-wuhan-city-where-outbreak-started.html.
- 27.Singapore to Close Schools, Most Workplaces with Rising Virus Cases. Bloomberg.com. Published 3 April 2020. [(accessed on 1 July 2020)]; Available online: https://www.bloomberg.com/news/articles/2020-04-03/singapore-pm-says-more-steps-coming-on-virus-lee-speaks-at-4pm.
- 28.All Schools in Japan Told to Close Until April over Virus Outbreak. The Japan Times. [(accessed on 1 July 2020)]; Available online: https://www.japantimes.co.jp/news/2020/02/27/national/hokkaido-coronavirus-school/
- 29.MOE Postpones Start of 2020 Spring Semester. Ministry of Education of the People’s Republic of China. [(accessed on 1 July 2020)]; Available online: https://en.moe.gov.cn/news/press_releases/202001/t20200130_417069.html.
- 30.CE Announces Activation of Emergency Response Level in Relation to Novel Coronavirus Infection. [(accessed on 1 July 2020)]; Available online: https://www.info.gov.hk/gia/general/202001/26/P2020012600087.htm.
- 31.CHP Closely Monitors Cluster of Pneumonia Cases on Mainland. [(accessed on 1 July 2020)]; Available online: https://www.info.gov.hk/gia/general/201912/31/P2019123100667.htm.
- 32.Ha B.T.T., Ngoc Quang L., Mirzoev T., Tai N.T., Thai P.Q., Dinh P.C. Combating the COVID-19 epidemic: Experiences from Vietnam. Int. J. Environ. Res. Public Health. 2020;17:3125. doi: 10.3390/ijerph17093125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Legislative Council of the Hong Kong Special Administrative Region. Panel on Health Services (Papers) [(accessed on 1 July 2020)]; Available online: https://www.legco.gov.hk/yr19-20/english/panels/hs/papers/hs_n6.htm.
- 34.Coronavirus Disease 19(COVID-19). Ministry of Health and Welfare. [(accessed on 1 July 2020)]; Available online: http://ncov.mohw.go.kr/en/
- 35.Guangdong Province Decides to Initiate a Primary Response to Major Public Health Emergencies. Highlights. [(accessed on 1 July 2020)]; Available online: http://www.sz.gov.cn/szzt2010/yqfk2020/ywjj/content/post_6685320.html.
- 36.Hubei Launches Level I Response to Major Public Health Emergencies. The Paper. [(accessed on 1 July 2020)]; Available online: https://www.thepaper.cn/newsDetail_forward_5621889.
- 37.Singapore Pledges $2.7 Billion More, Virus Measures Extended. Bloomberg.com. Published 21 April 2020. [(accessed on 1 July 2020)]; Available online: https://www.bloomberg.com/news/articles/2020-04-21/singapore-extends-partial-lockdown-measures-until-june-1.
- 38.Ministry of Health & Welfare: News & Welfare Services. [(accessed on 1 July 2020)]; Available online: https://www.mohw.go.kr/eng/nw/nw0101vw.jsp?PAR_MENU_ID=1007&MENU_ID=100701&page=1&CONT_SEQ=353953.
- 39.COVID-19 (Temporary Measures) (Control Order) Regulations 2020. Singapore Statutes Online. [(accessed on 1 July 2020)]; Available online: https://sso.agc.gov.sg/SL/COVID19TMA2020-S254-2020?DocDate=20200407.
- 40.Tokyo Governor Urges People to Stay Indoors over Weekend as Virus Cases Spike. The Japan Times. [(accessed on 1 July 2020)]; Available online: https://www.japantimes.co.jp/news/2020/03/25/national/science-health/tokyo-logs-40-coronavirus-cases/
- 41.COVID-19 Emergency Strength Disease Page. Health Ministry. [(accessed on 1 July 2020)]; Available online: https://ncov.moh.gov.vn/
- 42.Help Speed up Contact Tracing with TraceTogether. [(accessed on 1 July 2020)]; Available online: http://www.gov.sg/article/help-speed-up-contact-tracing-with-tracetogether.
- 43.South Korea Keeps Covid-19 at bay without a Total Lockdown. The Economist. [(accessed on 1 July 2020)]; Available online: http://www.economist.com/asia/2020/03/30/south-korea-keeps-covid-19-at-bay-without-a-total-lockdown.
- 44.COVID-19 Strategy: The Japan Model. [(accessed on 1 July 2020)]; Available online: https://thediplomat.com/2020/04/covid-19-strategy-the-japan-model/
- 45.Bingqin L., Xiao C. Proactive and coordinated response to COVID-19: Comparing the experience of China, South Korea and Singapore during the first 100 days. [(accessed on 1 July 2020)]; Available online: http://cikd.org/english/detail?leafId=213&docId=1540.
- 46.Wuhan City: Epidemiological Investigation and Testing of Five Types of Personnel. Hubei Provincial Health Commission. [(accessed on 1 July 2020)]; Available online: http://wjw.hubei.gov.cn/bmdt/mtjj/mtgz/202004/t20200421_2236177.shtml.
- 47.National Screening, Wuhan Fights again. Hubei Provincial Health Commission. [(accessed on 1 July 2020)]; Available online: http://wjw.hubei.gov.cn/bmdt/mtjj/mtgz/202005/t20200521_2283084.shtml.
- 48.Wong S.Y.S., Kwok K.O., Chan F.K.L. What can countries learn from Hong Kong’s response to the COVID-19 pandemic? Can. Med. Assoc. J. 2020;192:E511–E515. doi: 10.1503/cmaj.200563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: Big data analytics, new technology, and proactive testing. JAMA. 2020;323:1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 50.Ng Y. Evaluation of the effectiveness of surveillance and containment measures for the first 100 patients with COVID-19 in Singapore: 2 January–29 February 2020. MMWR Morb Mortal Wkly Rep. 2020;69:307. doi: 10.15585/mmwr.mm6911e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Viet Nam Has Conducted 275,000 COVID-19 Tests, Health Official Says—Viet Nam Has Conducted 275,000 COVID-19 Tests, Health Official Says. [(accessed on 1 July 2020)];VGP News. Available online: http://news.chinhphu.vn/Home/Viet-Nam-has-conducted-275000-COVID19-tests-health-official-says/20205/40083.vgp.
- 52.Siripala T. Japan’s Surge in COVID-19 Infections Threatens to Derail Healthcare System. [(accessed on 1 July 2020)]; Available online: https://thediplomat.com/2020/04/japans-surge-in-covid-19-infections-threatens-to-derail-healthcare-system/
- 53.KCDC [(accessed on 1 July 2020)]; Available online: http://www.cdc.go.kr.
- 54.Q32: Why do COVID-19 Patients Need Collective or Home Quarantine for 14 Days after Being Discharged from Hospitals? Center for International Knowledge on Development, China (CIKD) [(accessed on 1 July 2020)]; Available online: http://www.cikd.org/english/detail?leafId=213&docId=1321.
- 55.[Q&A] All Overseas Arrivals Required to Spend 2 Weeks in Quarantine as of 1 April. [(accessed on 1 July 2020)]; Available online: http://english.hani.co.kr/arti/english_edition/e_national/935085.html.
- 56.China (Taiwan) M of FA Republic of. FAQ: Taiwan’s 14-Day Quarantine Requirements. [(accessed on 1 July 2020)];Taiwan Today. 2020 Mar 18; Available online: https://taiwantoday.tw/news.php?unit=2&post=173589.
- 57.Everything You Need to Know about Quarantine Orders. [(accessed on 1 July 2020)]; Available online: http://www.gov.sg/article/everything-you-need-to-know-about-quarantine-orders.
- 58.New Covid-19 Tourism Policies in Vietnam. Vietnam Tourism. [(accessed on 1 July 2020)]; Available online: http://vietnam.travel/things-to-do/covid-19-travel-policies-vietnam.
- 59.Welle D. How Vietnam Is Winning Its “War” on Coronavirus. DW.COM. [(accessed on 1 July 2020)]; Available online: https://www.dw.com/en/how-vietnam-is-winning-its-war-on-coronavirus/a-52929967.
- 60.Coronavirus Travel Restrictions and Bans Globally: Updating List. [(accessed on 1 July 2020)];The New York Times. Available online: https://www.nytimes.com/article/coronavirus-travel-restrictions.html.
- 61.Japan Imposes 14-Day Self-Quarantine for Travelers from United States. Stars and Stripes. [(accessed on 1 July 2020)]; Available online: https://www.stripes.com/news/pacific/japan-imposes-14-day-self-quarantine-for-travelers-from-united-states-1.623498.
- 62.Chen L., Xiao C. China’s Strategies and Actions Against COVID-19 and Key Insights. [(accessed on 1 July 2020)]; Available online: http://www.cikd.org/english/detail?leafId=213&docId=1541.
- 63.Huynh T.L.D. The COVID-19 containment in Vietnam: What are we doing? J. Glob. Health. 2020;10:010338. doi: 10.7189/jogh.10.010338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.How to Redeem the New Reusable Mask. [(accessed on 1 July 2020)]; Available online: https://www.gov.sg/article/when-should-i-wear-a-mask.
- 65.Maintain Social Distancing, Wear Masks and Take Public Transportation to Prevent Wuhan Pneumonia. [(accessed on 1 July 2020)];Taiwan English News. Available online: https://www.taiwannews.com.tw/ch/news/3910606.
- 66.Cheng V.C., Wong S., Chuang V.W., So S.Y., Chen J.H., Sridhar S., To K.K., Chan J.F., Hung I.F., Ho P., et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020;81:107–114. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Face Masks in a Pandemic: From “Useless” to “Indispensable”. [(accessed on 1 July 2020)];The Japan Times. Available online: https://www.japantimes.co.jp/news/2020/05/01/world/science-health-world/face-masks-pandemic/
- 68.Environmental Cleaning Guidelines. National Environmental Agency of Singapore. [(accessed on 1 July 2020)]; Available online: https://www.nea.gov.sg/our-services/public-cleanliness/environmental-cleaning-guidelines.
- 69.Lin C., Braund W.E., Auerbach J., Chou J.H., Teng J.H., Tu P., Mullen J. Policy decisions and use of information technology to fight COVID-19, Taiwan. Emerg. Infect. Dis. J. 2020;26:1506. doi: 10.3201/eid2607.200574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.What Can Data on Testing Tell Us about the Pandemic? Our World in Data. [(accessed on 1 July 2020)]; Available online: https://ourworldindata.org/what-can-data-on-testing-tell-us-about-the-pandemic.
- 71.Nguyen D. Vietnam Successfully Designs Test Kit for New Coronavirus. Vietnam Insider. Published 4 March 2020. [(accessed on 1 July 2020)]; Available online: https://vietnaminsider.vn/vietnam-successfully-designs-test-kit-for-new-coronavirus/
- 72.Utzerath F.B.D.L.-J., Bird R., Cheng G. Contact Tracing Apps in China, Hong Kong, Singapore and South Korea | Lexology. [(accessed on 30 June 2020)]; Available online: https://www.lexology.com/library/detail.aspx?g=99dca469-455d-4f7a-b025-00bf1d10ff6b.
- 73.Q41: Health Code: What and How? Center for International Knowledge on Development, China (CIKD) [(accessed on 20 December 2020)]; Available online: http://www.cikd.org/english/detail?leafId=213&docId=1342.
- 74.Fighting Covid-19: East Asian Responses to the Pandemic. Institut Montaigne. [(accessed on 30 June 2020)]; Available online: https://www.institutmontaigne.org/en/publications/fighting-covid-19-east-asian-responses-pandemic.
- 75.Saiidi U. Hong Kong Is Putting Electronic Wristbands on Arriving Passengers to Enforce Coronavirus Quarantine. CNBC. Published 18 March 2020. [(accessed on 30 June 2020)]; Available online: https://www.cnbc.com/2020/03/18/hong-kong-uses-electronic-wristbands-to-enforce-coronavirus-quarantine.html.
- 76.Zou H., Shu Y., Feng T. How Shenzhen, China avoided widespread community transmission: A potential model for successful prevention and control of COVID-19. Infect. Dis. Poverty. 2020;9:1–4. doi: 10.1186/s40249-020-00714-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Park O., Park Y.J., Park S.Y., Kim Y.M., Kim J., Lee J., Park E., Kim D., Jeon B.H., Ryu B., et al. Contact transmission of COVID-19 in South Korea: Novel investigation techniques for tracing contacts. Osong Public Health Res. Perspect. 2020;11:60–63. doi: 10.24171/j.phrp.2020.11.1.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Vietnam’s Exemplary Response to COVID-19. The ASEAN Post. [(accessed on 30 June 2020)]; Available online: https://theaseanpost.com/article/vietnams-exemplary-response-covid-19.
- 79.Robots and Drones are Now Used to Fight COVID-19. [(accessed on 30 June 2020)]; Available online: https://www.forbes.com/sites/bernardmarr/2020/03/18/how-robots-and-drones-are-helping-to-fight-coronavirus/#580cc37b2a12.
- 80.Remote Platform, Bluezone App Launched in Support of Medical Treatment, Including COVID-19. [(accessed on 30 June 2020)];VGP News. Available online: http://news.chinhphu.vn/Home/Remote-platform-Bluezone-app-launched-in-support-of-medical-treatment-including-COVI19/20204/39790.vgp.
- 81.Japanese Ministry, METI, Launches Free Remote Health Consultation Service to Address COVID-19 Related Concerns. [(accessed on 30 June 2020)];Healthcare IT News. 2020 Mar 24; Available online: https://www.healthcareitnews.com/news/asia-pacific/japanese-ministry-meti-launches-free-remote-health-consultation-service-address.
- 82.Lee D., Lee J. Testing on the move: South Korea’s rapid response to the COVID-19 pandemic. Transp. Res. Interdiscip. Perspect. 2020;5:100111. doi: 10.1016/j.trip.2020.100111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.3 Ways China Is Using Drones to Fight Coronavirus. World Economic Forum. [(accessed on 30 June 2020)]; Available online: https://www.weforum.org/agenda/2020/03/three-ways-china-is-using-drones-to-fight-coronavirus/
- 84.Sealed in: Chinese Trapped at Home by Coronavirus Feel the Strain. Reuters. Published 22 February 2020. [(accessed on 30 June 2020)]; Available online: https://www.reuters.com/article/us-china-health-quarantine-idUSKCN20G0AY.
- 85.Hermesauto. Coronavirus: Stay Home for Singapore Portal Launched to Help People Make Purposeful Use of Time during Circuit Breaker. [(accessed on 30 June 2020)];The Straits Times. 2020 Apr 11; Available online: https://www.straitstimes.com/singapore/coronavirus-stay-home-for-singapore-portal-launched-to-help-people-make-purposeful-use-of.
- 86.Bi Q., Wu Y., Mei S., Ye C., Zou X., Zhang Z., Liu X., Wei L., Truelove S.A., Zhang T., et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts inShenzhen, China: A retrospective cohort study. Lancet Infect. Dis. 2020;20:911–919. doi: 10.1016/S1473-3099(20)30287-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chang M.-C., Kahn R., Li Y.-A., Lee C.-S., Buckee C.O., Chang H.-H. Modeling the impact of human mobility and travel restrictions on the potential spread of SARS-CoV-2 in Taiwan. medRxiv. 2020 doi: 10.1101/2020.04.07.20053439. [DOI] [Google Scholar]
- 88.Koo J.R., Cook A.R., Park M., Sun Y., Sun H., Tao J., Clarence L., Borame T., Dickens L. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: A modelling study. Lancet Infect. Dis. 2020;20:678–688. doi: 10.1016/S1473-3099(20)30162-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yoo K.J., Kwon S., Choi Y., Bishai D. Systematic Assessment of South Korea’s Capabilities to Control COVID-19. Health Policy J. 2021;125:568–576. doi: 10.1016/j.healthpol.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Variation in Government Responses to COVID-19. [(accessed on 21 December 2020)]; Available online: https://www.bsg.ox.ac.uk/research/publications/variation-government-responses-covid-19.
- 91.Koh W.C., Naing L., Wong J. Estimating the impact of physical distancing measures in containing COVID-19: An empirical analysis. Int. J. Infect. Dis. 2020;100:42–49. doi: 10.1016/j.ijid.2020.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dergiades T., Milas C., Panagiotidis T. How Effectively Have Governments Responded to COVID-19 so Far? British Politics and Policy at LSE. Published 1 June 2020. [(accessed on 21 December 2020)]; Available online: https://blogs.lse.ac.uk/politicsandpolicy/
- 93.Liu Y., Morgenstern C., Kelly J., Lowe R., CMMID COVID-19 Working Group. Jit M. The Impact of Non-Pharmaceutical Interventions on SARS-CoV-2 Transmission across 130 Countries and Territories. Health Policy. 2020;19:1–12. doi: 10.1101/2020.08.11.20172643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nkengasong J. China’s response to a novel coronavirus stands in stark contrast to the 2002 SARS outbreak response. Nat. Med. 2020;26:310–311. doi: 10.1038/s41591-020-0771-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Choi S.M.Y., Lam P.Y. Enhancing legal preparedness for the prevention and control of infectious diseases: Experience from severe acute respiratory syndrome in Hong Kong. Public Health. 2009;123:242–246. doi: 10.1016/j.puhe.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.NHCC [(accessed on 1 July 2020)]; Available online: https://www.cdc.gov.tw/En/Category/MPage/gL7-bARtHyNdrDq882pJ9Q.
- 97.Okabe N. Epidemiological situation on pandemic influenza H1N1 2009 in the world and in Japan. JMAJ. 2011;54:277–283. [Google Scholar]
- 98.2015 MERS outbreak in Republic of Korea. [(accessed on 23 December 2020)]; Available online: https://www.who.int/westernpacific/emergencies/2015-mers-outbreak.
- 99.Category of Communicable Disease Control. Taiwan Centers for Disease Control. [(accessed on 1 July 2020)]; Available online: https://www.cdc.gov.tw/En/Category/ListPage/HrXtdwzKFsLSdd6z2a1x5A.
- 100.Communicable Disease Control Act. Laws & Regulations Database of the Republic of China. [(accessed on 1 July 2020)]; Available online: https://law.moj.gov.tw/ENG/LawClass/LawHistory.aspx?pcode=L0050001.
- 101.Normile D. Coronavirus Cases Have Dropped Sharply in South Korea. What’s the Secret to its Success? Science|AAAS. Published 17 March 2020. [(accessed on 1 July 2020)]; Available online: https://www.sciencemag.org/news/2020/03/coronavirus-cases-have-dropped-sharply-south-korea-whats-secret-its-success.
- 102.Oh M., Park W.B., Park S., Choe P.G., Bang J.H., Song K., Kim E.S., Kim H.B., Kim N.J. Middle East respiratory syndrome: What we learned from the 2015 outbreak in the Republic of Korea. Korean J. Intern. Med. 2018;33:233–246. doi: 10.3904/kjim.2018.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used for analysis are all available in the manuscript and appendix.