Abstract
Background: The effect of Leg-Length Discrepancy (LLD) on dynamic gait parameters has been extensively discussed. Podobarography is the study of foot-to-ground pressure distribution. It has been used to test plantar footprint deviations that could reveal pathology. Purpose: The aim of this study is to determine the effects of simulated LLD on dynamic gait parameters measured with a pressure platform in healthy subjects. Methods: Thirty-seven healthy subjects participated in observational cross-sectional research. A procedure was performed to capture the dynamic parameters of each participant under five different simulated LLD conditions. Support time, mean pressure, and peak pressure measures were registered on three trials for each foot and LLD level per session. An analysis of variance (ANOVA) test for repeated measures was performed to check for differences between the different simulated LLD levels. Results: The stance time of the short leg had no significant changes. The stance time of the long leg increased by 3.51% (p < 0.001), mean pressure of the short leg increased by 1.23% (p = 0.005), and decreased by 5.89% in the long leg (p < 0.001). Peak pressure of the short leg decreased by 2.58% (p = 0.031) and the long leg decreased by 12.11% (p < 0.001). Conclusions: This study demonstrates that increasing LLD causes an asymmetrical foot-loading pattern, with decreased mean and peak pressure on the longer limb, and consequently an overload on the short side. Furthermore, an increasing LLD causes increased stance time on the long leg.
Keywords: leg length inequality, gait, reliability analysis, pressure platform, lower limbs
1. Introduction
Leg-length discrepancy (LLD) is a condition frequently described in the literature as the unequal length of lower limbs. It is estimated to involve 40–70% of the population and can exceed 2 cm of inequality in close to 0.1% [1]. Knutson et al. concluded in a meta-analysis of 573 subjects that only 10% of the population had equal-length lower limbs [2]. LLD has been a cause of controversy in the clinical and research community for a long time. There is no agreement on many facets, such as its impact on various neuromusculoskeletal disorders, assessment of measurement methods, prevalence, and the degree of its clinical significance [3].
LLD can be classified as anatomical when the difference is caused by structural deformities that can be measured directly in the lower limb bones, or as functional when the inequality is caused by postural defects [4]. Both categories have been associated with hip or knee osteoarthritis and other mechanical pathologies as a result of an incorrect distribution of load [5,6].
Asymmetries in the kinematics of gait have been associated with different degrees of true LLD [5]—essentially pelvic drop and hip adduction in the stance phase [7,8]. Several authors have found flexion anomalies in the sagittal plane of the hip, knee, and ankle [7,9]. Furthermore, LLD has been related to decreased load times, stride length, and gait velocity of the shorter limb and increased cadence [10]. Kinetics asymmetries induced by LLD also appear to be related to the etiology of plantar fasciitis, lower back pain, and knee [11,12,13].
Clinically, two methods are commonly used to measure LLD: the direct method, which measures the distance between anterior superior iliac spine and medial malleolus when in a supine decubitus using a calibrated tape measure [13]; and the indirect method, measuring LLD using lifts to level the pelvis, rather using a pelvic leveling device, in a standing position [14]. Radiographic scanogrammetry is considered the gold standard for limb-length measurement but exposes patients to ionizing radiation [15]. These methods cannot assess dynamic changes in leg length, as they are performed in a static position.
In the literature, there are two ways to approach the study of LLD: examining subjects with diagnosed LLD, or simulating LLD on healthy subjects, appraising its role on gait anomalies. Some authors consider the first method to be limited by physical anomalies that commonly develop in subjects with real LLD as a result of compensations. Thus, these cannot be treated as pure LLD subjects [3].
Betsch et al. described a non-invasive method to simulate and evaluate LLD and its impact on human gait using plantar lifts [16,17].
Podobarography is the study of foot-to-ground pressure distribution. It has been used to evaluate foot static and dynamic interactions with terrain, posture [18], and the screening of plantar footprint deviations that could reveal pathology [19].
The aim of this study is to analyze the effect of simulated LLD on dynamic parameters obtained from a pressure platform in normal individuals. We hypothesized that subjects would asymmetrically alter their foot-loading pattern.
2. Materials and Methods
2.1. Design and Sample
The sample size was calculated with software from Grupo de Investigación en Riesgo Cardiovascular y Nutrición and Grupo de Investigación en Epidemiología y Genética Cardiovascular, IMIM-Hospital del Mar. Barcelona [20], to detect the correlation between dynamic parameters of the gait and different degrees of simulated LLD, which were standard deviation (SD) 4.34–3.48 [21] with 80% statistical power (β = 20%) and an interval of confidence 95% (α = 0.05) and 2-tailed test. A total of 37 participants were required to detect a difference equal or higher than 0.4 units. An SD of 0.86 and loss to follow-up rate of 0% is assumed.
Thirty-seven healthy test subjects (13 men and 24 women) aged 19 to 61 years old participated in the study. An observational cross-sectional research design according to Strengthening The Reporting of Observational Studies in Epidemiology (STROBE) criteria [22] and non-random consecutive sampling technique were used. The inclusion criteria were: being over 18 years, a European footwear size of 36–45, and no history of musculoskeletal damage or pain during the last year. Furthermore, clinical exploration was accomplished by the principal researcher to exclude real LLD > 5 mm, limited joint range, or asymmetrical pronated feet [23].
2.2. Ethical Considerations
The Research and Ethics Committee of Universidad Rey Juan Carlos, Spain, issued a favorable authorization certificate n° 0904201907519 for this study, following the ethical principles of the Helsinki declaration [24]. All subjects signed an informed consent before participating in this study.
2.3. Dynamic Data Collection
LLD was simulated with Ethyl-Vinyl-Acetate plantar lifts of 70A shore hardness and 5, 10, 15, and 20mm height, secured to the right shoe of each subject. This proceeding emulates LLD by generating pelvic obliquity.
In order to capture the dynamic parameters, we used a Podoprint® platform (Namrol Group, Barcelona, Spain), which, in a previous publication, was used to assess the intra and intersession repeatability and reliability in healthy subjects with simulated LLD [25]. A self-calibrating system, with 1600 10 × 10 mm resistive sensors and a sample rate of 100 Hz, was installed into the center of a flat 4.8 m walkway at ground level (Table 1).
Table 1.
Technical specifications of the pressure platform.
| Specification | Description |
|---|---|
| Size (Length/Width/Height) | 615 × 565 × 23 mm |
| Weight | 3.15 kg |
| Sensor type | Calibrated resistive |
| Active surface | 400 × 400 mm |
| Sensor size | 10 × 10 mm |
| Sensor number | 1600 (40 × 40) |
| Minimum/maximum pressure range per sensor | 0.4 N/m2 (0.0004 kPa) to 100 N/m2 (0.1 kPa) |
| Acceptable temperature | 0 °C to +40 °C |
| Acquisition frequency | 100 Hz |
| Power | Via Universal Serial Bus (USB) 5V, 400 mA |
| Operating system required | Windows® 7, 8 or 10 |
Each volunteer was instructed to walk normally, looking straight ahead. The starting position was set to match the footstep on the platform. Participants walked at a self-selected speed for all the trials; however, it was controlled with digital video recording to ensure the normal cadence under laboratory conditions, which range from 81 to 138 steps per minute [26]. The procedure was performed to register the dynamic parameters of each participant under five different simulated LLD levels (0, 5, 10, 15, and 20 mm) in randomized order. Stance time (ms), mean pressure (g/cm2), and peak pressure (g/cm2) measures were recorded. These parameters were considered the most frequently employed in functional foot assessment of pathological conditions [27,28,29].
Two testing sessions were held on seven separate days. Three trials were performed for each foot and LLD level per session. Before capturing the dynamic data, all volunteers completed a three-minute walk on the walkway to habituate themselves with the platform and plantar lifts. Four steps of each foot were collected per trial using the platform’s “Multiple Dynamic” mode, which directly provides the averaged parameters. The sample rate was 100 Hz. The same researcher tested all the participants (Figure 1). The data obtained from the pressure platform system were stored and processed using manufacturer-specific software Podoprint® for Windows®, version 8.6.5 (Namrol Group, Barcelona, Spain).
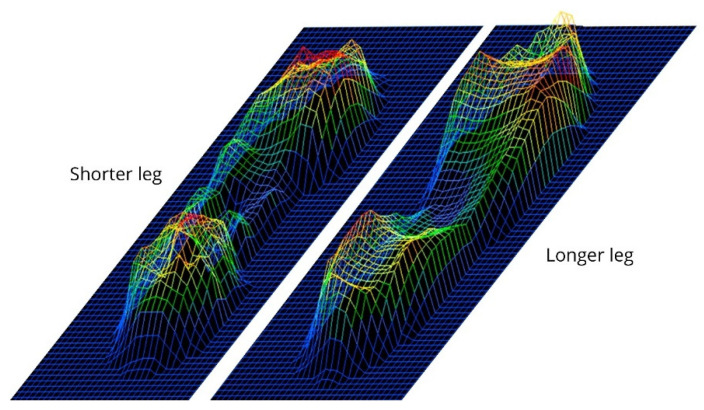
Figure 1.
An example of the plantar pressure curves of one subject during gait with a simulated LLD (20 mm).
2.4. Statistical Analysis
All data were verified for outliers and normal distribution by the one-sample Shapiro–Wilk test. Normally distributed data were presented as mean and standard deviation. Samples were removed individually if found to be greater than 3 SD from the group mean. The intrasession reliability was obtained by three repeated trials for each simulated DLL condition and each foot at the first and second testing sessions. The coefficient of variation (CoV) [30] was used to indicate the relationship between the size of the mean and the variability of each of the variables studied and it was calculated as . The intraclass correlation coefficient (ICC) obtained using the (2,1) model (two-way random, single measurement, absolute agreement ICC model) was calculated in order to analyze the reliability between trials [31]. The standard error of measurement (SEM) was calculated as and expressed as a percentage of the mean: [32].
Furthermore, the minimum detectable change (MDC) was calculated. This was described as the magnitude of the value variation of each scale, below which change can be interpreted as inherent to the variability of the measurement method, without any real change to the clinical situation of the subject. It was obtained as a standardized mean as and expressed as a percentage of the mean: [33,34].
Intersession reliability was determined by retesting all subjects seven days after the first session. The average of the measurements for each session, for each subject and LLD condition, was used to calculate the ICC3,1. For absolute comparison of the results obtained in the two sessions, CoV, SEM and MDC were expressed as percentages of the mean [33,34].
An analysis of variance (ANOVA) test for repeated measures was performed to check for differences between the different simulated LLD levels [35]. Bonferroni was used to adjust the type I error for multiple comparisons. To verify sphericity assumption, Mauchly’s test was used and subsequently corrected for lack of sphericity using the Greenhouse–Geisser correction. The level of significance was set at p < 0.05. To estimate the effect size, partial eta squared (η2p) were calculated. Cohen [36] provided benchmarks to define small (η2 = 0.01), medium (η2 = 0.06), and large (η2 = 0.14) effects.
The IBM® SPSS® for Windows®, version 22.0 statistical package, was used for data analysis and graphics (SPSS, Inc., Chicago, IL, USA).
3. Results
Thirty-seven healthy test subjects (13 men and 24 women) aged 19 to 61 years participated in the study (Table 2).
Table 2.
Descriptive data of the study participants showing demographics and anthropometric characteristics for the total sample by gender.
| Variable | Male n = 13 | Female n = 24 | Total n = 37 |
|---|---|---|---|
| Mean ± SD (95% CI) | Mean ± SD (95% CI) | Mean ± SD (95% CI) | |
| Age (years) | 39.21 ± 11.52 (32.56–45.87) | 38.91 ± 11.80 (33.81–44.02) | 39.03 ± 11.54 (35.18–42.87) |
| Weight (kg) | 73.50 ± 8.23 (68.74–78.25) | 61.08 ± 10.13 (56.70–65.47) | 65.78 ± 11.16 (62.06–69.50) |
| Height (m) | 1.75 ± 0.09 (1.69–1.80) | 1.64 ± 0.08 (1.61–1.68) | 1.68 ± 0.10 (1.65–1.72) |
| MBI | 23.99 ± 2.75 (22.40–25.58) | 22.40 ± 2.83 (21.17–23.63) | 23 ± 2.87 (22.04–23,96) |
| Foot size (EC) | 42.03 ± 2.07 (40.83–43.23) | 37.86 ± 1.20 (37.34–38.39) | 39.44 ± 2.57 (38.58–40.30) |
BMI, body mass index; SD, standard deviation; 95% CI, 95 percent confidence interval; EC, European countries.
The measurements were reproducible for an individual even if repeated during the same test session or when tested seven days later. Descriptive statistics, represented by mean and standard deviation, and reliability data, represented by CoV, ICC, SEM and MDC, were calculated for the first session. The Cov for intrasession reliability ranged from 0.13% to 2.13%, and the ICC ranged from 0.760 to 0.980. The SEM% ranged from 0.03% to 0.70%, and the MDC% ranged from 0.07% to 1.93%.
In the second session, CoV for intrasession reliability ranged from 0.12% to 1.64%, and the ICC ranged from 0.771 to 0.980. The SEM% ranged from 0.03% to 0.78%, and MDC% ranged from 0.08% to 1.91%.
The average measurements from both test sessions and intersession reliability data, represented by CoV, ICC, SEM% and MDC%, are presented in Table 3. The CoV for intersession reliability ranged from 0.39% to 1.65%, and the ICC ranged from 0.866 to 0.988. The SEM% ranged from 0.06% to 0.58% and MDC% ranged from 0.18% to 1.61%.
Table 3.
Intersession reliability of time and pressure variables for each foot under simulated LLD conditions.
| Variable | Mean (SD) | CoV (%) | ICC (95% CI) | SEM% | MDC% |
|---|---|---|---|---|---|
| 0 mm of LLD | |||||
| Stance time short (ms) | 761.42 (7.19) | 0.94 | 0.957 (0.932–0.976) | 0.20 | 0.54 |
| Stance time long (ms) | 754.05 (2.96) | 0.39 | 0.960 (0.936–0.977) | 0.08 | 0.22 |
| Mean pressure short (g/cm2) | 748.74 (5.12) | 0.68 | 0.955 (0.927–0.974) | 0.15 | 0.40 |
| Mean pressure long (g/cm2) | 750.95 (12.37) | 1.65 | 0.931 (0.889–0.960) | 0.43 | 1.20 |
| Peak pressure short (g/cm2) | 1427.82 (16.46) | 1.15 | 0.928 (0.886–0.959) | 0.31 | 0.86 |
| Peak pressure long (g/cm2) | 1417.26 (13.03) | 0.92 | 0.918 (0.869–0.953) | 0.26 | 0.73 |
| 5 mm of LLD | |||||
| Stance time short (ms) | 762.16 (5.77) | 0.76 | 0.981 (0.969–0.989) | 0.10 | 0.29 |
| Stance time long (ms) | 759.73 (5.03) | 0.66 | 0.980 (0.968–0.988) | 0.09 | 0.26 |
| Mean pressure short (g/cm2) | 746.61 (5.44) | 0.73 | 0.955 (0.928–0.974) | 0.15 | 0.43 |
| Mean pressure long (g/cm2) | 747.13 (11.88) | 1.59 | 0.866 (0.785–0.923) | 0.58 | 1.61 |
| Peak pressure short (g/cm2) | 1443.52 (14.39) | 1.00 | 0.925 (0.879–0.957) | 0.27 | 0.76 |
| Peak pressure long (g/cm2) | 1338.84 (9.45) | 0.71 | 0.927 (0.883–0.958) | 0.19 | 0.53 |
| 10 mm of LLD | |||||
| Stance time short (ms) | 763.82 (14.15) | 0.54 | 0.986 (0.977–0.992) | 0.06 | 0.18 |
| Stance time long (ms) | 765.09 (4.23) | 0.55 | 0.984 (0.974–0.991) | 0.07 | 0.19 |
| Mean pressure short (g/cm2) | 756.19 (7.65) | 1.01 | 0.970 (0.952–0.983) | 0.18 | 0.49 |
| Mean pressure long (g/cm2) | 723.24 (11.83) | 1.64 | 0.918 (0.869–0.953) | 0.47 | 1.30 |
| Peak pressure short (g/cm2) | 1435.58 (11.95) | 0.83 | 0.924 (0.878–0.956) | 0.23 | 0.64 |
| Peak pressure long (g/cm2) | 1274.77 (15.55) | 1.22 | 0.898 (0.837–0.941) | 0.39 | 1.08 |
| 15 mm of LLD | |||||
| Stance time short (ms) | 760.54 (4.39) | 0.58 | 0.988 (0.981–0.993) | 0.06 | 0.18 |
| Stance time long (ms) | 775.58 (4.19) | 0.54 | 0.986 (0.977–0.992) | 0.06 | 0.18 |
| Mean pressure short (g/cm2) | 760.41 (5.54) | 0.73 | 0.972 (0.955–0.984) | 0.12 | 0.34 |
| Mean pressure long (g/cm2) | 711.58 (5.25) | 0.74 | 0.929 (0.886–0.959) | 0.20 | 0.55 |
| Peak pressure short (g/cm2) | 1423.44 (17.28) | 1.21 | 0.928 (0.884–0.958) | 0.33 | 0.90 |
| Peak pressure long (g/cm2) | 1265.21 (17.58) | 1.39 | 0.935 (0.895–0.962) | 0.35 | 0.98 |
| 20 mm of LLD | |||||
| Stance time short (ms) | 766.98 (5.22) | 0.68 | 0.983 (0.976–0.990) | 0.09 | 0.25 |
| Stance time long (ms) | 783.51 (4.31) | 0.55 | 0.984 (0.974–0.991) | 0.07 | 0.19 |
| Mean pressure short (g/cm2) | 758 (3.51) | 0.46 | 0.962 (0.940–0.978) | 0.09 | 0.25 |
| Mean pressure long (g/cm2) | 706.71 (5.47) | 0.77 | 0.890 (0.824–0.937) | 0.26 | 0.71 |
| Peak pressure short (g/cm2) | 1409.33 (21.37) | 1.52 | 0.906 (0.850–0.946) | 0.46 | 1.29 |
| Peak pressure long (g/cm2) | 1245.60 (16.16) | 1.30 | 0.900 (0.841–0.943) | 0.41 | 1.14 |
SD, standard deviation; CoV, coefficient of variation; ICC, intraclass correlation coefficient; 95% CI, 95 percent confidence interval; SEM, standard error of measurement; MDC, minimum detectable change.
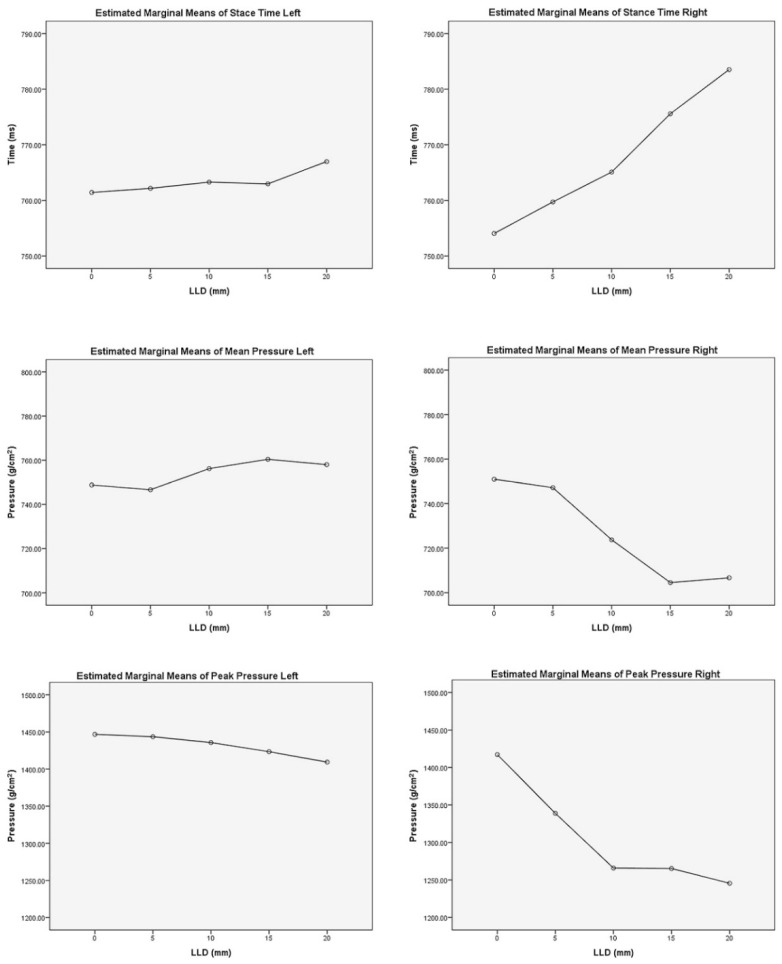
The results of repeated-measures ANOVA showed statistically significant changes in five of six studied variables under different simulated LLD conditions (Table 4). In addition, a pairwise comparison based on the estimated marginal means between different LLD levels of each dynamic variable was calculated (Table 5).
Table 4.
Repeated-measures analysis of variance (RM-ANOVA) including a test of influence of the sphericity assumption, analysis of effect, and a contrast analysis of the significant interaction effect.
| Variable | MT (p) | SS | DF | MS | F | p | η2p |
|---|---|---|---|---|---|---|---|
| Stance time short a | <0.001 | 682.97 | 2.18 | 313.00 | 0.30 | 0.758 | 0.008 † |
| Stance time long a | <0.001 | 21043.48 | 2.09 | 10025.73 | 11.90 | <0.001 ** | 0.249 ††† |
| Mean pressure short | 0.165 * | 5330.90 | 4 | 1332.72 | 3.92 | 0.005 ** | 0.098 †† |
| Mean pressure long a | <0.001 | 70469.07 | 2.63 | 26732.11 | 15.31 | <0.001 ** | 0.299 ††† |
| Peak pressure short a | 0.003 | 35130.29 | 2.79 | 12554.20 | 3.16 | 0.031** | 0.081 †† |
| Peak pressure long a | <0.001 | 754051.37 | 2.15 | 350219.50 | 32.54 | <0.001 ** | 0.475 ††† |
MT(p), Mauchly test probability; SS, sum of squares; DF, degrees of freedom; MS, mean square; F, variance ratio; p, probability; η2p, partial eta squared; a, Greenhouse–Geisser adjusted; *, sphericity assumed; **, reached level of significance; †, small effect; ††, medium effect; †††, large effect.
Table 5.
Pairwise comparison based on estimated marginal means.
| STS | STL | MPS | MPL | PPS | PPL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LLD (mm) |
MD (SE) | p a | MD (SE) | p a | MD (SE) | p a | MD (SE) | p a | MD (SE) | p a | MD (SE) | p a | |
| 0 | 5 | −0.73 (5.08) | 1.000 | −5.67 (4.40) | 1.000 | 2.13 (3.87) | 1.000 | 3.824 (8.10) | 1.000 | −14.80 (10.12) | 1.000 | 78.41 (12.38) | <0.0001* |
| 10 | −2.40 (7.28) | 1.000 | −11.03 (6.48) | 0.973 | −7.63 (4.89) | 1.000 | 27.71 (9.48) | 0.060 | −6.86 (10.84) | 1.000 | 142.49 (18.32) | <0.0001* | |
| 15 | 0.88 (6.97) | 1.000 | −21.53 (6.78) | 0.031 * | −11.66 (4.57) | 0.15 | 39.37 (10.12) | 0.004 * | 3.47 (13.35) | 1.000 | 152.05 (21.64) | <0.0001 * | |
| 20 | −5.28 (7.49) | 1.000 | −29.45 (6.68) | 0.001 * | −9.25 (4.87) | 0.66 | 44.24 (10.16) | 0.001 * | 16.68 (15.49) | 1.000 | 171.65 (23.79) | <0.0001 * | |
| 5 | 0 | 0.73 (5.08) | 1.000 | 5,67 (4.40) | 1.000 | −2.13 (3.87) | 1.000 | −3.82 (8.10) | 1.000 | 14.80 (10.12) | 1.000 | −78.41 (12.38) | <0.0001 * |
| 10 | −1.66 (3.89) | 1.000 | −5.36 (3.65) | 1.000 | −9.76 (4.50) | 0.37 | 23.89 (6.95) | 0.015 * | 7.94 (10.64) | 1.000 | 64.07 (14.81) | 0.001 * | |
| 15 | 1.62 (4.30) | 1.000 | −15.85 (4.16) | 0.005 * | −13.79 (4.33) | 0.03 * | 35.55 (6.89) | <0.0001 * | 18.27 (14.04) | 1.000 | 73.63 (20.84) | 0.011* | |
| 20 | −4.55 (4.91) | 1.000 | −23.78 (4.26) | 0.0001 * | −11.38 (4.77) | 0.23 | 40.42 (7.86) | <0.0001 * | 31.48 (13.89) | 0.3 | 93.24 (21.03) | 0.001 * | |
| 10 | 0 | 2.40 (7.28) | 1.000 | 11.03 (6.48) | 0.973 | 7.63 (4.89) | 1.000 | −27.71 (9.48) | 0.060 | 6.86 (10.84) | 1.000 | −142.49 (18.32) | <0.0001 * |
| 5 | 1.66 (3.89) | 1.000 | 5.36 (3.65) | 1.000 | 9.76 (4.50) | 0.37 | −23.89 (6.95) | 0.015 * | −7.94 (10.64) | 1.000 | −64.07 (14.81) | 0.001 * | |
| 15 | 3.28 (3.63) | 1.000 | −10.49 (3.78) | 0.087 | −4.03 (3.75) | 1.000 | 11.66 (5.77) | 0.511 | 10.33 (10.15) | 1.000 | 9.55 (12.77) | 1.000 | |
| 20 | −2.88 (3.70) | 1.000 | −18.42 (3.96) | 0.0001 * | −1.62 (3.71) | 1.000 | 16.53 (5.92) | 0.083 | 23.54 (11.04) | 0.4 | 29.16 (12.56) | 0.261 | |
| 15 | 0 | −0.88 (6.97) | 1.000 | 21.53 (6.78) | 0.031 * | 11.66 (4.57) | 0.15 | −39.37 (10.12) | 0.004 * | −3.47 (13.35) | 1.000 | −152.05 (21.64) | <0.0001 * |
| 5 | −1.62 (4.30) | 1.000 | 15.85 (4.16) | 0.005 * | 13.79 (4.33) | 0.03 * | −35.55 (6.89) | <0.0001 * | −18.27 (14.04) | 1.000 | −73.63 (20.84) | 0.011 * | |
| 10 | −3.28 (3.63) | 1.000 | 10.49 (3.78) | 0.087 | 4.03 (3.75) | 1.000 | −11.66 (5.77) | 0.511 | −10.33 (10.15) | 1.000 | −9.55 (12.77) | 1.000 | |
| 20 | −6.17 (3.21) | 0.63 | −7.92 (2.76) | 0.069 | 2.41 (3.41) | 1.000 | 4.86 (6.46) | 1.000 | 13.20 (13.20) | 1.000 | 19.60(12.94) | 1.000 | |
| 20 | 0 | 5.28 (7.49) | 1.000 | 29.45 (6.68) | 0.001 * | 9.25 (4.87) | 0.66 | −44.24 (10.16) | 0.001 * | −16.68 (15.49) | 1.000 | −171.65 (23.79) | <0.0001 * |
| 5 | 4.55 (4.91) | 1.000 | 23.78 (4.26) | 0.0001 * | 11.38 (4.77) | 0.23 | −40.42 (7.86) | <0.0001 * | −31.48 (13.89) | 0.296 | −93.24 (21.03) | 0.001 * | |
| 10 | 2.88 (3.70) | 1.000 | 18.42 (3.96) | 0.0001 * | 1.62 (3.71) | 1.000 | −16.53 (5.92) | 0.083 | −23.54 (11.04) | 0.4 | −29.16 (12.56) | 0.261 | |
| 15 | 6.17 (3.21) | 0.63 | 7.92 (2.76) | 0.069 | −2.41 (3.41) | 1.000 | −4.86 (6.46) | 1.000 | −13.20 (9.66) | 1.000 | −19.60 (12.94) | 1.000 | |
STS, stance time short; STL, stance time long; MPS, mean pressure short; MPL, mean pressure long; PPS, peak pressure short; PPL, peak pressure long; LLD, leg length discrepancy; MD, mean difference; SE, standard error; p, Probability; a, Bonferroni adjustment for multiple comparisons; *, reach level of significance.
Changes were observed in all pressure parameters, in the short and long leg, and in the stance time of the long leg: stance time of the long leg increased by 3.51% (p < 0.001), mean pressure of the short leg increased by 1.23% (p = 0.005) and decreased by 5.89% in the long leg (p < 0.001). Peak pressure of the short leg decreased by 2.58% (p = 0.031) and decreased by 12.11% in the long leg (p < 0.001). (Figure 2)
Figure 2.
Estimated marginal means of stance time, mean pressure and peak pressure.
4. Discussion
Different reports expose that LLD can generate substantial gait parameters deviations [3]. We can find in the literature two methods to evaluate LLD effects on gait: measuring subjects with real LLD or simulating LLD on healthy subjects. Using subjects with real LLD, it is more difficult to obtain a homogeneous sample, due to a greater diversity of LLD, ages, or associated pathologies that could potentially lead to confounding variables.
The objective of the current study was to understand the effect of simulated LLD on dynamic parameters measured with a pressure platform in healthy subjects. The number of participants was 37, a total of 74 limbs were evaluated, comprising 444 measurements.
This study demonstrates that as LLD increases, there is a decreased mean pressure and peak pressure on the long leg. As a result, the subjects asymmetrically alter their foot loading pattern. According to White [37], the shorter limb for the simulated LLD group supported greater loads and loading rates. In his study, the results showed short-term responses to an induced change in LLD. Over time, asymmetric limb loading could be reduced by compensatory strategies [38]. Disproportionate pressures and higher load rates under dynamic conditions could make the shorter limb susceptible to limb joint damage. Golightly et al. [39] found a positive relationship of LLD ≤20 mm with radiographic knee and hip osteoarthritis.
Total hip replacement surgery [40] usually results in mild postoperative LLD that could lead the prosthesis to higher pressures and potentially reduce the success of the surgery.
Evaluating which limb is bearing the greater load is a crucial issue after surgery because of the potential for stress to the prosthesis. It could contribute to patient dissatisfaction even when intervention had an outstanding result.
Furthermore, our research showed that stance times increased on the long leg when LLD increased. These findings are consistent with other studies [21,41]. The changes produced by mild LLD may appear minimal when viewed in simple measurements. However, they could generate major effects when it comes to repetitive loading. According to the meta-analysis by Crawford et al. [42], patients with foot plantar pressure overload and extended contact times have a high risk of developing a foot ulcer. The early evaluation of LLD with a pressure platform system in patients with diabetes mellitus could prevent ulcerations.
It should be noted that, in this study, lifts were always located under the right shoe. Some studies found differences between the dominant and non-dominant leg [43], which would be clinically interesting to test and evaluate in future studies. Furthermore, time and pressure parameters were evaluated for the total plantar surface. Previous studies have found intrasession variability when using regional analysis [27,44]. Future research should consider the study of asymmetries on pressure dynamic patterns as the predictive condition of LLD.
5. Conclusions
Increasing leg length discrepancy causes a decrease in both mean and peak pressure on the longer limb, and consequently, an overload on the short side. Furthermore, an increasing LLD causes an increased stance time on the long leg. Contrary to other studies, our findings suggest that an LLD smaller than 20 mm should not be ignored.
Author Contributions
Conceptualization, H.P.-B., R.B.-d.-B.-V., M.E.L.-I., D.L.-L., E.N.-F., E.M.M.-J., J.M. and C.C.-L.; data curation, H.P.-B.; formal analysis, H.P.-B., R.B.-d.-B.-V., M.E.L.-I., D.L.-L., E.N.-F., E.M.M.-J., J.M. and C.C.-L.; investigation, H.P.-B., R.B.-d.-B.-V., M.E.L.-I., D.L.-L., E.N.-F., E.M.M.-J. and J.M.; methodology, H.P.-B., R.B.-d.-B.-V., M.E.L.-I., D.L.-L., E.N.-F., E.M.M.-J., J.M. and C.C.-L.; supervision, H.P.-B., R.B.-d.-B.-V., M.E.L.-I., D.L.-L., E.N.-F., E.M.M.-J., J.M. and C.C.-L.; validation, R.B.-d.-B.-V.; writing—original draft, H.P.-B., R.B.-d.-B.-V., M.E.L.-I., D.L.-L., E.N.-F., E.M.M.-J., J.M. and C.C.-L.; writing—review and editing, H.P.-B., R.B.-d.-B.-V., M.E.L.-I., D.L.-L., E.N.-F., E.M.M.-J., J.M. and C.C.-L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
An ethics committee of the Universidad Rey Juan Carlos approved our research (number 0904201907519).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gurney B. Leg length discrepancy. Gait Posture. 2002;15:195–206. doi: 10.1016/S0966-6362(01)00148-5. [DOI] [PubMed] [Google Scholar]
- 2.Knutson G.A. Anatomic and functional leg-length inequality: A review and recommendation for clinical decision-making. Part II, the functional or unloaded leg-length asymmetry. Chiropr. Osteopat. 2005;13:12. doi: 10.1186/1746-1340-13-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khamis S., Carmeli E. Relationship and significance of gait deviations associated with limb length discrepancy: A systematic review. Gait Posture. 2017;57:115–123. doi: 10.1016/j.gaitpost.2017.05.028. [DOI] [PubMed] [Google Scholar]
- 4.Langer S. Structural leg shortage. A case report. J. Am. Podiatry Assoc. 1976;66:38–40. doi: 10.7547/87507315-66-1-38. [DOI] [PubMed] [Google Scholar]
- 5.McCaw S.T., Bates B.T. Biomechanical implications of mild leg length inequality. Br. J. Sports Med. 1991;25:10–13. doi: 10.1136/bjsm.25.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McWilliams A.B., Grainger A.J., O’Connor P.J., Redmond A.C., Stewart T.D., Stone M.H. A Review of Symptomatic Leg Length Inequality following Total Hip Arthroplasty. HIP Int. 2013;23:6–14. doi: 10.5301/HIP.2013.10631. [DOI] [PubMed] [Google Scholar]
- 7.Akşahin E., Güzel A., Erdoǧan A.O., Yüksel H.Y., Çelebi L., Aktekin C.N., Biçimoǧlu A. The patellofemoral kinematics in patients with untreated developmental dislocation of the hip suffering from patellofemoral pain. Knee Surg. Sports Traumatol. Arthrosc. 2012;20:2337–2347. doi: 10.1007/s00167-011-1807-3. [DOI] [PubMed] [Google Scholar]
- 8.Aiona M., Do K.P., Emara K., Dorociak R., Pierce R. Gait patterns in children with limb length discrepancy. J. Pediatr. Orthop. 2014;35:280–284. doi: 10.1097/BPO.0000000000000262. [DOI] [PubMed] [Google Scholar]
- 9.Li J., McWilliams A.B., Jin Z., Fisher J., Stone M.H., Redmond A.C., Stewart T.D. Unilateral total hip replacement patients with symptomatic leg length inequality have abnormal hip biomechanics during walking. Clin. Biomech. (Bristol Avon.) 2015;30:513–519. doi: 10.1016/j.clinbiomech.2015.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Resende R.A., Kirkwood R.N., Deluzio K.J., Morton A.M., Fonseca S.T. Mild leg length discrepancy affects lower limbs, pelvis and trunk biomechanics of individuals with knee osteoarthritis during gait. Clin. Biomech. 2016;38:1–7. doi: 10.1016/j.clinbiomech.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Mahmood S., Huffman L.K., Harris J.G. Limb-length discrepancy as a cause of plantar fasciitis. J. Am. Podiatr. Med. Assoc. 2010;100:452–455. doi: 10.7547/1000452. [DOI] [PubMed] [Google Scholar]
- 12.Kendall J.C., Bird A.R., Azari M.F. Foot posture, leg length discrepancy and low back pain—Their relationship and clinical management using foot orthoses—An overview. Foot. 2014;24:75–80. doi: 10.1016/j.foot.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Carlson M., Wilkerson J. Are differences in leg length predictive of lateral patello-femoral pain? Physiother. Res. Int. 2007;12:29–38. doi: 10.1002/pri.351. [DOI] [PubMed] [Google Scholar]
- 14.Petrone M.R., Guinn J., Reddin A., Sutlive T.G., Flynn T.W., Garber M.P. The accuracy of the Palpation Meter (PALM) for measuring pelvic crest height difference and leg length discrepancy. J. Orthop. Sports Phys. Ther. 2003;33:319–325. doi: 10.2519/jospt.2003.33.6.319. [DOI] [PubMed] [Google Scholar]
- 15.Murray K.J., Azari M.F. Leg length discrepancy and osteoarthritis in the knee, hip and lumbar spine. J. Can. Chiropr. Assoc. 2015;59:226–237. [PMC free article] [PubMed] [Google Scholar]
- 16.Betsch M., Wild M., Große B., Rapp W., Horstmann T. The effect of simulating leg length inequality on spinal posture and pelvic position: A dynamic rasterstereographic analysis. Eur. Spine J. 2012;21:691–697. doi: 10.1007/s00586-011-1912-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Betsch M., Rapp W., Przibylla A., Jungbluth P., Hakimi M., Schneppendahl J., Thelen S., Wild M. Determination of the amount of leg length inequality that alters spinal posture in healthy subjects using rasterstereography. Eur. Spine J. 2013;22:1354–1361. doi: 10.1007/s00586-013-2720-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Douglas Gross K., Felson D.T., Niu J., Hunter D.J., Guermazi A., Roemer F.W., Dufour A.B., Gensure E.H., Hannan M.T. Association of flat feet with knee pain and cartilage damage in older adults. Arthritis Care Res. 2011;63:937–944. doi: 10.1002/acr.20431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Bengoa Vallejo R.B., Iglesias M.E.L., Zeni J., Thomas S. Reliability and repeatability of the portable EPS-platform digital pressure-plate system. J. Am. Podiatr. Med. Assoc. 2013;103:197–203. doi: 10.7547/1030197. [DOI] [PubMed] [Google Scholar]
- 20.Marrugat J. Calculadora de Tamaño Muestral GRANMO. Versión 7.12 Abril 2012. [(accessed on 15 December 2019)]; Available online: https://www.imim.cat/ofertadeserveis/software-public/granmo/
- 21.O’Toole G.C., Makwana N.K., Lunn J., Harty J., Stephens M.M. The effect of leg length discrepancy on foot loading patterns and contact times. Foot Ankle Int. 2003;24:256–259. doi: 10.1177/107110070302400310. [DOI] [PubMed] [Google Scholar]
- 22.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int. J. Surg. 2014;12:1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 23.Rokkedal-Lausch T., Lykke M., Hansen M.S., Nielsen R.O. Normative values for the foot posture index between right and left foot: A descriptive study. Gait Posture. 2013;38:843–846. doi: 10.1016/j.gaitpost.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 24.General Assembly of the World Medical Association World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. J. Am. Coll. Dent. 2014;81:14–18. [PubMed] [Google Scholar]
- 25.Pereiro-Buceta H., Calvo-Lobo C., Becerro-de-Bengoa-Vallejo R., Losa-Iglesias M.E., Romero-Morales C., López-López D., Martínez-Jiménez E.-M. Intra and intersession repeatability and reliability of dynamic parameters in pressure platform assessments on subjects with simulated leg length discrepancy. A cross-sectional research. Sao Paulo Med. J. 2021 doi: 10.1590/1516-3180.2020.0791.r1.110321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tudor-Locke C., Rowe D.A. Using cadence to study free-living ambulatory behaviour. Sport. Med. 2012;42:381–398. doi: 10.2165/11599170-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 27.Gurney J.K., Kersting U.G., Rosenbaum D. Between-day reliability of repeated plantar pressure distribution measurements in a normal population. Gait Posture. 2008;27:706–709. doi: 10.1016/j.gaitpost.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 28.Martínez-Jiménez E.M., Losa-Iglesias M.E., Antolín-Gil M.S., López-López D., Romero-Morales C., Benito-De-pedro M., Calvo-Lobo C., Becerro-De-bengoa-vallejo R. Flexor digitorum brevis muscle dry needling changes surface and plantar pressures: A pre-post study. Life. 2021;11:48. doi: 10.3390/life11010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martínez-Jiménez E.M., Becerro-de-Bengoa-Vallejo R., Losa-Iglesias M.E., Díaz-Velázquez J.I., Palomo-López P., Rodríguez-Sanz D., Calvo-Lobo C., López-López D. Pressure and Traction Technique Improves Postural Control More Than Tactile Stimulation in Foot Plantar Fascia: A Randomized Single-Blind Trial. Arch. Phys. Med. Rehabil. 2020;101:978–984. doi: 10.1016/j.apmr.2020.01.017. [DOI] [PubMed] [Google Scholar]
- 30.Burdock E.I., Fleiss J.L., Hardestiny A.S. A new view of inter-observer agreement. Pers. Psychol. 1963;16:373–384. doi: 10.1111/j.1744-6570.1963.tb01283.x. [DOI] [Google Scholar]
- 31.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 32.Watkins M.P., Portney L. Foundations of Clinical Research : Applications to Practice. 3rd ed. Pearson Prentice Hall; Upper Saddle River, NJ, USA: 2009. [Google Scholar]
- 33.Bland J.M., Altman D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 34.Shrout P.E., Fleiss J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 35.Armstrong R.A. Recommendations for analysis of repeated-measures designs: Testing and correcting for sphericity and use of manova and mixed model analysis. Ophthalmic Physiol. Opt. 2017;37:585–593. doi: 10.1111/opo.12399. [DOI] [PubMed] [Google Scholar]
- 36.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Routledge; New York, NY, USA: 2013. [Google Scholar]
- 37.White S.C., Gilchrist L.A., Wilk B.E. Asymmetric Limb Loading with True or Simulated Leg-Length Differences. Clin. Orthop. Relat. Res. 2004;421:287–292. doi: 10.1097/01.blo.0000119460.33630.6d. [DOI] [PubMed] [Google Scholar]
- 38.Walsh M., Connolly P., Jenkinson A., O’Brien T. Leg length discrepancy—An experimental study of compensatory changes in three dimensions using gait analysis. Gait Posture. 2000;12:156–161. doi: 10.1016/S0966-6362(00)00067-9. [DOI] [PubMed] [Google Scholar]
- 39.Golightly Y.M., Allen K.D., Renner J.B., Helmick C.G., Salazar A., Jordan J.M. Relationship of limb length inequality with radiographic knee and hip osteoarthritis. Osteoarthr. Cartil. 2007;15:824–829. doi: 10.1016/j.joca.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Flecher X., Ollivier M., Argenson J.N. Lower limb length and offset in total hip arthroplasty. Orthop. Traumatol. Surg. Res. 2016;102:S9–S20. doi: 10.1016/j.otsr.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 41.Bhave A., Paley D., Herzenberg J.E. Improvement in Gait Parameters After Lengthening for the Treatment of Limb-length Discrepancy. J Bone Joint SurgAm. 1999;81:529–534. doi: 10.2106/00004623-199904000-00010. [DOI] [PubMed] [Google Scholar]
- 42.Crawford F., Inkster M., Kleijnen J., Fahey T. Review Predicting foot ulcers in patients with diabetes: A systematic review and meta-analysis. J. Assoc. Physicians. 2007;100:65–86. doi: 10.1093/qjmed/hcl140. [DOI] [PubMed] [Google Scholar]
- 43.Sadeghi H., Allard P., Prince F., Labelle H. Symmetry and limb dominance in able-bodied gait: A review. Gait Posture. 2000;12:34–45. doi: 10.1016/S0966-6362(00)00070-9. [DOI] [PubMed] [Google Scholar]
- 44.Ramanathan A.K., Kiran P., Arnold G.P., Wang W., Abboud R.J. Repeatability of the Pedar-X® in-shoe pressure measuring system. Foot Ankle Surg. 2010;16:70–73. doi: 10.1016/j.fas.2009.05.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.