Abstract
Dental biofilm is often found to be the source of bacteria that releases toxins, peptides, lipopolysaccharides as well as organic acids, which lead to gingival inflammation and tooth caries. Further, the persistent plaque may result in the continued destruction of the surrounding soft and hard tissues. During fixed orthodontic therapy, arch-wires, brackets, and elastic modules have been shown to be sites of significant plaque accumulation, making it difficult for a patient to maintain proper oral hygiene. The problem most dentists face is that they cannot visualize this biofilm completely to be able to carry out efficient plaque removal. Visual assessment is, to date, the most common method for plaque visualization, and various indexes have been demonstrated to be sufficient for quantification of the amount of plaque present. However, the problem is that visual assessments are inconsistent, operator dependent and often subjective, which can lead to inconsistency in results. Fluorescence is one such method that can be explored for its use in effective plaque identification and removal. Literature has it that dentists and patients find it particularly useful for monitoring oral hygiene status during treatment. Fluorescence has the capability of offering clinical orthodontists and researchers a new method of detection of demineralization during orthodontic treatment, furthermore, for efficient removal of orthodontic adhesive cements, fluorescent light may be used in conjunction with high-speed burs to deliver fast, less time consuming, and safer results. The benefit of direct visual treatment using fluorescence enhanced theragnosis is that the patient receives controlled and guided therapy. It has multiple benefits, such as early diagnosis of caries, biofilm identification, and even helps to achieve improved treatment outcomes by better resin selection for esthetic procedures.
Keywords: biofilm, fluorescence, orthodontics, theragnosis
1. Introduction
Dental plaque is formed by a variety of bacteria that form an adhesive layer on the tooth surface. These bacteria can accumulate rapidly and form colonies that lead to the development of a biofilm that collects in the interdental spaces and gingival margins [1,2]. Once the biofilm is formed, there is a release of toxins, peptides, lipo-polysaccharides, and organic acids. The accumulation of these products leads to gingival inflammation and tooth caries over time [3,4]. If this dental biofilm is removed in time, gingival health can be restored without any soft or hard tissue damage [5]. However, if the biofilm is allowed to persist and proliferate, it can damage the periodontal tissues and cause enamel caries [6,7]. With time, biofilm can even lead to the formation of periodontal pockets and move in a more sub-gingival direction because of the gradual development of a more complex non-aerobic local environment [8]. As long as the biofilm is present, there will be continued destruction of the surrounding soft and hard tissues. The problem most dentists face is that they cannot visualize this biofilm completely to be able to carry out efficient plaque removal. Orthodontists face an even more difficult problem as the presence of fixed attachments on teeth in brackets and wires makes it very complicated to estimate the plaque progression. They rely on the patients to maintain good oral hygiene during the treatment duration and can only carry out prophylaxis using disclosing solutions when they visit for a follow-up appointment [9].
During fixed orthodontic therapy, arch-wires, brackets, and elastic modules have been shown to be sites of significant plaque accumulation, making it difficult for a patient to maintain proper oral hygiene [10]. The prolonged presence of plaque can lead to demineralization in the 4-week interval between appointments [10]. At every follow-up appointment, a patient undergoing fixed orthodontic therapy must be clinically assessed for plaque accumulation, and the importance of good oral hygiene must be reinforced. Visual assessment is the most common method for plaque visualization, and various indexes have been demonstrated to be sufficient for quantification of the amount of plaque present [11]. While visual assessment is effective for plaque identification, it is not enough to visualize demineralization as considerable changes may occur below the surface before a white spot is visible [12]. Various studies conducted on oral hygiene reinforcement during orthodontic treatment have focused chiefly on analyzing periodontal health, techniques, and the quantification of plaque formation [13]. Research has also been conducted on improving oral hygiene in patients that have been positively reinforced with or without repeated oral hygiene instructions [14]. To motivate the patients, the first step has to be the visualization and assessment of the patient’s oral hygiene status. Various methods and interventions have been used to disclose agents, reward systems, report cards, and virtual reminders [15,16,17,18]. However, the problem is that visual assessments are inconsistent, operator dependent, and often subjective, which can lead to inconsistency in results. Methods such as disclosing solutions can lead to tissue staining and subsequent esthetic concerns, while the patients can always ignore reports and reminders.
A non-invasive and objective technique to detect and assess plaque clearly would be of great value in orthodontic patients [19]. Fluorescence is one such method that can be explored for its use in effective plaque identification and removal (Figure 1). Fluorescence has been explained as a process where substances absorb a shorter wavelength of light and emit longer wavelengths. These substances contain molecules called fluorophores that undergo de-excitement from a higher to a lower energy state on light absorption [20,21]. Previously published literature has shown that dental plaque fluoresces when exposed to 405 nm light even without using a disclosing agent [22]. On further research, it was also seen that old and cariogenic plaque is more susceptible to fluorescence than plaque recently formed [23]. Once the plaque emits fluorescent light, it can be easily detected using a dedicated camera that allows easy visualization and effective removal. Fluorescence has been found to be very effective in detecting oral mucosal alterations and early prediction of oral cancers [24]. It has also been shown to be effective in defining bone-resection margins in surgically treated cases of osteonecrosis [25].
Figure 1.
Graphical representation of how fluorescent light aids in visualization of deposits and demineralized areas. Different pathogenic bacteria within a biofilm produce porphyrins. Once excited with certain wavelengths these emit light in certain wavelengths. Special filters are needed by the viewer to correctly visualize the emitted light and diagnose bacterial presence. The wavelength of the exciting light has to fit into the spectrum of the targeted visualisation goal.
To understand the various benefits fluorescence can provide during fixed orthodontic therapy, various scenarios can be considered. This paper aimed to review existing literature related to fluorescence enhanced theragnosis and provide future uses and benefits of using this modality across various areas of orthodontic treatment.
2. Hygiene Motivation and Monitoring during Treatment
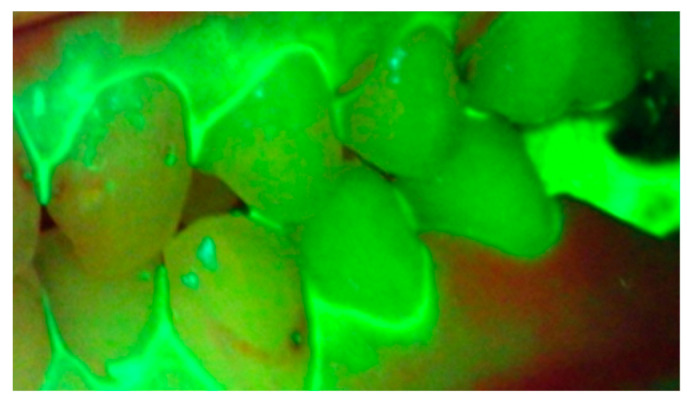
It has been seen that the leading cause of periodontal problems and dental caries during fixed orthodontic therapy is the failure to remove plaque efficiently, effectively, and promptly. Any additional costs can be avoided during orthodontic therapy by providing an effective preventive solution to identify and remove plaque [26,27]. During the active stages of treatment, it has been seen that there is increased plaque accumulation because of the role of brackets and wires in protecting plaque from saliva, mastication, and brushing [28,29,30,31]. Since plaque in orthodontic patients cannot be highlighted easily, it becomes difficult to assess, educate, and motivate patients to improve their oral hygiene status. Studies conducted using fluorescence have shown that dentists and patients find it particularly useful for monitoring oral hygiene status during treatment [32]. It was seen in such studies that there was a reduction in plaque coverage on the brackets, highlighting the importance of regular oral hygiene reinforcement during fixed orthodontic treatment (Figure 2). Furthermore, images recorded with fluorescent light may prove beneficial for diagnosis and be a valuable addition to the patient records for progress, medico-legal purposes, and research.
Figure 2.
Oral hygiene and plaque accumulation status highlighted using fluorescent light.
3. Early Demineralization Detection
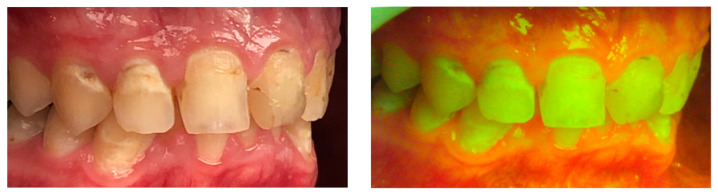
Demineralization is one of the most commonly occurring white spot lesions during orthodontic treatment [33,34]. Not only do these cause esthetic concerns but also predispose the affected teeth to caries. Previous research has shown that the incidence of white spot lesions is two times higher in patients undergoing fixed orthodontic therapy [35]. The incidence increases further with the consumption of dietary items containing sugar [35]. An aim of early demineralization detection is that remineralization can be carried out to avoid any aesthetic damage or the need for restorations. The use of fluorescent light is an indirect method of estimating the demineralization process, which utilizes the relation between the fluorescence intensity of the enamel and the mineralization status [36] (Figure 3). Fluorescence has the capability of offering clinical orthodontists and researchers a new method of detection of demineralization during orthodontic treatment.
Figure 3.
Comparison of intra-oral pictures depicting white spot lesions with and without fluorescent light.
4. Resin Cement Assessment and White Spot Lesions after Debonding
Previous research has confirmed the ability of fluorescence to measure white spot lesions and the presence of excess resin cement after debonding orthodontic brackets [37]. Teeth bonded with orthodontic brackets usually accumulate plaque and demonstrate white spot lesions of varying degrees when the treatment is completed, and the brackets removed [38]. Once the brackets are removed and the affected surface is exposed to saliva and brushing, these lesions are arrested, and remineralization can be carried out using fluoride-based agents [39]. Fluorescent light has been shown to be very effective in demonstrating white spot lesions as dark areas on images [40].
Even though bonding of orthodontic brackets is an established process, there are many challenges when it comes to removing the adhesive composite remnants [41]. Common problems encountered in removing the resin cement during debonding are varying degrees of accessibility, primarily in the molar regions, visualization, and the conditioning area required for different teeth [42]. For efficient removal of orthodontic adhesive cements, fluorescent light may be used in conjunction with high-speed burs to deliver fast, less time-consuming, and safer results.
5. Comparison of Various Orthodontic Materials in Terms of Plaque Accumulation
If we can positively utilize digital technology to deliver better care to our patients, it is our responsibility to do so. This requires constant research and innovation, and the data collected for such studies must be reliable [41]. Conventional plaque estimation methods include dyes followed by a visual assessment which is error-prone, may demonstrate bias, and is both time and cost-consuming [43]. The use of light-induced fluorescence-based devices can reduce the errors associated with many of the conventional data collection methods. The ability to measure even subtle changes in the minerals contained in the tooth structure makes this a convenient tool for research purposes [43].
6. Fluorescence Enhanced Theragnosis—The Next Stage of a Targeted Diagnostic Approach?
Daylight and magnification have both been long established as two pillars supporting oral diagnosis and treatment planning. Using a definite light spectrum, photoluminescence can be created, which can be visualized using specific filters. This is possible due to the inherent fluorescent properties of the tooth and porphyrins generated by caries causing bacteria. The benefit of direct visual treatment enhancement using theragnosis is that the patient receives controlled and guided therapy. Fluorescence enhanced theragnosis has multiple benefits, such as early diagnosis of caries, biofilm identification, and even helps achieve improved treatment outcomes by better resin selection for esthetic procedures (Figure 4). Fluorescence enhanced theragnosis for the diagnosis of demineralization is today more successful if accompanied by the use of external fluorophores with a direct focus on Ca ions. This does need more clinical trials to demonstrate its viability in clinical dentistry. Fluorescence enhanced theragnosis needs more attention and research to help incorporate this into a valuable diagnostic and treatment planning tool in orthodontics with such vast potential.
Figure 4.
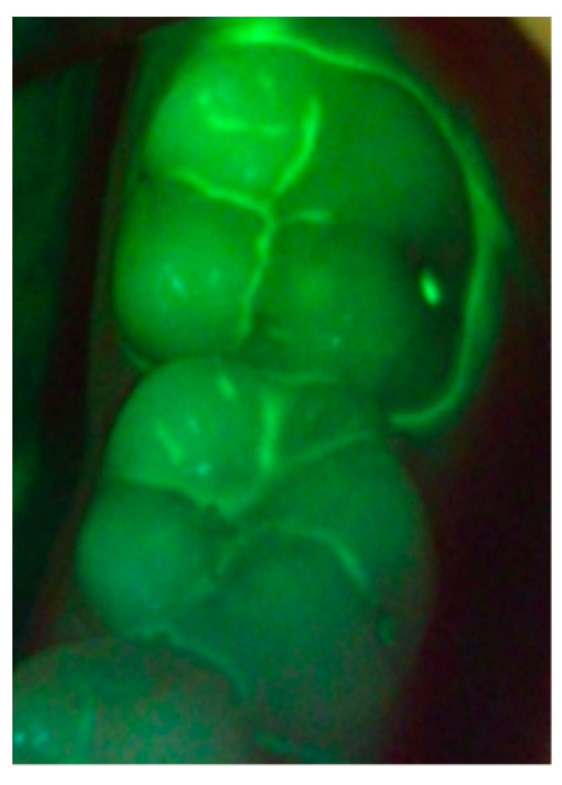
Definite and clear visualization of demineralized areas, caries, and plaque accumulation around the teeth using fluorescent light.
7. Areas of Improvement
Fluorescence enhanced theragnosis can be carried out using a wearable device called Reveal (Designs for Vision, Inc., Bohemia, NY, USA) [44]. This device consists of glasses with magnifying loupes, both coated with multiple protective layers to prevent any eye damage from the emitted light. With further use and mass production, the cost of these devices can be brought down to ensure wider use across the orthodontic community.
8. Conclusions
Since the advent of the digital era, orthodontists have been at the forefront of adopting various technological methods and techniques to help provide better treatment options to their patients. Aristotle said, “Well begun is half done,” and if we can ensure constant monitoring of treatment progress for a better outcome, we must take that responsibility.
Author Contributions
Conceptualization, A.M. and L.S.; methodology, M.I.K.; writing—original draft preparation, A.M.; writing—review and editing, L.S., A.V., and M.I.K. Authorship is limited to those who have contributed substantially to the work reported. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
Liviu Steier holds IP rights and touches royalties from Designs for Vision, the manufacturer of Reveal and Reveal FGS.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Paster B.J., Boches S.K., Galvin J.L., Ericson R.E., Lau C.N., Levanos V.A., Sahasrabudhe A., Dewhirst F.E. Bacterial Diversity in Human Subgingival Plaque. J. Bacteriol. 2001;183:3770–3783. doi: 10.1128/JB.183.12.3770-3783.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kolenbrander P.E. Oral Microbial Communities: Biofilms, Interactions, and Genetic Systems. Annu. Rev. Microbiol. 2000;54:413–437. doi: 10.1146/annurev.micro.54.1.413. [DOI] [PubMed] [Google Scholar]
- 3.Kornman K.S., Page R.C., Tonetti M.S. The host response to the microbial challenge in periodontitis: Assembling the players. Periodontology 2000. 1997;14:33–53. doi: 10.1111/j.1600-0757.1997.tb00191.x. [DOI] [PubMed] [Google Scholar]
- 4.Haffajee A.D., Socransky S.S. Microbial etiological agents of destructive periodontal diseases. Periodontology 2000. 1994;5:78–111. doi: 10.1111/j.1600-0757.1994.tb00020.x. [DOI] [PubMed] [Google Scholar]
- 5.Armitage G.C., Robertson P.B. The Biology, Prevention, Diagnosis and Treatment of Periodontal Diseases: Scientific Advances in the United States. J. Am. Dent. Assoc. 2009;140:36–43. doi: 10.14219/jada.archive.2009.0356. [DOI] [PubMed] [Google Scholar]
- 6.Offenbacher S. Periodontal Diseases: Pathogenesis. Ann. Periodontol. 1996;1:821–878. doi: 10.1902/annals.1996.1.1.821. [DOI] [PubMed] [Google Scholar]
- 7.Sharma N.C., Qaqish J., Klukowska M., Grender J., Rooney J. The plaque removal efficacy of a novel power brush head. J. Clin. Dent. 2011;22:19–22. [PubMed] [Google Scholar]
- 8.Raggio D.P., Braga M.M., Rodrigues J.A., Freitas P.M., Imparato J.C.P., Mendes F. Reliability and discriminatory power of methods for dental plaque quantification. J. Appl. Oral Sci. 2010;18:186–193. doi: 10.1590/S1678-77572010000200014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yavan M.A., Kocahan S., Ozdemir S., Sokucu O., Orthodontist G.P. The Effects of Using Plaque-Disclosing Tablets on the Removal of Plaque and Gingival Status of Orthodontic Patients. Turk. J. Orthod. 2019;32:207–214. doi: 10.5152/TurkJOrthod.2019.18084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Øgaard B., Ten Bosch J.J. Regression of white spot enamel lesions. A new optical method for quantitative longitudinal evaluation in vivo. Am. J. Orthod. Dentofac. Orthop. 1994;106:238–242. doi: 10.1016/S0889-5406(94)70042-7. [DOI] [PubMed] [Google Scholar]
- 11.Silness J., Löe H. Periodontal Disease in Pregnancy II. Correlation Between Oral Hygiene and Periodontal Condition. Acta Odontol. Scand. 1964;22:121–135. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 12.Pretty I.A., Pender N., Edgar W.M., Higham S.M. The in vitro detection of early enamel de-and remineralization adjacent to bonded orthodontic cleats using quantitative light-induced Fluorescence. Eur. J. Orthod. 2003;25:217–223. doi: 10.1093/ejo/25.3.217. [DOI] [PubMed] [Google Scholar]
- 13.Gray D., McIntyre G. Does oral health promotion influence the oral hygiene and gingival health of patients undergoing fixed appliance orthodontic treatment? A systematic literature review. J. Orthod. 2008;35:262–269. doi: 10.1179/14653120722770. [DOI] [PubMed] [Google Scholar]
- 14.Marini I., Bortolotti F., Parenti S.I., Gatto M.R., Bonetti G.A. Combined effects of repeated oral hygiene motivation and type of toothbrush on orthodontic patients: A blind randomized clinical trial. Angle Orthod. 2014;84:896–901. doi: 10.2319/112113-856.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boyd R.L. Longitudinal evaluation of a system for self-monitoring plaque control effectiveness in orthodontic patients. J. Clin. Periodontol. 1983;10:380–388. doi: 10.1111/j.1600-051X.1983.tb01287.x. [DOI] [PubMed] [Google Scholar]
- 16.Richter D.D., Nanda R.S., Sinha P.K., Smith D.W., Currier G.F. Effect of behavior modification on patient compliance in orthodontics. Angle Orthod. 1998;68 doi: 10.1043/0003-3219(1998)0682.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Lalic M., Aleksic E., Gajic M., Milic J., Malesevic D. Does oral health counseling effectively improve oral hygiene of orthodontic patients? Eur. J. Paediatr. Dent. 2012;13:181–186. [PubMed] [Google Scholar]
- 18.Eppright M., Shroff B., Best A., Barcoma E., Lindauer S.J. Influence of active reminders on oral hygiene compliance in orthodontic patients. Angle Orthod. 2013;84:208–213. doi: 10.2319/062813-481.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marsh P.D. Dental plaque as a biofilm and a microbial community—Implications for health and disease. BMC Oral Health. 2006;6:S14. doi: 10.1186/1472-6831-6-S1-S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anil K., Anand A. Fundamentals and Applications of Biophotonics in Dentistry. Volume 105–107. London Imperial College Press; London, UK: 2007. pp. 16–17. [Google Scholar]
- 21.Walsh L.J., Shakibaie F. Ultraviolet-Induced Fluorescence: Shedding New Light on Dental Biofilms and Dental Caries. Australas. Dent. Pract. 2007;18:1–7. [Google Scholar]
- 22.Heinrich-Weltzien R., Kühnisch J., Van Der Veen M., Jong E.D.J.D., Stösser L. Quantitative light-induced fluorescence (QLF)—A potential method for the dental practitioner. Quintessence Int. 2003;34:181–188. [PubMed] [Google Scholar]
- 23.Volgenant C.M., Hoogenkamp M.A., Buijs M.J., Zaura E., ten Cate J.B.M., van der Veen M.H. Red fluorescent biofilm: The thick, the old, and the cariogenic. J. Oral Microbiol. 2016;8:30346. doi: 10.3402/jom.v8.30346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Biamonte F., Buffone C., Santamaria G., Battaglia A.M., Mignogna C., Fortunato L., Costanzo F.S., Giudice A. Gene expression analysis of autofluorescence margins in leukoplakia and oral carcinoma: A pilot study. Oral Dis. 2020;27:193–203. doi: 10.1111/odi.13525. [DOI] [PubMed] [Google Scholar]
- 25.Giudice A., Bennardo F., Barone S., Antonelli A., Figliuzzi M., Fortunato L. Can Autofluorescence Guide Surgeons in the Treatment of Medication-Related Osteonecrosis of the Jaw? A Prospective Feasibility Study. J. Oral Maxillofac. Surg. 2018;76:982–995. doi: 10.1016/j.joms.2017.10.024. [DOI] [PubMed] [Google Scholar]
- 26.Karkhanechi M., Chow D., Sipkin J., Sherman D., Boylan R.J., Norman R.G., Craig R.G., Cisneros G.J. Periodontal status of adult patients treated with fixed buccal appliances and removable aligners over one year of active orthodontic therapy. Angle Orthod. 2012;83:146–151. doi: 10.2319/031212-217.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alexander S.A. Effects of orthodontic attachments on the gingival health of permanent second molars. Am. J. Orthod. Dentofac. Orthop. 1991;100:337–340. doi: 10.1016/0889-5406(91)70071-4. [DOI] [PubMed] [Google Scholar]
- 28.Ristic M., Svabic M.V., Sasic M., Zelic O. Clinical and microbiological effects of fixed orthodontic appliances on periodontal tissues in adolescents. Orthod. Craniofacial Res. 2007;10:187–195. doi: 10.1111/j.1601-6343.2007.00396.x. [DOI] [PubMed] [Google Scholar]
- 29.Butera A., Gallo S., Maiorani C., Molino D., Chiesa A., Preda C., Esposito F., Scribante A. Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters. Microorganisms. 2020;9:69. doi: 10.3390/microorganisms9010069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Preda C., Butera A., Pelle S., Pautasso E., Chiesa A., Esposito F., Oldoini G., Scribante A., Genovesi A., Cosola S. The Efficacy of Powered Oscillating Heads vs. Powered Sonic Action Heads Toothbrushes to Maintain Periodontal and Peri-Implant Health: A Narrative Review. Int. J. Environ. Res. Public Health. 2021;18:1468. doi: 10.3390/ijerph18041468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bollen A.M., Cunha-Cruz J., Bakko D.W., Huang G.J., Hujoel P.P. The effects of orthodontic therapy on periodontal health: A systematic review of controlled evidence. J. Am. Dent. Assoc. 2008;139:413–422. doi: 10.14219/jada.archive.2008.0184. [DOI] [PubMed] [Google Scholar]
- 32.Miller C.C., Burnside G., Higham S.M., Flannigan N.L. Quantitative Light-induced Fluorescence-Digital as an oral hygiene evaluation tool to assess plaque accumulation and enamel demineralization in orthodontics. Angle Orthod. 2016;86:991–997. doi: 10.2319/092415-648.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Şen S., Erber R., Deurer N., Orhan G., Lux C.J., Zingler S. Demineralization detection in orthodontics using an ophthalmic optical coherence tomography device equipped with a multicolor fluorescence module. Clin. Oral Investig. 2019;24:2579–2590. doi: 10.1007/s00784-019-03116-3. [DOI] [PubMed] [Google Scholar]
- 34.Scribante A., Farahani M.R.D., Marino G., Matera C., Baena R.R.Y., Lanteri V., Butera A. Biomimetic Effect of Nano-Hydroxyapatite in Demineralized Enamel before Orthodontic Bonding of Brackets and Attachments: Visual, Adhesion Strength, and Hardness in In Vitro Tests. BioMed Res. Int. 2020;2020 doi: 10.1155/2020/6747498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Reilly M.M., Featherstone J.D. Demineralization, and remineralization around orthodontic appliances: An in vivo study. Am. J. Orthod. Dentofac. Orthop. 1987;92:33–40. doi: 10.1016/0889-5406(87)90293-9. [DOI] [PubMed] [Google Scholar]
- 36.van der Veen M.H., de Josselin de Jong E. Application of quantitative light-induced Fluorescence for assessing early caries lesions. Monogr. Oral Sci. 2000;17:144–162. doi: 10.1159/000061639. [DOI] [PubMed] [Google Scholar]
- 37.Al-Khateeb S., Forsberg C.M., de Josselin de Jong E., AngmarMansson B. A longitudinal laser fluorescence study of white spot lesions in orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 1998;113:595–602. doi: 10.1016/S0889-5406(98)70218-5. [DOI] [PubMed] [Google Scholar]
- 38.Ren Y., Jongsma M.A., Mei L., Van Der Mei H.C., Busscher H.J. Orthodontic treatment with fixed appliances and biofilm formation—A potential public health threat? Clin. Oral Investig. 2014;18:1711–1718. doi: 10.1007/s00784-014-1240-3. [DOI] [PubMed] [Google Scholar]
- 39.Fontana M., Young D.A., Wolff M.S. Evidence-based caries, risk assessment, and treatment. Dent. Clin. N. Am. 2009;53:149–161. doi: 10.1016/j.cden.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 40.Lussi A., Hibst R., Paulus R. DIAGNOdent: An Optical Method for Caries Detection. J. Dent. Res. 2004;83:80–83. doi: 10.1177/154405910408301s16. [DOI] [PubMed] [Google Scholar]
- 41.Pignatta L.M.B., Júnior S.D., Santos E.C.A. Evaluation of enamel surface after bracket debonding and polishing. Dent. Press J. Orthod. 2012;17:77–84. doi: 10.1590/S2176-94512012000400017. [DOI] [Google Scholar]
- 42.Murray P.G., Millett D.T., Cronin M. Bonded molar tubes: A survey of their use by specialist orthodontists. J. Orthod. 2012;39:129–135. doi: 10.1179/1465312512Z.00000000016. [DOI] [PubMed] [Google Scholar]
- 43.Kim H.-E. Quantitative light-induced Fluorescence: A potential tool for dental hygiene process. J. Dent. Hyg. Sci. 2013;13:115–124. doi: 10.1016/j.jds.2012.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Steier L. Reveal: Fluorescence Enhanced Theragnosis by Designs for Vision. Eur. J. Dent. 2020;14:186–188. doi: 10.1055/s-0040-1705076. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.