Abstract
Objective
To understand how surrogates of critically ill patients adjusted to challenges that resulted from the COVID-19 pandemic.
Methods
Participants (N = 62) were surrogates of critically ill adults with COVID-19 in the ICU at an urban, academic medical center from March to June 2020. Participants were recruited using convenience sampling and took part in one-time qualitative individual interviews via telephone. Qualitative data were analyzed using thematic content analysis.
Results
Qualitative analyses yielded four types of challenges: Communication with the medical team, communication among family members, understanding and tracking medical information, and distress related to visitor restrictions. To adjust to challenges related to communication, participants developed routines for receiving updates from the medical team and providing updates to other family members. To adjust to the challenge related to comprehension, participants sought information from external sources such as family members in healthcare fields. To adjust to the challenge related to visitation, participants found some comfort in video calls with the patient.
Conclusions
Surrogates of critically ill patients with COVID-19 faced multiple types of challenges yet adjusted to those challenges.
Practical Implications
Future research should focus on ways to support the wellbeing of surrogates during times of restricted hospital visitation.
Clinical trial registered at ClinicalTrials.gov (NCT03969810).
Keywords: Family engagement, COVID-19, Shared decision making, Human centered design
1. Introduction
Family presence in the intensive care unit (ICU) is largely encouraged as it has been linked to positive patient outcomes, including a reduction in a patient’s risk for developing delirium and other distressing symptoms [1], [2], [3]. Furthermore, family members may have greater satisfaction with the ICU experience and may be less likely to develop emotional distress when they play an active role in a patient’s care [4], [5].
During the COVID-19 pandemic, many hospital systems restricted hospital visitation to limit the spread of the disease, which may have had a negative impact on the ICU experiences of both patients and their families [6], [7], [8]. In a previous study, surrogates of critically ill patients during the early phase of the COVID-19 pandemic were more likely to experience stress and depressive symptoms than those enrolled prior to the COVID-19 pandemic [9]. In another study, relatives of patients with COVID-19 had high levels of psychological distress three months after hospital discharge [10]. Possible explanations for these findings include the trauma of being separated from a critically ill loved one [11], an uncertain patient prognosis due to a novel disease, difficulty developing an emotional connection with the medical team, and challenges with bereavement during times of restrictive visitation [12].
The purpose of this study was to examine challenges experienced by surrogates of patients with COVID-19 at an urban, academic medical center from March to June 2020, the first wave of the pandemic. We also investigated how surrogates adjusted to participant-identified challenges. To assess challenges and related adjustments identified by surrogates, we employed a qualitative research design. More specifically, surrogates of critically ill patients with COVID-19 in the ICU took part in one-time, semi-structured individual interviews conducted via telephone. Qualitative research methodologies provide a detailed understanding of participant experiences when relatively little prior knowledge exists about a specific issue [13], [14]. Findings from this study may provide guidance for clinicians who aim to provide family-centered care during times where hospital visitation is restricted.
2. Methods
2.1. Participants
This study was conducted at Rush University Medical Center (RUMC), an academic, tertiary care medical center in Chicago, Illinois from March 20, 2020 to June 30, 2020, a period corresponding with a surge of COVID-19 positive patients. More than 1400 patients with COVID-19 were hospitalized at RUMC from March to June, 2020 [15]. For the current study, we conducted a preliminary analysis of an ongoing clinical trial dealing with the family experience because of the impact that COVID-19 has had on hospital policy and society in general (NCT03969810). Participants were randomly assigned to receive usual care without or usual care with written summaries of the patient’s care plan via email each day. The approach for creating daily written summaries was based on a pilot study of 30 patients without COVID-19 [16]. The clinical trial and the current study were both approved by an Institutional Review Board at RUMC (approval number 19042604-IRB01).
Participants were surrogates of adult patients in two “COVID-19 ICUs,” each consisting of 28 beds. We approached surrogates of non-decisional patients who required or were expected to require mechanical ventilation for at least three days but had not yet received mechanical ventilation for 14 days. To be eligible to participate, surrogates needed to be at least 18 years of age, be fluent in the English language, have a valid email address with access to their account, and self-identify as a decision maker for the patient. We did not approach surrogates of patients who were expected to die or transition to comfort care within the next 24 h or who were pregnant. Surrogates were emailed a copy of the consent form. They provided informed consent either by emailing/faxing a signed consent form or by providing consent via telephone, as approved by the RUMC IRB.
2.2. Hospital policies during the COVID-19 pandemic
From March 20, 2020 to June 30, 2020, RUMC restricted hospital visitation. Exceptions were made in cases where the medical team believed patient death was imminent or during planned withdrawal of life support. Families selected one primary contact person at the beginning of the patient’s hospitalization. Clinicians on the ICU team would typically provide an update to this family member once in the afternoon. The medical team would additionally contact the family if there was a change in the patient’s clinical status or consent was needed for a procedure. Families could call the ICU to speak directly to other members of the medical team such as the nurse or case manager. The ICU had the capability for video calls between patients and families; these calls were scheduled and coordinated by the patient’s nurse.
2.3. Measure: individual interview guide
Participants took part in one-time, semi-structured qualitative individual interviews regarding their ICU experience [17]. Prior to conducting these interviews with participants, we developed an interview guide (Supplemental Fig. 1). A guide is used to address specific content areas and representative questions related to an overall study purpose [18]. Content areas were based on previous literature, a pilot study pertaining to daily written summaries and family experiences, and ICU-based experiences of the authors. Content areas included: satisfaction with ICU care, communication with the ICU team, communication among family members, and understanding the patient’s condition.
2.4. Procedures
After participating in the study for at least five days, individuals were invited to take part in a one-time, semi-structured qualitative individual interview via telephone. Semi-structured interviews refer to the use of an individual interview guide with participants determining the flow of discussion. We recruited surrogates for the current study using a convenience sampling strategy. Participants were not interviewed if the patient was deceased. All interviews were conducted by the same study investigator (SB). Interviews typically occurred during the second week of the ICU stay; the timing was based on the patient’s clinical course and participant/interviewer availability. All interviews pertained to challenges faced by the surrogate during their loved one’s ICU stay and resultant adjustments. Prior to completing the individual interview, participants were also given the opportunity to discuss any topic they believed was relevant to their ICU experience. All interviews were conducted via telephone, were audio-recorded, and transcribed verbatim. Interviews lasted approximately 15 min.
2.5. Analysis
Individual interviews served as the unit of analysis with transcripts of the interviews representing primary data. We examined all data using thematic content analysis, an established qualitative approach to understanding personal or subjective perspectives [19]. Data analysis consisted of several steps. First, six members of the study team (JAG, SB, TQ, JB, NS, and SKO) independently coded transcripts from the initial 10 interviews. The study team then created a codebook comprising those codes. Two members of the study team (subset of the above investigators) coded each remaining transcript using the codebook. After the study team coded all transcripts, they categorized each code as either a challenge faced by a participant or as how a participant adjusted to a challenge. To ensure intercoder consistency, members of the study team discussed and reached consensus regarding each code and its assignment as a challenge or adjustment to a challenge [20]. Data analyses were conducted by hand, a traditional qualitative route.
3. Results
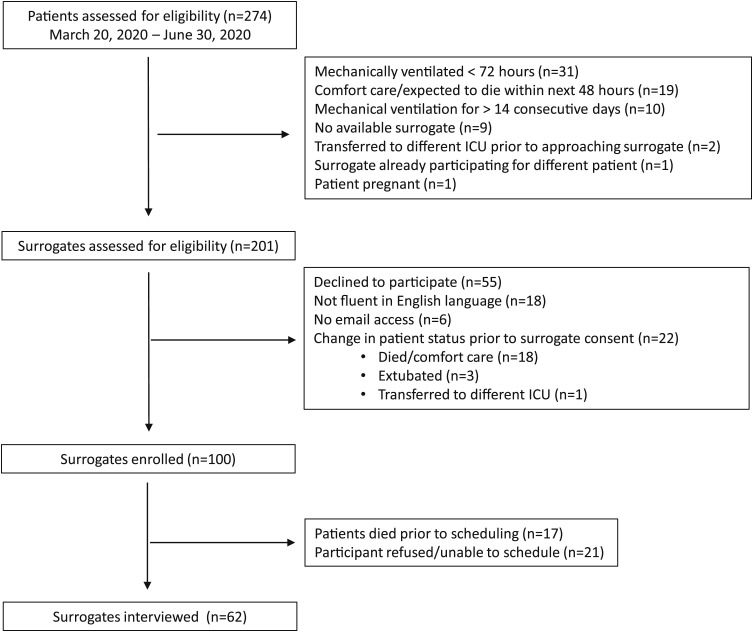
From March 20, 2020 and June 30, 2020, there were 201 surrogates who were assessed for eligibility to participate in an ongoing clinical trial of whom 100 were enrolled ( Fig. 1). Only 18 (9%) surrogates were excluded because they were not fluent in the English language and only 6 (3%) surrogates were excluded because they did not have access to email. Of the 100 participating surrogates, 62 participated in a telephone interview during the hospitalization. In 17 cases, the patient died prior to scheduling and in 21 cases, the interview was unable to be scheduled.
Fig. 1.
Enrollment.
The average age of participating surrogates was 42 years [SD = 13]. Participants were largely female (81%) and either children (46%) or spouses (29%) of ICU patients. The racial/ethnic breakdown of participants was Hispanic (47%), Black non-Hispanic (27%), White non-Hispanic (16%), and Other/Did not answer (10%). The average age of respective patients was 59 years [SD = 13]. Demographic characteristics of participating surrogates and respective patients are displayed in Table 1 .
Table 1.
Characteristics of participants (surrogates of critically ill patients) and respective patients.
| Surrogate participated in individual interview | |
|---|---|
| Surrogate (Subject) Characteristic | n = 62 |
| Relation to patient No (%) | |
| Spouse/partner | 18 (29) |
| Child | 28 (46) |
| Parent | 3 (5) |
| Sibling | 6 (10) |
| Other | 6 (10) |
| Years of Age, mean (SD) | 42 (13) |
| Gender No (%) | |
| Female | 50 (81) |
| Male | 12 (19) |
| Race/Ethnicity No (%) | |
| Hispanic | 29 (47) |
| Black, non-Hispanic | 17 (27) |
| White, non-Hispanic | 10 (16) |
| Other/Did not answer | 6 (10) |
| Religion No (%) | |
| Christian | 46 (77) |
| Other/Did not answer | 16 (23) |
| Religious Observance No (%) | |
| Not observant | 7 (11) |
| Somewhat observant | 22 (36) |
| Very observant | 26 (43) |
| Did not answer | 7 (10) |
| Education No (%) | |
| High School | 18 (29) |
| College | 31 (50) |
| Graduate/Professional School | 12 (19) |
| Did not answer | 1 (2) |
| Patient Characteristic | |
| Years of Age, mean [SD] | 59 (13) |
| Gender No (%) | |
| Male | 42 (68) |
| Female | 20 (32) |
| Race/Ethnicity No (%) | |
| Hispanic | 30 (48) |
| Black, non-Hispanic | 19 (31) |
| White, non-Hispanic | 9 (15) |
| Other | 4 (6) |
| Independent with activities of daily living No (%) | 55 (89) |
| Sequential Organ Failure Assessment (SOFA) score, mean [SD] | 7 (4) |
| Outcomes No (%) | |
| Tracheostomy | 16 (26) |
| New Renal Replacement Therapy | 24 (40) |
| ICU death | 14 (23) |
3.1. Challenges faced by participants
Participants indicated four types of challenges during the ICU stays of patients with COVID-19 ( Table 2).
Type 1: Communication with the medical team. Participants reported that it was difficult having to wait to receive medical updates by telephone. As stated, “it's so hard because you are not there so you just wait for updates and it's so hard to wait sometimes.” When participants did not receive telephone calls at the expected time, they often worried that the delay was because the patient’s health was declining. One participant stated, “a doctor called me at 10:30 in the morning, and then I don't hear anything again till 10:30 in the evening. It's very difficult emotionally not knowing.” Participants were also concerned about calling into the ICU too frequently because they did not want to disrupt clinicians who were caring for patients with COVID-19: “I don't want to bother them (the staff) and I know there are other patients.” During the telephone update, some participants reported that clinicians seemed rushed or that communication was hampered by a perceived lack of continuity among staff. As stated, “sometimes it's (communication is) more rushed and or like today, it wasn't very good.”
Type 2: Communication among family members. Physicians on the primary medical team typically updated one designated surrogate each day. The surrogate who received the update from the medical team reported that it was difficult and time consuming to provide accurate updates to other concerned family members throughout the day. One participant stated, “You wait the whole day and then you get family members calling saying "what's going on?" It's a little unnerving.” Another stated, “we just have a lot of family that wants to know different information.”
Type 3: Understanding and tracking medical information. Participants indicated that it was difficult to internalize a large amount of information during a short telephone call with one the patient’s physicians. One participant commented, “there's a lot of things going on…So it's, I guess it's hard to keep track of everything.” Participants noted that there were times that they did not understand the information in the daily telephone update either because of medical jargon or the communication style of the physician. Some participants thought it was difficult to keep track of changes with the patient in part because of perceived inconsistencies from day to day. As stated, “the nurse started giving me wrong information. And I wasn't really sure how come that was happening. And I didn't believe her because I could tell what she was saying was inaccurate.”
Type 4: Distress related to visitor restrictions. Participants noted feeling stressed for several reasons related to visitor restrictions. Participants feared that the patient would feel alone and would lack motivation to improve without encouragement from family members. They also feared that an aspect of the patient’s care would be missed without a family member to advocate for the patient, which could lead to the patient’s decline. Participants stated, “I would love to just whisper my husband here to try to get him to continue to fight” and “it's a panic for me to know, because she's (the patient is) alone and I can't be there. No one can be there.” In part because participants were not able to directly witness the care provided to the patient, they spent parts of the day fearing that the patient’s condition was worsening: "it is quite scary when you have a loved one going through something and you can't go and touch and speak to them."
Table 2.
Types of challenges experienced by participants (N = 62).
| Challenge type | Specific challenge | Representative quote |
|---|---|---|
| Communication with the medical team | Hard to get in touch with clinicians by telephone | “It's been a couple times that I've called up there and I didn't get an answer and I had to call back later, or I'll call two or three times… not get an answer and had to call back later.” |
| Need to wait for updates by telephone | “It's hard on our emotional status not knowing for 8,10, 12 hours.it's very difficult for us.” | |
| Do not want to disturb medical staff by calling too frequently | “I don't call too often because I know they (the nurses) are busy.” | |
| Doctors/nurses seem rushed on the phone | “Sometimes it (communication) is more rushed or, like today, it wasn't very good…I felt like the phone literally cut out at one point.” | |
| Lack of continuity among medical staff | “I feel like, we're using different doctors to fill in here, right? It's like a different doctor every day. It's a different team.” | |
| Communication among family members | Need to update multiple family members | “I usually have to call like five different people (family members), repeating it, and try to remember everything to tell them.” |
| Understanding and tracking medical information | Difficult to understand/keep track of medical information | “I mean, they (clinicians) do use some terms, you know, like for medicine and like his "inflammatory markers" and stuff that I don't understand.” |
| Received incomplete or inconsistent information from doctors/nurses | “He (the clinician) said my dad was not on any antibiotics and I'm just like, what is going on here?” | |
| Distress related to visitor restrictions | Difficult to not visit patient due to pandemic guidelines | “Is there any way possible that if I was to get PPE, if I can go in there and try to communicate and talk with my dad… feel him, rub him, hold his hand” |
| Fear of medical decline | “I know my anxiety is pretty high. And I think [for] both of my stepdaughters it is, too. it's such a roller coaster. So, I mean, the doctors reassure us that everything that they've seen is pretty much normal on a COVID patient, but it's still high anxiety.” |
3.2. Adjustments to challenges
Participants developed approaches to dealing with each type of challenges ( Table 3).
Type 1: Communication with the medical team. Although participants may have received only one telephone update from the ICU team each day, they reported being satisfied overall with their communication with the medical team. Their satisfaction was, in part, due to developing a communication routine that involved receiving a phone call from a doctor at approximately the same time each afternoon. Participants would often call the ICU to speak with nurses at the time of shift change (morning and evening). One participant stated, “I made it a point to call like before the shift change in the morning usually before 6:30 in the morning, to talk to the night nurse. And then I would check in later in the day and then before I would go to bed … I've been getting verbal calls from the doctor on the case, usually, in the early afternoon, mid-afternoon in terms of the progress.” Although many participants would have preferred to receive medical information in person, they appreciated that the medical staff took time for a daily update and tried to ensure surrogate understanding. Participants also understood that staff may have been too busy for additional communication. As stated, “I understand that the ICU is so busy and they're (the medical team are) dealing with so much.”
Type 2: Communication among family members. Participants adjusted to the challenge of needing to update other family members not only by making multiple phone calls or individual text messages throughout the day, but also by using group text messages and online platforms such as Facebook and CaringBridge. On participant stated, “I would send daily updates to the family twice a day; once in the morning and then once at night.”
Type 3: Understanding and tracking medical information. To better understand or keep track of information, participants took notes, looked up information on the internet, and sought clarification from family/friends who were in healthcare fields. As stated, “We ask a lot of questions and then we sort of take notes and then share with other family members because …one of the people we know is a nurse so she sort of explains if … we have any questions we can ask her.”
Type 4: Distress related to visitor restrictions. Although participants found it difficult to not be able to visit the patient, they understood the reasons for visitor restrictions, which helped them adjust. One participant stated, “It’s hard not to be able to go up there and be there at the bedside…but that’s out of my control right now.” The distress of being unable to visit the hospital was alleviated, to some degree, with the use of video calls. Participants found comfort in seeing and talking to the patient, even if the patient was unable to communicate with them. As stated, “I was fortunate enough to be able to do a FaceTime visit with him on Saturday and [on] the day he got taken off the ventilator, which helps a lot.”
Table 3.
Participant approaches for dealing with challenges due to COVID-19 (N = 62).
| Challenge type | Approach for dealing with challenge | Representative quote |
|---|---|---|
| Communication with the medical team | Typically speaking with the medical team at least once per day | “I received a phone call daily from the doctor, sometimes twice, just depending on what was going on and I was able to call in and the nurse if she was available.” |
| Understanding that medical staff is busy/stressed | “[If] it took a little bit for somebody to get back to me, it's because I knew that they were tending to patients who are the priority.” | |
| Communication among family members | Communicating with family by telephone | “My family members usually want an update since they're all worried about my mom. And then when I get an update from the nurse, I call and tell my dad.” |
| Communicating with family by group chat/website/email | “We also have a family group chat. And we do a lot of FaceTime or zoom. And that's how we that's how we keep the whole family updated.” | |
| Understanding and tracking medical information | Taking notes to keep track of information | “I always have a notebook and … I normally keep detailed notes, because I have to give it to the family.” |
| Family member/friend is in healthcare field who helps to interpret medical information | “One of the people we know is a nurse. she sort of explains if we didn't really understand at the moment.” | |
| Research information using the internet | “When they said they were going to put my mom on ECMOa. I didn't know what that was so I googled it.” | |
| Distress related to visitor restrictions | Video call with patient was meaningful in absence of being able to visit | “I think that the video [calls] really, really helped me because I felt like my mother could hear us, you know, and then I think that that's what caused her to want to fight and to try to [get] better.” |
| Understanding the purpose of visitor restrictions | “But obviously we do understand that right now it's not possible [to visit].” |
ECMO: extracorporeal membrane oxygenation
4. Discussion and conclusion
Qualitative analyses of individual interviews with surrogates of ICU patients during the early phase of the COVID-19 pandemic revealed four types of challenges: Communication with the medical team, communication among family members, understanding and tracking medical information, and distress related to visitor restrictions. The daily telephone call from one of the patient’s care providers was typically the focal point of the family experience each day. The challenge of communicating with the medical team was lessened when participants developed a routine for receiving telephone updates. After the daily telephone call, participants updated other family members individually by telephone or by using group texts/message boards. They often took notes during these phone calls to keep track of information; if there was something they did not understand, they sought clarification from external sources. For many family members, being able to see the patient on a video call relieved some distress. These findings reinforce the importance of family visitation in the ICU to facilitate understanding of the patient’s condition and the emotional health of the family. Our findings reveal the resourcefulness of families in developing their own ways to cope with stressful situations and seek out external resources.
Although participants in our study experienced multiple challenges, they were generally satisfied with communication and care provided by the medical team. Even though the daily phone calls were short in duration, they were often long enough for clinicians to build rapport and a trusting relationship with participants [21], [22]. Our findings support those of previous investigators in which family satisfaction was related to being able to reach the medical staff, to feeling emotionally supported, to receiving regular medical updates from the medical staff, to feeling informed, and to the availability of video calls [12], [23], [24]. Our findings also suggest that satisfaction was partly related to family expectations; because participants understood that the staff was busy, they appreciated that clinicians took time to provide at least one update each day. Although not being able to visit the patient caused distress, participants understood that the visitor restrictions were in place to limit the spread of COVID-19.
Compared to previous studies examining the family experience during COVID-19 [12], [23], [24], [25], our study has many unique features that add to the collective understanding of the family experience during the COVID-19 pandemic. First, we describe the experience of families of patients admitted to a large, urban academic center at the height of the first wave of the COVID-19 pandemic in the United States. Current study participants were demographically diverse; this feature of our cohort is important given the observation that persons who are Black/African American or Hispanic/Latino were possibly at higher risk of mortality from COVID-19 [26]. Second, many of the previous studies have focused specifically on the experience of bereaved family members who were interviewed after ICU discharge [12], [24], [25]. In contrast, participants in our study were interviewed during the ICU stay; as a result, their impressions focused primarily on the aspects of the ICU stay that were difficult or helped them cope. In addition, the statements by participants in our study were not subject to recall bias and were not negatively affected by the patient’s ultimate outcome.
This study has the following limitations. The experience of participants was unique because it was conducted at one medical center during an early phase of the COVID-19 pandemic, when clinicians were gaining familiarity managing COVID-19 and caring for an increased number of critically ill patients. Another aspect of this study that may affect its generalizability is related to the characteristics of participants. Although surrogates were excluded if they were not fluent in the English language or did not have email access, these were uncommon reasons for surrogate exclusion. In cases where the primary language of the patient’s legal decision was not English, families often designated a relative who was fluent in English as the point person for communication with the medical team. Further study is needed to determine the extent to which fluency in the English language or education level affects the experience of families of patients with COVID-19. Finally, a unique feature of this study was the racial and ethnic diversity of the participants. However, given the small sample size, we were not able to determine whether participant demographics were associated with specific challenges or adjustments to challenges. The ways that racial and ethnic characteristics impact the ICU experience should be the subject of future study.
4.1. Conclusion
Many of the challenges faced by families of critically ill patients during the early phase of the COVID-19 pandemic were related to the fact that they were unable to visit the hospital. Because participants understood why they could not visit and developed their own strategies for coping, they were generally satisfied with the ICU experience. It is not clear whether more could or should have been done to support the psychological wellbeing of families during this unique time. It will be important to continue to learn about the challenges faced by families of critically ill patients with COVID-19 and the approaches for family engagement that improve the family experience.
4.2. Practice Implications
The COVID-19 pandemic has led to a vast amount of ICU utilization and death worldwide and has had a negative impact on the psychological well-being of populations in general [27], [28]. Research has shown that during infectious disease outbreaks, clinicians need to adjust the way they provide care to patients and their families [29], [30]. Prior to the COVID-19 pandemic, investigators focused on in-person meetings with families to support the psychological needs of families and help make medical decisions on behalf of the patient [31], [32]. It is unclear whether results of these studies generalize to times when visitation is restricted and meetings would need to occur over telephone or video call [6]. In our study, a participant’s experience was based on many factors including their expectations for communication with the medical team, their comfort receiving medical information by phone, stressors in their life, and the patient’s clinical course. Further study is needed to determine the types of approaches that not only ensure that families receive complete information when hospital visitation is restricted, but also support the psychological wellbeing of family members and help with the medical decision-making process [33]. Clinicians should use telephone interactions with families not only to provide information, but also to recognize the difficult nature of the family experience and to form an emotional connection with the families [11]. Expanded uses for technology in the ICU may help families feel engaged and connected to the ICU experience even when they cannot be physically present [34].
Funding
This work was supported by the Rush Coronavirus Research Fund.
CRediT authorship contribution statement
Jared Greenberg: Conceptualization, Methodology, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. Santosh Basapur: Conceptualization, Methodology, Formal analysis, Investigation, Writing – review & editing. Thomas Quinn: Conceptualization, Methodology, Formal analysis, Investigation, Writing – review & editing. Jeffrey Bulger: Conceptualization, Methodology, Formal analysis, Investigation, Writing – review & editing. Nathanial Schwartz: Conceptualization, Methodology, Formal analysis, Investigation, Writing – review & editing. Soo Kyung Oh: Conceptualization, Methodology, Formal analysis, Investigation, Writing – review & editing. Raj Shah: Conceptualization, Methodology, Writing – review & editing. Crystal Glover: Conceptualization, Methodology, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Clinical trial registered at ClinicalTrials.gov (NCT03969810).
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.pec.2021.08.029.
Appendix A. Supplementary material
Supplementary material.
.
References
- 1.Davidson J.E., Aslakson R.A., Long A.C., Puntillo K.A., Kross E.K., Hart J., et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45(1):103–128. doi: 10.1097/CCM.0000000000002169. [DOI] [PubMed] [Google Scholar]
- 2.Rosa R.G., Tonietto T.F., da Silva D.B., Gutierres F.A., Ascoli A.M., Madeira L.C., et al. Effectiveness and safety of an extended ICU visitation model for delirium prevention: a before and after study. Crit Care Med. 2017;45(10):1660–1667. doi: 10.1097/CCM.0000000000002588. [DOI] [PubMed] [Google Scholar]
- 3.Westphal G.A., Moerschberger M.S., Vollmann D.D., Inacio A.C., Machado M.C., Sperotto G., et al. Effect of a 24-h extended visiting policy on delirium in critically ill patients. Intensive Care Med. 2018;44(6):968–970. doi: 10.1007/s00134-018-5153-5. [DOI] [PubMed] [Google Scholar]
- 4.Davidson J.E., Jones C., Bienvenu O.J. Family response to critical illness: postintensive care syndrome-family. Crit Care Med. 2012;40(2):618–624. doi: 10.1097/CCM.0b013e318236ebf9. [DOI] [PubMed] [Google Scholar]
- 5.Amass T.H., Villa G., S O.M., Badger J.M., McFadden R., Walsh T., et al. Family care rituals in the ICU to reduce symptoms of post-traumatic stress disorder in family members-a multicenter, multinational, before-and-after intervention trial. Crit Care Med. 2020;48(2):176–184. doi: 10.1097/CCM.0000000000004113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kennedy N.R., Steinberg A., Arnold R.M., Doshi A.A., White D.B., DeLair W., et al. Perspectives on telephone and video communication in the intensive care unit during COVID-19. Ann Am Thorac Soc. 2021;18:838–847. doi: 10.1513/AnnalsATS.202006-729OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valley T.S., Schutz A., Nagle M.T., Miles L.J., Lipman K., Ketcham S.W., et al. Changes to visitation policies and communication practices in Michigan ICUs during the COVID-19 pandemic. Am J Respir Crit Care Med. 2020;202:883–885. doi: 10.1164/rccm.202005-1706LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hwang D.Y., Zhang Q., Andrews A., LaRose K., Gonzalez M., Harmon L., et al. The initial impact of the coronavirus disease 2019 pandemic on ICU family engagement: lessons learned from a collaborative of 27 ICUs. Crit Care Explor. 2021;3(4):0401. doi: 10.1097/CCE.0000000000000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenberg J.A., Basapur S., Quinn T.V., Bulger J.L., Glover C.M., Shah R.C. Psychological symptoms among surrogates of critically Ill patients during and before the COVID-19 pandemic. Chest. 2021;159:2318–2320. doi: 10.1016/j.chest.2020.12.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vincent A., Beck K., Becker C., Zumbrunn S., Ramin-Wright M., Urben T., et al. Psychological burden in patients with COVID-19 and their relatives 90 days after hospitalization: a prospective observational cohort study. J Psychosom Res. 2021;147 doi: 10.1016/j.jpsychores.2021.110526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Montauk T.R., Kuhl E.A. COVID-related family separation and trauma in the intensive care unit. Psychol Trauma. 2020;12(S1):S96–S97. doi: 10.1037/tra0000839. [DOI] [PubMed] [Google Scholar]
- 12.Feder S., Smith D., Griffin H., Shreve S.T., Kinder D., Kutney-Lee A., et al. “Why couldn’t i go in to see him?” Bereaved families’ perceptions of end-of-life communication during COVID-19. J Am Geriatr Soc. 2021;69(3):587–592. doi: 10.1111/jgs.16993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Creswell J.W., Creswell J.D. fifth ed. SAGE; Los Angeles: 2018. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. [Google Scholar]
- 14.Creswell J.W., Poth C.N. fourth ed. SAGE; Los Angeles: 2018. Qualitative Inquiry & Research Design: Choosing Among Five Approaches. [Google Scholar]
- 15.Gottlieb M., Sansom S., Frankenberger C., Ward E., Hota B. Clinical course and factors associated with hospitalization and critical illness among COVID-19 patients in Chicago, Illinois. Acad Emerg Med. 2020;27(10):963–973. doi: 10.1111/acem.14104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bulger J.L., Quinn T.V., Glover C.M., Basapur S., Shah R.C., Greenberg J.A. Written care summaries facilitate communication between families and providers of ICU patients: a pilot study. Crit Care Explor. 2021;3(7):0473. doi: 10.1097/CCE.0000000000000473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kvale S. Sage Publications; Thousand Oaks, Calif.: 1996. Interviews: An Introduction to Qualitative Research Interviewing. [Google Scholar]
- 18.Given L.M. Sage Publications; Los Angeles, Calif.: 2008. The Sage Encyclopedia of Qualitative Research Methods. [Google Scholar]
- 19.Flick U. sixth ed. SAGE Publications; Thousand Oaks, CA: 2018. An Introduction to Qualitative Research. [Google Scholar]
- 20.Thomas J., Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bouchoucha S.L., Bloomer M.J. Family-centered care during a pandemic: the hidden impact of restricting family visits. Nurs Health Sci. 2021;23:4–6. doi: 10.1111/nhs.12748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koller D.F., Nicholas D.B., Goldie R.S., Gearing R., Selkirk E.K. When family-centered care is challenged by infectious disease: pediatric health care delivery during the SARS outbreaks. Qual Health Res. 2006;16(1):47–60. doi: 10.1177/1049732305284010. [DOI] [PubMed] [Google Scholar]
- 23.Chen C., Wittenberg E., Sullivan S.S., Lorenz R.A., Chang Y.P. The experiences of family members of ventilated COVID-19 patients in the intensive care unit: a qualitative study. Am J Hosp Palliat Care. 2021;38(7):869–876. doi: 10.1177/10499091211006914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kentish-Barnes N., Cohen-Solal Z., Morin L., Souppart V., Pochard F., Azoulay E. Lived experiences of family members of patients with severe COVID-19 who died in intensive care units in France. JAMA Netw Open. 2021;4(6) doi: 10.1001/jamanetworkopen.2021.13355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mohammadi F., Oshvandi K., Shamsaei F., Cheraghi F., Khodaveisi M., Bijani M. The mental health crises of the families of COVID-19 victims: a qualitative study. BMC Fam Pract. 2021;22(1):94. doi: 10.1186/s12875-021-01442-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gross C.P., Essien U.R., Pasha S., Gross J.R., Wang S.Y., Nunez-Smith M. Racial and ethnic disparities in population-level covid-19 mortality. J Gen Intern Med. 2020;35(10):3097–3099. doi: 10.1007/s11606-020-06081-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burn W., Mudholkar S. Impact of COVID-19 on mental health: update from the United Kingdom. Indian J Psychiatry. 2020;62(3):S365–S372. doi: 10.4103/psychiatry.IndianJPsychiatry_937_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weinberger D.M., Chen J., Cohen T., Crawford F.W., Mostashari F., Olson D., et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med. 2020;180(10):1336–1344. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chan S.S., Leung D., Chui H., Tiwari A.F., Wong E.M., Wong D.C., et al. Parental response to child’s isolation during the SARS outbreak. Ambul Pedia. 2007;7(5):401–404. doi: 10.1016/j.ambp.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Papadimos T.J., Marcolini E.G., Hadian M., Hardart G.E., Ward N., Levy M.M., et al. Ethics of outbreaks position statement. Part 2: family-centered care. Crit Care Med. 2018;46(11):1856–1860. doi: 10.1097/CCM.0000000000003363. [DOI] [PubMed] [Google Scholar]
- 31.Lautrette A., Darmon M., Megarbane B., Joly L.M., Chevret S., Adrie C., et al. A communication strategy and brochure for relatives of patients dying in the ICU. New Engl J Med. 2007;356(5):469–478. doi: 10.1056/NEJMoa063446. [DOI] [PubMed] [Google Scholar]
- 32.White D.B., Angus D.C., Shields A.M., Buddadhumaruk P., Pidro C., Paner C., et al. A randomized trial of a family-support intervention in intensive care units. New Engl J Med. 2018;378(25):2365–2375. doi: 10.1056/NEJMoa1802637. [DOI] [PubMed] [Google Scholar]
- 33.Kon A.A., Davidson J.E., Morrison W., Danis M., White D.B., American College of Critical Care M., et al. Shared decision making in ICUs: an American college of critical care medicine and American thoracic society policy statement. Crit Care Med. 2016;44(1):188–201. doi: 10.1097/CCM.0000000000001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang H., Poehler J.L., Ziegler J.L., Weiler C.C., Khan S.A. Patient care rounds in the intensive care unit during COVID-19. Jt Comm J Qual Patient Saf. 2020;46(10):600–601. doi: 10.1016/j.jcjq.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.