Abstract
Bacterial quorum sensing (QS) is a cell-cell communication system that regulates several bacterial mechanisms, including the production of virulence factors and biofilm formation. Thus, targeting microbial QS is seen as a plausible alternative strategy to antibiotics, with potentiality to combat multidrug-resistant pathogens. Many phytochemicals with QS interference activity are currently being explored. Herein, an extract and a compound of bioinspired origin were tested for their ability to inhibit biofilm formation and interfere with the expression of QS-related genes in Pseudomonas aeruginosa and Staphylococcus aureus. The extract, a carboxypyranoanthocyanins red wine extract (carboxypyrano-ant extract), and the pure compound, carboxypyranocyanidin-3-O-glucoside (carboxypyCy-3-glc), did not cause a visible effect on the biofilm formation of the P. aeruginosa biofilms; however, both significantly affected the formation of biofilms by the S. aureus strains, as attested by the crystal violet assay and fluorescence microscopy. Both the extract and the pure compound significantly interfered with the expression of several QS-related genes in the P. aeruginosa and S. aureus biofilms, as per reverse transcription-quantitative polymerase chain reaction (RT-qPCR) results. Indeed, it was possible to conclude that these molecules interfere with QS at distinct stages and in a strain-specific manner. An extract with anti-QS properties could be advantageous because it is easily obtained and could have broad, antimicrobial therapeutic applications if included in topical formulations.
Keywords: pyranoanthocyanins, biofilms, Pseudomonas aeruginosa, quorum sensing, Staphylococcus aureus, reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
1. Introduction
Antimicrobial resistance (AMR) is one of the most concerning global public health threats of today, resulting in a significant increase in mortality and morbidity due to bacterial infections that were once treatable but now are life threatening, entailing huge economic costs [1,2].
Over the last years, researchers have been striving to find and develop new antibiotics to effectively treat multidrug-resistant bacterial infections, particularly those caused by the so-called priority pathogens, which are bacterial species with critical, high, and medium antibiotic resistance [3]. The species considered critical include Acinetobacter baumannii, Pseudomonas aeruginosa and various Enterobacteriaceae (including Klebsiella pneumonia, Escherichia coli, Serratia spp., and Proteus spp.). However, a key challenge has not yet been timely addressed, and that is that sooner or later pathogens develop or acquire resistance to the new drugs by selective pressures [4,5].
Hence, it is urgent to develop alternative approaches to tackle multidrug-resistant bacterial infections. A recently explored strategy regards the use of anti-virulence agents, also known as drugs that can block the virulence factors of the pathogen, impairing its ability to cause infection [4,6]. These drugs can, in theory, control bacterial infections not by killing the pathogen, but by affecting other pathways and mechanisms, such as their communication system, known as quorum sensing (QS). Quorum sensing is a cell-cell communication system that coordinates several bacterial mechanisms and behaviors in a density-dependent manner, allowing bacteria to share information and modulate gene expression accordingly [7,8,9]. In fact, QS was shown to be involved in both the formation of biofilms and the expression of virulence factors, two key mechanisms that enable bacteria to colonize and harm the host [10,11]. Thus, inhibiting QS could reduce virulence factor production and biofilm formation, increasing consequently the sensibility of the pathogen to antimicrobials and allowing the host immune system to tackle the infection more easily [6,12,13]. Given the importance of QS in the pathogenesis, QS inhibitors (QSI) can represent a promising approach as novel, anti-virulence drugs. Moreover, compared with conventional antibiotics, anti-virulence agents and QSI are less likely to cause the selective pressures that induce the emergence of resistance mechanisms [4].
Quorum sensing inhibitors can be natural or synthetic compounds, enzymes or antibodies [14,15,16]. Among the natural compounds, some polyphenols, such as anthocyanins, have been studied for their activity as QSI [14,17]. Anthocyanins are secondary metabolites produced by many plants and have been proven to inhibit QS-dependent phenotypes, such as violacein production by Chromobacterium violaceum [18,19], biofilm formation and virulence factor production by P. aeruginosa, Shewanella baltica and K. pneumoniae [18,20,21,22,23]. Recently, we have also shown the ability of anthocyanin-related structures, including pyranoanthocyanin extracts and their isolated compounds, to inhibit the biofilm formation of P. aeruginosa and Staphylococcus aureus [24].
Gram-negative and Gram-positive bacteria communicate using different QS systems, but the basic mechanisms are identical. The communication is achieved by the production, detection and response to small extracellular signaling molecules, known as autoinducers (AIs), that are sensed by surrounding bacteria [25,26]. The main difference lies on the AIs produced. Gram-negative bacteria use acyl homoserine lactones (AHLs) as signal molecules, while Gram-positive microorganisms communicate using autoinducing peptides (AIPs) [25,26]. Bacteria monitor the AI concentration to reach high cell density, resulting in a synchronized response by the bacterial population [27].
P. aeruginosa highly depends on QS to induce infection, having four QS systems as follows: LasI/LasR, RhlI/RhlR, Pseudomonas quinolone signal (Pqs) and Integrated QS signal (Iqs), with each system producing and responding to a specific signal molecule, 3-oxo-C12-homoserine lactone (3OC12-HLS), butanoyl homoserine lactone (C4HLS), 2-heptyl-3-hydroxi-4-quinolone (PQS) and 2-(2-hydrodyphenyl)-thiazole-4-carbaldehyde (IQS), respectively [26,27,28,29]. These systems are hierarchically organized, with the LasI/LasR system at the top, activating all the other systems. On the other hand, the RhlI/RhlR system represses the Pqs system, while the Pqs activates RhlI/RhlR [30,31]. The interplay between the four systems results in the production of a variety of virulence factors [27,28,32,33].
The S. aureus pathogenesis depends on the production of virulence factors that are partially controlled by QS, via a two-component system encoded by the accessory gene regulator (agr) locus [10,34]. The AIP is synthesized from agrD and transported to the extracellular medium [10]. Upon AIP detection, the histidine kinase receptor activates a signaling cascade that leads to AgrA phosphorylation and the subsequent activation of two divergent promoters, P2 and P3, that result in the expression of a regulatory RNA, RNAIII, which in turn induces the expression of several virulence factors [10,27,34].
The aim of this study was to explore a carboxypyranoanthocyanins extract obtained from the reaction of red wine anthocyanins with pyruvic acid, and a pure carboxypyranocyanidin-3-O-glucoside, which have previously shown to effectively hamper the biofilm formation of P. aeruginosa ATCC 27853 and S. aureus ATCC 29213 [24], for their: (i) effect in the biofilm formation of the P. aeruginosa and S. aureus multidrug-resistant (MDR) isolates; (ii) ability to interfere with the expression of the QS-related genes of the P. aeruginosa and S. aureus reference strains and MDR isolates by reverse transcription-quantitative polymerase chain reaction (RT-qPCR); and (iii) toxicity in the Galleria mellonella larvae model.
2. Results
2.1. Antimicrobial and Biofilm Inhibition Activities of Carboxypyrano-ant Extract and CarboxypyCy-3-glc against P. aeruginosa and S. aureus MDR Isolates
The carboxypyrano-ant extract and carboxypyCy-3-glc had previously not shown antibacterial activity against several Gram-positive and Gram-negative reference strains [24]. Now, in this study, the MIC and MBC values were obtained against the MDR isolates of P. aeruginosa and S. aureus (Pa3, PA004, SA007 and SA011), and are presented in Table 1.
Table 1.
Minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) values (μg/mL) of carboxypyrano-ant extract and carboxypyCy-3-glc against PA004, Pa3, SA007 and SA011.
| PA004 | Pa3 | SA007 | SA011 | |
|---|---|---|---|---|
| MIC (MBC) | ||||
| Carboxypyrano-ant extract | >512 (−) | 512 (>512) | >512 (−) | >512 (−) |
| CarboxypyCy-3-glc | >512 (−) | >512 (−) | >512 (−) | >512 (−) |
(−) not determined.
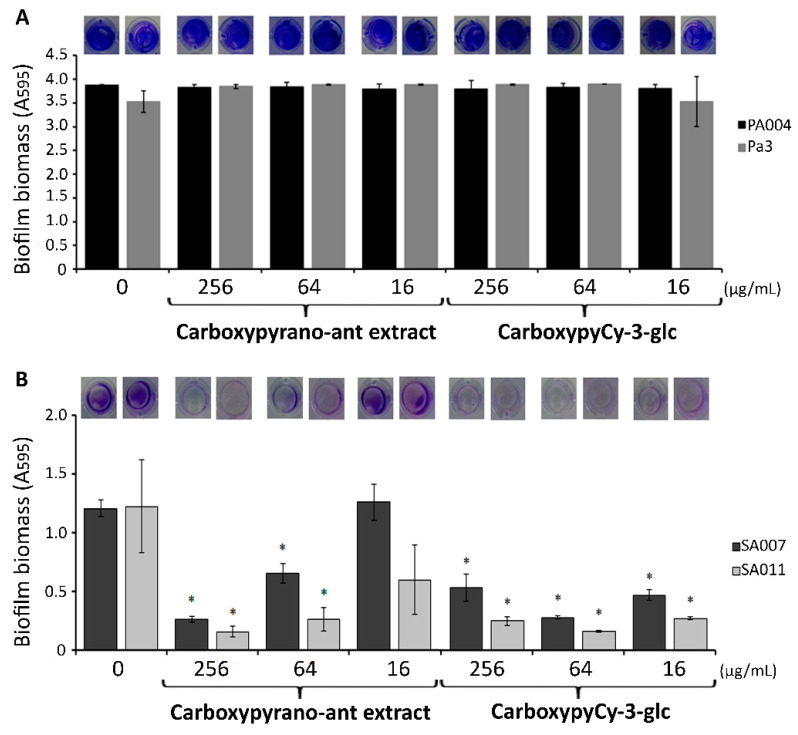
Equally, neither the carboxypyrano-ant extract nor the carboxypyCy-3-glc presented antibacterial activity against any of the isolates tested (MIC > 512 μg/mL). Subsequently, the ability of the carboxypyrano-ant extract and carboxypyCy-3-glc in interfering with the biofilm formation by those MDR isolates was also evaluated by using the crystal violet method. The results regarding the P. aeruginosa and S. aureus isolates are displayed in Figure 1.
Figure 1.
Biomass quantification using the crystal violet assay of (A) PA004 and Pa3 and (B) SA007 and SA011 biofilms formed in presence of carboxypyrano-ant extract and carboxypyCy-3-glc at 256, 64 and 16 μg/mL, and in absence of any compound or extract (control). Error bars represent SEM. Differences between the experimental groups and the respective controls were statistically significant for * p < 0.05.
The extract and the compound did not affect the biofilm formation by either of the two MDR P. aeruginosa isolates, at any of the tested concentrations (Figure 1A).
In the MDR S. aureus isolates, the carboxypyrano-ant extract significantly decreased the biofilm formation at 256 and 64 μg/mL, and in the presence of carboxypyCy-3-glc, significantly less biofilm biomass was quantified at all concentrations (Figure 1B).
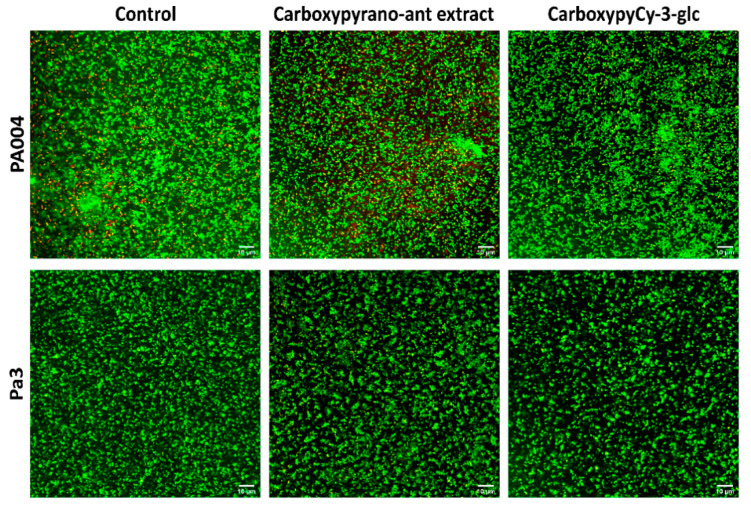
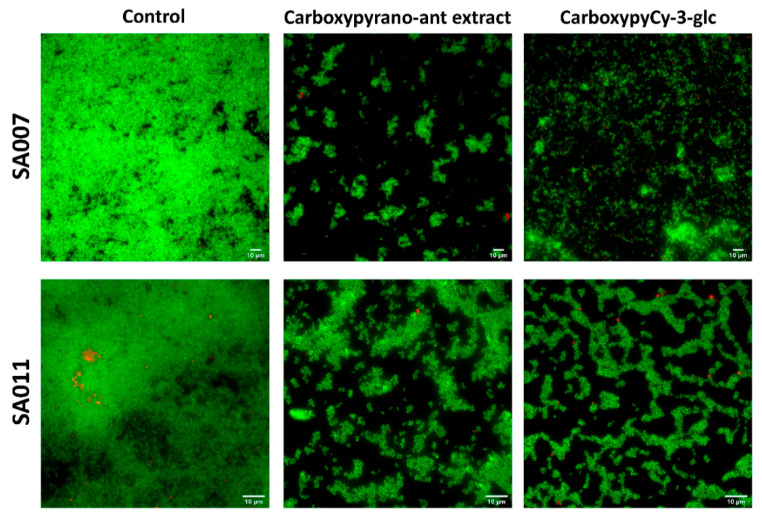
2.2. Impact of Carboxypyrano-ant Extract and CarboxypyCy-3-glc on the Biofilm Formation—Qualitative Microscopic Analysis
To further explore the phenotypic effects of the carboxypyrano-ant extract and carboxypyCy-3-glc on biofilm formation, the Live/Dead-staining technique coupled with fluorescence microscopy was performed on the biofilms of the MDR P. aeruginosa (PA004 and Pa3) and S. aureus isolates (SA007 and SA011). Regarding the biofilms of P. aeruginosa, we could observe a strong biofilm formation by both strains, either in the absence (controls) or presence of the extract and pure compound at 64 μg/mL (Figure 2).
Figure 2.
Confocal laser scanning microscopy images, after Live/Dead staining, of PA004 and Pa3 biofilms formed for 24 h in absence (control) and presence of carboxypyrano-ant extract or carboxypyCy-3-glc, at 64 µg/mL. Scale bar: 10 µm.
Strong biofilms were formed by these two strains, and no significant differences could be pinpointed between the biofilms formed in the presence and in the absence of the compounds, confirming the results that were obtained in the previous assay.
Concerning the S. aureus biofilms, images obtained undoubtedly showed the effect of these compounds in hampering the biofilm formation (Figure 3). In the presence of either the carboxypyrano-ant extract or carboxypyCy-3-glc nearly any biofilm was formed by the S. aureus isolates, with only a few cells and aggregates adhered to the surface.
Figure 3.
Fluorescence microscopy representative images, after Live/Dead staining, of SA007 and SA011 biofilms formed for 24 h in absence (control) and presence of carboxypyrano-ant extract or carboxypyCy-3-glc, at 64 µg/mL. Scale bar: 10 µm.
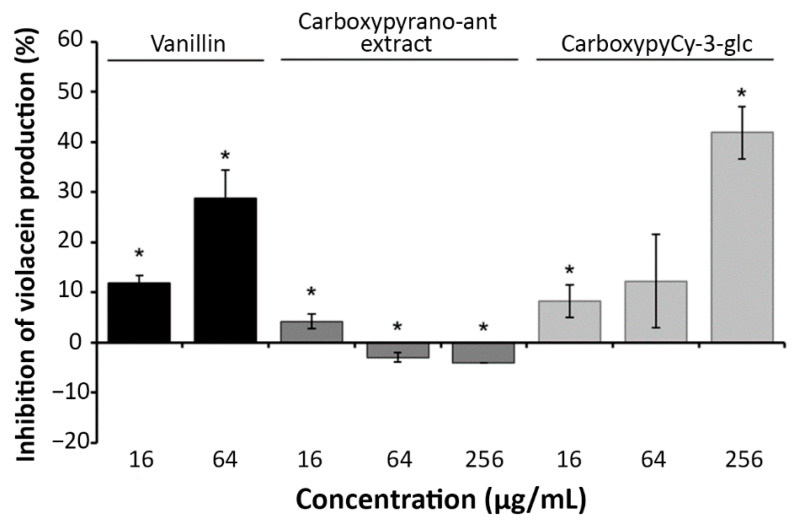
2.3. Interference of Carboxypyrano-ant Extract and CarboxypyCy-3-glc with the QS-Mediated Production of Violacein by C. violaceum
Quorum sensing inhibition activity of the carboxypyrano-ant extract and carboxypyCy-3-glc was primarily screened using C. violaceum ATCC 12472, which produces a purple pigment, violacein, under the regulation of a QS system. Thus, the inhibition of violacein production could indicate a potential interference with the QS communication system.
The quantitative determination of violacein production by HPLC (Figure 4) showed that carboxypyCy-3-glc appears to influence violacein production in a dose dependent manner, while the carboxypyrano-ant extract (at both 64 and 256 μg/mL) not only did not inhibit the production of violacein, but it also stimulated its production.
Figure 4.
Effect of carboxypyrano-ant extract and carboxypyCy-3-glc on violacein production by C. violaceum ATCC 12472. Vanillin, a known QSI, was included as a positive control. Error bars represent SEM. Differences between the experimental groups and the respective controls were statistically significant for * p < 0.05.
2.4. Interference of Carboxypyrano-ant Extract and CarboxypyCy-3-glc with the Expression of QS-Regulated Genes in P. aeruginosa and S. aureus Biofilms
As both individual carboxypyrano-ant extract and pure carboxypyCy-3-glc showed promising results in phenotypically inhibiting biofilm formation by S. aureus isolates, relative gene expression of several QS-related genes was quantified by RT-qPCR for S. aureus ATCC 29213, SA007 and SA011 biofilms formed in the presence of the carboxypyrano-ant extract or carboxypyCy-3-glc, at 64 μg/mL. Moreover, even though no significant effects were observed in the biofilm formation by the P. aeruginosa strains, the individual effect of both the extract and compound in the expression of genes associated with P. aeruginosa ATCC 27853 and Pa3 QS was also evaluated.
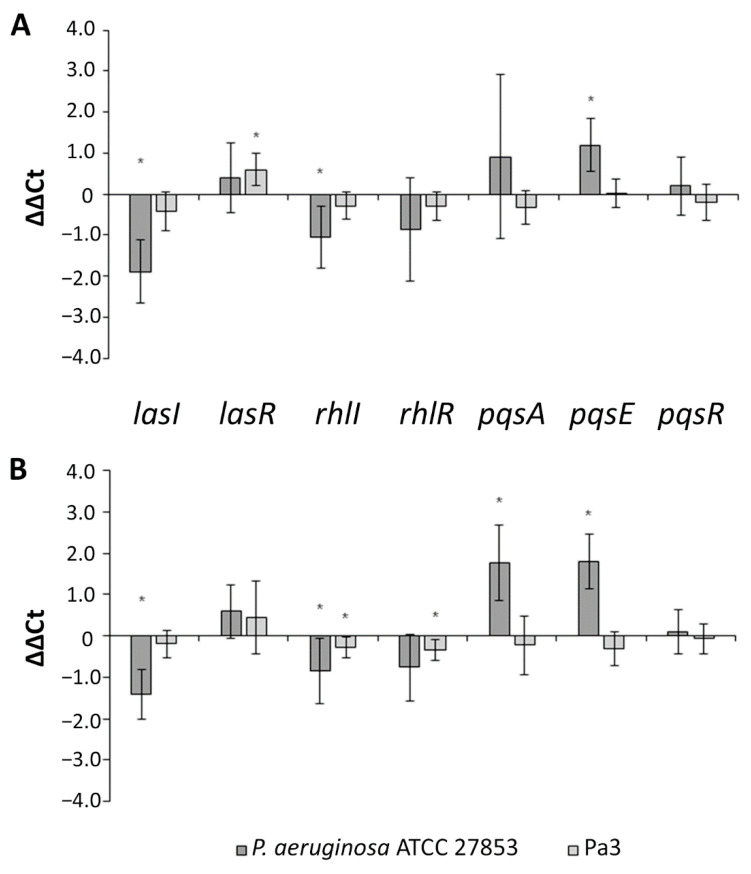
As presented in Figure 5A, the carboxypyrano-ant extract significantly downregulated the transcription of lasI and rhlI and upregulated the component of the Pqs system, pqsE, in P. aeruginosa ATCC 27853, whereas, in the Pa3 isolate, the extract caused upregulation of lasR expression. CarboxypyCy-3-glc also downregulated lasI and rhlI expression and in addition upregulated pqsA and pqsE expression in P. aeruginosa ATCC 27853; while in Pa3, it downregulated rhlI and rhlR expression (Figure 5B).
Figure 5.
Relative quantification of the QS-related genes lasI, lasR, rhlI, rhlR, pqsA, pqsE, pqsR in P. aeruginosa ATCC 27853 and Pa3 biofilms formed in the presence of carboxypyrano-ant extract (A) or carboxypyCy-3-glc (B), at 64 μg/mL. Results are expressed as ΔΔCt ± confidence interval at 95% confidence. Differences between the experimental group and the control (absence of extract or compound) were statistically significant (*) when the confidence interval does not contain the zero.
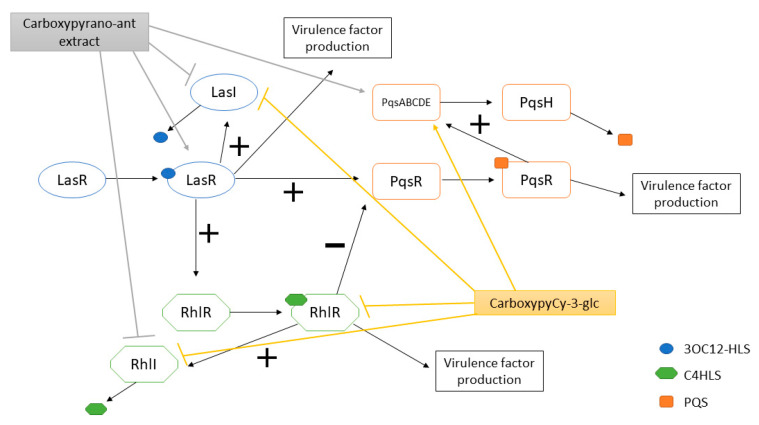
A schematic representation of the effects of the carboxypyrano-ant extract and carboxypyCy-3-glc on the QS systems of P. aeruginosa ATCC 27853 and/or Pa3 is presented in Figure 6.
Figure 6.
LasI/LasR, RhlI/RhlR and Pqs systems of P. aeruginosa and overview of the effects of carboxypyrano-ant extract and carboxypyCy-3-glc on the QS systems of P. aeruginosa ATCC 27853 and/or Pa3. (+): activation; (−): inhibition.
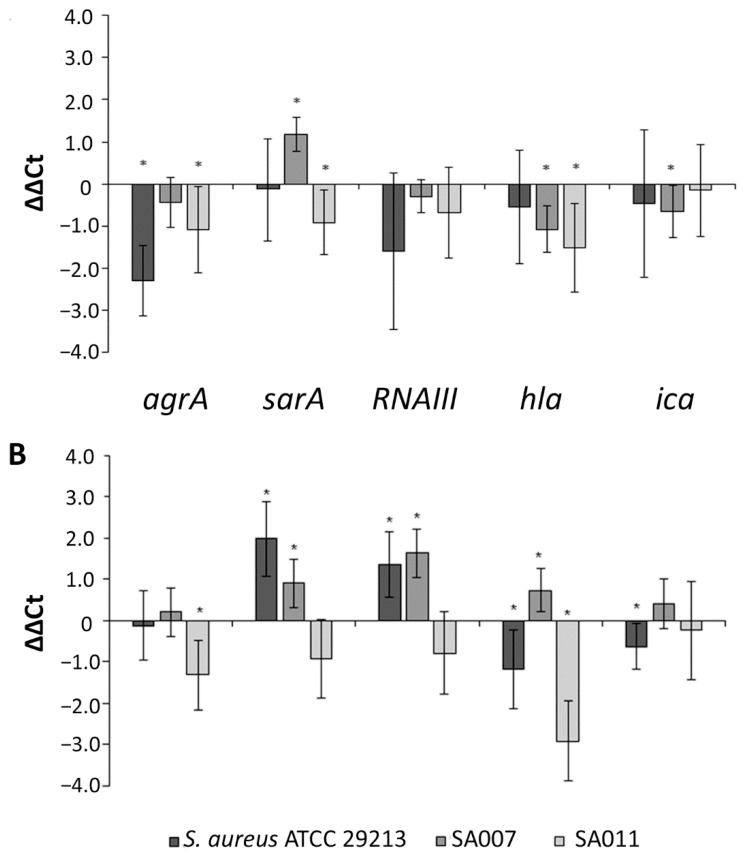
The effects of the carboxypyrano-ant extract in the expression of S. aureus QS-related genes are shown in Figure 7A.
Figure 7.
Relative quantification of the QS-related genes agrA, sarA, RNAIII, ica, hla in S. aureus ATCC 29213, SA007 and SA011 biofilms formed in the presence of carboxypyrano-ant extract (A) or carboxypyCy-3-glc (B), at 64 μg/mL. Results are expressed as ΔΔCt ± confidence interval at 95% confidence. Differences between the experimental group and the control (absence of extract or compound) were statistically significant (*) when the confidence interval does not contain the zero.
In S. aureus ATCC 29213, the carboxypyrano-ant extract significantly decreased the transcription of agrA, and that, as expected, led to downregulation of downstream genes, such as RNAIII and hla; however, not in a statistically significant way. In the SA007 isolate, treatment with the carboxypyrano-ant extract led to upregulation of sarA expression and concomitant downregulation of hla and ica, while in SA011, the extract decreased the expression of agrA, sarA and hla. As shown in Figure 7B, carboxypyCy-3-glc activated sarA and RNAIII transcription and downregulated hla and ica expression in S. aureus ATCC 29213, upregulated the expression of sarA, RNAIII and hla in SA007, and decreased agrA and hla transcription in SA011.
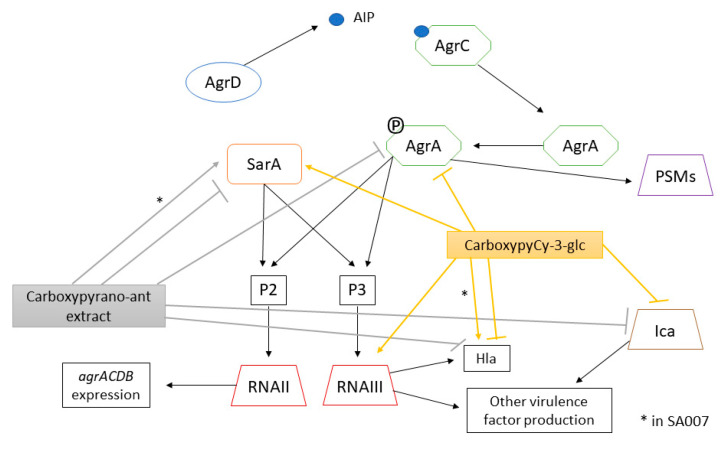
A schematic representation of the effects of the carboxypyrano-ant extract and carboxypyCy-3-glc on the QS system of S. aureus ATCC 29213 and/or SA007 and SA011 is shown in Figure 8.
Figure 8.
Agr system of S. aureus and overview of the effects of carboxypyrano-ant extract and carboxypyCy-3-glc on the QS system of S. aureus ATCC 29213 and/or SA007 and SA011. (*) points out the opposite effects of the extract or compound on the same gene among the strains.
2.5. Toxicity and Assessment of Carboxypyrano-ant Extract and CarboxypyCy-3-glc in G. mellonella
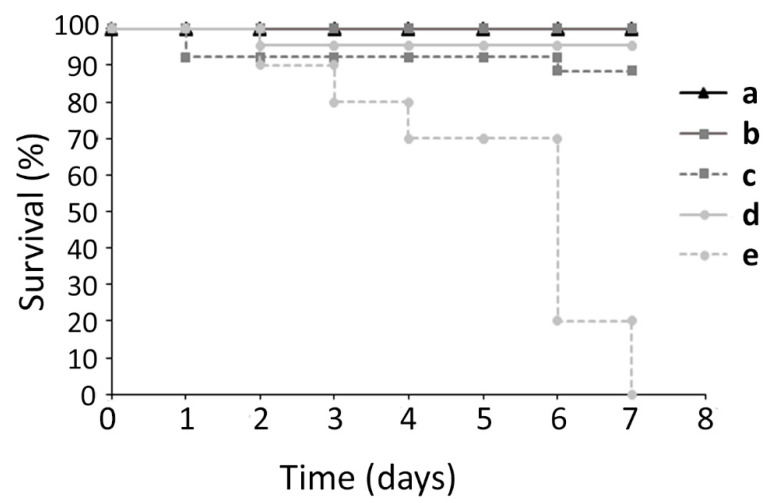
Due to its numerous advantages as an in vivo model, G. mellonella larvae were used to assess the toxicity of the carboxypyrano-ant extract and carboxypyCy-3-glc. The toxicity of the extract and pure compound was assessed at two concentrations, 25 and 50 mg/kg, which were considerably higher than the concentrations used in the biofilm formation assay and in the gene expression assays. As shown in Figure 9, carboxypyCy-3-glc showed a substantial toxic effect at 50 mg/kg on the larvae, whilst none of the remaining conditions tested (carboxypyCy-3-glc at 25 mg/kg and carboxypyrano-ant extract at 50 and 25 mg/kg) appeared to have significant toxicity in the G. mellonella model.
Figure 9.
Kaplan-Meier survival-curve of G. mellonella larvae injected with: (a) PBS, (b) carboxypyrano-ant extract at 25 mg/kg, (c) carboxypyrano-ant extract at 50 mg/kg, (d) carboxypyCy-3-glc at 25 mg/kg, and (e) carboxypyCy-3-glc at 50 mg/kg.
3. Discussion
The carboxypyrano-ant extract and carboxypyCy-3-glc did not affect the growth of any of the multidrug-resistant isolates assayed. Nevertheless, they both phenotypically hampered the biofilm formation by MRSA isolates, while not affecting the biofilm formation by MDR P. aeruginosa isolates. Given the fact that the biofilm formation of P. aeruginosa ATCC 27853 has been affected by the carboxypyrano-ant extract and carboxypyCy-3-glc [24], these results may suggest that either the compounds’ target is altered, inaccessible or absent, or regulated differently in MDR P. aeruginosa biofilms. Hypothesizing that the target of the compounds is the QS system, as we anticipate, and knowing that the QS mechanism involves the production, release, and detection of chemical signaling molecules, it is likely that differences between strains may occur in this system regulation upon the presence of these compounds [35,36,37].
The total content of carboxypyranoanthocyanins in the carboxypyrano-ant extract is nearly 20%, although there is a great contribution of other constituents (approximately 10% proteins, 5% lipids (palmitic, oleic and stearic acids) and approximately 2% simple sugars). It is worth to mention that besides the reduced phenolic content, the huge amount of polymeric anthocyaninic structures (not detected in any of the chromatographic or colorimetric assays) likely present in this extract may also account for the observed inhibitory effect on biofilm formation, acting synergistically. Besides, it was described that some compounds present in red wine, such as other flavonoids like flavonols derivatives (myricetin-O-(O-galloyl)arabinoside, myricetin-3-O-arabinoside, quercetin 3-methoxyhexoside and quercetin 3-O-glucuronide tentatively identified) present in our carboxypyrano-ant extract, also have anti-virulence activity and affect biofilm formation, and, therefore, they could also contribute to the inhibition of biofilm formation observed in the presence of the carboxypyrano-ant extract [19,38]. Moreover, the role of the other components of the extract cannot be dismissed as well, since fatty acids may act as inhibitors of biofilm development and virulence at low concentrations [39], and yeast mannoproteins also present in the extract may equally contribute to the inhibitory effect on biofilm formation [40]. Therefore, the observed effect may result from the joint contribution of the different components.
Next, we have used a natural indicator strain, C. violaceum, for QSI screening, which involves the quantification of violacein produced by the strain. CarboxypyCy-3-glc inhibited violacein production in a dose dependent manner, which corroborates with the results of biofilm formation obtained by the crystal violet assay in P. aeruginosa ATCC 27853 [24]. However, interestingly, herein the carboxypyrano-ant extract stimulated violacein production (at both 64 and 256 μg/mL). This observation may be explained by the fact that although they are both Gram-negative bacteria, P. aeruginosa and C. violaceum harbor different QS systems, so QS-inhibition occurs in distinct manners. While P. aeruginosa harbors the four QS systems previously described, C. violaceum QS system consists of the CviI and CviR components. CviI synthetizes an N-decanoyl-L-homoserine lactone (C10HSL) that binds to the receptor, CviR [41]. The complex CviRC10HSL autoinduces cviI expression and activates the vioA promoter of the vioABCDE operon that encodes the genes for violacein production [42]. It is thought that vanillin acts as a QSI by interacting with the receptor CviR in C. violaceum [43]. Thus, it is possible that the extract could act as a QSI in P. aeruginosa while being an enhancer of the QS pathway that leads to violacein production in C. violaceum.
Finally, relative gene expression of several QS-related genes was quantified by RT-qPCR for P. aeruginosa ATCC 27853, Pa3, S. aureus ATCC 29213, SA007 and SA011 biofilms formed in the presence of the carboxypyrano-ant extract or carboxypyCy-3-glc, at 64 μg/mL.
Four main QS systems are present in P. aeruginosa, and all of them are interconnected. The LasI/LasR system regulates all other three systems, while the RhlI/RhlR and the PqsABCDE/PqsR systems regulate each other, and the AmbBCDE/IqsR system regulates the PqsABCDE/PqsR system [30]. These systems are composed by a synthase that produces the respective signal molecule and by a receptor that recognizes the signal molecule and activates the pathways that result in the expression of several genes encoding for virulence factors and biofilm formation.
In P. aeruginosa ATCC 27853, the carboxypyrano-ant extract significantly downregulated the transcription of lasI and rhlI and upregulated pqsE. The activity of both LasI/LasR and RhlI/RhlR systems results in the production of N-acylhomoserine lactones, which bind to the respective QS receptor, LasR or RhlR, resulting in the activation of pathways that lead to virulence factor production and biofilm formation. The release of N-acylhomoserine lactones seems to be inhibited upon the presence of the carboxypyrano-ant extract. In turn, the RhlI/RhlR system is known to repress/inhibit the PqsABCDE/PqsR system, thus, if the former was affected, the latter system may be activated, explaining the tendency for upregulation of pqs genes, in fact, with the pqsE gene significantly upregulated. The PqsE enzyme is a synthase of an autoinducer that activates the QS receptor RhlR [44,45]. However, herein, the rhlR gene was not significantly affected. Furthermore, in the Pa3 isolate, the presence of the carboxypyrano-ant extract caused upregulation of lasR. Because lasR activates the Rhl and Pqs systems [26], it would be expected that its overexpression would lead to upregulation of rhlI, rhlR, and pqsAER, and that was not observed, meaning that an alternative transcription regulator could be responsible for suppressing RhlR and PqsR activation, such as algR or mexT, respectively [46,47].
Regarding the effect of carboxypyCy-3-glc in the QS-related gene expression of the same strains, this compound downregulated lasI and rhlI expression and upregulated pqsA and pqsE in P. aeruginosa ATCC 27853, possibly by the same mechanism observed in the biofilms formed in the presence of the carboxypyrano-ant extract. Whereas in Pa3, carboxypyCy-3-glc downregulated the expression of rhlI and rhlR, indicating that this compound successfully impaired the RhlI/RhlR system in this isolate. As observed in Figure 5, pqsAER expression was differently affected, being somehow even opposite, in the two strains. It is possible that different strains, especially clinical isolates, may harbor mutations in some QS components, resulting in a different regulation of the QS systems. For instance, a LasR-defective mutant was detected in the lungs of a cystic fibrosis patient, and it expressed a Rhl system that acted independently of the Las system [44,48].
In S. aureus, the agr quorum sensing system plays a major role in the regulation of virulence factors production [10]. The agr operon consists of four genes: agrB, agrD, agrC, and agrA. Transcription of the operon is driven by the P2 promoter, which is activated by the response regulator AgrA in an autoregulated fashion. Phosphorylated AgrA also promotes transcription at the P3 promoter, leading to the expression of RNAIII. RNAIII serves to enhance the expression of genes encoding toxins, such as α-hemolysin, while reducing the expression of genes encoding surface proteins. Although most of the QS regulation depends on RNAIII, it has been shown that AgrA, upon phosphorylation, is also directly responsible for the production of some virulence factors, such as phenol-soluble modulines (PSMs) [10]. It is believed that the agr system influences biofilms in vivo by upregulating PSMs expression, which are involved in the structure of biofilms by forming channels and promoting cell dispersal from the biofilm to further colonize the host [49,50]. The staphylococcal accessory regulator (SarA) represses extracellular proteases, such as aureolysin, otherwise they would degrade PSMs while also activating the expression of RNAIII [51]. The carboxypyrano-ant extract downregulated the expression of agrA in the three assayed strains, even though such downregulation was only statistically significant in S. aureus ATCC 29213 and SA011. In the SA007 isolate, the carboxypyrano-ant extract led to upregulation of sarA. It would be expected that an increased sarA expression would result in an increased expression of RNAIII, hla and ica. The ica locus encodes genes required for polysaccharide intercellular adhesion (PIA) production, which is essential for biofilm formation and is under positive regulation by SarA [52]. However, it is possible that a transcription regulator like CodY could be repressing the expression of these genes, despite sarA upregulation [53].
Moreover, in SA011, the carboxypyrano-ant extract also decreased significantly the expression of sarA and hla, indicating that this extract could interfere as expected, by impairing the major QS components.
CarboxypyCy-3-glc upregulated sarA and RNAIII expression and downregulated hla and ica expression in S. aureus ATCC 29213. These results could possibly be explained by repression of hla and ica by the same mechanism observed in SA007 biofilms formed in the presence of the extract. Regarding the effect of carboxypyCy-3-glc in the gene expression of MDR isolates, sarA, RNAIII and hla were overexpressed in SA007, while agrA and hla were downexpressed in SA011. It has been demonstrated that AgrA negatively regulates the production of proteases that degrade several virulence factors, such as coagulases and PSMs [10,54,55]. Thus, the inhibition of AgrA in SA011 and consequent protease de-repression might be the reason why the biofilm structure is so deeply affected in the presence of either the extract or the compound. Nevertheless, we observed that the SA007 biofilm structure was also phenotypically affected by both the extract and compound; however, while the carboxypyrano-ant extract might have an impact on biofilm structure by interfering with the ica locus expression, which is essential for biofilm formation, the effect of carboxypyCy-3-glc in the SA007 biofilm is still to be elucidated.
Although the carboxypyrano-ant extract and carboxypyCy-3-glc could interfere with QS-related genes both in P. aeruginosa and S. aureus, there were differences among the various strains within the same species. This suggests that the effect of these compounds might be strain-specific, as specific strain lineages may have different variants of QS components [32,56,57].
Additionally, the toxic effect of the carboxypyrano-ant extract and carboxypyCy-3-glc at higher doses, such as 25 and 50 mg/kg, were evaluated in vivo using the G. mellonella model. CarboxypyCy-3-glc, at 50 mg/kg, was toxic to larvae; however, it revealed no negative effect on the larvae survival at 25 mg/kg. The carboxypyrano-ant extract, at both concentrations, was not toxic. In fact, since the extract is a mixture of compounds, these are present in lower concentrations, therefore, it is reasonable that the extract did not cause any toxicity at the high concentration of 50 mg/kg as did the pure compound. Thus, we could be assured that at lower doses, as those involved in the inhibition of biofilm formation and in the interference with the QS-related genes expression, the extract and the pure compound will not be toxic.
4. Materials and Methods
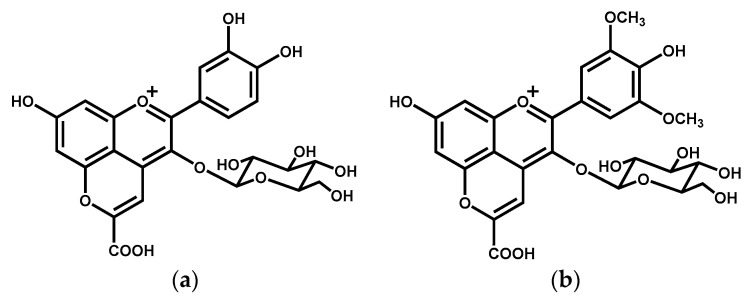
4.1. Synthesis of Carboxypyranocyanidin-3-O-glucoside and Carboxypyranoanthocyanins Extract
Carboxypyranocyanidin-3-O-glucoside (carboxypyranocy-3-glc) (Figure 10) was hemi-synthesized from the reaction of cyanidin-3-O-glucoside with pyruvic acid [58] and purified according to the procedure described in the literature [24]. The carboxypyranoanthocyanins extract (carboxypyrano-ant extract) was obtained from the reaction between anthocyanins present in a red wine extract with pyruvic acid according to the methodology described elsewhere [24]. The HPLC profile, at 520 nm, of the purified compound and the carboxypyrano-ant extract is present in Figure S1 of the Supplementary Materials.
Figure 10.
Chemical structures of (a) carboxypyranocyanidin-3-O-glucoside (carboxypyCy-3-glc) and (b) carboxypyranomalvidin-3-O-glucoside (carboxypyMv-3-glc), the main pyranoanthocyanin present in the carboxypyrano-ant extract.
The full composition of the extract (phenolic compounds, sugar, proteins and lipids) was determined as already reported in the literature [24], and is shown in Table 2.
Table 2.
Full composition of the carboxypyrano-ant extract.
| Components | (mg/mg ± SD) |
|---|---|
| Pyranoanthocyanins | 0.18 ± 0.002 |
| Low weight polyphenols | 0.010 ± 0.002 |
| Flavonols | 0.056 ± 0.006 |
| Protein content | 0.096 ± 0.002 |
| Total lipids | 0.05 ± 0.01 |
| Sugar content | 0.0184 ± 0.0023 |
4.2. Bacterial Strains and Growth Conditions
P. aeruginosa ATCC 27853 and S. aureus ATCC 29213, as well as multidrug-resistant (MDR) clinical isolates of P. aeruginosa (Pa3 and PA004) and of S. aureus (SA007 and SA011) were used in this study. The antimicrobial resistance profile of the MDR isolates is shown in Table S1 of the Supplementary Materials; SA007 and SA011 are methicillin-resistant S. aureus (MRSA). All bacteria were grown on Mueller-Hinton (MH) agar (Liofilchem srl, Roseto degli Abruzzi, Italy) from glycerol cultures, for approximately 20 h at 37 °C, before use in the preparation of inocula in the following assays. C. violaceum ATCC 12472 was also used and grown in LB agar (Liofilchem srl, Roseto degli Abruzzi, Italy) and incubated at 30 °C for 48 h.
4.3. Minimum Inhibitory Concentration (MIC) Assay and Biofilm Formation Assay against MDR Isolates
Herein, the MIC of the carboxypyrano-ant extract and carboxypyCy-3-glc was determined against the MDR isolates (Pa3, PA004, SA007 and SA011) through the microdilution technique, using cation-adjusted Mueller–Hinton broth (MHB2, Sigma-Aldrich, St. Louis, MO, USA) as fully described by us elsewhere [24]. Their effect was also evaluated in interfering with the biofilm formation ability of those MDR isolates, following the crystal violet assay as previously described [59]. Two independent experiments were performed for each assay and each crystal violet experiment was carried out at least in triplicate (the exception was for the P. aeruginosa isolates, where in each only one experiment for the crystal violet assay was carried out in several replicates).
4.4. Microscopic Visualization of Biofilm Formation
The biofilms were grown for 24 h on µ-Dishes 35 mm high, with a polymer coverslip bottom (ibidi GmbH, Gräfelfing, Germany), from a starting inoculum of 106 CFU/mL in a tryptic soy broth (TSB; Liofilchem s.r.l., Roseto degli Abruzzi, Italy), for PA004 and Pa3, or in TSBG (TSB + 1% Glucose), for SA007 and SA011. Biofilms were equally formed either in the presence of the carboxypyrano-ant extract or carboxypyCy-3-glc, each at 64 µg/mL. After 24 h at 37 °C, the planktonic phases were removed and the biofilms were rinsed with phosphate buffered saline (PBS, Sigma-Aldrich/Merck Life Science S.L.U., Algés, Portugal) and then stained with the Live/Dead staining mixture (LIVE/DEAD BacLight Bacterial Viability Kit, Thermo Fisher Scientific, Porto Salvo, Portugal) for 30 min at room temperature in the dark, rinsed again with the PBS, and then visualized under a fluorescence microscope Leica DMI6000 FFW (Leica Microsystems, Carnaxide, Portugal) or under a laser scanning confocal system Leica TCS SP5 II (Leica Microsystems, Carnaxide, Portugal), equipped with (i) an inverted microscope, Leica DMI6000-CS, using an HC PL APO CS 63× /1.30 glycerin 21 °C objective and the lasers diode 405 nm and DPSS561 561 nm; and (ii) the LAS AF software.
4.5. Effects on Violacein Production by C. violaceum
The effects of the carboxypyrano-ant extract and carboxypyCy-3-glc on violacein production by C. violaceum were assessed at 256, 64 and 16 µg/mL in a starting inoculum of 106 CFU/mL in an LB broth (Liofilchem s.r.l., Roseto degli Abruzzi, Italy). Vanillin (4-hydroxy-3-methoxybenzaldehyde, Sigma-Aldrich) was included as a positive control, while an inoculum without any compound was the negative control. Following incubation at 30 °C for 24 h, the cultures were centrifuged (11,739 g, 10 min) to precipitate the insoluble violacein, and the pellet was resuspended in dimethyl sulfoxide (DMSO, Sigma-Aldrich/Merck Life Science S.L.U., Algés, Portugal). The samples were centrifuged once more (11,739 g, 10 min) and the supernatant was kept at 4 °C. Afterwards, the formation of violacein by C. violaceum was quantified by reverse phase liquid chromatography (Dionex Ultimate 3000, (Thermo Fisher Scientific, Porto Salvo, Portugal), in a reversed-phase C18 column (Agilent) with 250 × 4.6 mm i.d., particle size 2.7 μm and at 25 °C. The eluents used were (i) 1% (v/v) formic acid in water; and (ii) 0.5 % (v/v) formic acid in 80% (v/v) acetonitrile and the elution gradient was performed from 40 to 85% (ii) for 50 min at a flow rate of 0.4 mL/ min. After 50 min, the column was washed with 100% (ii) for 10 min and then it was stabilized with the initial conditions for 10 min more. The percentage of the violacein inhibition was calculated as follows (Equation (1)):
| (1) |
and two independent experiments were performed, each allowing triplicate measurements for each condition assayed.
4.6. Biofilm Growth for RNA Extraction
The biofilms of the P. aeruginosa ATCC 27853 and Pa3, and of the S. aureus ATCC 29213, SA007 and SA011 were formed in TSB or TSBG, respectively, in the absence (controls) or presence of the carboxypyrano-ant extract or carboxypyCy-3-glc at 64 µg/mL. Each inoculum of approximately 106 CFU/mL was dispensed into 6-well plates (2 mL/well), in 2 to 4 wells, and incubated at 37 °C for 24 h. Then, the planktonic phase of each well was removed, the biofilm was rinsed once with PBS and then collected in the PBS, washed by centrifugation (9000 g, 2 min), resuspended in RNA later (Invitrogen, Thermo Fisher Scientific, Porto Salvo, Portugal), and stored overnight at 4 °C and then at −20 °C until further RNA extraction. In the case of controls, the biofilms were collected from 1 well only, while the biofilms formed in the presence of the carboxypyrano-ant extract or carboxypyCy-3-glc were collected from 3 to 4 wells.
4.7. RNA Extraction
The RNA was extracted using the GeneJET RNA Purification Kit (Thermo Fisher Scientific, Porto Salvo, Portugal) according to the manufacturer’s instructions with some modifications in the first steps. Briefly, P. aeruginosa samples were treated with lysozyme at 4.4 mg/mL (Omega Bio-tek, Norcross, GA, USA) and incubated at room temperature for 5 min. Then, approximately 25 mg of glass beads (Omega Bio-tek, Norcross, GA, USA) were added and the tubes were vortexed at maximum speed for 5 min. The cell debris and glass beads were removed by centrifugation at 7000 g for 2 min and the supernatant was transferred to a clean RNase/DNase free microcentrifuge tube. Regarding the S. aureus biofilms, the samples were treated with lysozyme at 2.5 mg/mL and lysostaphin at 0.1 mg/mL (Sigma-Aldrich/Merck Life Science S.L.U., Algés, Portugal) and incubated at 37 °C for 30 min. The RNA concentration and purity were evaluated using a NanoDrop One spectrophotometer (Thermo Fisher Scientific, Porto Salvo, Portugal).
4.7.1. Reverse Transcription-Quantitative Polymerase Chain Reaction (RT-qPCR) for P. aeruginosa
The qScript One-Step SYBR Green RT-qPCR Kit (Quantabio, Beverly, MA, USA) was used. Each 10 µL reaction contained an RNA template at 100 ng/µL, One-Step SYBR Green Master Mix, and each primer (Table S2 of the Supplementary Materials), at 200 nM. A ‘no template’ control (NTC) and a ‘no reverse transcriptase enzyme’ control (NRT) were included. Thermal cycling conditions were as follows: an initial reverse transcription step at 50 °C for 10 min, an activation cycle of 95 °C for 60 s, followed by 35 cycles of 95 °C for 10 s and 60 °C for 30 s. A melt curve analysis was performed at a temperature range of 69 to 95 °C with 0.3 °C/s intervals. All measurements were carried out in 3 biological replicates, each in technical duplicates.
4.7.2. Reverse Transcription-Quantitative Polymerase Chain Reaction (RT-qPCR) for S. aureus
Regarding the S. aureus samples, the RT-qPCR was performed in 2 steps. First, cDNA synthesis was performed using the qScript cDNA Synthesis Kit (Quantabio, Beverly, MA, USA) and 1 µg of purified RNA. Then, in the amplification step, 10 µL PCR reaction contained 1 µL cDNA template at 5 ng/µL, 5 µL PerfeCTa SYBR Green FastMix (Quantabio, Beverly, MA, USA) each primer at 500 mM (Table S3 of the Supplementary Materials). An NTC and a control using the purified RNA as a template (not subjected to cDNA synthesis) were included. Thermal cycling conditions were as follows: an initial activation step of 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s and 60 °C for 60 s. A melt curve analysis was performed at a temperature range of 69 °C to 95 °C with 0.3 °C/s intervals. All measurements were carried out in 3 biological replicates, each in technical duplicates.
4.8. Galleria Mellonella Larvae Toxicity Assay
The greater wax moth larvae were obtained from Biosystems (Biosystems Technology, Crediton, UK). Groups of 16 larvae in the final instar stage weighing between 180 and 350 mg were used for each experimental condition. The larvae were injected in the last left proleg with 10 µL of the carboxypyrano-ant extract or carboxypyCy-3-glc at 25 and 50 mg/kg. Controls included a group of larvae that did not receive any injection and another group of larvae that were injected with 10 µL of PBS. The larvae were then incubated in the dark at 37 °C and they were assessed daily for survival for up to 7 days post-injection. The larvae were considered dead when no movement was displayed in response to any stimulation by touch. Two independent experiments were performed for each condition.
4.9. Statistical Analysis
The results regarding the inhibition of biofilm formation, C. violaceum assay and toxicity assessment in G. mellonella are expressed as mean values ± standard error of the mean (SEM). The statistical significance of differences between controls and experimental groups was determined using Student’s t-test and p values < 0.05 were considered statistically significant.
Regarding the RT-qPCR analyses, the Q software (Quantabio, Beverly, MA, USA) generated the cycle-threshold (Ct) values, and then the relative levels of gene expression were calculated by the ∆∆Ct method, using the rpoS or 16S rRNA genes as internal controls (reference genes) for P. aeruginosa or S. aureus, respectively, as follows (Equations (2)–(4)):
| ∆Ct (control) = Ct Gene of interest (control) − Ct Reference Gene (control) | (2) |
| ∆Ct (treated) = Ct Gene of interest (treated) – Ct Reference Gene (treated), | (3) |
| ∆∆Ct = ∆Ct (treated) − ∆Ct (control), | (4) |
results are expressed as ∆∆Ct ± confidence interval at 95% confidence. If the confidence interval does not include the null value (zero), then we concluded that there was a statistically significant difference between the groups. The statistical analyses were performed in Microsoft Excel and RStudio.
5. Conclusions
In this study, we have explored one pyranoanthocyanin, carboxypyCy-3-glc, and one extract, carboxypyrano-ant extract, and found that they both could (i) strongly impair the biofilm formation by S. aureus multidrug-resistant isolates, while not evidently affecting P. aeruginosa biofilm formation; (ii) interfere with QS signaling in both P. aeruginosa and S. aureus, even if at different levels; and (iii) show low toxicity in the in vivo larvae model of G. mellonella. Although their mechanism of action is still to be unraveled, these compounds appear to be promising in interfering with the QS system of both susceptible and MDR strains of P. aeruginosa and S. aureus. Nonetheless, more in-depth studies (e.g., proteomics, transcriptomics, in silico analysis) need to be conducted with several other pathogenic bacterial strains, susceptible and MDR, to assess the potential of these compounds in inhibiting QS, and by which mechanism, and thus in impairing virulence factors production and biofilm formation.
The obtainment process of an extract is simpler and shorter than that of a pure compound, and therefore, could be an advantage for the extract use over the pure compound when both have a similar activity. The carboxypyrano-ant extract interfered with the QS systems of both P. aeruginosa and S. aureus, thus, it may hold potential in further research and development of novel products aiming at effectively restraining the pathogenicity of strains responsible for causing biofilm-associated cutaneous infections, particularly those related to chronic infected wounds.
6. Patents
Provisional patent application N. 117058: Process for extraction and hemi-synthesis of pyranoanthocyanins and skincare cosmetic formulations containing them.
Acknowledgments
This work was financial supported by the project PTDC/QUI-OUT/29013/2017 funded by FCT and FEDER., P.A. and A.R.P. gratefully acknowledge their doctoral grants from FCT (SFRH/BD/143309/2019 and SFRH/BD/146549/2019, respectively). J.O. would like to thank the FCT for her IF contract (IF/00225/2015), I.F for her research contract (SFRH/BPD/86173/2012). Authors thank Ângelo Mendes from Institute of Biodiversity, Animal Health and Comparative Medicine, University of Glasgow for his support with statistical analysis in RStudio.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijms22168559/s1.
Author Contributions
Conceptualization, L.J.B., I.F. and J.O.; methodology, P.C., L.J.B., I.F., J.O., P.A. and A.R.P.; validation, P.C., P.A. and A.R.P.; formal analysis, P.C. and L.J.B.; investigation, P.C. and L.J.B.; resources, P.G., I.F. and J.O.; data curation, P.C.; writing—original draft preparation, P.C. and L.J.B.; writing—review and editing, P.C., I.F., J.O. and L.J.B.; visualization, P.C. and L.J.B.; supervision, L.J.B.; project administration, I.F., J.O. and L.J.B.; funding acquisition, I.F., J.O. and P.G. All authors have read and agreed to the published version of the manuscript.
Funding
This work was financed by National Funds through FCT/MCTES—Portuguese Foundation for Science and Technology within the scope of the project UIDB/50006/2020.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are openly available in [FigShare] at [doi], reference number [10.6084/m9.figshare.14912460].
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.O’Neill J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations The Review on Antimicrobial Resistance. [(accessed on 15 April 2020)];2016 Available online: https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf.
- 2.WHO Global Action Plan on Antimicrobial Resistance. Microbe. 2015;10:354–355. doi: 10.1128/microbe.10.354.1. [DOI] [Google Scholar]
- 3.WHO Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics. [(accessed on 20 October 2020)];2017 Available online: https://www.who.int/medicines/publications/WHO-PPL-Short_Summary_25Feb-ET_NM_WHO.pdf.
- 4.Rossiter S.E., Fletcher M.H., Wuest W.M. Natural Products as Platforms to Overcome Antibiotic Resistance. Chem. Rev. 2017;117:12415–12474. doi: 10.1021/acs.chemrev.7b00283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dodds D.R. Antibiotic Resistance: A Current Epilogue. Biochem. Pharmacol. 2017;134:139–146. doi: 10.1016/j.bcp.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Allegretta G., Maurer C.K., Eberhard J., Maura D., Hartmann R.W., Rahme L., Empting M. In-Depth Profiling of MvfR-Regulated Small Molecules in Pseudomonas aeruginosa after Quorum Sensing Inhibitor Treatment. Front. Microbiol. 2017;8:924. doi: 10.3389/fmicb.2017.00924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abisado R.G., Benomar S., Klaus J.R., Dandekar A.A., Chandler J.R. Bacterial Quorum Sensing and Microbial Community Interactions. mBio. 2018;9:e02331-17. doi: 10.1128/mBio.02331-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bäuerle T., Fischer A., Speck T., Bechinger C. Self-Organization of Active Particles by Quorum Sensing Rules. Nat. Commun. 2018;9:3232. doi: 10.1038/s41467-018-05675-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turan N.B., Chormey D.S., Büyükpınar Ç., Engin G.O., Bakirdere S. Quorum Sensing: Little Talks for an Effective Bacterial Coordination. TrAC Trend Anal. Chem. 2017;91:1–11. doi: 10.1016/j.trac.2017.03.007. [DOI] [Google Scholar]
- 10.Butrico C.E., Cassat J.E. Quorum Sensing and Toxin Production in Staphylococcus aureus Osteomyelitis: Pathogenesis and Paradox. Toxins. 2020;12:516. doi: 10.3390/toxins12080516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Papenfort K., Bassler B.L. Quorum Sensing Signal-Response Systems in Gram-Negative Bacteria. Nat. Rev. Microbiol. 2016;14:576–588. doi: 10.1038/nrmicro.2016.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jiang Y., Geng M., Bai L. Targeting Biofilms Therapy: Current Research Strategies and Development Hurdles. Microorganisms. 2020;8:1222. doi: 10.3390/microorganisms8081222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiang Q., Chen J., Yang C., Yin Y., Yao K., Song D. Quorum Sensing: A Prospective Therapeutic Target for Bacterial Diseases. Biomed. Res. Int. 2019;2019:2015978. doi: 10.1155/2019/2015978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paczkowski J.E., Mukherjee S., McCready A.R., Cong J.P., Aquino C.J., Kim H., Henke B.R., Smith C.D., Bassler B.L. Flavonoids Suppress Pseudomonas aeruginosa Virulence through Allosteric Inhibition of Quorum-Sensing Receptors. Int. J. Biol. Chem. 2017;292:4064–4076. doi: 10.1074/jbc.M116.770552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palliyil S., Downham C., Broadbent I., Charlton K., Porter A.J. High-Sensitivity Monoclonal Antibodies Specific for Homoserine Lactones Protect Mice from Lethal Pseudomonas aeruginosa Infections. Appl Environ. Microbiol. 2014;80:462–469. doi: 10.1128/AEM.02912-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soh E.Y.C., Chhabra S.R., Halliday N., Heeb S., Müller C., Birmes F.S., Fetzner S., Cámara M., Chan K.G., Williams P. Biotic Inactivation of the Pseudomonas aeruginosa Quinolone Signal Molecule. Environ. Microbiol. 2015;17:4352–4365. doi: 10.1111/1462-2920.12857. [DOI] [PubMed] [Google Scholar]
- 17.Truchado P., Larrosa M., Castro-Ibáñez I., Allende A. Plant Food Extracts and Phytochemicals: Their Role as Quorum Sensing Inhibitors. Trends Food Sci. Technol. 2015;43:189–204. doi: 10.1016/j.tifs.2015.02.009. [DOI] [Google Scholar]
- 18.Gopu V., Kothandapani S., Shetty P.H. Quorum Quenching Activity of Syzygium cumini (L.) Skeels and Its Anthocyanin Malvidin against Klebsiella pneumoniae. Microb. Pathog. 2015;79:61–69. doi: 10.1016/j.micpath.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Deryabin D., Galadzhieva A., Kosyan D., Duskaev G. Plant-Derived Inhibitors of AHL-Mediated Quorum Sensing in Bacteria: Modes of Action. Int. J. Mol. Sci. 2019;20:5588. doi: 10.3390/ijms20225588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gopu V., Shetty P.H. Cyanidin Inhibits Quorum Signalling Pathway of a Food Borne Opportunistic Pathogen. J. Food Sci. Technol. 2016;53:968–976. doi: 10.1007/s13197-015-2031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang Y., Wang F., Bao X., Feng J., Fu L. Inhibition of Biogenic Amines in Shewanella baltica by Anthocyanins Involving a Quorum Sensing System. J. Food Prot. 2019;82:589–596. doi: 10.4315/0362-028X.JFP-18-445. [DOI] [PubMed] [Google Scholar]
- 22.Pejin B., Ciric A., Dimitric Markovic J., Glamoclija J., Nikolic M., Sokovic M. An Insight into Anti-Biofilm and Anti-Quorum Sensing Activities of the Selected Anthocyanidins: The Case Study of Pseudomonas aeruginosa PAO1. Nat. Prod. Res. 2017;31:1177–1180. doi: 10.1080/14786419.2016.1222386. [DOI] [PubMed] [Google Scholar]
- 23.Kordbacheh H., Eftekhar F., Ebrahimi S.N. Anti-Quorum Sensing Activity of Pistacia atlantica against Pseudomonas aeruginosa PAO1 and Identification of Its Bioactive Compounds. Microb. Pathog. 2017;110:390–398. doi: 10.1016/j.micpath.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 24.Correia P., Araújo P., Ribeiro C., Oliveira H., Pereira A.R., Mateus N., de Freitas V., Brás N.F., Gameiro P., Coelho P., et al. Anthocyanin-Related Pigments: Natural Allies for Skin Health Maintenance and Protection. Antioxidants. 2021;10:1038. doi: 10.3390/antiox10071038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Monnet V., Gardan R. Quorum-Sensing Regulators in Gram-Positive Bacteria: “Cherchez Le Peptide. ” Mol. Microbiol. 2015;97:181–184. doi: 10.1111/mmi.13060. [DOI] [PubMed] [Google Scholar]
- 26.Hemmati F., Salehi R., Ghotaslou R., Kafil H.S., Hasani A., Gholizadeh P., Nouri R., Rezaee M.A. Quorum Quenching: A Potential Target for Antipseudomonal Therapy. Infect. Drug Resist. 2020;13:2989–3005. doi: 10.2147/IDR.S263196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rutherford S.T., Bassler B.L. Bacterial Quorum Sensing: Its Role in Virulence and Possibilities for Its Control. Cold Spring Harb. Perspect. Med. 2012;2:a012427. doi: 10.1101/cshperspect.a012427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li S., Chen S., Fan J., Cao Z., Ouyang W., Tong N., Hu X., Hu J., Li P., Feng Z., et al. Anti-Biofilm Effect of Novel Thiazole Acid Analogs against Pseudomonas aeruginosa through IQS Pathways. Eur. J. Med. Chem. 2018;145:64–73. doi: 10.1016/j.ejmech.2017.12.076. [DOI] [PubMed] [Google Scholar]
- 29.Fong J., Yuan M., Jakobsen T.H., Mortensen K.T., Delos Santos M.M.S., Chua S.L., Yang L., Tan C.H., Nielsen T.E., Givskov M. Disulfide Bond-Containing Ajoene Analogues As Novel Quorum Sensing Inhibitors of Pseudomonas aeruginosa. J. Med. Chem. 2017;60:215–227. doi: 10.1021/acs.jmedchem.6b01025. [DOI] [PubMed] [Google Scholar]
- 30.Pérez-Pérez M., Jorge P., Pérez Rodríguez G., Pereira M.O., Lourenço A. Quorum Sensing Inhibition in Pseudomonas aeruginosa Biofilms: New Insights through Network Mining. Biofouling. 2017;33:128–142. doi: 10.1080/08927014.2016.1272104. [DOI] [PubMed] [Google Scholar]
- 31.Sun S., Zhou L., Jin K., Jiang H., He Y.W. Quorum Sensing Systems Differentially Regulate the Production of Phenazine-1-Carboxylic Acid in the Rhizobacterium Pseudomonas aeruginosa PA1201. Sci. Rep. 2016;6:30352. doi: 10.1038/srep30352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Feltner J.B., Wolter D.J., Pope C.E., Groleau M.C., Smalley N.E., Greenberg E.P., Mayer-Hamblett N., Burns J., Déziel E., Hoffman L.R., et al. LasR Variant Cystic Fibrosis Isolates Reveal an Adaptable Quorum-Sensing Hierarchy in Pseudomonas aeruginosa. mBio. 2016;7:e01513-16. doi: 10.1128/mBio.01513-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee J., Zhang L. The Hierarchy Quorum Sensing Network in Pseudomonas aeruginosa. Protein Cell. 2014;6:26–41. doi: 10.1007/s13238-014-0100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jenul C., Horswill A.R. Regulation of Staphylococcus aureus Virulence. Microbiol. Spectr. 2019;7:7. doi: 10.1128/microbiolspec.GPP3-0031-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin M.F., Lin Y.Y., Tu C.C., Lan C.Y. Distribution of Different Efflux Pump Genes in Clinical Isolates of Multidrug-Resistant Acinetobacter baumannii and Their Correlation with Antimicrobial Resistance. J. Microbiol. Immunol. Infect. 2017;50:224–231. doi: 10.1016/j.jmii.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 36.Martinez J.L. General Principles of Antibiotic Resistance in Bacteria. Drug Discov. Today Technol. 2014;11:33–39. doi: 10.1016/j.ddtec.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 37.Pontes D.S., de Araujo R.S.A., Dantas N., Scotti L., Scotti M.T., de Moura R.O., Mendonca-Junior F.J.B. Genetic Mechanisms of Antibiotic Resistance and the Role of Antibiotic Adjuvants. Curr. Top. Med. Chem. 2018;18:42–74. doi: 10.2174/1568026618666180206095224. [DOI] [PubMed] [Google Scholar]
- 38.Cho H.S., Lee J.H., Cho M.H., Lee J. Red Wines and Flavonoids Diminish Staphylococcus aureus Virulence with Anti-Biofilm and Anti-Hemolytic Activities. Biofouling. 2015;31:37–41. doi: 10.1080/08927014.2014.991319. [DOI] [PubMed] [Google Scholar]
- 39.Kumar P., Lee J.H., Beyenal H., Lee J. Fatty Acids as Antibiofilm and Antivirulence Agents. Trends Microbiol. 2020;28:753–768. doi: 10.1016/j.tim.2020.03.014. [DOI] [PubMed] [Google Scholar]
- 40.Saidi N., Owlia P., Marashi S.M.A., Saderi H. Inhibitory Effect of Probiotic Yeast Saccharomyces cerevisiae on Biofilm Formation and Expression of α-Hemolysin and Enterotoxin A Genes of Staphylococcus aureus. Iran. J. Microbiol. 2019;11:246–254. doi: 10.18502/ijm.v11i3.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kothari V., Sharma S., Padia D. Recent Research Advances on Chromobacterium violaceum. Asian Pac. J. Trop. Med. 2017;10:744–752. doi: 10.1016/j.apjtm.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 42.Devescovi G., Kojic M., Covaceuszach S., Cámara M., Williams P., Bertani I., Subramoni S., Venturi V. Negative Regulation of Violacein Biosynthesis in Chromobacterium violaceum. Front. Microbiol. 2017;8:349. doi: 10.3389/fmicb.2017.00349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mok N., Chan S.Y., Liu S.Y., Chua S.L. Vanillin Inhibits PqsR-Mediated Virulence in Pseudomonas aeruginosa. Food Funct. 2020;11:6496–6508. doi: 10.1039/D0FO00046A. [DOI] [PubMed] [Google Scholar]
- 44.Groleau M.-C., de Oliveira Pereira T., Dekimpe V., Déziel E. PqsE Is Essential for RhlR-Dependent Quorum Sensing Regulation in Pseudomonas aeruginosa. mSystems. 2020;5:e00194-20. doi: 10.1128/mSystems.00194-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mukherjee S., Moustafa D.A., Stergioula V., Smith C.D., Goldberg J.B., Bassler B.L. The PqsE and RhlR Proteins Are an Autoinducer Synthase–Receptor Pair That Control Virulence and Biofilm Development in Pseudomonas aeruginosa. Proc. Natl. Acad. Sci. USA. 2018;115:9411–9418. doi: 10.1073/pnas.1814023115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kostylev M., Kim D.Y., Smalley N.E., Salukhe I., Peter Greenberg E., Dandekar A.A. Evolution of the Pseudomonas aeruginosa Quorum-Sensing Hierarchy. Proc. Natl. Acad. Sci. USA. 2019;116:7027–7032. doi: 10.1073/pnas.1819796116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Okkotsu Y., Tieku P., Fitzsimmons L.F., Churchill M.E., Schurr M.J. Pseudomonas aeruginosa AlgR Phosphorylation Modulates Rhamnolipid Production and Motility. J. Bacteriol. 2013;195:5499–5515. doi: 10.1128/JB.00726-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen R., Déziel E., Groleau M.-C., Schaefer A.L., Greenberg E.P. Social Cheating in a Pseudomonas aeruginosa Quorum-Sensing Variant. Proc. Natl. Acad. Sci. USA. 2019;116:7021–7026. doi: 10.1073/pnas.1819801116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dastgheyb S.S., Villaruz A.E., Le K.Y., Tan V.Y., Duong A.C., Chatterjee S.S., Cheung G.Y.C., Joo H.S., Hickok N.J., Otto M. Role of Phenol-Soluble Modulins in Formation of Staphylococcus aureus Biofilms in Synovial Fluid. Infect. Immun. 2015;83:2966–2975. doi: 10.1128/IAI.00394-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang R., Khan B.A., Cheung G.Y.C., Bach T.H.L., Jameson-Lee M., Kong K.F., Queck S.Y., Otto M. Staphylococcus epidermidis Surfactant Peptides Promote Biofilm Maturation and Dissemination of Biofilm-Associated Infection in Mice. J. Clin. Investig. 2011;121:238–248. doi: 10.1172/JCI42520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zielinska A.K., Beenken K.E., Joo H.S., Mrak L.N., Griffin L.M., Luong T.T., Lee C.Y., Otto M., Shaw L.N., Smeltzer M.S. Defining the Strain-Dependent Impact of the Staphylococcal accessory regulator (SarA) on the Alpha-Toxin Phenotype of Staphylococcus aureus. J. Bacteriol. 2011;193:2948–2958. doi: 10.1128/JB.01517-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Omidi M., Firoozeh F., Saffari M., Sedaghat H., Zibaei M., Khaledi A. Ability of Biofilm Production and Molecular Analysis of spa and ica Genes among Clinical Isolates of Methicillin-Resistant Staphylococcus aureus. BMC Res. Notes. 2020;13:19. doi: 10.1186/s13104-020-4885-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Montgomery C.P., Boyle-Vavra S., Roux A., Ebine K., Sonenshein A.L., Daumb R.S. CodY Deletion Enhances in vivo Virulence of Community-Associated Methicillin-Resistant Staphylococcus aureus Clone USA300. Infect. Immun. 2012;80:2382–2389. doi: 10.1128/IAI.06172-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cassat J.E., Hammer N.D., Campbell J.P., Benson M.A., Perrien D.S., Mrak L.N., Smeltzer M.S., Torres V.J., Skaar E.P. A Secreted Bacterial Protease Tailors the Staphylococcus aureus Virulence Repertoire to Modulate Bone Remodeling during Osteomyelitis. Cell Host Microbe. 2013;13:759–772. doi: 10.1016/j.chom.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kolar S.L., Antonio Ibarra J., Rivera F.E., Mootz J.M., Davenport J.E., Stevens S.M., Horswill A.R., Shaw L.N. Extracellular Proteases Are Key Mediators of Staphylococcus aureus Virulence via the Global Modulation of Virulence-Determinant Stability. Microbiol. 2013;2:18–34. doi: 10.1002/mbo3.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lozano C., Azcona-Gutiérrez J.M., van Bambeke F., Sáenz Y. Great Phenotypic and Genetic Variation among Successive Chronic Pseudomonas aeruginosa from a Cystic Fibrosis Patient. PLoS ONE. 2018;13:e0204167. doi: 10.1371/journal.pone.0204167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tan L., Li S.R., Jiang B., Hu X.M., Li S. Therapeutic Targeting of the Staphylococcus aureus Accessory Gene Regulator (Agr) System. Front. Microbiol. 2018;9:55. doi: 10.3389/fmicb.2018.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Oliveira J., Fernandes V., Miranda C., Santos-Buelga C., Silva A., de Freitas V., Mateus N. Color Properties of Four Cyanidin-Pyruvic Acid Adducts. J. Agric. Food Chem. 2006;54:6894–6903. doi: 10.1021/jf061085b. [DOI] [PubMed] [Google Scholar]
- 59.Bessa L.J., Eaton P., Dematei A., Plácido A., Vale N., Gomes P., Delerue-Matos C., Leite J.R.S.A., Gameiro P. Synergistic and Antibiofilm Properties of Ocellatin Peptides against Multidrug-Resistant Pseudomonas aeruginosa. Future Microbiol. 2018;13:151–163. doi: 10.2217/fmb-2017-0175. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are openly available in [FigShare] at [doi], reference number [10.6084/m9.figshare.14912460].