Abstract
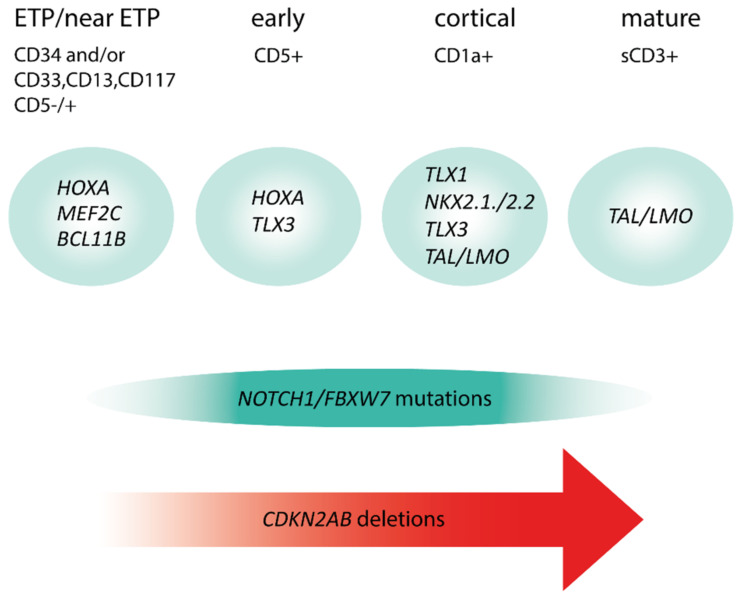
T-cell acute lymphoblastic leukemias (T-ALL) are immature lymphoid tumors localizing in the bone marrow, mediastinum, central nervous system, and lymphoid organs. They account for 10–15% of pediatric and about 25% of adult acute lymphoblastic leukemia (ALL) cases. It is a widely heterogeneous disease that is caused by the co-occurrence of multiple genetic abnormalities, which are acquired over time, and once accumulated, lead to full-blown leukemia. Recurrently affected genes deregulate pivotal cell processes, such as cycling (CDKN1B, RB1, TP53), signaling transduction (RAS pathway, IL7R/JAK/STAT, PI3K/AKT), epigenetics (PRC2 members, PHF6), and protein translation (RPL10, CNOT3). A remarkable role is played by NOTCH1 and CDKN2A, as they are altered in more than half of the cases. The activation of the NOTCH1 signaling affects thymocyte specification and development, while CDKN2A haploinsufficiency/inactivation, promotes cell cycle progression. Among recurrently involved oncogenes, a major role is exerted by T-cell-specific transcription factors, whose deregulated expression interferes with normal thymocyte development and causes a stage-specific differentiation arrest. Hence, TAL and/or LMO deregulation is typical of T-ALL with a mature phenotype (sCD3 positive) that of TLX1, NKX2-1, or TLX3, of cortical T-ALL (CD1a positive); HOXA and MEF2C are instead over-expressed in subsets of Early T-cell Precursor (ETP; immature phenotype) and early T-ALL. Among immature T-ALL, genomic alterations, that cause BCL11B transcriptional deregulation, identify a specific genetic subgroup. Although comprehensive cytogenetic and molecular studies have shed light on the genetic background of T-ALL, biomarkers are not currently adopted in the diagnostic workup of T-ALL, and only a limited number of studies have assessed their clinical implications. In this review, we will focus on recurrent T-ALL abnormalities that define specific leukemogenic pathways and on oncogenes/oncosuppressors that can serve as diagnostic biomarkers. Moreover, we will discuss how the complex genomic profile of T-ALL can be used to address and test innovative/targeted therapeutic options.
Keywords: T-ALL, genomic profile, molecular-cytogenetic markers
1. Introduction
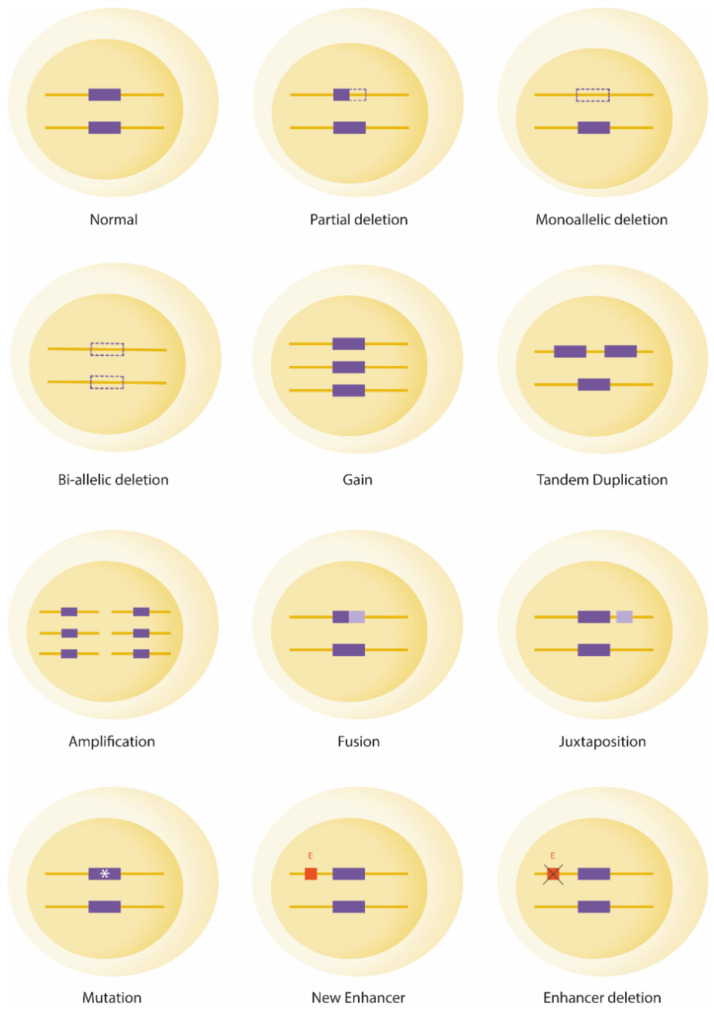
T-cell acute lymphoblastic leukemia (T-ALL) represents 15% of pediatric and 25% of adult ALL cases. Historically considered an aggressive subtype of ALL, new pediatric-oriented protocols, in adults, and intensified treatments, based on the persistence of minimal residual disease (MRD) in both children and adults, have greatly improved patient outcomes [1]. The genetic background of T-ALL is widely heterogeneous as a huge number of oncogenes and oncosuppressors, often intersecting on a few pivotal cellular processes, have been associated with the onset and/or progression of the leukemia. Furthermore, alternative molecular mechanisms can cause gene deregulation (Figure 1). Hence, the molecular cytogenetic diagnosis of T-ALL is not currently adopted, as a unifying test able to pick up the large spectrum of the involved genes and the alternative molecular mechanisms underlying their deregulation, is not available for clinical purposes. Therefore, although our knowledge on the genetic background of T-ALL has been greatly elucidated in the last decade, and specific leukemogenic pathways have been identified, the clinical impact of this bio-molecular information is still largely unknown. The majority of available studies focused on individual markers, sometimes yielding misleading results, as they overlooked the complexity and heterogeneity of the disease. On the other hand, when more than one T-ALL associated abnormality is taken into account, a strong predictive value of the leukemia genomic profile emerged. If it is combined with MRD determination, a significant improvement of risk assessment in both pediatric and adult patients has been obtained [2,3].
Figure 1.
Schematic representation of genomic mechanisms of gene deregulation in T-ALL. Dotted lines: deletion; *: mutation; E: enhancer.
This review will focus on the most relevant biological aspects of T-ALL, describing how these leukemias can be classified into relevant genetic entities closely related to the stage of immunophenotypic T-cell differentiation. In addition, we will report on the incidence and distribution of recurrent abnormalities that can be regarded as putative prognostic and/or actionable targets.
2. Driver Oncogenic Events: Classification into Type A and Type B Abnormalities
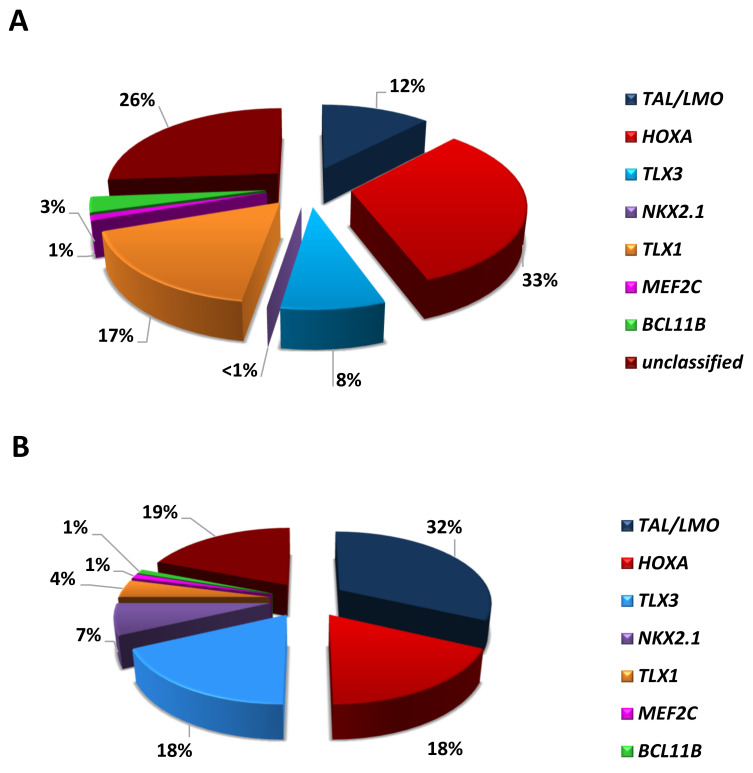
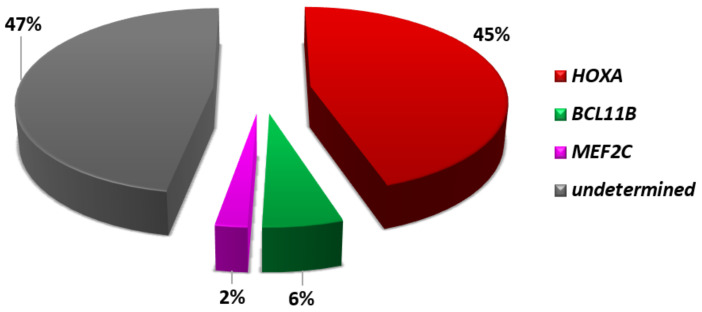
According to their reciprocal distribution and effects of their deregulation, T-ALL-related abnormalities can be distinguished as type A and type B [4]. Type A abnormalities are mutually exclusive and cause the up-regulation of (onco)genes coding for transcription factors critical in hematopoiesis and/or T-cell development, maturation, and differentiation. These genetic events mark distinct subgroups, i.e., TAL/LMO, HOXA, TLX3, TLX1, NKX2-1/2-2, MEF2C, allowing the molecular classification of at least 70% of T-ALL cases, with different distribution in children and adults (Figure 2) [5,6,7,8,9]. Type B abnormalities, on the other hand, involve genes that code for different protein families, such as epigenetic factors, tyrosine kinases, ribosomal proteins, and proteins that belong to signaling pathways. They are distributed across all genetic subgroups, albeit not randomly, as privileged associations occur between primary and secondary genetic changes. Thus, concurrent primary and secondary events trace unique leukemogenic pathways that rely on specific cooperative activities.
Figure 2.
Distribution of the main genetic subgroups in T-ALL of: (A) adults and (B) children [7,8,9,10].
3. Mature T-ALL and the TAL/LMO Transcriptional Complex
First identified by Ferrando A et al. [5], TAL1 overexpression characterizes 30–45% of pediatric and 10–15% of adult T-ALL (Figure 2). These T-ALL harbor chromosomal rearrangements, or alternatively noncoding sequence mutations, which cause the activation of members of the basic helix-loop-helix (bHLH) family of transcription factors (TAL1 and TAL2) and/or of the LIM-only domain (LMO1, LMO2, and LMO3) proteins [8,11,12,13]. TAL and LMO proteins belong to the same transcriptional complex and are frequently co-deregulated in T-ALL, suggesting a cooperative role in T-leukemogenesis. Consistent with this model, the oncogenic activity of LMO1 or LMO2 is markedly enhanced by TAL1, in transgenic mice [14,15]. TAL and LMO leukemogenic activity, demonstrated in in vitro and in vivo studies, was the consequence of the altered expression of their downstream targets, such as TRIB2, NKX3.1, RUNX1, GATA3, and MYB [16,17].
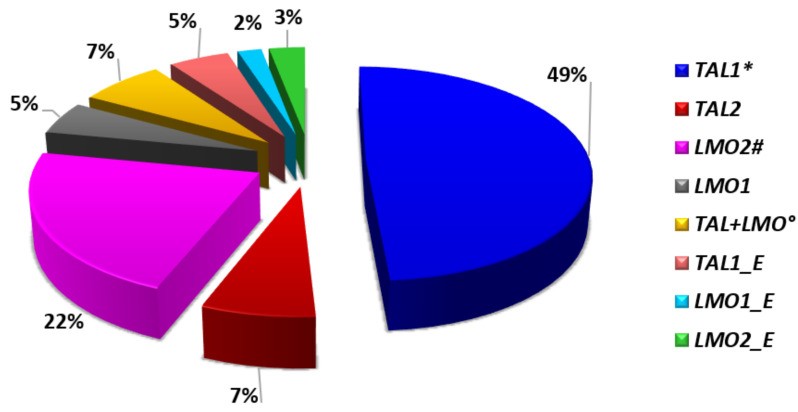
Due to the aforementioned characteristics, T-ALL with abnormalities of TAL and/or LMO genes (Figure 3), are typically grouped together into the TAL/LMO category as they share the same gene expression signature. Their immunophenotype mostly resemble mature T-cell development arrest (sCD3 positive), and while showing a low incidence of NOTCH1 mutations (~40% of cases) (Figure 4), have a privileged association with PTEN inactivation, 6q14-q16 deletions, and MYC translocations, all behaving as poor prognostic markers [8,18,19].
Figure 3.
TAL/LMO genetic subgroup: Frequency of TAL and/or LMO rearrangements [8,9]. * In this group, including all rearrangements of TAL1, 47% of cases are represented by STIL-TAL1 fusions; °TAL1+LMO1, or TAL1+LMO2, or TAL1-LMO3; #LMO2 abnormalities are rarely combined with the rearrangement of LYL1; _E, super-enhancer created by mutations of noncoding intergenic sequences [8].
Figure 4.
Stages of T-ALL differentiation and distribution of NOTCH1/FBXW7 mutations and CDKN2AB deletions.
MYC translocations occur in approximately 5% of pediatric and adult T-ALL, involve both TR and non-TR partners, and invariably cause MYC over-expression [8,18]. They mark a subgroup of NOTCH1-independent T-ALL, which are characterized by a high incidence of PTEN deletions/loss-of-function mutations. Preliminary studies suggested that MYC translocations were high risk markers, since they have been associated with high white blood cell count, poor response to glucocorticoid pretreatment, and poor response to standard chemotherapy [18,19,20]. Interestingly, the therapeutic sensitivity of MYC-positive T-ALL towards BET bromodomain inhibitors has been observed in preclinical models [19].
Although widely heterogeneous, 6q14-q16 deletions encompass the oncosuppressor CASP8AP2/6q15 in ~90% of cases, where it is significantly downregulated [21]. Particularly, deletion of CASP8AP2/6q15 occurs in ~20% of TAL/LMO T-ALL and predicts poor response to therapy with the persistence of minimal residual disease (MRD) [8,21]. Besides CASP8AP2, two further candidate tumor suppressor genes, i.e., SYNCRIP (encoding hnRNP-Q) and SNHG5 (that hosts snoRNAs), have been recently identified at 6q14.3, ~4Mb apart from CASP8AP2. When codeleted/haploinsufficient, SYNCRIP and SNHG5, alter ribosomal functions, increase leukemia-initiating cell activity, and induce tumor progression [22]. The size of the 6q deletions and the involvement of several putative tumor suppressors suggest that the haploinsufficiency of more than one gene may be at the basis of these genomic losses. Furthermore, diverse types of 6q deletions might be related to distinct genetic subgroups.
4. Early/Immature T-ALL: Transcriptome and HOXA, MEF2C, and BCL11B Oncogene Deregulation
Early and immature T-ALL are two distinct subtypes of T-cell differentiation arrest of leukemia. Early T-ALL, also known as pre-T ALL, were first defined by the EGIL group [23], by the expression of the cCD3 T-cell lymphoid markers with/without CD2, CD5, and CD8, but negative for CD1a and sCD3. Even more immature is the so-called early T-cell precursor (ETP) ALL, which was first reported by Coustan-Smith in 2009, and that largely overlaps with the pro-T subtype of the EGIL classification [23,24]. ETP-ALL are recognized by a distinct immature phenotype, characterized by the expression of at least one stem cell (CD34, CD117) and/or myeloid markers (CD13, CD33, HLA-DR, CD11b, CD65) in at least 25% of leukemic cells, negativity or weak expression (<75%) of CD5, and no expression of CD4 and CD8 [24]. It is worth mentioning that, similar to ETP ALL is a subset of immature T-ALL, called near-ETP, which despite having overlapping characteristics, exhibits CD5 antigen expression at levels that are not low enough to meet ETP-ALL criteria [9,24].
It has been demonstrated that the state of maturation arrest of T-cell leukemias, determines the specific anti-apoptotic protein on which depends cell survival [25]. In ETP-ALL, leukemic blasts depend on the anti-apoptotic protein BCL2, which is widely over-expressed in this subtype of T-ALL [5,25]. Based on these data, preclinical in vitro studies have exploited BCL2 as a putative target in immature T-ALL, using the specific inhibitor BH3 mimetic ABT-199, also known as venetoclax [26]. ABT-199 showed a strong anti-leukemic activity and a synergistic effect when combined with chemotherapy or steroids in immature T-ALL but not in more mature T-ALL subtypes [26]. A remarkable result in the use of venetoclax in patients with immature T-ALL, has been obtained by our group, in collaboration with Dr. G Roti, University of Parma. Combining molecular-cytogenetic and Drug Sensitivity and Resistance Profiling (DSRP) studies, we confirmed BCL2 over-expression in three cases of immature T-ALL, and used this marker to prioritize the selection of the most effective compounds, as identified by DSRP. Accordingly, these patients, all with refractory/early relapsed ETP/near ETP ALL, were treated with ABT-199 combined with bortezomib, the latter used to overcome known resistance linked to ABT-199 administration, and obtained complete/partial hematological remission. Subsequently, two underwent hematopoietic stem cell transplantation, and achieved a stable cytogenetic remission [27].
ETP-ALL have a distinctive gene expression signature characterized by high levels of expression of myeloid markers, i.e., LYL1, LMO2, CD34, CCND2, KIT, GATA2, and CEBPA, and low levels of expression of genes related to thymocyte differentiation, such as CD1, CD4, CD8, TCF7, and LEF1 [5,6,24]. Although ETP ALL cases share a specific signature, their genomic profile is extremely heterogeneous, with alterations of many different genes. They include activating mutations of genes encoding for cytokine receptors and RAS signaling (NRAS, KRAS, FLT3, IL7R, JAK3, JAK1, SH2B3, and BRAF), deletions/loss-of-function mutations of genes involved in hematopoietic development (GATA3, ETV6, RUNX1, IKZF1, and EP300), and abnormalities of histone-modifying genes (EZH2, EED, SUZ12, and SETD2). On the other hand, abnormalities of T-ALL-related genes, such as NOTCH1 and CDKN2AB, are rare (Figure 4) [28,29]. Despite the genomic heterogeneity, activation of HOXA, MEF2C, or BCL11B, characterize specific subtypes of immature cases, accounting for approximately half of ETP-ALL (Figure 5).
Figure 5.
4.1. HOXA Cluster Genes
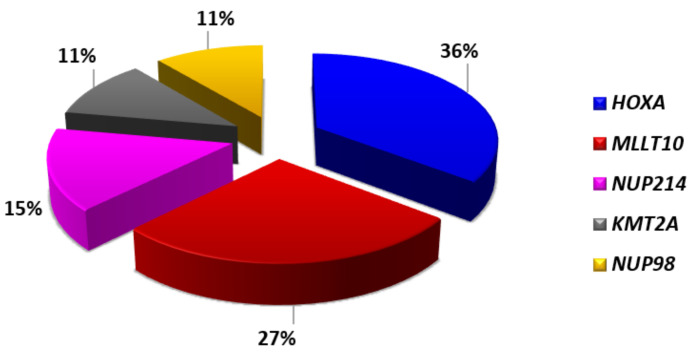
The first evidence of an oncogenic role of HOXA genes in T-ALL pathogenesis was highlighted by gene expression profile through the identification of a distinct subgroup of T-ALL with high HOXA expression [6]. HOXA positive T-ALL harbored a wide spectrum of different genomic abnormalities affecting HOXA itself, KMT2A, or MLLT10, indicating different mechanisms of cis or trans activation of the HOXA cluster genes can occur [6,30,31]. Further enriching the HOXA T-ALL subgroup, there are abnormalities of two promiscuous shuttling nucleoporins, i.e., NUP98 or NUP214, which represent additional mechanisms of HOXA activation in both pediatric and adult T-ALL (Figure 6) [32,33,34]. Although usually mutually exclusive, concomitant rearrangements of the HOXA and MLLT10 genes have been reported in rare cases of T-ALL [8,35].
Figure 6.
HOXA genetic subgroup: Genes associated with high levels of HOXA expression and frequency of their alterations [8,9].
HOXA-positive T-ALL have an immature, ETP, or near ETP phenotype, in 40–45% of cases [8,36]. The poor overall survival of HOXA positive T-ALL patients, as a whole, as well as the unfavorable predictive/prognostic impact of genomic abnormalities underlying HOXA up-regulation, have been reported by several groups [36,37,38,39]. However, HOXA related abnormalities do not appear to predict a poor outcome when occurring in non-ETP-ALL cases [36,38,40].
4.2. MEF2C Expression
In 2011, Homminga et al. [7] described an immature cluster of T-ALL that included cases with HOXA-activating abnormalities and cases lacking known driving oncogenic events. About 30% of these cases was characterized by high levels of expression of MEF2C, which was supposed to be driven by rearrangements of MEF2C, or of transcription factors that target MEF2C (NKX2.5, PU.1), or MEF2C-associated cofactors (NCOA2) [7]. Functional experiments conducted in T-ALL cell lines supported the role of MEF2C as a transcriptional regulator of genes that are highly expressed in immature T-ALL cases, such as LMO2, LYL1, and HHEX [7]. Moreover, they also showed that MEF2C causes a T-cell differentiation block at the immature stage of differentiation [7]. It is however worth mentioning that high levels of MEF2C expression can also be found in non-ETP-ALL [41,42].
4.3. The BCL11B-a Entity
BCL11B, a transcription factor essential for the early T-cell lineage commitment, is typically expressed in thymocytes, starting from the transition between DN2a and DN2b stage. In human T-ALL, it undergoes translocations alternatively activating TLX3 or NKX2-5, but it may also act as a tumor suppressor gene undergoing loss-of-function mutations and/or deletions in 13% and 3% of T-ALL and ETP-ALL, respectively.
A new leukemia subtype (BCL11B-a), with a variable phenotype, characterized by coexpression of myeloid and T-lymphoid markers, and ranging from ETP-ALL to immature AML, has been recently identified by our group in adults and by Montefiori LE et al. in children [10,43]. This immature form of leukemia is driven by transcriptional activation of BCL11B, due to chromosomal rearrangements that juxtapose BCL11B to diverse, active super-enhancers, or to the ZEB2 gene, generating a ZEB2-BCL11B fusion. These rearrangements differ from the other T-ALL translocations involving the 14q32 region, such as the t(5;14)(q35;q32)/BCL11B-TLX3 (see above), due to a more centromeric cluster of 14q32 breakpoints that can be reliably identified with a specifically designed fluorescence in situ hybridization assay. An alternative mechanism of BCL11B activation is represented by a focal 2.5Kb amplification that generates a super-enhancer from a noncoding element distal to the gene [43]. In vitro studies have shown that BCL11B, even in the absence of Notch signaling, is sufficient to drive a T lineage expression program in hematopoietic progenitor cells through the activation of genes characteristic of T-cell differentiation, block of the myeloid differentiation, and expansion of a subpopulation with a T-lineage immunophenotype.
BCL11B/14q32 rearrangements/over-expression behave as disease biomarkers present at diagnosis and relapse, but not at remission. They typically cooccur with FLT3 mutations and mutations of epigenetic modulators, most frequently DNMT3A, TET2, and/or WT1 gene. Furthermore, BCL11B-a AL have a distinct expression profile, characterized by deregulation of BCL11B target genes, inhibition of the T-cell differentiation program, and activation of the JAK/STAT. As predicted by the genomic profile, BCL11B-a AL cases are sensitive to tyrosine kinase and JAK/STAT inhibitors, i.e., NVP-BVB808, Momelotinib, Fedratinib, and NVP-BSK805 [10]
5. Cortical CD1a Positive T-ALL Are Characterized by TLX1, NKX2-1, or TLX3 Over-Expression
Common features of this subgroup of T-ALL are CD1a expression, differentiation arrest at the cortical (DN3-DP) stage of T-cell development, and rearrangement/over-expression of TLX1 (in adults) or NKX2.1 (in children) [5,7]. The latter subgroup includes pediatric cases harboring rearrangements of NKX2.1, NKX2.2, or MYB [7]. Transcriptome studies have shown that these cases are characterized by the altered cell cycle, DNA replication, and spindle assembly [5,7]. While mitotic defects represent a direct effect of TLX1 over-expression, which drives aneuploidy in the earliest stage of leukemogenesis, altered cell cycle might be related to deletion of CDKN2AB (85%) and/or CDKN1B (25%) cell cycle regulators [8]. These leukemia subtype has a high prevalence of NOTCH1 mutations (Figure 4) [9]. Other recurrent secondary events are deletions/mutations of BCL11B (12% vs. 3% in the overall population), herein behaving as a putative oncosuppressor, and mono-/bi-allelic deletions of PTPN2, a ubiquitous nontransmembrane tyrosine phosphatase, found in 20% of TLX1/NKX2.1 positive cases [8,9,44]. In addition, pediatric NKX2.1-positive cases have a high rate of deletions of LEF1, a DNA-binding transcription factor, which interacts with nuclear β-catenin in the WNT signaling pathway, and of mutations of RPL10, a ribosomal protein belonging to the 60S ribosomal subunit [8,9,45,46]. Amongst T-ALL, TLX1/NKX2.1 positive cases have been associated with the best treatment outcome, in both children and adults [47,48,49,50].
It is worth mentioning that, besides TLX1/NKX2.1 rearrangements, which are virtually always associated with a cortical phenotype, also abnormalities of TAL/LMO, HOXA, and TLX3 can be detected in T-ALL, at this stage of differentiation. Notably, ~40% of TLX3-positive cases display a cortical phenotype, although this oncogene may also be involved in immature, early, and mature T-ALL [8]. TLX3 rearrangements mainly occur as a result of t(5;14)(q35;q32) translocation that places the gene under the control of a strong regulatory sequence downstream BCL11B at 14q32. In sporadic cases, rearrangement of TLX3 with TRB, TRAD, CDK6, or unknown partners, have been reported [8,51]. TLX1 and TLX3 are closely related genes that belong to the NKL family of homeobox transcription factors and regulate the transcription of a widely overlapping set of genes. Accordingly, gene expression-based hierarchical and genomic studies have shown that TLX1 and TLX3 positive T-ALL share common oncogenic pathways, although they also have distinguishing features, and a different clinical outcome [5,7,52,53]. In children, high levels of TLX3 expression, as well as TLX3 cytogenetic abnormalities, have been associated with both poor and good prognosis, or have not been related to disease outcome [37,49,52,54]. These conflicting data may reflect bias in patient selection, especially with respect to the number of immature and cortical cases included in the study cohorts, and differences in drug sensitivity of this specific T-ALL subtype [55].
6. Actionable Deregulated Pathways and Cellular Processes
6.1. NOTCH Pathway Activation
The Notch signaling is essential for T-cell lineage development and survival, and for the proliferation of committed T-cell progenitors. In T-ALL, NOTCH1 is a driving oncogene, whose gain-of-function mutations induce the development of pre-T-cells to leukemia [56]. The first evidence of NOTCH1 involvement in T-ALL has been provided by the identification of a rare t(7;9)(q34;q34) translocation that involves TRB and NOTCH1, cell lines, and primary samples [57]. Later on, another rare NOTCH1 translocation, the t(9;14)(q34;q11) that juxtaposes the gene to the TRAD locus, has been described [58,59]. Both translocations cause the transcriptional activation of NOTCH1 by the TR enhancer regions. Nevertheless, the activation of the NOTCH signaling is largely dependent on gain-of-function mutations that typically occur at the HD and PEST domains [60]. In addition to NOTCH1 alterations, the NOTCH pathway can be activated by loss-of-function mutations/deletions of FBXW7, encoding for a ubiquitin protein that promotes and mediates the degradation of NOTCH1 [61,62]. NOTCH1 and/or FBXW7 mutations can occur jointly, and are unequally distributed amongst the main genetic subgroup (Figure 4) [61,62,63]. Indeed, present in over 70% of TLX1, TLX3, and NKX2.1 positive T-ALL cases, their incidence decreases significantly in both immature and mature T-ALL (≤40% of cases) [8,28,29].
NOTCH1 mutations have been regarded as both prognostic and predictive biomarkers. However, the prognostic impact of NOTCH1 mutations, although extensively studied, did not reach unambiguous conclusions, as no good, or even unfavorable, outcomes have been reported for NOTCH1-positive T-ALL [64,65,66,67]. These discordant findings can be explained by the variable genomic background, accompanying NOTCH activation, which can differently influence the response to therapy. It has also been suggested that differences in therapy intensification may influence the prognostic impact of NOTCH1/FBXW7 positive T-ALL [39].
While NOTCH1/FBXW7 cannot be used alone as prognostic markers, there is a general agreement in considering the NOTCH signaling as a good candidate for tailored therapy. Preclinical studies have shown a strong therapeutic effect of different NOTCH1 inhibitors, such as γ-Secretase (GS) and ADAM (Disintegrin Metalloproteases) inhibitors, monoclonal antibody, and molecules that block the activity of the NOTCH1 transcription factor complex, in both T-ALL cell lines and primary samples [68]. In addition, therapeutic targeting of the E3 ubiquitin ligase SKP2, whose expression is regulated by NOTCH signaling, has been proven to block T-ALL proliferation in in vitro and in vivo models [69]. Lastly, the sarco-endoplasmic reticulum Ca2+-ATPase (SERCA) inhibition appeared a valuable way to suppress oncogenic NOTCH1 signaling, although the severe side effects observed in mouse models precluded their use in humans. Interestingly, promising results with a new SERCA inhibitor, the CAD204520, have been recently reported, since CAD204520 exerts a significant anti-leukemic activity in in vitro and xenograft models of NOTCH-dependent T-ALL, with very reduced/no off-target toxicity [70].
Although acting as leukemogenic driver events, NOTCH1 mutations can be primary “initiating events”, even arising prenatally [71], or “late events”, detected in cellular subclones that are lost during disease progression/relapse [72,73,74,75]. These results warn about the use of NOTCH1 as a marker for MRD determination and also to select patients for testing NOTCH1 inhibitors, especially when considering these treatments in refractory/relapsed patients. [76].
6.2. IL7R/JAK/STAT Signaling Activation
The Interleukin 7 receptor (IL-7R) signaling is required for the commitment, proliferation, and survival of early T-cell progenitors [77]. IL7R activation, through its ligand IL7, induces reciprocal JAK1 and JAK3 phosphorylation, and subsequent recruitment and activation of the transcription regulator STAT5. Once phosphorylated, STAT5 homodimerizes and migrates into the nucleus, acting as a transcription factor [77,78].
About 10% of T-ALL, shows gain-of-function mutations in IL7R that drive the constitutive activation of the JAK/STAT signaling [79]. Activation of JAK/STAT signaling can also be achieved by JAK3, JAK1, or STAT5B mutations, reported in approximately 7%, 4%, and 1% of T-ALL cases, respectively. Finally, inactivation of PTPN2 or DNM2, both negative regulators of this cascade, can be detected in 10–20% of T-ALL cases [8,80,81]. Overall, abnormalities underlying the JAK/STAT activation, are predominantly associated with TLX1, TLX3, and HOXA subgroups, and with the ETP subtype [9,28,79,82,83,84].
Due to its recurrent involvement, the JAK/STAT pathway has been regarded as a putative actionable target. In murine xenograft models of ETP-ALL with aberrant activation of this signaling, the JAK1/2 inhibitor ruxolitinib, was shown to be highly effective [85]. Furthermore, the combination of dexamethasone and ruxolinitib seems to overcome IL7-induced glucocorticoid resistance in T-ALL samples [86].
Being one of the effectors of the JAK/STAT pathway, the treonin/serin kinase PIM1 emerged as a putative downstream hit, in T-ALL with JAK/STAT activation. It is worth noting that high levels of PIM1 expression are typically found in T-ALL harboring activating mutations of IL7RA, JAK1, JAK3, and STAT5B, and/or loss of function of PTPN2. Accordingly, the highest levels of PIM1 expression have been observed in T-ALL of the TLX1, TLX3, and HOXA subgroups [87,88]. Furthermore, PIM1 is expressed at high levels, in T-ALL/LBL with a rare t(6;7)(p21;q34) translocation, which by moving the regulatory sequences of TRB close to PIM1, causes its transcriptional activation [87,88]. Preclinical in vitro and in vivo studies demonstrated that TRB-PIM1, as well as IL7R positive T-ALL/LBL, benefit from treatments with one of the two pan-PIM inhibitors AZD1208 and TP3654, combined with glucocorticoids or chemotherapy. Overall, these data point to PIM1, as a valid actionable hit, in approximately 30% of T-ALL/T-LBL [89,90].
6.3. The ABL1/Src-Family Kinases and the Rationale for the Use of Tyrosine-Kinase Inhibitors
Graux et al., for the first time, demonstrated that 6% of pediatric T-ALL express the constitutively phosphorylate tyrosine kinase NUP214-ABL1. This rearrangement originates from the fusion and amplification of NUP214 and ABL1 in the extrachromosomal structure called episomes. This abnormality is a late event that often cooccurs with CDKN2A deletion and/or NOTCH1 mutations and is typically associated with TLX1 and TLX3 subgroups [9,91,92].
T-ALL harboring NUP214-ABL1 are sensitive to selective tyrosine-kinase inhibitors (TKi), such as imatinib and dasatinib. Interestingly, another imatinib sensitive ABL1 fusion, the EML1-ABL1, has been reported in a single case of T-ALL with a cryptic t(9;14)(q34;q32) [93]. Moreover, it has been recently reported that ABL2, PDGFRA, and PDGFRB, other ABL-class tyrosin-kinases are also recurrently involved in T-ALL, and that they all predict sensitivity towards TKi [94].
The functional consequences of ABL-class protein constitutive activation have been referred to the activity of LCK, a protein of the SRC family, which is required for the proliferation of NUP214-ABL1 transformed cells, as demonstrated by in vitro and in vivo studies [95,96]. Furthermore, T-ALL dependency from LCK goes beyond the presence of rearrangements of ABL-class proteins, as recently shown in pediatric ETP-ALL patients [97]. High levels of LCK expression have been related to poor response to glucocorticoid pretreatment, which can, however, be reverted by LCK inhibitors, such as dasatinib, bosutinib, nintedanib, and WH-4-023 [98]. Thus, the use of LCK inhibitors could be exploited in approximately 30% of T-ALL patients, regardless of the presence of the typical ABL-class fusions [99].
6.4. PI3K/AKT/mTOR Signaling Predicts Glucocorticoid Resistance
Another oncogenic pathway recurrently activated in T-ALL is the PI3K/AKT/mTOR. The activation of this signaling is mainly due to abnormalities/mutations of genes encoding for PI3K members, AKT, and/or PTEN. Deletions and/or loss-of-function mutations of PTEN, the main negative regulator of the PI3K/AK/mTOR pathway, were first described in 2007 [100], and linked to resistance to NOTCH1 inhibition in T-ALL cell lines [101]. An additional mechanism of PTEN inactivation has been recently found in about 1% of T-ALL, where a 200Kb-1.4Mb deletion, downstream PTEN, abrogates the activity of a highly conserved enhancer that modulates PTEN transcription [102]. Overall, PTEN haploinsufficiency/inactivation occurs in 10–15% of cases [8,102,103], is almost exclusively associated with abnormalities of the TAL/LMO subgroup (~20% of cases), and rarely cooccur with NOTCH1/FBXW7 mutations [104]. While PTEN mutations have not been associated with the prognosis, deletions appear to predict lower event-free and overall survival [21,105,106].
Although less frequently, the PI3K/AKT/mTOR pathway can be activated by alterations of members of the PI3K complex, such as PIK3CD and PIK3R1, or of the downstream effector AKT1 (overall about 2% of cases) [9,107]. A remarkable finding has been recently observed in a pediatric patient with Short syndrome, who developed T-ALL at the age of 13 [108]. The patient had an atypical germline variant of PIK3R1 [NM_181523.3:c.1457C>T, p.(Ala486Val)] in the iSH2 domain, which is a rare site of germline mutations, in patients with Short syndrome. Still, it is the typical hot-spot region of acquired PIK3R1 mutations in pediatric T-ALL [9]. Strengthening the close cooperation between this pathway and the TAL/LMO transcriptional complex, the leukemic blasts acquired an additional PTEN deletion and a STIL-TAL1 fusion [108]. This clinical observation suggests that SHORT syndrome, due to variants in the iSH2 domain of PIK3R1, might be a leukemia predisposing syndrome.
Any alteration causing the activation of the PI3K/AKT signaling, has been linked to glucocorticoid resistance. At the same time, preclinical models have shown a synergistic cytotoxic effect of PI3K/AKT inhibitors and steroids. For example, combined treatment with AS605240, a selective PI3Kγ inhibitor, and steroids resulted in a synergist cytotoxic effect in several T-ALL cell lines, and prevented leukemia progression in PDX T-ALL models [109]. Collectively, these data suggest that T-ALL with any genomic abnormality resulting in activation of the PI3K/AKT pathway, can benefit from PI3K targeted therapy [109,110].
6.5. RAS/MAPK Activation
Abnormalities that activate the RAS/MAPK pathway are extremely frequent in pediatric T-ALL at relapse, being detected in approximately 40% of cases, whereas their incidence at diagnosis is much lower (15%) [9,111,112]. Overall, they include hot-spot mutations of KRAS/NRAS or BRAF [113], gain-of-function mutations of the upstream tyrosin-kinase receptor FLT3, or abnormalities of the two negative regulators NF1 and PTPN11 [113,114]. The activation of the RAS/MAPK signaling has been related to chemoresistance [115,116]. Namely, activation of the RAS/MAPK signaling predicts resistance to steroids and methotrexate [112]. These effects can be overtaken by MEK1/2 inhibitors, such as selumetinib and trametinib that after validation in preclinical studies, have been approved for a phase 2 clinical trial in ALL [111,117]. Abnormalities of the RAS/MAPK signaling display a strong enrichment in ETP-ALL and HOXA subgroups, but also occur in TLX1, TLX3, NKX2.1, and NKX2.2 positive T-ALL, although at a lesser extent, while they are absent in the TAL/LMO subgroup [9].
6.6. Epigenetics in T-ALL
The epigenetic regulators most frequently reported to be involved in T-ALL, are PHF6, KDM6A, and the members of the Polymcomb repressor complex 2 (PRC2), i.e., EED, EZH2, and SUZ12.
PHF6 maps at Xq26 undergo deletions and/or loss-of-function mutations in about 15% of pediatric and 35–40% of adult T-ALL. They are almost exclusively found in male patients and are significantly enriched within the TLX1 and TLX3 subgroups [118]. PHF6 inactivation is often associated with genetic lesions of the JAK/STAT members, i.e., IL7R, JAK1, JAK3, and/or STAT5B, suggesting a close cooperation in the leukemogenic process [83]. Germline PHF6 mutations cause the Börjeson–Forssman–Lehmann syndrome (BFLS) [119], a hereditary X-linked disorder presenting with mental retardation and physical deformities. It has been suggested that BFLS may represent a cancer-predisposing syndrome as one patient with BFLS developed a T-ALL at the age of 9 [120].
The role of PHF6 in chromatin remodeling and transcriptional regulation has been indicated by its interaction with the chromatin remodeling complex nucleosome remodeling and deacetylase (NurD) and with multiple subunits of the PAF1 transcriptional elongation machinery [121,122,123]. It has been demonstrated that loss of PHF6 is an early mutational event in leukemia transformation and that Phf6 inactivation enhances hematopoietic stem cell (HSC) long-term self-renewal, and hematopoietic recovery after chemotherapy, thus rendering Phf6 knockout HSCs more quiescent and less prone to stress-induced activation [124]. Further supporting its leukemia-initiating tumor suppressor role, inactivating Phf6 in hematopoietic progenitors, favors the development of NOTCH1-induced T-ALL [124].
KDM6A (also known as UTX) is an H3K27me3 histone demethylase that functions as a tumor suppressor gene, targeted by loss-of-function mutations in approximately 5–15% of T-ALLs [125,126,127]. KDM6A mutations are gender-restricted variants as they have been exclusively found in male patients. It is worth noting that, in females, KDM6A escapes chromosome X-inactivation suggesting that females are protected against single copy loss of the gene. Thus, inactivation of one KDM6A allele in males contributes to tumor development, while in females, it does not, because cells still express the second wild type allele [127]. Interestingly, KDM6A, as well as PHF6, is an X-linked tumor suppressor gene that might partially explain the skewed gender distribution in T-ALL toward males on a genetic level.
EZH2, EED, and SUZ12 belong to the PRC2 (polycomb repressive complex 2) complex, which is an epigenetic modulator that mediates the methylation of H3K27. Reduced or abolished PRC2 activity leads to reduction of H3K27 methylation, with transcriptional activation of targets, and also induces a mitochondrial-mediated apoptosis resistance. It is interesting to note that a recent study on T-ALL, reported an association between PRC2 deficiency and a hyper-methylation profile [128].
Overall, mutations or deletions of at least one of the three PRC2 members take place in 25–30% of T-ALL cases, particularly in immature T-ALL, and have been associated with poor response to chemotherapy [28,129,130]. Similar to PHF6, a significant association between Suz12 inactivation and JAK3 mutations was found in primary T-ALL [131]. In line with these findings, the inactivation of Suz12 cooperates with mutant JAK3 to drive T-cell transformation, and T-ALL development [131]. Interestingly, drug screening has identified inhibitors of the PI3K/AKT/mTOR and Vascular endothelial growth factor receptor signaling, and of histone deacetylases, as the most effective compounds towards T-cell lymphoblasts that harbor both SUZ12 and JAK3 abnormalities [131].
7. Infant T-ALL
T-ALL is very rare in infants (≤12 months), where it has been associated with dismal outcomes. Although still poorly defined, infant T-ALL (iT-ALL) appears to have distinctive genomic and transcriptome profiles with respect to pediatric and adult cases [132,133]. Alterations typically observed in T-ALL, such as NOTCH1 or FBXW7 mutations, and CDKN2AB deletion, are present at a lower frequency than in adults and children, while new markers, such as the complete deletion of MLF1, appear to be specific and recurrent in iT-ALL [132]. Notably, the t(6;7)(q23;q34)/TRB-MYB, a very rare translocation in pediatric T-ALL (<3% of cases), was reported in three female patients with iT-ALL, displaying high white blood cell count, central nervous system involvement, and refractory disease or late relapse [134,135,136]. In addition, transcriptome and miRNome sequencing showed a clear separation between infant and pediatric T-ALL with 760 differentially expressed mRNAs and 58 differentially expressed miRNAs. Among others, a significant upregulation of BRD3, KIT, BLK, FLT1, NTRK1, and ERBB4, for which clinically approved compounds were under investigation, has been detected [133]. As observed in B-cell ALL, an amount of evidence indicate that some of the genetic abnormalities of iT-ALL can be acquired during pregnancy [132].
8. Therapeutic Opportunity to Be Exploited in T-ALL
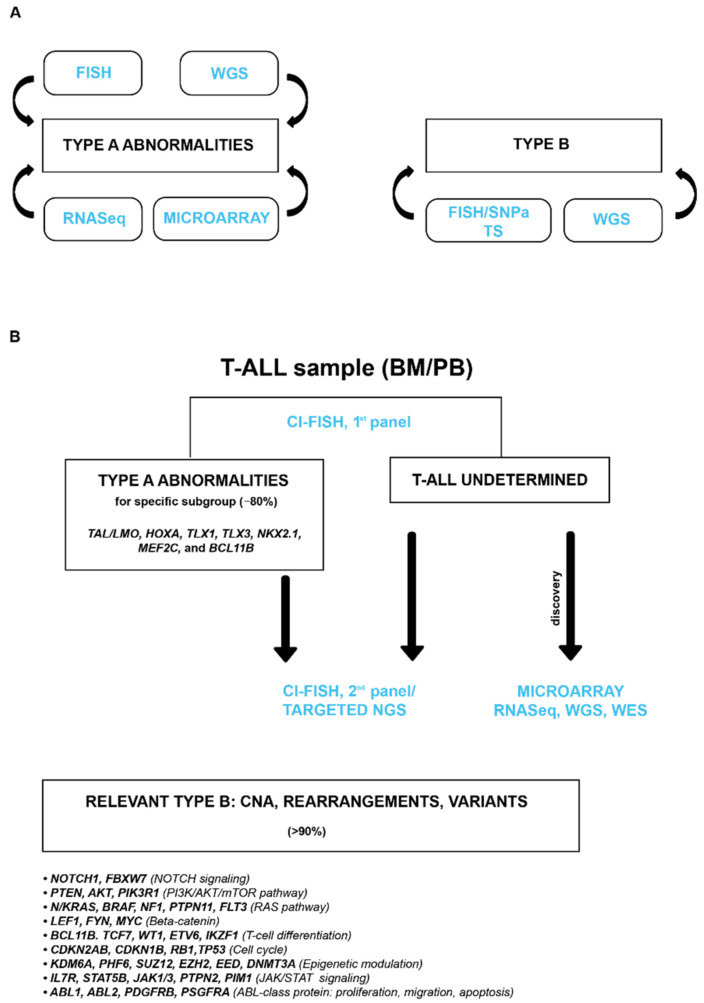
While still challenging, we expect great improvement in the diagnosis of T-ALL in the near future. To translate biomolecular information in the clinical practice, however, we need a consensus genetic diagnostic algorithm that integrates different molecular and cytogenetic techniques aiming to collect key leukemogenic events and to carry out a reliable genetic classification (Figure 7A). The challenge is that this rare leukemia subtype exhibits a wide range of complexity and inter-individual variability, thus identifying prognostic and predictive markers, a long-lasting process in large cohorts of prospectively enrolled patients. Furthermore, as each individual case shows various actionable genetic and epigenetic targets [137], a comprehensive study integrating bio-molecular data with drug sensitivity/resistance profile, would be a valuable approach to identify effective combinatorial treatments, thus implementing a personalized medicine (Figure 7B). These new therapeutic opportunities, associated with emerging immunotherapy, i.e., monoclonal antibodies (anti-CD33 in immature T-ALL or anti-CD30 in antigen-expressing cases), or CART-T or NK cell approaches directed against CD4, CD3, CD1a, CD5 T-cell antigens, will hopefully change the outlook of this aggressive subtype of leukemias.
Figure 7.
(A) Available molecular-cytogenetics techniques; (B) Diagnostic algorythm_Personal Experience. CI-FISH (combined interphase-fluorescence in situ hybridization) assay is fully described in La Starza R et al. [8]; CNA, Copy Number Alterations; NGS, Next Generations Sequencing; WGS, Whole Genome Sequencing; WES, Whole Exome Sequencing; RNASeq, RNA sequencing; TS, Targeted Sequencing.
Funding
This research was funded by: PRIN 2017 (code 2017PPS2X4) (CM and RLS); Sergio Luciani Association, Fabriano, Italy (CM); Associazione “Daniele Chianelli” (CM,TP); Roche per la Medicina di Precisione, bando 2020 (DDG).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bassan R., Bourquin J.-P., DeAngelo D.J., Chiaretti S. New Approaches to the Management of Adult Acute Lymphoblastic Leukemia. J. Clin. Oncol. 2018;36:3504–3519. doi: 10.1200/JCO.2017.77.3648. [DOI] [PubMed] [Google Scholar]
- 2.Beldjord K., Chevret S., Asnafi V., Huguet F., Boulland M.L., Leguay T., Thomas X., Cayuela J.M., Grardel N., Chalandon Y., et al. Oncogenetics and Minimal Residual Disease Are Independent Outcome Predictors in Adult Patients with Acute Lymphoblastic Leukemia. Blood. 2014;123:3739–3749. doi: 10.1182/blood-2014-01-547695. [DOI] [PubMed] [Google Scholar]
- 3.Petit A., Trinquand A., Chevret S., Ballerini P., Cayuela J.M., Grardel N., Touzart A., Brethon B., Lapillonne H., Schmitt C., et al. Oncogenetic Mutations Combined with MRD Improve Outcome Prediction in Pediatric T-Cell Acute Lymphoblastic Leukemia. Blood. 2018;131:289–300. doi: 10.1182/blood-2017-04-778829. [DOI] [PubMed] [Google Scholar]
- 4.Van Vlierberghe P., Pieters R., Beverloo H.B., Meijerink J.P.P. Molecular-Genetic Insights in Paediatric T-Cell Acute Lymphoblastic Leukaemia. Br. J. Haematol. 2008;143:153–168. doi: 10.1111/j.1365-2141.2008.07314.x. [DOI] [PubMed] [Google Scholar]
- 5.Ferrando A.A., Neuberg D.S., Staunton J., Loh M.L., Huard C., Raimondi S.C., Behm F.G., Pui C.H., Downing J.R., Gilliland D.G., et al. Gene Expression Signatures Define Novel Oncogenic Pathways in T Cell Acute Lymphoblastic Leukemia. Cancer Cell. 2002;1:75–87. doi: 10.1016/S1535-6108(02)00018-1. [DOI] [PubMed] [Google Scholar]
- 6.Soulier J., Clappier E., Cayuela J.M., Regnault A., García-Peydró M., Dombret H., Baruchel A., Toribio M.L., Sigaux F. HOXA Genes are Included in Genetic and Biologic Networks Defining Human Acute T-Cell Leukemia (T-ALL) Blood. 2005;106:274–286. doi: 10.1182/blood-2004-10-3900. [DOI] [PubMed] [Google Scholar]
- 7.Homminga I., Pieters R., Langerak A.W., de Rooi J.J., Stubbs A., Verstegen M., Vuerhard M., Buijs-Gladdines J., Kooi C., Klous P., et al. Integrated Transcript and Genome Analyses Reveal NKX2-1 and MEF2C as Potential Oncogenes in T Cell Acute Lymphoblastic Leukemia. Cancer Cell. 2011;19:484–497. doi: 10.1016/j.ccr.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 8.La Starza R., Pierini V., Pierini T., Nofrini V., Matteucci C., Arniani S., Moretti M., Lema Fernandez A.G., Pellanera F., di Giacomo D., et al. Design of a Comprehensive Fluorescence in Situ Hybridization Assay for Genetic Classification of T-Cell Acute Lymphoblastic Leukemia. J. Mol. Diagn. 2020;22:629–639. doi: 10.1016/j.jmoldx.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 9.Liu Y., Easton J., Shao Y., Maciaszek J., Wang Z., Wilkinson M.R., McCastlain K., Edmonson M., Pounds S.B., Shi L., et al. The Genomic Landscape of Pediatric and Young Adult T-Lineage Acute Lymphoblastic Leukemia. Nat. Genet. 2017;49:1211–1218. doi: 10.1038/ng.3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Di Giacomo D., La Starza R., Gorello P., Pellanera F., Kalender Atak Z., De Keersmaecker K., Pierini V., Harrison C.J., Arniani S., Moretti M., et al. 14q32 Rearrangements Deregulating BCL11B Mark a Distinct Subgroup of T and Myeloid Immature Acute Leukemia. Blood. 2021 doi: 10.1182/blood.2020010510. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mansour M.R., Abraham B.J., Anders L., Berezovskaya A., Gutierrez A., Durbin A.D., Etchin J., Lee L., Sallan S.E., Silverman L.B., et al. An Oncogenic Super-Enhancer Formed through Somatic Mutation of a Noncoding Intergenic Element. Science. 2014;346:1373–1377. doi: 10.1126/science.1259037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Z., Abraham B.J., Berezovskaya A., Farah N., Liu Y., Leon T., Fielding A., Tan S.H., Sanda T., Weintraub A.S., et al. APOBEC Signature Mutation Generates an Oncogenic Enhancer That Drives LMO1 Expression in T-ALL. Leukemia. 2017;31:2057–2064. doi: 10.1038/leu.2017.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rahman S., Magnussen M., León T.E., Farah N., Li Z., Abraham B.J., Alapi K.Z., Mitchell R.J., Naughton T., Fielding A.K., et al. Activation of the LMO2 Oncogene through a Somatically Acquired Neomorphic Promoter in T-Cell Acute Lymphoblastic Leukemia. Blood. 2017;129:3221–3226. doi: 10.1182/blood-2016-09-742148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aplan P.D., Jones C.A., Chervinsky D.S., Zhao X.F., Ellsworth M.K., Wu C., McGuire E.A., Gross K.W. An Scl Gene Product Lacking the Transactivation Domain Induces Bony Abnormalities and Cooperates with LMO1 to Generate T-Cell Malignancies in Transgenic Mice. EMBO J. 1997;16:2408–2419. doi: 10.1093/emboj/16.9.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tremblay M., Tremblay C.S., Herblot S., Aplan P.D., Hébert J., Perreault C., Hoang T. Modeling T-Cell Acute Lymphoblastic Leukemia Induced by the SCL and LMO1 Oncogenes. Genes Dev. 2010;24:1093–1105. doi: 10.1101/gad.1897910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kusy S., Gerby B., Goardon N., Gault N., Ferri F., Gérard D., Armstrong F., Ballerini P., Cayuela J.M., Baruchel A., et al. NKX3.1 Is a Direct TAL1 Target Gene That Mediates Proliferation of TAL1-Expressing Human T Cell Acute Lymphoblastic Leukemia. J. Exp. Med. 2010;207:2141–2156. doi: 10.1084/jem.20100745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanda T., Lawton L.N., Barrasa M.I., Fan Z.P., Kohlhammer H., Gutierrez A., Ma W., Tatarek J., Ahn Y., Kelliher M.A., et al. Core Transcriptional Regulatory Circuit Controlled by the TAL1 Complex in Human T Cell Acute Lymphoblastic Leukemia. Cancer Cell. 2012;22:209–221. doi: 10.1016/j.ccr.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.La Starza R., Borga C., Barba G., Pierini V., Schwab C., Matteucci C., Lema Fernandez A.G., Leszl A., Cazzaniga G., Chiaretti S., et al. Genetic Profile of T-Cell Acute Lymphoblastic Leukemias with MYC Translocations. Blood. 2014;124:3577–3582. doi: 10.1182/blood-2014-06-578856. [DOI] [PubMed] [Google Scholar]
- 19.Milani G., Matthijssens F., van Loocke W., Durinck K., Roels J., Peirs S., Thénoz M., Pieters T., Reunes L., Lintermans B., et al. Genetic Characterization and Therapeutic Targeting of MYC -rearranged T Cell Acute Lymphoblastic Leukaemia. Br. J. Haematol. 2019;185:169–174. doi: 10.1111/bjh.15425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parolini M., Mecucci C., Matteucci C., Giussani U., Intermesoli T., Tosi M., Rambaldi A., Bassan R. Highly Aggressive T-Cell Acute Lymphoblastic Leukemia with t(8;14)(Q24;Q11): Extensive Genetic Characterization and Achievement of Early Molecular Remission and Long-Term Survival in an Adult Patient. Blood Cancer J. 2014;4:e176. doi: 10.1038/bcj.2013.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Remke M., Pfister S., Kox C., Toedt G., Becker N., Benner A., Werft W., Breit S., Liu S., Engel F., et al. High-Resolution Genomic Profiling of Childhood T-ALL Reveals Frequent Copy-Number Alterations Affecting the TGF-β and PI3K-AKT Pathways and Deletions at 6q15-16.1 as a Genomic Marker for Unfavorable Early Treatment Response. Blood. 2009;114:1053–1062. doi: 10.1182/blood-2008-10-186536. [DOI] [PubMed] [Google Scholar]
- 22.Gachet S., El-Chaar T., Avran D., Genesca E., Catez F., Quentin S., Delord M., Thérizols G., Briot D., Meunier G., et al. Deletion 6q Drives T-Cell Leukemia Progression by Ribosome Modulation. Cancer Discov. 2018;8:1614–1631. doi: 10.1158/2159-8290.CD-17-0831. [DOI] [PubMed] [Google Scholar]
- 23.Bene M.C., Castoldi G., Knapp W., Ludwig W.D., Matutes E., Orfao A., van’t Veer M.B. Proposals for the Immunological Classification of Acute Leukemias. European Group for the Immunological Characterization of Leukemias (EGIL) Leukemia. 1995;9:1783–1786. [PubMed] [Google Scholar]
- 24.Coustan-Smith E., Mullighan C.G., Onciu M., Behm F.G., Raimondi S.C., Pei D., Cheng C., Su X., Rubnitz J.E., Basso G., et al. Early T-Cell Precursor Leukaemia: A Subtype of Very High-Risk Acute Lymphoblastic Leukaemia. Lancet Oncol. 2009;10:147–156. doi: 10.1016/S1470-2045(08)70314-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ni Chonghaile T., Roderick J.E., Glenfield C., Ryan J., Sallan S.E., Silverman L.B., Loh M.L., Hunger S.P., Wood B., DeAngelo D.J., et al. Maturation Stage of T-Cell Acute Lymphoblastic Leukemia Determines BCL-2 versus BCL-XL Dependence and Sensitivity to ABT-199. Cancer Discov. 2014;4:1074–1087. doi: 10.1158/2159-8290.CD-14-0353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peirs S., Matthijssens F., Goossens S., Van De Walle I., Ruggero K., De Bock C.E., Degryse S., Canté-Barrett K., Briot D., Clappier E., et al. ABT-199 Mediated Inhibition of BCL-2 as a Novel Therapeutic Strategy in T-Cell Acute Lymphoblastic Leukemia. Blood. 2014;124:3738-3738. doi: 10.1182/blood-2014-05-574566. [DOI] [PubMed] [Google Scholar]
- 27.La Starza R., Cambò B., Pierini A., Bornhauser B., Montanaro A., Bourquin J.-P., Mecucci C., Roti G. Venetoclax and Bortezomib in Relapsed/Refractory Early T-Cell Precursor Acute Lymphoblastic Leukemia. JCO Precis. Oncol. 2019:3. doi: 10.1200/PO.19.00172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang J., Ding L., Holmfeldt L., Wu G., Heatley S.L., Payne-Turner D., Easton J., Chen X., Wang J., Rusch M., et al. The Genetic Basis of Early T-Cell Precursor Acute Lymphoblastic Leukaemia. Nature. 2012;481:520–524. doi: 10.1038/nature10745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Neumann M., Heesch S., Gökbuget N., Schwartz S., Schlee C., Benlasfer O., Farhadi-Sartangi N., Thibaut J., Burmeister T., Hoelzer D., et al. Clinical and Molecular Characterization of Early T-Cell Precursor Leukemia: A High-Risk Subgroup in Adult T-ALL with a High Frequency of FLT3 Mutations. Blood Cancer J. 2012;2:e55. doi: 10.1038/bcj.2011.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brandimarte L., Pierini V., Di Giacomo D., Borga C., Nozza F., Gorello P., Giordan M., Cazzaniga G., Te Kronnie G., La Starza R., et al. New MLLT10 Gene Recombinations in Pediatric T-Acute Lymphoblastic Leukemia. Blood. 2013;121:5064–5067. doi: 10.1182/blood-2013-02-487256. [DOI] [PubMed] [Google Scholar]
- 31.Brandimarte L., la Starza R., Gianfelici V., Barba G., Pierini V., di Giacomo D., Cools J., Elia L., Vitale A., Luciano L., et al. DDX3X-MLLT10 Fusion in Adults with NOTCH1 Positive T-Cell Acute Lymphoblastic Leukemia. Haematologica. 2014;99:64–66. doi: 10.3324/haematol.2013.101725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Van Vlierberghe P., Van Grotel M., Tchinda J., Lee C., Beverloo H.B., Van Der Spek P.J., Stubbs A., Cools J., Nagata K., Fornerod M., et al. The Recurrent SET-NUP214 Fusion as a New HOXA Activation Mechanism in Pediatric T-Cell Acute Lymphoblastic Leukemia. Blood. 2008;111:4668–4680. doi: 10.1182/blood-2007-09-111872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gorello P., La Starza R., Varasano E., Chiaretti S., Elia L., Pierini V., Barba G., Brandimarte L., Crescenzi B., Vitale A., et al. Combined Interphase Fluorescence in Situ Hybridization Elucidates the Genetic Heterogeneity of T-Cell Acute Lymphoblastic Leukemia in Adults. Haematologica. 2010;95:79. doi: 10.3324/haematol.2009.010413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen B., Jiang L., Zhong M.-L., Li J.-F., Li B.-S., Peng L.-J., Dai Y.-T., Cui B.-W., Yan T.-Q., Zhang W.-N., et al. Identification of Fusion Genes and Characterization of Transcriptome Features in T-Cell Acute Lymphoblastic Leukemia. Proc. Natl. Acad. Sci. USA. 2018;115:373–378. doi: 10.1073/pnas.1717125115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bergeron J., Clappier E., Cauwelier B., Dastugue N., Millien C., Delabesse E., Beldjord K., Speleman F., Soulier J., Macintyre E., et al. HOXA Cluster Deregulation in T-ALL Associated with Both a TCRD-HOXA and a CALM-AF10 Chromosomal Translocation. Leukemia. 2006;20:1184–1187. doi: 10.1038/sj.leu.2404187. [DOI] [PubMed] [Google Scholar]
- 36.Bond J., Marchand T., Touzart A., Cieslak A., Trinquand A., Sutton L., Radford-Weiss I., Lhermitte L., Spicuglia S., Dombret H., et al. An Early Thymic Precursor Phenotype Predicts Outcome Exclusively in HOXA-Overexpressing Adult T-Cell Acute Lymphoblastic Leukemia: A Group for Research in Adult Acute Lymphoblastic Leukemia Study. Haematologica. 2016;101:732. doi: 10.3324/haematol.2015.141218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Van Grotel M., Meijerink J.P.P., Beverloo H.B., Langerak A.W., Buys-Gladdines J.G.C.A.M., Schneider P., Poulsen T.S., den Boer M.L., Horstmann M., Kamps W.A., et al. The Outcome of Molecular-Cytogenetic Subgroups in Pediatric T-Cell Acute Lymphoblastic Leukemia: A Retrospective Study of Patients Treated According to DCOG or COALL Protocols. Haematologica. 2006;91:1212–1221. [PubMed] [Google Scholar]
- 38.Ben Abdelali R., Asnafi V., Petit A., Micol J.B., Callens C., Villarese P., Delabesse E., Reman O., Lepretre S., Cahn J.Y., et al. The Prognosis of CALM-AF10-Positive Adult T-Cell Acute Lymphoblastic Leukemias Depends on the Stage of Maturation Arrest. Haematologica. 2013;98:1711. doi: 10.3324/haematol.2013.086082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abdelali R.B., Roggy A., Leguay T., Cieslak A., Renneville A., Touzart A., Banos A., Randriamalala E., Caillot D., Lioure B., et al. Brief Report LYMPHOID NEOPLASIA SET-NUP214 Is a Recurrent Gd Lineage-Specific Fusion Transcript Associated with Corticosteroid/Chemotherapy Resistance in Adult T-ALL. Blood J. Am. Soc. Hematol. 2014;123:61–69. doi: 10.1182/blood-2013-08. [DOI] [PubMed] [Google Scholar]
- 40.Matlawska-Wasowska K., Kang H., Devidas M., Wen J., Harvey R.C., Nickl C.K., Ness S.A., Rusch M., Li Y., Onozawa M., et al. MLL Rearrangements Impact Outcome in HOXA-Deregulated T-Lineage Acute Lymphoblastic Leukemia: A Children’s Oncology Group Study. Leukemia. 2016;30:1909–1912. doi: 10.1038/leu.2016.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zuurbier L., Gutierrez A., Mullighan C.G., Canté-Barrett K., Gevaert A.O., De Rooi J., Li Y., Smits W.K., Buijs-Gladdines J.G.C.A.M., Sonneveld E., et al. Immature MEF2C-Dysregulated T-Cell Leukemia Patients Have an Early T-Cell Precursor Acute Lymphoblastic Leukemia Gene Signature and Typically Have Non-Rearranged t-Cell Receptors. Haematologica. 2014;99:94. doi: 10.3324/haematol.2013.090233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Colomer-Lahiguera S., Pisecker M., König M., Nebral K., Pickl W.F., Kauer M.O., Haas O.A., Ullmann R., Attarbaschi A., Dworzak M.N., et al. MEF2C-Dysregulated Pediatric T-Cell Acute Lymphoblastic Leukemia Is Associated with CDKN1B Deletions and a Poor Response to Glucocorticoid Therapy. Leuk. Lymphoma. 2017;58:2895–2904. doi: 10.1080/10428194.2017.1312383. [DOI] [PubMed] [Google Scholar]
- 43.Montefiori L.E., Bendig S., Gu Z., Chen X., Polonen P., Ma X., Murison A., Zeng A., Garcia-Prat L., Dickerson K., et al. Enhancer Hijacking Drives Oncogenic BCL11B Expression in Lineage Ambiguous Stem Cell Leukemia. Cancer Discov. 2021 doi: 10.1158/2159-8290.CD-21-0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.De Keersmaecker K., Real P.J., Gatta D., Palomero T., Sulis M.L., Tosello V., Van Vlierberghe P., Barnes K., Castillo M., Sole X., et al. The TLX1 Oncogene Drives Aneuploidy in T Cell Transformation. Nat. Med. 2010;16:1321–1327. doi: 10.1038/nm.2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.De Keersmaecker K., Atak Z.K., Li N., Vicente C., Patchett S., Girardi T., Gianfelici V., Geerdens E., Clappier E., Porcu M., et al. Exome Sequencing Identifies Mutation in CNOT3 and Ribosomal Genes RPL5 and RPL10 in T-Cell Acute Lymphoblastic Leukemia. Nat. Genet. 2013;45:186–190. doi: 10.1038/ng.2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gutierrez A., Tschumper R.C., Wu X., Shanafelt T.D., Eckel-Passow J., Huddleston P.M., Slager S.L., Kay N.E., Jelinek D.F. LEF-1 Is a Prosurvival Factor in Chronic Lymphocytic Leukemia and Is Expressed in the Preleukemic State of Monoclonal B-Cell Lymphocytosis. Blood. 2010;116:2975–2983. doi: 10.1182/blood-2010-02-269878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ferrando A.A., Neuberg D.S., Dodge R.K., Paietta E., Larson R.A., Wiernik P.H., Rowe J.M., Caligiuri M.A., Bloomfield C.D., Look A.T. Prognostic Importance of TLX1 (HOX11) Oncogene Expression in Adults with T-Cell Acute Lymphoblastic Leukaemia. Lancet. 2004;363:535–536. doi: 10.1016/S0140-6736(04)15542-6. [DOI] [PubMed] [Google Scholar]
- 48.Bergeron J., Clappier E., Radford I., Buzyn A., Millien C., Soler G., Ballerini P., Thomas X., Soulier J., Dombret H., et al. Prognostic and Oncogenic Relevance of TLX1/HOX11 Expression Level in T-ALLs. Blood. 2007;110:2324–2330. doi: 10.1182/blood-2007-04-079988. [DOI] [PubMed] [Google Scholar]
- 49.Ballerini P., Landman-Parker J., Cayuela J.M., Asnafi V., Labopin M., Gandemer V., Perel Y., Michel G., Leblanc T., Schmitt C., et al. Impact of Genotype on Survival of Children with T-Cell Acute Lymphoblastic Leukemia Treated According to the French Protocol FRALLE-93: The Effect of TLX3/HOX11L2 Gene Expression on Outcome. Haematologica. 2008;93:1658–1665. doi: 10.3324/haematol.13291. [DOI] [PubMed] [Google Scholar]
- 50.Van der Zwet J.C.G., Cordo V., Canté-Barrett K., Meijerink J.P.P. Multi-Omic Approaches to Improve Outcome for T-Cell Acute Lymphoblastic Leukemia Patients. Adv. Biol. Regul. 2019;74:100647. doi: 10.1016/j.jbior.2019.100647. [DOI] [PubMed] [Google Scholar]
- 51.Hansen-Hagge T.E., Schäfer M., Kiyoi H., Morris S.W., Whitlock J.A., Koch P., Mahotka C., Bartram C.R., Janssen J.W.G. Disruption of the RanBP17/Hox11L2 Region by Recombination with the TCRδ Locus in Acute Lymphoblastic Leukemias with t(5;14)(Q34;Q11) Leukemia. 2002;16:2205–2212. doi: 10.1038/sj.leu.2402671. [DOI] [PubMed] [Google Scholar]
- 52.Ballerini P., Blaise A., Busson-Le Coniat M., Su X.Y., Zucman-Rossi J., Adam M., van den Akker J., Perot C., Pellegrino B., Landman-Parker J., et al. HOX11L2 Expression Defines a Clinical Subtype of Pediatric T-ALL Associated with Poor Prognosis. Blood. 2002;100:991–997. doi: 10.1182/blood-2001-11-0093. [DOI] [PubMed] [Google Scholar]
- 53.Baak U., Gökbuget N., Orawa H., Schwartz S., Hoelzer D., Thiel E., Burmeister T. Thymic Adult T-Cell Acute Lymphoblastic Leukemia Stratified in Standard- and High-Risk Group by Aberrant HOX11L2 Expression: Experience of the German Multicenter ALL Study Group. Leukemia. 2008;22:1154–1160. doi: 10.1038/leu.2008.52. [DOI] [PubMed] [Google Scholar]
- 54.Cavé H., Suciu S., Preudhomme C., Poppe B., Robert A., Uyttebroeck A., Malet M., Boutard P., Benoit Y., Mauvieux L., et al. Clinical Significance of HOX11L2 Expression Linked to t(5;14)(Q35;Q32), of HOX11 Expression, and of SIL-TAL Fusion in Childhood T-Cell Malignancies: Results of EORTC Studies 58881 and 58951. Blood. 2004;103:442–450. doi: 10.1182/blood-2003-05-1495. [DOI] [PubMed] [Google Scholar]
- 55.Gottardo N.G., Jacoby P.A., Sather H.N., Reaman G.H., Baker D.L., Kees U.R. Significance of HOX11L2/TLX3 Expression in Children with T-Cell Acute Lymphoblastic Leukemia Treated on Children’s Cancer Group Protocols. Leukemia. 2005;19:1705–1708. doi: 10.1038/sj.leu.2403834. [DOI] [PubMed] [Google Scholar]
- 56.García-Peydró M., Fuentes P., Mosquera M., García-León M.J., Alcain J., Rodríguez A., De Miguel P.G., Menéndez P., Weijer K., Spits H., et al. The NOTCH1/CD44 Axis Drives Pathogenesis in a T Cell Acute Lymphoblastic Leukemia Model. J. Clin. Investig. 2018;128:2802–2818. doi: 10.1172/JCI92981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Grabher C., von Boehmer H., Look A.T. Notch 1 Activation in the Molecular Pathogenesis of T-Cell Acute Lymphoblastic Leukaemia. Nat. Rev. Cancer. 2006;6:347–359. doi: 10.1038/nrc1880. [DOI] [PubMed] [Google Scholar]
- 58.Gesk S., Martín-Subero J.I., Harder L., Luhmann B., Schlegelberger B., Calasanz M.J., Grote W., Siebert R. Molecular Cytogenetic Detection of Chromosomal Breakpoints in T-Cell Receptor Gene Loci. Leukemia. 2003;17:738–745. doi: 10.1038/sj.leu.2402884. [DOI] [PubMed] [Google Scholar]
- 59.Suzuki S., Nagel S., Schneider B., Chen S., Kaufmann M., Uozumi K., Arima N., Drexler H.G., MacLeod R.A.F. A Second NOTCH1 Chromosome Rearrangement: T(9;14)(Q34.3;Q11.2) in T-Cell Neoplasia. Leukemia. 2009;23:1003–1006. doi: 10.1038/leu.2008.366. [DOI] [PubMed] [Google Scholar]
- 60.Weng A.P., Ferrando A.A., Lee W., Morris J.P., IV, Silverman L.B., Sanchez-Irizarry C., Blacklow S.C., Look A.T., Aster J.C. Activating Mutations of NOTCH1 in Human T Cell Acute Lymphoblastic Leukemia. Science. 2004;306:269–271. doi: 10.1126/science.1102160. [DOI] [PubMed] [Google Scholar]
- 61.O’Neil J., Grim J., Strack P., Rao S., Tibbitts D., Winter C., Hardwick J., Welcker M., Meijerink J.P., Pieters R., et al. FBW7 Mutations in Leukemic Cells Mediate NOTCH Pathway Activation and Resistance to γ-Secretase Inhibitors. J. Exp. Med. 2007;204:1813–1824. doi: 10.1084/jem.20070876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thompson B.J., Buonamici S., Sulis M.L., Palomero T., Vilimas T., Basso G., Ferrando A., Aifantis I. The SCFFBW7 Ubiquitin Ligase Complex as a Tumor Suppressor in T Cell Leukemia. J. Exp. Med. 2007;204:1825–1835. doi: 10.1084/jem.20070872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tosello V., Ferrando A.A. The NOTCH Signaling Pathway: Role in the Pathogenesis of T-Cell Acute Lymphoblastic Leukemia and Implication for Therapy. Ther. Adv. Hematol. 2013;4:199–210. doi: 10.1177/2040620712471368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mansour M.R., Sulis M.L., Duke V., Foroni L., Jenkinson S., Koo K., Allen C.G., Gale R.E., Buck G., Richards S., et al. Prognostic Implications of NOTCH1 and FBXW7 Mutations in Adults with T-Cell Acute Lymphoblastic Leukemia Treated on the MRC UKALLXII/ECOG E2993 Protocol. J. Clin. Oncol. 2009;27:4352. doi: 10.1200/JCO.2009.22.0996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Clappier E., Collette S., Grardel N., Girard S., Suarez L., Brunie G., Kaltenbach S., Yakouben K., Mazingue F., Robert A., et al. NOTCH1 and FBXW7 Mutations Have a Favorable Impact on Early Response to Treatment, but Not on Outcome, in Children with T-Cell Acute Lymphoblastic Leukemia (T-ALL) Treated on EORTC Trials 58881 and 58951. Leukemia. 2010;24:2023–2031. doi: 10.1038/leu.2010.205. [DOI] [PubMed] [Google Scholar]
- 66.Zuurbier L., Homminga I., Calvert V., Winkel M.T., Buijs-Gladdines J.G.C.A.M., Kooi C., Smits W.K., Sonneveld E., Veerman A.J.P., Kamps W.A., et al. NOTCH1 and/or FBXW7 Mutations Predict for Initial Good Prednisone Response but Not for Improved Outcome in Pediatric T-Cell Acute Lymphoblastic Leukemia Patients Treated on DCOG or COALL Protocols. Leukemia. 2010;24:2014–2022. doi: 10.1038/leu.2010.204. [DOI] [PubMed] [Google Scholar]
- 67.Callens C., Baleydier F., Lengline E., Ben Abdelali R., Petit A., Villarese P., Cieslak A., Minard-Colin V., Rullier A., Moreau A., et al. Clinical Impact of NOTCH1 and/or FBXW7 Mutations, FLASH Deletion, and TCR Status in Pediatric T-Cell Lymphoblastic Lymphoma. J. Clin. Oncol. 2012;30:1966–1973. doi: 10.1200/JCO.2011.39.7661. [DOI] [PubMed] [Google Scholar]
- 68.Zheng R., Li M., Wang S., Liu Y. Advances of Target Therapy on NOTCH1 Signaling Pathway in T-Cell Acute Lymphoblastic Leukemia. Exp. Hematol. Oncol. 2020;9:31. doi: 10.1186/s40164-020-00187-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rodriguez S., Abundis C., Boccalatte F., Mehrotra P., Chiang M.Y., Yui M.A., Wang L., Zhang H., Zollman A., Bonfim-Silva R., et al. Therapeutic Targeting of the E3 Ubiquitin Ligase SKP2 in T-ALL. Leukemia. 2020;34:1241–1252. doi: 10.1038/s41375-019-0653-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Marchesini M., Gherli A., Montanaro A., Patrizi L., Sorrentino C., Pagliaro L., Rompietti C., Kitara S., Heit S., Olesen C.E., et al. Blockade of Oncogenic NOTCH1 with the SERCA Inhibitor CAD204520 in T Cell Acute Lymphoblastic Leukemia. Cell Chem. Biol. 2020;27:678–697. doi: 10.1016/j.chembiol.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Eguchi-Ishimae M., Eguchi M., Kempski H., Greaves M. NOTCH1 Mutation Can Be an Early, Prenatal Genetic Event in T-ALL. Blood. 2008;111:376–378. doi: 10.1182/blood-2007-02-074690. [DOI] [PubMed] [Google Scholar]
- 72.Pear W.S., Aster J.C., Scott M.L., Hasserjian R.P., Soffer B., Sklar J., Baltimore D. Exclusive Development of T Cell Neoplasms in Mice Transplanted with Bone Marrow Expressing Activated Notch Alleles. J. Exp. Med. 1996;183:2283–2291. doi: 10.1084/jem.183.5.2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.O’Neil J., Calvo J., McKenna K., Krishnamoorthy V., Aster J.C., Bassing C.H., Alt F.W., Kelliher M., Look A.T. Activating Notch1 Mutations in Mouse Models of T-ALL. Blood. 2006;107:781–785. doi: 10.1182/blood-2005-06-2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lin Y.W., Nichols R.A., Letterio J.J., Aplan P.D. Notch1 Mutations Are Important for Leukemic Transformation in Murine Models of Precursor-T Leukemia/Lymphoma. Blood. 2006;107:2540–2543. doi: 10.1182/blood-2005-07-3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Albertí-Servera L., Demeyer S., Govaerts I., Swings T., De Bie J., Gielen O., Brociner M., Michaux L., Maertens J., Uyttebroeck A., et al. Single-Cell DNA Amplicon Sequencing Reveals Clonal Heterogeneity and Evolution in T-Cell Acute Lymphoblastic Leukemia. Blood. 2021;137:801–811. doi: 10.1182/blood.2020006996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mansour M.R., Duke V., Foroni L., Patel B., Allen C.G., Ancliff P.J., Gale R.E., Linch D.C. Notch-1 Mutations Are Secondary Events in Some Patients with T-Cell Acute Lymphoblastic Leukemia. Clin. Cancer Res. 2007;13:6964–6969. doi: 10.1158/1078-0432.CCR-07-1474. [DOI] [PubMed] [Google Scholar]
- 77.Mazzucchelli R., Durum S.K. Interleukin-7 Receptor Expression: Intelligent Design. Nat. Rev. Immunol. 2007;7:144–154. doi: 10.1038/nri2023. [DOI] [PubMed] [Google Scholar]
- 78.Vainchenker W., Constantinescu S.N. JAK/STAT Signaling in Hematological Malignancies. Oncogene. 2013;32:2601–2613. doi: 10.1038/onc.2012.347. [DOI] [PubMed] [Google Scholar]
- 79.Zenatti P.P., Ribeiro D., Li W., Zuurbier L., Silva M.C., Paganin M., Tritapoe J., Hixon J.A., Silveira A.B., Cardoso B.A., et al. Oncogenic IL7R Gain-of-Function Mutations in Childhood T-Cell Acute Lymphoblastic Leukemia. Nat. Genet. 2011;43:932–939. doi: 10.1038/ng.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tremblay C.S., Brown F.C., Collett M., Saw J., Chiu S.K., Sonderegger S.E., Lucas S.E., Alserihi R., Chau N., Toribio M.L., et al. Loss-of-Function Mutations of Dynamin 2 Promote T-ALL by Enhancing IL-7 Signalling. Leukemia. 2016;30:1993–2001. doi: 10.1038/leu.2016.100. [DOI] [PubMed] [Google Scholar]
- 81.Belver L., Ferrando A. The Genetics and Mechanisms of T Cell Acute Lymphoblastic Leukaemia. Nat. Rev. Cancer. 2016;16:494–507. doi: 10.1038/nrc.2016.63. [DOI] [PubMed] [Google Scholar]
- 82.Kleppe M., Tousseyn T., Geissinger E., Atak Z.K., Aerts S., Rosenwald A., Wlodarska I., Cools J. Mutation Analysis of the Tyrosine Phosphatase PTPN2 in Hodgkin’s Lymphoma and T-Cell Non-Hodgkin’s Lymphoma. Haematologica. 2011;96:1723. doi: 10.3324/haematol.2011.041921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Vicente C., Schwab C., Broux M., Geerdens E., Degryse S., Demeyer S., Lahortiga I., Elliott A., Chilton L., La Starza R., et al. Targeted Sequencing Identifies Associations between IL7R-JAK Mutations and Epigenetic Modulators in T-Cell Acute Lymphoblastic Leukemia. Haematologica. 2015;100:1301. doi: 10.3324/haematol.2015.130179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kontro M., Kuusanmäki H., Eldfors S., Burmeister T., Andersson E.I., Bruserud Ø., Brümmendorf T.H., Edgren H., Gjertsen B.T., Itälä-Remes M., et al. Novel Activating STAT5B Mutations as Putative Drivers of T-Cell Acute Lymphoblastic Leukemia. Leukemia. 2014;28:1738–1742. doi: 10.1038/leu.2014.89. [DOI] [PubMed] [Google Scholar]
- 85.Maude S.L., Dolai S., Delgado-Martin C., Vincent T., Robbins A., Selvanathan A., Ryan T., Hall J., Wood A.C., Tasian S.K., et al. Efficacy of JAK/STAT Pathway Inhibition in Murine Xenograft Models of Early T-Cell Precursor (ETP) Acute Lymphoblastic Leukemia. Blood. 2015;125:1759–1767. doi: 10.1182/blood-2014-06-580480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Delgado-Martin C., Meyer L.K., Huang B.J., Shimano K.A., Zinter M.S., Nguyen J.V., Smith G.A., Taunton J., Winter S.S., Roderick J.R., et al. JAK/STAT Pathway Inhibition Overcomes IL7-Induced Glucocorticoid Resistance in a Subset of Human T-Cell Acute Lymphoblastic Leukemias. Leukemia. 2017;31:2568–2576. doi: 10.1038/leu.2017.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.La Starza R., Messina M., Gianfelici V., Pierini V., Matteucci C., Pierini T., Limongi M.Z., Vitale A., Roti G., Chiaretti S., et al. High PIM1 Expression Is a Biomarker of T-Cell Acute Lymphoblastic Leukemia with JAK/STAT Activation or t(6;7)(P21;Q34)/TRB@-PIM1 Rearrangement. Leukemia. 2018;32:1807–1810. doi: 10.1038/s41375-018-0031-2. [DOI] [PubMed] [Google Scholar]
- 88.De Smedt R., Peirs S., Morscio J., Matthijssens F., Roels J., Reunes L., Lintermans B., Goossens S., Lammens T., van Roy N., et al. Pre-Clinical Evaluation of Second Generation PIM Inhibitors for the Treatment of T-Cell Acute Lymphoblastic Leukemia and Lymphoma. Haematologica. 2019;104:e17–e20. doi: 10.3324/haematol.2018.199257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Padi S.K.R., Luevano L.A., An N., Pandey R., Singh N., Song J.H., Aster J.C., Yu X.Z., Mehrotra S., Kraft A.S. Targeting the PIM Protein Kinases for the Treatment of a T-Cell Acute Lymphoblastic Leukemia Subset. Oncotarget. 2017;8:30199. doi: 10.18632/oncotarget.16320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.De Smedt R., Morscio J., Reunes L., Roels J., Bardelli V., Lintermans B., van Loocke W., Almeida A., Cheung L.C., Kotecha R.S., et al. Targeting Cytokine–and Therapy-Induced PIM1 Activation in Preclinical Models of T-Cell Acute Lymphoblastic Leukemia and Lymphoma. Blood. 2020;135:1685–1695. doi: 10.1182/blood.2019003880. [DOI] [PubMed] [Google Scholar]
- 91.Graux C., Cools J., Melotte C., Quentmeier H., Ferrando A., Levine R., Vermeesch J.R., Stul M., Dutta B., Boeckx N., et al. Fusion of NUP214 to ABL1 on Amplified Episomes in T-Cell Acute Lymphoblastic Leukemia. Nat. Genet. 2004;36:1084–1089. doi: 10.1038/ng1425. [DOI] [PubMed] [Google Scholar]
- 92.Hagemeijer A., Graux C. ABL1 Rearrangements in T-Cell Acute Lymphoblastic Leukemia. Genes Chromosomes Cancer. 2010;49:299–308. doi: 10.1002/gcc.20743. [DOI] [PubMed] [Google Scholar]
- 93.De Keersmaecker K., Graux C., Odero M.D., Mentens N., Somers R., Maertens J., Wlodarska I., Vandenberghe P., Hagemeijer A., Marynen P., et al. Fusion of EML1 to ABL1 in T-Cell Acute Lymphoblastic Leukemia with Cryptic t(9;14)(Q34;Q32) Blood. 2005;105:4849–4852. doi: 10.1182/blood-2004-12-4897. [DOI] [PubMed] [Google Scholar]
- 94.Moorman A.V., Schwab C., Winterman E., Hancock J., Castleton A., Cummins M., Gibson B., Goulden N., Kearns P., James B., et al. Adjuvant Tyrosine Kinase Inhibitor Therapy Improves Outcome for Children and Adolescents with Acute Lymphoblastic Leukaemia Who Have an ABL-Class Fusion. Br. J. Haematol. 2020;191:844–851. doi: 10.1111/bjh.17093. [DOI] [PubMed] [Google Scholar]
- 95.De Keersmaecker K., Porcu M., Cox L., Girardi T., Vandepoel R., De Beeck J.O., Gielen O., Mentens N., Bennett K.L., Hantschel O. NUP214-ABL1-Mediated Cell Proliferation in T-Cell Acute Lymphoblastic Leukemia Is Dependent on the LCK Kinase and Various Interacting Proteins. Haematologica. 2014;99:85. doi: 10.3324/haematol.2013.088674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Quintás-Cardama A., Tong W., Manshouri T., Vega F., Lennon P.A., Cools J., Gilliland D.G., Lee F., Cortes J., Kantarjian H., et al. Activity of Tyrosine Kinase Inhibitors against Human NUP214-ABL1-Positive T Cell Malignancies. Leukemia. 2008;22:1117–1124. doi: 10.1038/leu.2008.80. [DOI] [PubMed] [Google Scholar]
- 97.Serafin V., Lissandron V., Buldini B., Bresolin S., Paganin M., Grillo F., Andriano N., Palmi C., Cazzaniga G., Marmiroli S., et al. Phosphoproteomic Analysis Reveals Hyperactivation of MTOR/STAT3 and LCK/Calcineurin Axes in Pediatric Early T-Cell Precursor ALL. Leukemia. 2017;31:1007–1011. doi: 10.1038/leu.2017.13. [DOI] [PubMed] [Google Scholar]
- 98.Serafin V., Capuzzo G., Milani G., Minuzzo S.A., Pinazza M., Bortolozzi R., Bresolin S., Porcù E., Frasson C., Indraccolo S., et al. Glucocorticoid Resistance Is Reverted by LCK Inhibition in Pediatric T-Cell Acute Lymphoblastic Leukemia. Blood. 2017;130:2750. doi: 10.1182/blood-2017-05-784603. [DOI] [PubMed] [Google Scholar]
- 99.Frismantas V., Dobay M.P., Rinaldi A., Tchinda J., Dunn S.H., Kunz J., Richter-Pechanska P., Marovca B., Pail O., Jenni S., et al. Ex Vivo Drug Response Profiling Detects Recurrent Sensitivity Patterns in Drug-Resistant Acute Lymphoblastic Leukemia. Blood. 2017;129:e26–e37. doi: 10.1182/blood-2016-09-738070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mullighan C.G., Goorha S., Radtke I., Miller C.B., Coustan-Smith E., Dalton J.D., Girtman K., Mathew S., Ma J., Pounds S.B., et al. Genome-Wide Analysis of Genetic Alterations in Acute Lymphoblastic Leukaemia. Nature. 2007;446:758–764. doi: 10.1038/nature05690. [DOI] [PubMed] [Google Scholar]
- 101.Palomero T., Sulis M.L., Cortina M., Real P.J., Barnes K., Ciofani M., Caparros E., Buteau J., Brown K., Perkins S.L., et al. Mutational Loss of PTEN Induces Resistance to NOTCH1 Inhibition in T-Cell Leukemia. Nat. Med. 2007;13:1203–1210. doi: 10.1038/nm1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tottone L., Lancho O., Loh J.-W., Singh A., Kimura S., Roels J., Kuchmiy A., Strubbe S., Lawlor M.A., da Silva-Diz V., et al. A Tumor Suppressor Enhancer of PTEN in T-Cell Development and Leukemia. Blood Cancer Discov. 2021;2:92. doi: 10.1158/2643-3230.BCD-20-0201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gutierrez A., Kentsis A., Sanda T., Holmfeldt L., Chen S.C., Zhang J., Protopopov A., Chin L., Dahlberg S.E., Neuberg D.S., et al. The BCL11B Tumor Suppressor Is Mutated across the Major Molecular Subtypes of T-Cell Acute Lymphoblastic Leukemia. Blood. 2011;118:4169–4173. doi: 10.1182/blood-2010-11-318873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Trinquand A., Tanguy-Schmidt A., Abdelali R.B., Lambert J., Beldjord K., Lengliné E., De Gunzburg N., Payet-Bornet D., Lhermitte L., Mossafa H., et al. Toward a NOTCH1/FBXW7/RAS/PTEN-Based Oncogenetic Risk Classification of Adult T-Cell Acute Lymphoblastic Leukemia: A Group for Research in Adult Acute Lymphoblastic Leukemia Study. J. Clin. Oncol. 2013;31:4333–4342. doi: 10.1200/JCO.2012.48.5292. [DOI] [PubMed] [Google Scholar]
- 105.Gutierrez A., Sanda T., Grebliunaite R., Carracedo A., Salmena L., Ahn Y., Dahlberg S., Neuberg D., Moreau L.A., Winter S.S., et al. High Frequency of PTEN, PI3K, and AKT Abnormalities in T-Cell Acute Lymphoblastic Leukemia. Blood. 2009;114:647–650. doi: 10.1182/blood-2009-02-206722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tesio M., Trinquand A., Ballerini P., Hypolite G., Lhermitte L., Petit A., Ifrah N., Baruchel A., Dombret H., Macintyre E., et al. Age-Related Clinical and Biological Features of PTEN Abnormalities in T-Cell Acute Lymphoblastic Leukaemia. Leukemia. 2017;31:2594–2600. doi: 10.1038/leu.2017.157. [DOI] [PubMed] [Google Scholar]
- 107.Michalovich D., Nejentsev S. Activated PI3 Kinase Delta Syndrome: From Genetics to Therapy. Front. Immunol. 2018;9:369. doi: 10.3389/fimmu.2018.00369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Marzollo A., Maestrini G., la Starza R., Elia L., Malfona F., Pierini T., Tretti Parenzan C., Coppe A., Bortoluzzi S., Biffi A., et al. A Novel Germline Variant in PIK3R1 Results in SHORT Syndrome Associated with TAL/LMO T-cell Acute Lymphoblastic Leukemia. Am. J. Hematol. 2020;95:E335–E338. doi: 10.1002/ajh.25998. [DOI] [PubMed] [Google Scholar]
- 109.Silveira A.B., Laranjeira A.B.A., Rodrigues G.O.L., Leal P.C., Cardoso B.A., Barata J.T., Yunes R.A., Zanchin N.I.T., Brandalise S.R., Yunes J.A. PI3K Inhibition Synergizes with Glucocorticoids but Antagonizes with Methotrexate in T-Cell Acute Lymphoblastic Leukemia. Oncotarget. 2015;6:13105. doi: 10.18632/oncotarget.3524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Follini E., Marchesini M., Roti G. Strategies to Overcome Resistance Mechanisms in T-Cell Acute Lymphoblastic Leukemia. Int. J. Mol. Sci. 2019;20:3021. doi: 10.3390/ijms20123021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Irving J., Matheson E., Minto L., Blair H., Case M., Halsey C., Swidenbank I., Ponthan F., Kirschner-Schwabe R., Groeneveld-Krentz S., et al. Ras Pathway Mutations Are Prevalent in Relapsed Childhood Acute Lymphoblastic Leukemia and Confer Sensitivity to MEK Inhibition. Blood. 2014;124:3420–3430. doi: 10.1182/blood-2014-04-531871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Oshima K., Khiabanian H., Da Silva-Almeida A.C., Tzoneva G., Abate F., Ambesi-Impiombato A., Sanchez-Martin M., Carpenter Z., Penson A., Perez-Garcia A., et al. Mutational Landscape, Clonal Evolution Patterns, and Role of RAS Mutations in Relapsed Acute Lymphoblastic Leukemia. Proc. Natl. Acad. Sci. USA. 2016;113:11306–11311. doi: 10.1073/pnas.1608420113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.De Smedt R., Morscio J., Goossens S., van Vlierberghe P. Targeting Steroid Resistance in T-Cell Acute Lymphoblastic Leukemia. Blood Rev. 2019;38:100591. doi: 10.1016/j.blre.2019.100591. [DOI] [PubMed] [Google Scholar]
- 114.Balgobind B.V., Van Vlierberghe P., Van Den Ouweland A.M.W., Beverloo H.B., Terlouw-Kromosoeto J.N.R., Van Wering E.R., Reinhardt D., Horstmann M., Kaspers G.J.L., Pieters R., et al. Leukemia-Associated NF1 Inactivation in Patients with Pediatric T-ALL and AML Lacking Evidence for Neurofibromatosis. Blood. 2008;111:4322–4328. doi: 10.1182/blood-2007-06-095075. [DOI] [PubMed] [Google Scholar]
- 115.Gianfelici V., Chiaretti S., Demeyer S., Di Giacomo F., Messina M., La Starza R., Peragine N., Paoloni F., Geerdens E., Pierini V., et al. RNA Sequencing Unravels the Genetics of Refractory/Relapsed T-Cell Acute Lymphoblastic Leukemia. Prognostic and Therapeutic Implications. Haematologica. 2016;101:941. doi: 10.3324/haematol.2015.139410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Richter-Pechańska P., Kunz J.B., Hof J., Zimmermann M., Rausch T., Bandapalli O.R., Orlova E., Scapinello G., Sagi J.C., Stanulla M., et al. Identification of a Genetically Defined Ultra-High-Risk Group in Relapsed Pediatric T-Lymphoblastic Leukemia. Blood Cancer J. 2017;7:e523. doi: 10.1038/bcj.2017.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lonetti A., Cappellini A., Bertaina A., Locatelli F., Pession A., Buontempo F., Evangelisti C., Evangelisti C., Orsini E., Zambonin L., et al. Improving Nelarabine Efficacy in T Cell Acute Lymphoblastic Leukemia by Targeting Aberrant PI3K/AKT/MTOR Signaling Pathway. J. Hematol. Oncol. 2016;9:1–16. doi: 10.1186/s13045-016-0344-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Van Vlierberghe P., Palomero T., Khiabanian H., Van Der Meulen J., Castillo M., Van Roy N., De Moerloose B., Philippé J., González-García S., Toribio M.L., et al. PHF6 Mutations in T-Cell Acute Lymphoblastic Leukemia. Nature Genet. 2010;42:338–342. doi: 10.1038/ng.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jahani-Asl A., Cheng C., Zhang C., Bonni A. Pathogenesis of Börjeson-Forssman-Lehmann Syndrome: Insights from PHF6 Function. Neurobiol. Dis. 2016;96:227–235. doi: 10.1016/j.nbd.2016.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chao M.M., Todd M.A., Kontny U., Neas K., Sullivan M.J., Hunter A.G., Picketts D.J., Kratz C.P. T-Cell Acute Lymphoblastic Leukemia in Association with Börjeson-Forssman-Lehmann Syndrome Due to a Mutation in PHF6. Pediatric Blood Cancer. 2010;55 doi: 10.1002/pbc.22574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Todd M.A.M., Picketts D.J. PHF6 Interacts with the Nucleosome Remodeling and Deacetylation (NuRD) Complex. J. Proteome Res. 2012;11:4326–4337. doi: 10.1021/pr3004369. [DOI] [PubMed] [Google Scholar]
- 122.Wang J., Leung J.W.C., Gong Z., Feng L., Shi X., Chen J. PHF6 Regulates Cell Cycle Progression by Suppressing Ribosomal RNA Synthesis. J. Biol. Chem. 2013;288:3174–3183. doi: 10.1074/jbc.M112.414839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhang C., Mejia L.A., Huang J., Valnegri P., Bennett E.J., Anckar J., Jahani-Asl A., Gallardo G., Ikeuchi Y., Yamada T., et al. The X-Linked Intellectual Disability Protein PHF6 Associates with the PAF1 Complex and Regulates Neuronal Migration in the Mammalian Brain. Neuron. 2013;78:986–993. doi: 10.1016/j.neuron.2013.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wendorff A.A., Quinn S.A., Rashkovan M., Madubata C.J., Ambesi-Impiombato A., Litzow M.R., Tallman M.S., Paietta E., Paganin M., Basso G., et al. Phf6 Loss Enhances HSC Self-Renewal Driving Tumor Initiation and Leukemia Stem Cell Activity in T-All. Cancer Discov. 2019;9:436–451. doi: 10.1158/2159-8290.CD-18-1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ntziachristos P., Tsirigos A., Welstead G.G., Trimarchi T., Bakogianni S., Xu L., Loizou E., Holmfeldt L., Strikoudis A., King B., et al. Contrasting Roles of Histone 3 Lysine 27 Demethylases in Acute Lymphoblastic Leukaemia. Nature. 2014;514:513–517. doi: 10.1038/nature13605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lan F., Bayliss P.E., Rinn J.L., Whetstine J.R., Wang J.K., Chen S., Iwase S., Alpatov R., Issaeva I., Canaani E., et al. A Histone H3 Lysine 27 Demethylase Regulates Animal Posterior Development. Nature. 2007;449:689–694. doi: 10.1038/nature06192. [DOI] [PubMed] [Google Scholar]
- 127.Van Der Meulen J., Sanghvi V., Mavrakis K., Durinck K., Fang F., Matthijssens F., Rondou P., Rosen M., Pieters T., Vandenberghe P., et al. The H3K27me3 Demethylase UTX Is a Gender-Specific Tumor Suppressor in T-Cell Acute Lymphoblastic Leukemia. Blood. 2015;125:13–21. doi: 10.1182/blood-2014-05-577270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Roels J., Thénoz M., Szarzyńska B., Landfors M., De Coninck S., Demoen L., Provez L., Kuchmiy A., Strubbe S., Reunes L., et al. Aging of Preleukemic Thymocytes Drives CpG Island Hypermethylation in T-Cell Acute Lymphoblastic Leukemia. Blood Cancer Discov. 2020;1:274. doi: 10.1158/2643-3230.BCD-20-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ariës I.M., Bodaar K., Karim S.A., Chonghaile T.N., Hinze L., Burns M.A., Pfirrmann M., Degar J., Landrigan J.T., Balbach S., et al. PRC2 Loss Induces Chemoresistance by Repressing Apoptosis in T Cell Acute Lymphoblastic Leukemia. J. Exp. Med. 2018;215:3094–3114. doi: 10.1084/jem.20180570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ntziachristos P., Tsirigos A., Vlierberghe P.V., Nedjic J., Trimarchi T., Flaherty M.S., Ferres-Marco D., Da Ros V., Tang Z., Siegle J., et al. Genetic Inactivation of the Polycomb Repressive Complex 2 in T Cell Acute Lymphoblastic Leukemia. Nat. Med. 2012;18:296–301. doi: 10.1038/nm.2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Broux M., Prieto C., Demeyer S., Bempt M.V., Alberti-Servera L., Lodewijckx I., Vandepoel R., Mentens N., Gielen O., Jacobs K., et al. Suz12 Inactivation Cooperates with JAK3 Mutant Signaling in the Development of T-Cell Acute Lymphoblastic Leukemia. Blood. 2019;134:1323–1336. doi: 10.1182/blood.2019000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mansur M.B., van Delft F.W., Colman S.M., Furness C.L., Gibson J., Emerenciano M., Kempski H., Clappier E., Cave H., Soulier J., et al. Distinctive Genotypes in Infants with T-Cell Acute Lymphoblastic Leukaemia. Br. J. Haematol. 2015;171:574–584. doi: 10.1111/bjh.13613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Doerrenberg M., Kloetgen A., Hezaveh K., Wössmann W., Bleckmann K., Stanulla M., Schrappe M., McHardy A.C., Borkhardt A., Hoell J.I. T-Cell Acute Lymphoblastic Leukemia in Infants Has Distinct Genetic and Epigenetic Features Compared to Childhood Cases. Genes Chromosomes Cancer. 2017;56:159–167. doi: 10.1002/gcc.22423. [DOI] [PubMed] [Google Scholar]
- 134.Clappier E., Cuccuini W., Kalota A., Crinquette A., Cayuela J.-M., Dik W.A., Langerak A.W., Montpellier B., Nadel B., Walrafen P., et al. The C-MYB Locus Is Involved in Chromosomal Translocation and Genomic Duplications in Human T-Cell Acute Leukemia (T-ALL), the Translocation Defining a New T-ALL Subtype in Very Young Children. Blood. 2007;110:1251–1261. doi: 10.1182/blood-2006-12-064683. [DOI] [PubMed] [Google Scholar]
- 135.Bardelli V., Arniani S., Pierini V., Pierini T., di Giacomo D., Gorello P., Moretti M., Pellanera F., Elia L., Vitale A., et al. MYB Rearrangements and Over-expression in T-cell Acute Lymphoblastic Leukemia. Genes Chromosomes Cancer. 2021;60:482–488. doi: 10.1002/gcc.22943. [DOI] [PubMed] [Google Scholar]
- 136.Ramdeny P.S., Mullanfroze K., Lorenzo P., Grazia Valsecchi M., Meijerink J., Pieters R., Baruchel A., Vora A. Infant T-cell Acute Lymphoblastic Leukaemia with t(6;7)(TCRB-MYB) Translocation. Br. J. Haematol. 2021:17609. doi: 10.1111/bjh.17609. [DOI] [PubMed] [Google Scholar]
- 137.Gębarowska K., Mroczek A., Kowalczyk J.R., Lejman M. MicroRNA as a Prognostic and Diagnostic Marker in T-Cell Acute Lymphoblastic Leukemia. Int. J. Mol. Sci. 2021;22:5317. doi: 10.3390/ijms22105317. [DOI] [PMC free article] [PubMed] [Google Scholar]