Abstract
The vagina is colonized by a variety of microbes that serve vital roles in the maintenance of vaginal health. The purpose of the present study was to explore the underlying mechanism by which Gardnerella vaginalis (GV) can induce bacterial vaginosis (BV). The viability of primary mouse macrophages and THP-1 cells was detected using a Cell Counting Kit-8 assay. Lactate dehydrogenase and caspase-1 activity in the culture medium of macrophages and THP-1 cells were measured using a colorimetric assay and a caspase-1 activity assay kit, respectively. In the macrophages and THP-1 cells, the levels of TNF-α, IL-1β and IL-18 were detected using ELISA whereas reactive oxygen species (ROS) levels were detected using flow cytometry. The pyroptosis of macrophages and THP-1 cells was detected using calcein-AM/PI double staining. Expression of proteins associated with the nucleotide-binding oligomerization domain, leucine rich repeat and pyrin domain-containing protein 3 inflammasome (NLRP3), including NLRP3, apoptosis associated speck-like protein (ASC), caspase-1 and pro-caspase-1, were measured by western blotting and reverse transcription-quantitative PCR. GV significantly inhibited cell viability and increased LDH activity in macrophages and THP-1 cells. In addition, GV markedly promoted the production of TNF-α, IL-1β, IL-18 and ROS by macrophages and THP-1 cells. GV significantly promoted caspase-1 activation-mediated pyroptosis in macrophages and THP-1 cells. Treatment with GV significantly increased the protein and mRNA expression of NLRP3, ASC and caspase-1 in macrophages and THP-1 cells. To conclude, data from the present study suggest that G. vaginalis can induce BV by promoting NLRP3 inflammasome-mediated pyroptosis, which provides one of the molecular mechanisms by which G. vaginalis can induce BV.
Keywords: Gardnerella vaginalis, bacterial vaginosis, nucleotide-binding oligomerization domain, leucine rich repeat and pyrin domain-containing protein 3 inflammasome, pyroptosis, inflammation
Introduction
Bacterial vaginosis (BV) is a common chronic microbial genital tract infection in women that is characterized by vaginal pH elevation, malodorous discharge and inflammation (1,2). The female vagina is colonized by a variety of microbes, which serve important roles in maintaining vaginal health (3,4). Disruptions in the vaginal microbiota can lead to BV by promoting infection from several species of pathogens, including Gardnerella vaginalis (G. vaginalis) and gram-negative anaerobes, such as Prevotella, Mobiluncus and Bacteroides species (5,6). An increasing number of studies have demonstrated that G. vaginalis a major class of bacteria that can cause BV (7,8). However, the underlying mechanism by which G. vaginalis induces BV remain unclear.
Nucleotide-binding oligomerization domain, leucine rich repeat, pyrin (NLRP) and HIN domaintein and absent in melanoma 2 are considered to be major members of the inflammasome family (9). The NLRP3 inflammasome consists of NLRP3-containing protein 3 (NLRP3), apoptosis associated speck-like protein (ASC) and pro-caspase-1, which is an important mediator of immune responses and can be activated by a variety of stimuli, including pathogens and tissue damage (10,11). Once NLRP3 is activated, it causes the cleavage of pro-caspase-1 into active caspase-1, which can induce the secretion of proinflammatory cytokines, such as IL-1β and IL-18, in turn causing pyroptotic cell death (12,13). Schroder and Tschopp (12) previously reported that monocytes and macrophages are commonly present in the lamina propria of vaginal tissues, which not only secrete proinflammatory cytokines but can also regulate the formation of various inflammasome complexes (NLRP1 and NLRP3) under the action of various microbial stressors. In addition, a study has suggested that G. vaginalis frequently infects the vagina and can activate the NLRP3 inflammasome, leading to BV (14). However, whether G. vaginalis induces BV by activating the NLRP3 inflammasome remains unclear.
Therefore, in the present study, the underlying mechanisms by which G. vaginalis induces BV were explored. Specifically, the effect of G. vaginalis infection on NLRP3 inflammasome-mediated pyroptosis in macrophages was investigated. The results of the present study may provide a promising therapeutic direction for BV.
Materials and methods
Bacterial culture
G. vaginalis (GV; type strain no. KCTC5096) was supplied by the Korean Collection for Type Cultures (Daejon, Korea). GV was incubated in the brain heart infusion broth (Becton-Dickinson and Company) supplemented with yeast extract (1%; Beyotime Institute of Biotechnology), maltose (0.1%; Beyotime Institute of Biotechnology), glucose (0.1%, Sigma-Aldrich; Merck KGaA) and horse serum (10%; Beyotime Institute of Biotechnology) at 37˚C for 36 h under anaerobic conditions (controlled atmosphere composed of 10% carbon dioxide, 10% helium and 80% nitrogen in an anaerobic jar). GV was then suspended in PBS for subsequent in vitro experiments.
Primary culture of mouse peritoneal macrophages and THP-1 monocyte cell culture
The primary culture of mouse peritoneal macrophages was established as described previously (15). A total of 36 female ICR mice (8 weeks old, 25±1 g) were supplied by Beijing Vital River Laboratory Animal Technology Co., Ltd. The mice were housed in wire cages under climate-controlled conditions (humidity, 5±10%; temperature, 20-22°C; 12 h light/dark cycle) and received ad libitum access to standard laboratory chow and water. The mice were intraperitoneally injected with 2 ml 4% thioglycolate (Sigma-Aldrich; Merck KGaA). After 3 days, all mice were sacrificed by cervical dislocation before the peritoneal cavity fluid was collected and pooled together. This sample was then centrifuged at 3,000 x g at 4˚C for 10 min and the cells collected, washed with RPMI-1640 medium (Invitrogen; Thermo Fisher Scientific, Inc.) and suspended in RPMI-1640 medium supplemented with 10% FBS (Gibco; Thermo Fisher Scientific, Inc.) and 1% penicillin/streptomycin (Sigma-Aldrich; Merck-KGaA). Subsequently, the cells were cultured for 20 h at 37˚C and the adherent cells were defined as macrophages (16). The present study was approved by the committee of ethical animal care and use of laboratory animals of Shandong Provincial Third Hospital (approval no. DWKYLL-2020001).
THP-1 monocyte cells were obtained from the American Type Culture Collection and cultured in RPMI 1640 medium containing 10% FBS, 50 µM 2-mercaptoethanol and 1% penicillin/streptomycin at 37˚C in 5% CO2. The THP-1 monocytes were differentiated by treating the cells with 100 nM phorbol 12-myristate 13-acetate (Thermo Fisher Scientific, Inc.) for 24 h at 37˚C.
For treatment, the primary mouse macrophages and THP-1 cells were respectively seeded at 2x106 cells/well into six-well plates before they were treated with either fresh medium, medium containing 1 µg/ml LPS (Sigma-Aldrich; Merck KGaA), medium containing GV at a multiplicity of infection of 10 or medium containing both LPS and GV, at 37˚C for 12 h.
Cell viability assay
Cell viability was detected using a Cell Counting Kit-8 (CCK-8) assay kit (Dojindo Molecular Technologies, Inc.) according to the manufacturer's protocols. The macrophages and THP-1 cells were seeded into 96-well plates at a density of 1x104 cells/well. After exposure to LPS and GV, CCK-8 (10 µl) was added into each well and the plates were incubated at 37˚C for 1 h in the dark. Finally, the absorbance was measured using a microplate reader at a wavelength of 450 nm.
LDH level analysis
The activity of lactate dehydrogenase (LDH) in the culture medium of THP-1 cells and macrophages was analyzed using a colorimetric assay (cat. no. A020-1-2; Nanjing Jiancheng Bioengineering Institute) by following the manufacturer's protocols. The absorbance at 490 nm was determined with a microplate reader.
Detection of reactive oxygen species (ROS)
The fluorescent probe dichloro-dihydro-fluorescein diacetate (DCFH-DA; Sigma-Aldrich; Merck KGaA) was used to measure intracellular ROS levels by following the manufacturer's protocols. Briefly, the macrophages and THP-1 cells (5x105 cells/ml) were incubated with 40 µM DCFH-DA in serum-free medium for 30 min in the dark at 37˚C and then washed with PBS three times. Finally, the fluorescence of the cells was examined by using flow cytometry (FACSCalibur; BD Biosciences) at excitation and emission wavelengths of 488 and 525 nm. The data were analyzed using FlowJo software (version v7.6.5; FlowJo LLC).
Measurement of caspase-1 activity
Caspase-1 activity in the culture supernatant of THP-1 cells and macrophages was measured using a caspase-1 activity assay kit (cat. no. C1102; Beyotime Institute of Biotechnology) by following the manufacturer's protocols. Absorbance at 405 nm was determined for each well with a microplate reader.
ELISA
The levels of TNF-α (mouse cat. no. PMTA00B; human cat. no. PDTA00D), IL-1β (mouse cat. no. PMLB00C; human cat. no. PDLB50) and IL-18 (mouse cat. no. DY7625-05; human cat. no. DY318-05) in the culture supernatant of macrophages and THP-1 cells were detected by using their corresponding ELISA kits (all from R&D systems, Inc.) according to the protocols of the manufacturer.
Calcein-AM/propidium Iodide (PI) staining assay
Calcein-AM/PI double staining (cat. no. C2015M; Beyotime Institute of Biotechnology) was used to quantify the number of living and dead cells as a cell death assay. Briefly, the macrophages and THP-1 cells (5x105 cells/ml) were mixed with 1X assay buffer and then stained with 2 µM calcein-AM and 4.5 µM PI per well for 30 min at 37˚C. The percentage of positive cells was counted and the image were scanned with a fluorescence microscope (magnification, x100). The number of PI positive cells represented pyroptosis, which was calculated using the following equation: PI positive cells (%)=(PI positive cells/Calcein-AM positive cells) x100%.
Reverse transcription-quantitative PCR (RT-qPCR)
TRIzol® reagent (Invitrogen; Thermo Fisher Scientific, Inc.) was applied to extract total RNA from the macrophages and THP-1 cells. The synthesis of cDNA was performed using the PrimeScript II 1st Strand cDNA Synthesis kit (cat. no. 6210A; Takara Bio, Inc.). The conditions for RT were as follows: 25˚C for 5 min, 55˚C for 20 min and 85˚C for 5 min. qPCR was performed using SYBR® Premix Ex Taq™ (cat. no. RR42LR; Takara Bio, Inc.) in the ABI StepOne Plus™ RT-PCR System (Applied Biosystems; Thermo Fisher Scientific, Inc.). Primers were supplied by Shanghai GenePharma Co., Ltd. The sequences were as follows: NLRP3 forward, 5'-GCTGGTCTTGAATTCCTCA-3' and reverse, 5'-GGCACACGGATGAGTCTTT-3'; ASC forward, 5'-CCAAATGCTTCCCCCATCCT-3' and reverse, 5'-GCCCTTTGGTACATGCCTCT-3'; caspase-1 forward, 5'-CTACTTCCCTGAATGCTTGGC-3' and reverse, 5'-GCTCCTGGGTTTGTCCACTC-3' and GAPDH forward, 5'-GCACCGTCAAGGCTGAGAAC-3' and reverse, 5'-GCCTTCTCCATGGTGGTGAA-3'. The thermocycling conditions for qPCR were follows: Initial denaturation at 95˚C for 3 min, followed by 40 cycles of 95˚C for 10 sec, 60˚C for 30 sec and 72˚C for 30 sec. GAPDH was used as the internal reference. The relative gene expression levels were calculated using the 2-ΔΔCq method (17).
Western blot analysis
Total protein was extracted from macrophages and THP-1 cells using RIPA lysis buffer (Beyotime Institute of Biotechnology). Subsequently, the protein concentrations were determined by a BCA protein Assay kit (Roche Diagnostics). Protein (50 µg) was separated by 10% SDS-PAGE and then transferred onto PVDF membranes. After blocking for 2 h in 5% skim milk at room temperature, the membranes were incubated overnight at 4˚C with the following primary antibodies: Rabbit monoclonal antibody against NLRP3 (cat. no. 15101; 1:500; Cell Signaling Technology, Inc.), rabbit monoclonal antibody against ASC (cat. no. ab47092; 1:1,000, Abcam), rabbit polyclonal antibody against pro-caspase-1 (cat. no. 22915-1-AP; 1:1,000, Proteintech Group, Inc.), rabbit polyclonal antibody against caspase-1 (cat. no. 22915-1-AP; p10; 1:500; Proteintech Group, Inc.) and rabbit polyclonal antibody against GAPDH (cat. no. 10494-1-AP; 1:2,000, Proteintech Group, Inc.). After washing with PBST three times, the membranes were incubated with the horseradish peroxidase-conjugated secondary antibodies (cat. no. SA00001-2; 1:5,000; Proteintech Group, Inc.) for 2 h at room temperature. Finally, Proteins were visualized using the Immobilon Western Chemiluminescent HRP substrate (cat. no. WBKLS0500; EMD Millipore), and then the blots were analyzed using the ChemiDoc XRS system (Bio-Rad Laboratories, Inc.). The density of the protein bands was quantified using ImageJ software (version V1.8.0; National Institutes of Health).
Statistical analysis
All statistical analyses were performed using the SPSS 22.0 Statistical Software (IBM Corp.). The results were presented as the mean ± standard error of the mean. One-way ANOVA followed by Tukey's post hoc test was used to compare differences among the treatment groups. P<0.05 was considered to indicate a statistically significant difference. Each experiment was performed at least three times.
Results
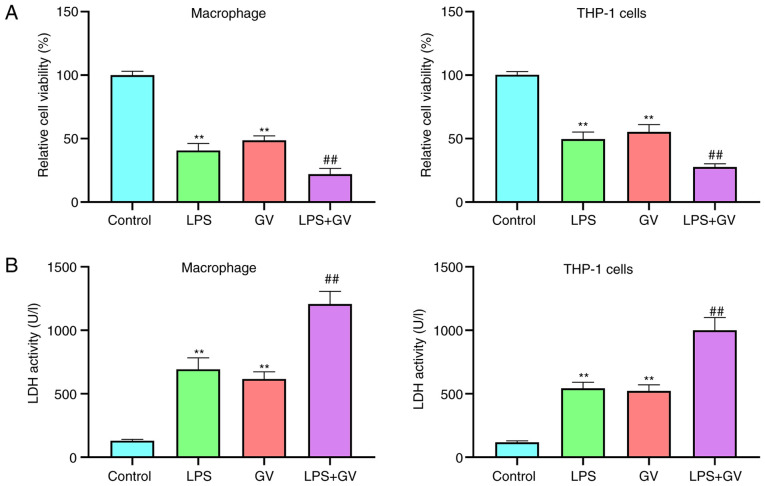
GV inhibits cell viability and promotes LDH release from primary mouse macrophages and THP-1 cells
In the present study, treatment of LPS was used as the positive control for NLRP3-mediated inflammasome activation (14). To explore the effect of GV on cellular physiology, cell viability and LDH release from macrophages and THP-1 cells were measured. Results from the CCK-8 assay revealed that the viability of macrophages and THP-1 cells was significantly decreased in the LPS or GV groups compared with that in the Control group (P<0.01; Fig. 1A). Compared with the LPS or GV groups, cell viability was significantly reduced in the LPS + GV group (P<0.01; Fig. 1A). In addition, LDH activities in the cell culture supernatant of the LPS or GV groups were significantly higher compared with those in the Control group (P<0.01; Fig. 1B). However, LDH activities in the cell culture supernatant of the LPS or GV groups were both significantly lower than those in the LPS + GV group (P<0.01; Fig. 1B). These results suggested that GV induced macrophage and THP-1 cell injury.
Figure 1.
GV inhibits cell viability and promotes LDH release from primary mouse macrophages and THP-1 cells. (A) Viability of macrophages and THP-1 cells was detected using Cell Counting Kit-8 assay. (B) LDH release from macrophages and THP-1 cells was measured in their respective cell culture supernatants. **P<0.01 vs. Control; ##P<0.01 vs. LPS or GV groups. GV, Gardnerella vaginalis; LDH, lactate dehydrogenase; LPS, liposaccharide.
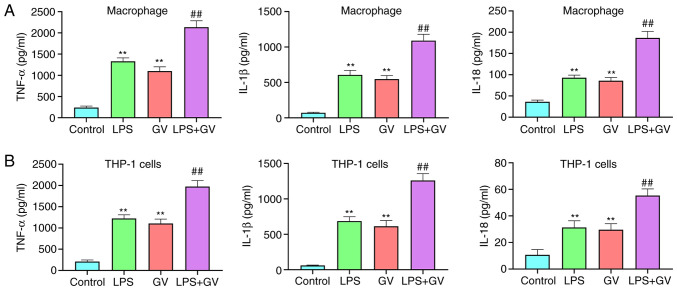
GV promotes the production of proinflammatory cytokines in primary mouse macrophages and THP-1 cells
As presented in Fig. 2A and B, pretreatment with LPS or GV significantly increased the levels of TNF-α, IL-1β and IL-18 in the macrophages and THP-1 cells compared with those in the Control group (P<0.01). In addition, co-treatment with both LPS and GV significantly promoted the levels of TNF-α, IL-1β and IL-18 in macrophages and THP-1 cells compared with those in the LPS or GV groups (P<0.01). These data suggested that GV can promote the production of proinflammatory cytokines in macrophages and THP-1 cells.
Figure 2.
GV promotes the production of proinflammatory cytokines in primary mouse macrophages and THP-1 cells. The levels of TNF-α, IL-1β and IL-18 in the culture medium of (A) macrophages and (B) THP-1 cells were measured by ELISA. **P<0.01 vs. Control; ##P<0.01 vs. LPS or GV. GV, Gardnerella vaginalis; LPS, liposaccharide.
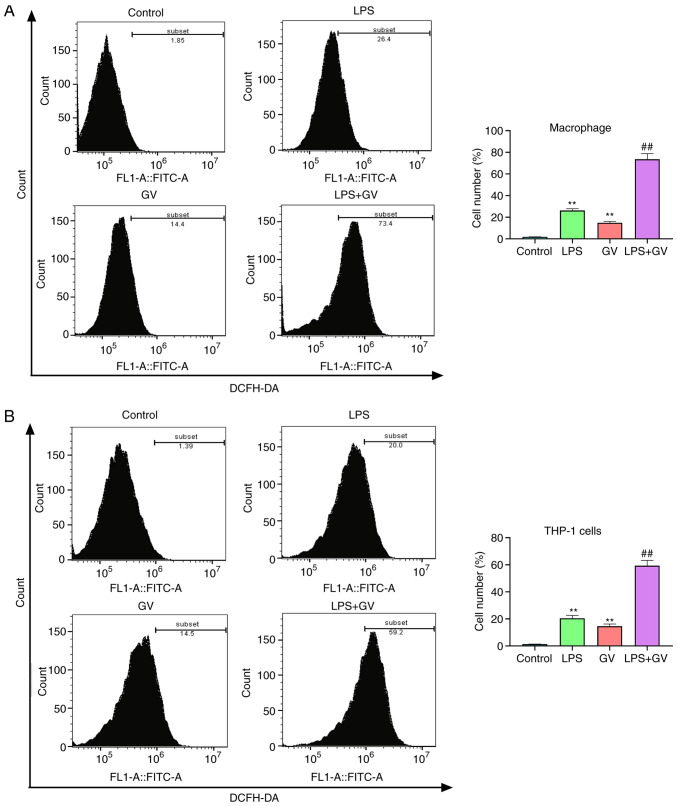
GV promotes the production of ROS in primary mouse macrophages and THP-1 cells
ROS production has been reported to be one of the mechanisms responsible for NLRP3 inflammasome activation and pyroptosis (18,19). According to Fig. 3A and B, treatment with LPS or GV significantly elevated the levels of ROS in macrophages and THP-1 cells compared with those in the Control group (P<0.01). In addition, combined treatment with both LPS and GV significantly increased ROS amounts in macrophages and THP-1 cells relative to those in the LPS or GV groups (P<0.01). These results aforementioned suggested that GV can promote the production of ROS in macrophages and THP-1 cells.
Figure 3.
GV promotes the production of ROS in primary mouse macrophages and THP-1 cells. ROS levels in (A) macrophages and (B) THP-1 cells were measured using dichloro-dihydro-fluorescein diacetate staining and flow cytometry. **P<0.01 vs. Control; ##P<0.01 vs. LPS or GV. GV, Gardnerella vaginalis; LPS, liposaccharide; ROS, reactive oxygen species.
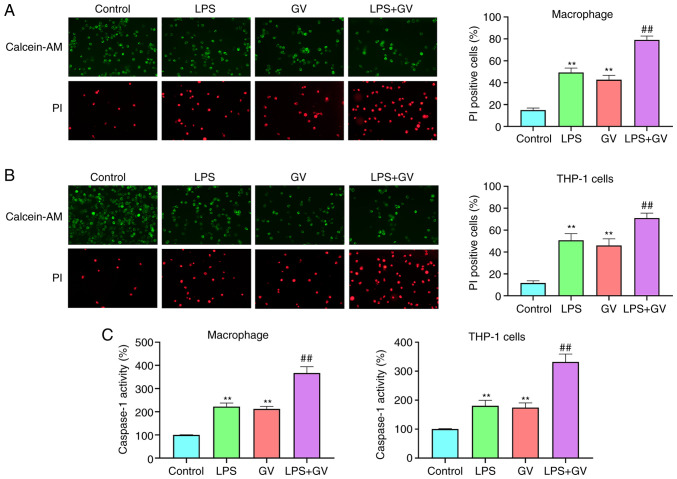
GV promotes the pyroptosis of macrophages and THP-1 cells
To assess if GV-induced injury of macrophages and THP-1 cells was associated with caspase-1 activation-mediated pyroptosis, caspase-1 activity was measured and cells positive for pyroptosis were detected by calcein-AM/PI double staining. LPS or GV treatment significantly facilitated pyroptotic cell death relative to that in the Control group (P<0.01; Fig. 4A and B). Furthermore, combined LPS and GV treatment significantly increased pyroptotic cell death in macrophages and THP-1 cells compared with that in the LPS or GV groups (P<0.01; Fig. 4A and B). Caspase-1 activity in the LPS or GV groups was also found to be significantly higher compared with that in the Control group (P<0.01; Fig. 4C), which in turn was significantly lower compared with that in the LPS + GV group (P<0.01; Fig. 4C). These results indicated that GV can promote the pyroptosis of macrophages and THP-1 cells.
Figure 4.
GV promotes the pyroptosis in primary mouse macrophages and THP-1 cells. (A) The pyroptosis of (A) macrophages and (B) THP-1 cells was detected by Calcein-AM/PI double staining was detected by Calcein-AM/PI double staining (magnification, x100). (C) Caspase-1 activity in macrophages and THP-1 cells was measured using a caspase-1 activity assay kit. **P<0.01 vs. Control; ##P<0.01 vs. LPS or GV. GV, Gardnerella vaginalis; LPS, liposaccharide.
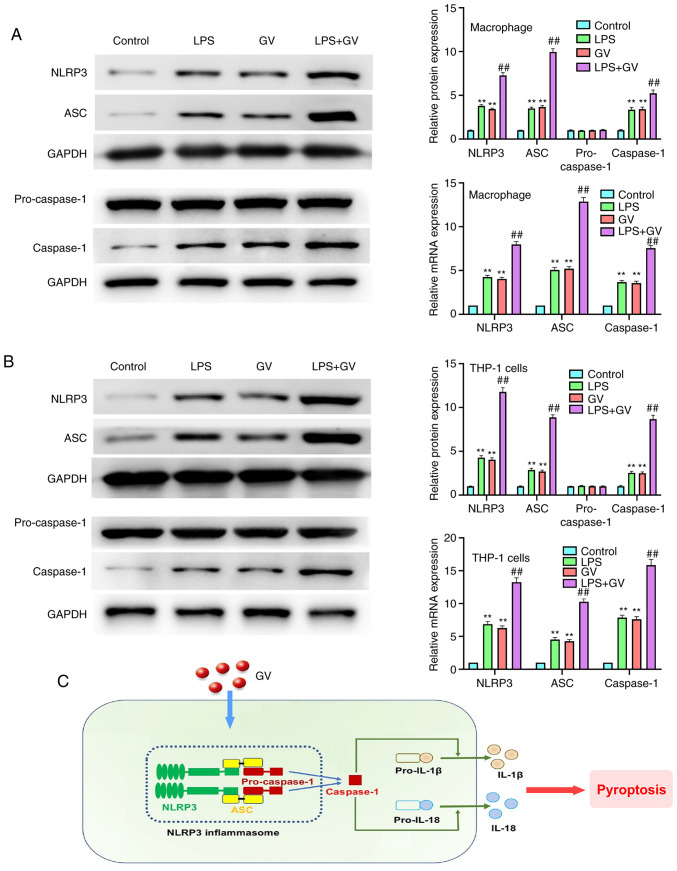
GV promotes the activation of NLRP3 inflammasomes in primary mouse macrophages and THP-1 cells
As presented in Fig. 5A and B, the protein and mRNA expression of NLRP3, ASC and caspase-1 in macrophages and THP-1 cells were significantly increased in the LPS or GV groups compared with those in the Control group (P<0.01). By contrast, the protein and mRNA expression of NLRP3, ASC and caspase-1 in the LPS or GV groups were significantly lower compared with those in the LPS + GV group (P<0.01). However, no changes in the pro-caspase-1 protein expression levels were observed. All these observations suggested that GV can promote the activation of NLRP3 inflammasomes in macrophages and THP-1 cells.
Figure 5.
GV promotes the activation of the NLRP3 inflammasome in primary mouse macrophages and THP-1 cells. The protein and mRNA expression of NLRP3, ASC, pro-caspase-1 and caspase-1 in (A) macrophages and (B) THP-1 cells were detected by western blotting and reverse transcription-quantitative PCR. (C) Proposed model of GV-induced NLRP3/ASC/caspase-1-dependent pyroptosis in primary mouse macrophages and THP-1 cells.**P<0.01 vs. Control; ##P<0.01 vs. LPS or GV. GV, Gardnerella vaginalis; LPS, liposaccharide; NLRP3, nucleotide-binding oligomerization domain, leucine rich repeat and pyrin domain-containing protein 3; ASC, apoptosis associated speck-like protein.
Discussion
BV is an inflammatory vaginal disease that is caused by the displacement of lactic-acid producing Lactobacillus spp. of bacteria with anaerobic bacteria, including G. vaginalis, Prevotella spp., Sneathia spp. and Atopobium vaginae (20). Previous studies have documented that G. vaginalis infection is present in all cases of BV, which can contribute to BV pathogenesis (21,22). At present, although antimicrobials are commonly used for treating BV, they do not prevent its recurrence. In addition, a growing body of evidence suggests that resistant G. vaginalis can arise from long-term antimicrobial treatment (23). Therefore, there is a demand for investigating the underlying mechanism by which G. vaginalis induces BV. In the present study, a novel mechanism was revealed, by which G. vaginalis can activate the NLRP3/ASC/caspase-1 pathway in macrophages and THP-1 cells to induce pyroptosis (Fig. 5C).
A number studies have suggested previously that the level of cytokines and chemokines, such as TNF-α and IL-1β, is upregulated in the vaginal fluid of women with BV (24,25). Mechanisms underlying the host immune response to key BV-associated bacteria have also been investigated using in vitro or in vivo models (26,27). G. vaginalis and Atopobium vaginae have both been reported to amplify proinflammatory responses to Trichomonas vaginalis (28). Macrophages and monocytes are commonly present in the lamina propria of vaginal tissues, which have been shown to regulate the expression of innate immune response receptors (12,29). During G. vaginalis infection, proinflammatory cytokines are secreted from monocytes and macrophages (14). The present study confirmed that GV can significantly promote the production of TNF-α, IL-1β and IL-18 in primary mouse macrophages and THP-1 cells. This is consistent with a previous study performed by Anahtar et al (30), who reported that Sneathia spp. can induce IL-1β and IL-18, but not TNF-α, in vaginal epithelial monolayer cultures. Large quantities of ROS are produced during the inflammatory process, which aggravate cell injury and cell death (31). In the present study, GV was found to promote the production of ROS in macrophages and THP-1 cells. Previously, several studies have demonstrated that the production of ROS is an important mechanism responsible for pyroptosis and NLRP3 inflammasome activation (18,19). Pyroptosis is a unique form of programmed cell death that is mediated by inflammasome and caspase-1 activation (32,33). Caspase-1-mediated pyroptosis has been suggested to serve an important role in bacterial- and inflammation-related diseases, including Trichomonas vaginalis infection and myocardial infarction (34). In the present study, the effects of GV on pyroptosis were assessed by Calcein-AM/PI double staining, which revealed that GV promoted caspase-1 activation-mediated pyroptosis in macrophages and THP-1 cells.
Activation of caspase-1 during pyroptosis requires a protein platform called inflammasomes (35). Among the inflammasome complexes currently known, the NLRP3 inflammasome has been extensively characterized and consists of NLRP3, ASC and pro-caspase-1 (36,37). Upon activation, NLRP3 recruits ASC and induces the activation of caspase-1, thereby promoting the secretion of proinflammatory cytokines to ultimately induce pyroptotic cell death (38). Over the past decade, the NLRP3 inflammasome is garnering attention due to its reported involvement in the development of a variety of diseases, including knee osteoarthritis, atherosclerosis and mastitis (39). The NLRP3 inflammasome can be activated by a number of stimuli, including bacterial, viral and mitochondrial damage (40). In addition, macrophages and monocytes in the lamina propria of vaginal tissue can not only secrete proinflammatory cytokines, but also regulate the formation of various inflammasome complexes in response to multiple microbial stimuli (12). In the present study, to investigate if G. vaginalis can induce BV by activating the NLRP3 inflammasome, the expression levels of NLRP3, ASC, pro-caspase-1 and caspase-1 were measured by western blotting and RT-qPCR. It was revealed that pretreatment with GV significantly increased the protein and mRNA expression of NLRP3, ASC and caspase-1 in macrophages and THP-1 cells. This supports the notion that GV can promote the activation of NLRP3 inflammasomes in macrophages and THP-1 cells, which is a novel pathological mechanism by which G. vaginalis can mediate BV. However, there are limitations in the present study. Only the impact of G. vaginalis on the activation of the canonical inflammasome was examined. In further experiments, the effects of G. vaginalis on the activation status of non-canonical inflammasomes in macrophages and THP-1 cells should be assessed.
In conclusion, the present study demonstrated that G. vaginalis can induce BV by promoting NLRP3 inflammasome-mediated pyroptosis. The findings of the present study may provide a promising therapeutic direction for BV.
Acknowledgements
Not applicable.
Funding Statement
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
NX made substantial contributions to conception and design. NX, TY and TC prepared the experimental materials, performed the experiments, interpreted and analyzed the data, and performed statistical analysis. TC revised and approved the final version of the manuscript. NX, TY and TC confirmed the authenticity of all the raw data. All authors read and approved the manuscript and agree to be accountable for all aspects of the work in ensuring that the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics approval and consent to participate
The present study was approved by the Committee of Ethical Animal Care and Use of Laboratory Animals of Shandong Provincial Third Hospital (approval no. DWKYLL-2020001).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Joo HM, Hyun YJ, Myoung KS, Ahn YT, Lee JH, Huh CS, Han MJ, Kim DH. Lactobacillus johnsonii HY7042 ameliorates Gardnerella vaginalis-induced vaginosis by killing Gardnerella vaginalis and inhibiting NF-κB activation. Int Immunopharmacol. 2011;11:1758–1765. doi: 10.1016/j.intimp.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 2.Hawes SE, Hillier SL, Benedetti J, Stevens CE, Koutsky LA, Wolner-Hanssen P, Holmes KK. Hydrogen peroxide-producing lactobacilli and acquisition of vaginal infections. J Infect Dis. 1996;174:1058–1063. doi: 10.1093/infdis/174.5.1058. [DOI] [PubMed] [Google Scholar]
- 3.Ravel J, Gajer P, Abdo Z, Schneider GM, Koenig SS, McCulle SL, Karlebach S, Gorle R, Russell J, Tacket CO, et al. Vaginal microbiome of reproductive-age women. Proc Natl Acad Sci USA. 2011;108 (Suppl 1):S4680–S4687. doi: 10.1073/pnas.1002611107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pybus V, Onderdonk AB. Microbial interactions in the vaginal ecosystem, with emphasis on the pathogenesis of bacterial vaginosis. Microb Infect. 1999;1:285–292. doi: 10.1016/s1286-4579(99)80024-0. [DOI] [PubMed] [Google Scholar]
- 5.Sobel JD. Bacterial vaginosis. Ann Rev Med. 2000;51:349–356. doi: 10.1146/annurev.med.51.1.349. [DOI] [PubMed] [Google Scholar]
- 6.Mendling W. Vaginal microbiota. Adv Exp Med Biol. 2016;902:83–93. doi: 10.1007/978-3-319-31248-4_6. [DOI] [PubMed] [Google Scholar]
- 7.Sobel JD. Vaginal infections in adult women. Med Clin North Am. 1990;74:1573–1602. doi: 10.1016/s0025-7125(16)30496-5. [DOI] [PubMed] [Google Scholar]
- 8.Gergova RT, Strateva TV, Mitov IG. Gardnerella vaginalis-associated bacterial vaginosis in Bulgarian women. Braz J Infect Dis. 2013;17:313–318. doi: 10.1016/j.bjid.2012.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Broz P. Inflammasomes: Intracellular detection of extracellular bacteria. Cell research. 2016;26:859–860. doi: 10.1038/cr.2016.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Broz P, Dixit VM. Inflammasomes: Mechanism of assembly, regulation and signalling. Nat Rev Immunol. 2016;16:407–420. doi: 10.1038/nri.2016.58. [DOI] [PubMed] [Google Scholar]
- 11.Tang T, Lang X, Xu C, Wang X, Gong T, Yang Y, Cui J, Bai L, Wang J, Jiang W, Zhou R. CLICs-dependent chloride efflux is an essential and proximal upstream event for NLRP3 inflammasome activation. Nat Commun. 2017;8(202) doi: 10.1038/s41467-017-00227-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schroder K, Tschopp J. The inflammasomes. Cell. 2010;140:821–832. doi: 10.1016/j.cell.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 13.Latz E. The inflammasomes: Mechanisms of activation and function. Curr Opin Immunol. 2010;22:28–33. doi: 10.1016/j.coi.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vick EJ, Park HS, Huff KA, Brooks KM, Farone AL, Farone MB. Gardnerella vaginalis triggers NLRP3 inflammasome recruitment in THP-1 monocytes. J Reprod Immunol. 2014;106:67–75. doi: 10.1016/j.jri.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 15.Schleicher U, Bogdan C. Generation, culture and flow-cytometric characterization of primary mouse macrophages. Methods Mol Biol. 2009;531:203–224. doi: 10.1007/978-1-59745-396-7_14. [DOI] [PubMed] [Google Scholar]
- 16.Jang SE, Jeong JJ, Choi SY, Kim H, Han MJ, Kim DH. Lactobacillus rhamnosus HN001 and Lactobacillus acidophilus La-14 attenuate Gardnerella vaginalis-infected bacterial vaginosis in mice. Nutrients. 2017;9(531) doi: 10.3390/nu9060531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 18.Geng Y, Ma Q, Liu YN, Peng N, Yuan FF, Li XG, Li M, Wu YS, Li BL, Song WB, et al. Heatstroke induces liver injury via IL-1β and HMGB1-induced pyroptosis. J Hepatol. 2015;63:622–633. doi: 10.1016/j.jhep.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 19.Zhou R, Yazdi AS, Menu P, Tschopp J. A role for mitochondria in NLRP3 inflammasome activation. Nature. 2011;469:221–225. doi: 10.1038/nature09663. [DOI] [PubMed] [Google Scholar]
- 20.Muzny CA, Łaniewski P, Schwebke JR, Herbst-Kralovetz MM. Host-vaginal microbiota interactions in the pathogenesis of bacterial vaginosis. Curr Opin Infect Dis. 2020;33:59–65. doi: 10.1097/QCO.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McDuffie RS Jr, Kunze M, Barr J, Wolf D, Sze CI, Shikes R, Sherman M, Gibbs RS. Chronic intrauterine and fetal infection with Gardnerella vaginalis. Am J Obstet Gynecol. 2002;187:1263–1266. doi: 10.1067/mob.2002.127129. [DOI] [PubMed] [Google Scholar]
- 22.Hashemi FB, Ghassemi M, Roebuck KA, Spear GT. Activation of human immunodeficiency virus type 1 expression by Gardnerella vaginalis. J Infect Dis. 1999;179:924–930. doi: 10.1086/314674. [DOI] [PubMed] [Google Scholar]
- 23.Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64:1–137. Centers for Disease Control and Prevention. [PMC free article] [PubMed] [Google Scholar]
- 24.Hedges SR, Barrientes F, Desmond RA, Schwebke JR. Local and systemic cytokine levels in relation to changes in vaginal flora. J Infect Dis. 2006;193:556–562. doi: 10.1086/499824. [DOI] [PubMed] [Google Scholar]
- 25.Zariffard MR, Novak RM, Lurain N, Sha BE, Graham P, Spear GT. Induction of tumor necrosis factor- alpha secretion and toll-like receptor 2 and 4 mRNA expression by genital mucosal fluids from women with bacterial vaginosis. J Infect Dis. 2005;191:1913–1921. doi: 10.1086/429922. [DOI] [PubMed] [Google Scholar]
- 26.Gilbert NM, Lewis WG, Li G, Sojka DK, Lubin JB, Lewis AL. Gardnerella vaginalis and prevotella bivia trigger distinct and overlapping phenotypes in a mouse model of bacterial vaginosis. J Infect Dis. 2019;220:1099–1108. doi: 10.1093/infdis/jiy704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim DE, Kim JK, Han SK, Jang SE, Han MJ, Kim DH. Lactobacillus plantarum NK3 and Bifidobacterium longum NK49 alleviate bacterial vaginosis and osteoporosis in mice by suppressing NF-κB-linked TNF-α expression. J Med Food. 2019;22:1022–1031. doi: 10.1089/jmf.2019.4419. [DOI] [PubMed] [Google Scholar]
- 28.Łaniewski P, Gomez A, Hire G, So M, Herbst-Kralovetz MM. Human three-dimensional endometrial epithelial cell model to study host interactions with vaginal bacteria and Neisseria gonorrhoeae. Infect Immun. 2017;85:e01049–16. doi: 10.1128/IAI.01049-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shen R, Richter HE, Clements RH, Novak L, Huff K, Bimczok D, Sankaran-Walters S, Dandekar S, Clapham PR, Smythies LE, Smith PD. Macrophages in vaginal but not intestinal mucosa are monocyte-like and permissive to human immunodeficiency virus type 1 infection. J Virol. 2009;83:3258–3267. doi: 10.1128/JVI.01796-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anahtar MN, Byrne EH, Doherty KE, Bowman BA, Yamamoto HS, Soumillon M, Padavattan N, Ismail N, Moodley A, Sabatini ME, et al. Cervicovaginal bacteria are a major modulator of host inflammatory responses in the female genital tract. Immunity. 2015;42:965–976. doi: 10.1016/j.immuni.2015.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li C, Wang X, Kuang M, Li L, Wang Y, Yang F, Wang G. UFL1 modulates NLRP3 inflammasome activation and protects against pyroptosis in LPS-stimulated bovine mammary epithelial cells. Mol Immunol. 2019;112:1–9. doi: 10.1016/j.molimm.2019.04.023. [DOI] [PubMed] [Google Scholar]
- 32.Man SM, Karki R, Kanneganti TD. Molecular mechanisms and functions of pyroptosis, inflammatory caspases and inflammasomes in infectious diseases. Immunol Rev. 2017;277:61–75. doi: 10.1111/imr.12534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qiu Z, He Y, Ming H, Lei S, Leng Y, Xia ZY. Lipopolysaccharide (LPS) aggravates high glucose- and hypoxia/reoxygenation-induced injury through activating ROS-dependent NLRP3 inflammasome-mediated pyroptosis in H9C2 cardiomyocytes. J Diabetes Res. 2019;2019(8151836) doi: 10.1155/2019/8151836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Danelishvili L, Bermudez LE. Analysis of pyroptosis in bacterial infection. Methods Mol Biol. 2013;1004:67–73. doi: 10.1007/978-1-62703-383-1_6. [DOI] [PubMed] [Google Scholar]
- 35.Franchi L, Eigenbrod T, Muñoz-Planillo R, Nuñez G. The inflammasome: A caspase-1-activation platform that regulates immune responses and disease pathogenesis. Nat Immunol. 2009;10:241–247. doi: 10.1038/ni.1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tschopp J, Schroder K. NLRP3 inflammasome activation: The convergence of multiple signalling pathways on ROS production? Nat Rev Immunol. 2010;10:210–215. doi: 10.1038/nri2725. [DOI] [PubMed] [Google Scholar]
- 37.Miao EA, Leaf IA, Treuting PM, Mao DP, Dors M, Sarkar A, Warren SE, Wewers MD, Aderem A. Caspase-1-induced pyroptosis is an innate immune effector mechanism against intracellular bacteria. Nat Immunol. 2010;11:1136–1142. doi: 10.1038/ni.1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sagulenko V, Thygesen SJ, Sester DP, Idris A, Cridland JA, Vajjhala PR, Roberts TL, Schroder K, Vince JE, Hill JM, et al. AIM2 and NLRP3 inflammasomes activate both apoptotic and pyroptotic death pathways via ASC. Cell Death Differ. 2013;20:1149–1160. doi: 10.1038/cdd.2013.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Strowig T, Henao-Mejia J, Elinav E, Flavell R. Inflammasomes in health and disease. Nature. 2012;481:278–286. doi: 10.1038/nature10759. [DOI] [PubMed] [Google Scholar]
- 40.Zhao LR, Xing RL, Wang PM, Zhang NS, Yin SJ, Li XC, Zhang L. NLRP1 and NLRP3 inflammasomes mediate LPS/ATP-induced pyroptosis in knee osteoarthritis. Mol Med Rep. 2018;17:5463–5469. doi: 10.3892/mmr.2018.8520. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.