Summary
Background:
Recognition of childhood weight status is important to the adoption of healthy lifestyle behaviours.
Objectives:
We assessed whether an exam room educational poster addressing weight and healthy lifestyle behaviours was acceptable to parents, prompted parent-provider communication or improved parental weight perception accuracy.
Methods:
In this multi-site randomized controlled trial, exam rooms were randomized to display the posters (English and Spanish) or not. Children ages 3 to 8 years (N = 965) attending well visits were weighed and roomed per usual clinic protocol. After the visit, parents completed a questionnaire assessing demographics, child weight status perceptions and whether they discussed weight status with provider or were shown growth charts. We used separate logistic regression analyses to examine associations between intervention status and: asking provider about child weight, being shown growth charts, and accuracy of weight perception, adjusting for covariates and clustering by exam room.
Results:
Of the parents who saw the poster, 97% liked seeing it and reported greater understanding of weight status visualization (96%) and healthy lifestyle behaviours (94%). Parents who saw the poster were more likely to report being shown a growth chart (OR 1.87, 95% 1.06, 3.30) but were not more likely to ask about their child’s weight status nor accurately report their child’s weight status.
Conclusions:
An educational exam room poster about healthy weight was well-received by parents and prompted providers to show the child’s growth chart but did not prompt parent-initiated conversations about weight status nor improve parental weight perception accuracy.
Keywords: communication, education, weight, weight perception
1 |. INTRODUCTION
Childhood obesity rates have increased substantially since 1988,1 with recent reports showing upward trends in severe obesity, as well.2 Childhood obesity is associated with significant physical and psychological comorbidities,3,4 making obesity prevention and treatment a priority for many public health experts.5–8 More than half of parents of children with obesity or overweight underestimate their child’s weight status9–13 or report never having heard from a health care provider that their child with overweight was overweight,14 which may pose a barrier to making behaviour changes that may help improve their child’s weight status.15
Several studies have found that most parents of children with overweight did not report concern about their child’s weight.16–18 Parental underestimation of child weight, and its associated lack of concern for child weight, makes parents less likely to make healthy changes that may improve their child’s body mass index (BMI) trajectory.15,16,19,20 Underestimation of child weight is not unique to children with obesity; about 10% to 15% of parents perceive their children with a healthy weight as ‘too skinny’ or underweight10,21–23 with greater percent at age 4 and 5 than at age 9.24 Younger children in general are more at risk for parental underestimation of weight than older children and adolescents,12,21,23,25,26 aligning with the timing of the physiologic adiposity nadir, which happens between 3 and 8 years, following toddlerhood.
Pediatricians use BMI charts for tracking child weight status and growth.27,28 BMI charts are also commonly used by pediatricians to illustrate to families the child’s current weight status and weight trajectory in relation to standardized norms. Prior studies have shown that color-coded (green, yellow and red) BMI charts are more easily understood than typical BMI charts, especially for parents with lower literacy and numeracy.29 Parents using color-coded charts had greater odds of answering BMI chart questions correctly compared to parents using standard charts and also frequently adopt the language of ‘red zone’, and ‘green zone’, when describing their child’s weight status. Color-coded BMI charts help pediatricians improve parents’ perception of their children’s weight status.30 However, considering the high rate of incorrect parental perception of child weight, additional visual aids that display healthy weight children may be warranted in order to assist parents in recognizing a healthy child weight status, especially around the age of the BMI nadir when children at a healthy weight are most likely perceived as ‘too skinny’.31
Posters are a successful pediatric public health education tool. For example, a poster for health departments educating on risks of human papilloma virus increased the probability of vaccination.32 Posters encouraging conversations with providers have been used to support BMI screening33 and have been suggested as a way to ‘visualize’ healthy weight.31 Additionally, posters depicting color-coded BMI zones have been shown to promote dialogue about healthy weight between parents and WIC nutritionists.34 Despite the abundance of educational materials with health promoting and obesity prevention messages, very few studies have examined their effectiveness in clinical settings. Therefore, we aimed to assess whether an exam room educational poster addressing healthy weight and healthy lifestyle behaviours was acceptable to parents, prompted communication with providers, or improved accuracy of parent’s perception of their child’s weight status. We also aimed to assess whether these outcomes varied by child race/ethnicity or weight status, parent education, or household income.
2 |. PATIENTS AND METHODS
2.1 |. Study design and participants
This was a cross-sectional randomized controlled trial performed at seven clinics in the United States located in Winston-Salem, North Carolina (N = 2); Durham, North Carolina (N = 2); Bellevue, Washington; Huntsville, Alabama; and Crestview Hills, Kentucky. Clinic types included private practice, hospital affiliated, resident continuity clinic, and public health center. Clinic exam rooms were randomized to either intervention (posters were hung in prominent places of the exam room) or control (no posters). Clinics who see both English and Spanish speaking patients hung posters in both English and Spanish (N = 4), and clinics with only English-speaking patients chose to have just English posters hung (N = 3). The number of total exam rooms (and how many of those exam rooms had an intervention poster) varied by clinic: 6 total rooms (4 rooms with intervention posters), 8 (4 intervention), 12 (6 intervention), 13 (6 intervention), 18 (8 intervention), 19 (8 intervention) and 21 (11 intervention). Randomization for rooms at all sites was performed by a single investigator (CLB) using a random number generator with values ranging from 0 to 1. Providers saw patients in their usual rooms and were not randomized.
Parent-child dyads were recruited from participating clinics if the child was 3 to 8 years old and coming to clinic for a preventive health services visit, and if the parent spoke English or Spanish and could complete a written survey. Exclusion criteria included parent age <18 years or the child having a diagnosed medical condition that affects weight gain or growth such as failure to thrive, congenital heart defect and so on. At the conclusion of the visit, the provider determined whether the child and parent met inclusion criteria. Parents of eligible children were surveyed in English or Spanish according to preferred language about topics including healthy lifestyle behaviours, communication with their provider and their perception of their child’s weight status, as described in detail below. Data collection occurred between 06/12/2017 and 4/27/2018. This study was approved by the institutional review board (IRB) at Wake Forest University as well as the IRB at Duke University. Other sites used a reliance agreement with the Wake Forest IRB (University of Alabama at Birmingham) or an individual investigator agreement with the Wake Forest IRB (all other sites). This study was registered on ClinicalTrials.gov, #NCT03128112.
2.2 |. Study procedures
The poster was developed by content experts with goals of (a) displaying what young children of a healthy weight look like, (b) encouraging parents to ask their child’s doctor about their child’s weight status and (c) introducing healthy lifestyle behaviours that would apply to all families. Poster design was refined after cognitive interviews with five parents. The poster was translated into Spanish by a certified translator and then back translated into English by a separate translator. The translation and back-translation were reviewed by multiple native Spanish speakers as well to ensure accuracy. Posters in English and Spanish (Figure 1) included pictures of three healthy weight children, a color-coded growth chart stating that the green zone is a healthy weight, the statement that ‘it is normal for 3-8 year old children to look “skinny”’, encouragement to ask their doctor if their child has a healthy BMI, and a display of 5-3-2-1-0 healthy lifestyle behaviours. The 53 210 message is an adaptation of the 5210 message that was used in North Carolina’s Eat Smart Move More campaign and includes messaging about eating 5 servings of fruits and vegetables, eating 3 meals a day (and more meals prepared at home), watching less than 2 hours of screen time, getting 1 hour of physical activity and drinking 0 sugary beverages.35 The three message was added to encourage families to not skip meals and to eat as many meals as possible at home instead of eating out. The posters were printed, laminated and displayed in each intervention examination room in a location prominent to parents waiting for care (Figure 1). Providers were notified of the study but were not were not asked to change their usual clinical care or given any training on utilizing the poster.
FIGURE 1.
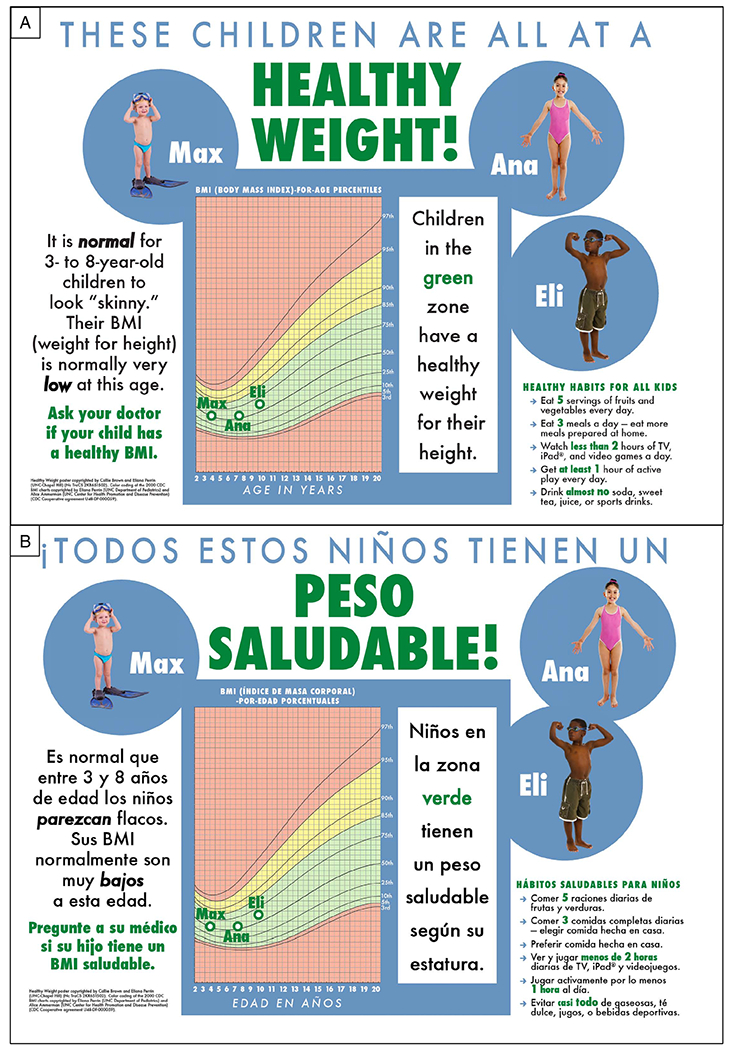
Posters depicting healthy weight children, in English (A) and Spanish (B)
Nursing staff measured vital signs and placed families in an exam room per usual clinical protocol. Nursing or study staff recorded the provider that was seeing the patient, exam room they were in, and their measured height and weight. After the completion of their visit, providers offered parents a short questionnaire. The first page of the questionnaire explained the voluntary nature of the study and informed parents that completion of the questionnaire implied consent. The provider then left the family to complete the survey independently. Parents who completed the questionnaire were given a small incentive.
2.3 |. Study instruments and measurements
After the completion of their visit we assessed all parents’ perception of their children’s weight by asking ‘Right now, do you think your child is: very underweight, underweight, at a healthy weight, overweight, or obese?’ Parents were also asked ‘Did you ask your doctor today if your child is at a healthy weight?’ and ‘Did your pediatrician today show you a chart with your child’s body mass index (BMI)?’ Parents reported whether pediatricians discussed healthy lifestyle behaviours with them and/or their child, including advice about eating, physical activity or screen time. Parents’ self-reported demographics including the child’s sex, Hispanic ethnicity, and race (Asian, Black, White, Other), the parent’s highest level of completed education (<sixth grade, some middle school, some high school, high school graduate, associate degree, bachelor’s degree or Master’s degree or higher). Parents also estimated how long they waited in the exam room to see their pediatrician for that visit.
Parents in an intervention room were additionally asked whether they asked their child’s doctor about their weight status because of the poster on the wall and whether the pediatrician used the poster to teach about healthy lifestyle behaviours, including weight, eating, physical activity or screen time. Parents then were asked their opinion about the poster with response options of strongly agree, agree, disagree, or strongly disagree. They reported whether they ‘liked seeing a poster with pictures and information like this in my doctor’s office’ and whether the poster helped them to understand ‘what a healthy weight looks like for children of different ages’, ‘healthy advice about eating or exercise’ and ‘whether my child is a healthy weight’. Finally, parents reported whether the poster helped them to have a conversation with the doctor about their child’s weight, eating, physical activity, screen time or other.
2.4 |. Statistical analysis
The child’s BMI was calculated according to their measured height and weight during the exam and standardized CDC age- and sex-specific percentiles.36 We compared parents’ assessment of their children’s weight status (underweight, healthy weight and overweight/obese) with the children’s measured weight category (underweight, healthy weight and overweight/obese) and categorized as accurate or inaccurate. Because there were so few children who were underweight and because the factors that might affect the weight status perception of their child who is underweight is likely very different than that of children who are at a healthy weight or have overweight/obesity, we opted to exclude children who were underweight from this analysis (N = 37). We also excluded children with any missing data (N = 136, mostly with missing weight or height). Using a two-sample test for proportions and anticipating a 5% improvement in parental perception, we would require 700 patients to detect this difference with a power of 90%.
We used Pearson’s chi-square tests and T-tests to compare characteristics by intervention status, weight perception accuracy, and whether parents asked their doctor about the child’s weight status. Variables that were significant in the bivariate analysis with a P < .2 were included in the multivariate analysis. Separate logistic regression analyses were performed examining whether intervention status was associated with outcomes of whether parents asked the physician about their child’s weight status and accuracy of weight perception, adjusting for child age, sex, race/ethnicity and weight status and clustering by exam room (the level of randomization). Of note, analyses were also performed with exam room as a covariate and excluding exam room from the multivariate analysis and results were not significantly different. We also performed sensitivity analyses examining whether these outcomes varied by child race/ethnicity or weight status, parent education or household income.
3 |. RESULTS
3.1 |. Study sample and patient characteristics
Of the 1029 eligible parents who were approached about the study, 965 participated, a response rate of 94% (Figure 2). Children came from diverse backgrounds in respect to race/ethnicity (37% white, 38% Black and 30% Hispanic) and annual household income (30% < $20 000/year, 23% $20 000-$39 999, 13% $40 000-$59 999, 13% $60 000-$99 999 and 22% ≥ $60 000/year). One-quarter (24%) of parents had less than a high-school degree, 30% graduated from high-school, 28% had an associate’s or bachelor’s degree and 19% had a master’s degree or higher. Children had a mean age of 5.6 years (SD 2.0), and 50% were male. Almost two-thirds (64%) of children were healthy weight, 15% had overweight and 17% had obesity. Demographics did not differ by intervention status (Table 1).
FIGURE 2.
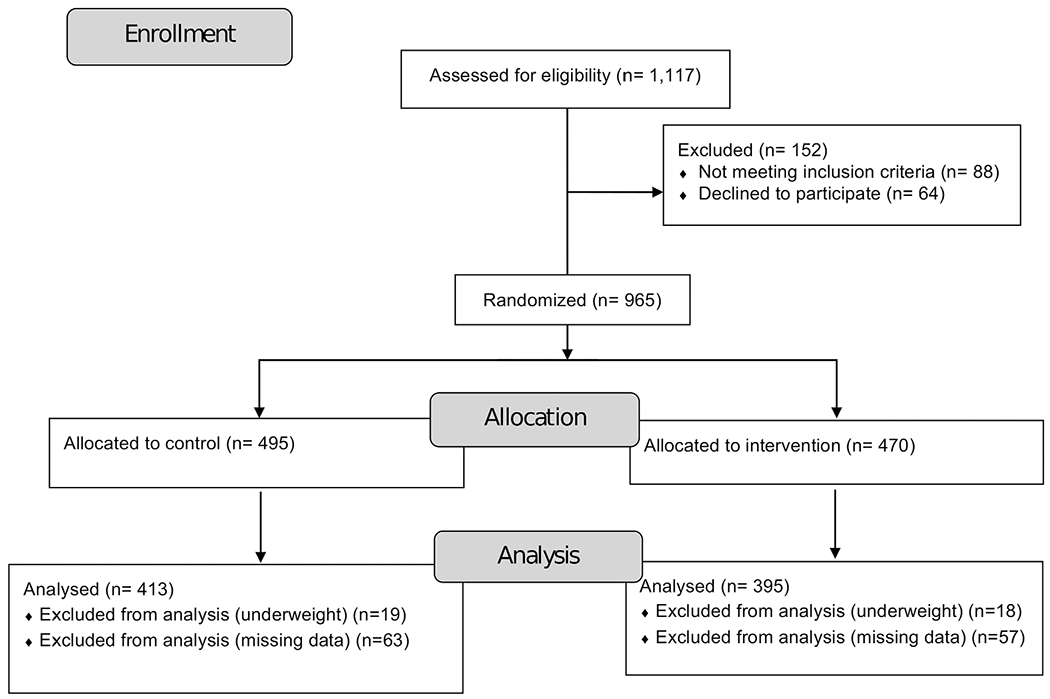
Consort flow diagram
TABLE 1.
Participant demographics by intervention status
| Total N (%) or mean (SD) N = 965 | Control N (%) or mean (SD) N = 495 | Intervention N (%) or mean (SD) N = 470 | P-valuea | |
|---|---|---|---|---|
| Age in years (N = 862) | 5.6 (2.0) | 5.5 (1.9) | 5.6 (2.0) | .5 |
|
| ||||
| Male (N = 955) | 477 (50.1%) | 243 (49.6%) | 234 (50.5%) | .8 |
|
| ||||
| Parent education (N = 933) | .6 | |||
| <Sixth | 56 (6.0%) | 26 (5.4%) | 30 (6.7%) | |
| Some middle | 72 (7.7%) | 41 (8.5%) | 31 (6.9%) | |
| Some high | 92 (9.9%) | 45 (9.4%) | 47 (10.4%) | |
| HS grad | 271 (29.1%) | 146 (30.4%) | 125 (27.8%) | |
| Associate’s degree | 85 (9.1%) | 49 (10.2%) | 36 (8.0%) | |
| Bachelor’s degree | 179 (19.2%) | 86 (17.9%) | 93 (20.7%) | |
| Master’s or higher | 176 (18.9%) | 88 (18.3%) | 88 (19.6%) | |
|
| ||||
| Household income ($) (N = 922) | .4 | |||
| <20 000 | 272 (29.6%) | 148 (31.2%) | 124 (27.9%) | |
| 20 000-39 999 | 212 (23.0%) | 111 (23.4%) | 101 (22.7%) | |
| 40 000-59 999 | 115 (12.5%) | 63 (13.3%) | 52 (11.7%) | |
| 60 000-99 999 | 118 (12.9%) | 52 (11.0%) | 66 (14.8%) | |
| >100 000 | 203 (22.1%) | 101 (21.3%) | 102 (22.9%) | |
|
| ||||
| Language: English (N = 960) | 760 (79.3%) | 379 (77.4%) | 381 (81.4%) | .1 |
|
| ||||
| Race/ethnicity (N = 945) | .4 | |||
| White | 348 (36.9%) | 170 (35.1%) | 178 (38.8%) | |
| Black | 268 (28.4%) | 135 (27.9%) | 133 (29.0%) | |
| Hispanic | 282 (29.9%) | 153 (31.6%) | 129 (28.1%) | |
| Other | 45 (4.8%) | 26 (5.4%) | 19 (4.1%) | |
|
| ||||
| Waiting time in examination room during visit (N = 619) | .6 | |||
| <10 | 294 (47.7%) | 146 (47.1%) | 148 (48.2%) | |
| 10-<20 | 198 (32.1%) | 98 (31.6%) | 100 (32.6%) | |
| 20-<30 | 50 (8.1%) | 23 (7.4%) | 27 (8.8%) | |
| 30+ | 75 (12.2%) | 43 (13.9%) | 32 (10.4%) | |
|
| ||||
| Child BMI categorical (N = 839) | .9 | |||
| Underweight | 37 (4.4%) | 19 (4.4%) | 18 (4.4%) | |
| Healthy Weight | 538 (64.3%) | 273 (63.5%) | 265 (65.1%) | |
| Overweight | 124 (14.8%) | 66 (15.4%) | 58 (14.3%) | |
| Obese | 138 (16.5%) | 72 (16.7%) | (16.2%) | |
|
| ||||
| Child BMI z-score (N = 839) | 0.46 (1.2) | .49 (1.2) | .42 (1.2) | .4 |
|
| ||||
| Parent weight perception (N = 833) | .7 | |||
| Underweight | 45 (4.7%) | 24 (4.9%) | 21 (4.5%) | |
| Healthy Weight | 801 (83.8%) | 407 (82.9%) | 394 (84.7%) | |
| Overweight or obese | 110 (11.5%) | 60 (12.2%) | 50 (10.8%) | |
|
| ||||
| Accuracy of weight perception (N = 833) | .9 | |||
| Underestimated | 205 (24.7%) | 106 (24.8%) | 99 (24.6%) | |
| Correct | 596 (71.7%) | 308 (72.0%) | 288 (71.5%) | |
| Overestimated | 30 (3.6%) | 14 (3.3%) | 16 (4.0%) | |
P-value denotes difference between control and intervention by Pearson’s chi-squared or t-test.
3.2 |. Parental acceptability of the poster
Of the parents who saw the poster (N = 470), almost all (97%) agreed (agree or strongly agree) that they liked seeing this poster with pictures and information like this in their doctor’s office. The vast majority reported that the poster helped them understand what a healthy weight looks like for children of different ages (96%), understand healthy advice about eating or exercise (94%) and understand whether their child is at a healthy weight (94%).
3.3 |. Communication with pediatrician
Parents in a room with a poster were significantly more likely to report being shown a chart with their child’s BMI (85% vs 75%, respectively, P = .001). About half of parents (52%) asked their child’s pediatrician about their child’s weight status, and this was not significantly different between intervention and control (53% vs 48%, respectively, P = .2). Whether the pediatrician discussed healthy lifestyle behaviours, weight, eating, physical activity or screen time with the parent did not vary by intervention status (Table 2). When adjusting for key covariates in multivariate analysis, the intervention remained associated with being shown a growth chart (OR 1.87, 95% CI 1.06-3.30) and unassociated with asking the child’s physician about their weight status (OR 1.22, 95% CI 0.85-1.74).
TABLE 2.
Communication with parents by intervention status
| Total N(%) | Control N(%) | Intervention N(%) | P-value a | |
|---|---|---|---|---|
| Parent asked doctor about child’s weight status | 381 (50.2%) | 183 (47.9%) | 198 (52.5%) | .2 |
|
| ||||
| Provider showed a growth chart | 592 (79.7%) | 282 (74.8%) | 310 (84.7%) | .001 |
|
| ||||
| Provider discussed any healthy lifestyle behaviours | 651 (86.2%) | 320 (84.7%) | 331 (87.8%) | .2 |
| Weight | 546 (71.9%) | 273 (71.5%) | 273 (72.4%) | .7 |
| Eating | 471 (62.1%) | 231 (60.5%) | 240 (63.7%) | .4 |
| Physical activity | 267 (35.2%) | 133 (34.8%) | 134 (35.5%) | .8 |
P-value denotes difference between control and intervention status by Pearson’s chi-squared.
3.4 |. Perception of child’s weight status
Parents overwhelmingly perceived their child as healthy weight (83.8%) and rarely as very underweight (0.3%), underweight (4.4%), overweight (10.9%) or obese (0.6%). When compared with the child’s measured weight status, 71.7% of parents accurately assessed their child’s weight status, 24.7% underestimated and 3.6% overestimated. When children who were underweight were excluded, 73.9% of parents accurately assessed their child’s weight status, 25.8% underestimated and 0.3% overestimated. Accuracy of parent weight perception did not differ between intervention and control subjects (73.8% vs 74.1%, respectively, P = .9). When adjusting for key covariates in multivariate analysis the intervention remained unassociated with accuracy of parental weight perception (OR 0.80, 95% CI 0.48-1.32).
3.5 |. Sensitivity analyses
We also aimed to assess whether these outcomes varied by child race/ethnicity or weight status, parent education, or household income. Among participants of Hispanic ethnicity, the intervention was associated with increased odds of asking the child’s physician about their weight status (OR 2.85, 95% CI 1.22-6.65) and was not associated with being shown a growth chart (OR 1.62, 95% CI 0.82-3.24) or accuracy of parental weight perception (OR 0.73, 95% CI 0.31-1.73). Among children with overweight or obesity, the intervention was associated with increased odds of asking the child’s physician about their weight status (OR 1.84, 95% CI 1.07-3.15) and was not associated with being shown a growth chart (OR 1.88, 95% CI 0.98-3.63) or accuracy of parental weight perception (OR 0.90, 95% CI 0.49-1.65). Among parents with less than a high school degree the intervention was not associated with asking the child’s physician about their weight status (OR 1.43, 95% CI 0.52-3.89), being shown a growth chart (OR 1.42, 95% CI 0.58-3.53), or accuracy of parental weight perception (OR 1.13, 95% CI 0.61-2.10). Among families with a household income <$60 000 per year, the intervention was associated with increased odds of being shown a growth chart (OR 2.07, 95% CI 1.21-3.53) and was not associated with asking the child’s physician about their weight status (OR 1.39, 95% CI 0.91-2.14) or accuracy of parental weight perception (OR 0.84, 95% CI 0.56-1.24).
No harms or unintended effects were reported by participants or noted by the study team for either group.
4 |. DISCUSSION
In this randomized, controlled trial, our educational exam room poster was well-liked by a diverse group of parents, and contributed to their reported understanding of weight status and healthy lifestyle behaviours. When providers and families were in a room with a poster, parents were more likely to report that the provider showed them a growth chart, compared to parents in a room without a poster. However, parents who saw the poster were not any more likely to ask their provider about their child’s weight status nor were they more likely to have an accurate perception of their children’s weight when compared to parents in a room without a poster. Sensitivity analyses revealed that parents who were Hispanic or had a child who had overweight or obesity were more likely to ask the physician about their child’s weight status, revealing that these posters may have greater impact with these populations.
Our finding that 25% of parents inaccurately perceived their child’s weight status and that most of these misperceptions were underestimations (ie, perceiving a child who was overweight as at a healthy weight or a child who was at a healthy weight as underweight), is similar to previous research.10,22 Existing literature on the association of weight perception and future weight gain is mixed. Some studies have shown that children whose parents underestimate their weight status gain more weight over time than children whose parents correctly recognize their weight status15,16,19,20,37,38; however, other studies have demonstrated conflicting results.22 In adults, correct recognition of overweight is associated with increased weight loss attempts but increased weight gain over time.39 Therefore, we posit that providers should spend their time counselling families concentrating on growth with respect to health and health behaviours and reassuring families in the BMI dip about their children looking leaner rather than focusing on the accurate understanding of overweight or obese terminology.
Parents who saw the poster were not any more likely to ask their provider about their child’s weight status than parents who did not see the poster. It is possible that these parents did not want to initiate a conversation with their child’s provider about their child’s weight status because of concern about weight bias or stigma. Children with obesity often experience weight-based teasing,40,41 and parents may want to avoid these conversations in front of their children. Children and adults with obesity also experience weight bias and stigma in the healthcare setting,40,42 so it is also possible that parents are hoping to avoid these manifestations during the encounter. Future qualitative work is necessary to understand what factors influence whether parents want to discuss their child’s weight status with the provider. It is important that providers maintain a focus on health and healthy lifestyle behaviours to help destigmatize obesity and reduce the risk of future eating disorders.43
This study is strengthened by its large sample size and its diversity with regard to clinic location and type and participant race and socioeconomic status, which improves generalizability. Limitations include that parental weight perception was asked with a single question and that all data about communication with the physician was based on self-report by the parent. We do not know whether providers used motivational interviewing to counsel families about weight nor whether families set a specific healthy lifestyle goal at the conclusion of the visit or were more inclined to follow healthy lifestyle advice in their day-to-day lives. Additionally, it is not known in which direction desirability bias might point, as the desire for a healthy weight can mean different appearances to different people. It is also possible that parents may have been concerned about stigmatizing their child about their weight status, and hesitated to ask the provider in order to protect their child; this was not assessed by our survey. As surveys were collected as part of a routine clinic visit in a variety of real-world settings, height and weight were only measured once by clinic staff, and about 14% of surveys had missing data. Finally, no questions were asked of the pediatrician as to whether the posters aided counselling. Future work should examine whether posters that are appreciated and reportedly aid in understanding actually contribute to behaviour change and the effects of educational tools of novel formats (such as videos) on provider or parent behaviours and in other types of offices, for example, in WIC offices.
During early childhood, the primary care provider is uniquely positioned to deliver anticipatory guidance about weight and appropriate growth that may impact the child’s long-term growth trajectory. Throughout this time children see their primary care providers frequently and parents may be especially receptive to behaviour modifcations.44 Exam room posters are a novel way to educate parents about healthy weight perception and make good use of downtime while waiting to see their provider by delivering messages that mirror anticipatory guidance given by providers. Posters depicting healthy weight children and color-coded BMI charts may be especially useful and appreciated during the adiposity nadir, when parents may be most concerned their child is underweight.
5 |. CONCLUSION
This educational exam room poster may represent a low-cost way for providers and public health professionals to introduce ideas about healthy growth and lifestyle behaviours in a sensitive and family-desired way. Parents liked the presence of a visual aid to help them understand healthy eating and activity advice; even if the poster itself does not change the parent’s perception of their child’s weight status, it may be a useful supplement to provider’s counseling. Providers showed parents a growth chart more commonly when in rooms where the poster was displayed than in those where it was not displayed, revealing that these exam room posters may be changing provider behaviour. This deserves further exploration as a novel strategy to improve counselling and drive healthy behaviour change.
ACKNOWLEDGEMENTS
The authors are extremely grateful to the pediatric practices and providers who facilitated data collection: Downtown Health Plaza (Laurie Albertini, Winston-Salem, NC), Ford Simpson Lively and Rice Pediatrics (Carrie Erickson, Winston-Salem, NC), Pediatric Associates of Northern Kentucky (Christopher Bolling, Crestview Hills, KY), Eastgate Public Health Center (Nancy Danoff, Bellevue, WA), University of Alabama Birmingham Health Center Huntsville (Gina White; Huntsville, AL), Duke Children’s Primary Care Brier Creek (Martha Snyder; Raleigh, NC), and Duke Children’s Primary Care Roxboro Street (Elizabeth Landolfo; Durham, NC). The authors would also like to thank Javier Rodriguez at Duke Children’s Primary Care for his assistance with translation. The project described was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR001420. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
CONFLICT OF INTEREST
Drs. Callie Brown and Eliana Perrin have copyright rights for the poster.
REFERENCES
- 1.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. Jama. 2016;315(21):2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999-2016. Pediatrics. 2018;141(3):e20173459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(Suppl. 2):518–525. [PubMed] [Google Scholar]
- 4.Reilly JJ, Methven E, McDowell ZC, et al. Health consequences of obesity. Arch Dis Child. 2003;88(9):748–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Office of the Surgeon General. The Surgeon General’s Call to Action to Prevent and Decrease Overweight and Obesity; 2001. [PubMed] [Google Scholar]
- 6.Koplan JP, Liverman CT, Kraak VI. Preventing childhood obesity: health in the balance: executive summary. J Am Diet Assoc. 2005;105(1):131–138. [DOI] [PubMed] [Google Scholar]
- 7.Kumanyika SK, Obarzanek E, Stettler N, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on epidemiology and prevention, interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science). Circulation. 2008; 118(4):428–464. [DOI] [PubMed] [Google Scholar]
- 8.Barlow SE, Expert C. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. [DOI] [PubMed] [Google Scholar]
- 9.Doolen J, Alpert PT, Miller SK. Parental disconnect between perceived and actual weight status of children: a metasynthesis of the current research. J Am Acad Nurse Pract. 2009;21(3):160–166. [DOI] [PubMed] [Google Scholar]
- 10.Lundahl A, Kidwell KM, Nelson TD. Parental underestimates of child weight: a meta-analysis. Pediatrics. 2014;133(3):e689–e703. [DOI] [PubMed] [Google Scholar]
- 11.Parry LL, Netuveli G, Parry J, Saxena S. A systematic review of parental perception of overweight status in children. J Ambul Care Manage. 2008;31(3):253–268. [DOI] [PubMed] [Google Scholar]
- 12.Rietmeijer-Mentink M, Paulis WD, Middelkoop M, Bindels PJE, Wouden JC. Difference between parental perception and actual weight status of children: a systematic review. Matern Child Nutr. 2013;9(1):3–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Towns N, D’Auria J. Parental perceptions of their child’s overweight: an integrative review of the literature. J Pediatr Nurs. 2009;24(2):115–130. [DOI] [PubMed] [Google Scholar]
- 14.Perrin EM, Skinner AC, Steiner MJ. Parental recall of doctor communication of weight status: national trends from 1999 through 2008. Arch Pediatr Adolesc Med. 2012;166(4):317–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rhee KE, De Lago CW, Arscott-Mills T, Mehta SD, Davis RK. Factors associated with parental readiness to make changes for overweight children. Pediatrics. 2005;116(1):e94–e101. [DOI] [PubMed] [Google Scholar]
- 16.Wake M, Salmon L, Waters E, Wright M, Hesketh K. Parent-reported health status of overweight and obese Australian primary school children: a cross-sectional population survey. Int J Obes Relat Metab Disord. 2002;26(5):717–724. [DOI] [PubMed] [Google Scholar]
- 17.Lampard AM, Byrne SM, Zubrick SR, Davis EA. Parents’ concern about their children’s weight. Int J Pediatr Obes. 2008;3(2):84–92. [DOI] [PubMed] [Google Scholar]
- 18.Duncan DT, Hansen AR, Wang W, Yan F, Zhang J. Change in misperception of Child’s body weight among parents of American pre-school children. Child Obes. 2015;11(4):384–393. [DOI] [PubMed] [Google Scholar]
- 19.Moore LC, Harris CV, Bradlyn AS. Exploring the relationship between parental concern and the management of childhood obesity. Matern Child Health J. 2012;16(4):902–908. [DOI] [PubMed] [Google Scholar]
- 20.Soto C, White JH. School health initiatives and childhood obesity: BMI screening and reporting. Policy Polit Nurs Pract. 2010;11(2):108–114. [DOI] [PubMed] [Google Scholar]
- 21.Eckstein KC, Mikhail LM, Ariza AJ, Thomson JS, Millard SC, Binns HJ. Parents’ perceptions of their child’s weight and health. Pediatrics. 2006;117(3):681–690. [DOI] [PubMed] [Google Scholar]
- 22.Robinson E, Sutin AR. Parental perception of weight status and weight gain across childhood. Pediatrics. 2016;137:e20153957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maynard LM, Galuska DA, Blanck HM, Serdula MK. Maternal perceptions of weight status of children. Pediatrics. 2003;111(Supplement 1):1226–1231. [PubMed] [Google Scholar]
- 24.Robinson E, Sutin AR. Parents’ perceptions of their children as overweight and children’s weight concerns and weight gain. Psychol Sci. 2017;28(3):320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wake M, Kerr JA, Jansen PW. Child BMI over time and parent-perceived overweight. Pediatrics. 2018;142(6):e20173985. [DOI] [PubMed] [Google Scholar]
- 26.Vuorela N, Saha MT, Salo MK. Parents underestimate their childs overweight. Acta Paediatr. 2010;99(9):1374–1379. [DOI] [PubMed] [Google Scholar]
- 27.Krebs NF, Jacobson MS. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112(2):424–430. [DOI] [PubMed] [Google Scholar]
- 28.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 2002; 11(246):1–190. [PubMed] [Google Scholar]
- 29.Oettinger MD, Finkle JP, Esserman D, et al. Color-coding improves parental understanding of body mass index charting. Acad Pediatr. 2009;9(5):330–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perrin EM, Jacobson Vann JC, Benjamin JT, Skinner AC, Wegner S, Ammerman AS. Use of a pediatrician toolkit to address parental perception of children’s weight status, nutrition, and activity behaviors. Acad Pediatr. 2010;10(4):274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perrin EM. Respecting cultural values of toddler weight perception while discouraging parental overfeeding: comment on “maternal perceptions of toddler body size”. Arch Pediatr Adolesc Med. 2012;166(5):422–423. [DOI] [PubMed] [Google Scholar]
- 32.Cates JR, Diehl SJ, Crandell JL, Coyne-Beasley T. Intervention effects from a social marketing campaign to promote HPV vaccination in preteen boys. Vaccine. 2014;32(33):4171–4178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gee S, Chin D, Ackerson L, Woo D, Howell A. Prevalence of childhood and adolescent overweight and obesity from 2003 to 2010 in an integrated health care delivery system. J Obes. 2013;2013:417907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Herrera J, Lockner D, Kibbe D, Marley SC, Trowbridge F, Bailey A. Innovative tools help counselors discuss childhood obesity with parents. Childhood Obes. 2013;9(2):144–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rogers VW, Hart PH, Motyka E, Rines EN, Vine J, Deatrick DA. Impact of Let’s go! 5-2-1-0: a community-based, multisetting childhood obesity prevention program. J Pediat Psychol. 2013;38(9):1010–1020. [DOI] [PubMed] [Google Scholar]
- 36.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;(314):1–27. [PubMed] [Google Scholar]
- 37.Rhee KE, Lumeng JC, Appugliese DP, Kaciroti N, Bradley RH. Parenting styles and overweight status in first grade. Pediatrics. 2006;117(6):2047–2054. [DOI] [PubMed] [Google Scholar]
- 38.Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. 2002;76(3):653–658. [DOI] [PubMed] [Google Scholar]
- 39.Haynes A, Kersbergen I, Sutin A, Daly M, Robinson E. A systematic review of the relationship between weight status perceptions and weight loss attempts, strategies, behaviours and outcomes. Obes Rev. 2018;19(3):347–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17(5):941–964. [DOI] [PubMed] [Google Scholar]
- 41.Schvey NA, Marwitz SE, Mi SJ, et al. Weight-based teasing is associated with gain in BMI and fat mass among children and adolescents at-risk for obesity: a longitudinal study. Pediatr Obes. 2019;14(10):e12538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Golden NH, Schneider M, Wood C. Preventing obesity and eating disorders in adolescents. Pediatrics. 2016;138(3):e20161649. [DOI] [PubMed] [Google Scholar]
- 44.Gillman MW, Ludwig DS. How early should obesity prevention start? New Eng J Med. 2013;369(23):2173–2175. [DOI] [PubMed] [Google Scholar]


