Abstract
Background
The very long-term consequences of absence of remission in lupus nephritis (LN) remain understudied.
Methods
In this retrospective analysis, we studied a selected cohort of 128 patients with biopsy-proven class III, IV or V incident LN followed for a median period of 134 months (minimum 25). Remission was defined as a urine protein to creatinine (uP:C) ratio <0.5 g/g and a serum creatinine value <120% of baseline. Renal relapse was defined as the reappearance of a uP:C >1 g/g, leading to a repeat kidney biopsy and treatment change. Poor long-term renal outcome was defined as the presence of chronic kidney disease (CKD).
Results
Twenty per cent of patients never achieved renal remission. Their baseline characteristics did not differ from those who did. Absence of renal remission was associated with a threefold higher risk of CKD (48% vs 16%) and a 10-fold higher risk of end-stage renal disease (20% vs 2%). Patients achieving early remission had significantly higher estimated glomerular filtration rate (eGFR) at last follow-up compared with late remitters. Accordingly, patients with CKD at last follow-up had statistically longer time to remission. Among patients who achieved remission, 32% relapsed, with a negative impact on renal outcome, that is, lower eGFR values and higher proportion of CKD (33% vs 8%).
Conclusion
Early remission should be achieved to better preserve long-term renal function.
Keywords: lupus nephritis, outcome assessment, health care, lupus erythematosus, systemic
Key messages.
What is already known about this subject?
Recent clinical trials in lupus nephritis are focusing on achieving early remission.
Yet the very long-term consequences of absence of remission or late remission are understudied.
What does this study add?
We took advantage of our incident lupus nephritis cohort with long-term follow-up to highlight the burden of absence of remission.
Late remission is also associated with poorest long-term outcome.
How might this impact on clinical practice or future developments?
Early remission is thus a relevant endpoint for future clinical trials and an important goal in every patient at bedside.
Introduction
Chronic kidney disease (CKD) remains one of the major challenges in lupus nephritis (LN), with 20%–60% of patients developing renal impairment with significant impact on morbidity, mortality and quality of life.1 2
Achievement of renal remission is one of the main therapeutic goals, as illustrated by recent LN trials aimed at testing new drugs used in combination with standard-of-care immunosuppression.3–5 By achieving higher rates of early remission, the hope is to reduce the percentage of patients with LN with CKD in the long term. Yet the long-term consequences of achieving remission or not and of achieving early versus late remission are understudied.
To address this issue, we took advantage of our cohort of incident LN cases followed over a very long period in a single tertiary centre in Brussels. More specifically, we retrospectively studied our cases of incident LN for whom sufficient data were available over a prolonged period of time to investigate whether achieving remission, in particular early remission, correlates with a better renal outcome.
Patients and methods
Patient selection
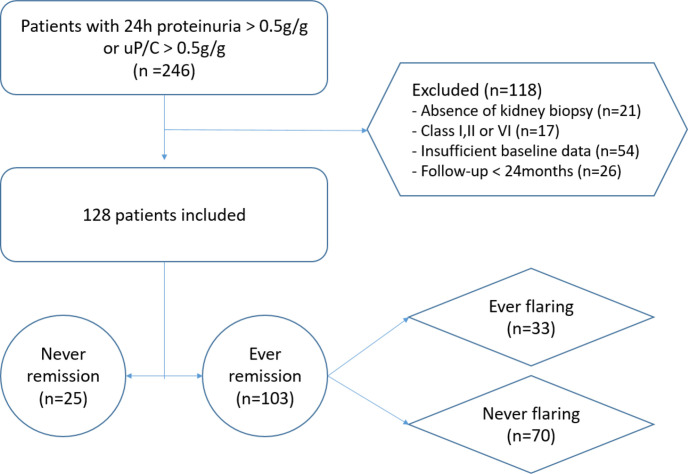
Between 1989 and 2020, 246 incident cases of LN were diagnosed at the Cliniques Universitaires Saint-Luc. All had a proteinuria >0.5 g/L in a 24-hour urine collection or a urine protein to creatinine (uP:C) ratio >0.5 g/g. As shown in figure 1, for the purpose of this analysis, we excluded patients who did not have a renal biopsy at the time proteinuria was discovered (21 of 246), those with International Society of Nephrology/Renal Pathological Society (ISN/RPS) class I, II and VI, or with insufficient baseline data, as well as patients who had a follow-up <24 months. At the end of this selection process, 128 patients were retrieved.
Figure 1.
Patients’ disposition. uP:C, urine protein to creatinine ratio.
Outcomes
Renal remission was defined by a uP:C value <0.5 g/g (on at least two subsequent samples) combined with a serum creatinine value <120% of baseline. Renal relapse was defined as the reappearance of a uP:C >1 g/g, leading to a repeat kidney biopsy and intensification or change of the immunosuppressive regimen. Poor long-term renal outcome was defined as CKD at last follow-up, that is, an estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m².
Histological analysis
Biopsies were classified according to the ISN/RPS 2003 classification criteria.6
Activity and chronicity indices (AI and CI) were computed according to a semiquantitative scoring system proposed by Morel-Maroger et al.7 Briefly, in the Morel-Maroger et al7 scoring system, AI is based on scoring of four hyperactive lesions (gross haematoxylin bodies, circumferential crescents, glomerular necrosis and necrotising angiitis) and six activity lesions (endocapillary proliferation, partial crescents, wire loops, hyaline thrombi, nuclear debris and acute tubulointerstitial lesions), graded from 0 to 3 (graded 0–3: absent, mild, moderate and severe), with hyperactive lesions weighted by a factor of 2 since they are considered more representative of the intensity of activity. The maximum AI score is 42. CI is the sum of two types of chronic lesions graded from 0 to 3 (glomerular and interstitial fibrosis); the maximum score is therefore 6.
Statistical analysis
χ2 test, Fisher’s exact test, unpaired t-test and Mann-Whitney test were performed as appropriate with GraphPad Prism V.5.0. Survival curves, drawn according to Kaplan-Meier method, were statistically tested by log-rank test.
Results
Patient characteristics
We studied 128 cases of incident LN, selected as described in figure 1. The mean age (±SD) at diagnosis was 30.3 years and 91% of patients were women. Most (73%) were Caucasians, followed by Africans (10%), North Africans (9%) and Asians (7%). Most cases accounted for ISN/RPS class III or IV proliferative glomerulonephritis (91%), with 31 class III and 86 class IV. They were associated with class V in 24% of the cases. Only 11 cases of isolated class V (9%) were diagnosed. Initial immunosuppressive therapy was based on intravenous cyclophosphamide in most cases (75%), while 22 patients received mycophenolate mofetil and 3 other treatments. Of the patients, 74% received intravenous methylprednisolone (95 out of 128). The median follow-up time was 134 months, with extremes ranging from 25 to 371 months. At last follow-up, 29 patients (23%) suffered from CKD, of whom 7 (6%) reached end-stage renal disease (ESRD).
Comparison of patients ever or never achieving renal remission
Twenty per cent of patients never achieved renal remission, without association with age, gender or ethnicity (data not shown). As detailed in table 1, the baseline characteristics of patients achieving remission or not did not differ, except for a slightly lower serum C3 level in patients who remit. Titres of serum anti-DNA antibodies (by Farr assay) at baseline did not differ between the two groups, nor did the histological subsets. CI was higher in patients not achieving remission. Patients who achieved remission received slightly higher initial oral doses of prednisolone. At last follow-up, patients never achieving remission were statistically more likely to suffer from CKD (48% vs 16%) and ESRD (20% vs 2%).
Table 1.
Baseline characteristics and long-term renal outcome of patients who will never remit, remit early or late
| Ever remission n=103 |
Never remission n=25 |
P value | Early remission n=52 |
Late remission n=51 |
P value | |
| Baseline characteristics | ||||||
| Serum creatinine (mg/dL) | 0.96 (0.4) | 1.11 (0.6) | 0.29 | 0.96 (0.4) | 0.96 (0.4) | 0.7 |
| eGFR (mL/min/1.73 m2) | 94.3 (34) | 86.8 (40) | 0.44 | 94.4 (34) | 94.2 (34) | 0.89 |
| uP:C (g/g) | 3.04 (2.7) | 3.84 (3.2) | 0.21 | 2.66 (2.3) | 3.43 (3.1) | 0.08 |
| C3 (g/L) | 0.58 (0.27) | 0.72 (0.35) | 0.05 | 0.57 (0.27) | 0.59 (0.27) | 0.84 |
| C4 (g/L) | 0.1 (0.06) | 0.09 (0.04) | 0.66 | 0.08 (0.04) | 0.10 (0.07) | 0.14 |
| Activity index, median (range) | 7 (0–22) | 7 (0–21) | 0.9 | 6 (1–22) | 10 (0–19) | 0.15 |
| Chronicity index, median (range) | 0 (0–3) | 1 (0–2) | 0.02 | 0 (0–3) | 0 (0–2) | 0.82 |
| Intravenous MP dose (g) | 1.85 (1.3) | 1.83 (1.4) | 0.41 | 1.89 (1.0) | 1.8 (1.4) | 0.73 |
| Oral prednisolone intake (mg) | 37 (17) | 29.7 (19) | 0.03 | 37.2 (17) | 36.9 (18) | 0.93 |
| Decade of diagnosis, n patients (%) | 0.16 | 0.81 | ||||
| 1989–1999 | 20 (19) | 3 (12) | 9 (17) | 11 (21) | ||
| 2000–2009 | 51 (50) | 9 (36) | 27 (52) | 24 (27) | ||
| 2010–2020 | 32 (31) | 13 (52) | 16 (31) | 16 (32) | ||
| Last follow-up | ||||||
| Follow-up (months), median (range) | 138 (25–371) | 71 (25–303) | 0.02 | 136 (25–349) | 147 (28–371) | 0.87 |
| eGFR (mL/min/1.73 m2) | 95 (27) | 77 (37) | 0.03 | 101 (23) | 88 (29) | 0.03 |
| CKD, n patients (%) | 17 (16) | 12 (48) | 0.002 | 6 (12) | 11 (21) | 0.19 |
| ESRD, n patients (%) | 2 (2) | 5 (20) | 0.003 | 1 (2) | 1 (2) | 1.00 |
| Death, n patients (%) | 3 (3) | 3 (12) | 0.08 | 2 (4) | 1 (2) | 1.00 |
Unless stated otherwise, values are mean±SD.
Patients achieving remission were divided into two subgroups (early and late remission) using median time to remission (ie, 7 months) as cut-off.
P value <0.05 was considered statistically significant.
CKD, chronic kidney disease, ie, eGFR <60 mL/min/m²; eGFR, estimated glomerular filtration rate; ESRD, end-stage renal disease, ie, requiring dialysis or transplantation; MP, methylprednisolone; uP:C, urine protein to creatinine ratio.
Comparison of patients achieving early or late renal remission
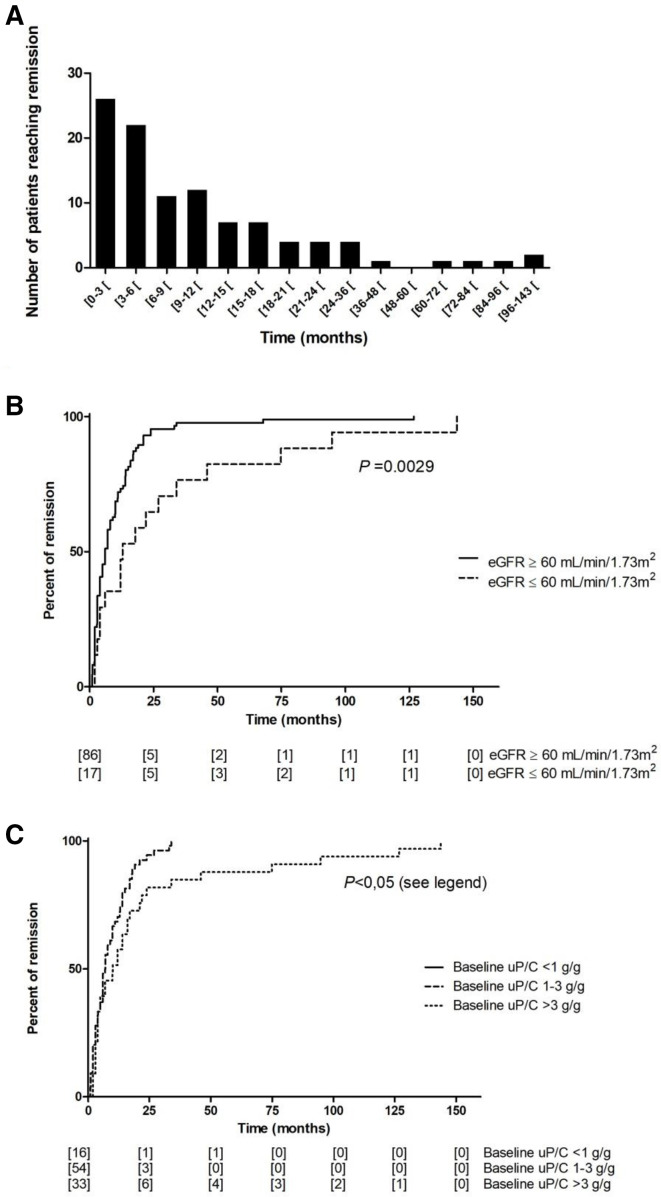
The mean (SD) and median (range) time to remission, observed in 80% of patients, were 14 (23) and 7 (1–144) months, respectively. Remission was achieved within the first year of treatment in 71 patients (69% of patients ever achieving remission) (figure 2A).
Figure 2.
Time to remission. (A) Histogram representing the number of patients achieving remission within the time intervals indicated between the brackets (months). (B) Kaplan-Meier analysis of time to remission in patients with good or poor renal outcome at last follow-up, defined by the absence or presence of chronic kidney disease (eGFR ≥60 or <60 mL/min/1.73 m2). Number between brackets along the abscissa corresponds to the number of patients at risk. (C) Kaplan-Meier analysis of time to remission according to baseline proteinuria (uP:C <1 g/g, between 1 g/g and 3 g/g and >3 g/g). Number between brackets along the abscissa corresponds to the number of patients at risk. Baseline uP:C >3 g/g group had a significantly different time to remission compared with baseline uP:C 1–3 g/g group (p=0.02) and baseline uP:C <1 g/g group (p=0.01). eGFR, estimated glomerular filtration rate; uP:C, urine protein to creatinine ratio. IV MP, Intravenous Methylprednisolone; CKD, Chronic Kidney Disease, i.e. eGFR <60 mL/min/m²; ESRD, End Stage Renal Disease, i.e. requiring dialysis or transplantation.
We compared early versus late remitting patients using the median time to remission as cut-off. As indicated in table 1, none of the baseline characteristics, including serum creatinine and proteinuria, differed between the two groups. Interestingly, more patients achieving late remission suffered from CKD at last-follow-up, although the difference was not statistically significant, and their mean eGFR was significantly lower compared with patients achieving early remission. Accordingly, time to remission was statistically longer in patients with CKD at last follow-up (figure 2B), with a median time to remission of 6 months (for patients without CKD) vs 12 months (for patients with CKD) (p=0.003). As expected, remission was achieved earlier in patients with lower baseline proteinuria (figure 2C).
Renal flares in patients achieving remission
As indicated in figure 1, one-third (32%) of the patients achieving remission suffered from at least one renal flare, without differences between early (33%) or late (31%) remitters. As expected, flaring patients had poorer renal outcome, with lower mean eGFR values at last follow-up (85 vs 99 mL/min/1.73 m2, p=0.02) and a higher proportion of CKD (33% vs 8%, p=0.001).
Discussion
The very long-term follow-up of our incident LN cohort demonstrates that absence of renal remission during the course of the disease has a major impact on renal outcome, with a threefold higher rate of CKD and a 10-fold higher rate of ESRD in patients never achieving renal remission. Moreover, our data indicate that a shorter time to renal remission is associated with a better outcome. Strikingly, patients with early remission had 13 mL/min/1.73 m2 higher mean eGFR at last-follow-up, a relevant difference in a young population regarding long-term preservation of renal function.
The retrospective nature of our study obviously limits the strength of these conclusions. Yet it should be stressed that the cohort of patients with LN discussed here was followed in the same single tertiary centre, supervised by the same senior clinician applying similar follow-up methods and up-to-date therapeutic recommendations over three decades. Actually, only such long-term clinical research, performed in an academic setting, allows unmasking of the real-world rates of CKD and ESRD caused by LN.
It is unfortunate that we were not able to identify patients at baseline who will never achieve remission. Our previous studies have demonstrated that an early decrease in proteinuria has a very high positive predictive value for a good long-term renal outcome,8 9 which was confirmed by others.10 Of note, the importance of a prompt decrease in proteinuria for a good long-term outcome was also observed in this series since patients achieving a uP:C target <0.7 g/g at month 12 had a significantly higher eGFR (94 vs 75 mL/min/1.73 m2, p=0.017) and tended to have a lower rate of CKD (11% vs 27%, p=0.11) at last follow-up compared with patients who did not reach the proteinuria target.
The observation that patients ever achieving remission had received a slightly higher initial oral dose of glucocorticoids (GC) is challenging,11 but likely explained by the fact that a (non-significant) higher percentage of patients in this subgroup were treated during a previous decade, when higher doses of GC were prescribed. In our view, this observation, yet worth mentioning, does not indicate a causal relationship.
Taken together, the data presented here strongly suggest that remission is a very appropriate therapeutic goal. In this respect, the results of three recent controlled clinical trials demonstrating a 10%–20% higher rate of renal remission in patients given combination therapy with belimumab,3 voclosporin4 or obinutuzumab5 are most welcome after decades of use of standard immunosuppression with cyclophosphamide, azathioprine or mycophenolate mofetil, which are associated with only a 25% rate of renal remission after 6 months of treatment.12
Footnotes
VP and AE contributed equally.
Contributors: VP collected the data. VP and AE performed the statistical analysis. All authors discussed the results and contributed to the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; internally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Almaani S, Meara A, Rovin BH. Update on lupus nephritis. CJASN 2017;12:825–35. 10.2215/CJN.05780616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cervera R, Khamashta MA, Font J, et al. Morbidity and mortality in systemic lupus erythematosus during a 10-year period: a comparison of early and late manifestations in a cohort of 1,000 patients. Medicine 2003;82:299–308. 10.1097/01.md.0000091181.93122.55 [DOI] [PubMed] [Google Scholar]
- 3.Furie R, Rovin BH, Houssiau F, et al. Two-Year, randomized, controlled trial of belimumab in lupus nephritis. N Engl J Med 2020;383:1117–28. 10.1056/NEJMoa2001180 [DOI] [PubMed] [Google Scholar]
- 4.Rovin BH, Teng YKO, Ginzler EM, et al. Efficacy and safety of voclosporin versus placebo for lupus nephritis (Aurora 1): a double-blind, randomised, multicentre, placebo-controlled, phase 3 trial. The Lancet 2021;397:2070–80. 10.1016/S0140-6736(21)00578-X [DOI] [PubMed] [Google Scholar]
- 5.Furie R, Aroca G, Alvarez A. Two-Year results from a randomized, controlled study of Obinutuzumab for proliferative lupus nephritis. ACR meeting Abstracts, 2020. Available: https://acrabstracts.org/abstract/two-year-results-from-a-randomized-controlled-study-of-obinutuzumab-for-proliferative-lupus-nephritis/ [Accessed 05 Jul 2021].
- 6.Weening JJ, D'Agati VD, Schwartz MM, et al. The classification of glomerulonephritis in systemic lupus erythematosus revisited. J Am Soc Nephrol 2004;15:241–50. 10.1097/01.ASN.0000108969.21691.5D [DOI] [PubMed] [Google Scholar]
- 7.Morel-Maroger L, Méry JP, Droz D, et al. The course of lupus nephritis: contribution of serial renal biopsies. Adv Nephrol Necker Hosp 1976;6:79–118. [PubMed] [Google Scholar]
- 8.Tamirou F, Lauwerys BR, Dall'Era M, et al. A proteinuria cut-off level of 0.7 g/day after 12 months of treatment best predicts long-term renal outcome in lupus nephritis: data from the maintain nephritis trial. Lupus Sci Med 2015;2:e000123. 10.1136/lupus-2015-000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dall'Era M, Cisternas MG, Smilek DE, et al. Predictors of long-term renal outcome in lupus nephritis trials: lessons learned from the Euro-Lupus nephritis cohort. Arthritis Rheumatol 2015;67:1305–13. 10.1002/art.39026 [DOI] [PubMed] [Google Scholar]
- 10.Ugolini-Lopes MR, Seguro LPC, Castro MXF, et al. Early proteinuria response: a valid real-life situation predictor of long-term lupus renal outcome in an ethnically diverse group with severe biopsy-proven nephritis? Lupus Sci Med 2017;4:e000213. 10.1136/lupus-2017-000213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tselios K, Gladman DD, Al-Sheikh H, et al. Medium versus high initial prednisone dose for remission induction in lupus nephritis: a propensity score matched analysis. Arthritis Care Res 2021. 10.1002/acr.24592. [Epub ahead of print: 04 Mar 2021]. [DOI] [PubMed] [Google Scholar]
- 12.Appel GB, Contreras G, Dooley MA, et al. Mycophenolate mofetil versus cyclophosphamide for induction treatment of lupus nephritis. J Am Soc Nephrol 2009;20:1103–12. 10.1681/ASN.2008101028 [DOI] [PMC free article] [PubMed] [Google Scholar]