Abstract
Wuhan, China was the first city to discover COVID-19. With the government's macro-control and the active cooperation of the public, the spread of COVID-19 has been effectively controlled. In order to understand the additional impact of these measures on the prevalence of common influenza, we have collected flu test data from the Pediatric Clinic of Zhongnan Hospital of Wuhan University from September to December 2020, and compared them with the same period in 2018 and 2019. It is found that compared with the same period in 2018 and 2019, the rate of children's influenza activity in 2020 has significantly decreased, which indicates that the protective measures against COVID-19 have effectively reduced the level of influenza activity.
Keywords: Severe acute respiratory syndrome coronavirus 2, Respiratory infections, SARS-CoV-2, COVID-19, Influenza, Infection control measures
Wuhan, China, is the first city to have Coronavirus disease 2019 (COVID-19) pandemic. In the early stage of the epidemic, under the strong control of the government, the city was closed and traffic restricted, which effectively restricted the further spread of the virus. Finally, with the joint efforts of the people across the country, the epidemic has been fully controlled, and the people have gradually returned to normal production and life. However, the Chinese government and people remain highly vigilant against COVID-19 and have adopted various protective measures to prevent the epidemic from spreading again on a large scale. For example, avoid gatherings, maintain social distancing (one meter apart), wash hands frequently, wear masks when going out, monitor body temperature daily, record travel trajectory in real time, and national nucleic acid testing, etc. [1]. Measures such as wearing masks when going out have also become the daily habits of citizens. These measures not only successfully limited the spread of COVID-19, but also significantly reduced the incidence of influenza according to the testing data of the Chinese National Influenza Center (http://www.chinaivdc.cn/cnic/). At the same time, it is reported that influenza activity in Taiwan, Singapore, and the United States has also decreased [[2], [3], [4]].
But at present, as the first outbreak site of COVID-19, there is no report showing that the prevalence of influenza in Wuhan has changed. In order to understand whether relevant measures to prevent COVID-19 really brought additional benefits to the prevalence of influenza in Wuhan, we conducted this retrospective analysis. After the epidemic, the country will gradually resume normal production and life in July 2020. As we all know, children are susceptible to influenza, and from September to December every year, affected by the beginning of school and the change of seasons, it has always been a period of high incidence of influenza [5]. We collected patient data (Supplementary data) who attended the Pediatric Clinic of Zhongnan Hospital of Wuhan University and were tested for influenza between September and December 2018, 2019, and 2020. Since this analysis is a retrospective analysis, some data such as the number of daily visits in the pediatric clinic are no longer available. However, considering that blood routine is the most common examination, the number of examinations may potentially reflect the number of outpatients, and this analysis only compares the relative level of influenza prevalence, not as an absolute influenza prevalence value. Therefore, the error caused by estimating the total number of pediatric clinics based on the number of blood routine in pediatric clinics can be ignored.
We counted the number of pediatric outpatients, the number of influenza tests, and the number of positive influenza tests during the period from September to December 2018−2020. Influenza type A and B nucleoprotein antigens extracted from the nasal swab specimen were detected by One Step Influenza A&B Test (Wondfo) [6]. And calculated the flu test rate (number of people tested for flu/number of outpatients) and flu positive rate (number of people tested positive for flu/number of people tested for flu). Table 1 is the detailed comparative data for the period from September to December 2018−2020. It can be found that due to the impact of epidemic prevention and control measures, the number of pediatric outpatient clinics will be significantly reduced in 2020, but the flu detection rate is relatively stable, with an average of 28.7%. The flu detection rate in 2018 and 2019 fluctuated greatly. The flu detection rate in September–October was low, while the flu detection rate in November–December rose sharply, which is closely related to temperature changes. The flu detection rate in November-December rose sharply, which is closely related to temperature changes. However, the detection rate in 2020 has not been affected, and it has been preliminarily shown that COVID-19 has had an impact on influenza activities. Although the influenza positive rate in 2018 and 2019 fluctuated greatly, they were significantly higher than in 2020. The average influenza positive rate in 2018 was 14%, in 2019 it was 28.7%, while the positive rate of influenza in 2020 has been at a low level, with an average of 4.3%. This further confirms that the COVID-19 outbreak and related protective measures have significantly reduced the incidence of influenza.
Table 1.
Influenza statistics table of pediatric outpatient department of Zhongnan Hospital of Wuhan University.
| Time | Outpatient number |
Influenza detection number |
Influenza positive number |
Influenza detection rate |
Influenza positive rate |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2018 | 2019 | 2020 | 2018 | 2019 | 2020 | 2018 | 2019 | 2020 | 2018 | 2019 | 2020 | 2018 | 2019 | 2020 | |
| Early Sep | 1485 | 1702 | 1143 | 53 | 344 | 388 | 6 | 33 | 10 | 0.036 | 0.202 | 0.339 | 0.113 | 0.096 | 0.026 |
| Late Sep | 1883 | 2285 | 878 | 47 | 456 | 233 | 2 | 50 | 11 | 0.025 | 0.200 | 0.265 | 0.043 | 0.110 | 0.047 |
| Early Oct | 2176 | 1946 | 802 | 61 | 308 | 198 | 6 | 27 | 9 | 0.028 | 0.158 | 0.247 | 0.098 | 0.088 | 0.045 |
| Late Oct | 2481 | 2224 | 1386 | 98 | 286 | 426 | 12 | 26 | 16 | 0.040 | 0.129 | 0.307 | 0.122 | 0.091 | 0.038 |
| Early Nov | 2112 | 2254 | 1361 | 211 | 385 | 405 | 24 | 48 | 28 | 0.100 | 0.171 | 0.298 | 0.114 | 0.125 | 0.069 |
| Late Nov | 2110 | 2168 | 1021 | 315 | 635 | 292 | 39 | 105 | 8 | 0.149 | 0.293 | 0.286 | 0.124 | 0.165 | 0.027 |
| Early Dec | 2249 | 3617 | 972 | 375 | 2178 | 269 | 33 | 735 | 11 | 0.167 | 0.602 | 0.277 | 0.088 | 0.337 | 0.041 |
| Late Dec | 2809 | 4765 | 1203 | 854 | 4316 | 309 | 160 | 1533 | 15 | 0.304 | 0.906 | 0.257 | 0.187 | 0.355 | 0.049 |
| Summary | 17,305 | 20,961 | 8766 | 2014 | 8908 | 2520 | 282 | 2557 | 108 | 0.116 | 0.425 | 0.287 | 0.140 | 0.287 | 0.043 |
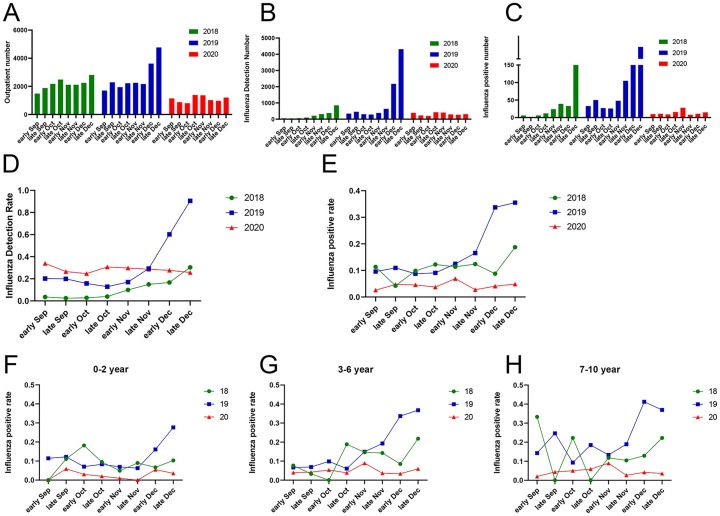
Fig. 1 depicts the comparison results of influenza activities from September to December 2018−2020. Fig. 1A–C shows that compared with the same period in 2018 and 2019, the number of influenza tests in pediatric outpatient clinics in 2020 has decreased significantly. Subsequently, we used GraphPad Prism8 to perform a paired t-test to compare the influenza activity in the pediatric outpatient clinic of Zhongnan Hospital of Wuhan University from September to December 2020 with the activity levels in the same period in 2018 and 2019. The results showed that compared with the same period in 2018, the pediatric outpatient influenza detection rate in 2020 increased by 17.84% (p = 0.0027), but the influenza positive rate decreased by 6.838% (p = 0.0027). Compared with 2019, the pediatric outpatient influenza detection rate did not differ (p = 0.6526), but the influenza positive rate was reduced by 12.81% (p = 0.0136) (Fig. 1D–E). We also compared the positive rates of influenza testing in different age groups (infancy: 0−2 year, Preschool education period: 3−6 year, school-age: 7−10 year). Fig. 1F–H shows that in different age groups, the flu-positive rate in 2020 has been at a low level. The flu infection rate in 2018 and 2019 fluctuates greatly, and December is the peak period of flu infection in all age groups. Among them, the influenza infection rate of 0−2 years old is lower than that of 3−6 years old and 7−10 years old. Taking into account that there is no ability to take care of themselves at the age of 0−2 years, most of the time they stay at home, have less contact with the external environment, and the chance of exposure to infection is greatly reduced. And in 2020, affected by the epidemic, the whole people will reduce unnecessary travel and gathering, so the chance of exposure to infection will also be reduced. In addition, daily habits such as wearing masks when going out also limit the spread of influenza virus among people. This shows that protective measures such as home isolation and wearing masks when going out have effectively reduced the spread of the virus and are of great significance to the prevention and treatment of COVID-19 and influenza.
Fig. 1.
From September to December 2020, comparison of influenza activities in the Pediatric Clinic of Zhongnan Hospital of Wuhan University with the same period in 2018 and 2019. (A) Total number of pediatric clinics. (B) The number of pediatric influenza tested. (C) The number of positive pediatric influenza tests. (D) Pediatric influenza detection rate (the number of pediatric influenza tested/total number of pediatric clinics). (E) Pediatric influenza test positive rate (the number of positive pediatric influenza tests/the number of pediatric influenza tested). (F) The positive rate of influenza test in children aged 0–2 years. (G) The positive rate of influenza test in children aged 3–6 years. (H) The positive rate of influenza in children aged 7–10 years.
Our data analysis found that after the epidemic, from September to December 2020, the positive rate of influenza testing in the Pediatric Clinic of Wuhan University Zhongnan Hospital was significantly lower than that in 2018 and the same period in 2019. This is compared with home isolation, reducing unnecessary outings, and going out. Wearing masks and other protective measures to prevent the spread of COVID-19 are closely related. Both COVID-19 and common flu are respiratory-transmitted viruses, and their spread in the population is the same, so the measures to prevent and treat COVID-19 are also effective for common flu. However, our research has limitations. Firstly, only the pediatric outpatient influenza test data was included in the research subjects, and the analysis of the broad population was lacking. Secondly, in terms of research scope, only one hospital in Wuhan was analyzed for influenza data, lacking more data support. However, our research shows that compared with the same period in 2019 and 2018, influenza activity in 2020 is indeed significantly reduced, which is closely related to the protective measures for COVID-19. In short, we believe that the protective measures against COVID-19 have effectively reduced the level of influenza activity.
Competing interests
None declared.
Ethical approval
Not required.
Acknowledgements
This work was supported by grant from National Natural Science Foundation of China (81272372) and by Zhongnan Hospital of Wuhan University Science, Technology and Innovation Seed Fund (znpy2016033).
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.jiph.2021.08.027.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Agalar C., Ozturk Engin D. Protective measures for COVID-19 for healthcare providers and laboratory personnel. Turk J Med Sci. 2020;50(SI–1):578–584. doi: 10.3906/sag-2004-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuo S.C., Shih S.M., Chien L.H., Hsiung C.A. Collateral benefit of COVID-19 control measures on influenza activity, Taiwan. Emerging Infect Dis. 2020;26(8):1928–1930. doi: 10.3201/eid2608.201192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olsen S.J., Azziz-Baumgartner E., Budd A.P., Brammer L., Sullivan S., Pineda R.F., et al. Decreased influenza activity during the COVID-19 pandemic-United States, Australia, Chile, and South Africa, 2020. Am J Transplant. 2020;20(12):3681–3685. doi: 10.1111/ajt.16381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soo R.J.J., Chiew C.J., Ma S., Pung R., Lee V. Decreased Influenza Incidence under COVID-19 Control Measures, Singapore. Emerging Infect Dis. 2020;26(8):1933–1935. doi: 10.3201/eid2608.201229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feng L., Feng S., Chen T., Yang J., Lau Y.C., Peng Z., et al. Burden of influenza-associated outpatient influenza-like illness consultations in China, 2006–2015: a population-based study. Influenza Other Respir Viruses. 2020;14(2):162–172. doi: 10.1111/irv.12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peng Y., Wu J., Liu X., Wang J., W Li. Evaluation of Wondfo influenza A&B fast test based on immunochromatography assay for rapid diagnosis of influenza A H1N1. Braz J Infect Dis. 2013;17(2):247–250. doi: 10.1016/j.bjid.2012.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.