Synopsis
With improvement in cure of childhood cancer came the responsibility to investigate the long-term morbidity and mortality associated with the treatments accountable for this increase in survival. Several large cohorts of childhood cancer survivors have been established throughout Europe and North America to facilitate research on long-term complications of cancer treatment. The cohorts have made significant contributions to the understanding of early mortality, somatic late complications and psychosocial outcomes among childhood cancer survivors, which has been translated into the design of new treatment protocols for pediatric cancers, with the goal to reduce the potential risk and severity of late effects. Furthermore, they have been instrumental in the formulation of specific follow-up recommendations for survivors. As treatment modalities are consecutively modified over time, continuing studies to assess late effects of more recent treatment regimens are an ongoing priority.
Keywords: Childhood cancer survivors, survivor cohorts, cancer research, late effects, long-term complications
Introduction
With improvement in cure has come the responsibility to investigate the long-term morbidity and mortality associated with the treatment modalities leading to this increase in survival1,2. Treatment-related effects on normal growth and development, neuropsychological functioning and reproductive capacity are some of the main concerns raised by parents and by patients themselves3. These concerns were already expressed more than 40 years ago by Dr. Giulio J. D’Angio:“It is clear that the child cured of cancer must be followed for life, not so much because late recurrence of disease is feared as to permit detection of the delayed consequences of radio- and chemotherapy. Careful studies of these late effects must be conducted”4.
To facilitate research on health later in life, several large cohorts of childhood cancer survivors have been established throughout Europe and North America in recent decades5,6. These cohorts have facilitated a vast amount of research on late effects and continue to provide the basis for investigating many different health-related aspects of cancer and cancer treatment at a young age. Some of the pioneering research of late effects after childhood cancer were the studies from the Late Effects Study Group (LESG) which was initiated in the early 1970s7. These studies, investigating the risk of second malignant neoplasms (SMN), and the role of first primary tumor type, genetic predisposition and radiotherapy treatment, demonstrated the value and need of establishing large and well-designed cohorts of childhood cancer survivors7–9.
In 2001, the Journal of Clinical Oncology published two landmark studies on subsequent mortality and its causes in childhood cancer survivors – a Scandinavian population-based study10 and an American hospital-based study11. Both studies showed that 5-year survivors had a 10.8-fold increased mortality rate, but while modern treatments had reduced mortality from the primary cancer, there was an increased rate of long-term treatment-related deaths. These studies provided an important resource for understanding risk factors associated with increased mortality and morbidity. They also allowed the identification of treatment modifications that could reduce the noted treatment-related consequences for future childhood cancer patients10,11. Years later, in 2016 and 2018, two studies from the North American Childhood Cancer Survivor Study (CCSS) confirmed that adjusted treatment regimens designed to reduce the potential risk and severity of late effects have indeed led to fewer late effects as well as better survival rates12–14.
When cure is no longer the only goal, multidisciplinary and international collaborative studies must be designed to improve the outcomes for this large and steadily growing cohort of long-term survivors of childhood cancer. It is, however, a challenge to develop strategies for the long-term follow-up of survivors addressing their needs15. Early efforts to describe late effects were largely conducted through single-institution and smaller consortia studies. However, by the mid-1980s, it became increasingly clear that these approaches had inherent limitations, including small sample size, incompletely characterized populations, and limited length of follow-up. Consequently, over the past 25 years several cohorts of childhood cancer survivors have been established across Europe and North America. In this article, we provide an overview of these cohorts and point out some of their most significant contributions to the area of late effects. Characteristics of the childhood cancer survivor cohorts are presented in Table 1.
Table 1A.
Characteristics of North American childhood cancer survivor cohorts
| Characteristics | CCSS | SJLIFE | CAYACS |
|---|---|---|---|
| Country or province | USA and Canada | USA | British Columbia, Canada |
| Year of establishment | 1994 | 2007 | 2005 |
| Period of cancer diagnosis | 1970–1999 | 1962–2012 | 1970–2010 |
| Cohort size | 37,593 (25,664 active participants) | 8,245 (6,004 active participants) | 8,735 |
| Survival at entry | ≥5 years | ≥5 years | 0 years |
| Age at cancer diagnosis (years) | 0–20 | 0–24 | 0–24 |
| Type of cancer | Leukemia, CNS, Hodgkin’s lymphoma, non-Hodgkin’s lymphoma, neuroblastoma, soft tissue sarcoma, Wilms, bone tumors | All types | All types |
| Study design | Hospital-based retrospective cohort with prospective follow-up | Hospital-based retrospective cohort with prospective follow-up | Retrospective population-based cohort with prospective follow-up |
| Obtained information | Surveys, medical records | Clinical assessments, surveys, medical records | Registries, administrative databases, medical records |
| Comparison population | Siblings, general population | Frequency matched community controls, general population | Random sample from the general population of British Columbia |
| Therapeutic exposures | Yes (>90%) | Yes (100%) | Yes |
| Collection of germline DNA | For some (<60%) | Yes (>95%) | NA |
Childhood cancer survivor cohorts in Europe and North America
The North American Childhood Cancer Survivor Study (CCSS)
The CCSS was the first large childhood cancer survivor cohort to be initiated and was funded by the USA’s National Cancer Institute in 19946. The CCSS is a unique resource because of its large size combined with comprehensive data and banked biologic samples, thus overcoming some of the limitations from earlier studies. CCSS originally included more than 20,000 five-year survivors diagnosed from 1970–1986 before age 21 years and treated at 26 clinical centers in the United States and Canada16. Subsequently, the cohort was expanded to include 37,593 eligible survivors diagnosed through 1999 with 25,664 participating17. More than 370 peer-reviewed publications investigating various aspects of pediatric cancer and its treatment on later health have been carried out within the CCSS cohort16.
One of the early significant contributions of the CCSS was published in 200118. CCSS investigators noted a modest increased frequency of SMN in survivors even for the subgroups of survivors carrying the greatest risks. However, given the trajectory of the cumulative incidence curve, with no evidence of plateau, survivors were at increased risk for SMNs across their lifespan. A subsequent CCSS study, published in 2006, showed that almost three fourths of childhood cancer survivors treated in the 1970s and 1980s had a chronic health condition with more than 40% having serious health problems19. The incidence of health conditions increased with time, emphasizing the need for ongoing close monitoring of survivors as an important part of their overall health care19. Lastly, a study published in 2016 confirmed that more recent pediatric cancer treatment regimens designed to reduce the potential risk and severity of late effects, in fact do so. Thus, along with increased promotion of approaches for early detection and improvements in medical care for late effects, this study presented quantitative evidence that the strategy of lowering therapeutic exposures has contributed to extending the lifespan for many survivors of childhood cancer12.
St. Jude Lifetime Cohort Study (SJLIFE)
The St. Jude Children’s Research Hospital initiated the SJLIFE in 2007, with the aim of establishing a lifetime cohort of survivors to perform prospective medical assessment of health outcomes. The SJLIFE study is a retrospective cohort design with prospective clinical follow-up and ongoing accrual of five-year survivors of all childhood cancers diagnosed and treated at St. Jude Children’s Research Hospital since its opening in 196220. As of March 2020, over 6000 survivors have been enrolled into the SJLIFE cohort as well as 735 age-, sex-and race-matched controls. This unique cohort, funded by St. Jude and a grant from the US National Cancer Institute, has published over 120 peer-reviewed manuscripts, describing various aspects of the long-term consequences experienced by cohort participants.
In 2013, SJLIFE investigators estimated that at age 45 years, the cumulative prevalence of any chronic health condition was 95.5% and 80.5% for a serious/disabling or life-threatening chronic condition21. This publication also detailed the yield from conducting risk-based screening. A few years after, in 2017, a subsequent study demonstrated that by age 50 years, a survivor would experience, on average, 17.1 chronic health conditions of any grade, of which 4.7 were severe/disabling, life-threatening or fatal22. Lastly, using whole genome sequencing of 3,006 survivors, SJLIFE investigators assessed the prevalence of pathogenic/likely pathogenic mutations in 60 cancer predisposition genes with autosomal dominant inheritance and moderate to high penetrance and evaluated the association with risk of subsequent neoplasms23. Mutations were identified in 5.8% of survivors and were associated with significantly increased rates of subsequent breast cancer and sarcoma among irradiated survivors and with increased rates of developing any subsequent neoplasm among non-irradiated survivors. These findings support referral of all survivors for genetic counseling with potential clinical genetic testing.
The Childhood, Adolescent, and Young Adult Cancer Survivors Research Program (CAYACS)
A multidisciplinary research team in British Columbia (BC), Canada, initiated the first steps towards the establishment of the CAYACS research program with the overall aim to study late effects and healthcare outcomes in childhood cancer survivors by linking different data sources in BC24. The initial study was funded by the Canadian Institutes for Health Research from 2001–2004 and utilized the benefits of population files with complete follow-up and data linkage to reduce the risk of misclassification of cancer patients and outcomes. This work formed the basis for the CAYACS research program, funded by the Canadian Cancer Society Research Institute from 2005–2015, which so far has resulted in 20 peer-reviewed studies. The cohort includes all residents in BC diagnosed with cancer from 1970–2010 before 25 years of age and examines health, education, and income outcomes with appropriate population-based control groups.
Based on CAYACS, the risk for hospitalization-related late morbidity was found to be highest in survivors of leukemia, CNS tumors, bone and soft tissue sarcomas, and kidney cancer. Importantly, hospitalizations due to other diseases than cancer became more prevalent over time25. Significant findings from CAYACS have also brought awareness of the late complications in survivors among stakeholders. The results from a comprehensive study showing lower educational attainment among childhood cancer survivors26 were disseminated to system funders and policy-makers (BC Ministry of Education), program managers, and teachers to act on the educational challenges in the survivors. The CAYACS has also been a leading resource to estimate the healthcare costs for childhood cancer patients, useful for evidence-informed policy development and healthcare delivery of follow-up and management27.
The British Childhood Cancer Survivor Study (BCCSS)
Studies from the early 1990s reporting an increased risk of secondary cancers28,29 and causes of increased late mortality in childhood cancer survivors30 led to the establishment of the BCCSS. The aim of the BCCSS was to obtain estimates of the risk for selected adverse health and social outcomes occurring among survivors and their offspring and to investigate variation of such risks in relation to different risk factors, including type of childhood cancer and its treatment31. Hence, the BCCSS was established in 199831 including almost 18,000 five-year survivors of all types of childhood cancer diagnosed before age 15 years in England, Wales and Scotland. To date more than 70 peer-reviewed studies have been published based on BCCSS data.
Some of the most significant contributions achieved through the BCCSS cohort to date were the results from a study published in 2010, reporting that second cancers and cardiovascular outcomes accounted for 50% and 25% of the excess number of deaths in adult survivors of childhood cancer32. This important information allowed for developing strategies to decrease early mortality. The year after, a study reported that the majority of the excess second cancers observed among long-term survivors were also the common cancers in the general population and that abdominal irradiation was associated with a similar risk of bowel cancer to that experienced by individuals with two affected first-degree relatives33. Lastly, a study from 2017 provided a risk stratification tool for specific causes of death, SMNs and non-fatal non-neoplastic outcomes for childhood cancer survivors. These data were used in a new Service Specification by the National Health Service (NHS) England concerning the clinical follow-up of survivors throughout England34.
Adult Life after Childhood Cancer in Scandinavia (ALiCCS)
In the early 1990s and 2000s Nordic, population-based studies on SMNs and late mortality in childhood cancer survivors were published10,35,36. The risk estimates from these studies were lower than those previously reported in most hospital-based studies, emphasizing the necessity of conducting large, population-based studies. Further, the early studies of late effects were mainly conducted in US populations7–9. In order to determine whether the US findings were applicable elsewhere, other countries initiated their own programs. This led to the population-based Nordic ALiCCS research program37 initiated in 2010 comprising 33,160 1-year survivors of all childhood cancers diagnosed between 1943–2008 in Denmark, Finland, Iceland, Norway and Sweden. Due to the size and age of the survivor cohort as well as the meticulous registration in the Nordic registries, the ALiCCS program enables studies of specific cancer types and rare medical disorders in both adulthood and senescence. To date over 20 peer-reviewed studies have been published.
One of the first ALiCCS studies provided an exhaustive endocrine risk profile of childhood cancer survivors treated in northern Europe. At age 60 years, survivors had a cumulative risk of more than 40% for endocrine disorders requiring a hospital contact38. Another study, linking long-term neuroblastoma survivors with patient and clinical registries, illustrated the high risk of late effects, particularly among survivors of high-risk neuroblastoma, who are some of the most intensively treated patients within pediatric oncology and for whom very little is known about later adverse health outcomes39. Recently, it was shown that 5-year survivors of a CNS tumor had an increased risk of nervous system diseases. Due to a complete hospital history for each survivor, both before and after diagnosis, it was possible to show that the risk of epilepsy was highly increased several years before the cancer diagnosis, emphasizing the importance of following children with epilepsy for CNS tumors.
Swiss Childhood Cancer Survivor Study (SCCSS)
The SCCSS is a nationwide population-based cohort study established in 2007 including 5,737 5-year survivors of childhood cancer diagnosed between 1976–2018 with ongoing enrollment of study participants. The aim of this collaborative is to evaluate long-term consequences of childhood cancer, with a special focus on the incidence of late effects, risk factors for late effects, health care use and medical follow-up, as well as health-related behaviors and their determinants. Before the official establishment of the SCCSS a first multicenter hospital-based study was conducted in 1992–1994 in which detailed information on somatic, psychosocial and socio-economic outcomes in survivors was collected. Since 2007, regular national questionnaire surveys, supplemented by nested hospital-based studies, have been conducted on a national level40. To date more than 170 peer-reviewed studies have been published based on SCCSS data.
The population-based approach with detailed clinical information and questionnaire data enables studies elucidating many different aspects of late complications. In the SCCSS, pulmonary diseases, particularly pneumonia and chest wall abnormalities, were reported to be up to four to six times more common in survivors than in siblings41, indicating that long-term monitoring is required to give insight into the progression of lung disease, risk factors and potential prevention. Another study reported that the prevalence of self-reported hearing loss among survivors was high (10%), especially after a CNS tumor (25%). The burden of hearing loss was stabilized in survivors treated more recently, suggesting a positive impact of new treatment regimens with less ototoxic radiation and more carefully dosed platinum compounds42. The majority of survivors reported low levels of psychological distress – though, one fourth of survivors still reported distress to a degree that makes closer observation and potentially counseling worthwhile43.
The French Childhood Cancer Survivor Study (FCCSS)
The basis for the FCCSS started with two single-center studies of 634 five-year survivors treated for solid tumors in childhood at Gustave Roussy in Paris between 1942–1969. One study reported the long-term risk for SMNs44 and the other assessed the role of chemotherapy and radiation dose and site on this risk45. The results revealed that the relative risk of SMN was highly increased in survivors treated with both radiation and chemotherapy. These early findings led to an expansion of the cohort including several treatment centers in France as well as three centers from Great Britain to study the risk of different late complications in 4,122 five-year survivors in the Euro2K cohort, including cardiac disease46 and diabetes47. In 2015, the FCCSS combined the 3,172 French survivors from the Euro2K treated between 1942–1985 and 4,498 survivors treated between 1985–2000 at the Gustave Roussy and at the Curie Centre48. To date 68 peer-reviewed studies have been published based on FCCSS data.
The FCCSS has contributed important knowledge on different late complications due to the very detailed level of treatment information. One study reported on the association between radiation dose to the tail of the pancreas as part of the cancer treatment and diabetes as a late complication47 whereas another study demonstrated that both anthracyclines and heart radiation doses were highly associated with cardiac disease - two important results with clinical implications for follow-up of childhood cancer survivors49.
The French Childhood Cancer Survivor Study for Leukaemia (LEA Cohort)
The LEA cohort is a French multicenter follow-up program exclusively including children treated for acute leukemia since 1980. LEA was initiated in 2004 with the aim to study the medical, socioeconomic, behavioral and environmental determinants of health outcomes in patients treated for childhood acute leukemia. The 5,160 patients included were treated at 17 pediatric hematology and oncology centers throughout France, covering approximately 80% of all French children diagnosed with acute leukemia50. Until now, 31 studies have been published based on data from the LEA cohort.
The combination of clinical and therapeutic information retrieved from medical records, physical and laboratory examinations, and questionnaire data makes LEA an important source for studying a wide range of late complications in childhood acute leukemia survivors. One study reported an increased risk for reduced femoral bone mineral density among adult survivors with gonadal deficiency who received hematopoietic stem cell transplantation, which might increase their risk for fractures later in life51. Another study disclosed a higher risk for metabolic syndrome among survivors, independent of the treatment received suggesting that early detection, followed by changes in lifestyle, might prevent cardiovascular events among survivors52. Finally, a study of late cardiomyopathy in 185 survivors of acute myeloid leukemia revealed that the development of late cardiomyopathy is associated with previous history of relapse and cumulative dose of anthracyclines53.
Dutch Childhood Cancer Survivorship LATER Cohort Study (LATER Study)
Since 2006, the LATER study group, a collaboration between healthcare providers, researchers, survivors and the Dutch Childhood Oncology Group (DCOG) has been establishing the Dutch Childhood Cancer Survivorship LATER Cohort Study. The aims of the LATER Study are to determine the risk and severity of therapy-related health problems in childhood cancer survivors and to gain insight into genetic and personal risk factors for health problems. Furthermore, the LATER study aims to identify diagnostic tests to detect and treat late effects at an early stage and to understand which possible interventions can improve the quality of life in survivors. For the first part of the LATER study, data were collected from questionnaires and linkage studies for more than 6000 survivors alive 5 years after diagnosis and diagnosed between 1965–2001 and their siblings. For the LATER part 2 study data from a visit to the outpatient clinic between 2016 and 2020 of nearly 2500 survivors and 750 siblings were collected. The unique combination of information from medical records, questionnaires, clinical examinations and clinical material enables the LATER Study to generate new knowledge for improving the care of childhood cancer patients and survivors. To date more than 30 papers have been published based on the LATER Study cohort.
A study on subsequent breast cancer, sarcoma and solid cancers, following treatment with different chemotherapeutical agents, suggested that doxorubicin exposure increased the risk of all solid cancers and breast cancer, whereas exposure to cyclophosphamide increased the risk of sarcomas. These results may be used to adjust future treatment protocols for childhood cancer patients and for setting up surveillance guidelines for survivors54. Another important LATER study underscored the crucial role of primary care physicians in the care of childhood cancer survivors. The study pointed to the need for collaboration across care professions and the importance of having a care plan for every survivor that can be used by different health care providers55. Lastly, in a collaborative study combining data from three survivorship cohorts - the LATER Study, SJLIFE and CCSS - the risk of late-onset cardiomyopathy in childhood cancer survivors was examined. The study revealed, that daunorubicin was associated with decreased risk for cardiomyopathy compared with doxorubicin, whereas epirubicin was approximately isoequivalent. The current hematologic-based doxorubicin dose equivalency of mitoxantrone (4:1), however, appeared to underestimate the association of mitoxantrone with long-term risk of cardiomyopathy56.
The Italian Study on off-therapy Childhood Cancer Survivors (OTR)
The OTR was established in 1980 as a multi-institutional register of off therapy pediatric patients treated at one of the institutions of the Italian Association of Pediatric Hematology and Oncology (AIEOP). The main purpose of the OTR was to improve the understanding of the clinical need for long-term follow-up of childhood cancer survivors. In 1989, AIEOP started a cancer register, where all children with cancer were included since diagnosis. Through linkage with the cancer register, the OTR has identified off therapy patients since 199657.
The OTR is an important resource for studying childhood cancer survivors from Southern Europe. So far, seven studies of late complications based on the OTR have been published. The late mortality among five-year survivors compared to the general Italian population has been described, providing insight into the specific causes of death among Italian childhood cancer survivors58. The OTR group initiated an international consensus paper together with the International Berlin-Frankfurt-Munster Early and Late Toxicity Educational Committee to generate a statement of cure and care for survivors of childhood cancer59. This important document became the basis for the European PanCare Foundation established in 2008.
European consortia
The aim of the PanCare network (www.pancare.eu) established in 2008 as a multidisciplinary European network of professionals, survivors and their families is to reduce the frequency, severity and impact of late effects of cancer treatment in children and adolescents with cancer as well as to ensure optimal long-term care60. PanCare is presently the backbone of late effect studies in Europe. Within Europe, complementing the large-scale cohort studies using population-based registries, are the well-established hospital-based cohort studies, which benefit from detailed information on individual patients rarely available to population-based cohort studies such as treatment information and outcomes of clinical tests.
In recent years, great strides have been taken to coordinate efforts to exploit these advantages in the European context through the establishment of three EU-funded collaborative research projects by investigators from several European countries, i.e. PanCareSurFup focusing on cardiac disease, subsequent primary neoplasms and late mortality in survivors as well as development of guidelines to improve lives for survivors (www.pancaresurfup.eu)61, PanCareLIFE focusing on female infertility, cisplatin-induced ototoxicity, and quality of life (www.pancarelife.eu), and PanCareFollowUp aiming at setting up state-of-the-art late effect clinics based on international guidelines for surveillance of late effects and a new innovative model for integrated care for survivors (www.pancarefollowup). These large consortia have several advantages including very large cohort studies combining both register- and hospital-based data with data from surveys, clinical case-control studies with detailed treatment information and dosimetry evaluation, as well as genetic evaluations.
A recent study from the PanCareSurFup consortium reported a four-fold increased risk of developing subsequent primary leukaemia in childhood cancer survivors, which remained significantly elevated beyond 20 years from first primary malignancy61. Further, two sister studies provided new insight into the risk of SMNs, demonstrating a 22-fold increased risk of subsequent soft-tissue sarcomas62 and a 30-fold increased risk for bone cancers when compared to population norms63. A study from PanCareLIFE64 investigating genetic variation of cisplatin-induced ototoxicity in pediatric patients confirmed the previously observed association between cumulative dose of cisplatin and risk of ototoxicity and found an association between the single nucleotide polymorphisms ACYP2 rs1872328 and SLC22A2 rs316019 and ototoxicity in a meta-analysis. Further, an intervention study successfully raised the level of fertility preservation knowledge in parents of older patients as well as parents with higher educational levels and further improved patient and parent empowerment65.
Discussion
The responsibility to investigate the long-term morbidity and mortality that came along with the treatment modalities leading to the improvements in cure has led to the establishment of an impressive number of childhood cancer survivor cohorts throughout Europe and North America. These cohorts, complement each other with their different designs and methodology and have facilitated a vast amount of research on a wide spectrum of long-term adverse health consequences of the life-saving cancer treatments2. Published findings on late effects have led to a more thorough understanding of the lifelong, often very complex and serious disease pattern that childhood cancer survivors encounter after finishing treatment. These findings all stress that survivors need tailored follow-up care to identify health problems after treatment at an early stage.
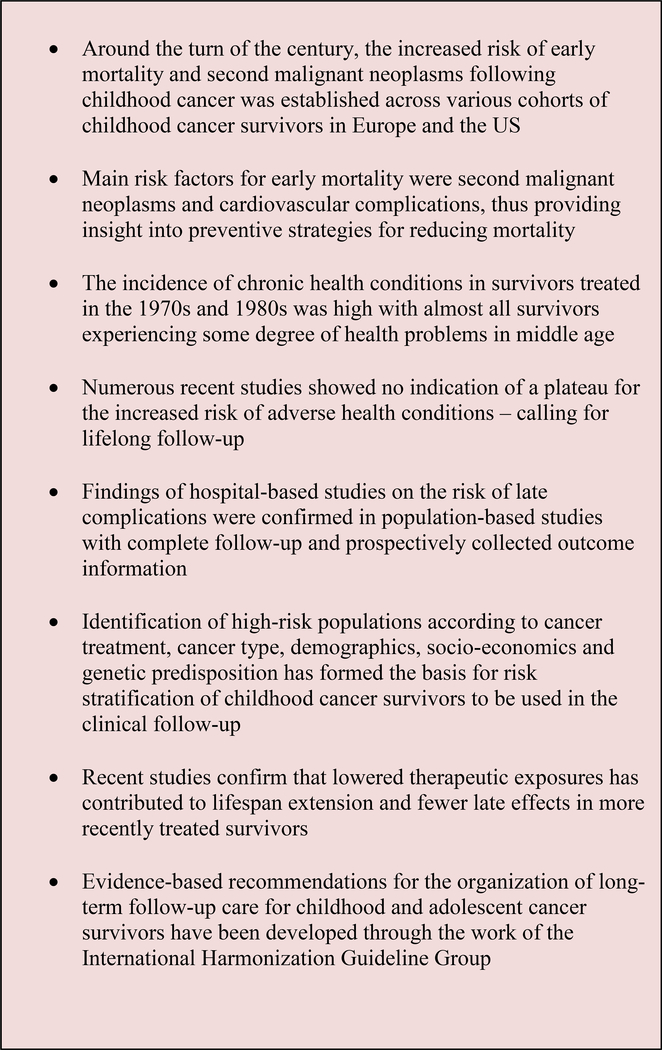
In this article, we provided an overview of childhood cancer survivor cohorts across Europe and North America that have emerged since the mid-1990s, including the historic background for the establishment of these cohorts as well as some of the most significant contributions to the research area of late effects. A summarization of these contributions is presented in Figure 1. Implementing follow-up care for childhood cancer survivors has proven challenging across the globe. Findings from a recent survey, providing the current state of survivorship care in 18 countries across five continents, indicated that a large proportion of pediatric-age survivors were seen by a physician being familiar with late effects, whereas far fewer survivors had access to an expert after transition to adulthood, stressing that long-term follow-up is still only available for a small proportion of children diagnosed with cancer15,66.
Figure 1.
Summarization of findings with significant clinical implications for the treatment and/or follow-up of childhood cancer patients
Lack of harmonized evidence-based guidelines might partly explain why survivors do not receive optimum care. Thus, in 2010, a worldwide collaboration to harmonize guidelines for long-term follow-up of childhood and young adult cancer survivors was initiated, the International Harmonization Guideline Group (IGHG), providing uniform surveillance guidelines in collaboration with PanCare based on a large expert panel (www.ighg.org)67,68. Another reason is the challenge of providing comprehensive, risk-based survivorship care.
These issues will be addressed by PanCareFollowUp, a third EU-funded consortium initiated in 2019. With the aim of improving follow-up care for adult survivors of childhood cancer, a new intervention will be developed – the PanCareFollowUp Care, a person-centered approach to survivorship care based on international clinical guidelines for surveillance of late effects empowering survivors to play an active role in their own health management. Setting up state-of-the-art late effect clinics in four European countries, Belgium, Czech Republic, Italy and Sweden, the impact of this Care intervention will be assessed in terms of effectiveness measured as quality of life, physical and psychosocial outcomes, value, cost-effectiveness, acceptability and feasibility (www.pancarefollowup.eu).
Despite the wealth of information published about adverse outcomes in childhood cancer survivors, our current understanding of several important areas of long-term health is still limited. To address knowledge deficits in childhood cancer survivors, longitudinal systematic medical assessment is needed in order to elucidate the pathophysiology of cancer treatment-related morbidity, identification of biomarkers of subclinical organ dysfunction, and characterization of high-risk groups who may benefit from interventions to preserve health. Further, since late effects are by definition effects of treatments given in the past, future studies set up to detect treatment-induced adverse effects of contemporary drugs used to treat pediatric cancers are essential, as for example the potential adverse effects of immunotherapy used as part of some treatments today
The overall goal of ongoing and future collaborations based on these large and rich survivor cohorts is to provide every childhood cancer survivor with better care and long-term health for survivors to reach their full potential, and to the degree possible, enjoy the same quality of life and opportunities as their peers.
Table 1B.
Characteristics of European childhood cancer survivor cohorts
| Characteristics | BCCSS | ALiCCS | SCCSS | FCCSS | LEA | LATER Study | OTR |
|---|---|---|---|---|---|---|---|
| Country or region | England, Wales, Scotland | Denmark, Finland, Iceland, Norway, Sweden | Switzerland | Selected regions in France | France (the participating pediatric-oncology centers cover nearly 75% of all childhood acute leukemia survivors diagnosed since 1980) | Netherlands | Italy |
| Year of establishment | 1998 | 2010 | 2007 | 2015 | 2004 | 2006 | 1980 |
| Period of cancer diagnosis | 1940–1991 in original cohort; 1940–2006 in extended cohort | 1943–2012 | 1976–2018 (ongoing) | 1946–1999 | 1980–2019 (ongoing) | 1963–2002 | 1960–2004 |
| Cohort size | 17,981 in original cohort; 34,490 in extended cohort | 33,160 | 5,737 | 7,670 | 14,201 | 6,165 | 14,201 |
| Survival at entry | ≥5 years | ≥1 year | ≥5 years | ≥5 years | ≥2 years | ≥5 years | End of treatment |
| Age at cancer diagnosis (years) | 0–14 | 0–19 | 0–20 | 0–19 | 0–18 | 0–18 | 0–19 |
| Type of cancer | All types | All types | All types | All but leukemia | Leukemia | All types | All types |
| Study design | Retrospective population-based cohort study | Retrospective population-based cohort study | Retrospective population-based cohort study with prospective follow-up | Hospital-based retrospective cohort with prospective follow-up | Retrospective hospital- and local register-based cohort study with prospective follow-up | Hospital-based retrospective cohort study with prospective follow-up | Retrospective and prospective national hospital-based from AIEOP clinics with prospective follow-up |
| Obtained information | Registries, surveys, medical records | Nordic registries, medical records | Registries, surveys, medical records | National hospital and medical insurance databases, clinical visits, surveys | Registries,, clinical visits, surveys, medical records | Registries, clinical visits, surveys, medical records | Regional registries, hospital data |
| Comparison population | General population | Matched population comparisons | Siblings and population comparisons | From national statistics | Comparisons from a national database of health care | Siblings and matched population controls | Population data |
| Therapeutic exposures | Crude in main cohort; detailed in case-control studies | Detailed in case-cohort studies | Crude in main cohort, detailed in nested studies | Yes (<95%), including whole body dose reconstruction for radiotherapy | Crude in main cohort; detailed in case-control studies | Yes | Crude for all; detailed for a selected group (in survivorship passports) |
| Collection of germline DNA | NA | NA | Yes | Yes (60%) | NA | Yes (50%) | N/A |
Childhood cancer cohorts: CCSS (Childhood Cancer Survivor Study), SJLIFE (St. Jude Lifetime Cohort Study), CAYACS (Childhood, Adolescent, Young Adult Cancer Survivors), BCCSS (British Childhood Cancer Survivor Study), ALiCCS (Adult Life after Childhood Cancer in Scandinavia), SCCSS (Swiss Childhood Cancer Survivor Study), FCCSS (French Childhood Cancer Survivor Study), LEA (The French Childhood Cancer Survivor Study for Leukaemia), LATER Study (Dutch Childhood Cancer Survivorship LATER Cohort Study), OTR (The Italian Study on off-therapy Childhood Cancer Survivors)
Other abbreviations: AIEOP = Associazione Italiana di Ematologia e Oncologia Pediatrica; NA = not available; NDI = National Death Index
Key points:
Overview of childhood cancer survivor cohorts across Europe and North America including their historical background
Selected publications with significant clinical impact for the treatment and follow-up of childhood cancer patients within each childhood cancer survivor cohort
An up to date summarization of the contributions to the research from childhood cancer survivor cohorts in Europe and North America
Footnotes
Disclosure statement: The authors have nothing to disclose
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gatta G, Botta L, Rossi S, et al. Childhood cancer survival in Europe 1999–2007: results of EUROCARE-5--a population-based study. Lancet Oncol. 2014;15(1):35–47. [DOI] [PubMed] [Google Scholar]
- 2.Robison LL, Hudson MM. Survivors of childhood and adolescent cancer: life-long risks and responsibilities. Nat Rev Cancer. 2014;14(1):61–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wallace HGD. Introduction. In: Wallace HGD, ed. Late Effects of Childhood Cancer. 1 ed. New York: Oxford University Press; 2004:1–2. [Google Scholar]
- 4.D’Angio GJ. Pediatric cancer in perspective: cure is not enough. Cancer. 1975;35(3 suppl):866–870. [DOI] [PubMed] [Google Scholar]
- 5.Winther JF, Kenborg L, Byrne J, et al. Childhood cancer survivor cohorts in Europe. Acta Oncol. 2015;54(5):655–668. [DOI] [PubMed] [Google Scholar]
- 6.Robison LL, Mertens AC, Boice JD, et al. Study design and cohort characteristics of the Childhood Cancer Survivor Study: a multi-institutional collaborative project. Med Pediatr Oncol. 2002;38(4):229–239. [DOI] [PubMed] [Google Scholar]
- 7.Meadows AT, Baum E, Fossati-Bellani F, et al. Second malignant neoplasms in children: an update from the Late Effects Study Group. J Clin Oncol. 1985;3(4):532–538. [DOI] [PubMed] [Google Scholar]
- 8.Meadows AT, D’Angio GJ, Mike V, et al. Patterns of second malignant neoplasms in children. Cancer. 1977;40(4 Suppl):1903–1911. [DOI] [PubMed] [Google Scholar]
- 9.Mike V, Meadows AT, D’Angio GJ. Incidence of second malignant neoplasms in children: results of an international study. Lancet. 1982;2(8311):1326–1331. [DOI] [PubMed] [Google Scholar]
- 10.Moller TR, Garwicz S, Barlow L, et al. Decreasing late mortality among five-year survivors of cancer in childhood and adolescence: a population-based study in the Nordic countries. J Clin Oncol. 2001;19(13):3173–3181. [DOI] [PubMed] [Google Scholar]
- 11.Mertens AC, Yasui Y, Neglia JP, et al. Late mortality experience in five-year survivors of childhood and adolescent cancer: the Childhood Cancer Survivor Study. J Clin Oncol. 2001;19(13):3163–3172. [DOI] [PubMed] [Google Scholar]
- 12.Armstrong GT, Chen Y, Yasui Y, et al. Reduction in Late Mortality among 5-Year Survivors of Childhood Cancer. N Engl J Med. 2016;374(9):833–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gibson TM, Mostoufi-Moab S, Stratton KL, et al. Temporal patterns in the risk of chronic health conditions in survivors of childhood cancer diagnosed 1970–99: a report from the Childhood Cancer Survivor Study cohort. Lancet Oncol. 2018;19(12):1590–1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turcotte LM, Liu Q, Yasui Y, et al. Temporal Trends in Treatment and Subsequent Neoplasm Risk Among 5-Year Survivors of Childhood Cancer, 1970–2015. JAMA. 2017;317(8):814–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Winther JF, Kremer L. Long-term follow-up care needed for children surviving cancer: still a long way to go. Lancet Oncol. 2018;19(12):1546–1548. [DOI] [PubMed] [Google Scholar]
- 16.Robison LL, Armstrong GT, Boice JD, et al. The Childhood Cancer Survivor Study: a National Cancer Institute-supported resource for outcome and intervention research. J Clin Oncol. 2009;27(14):2308–2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.webpage CCSS. Demographic and cancer treatment of participants in the expansion, original and overall cohorts. https://ccss.stjude.org/content/dam/en_US/shared/ccss/documents/data/treatment-exposure-tables.pdf. Accessed 29/10-2019.
- 18.Neglia JP, Friedman DL, Yasui Y, et al. Second malignant neoplasms in five-year survivors of childhood cancer: childhood cancer survivor study. J Natl Cancer Inst. 2001;93(8):618–629. [DOI] [PubMed] [Google Scholar]
- 19.Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355(15):1572–1582. [DOI] [PubMed] [Google Scholar]
- 20.Hudson MM, Ehrhardt MJ, Bhakta N, et al. Approach for Classification and Severity Grading of Long-term and Late-Onset Health Events among Childhood Cancer Survivors in the St. Jude Lifetime Cohort. Cancer Epidemiol Biomarkers Prev. 2017;26(5):666–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hudson MM, Ness KK, Gurney JG, et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA. 2013;309(22):2371–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bhakta N, Liu Q, Ness KK, et al. The cumulative burden of surviving childhood cancer: an initial report from the St Jude Lifetime Cohort Study (SJLIFE). Lancet. 2017;390(10112):2569–2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang Z, Wilson CL, Easton J, et al. Genetic Risk for Subsequent Neoplasms Among Long-Term Survivors of Childhood Cancer. J Clin Oncol. 2018;36(20):2078–2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McBride ML, Rogers PC, Sheps SB, et al. Childhood, adolescent, and young adult cancer survivors research program of British Columbia: objectives, study design, and cohort characteristics. Pediatr Blood Cancer. 2010;55(2):324–330. [DOI] [PubMed] [Google Scholar]
- 25.Lorenzi MF, Xie L, Rogers PC, et al. Hospital-related morbidity among childhood cancer survivors in British Columbia, Canada: report of the childhood, adolescent, young adult cancer survivors (CAYACS) program. Int J Cancer. 2011;128(7):1624–1631. [DOI] [PubMed] [Google Scholar]
- 26.Lorenzi M, McMillan AJ, Siegel LS, et al. Educational outcomes among survivors of childhood cancer in British Columbia, Canada: report of the Childhood/Adolescent/Young Adult Cancer Survivors (CAYACS) Program. Cancer. 2009;115(10):2234–2245. [DOI] [PubMed] [Google Scholar]
- 27.McBride ML, de Oliveira C, Duncan R, et al. Comparing Childhood Cancer Care Costs in Two Canadian Provinces. Healthc Policy. 2020;15(3):76–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hawkins MM, Wilson LM, Stovall MA, et al. Epipodophyllotoxins, alkylating agents, and radiation and risk of secondary leukaemia after childhood cancer. BMJ. 1992;304(6832):951–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hawkins MM, Wilson LM, Burton HS, et al. Radiotherapy, alkylating agents, and risk of bone cancer after childhood cancer. J Natl Cancer Inst. 1996;88(5):270–278. [DOI] [PubMed] [Google Scholar]
- 30.Robertson CM, Hawkins MM, Kingston JE. Late deaths and survival after childhood cancer: implications for cure. BMJ. 1994;309(6948):162–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hawkins MM, Lancashire ER, Winter DL, et al. The British Childhood Cancer Survivor Study: Objectives, methods, population structure, response rates and initial descriptive information. Pediatr Blood Cancer. 2008;50(5):1018–1025. [DOI] [PubMed] [Google Scholar]
- 32.Reulen RC, Winter DL, Frobisher C, et al. Long-term cause-specific mortality among survivors of childhood cancer. JAMA. 2010;304(2):172–179. [DOI] [PubMed] [Google Scholar]
- 33.Reulen RC, Frobisher C, Winter DL, et al. Long-term risks of subsequent primary neoplasms among survivors of childhood cancer. JAMA. 2011;305(22):2311–2319. [DOI] [PubMed] [Google Scholar]
- 34.Frobisher C, Glaser A, Levitt GA, et al. Risk stratification of childhood cancer survivors necessary for evidence-based clinical long-term follow-up. Br J Cancer. 2017;117(11):1723–1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garwicz S, Anderson H, Olsen JH, et al. Second malignant neoplasms after cancer in childhood and adolescence: a population-based case-control study in the 5 Nordic countries. The Nordic Society for Pediatric Hematology and Oncology. The Association of the Nordic Cancer Registries. Int J Cancer. 2000;88(4):672–678. [DOI] [PubMed] [Google Scholar]
- 36.Olsen JH, Garwicz S, Hertz H, et al. Second malignant neoplasms after cancer in childhood or adolescence. Nordic Society of Paediatric Haematology and Oncology Association of the Nordic Cancer Registries. BMJ. 1993;307(6911):1030–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Asdahl PH, Winther JF, Bonnesen TG, et al. The Adult Life After Childhood Cancer in Scandinavia (ALiCCS) Study: Design and Characteristics. Pediatr Blood Cancer. 2015;62(12):2204–2210. [DOI] [PubMed] [Google Scholar]
- 38.de Fine Licht S, Winther JF, Gudmundsdottir T, et al. Hospital contacts for endocrine disorders in Adult Life after Childhood Cancer in Scandinavia (ALiCCS): a population-based cohort study. Lancet. 2014;383(9933):1981–1989. [DOI] [PubMed] [Google Scholar]
- 39.Norsker FN, Rechnitzer C, Cederkvist L, et al. Somatic late effects in 5-year survivors of neuroblastoma: a population-based cohort study within the Adult Life after Childhood Cancer in Scandinavia study. Int J Cancer. 2018;143(12):3083–3096. [DOI] [PubMed] [Google Scholar]
- 40.Kuehni CE, Rueegg CS, Michel G, et al. Cohort profile: the Swiss childhood cancer survivor study. Int J Epidemiol. 2012;41(6):1553–1564. [DOI] [PubMed] [Google Scholar]
- 41.Kasteler R, Weiss A, Schindler M, et al. Long-term pulmonary disease among Swiss childhood cancer survivors. Pediatr Blood Cancer. 2018;65(1). [DOI] [PubMed] [Google Scholar]
- 42.Weiss A, Sommer G, Kasteler R, et al. Long-term auditory complications after childhood cancer: A report from the Swiss Childhood Cancer Survivor Study. Pediatr Blood Cancer. 2017;64(2):364–373. [DOI] [PubMed] [Google Scholar]
- 43.Michel G, Rebholz CE, von der Weid NX, et al. Psychological distress in adult survivors of childhood cancer: the Swiss Childhood Cancer Survivor study. J Clin Oncol. 2010;28(10):1740–1748. [DOI] [PubMed] [Google Scholar]
- 44.de Vathaire F, Schweisguth O, Rodary C, et al. Long-term risk of second malignant neoplasm after a cancer in childhood. Br J Cancer. 1989;59(3):448–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.de Vathaire F, Francois P, Hill C, et al. Role of radiotherapy and chemotherapy in the risk of second malignant neoplasms after cancer in childhood. Br J Cancer. 1989;59(5):792–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tukenova M, Guibout C, Oberlin O, et al. Role of cancer treatment in long-term overall and cardiovascular mortality after childhood cancer. J Clin Oncol. 2010;28(8):1308–1315. [DOI] [PubMed] [Google Scholar]
- 47.de Vathaire F, El-Fayech C, Ben Ayed FF, et al. Radiation dose to the pancreas and risk of diabetes mellitus in childhood cancer survivors: a retrospective cohort study. Lancet Oncol. 2012;13(10):1002–1010. [DOI] [PubMed] [Google Scholar]
- 48.Demoor-Goldschmidt C, Allodji RS, Journy N, et al. Risk Factors for Small Adult Height in Childhood Cancer Survivors. J Clin Oncol. 2020:JCO1902361. [DOI] [PubMed] [Google Scholar]
- 49.Haddy N, Diallo S, El-Fayech C, et al. Cardiac Diseases Following Childhood Cancer Treatment: Cohort Study. Circulation. 2016;133(1):31–38. [DOI] [PubMed] [Google Scholar]
- 50.Berbis J, Michel G, Baruchel A, et al. Cohort Profile: the French childhood cancer survivor study for leukaemia (LEA Cohort). Int J Epidemiol. 2015;44(1):49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Le Meignen M, Auquier P, Barlogis V, et al. Bone mineral density in adult survivors of childhood acute leukemia: impact of hematopoietic stem cell transplantation and other treatment modalities. Blood. 2011;118(6):1481–1489. [DOI] [PubMed] [Google Scholar]
- 52.Oudin C, Berbis J, Bertrand Y, et al. Prevalence and characteristics of metabolic syndrome in adults from the French childhood leukemia survivors’ cohort: a comparison with controls from the French population. Haematologica. 2018;103(4):645–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Barlogis V, Auquier P, Bertrand Y, et al. Late cardiomyopathy in childhood acute myeloid leukemia survivors: a study from the L.E.A. program. Haematologica. 2015;100(5):e186–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Teepen JC, van Leeuwen FE, Tissing WJ, et al. Long-Term Risk of Subsequent Malignant Neoplasms After Treatment of Childhood Cancer in the DCOG LATER Study Cohort: Role of Chemotherapy. J Clin Oncol. 2017;35(20):2288–2298. [DOI] [PubMed] [Google Scholar]
- 55.Streefkerk N, Heins MJ, Teepen JC, et al. The involvement of primary care physicians in care for childhood cancer survivors. Pediatr Blood Cancer. 2019;66(8):e27774. [DOI] [PubMed] [Google Scholar]
- 56.Feijen EAM, Leisenring WM, Stratton KL, et al. Derivation of Anthracycline and Anthraquinone Equivalence Ratios to Doxorubicin for Late-Onset Cardiotoxicity. JAMA Oncol. 2019;5(6):864–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zurlo MG, Pastore G, Masera G, et al. Italian registry of patients off therapy after childhood acute lymphoblastic leukemia. Results after first phase of data collection. Cancer. 1986;57(5):1052–1055. [DOI] [PubMed] [Google Scholar]
- 58.Bagnasco F, Caruso S, Andreano A, et al. Late mortality and causes of death among 5-year survivors of childhood cancer diagnosed in the period 1960–1999 and registered in the Italian Off-Therapy Registry. Eur J Cancer. 2019;110:86–97. [DOI] [PubMed] [Google Scholar]
- 59.Haupt R, Spinetta JJ, Ban I, et al. Long term survivors of childhood cancer: cure and care. The Erice statement. Eur J Cancer. 2007;43(12):1778–1780. [DOI] [PubMed] [Google Scholar]
- 60.Byrne J, Alessi D, Allodji RS, et al. The PanCareSurFup consortium: research and guidelines to improve lives for survivors of childhood cancer. Eur J Cancer. 2018;103:238–248. [DOI] [PubMed] [Google Scholar]
- 61.Allodji RS, Hawkins MM, Bright CJ, et al. Risk of subsequent primary leukaemias among 69,460 five-year survivors of childhood cancer diagnosed from 1940 to 2008 in Europe: A cohort study within PanCareSurFup. Eur J Cancer. 2019;117:71–83. [DOI] [PubMed] [Google Scholar]
- 62.Bright CJ, Hawkins MM, Winter DL, et al. Risk of Soft-Tissue Sarcoma Among 69 460 Five-Year Survivors of Childhood Cancer in Europe. J Natl Cancer Inst. 2018;110(6):649–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fidler MM, Reulen RC, Winter DL, et al. Risk of Subsequent Bone Cancers Among 69 460 Five-Year Survivors of Childhood and Adolescent Cancer in Europe. J Natl Cancer Inst. 2018;110(2). [DOI] [PubMed] [Google Scholar]
- 64.Clemens E, Broer L, Langer T, et al. Genetic variation of cisplatin-induced ototoxicity in non-cranial-irradiated pediatric patients using a candidate gene approach: The International PanCareLIFE Study. Pharmacogenomics J. 2019. [DOI] [PubMed] [Google Scholar]
- 65.Borgmann-Staudt A, Kunstreich M, Schilling R, et al. Fertility knowledge and associated empowerment following an educational intervention for adolescent cancer patients. Psychooncology. 2019. [DOI] [PubMed] [Google Scholar]
- 66.Tonorezos ES, Barnea D, Cohn RJ, et al. Models of Care for Survivors of Childhood Cancer From Across the Globe: Advancing Survivorship Care in the Next Decade. J Clin Oncol. 2018;36(21):2223–2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kremer LC, Mulder RL, Oeffinger KC, et al. A worldwide collaboration to harmonize guidelines for the long-term follow-up of childhood and young adult cancer survivors: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Pediatr Blood Cancer. 2013;60(4):543–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Michel G, Mulder RL, van der Pal HJH, et al. Evidence-based recommendations for the organization of long-term follow-up care for childhood and adolescent cancer survivors: a report from the PanCareSurFup Guidelines Working Group. J Cancer Surviv. 2019;13(5):759–772. [DOI] [PubMed] [Google Scholar]