Abstract
Tumor necrosis factor-alpha (TNFα) can bind two distinct receptors (TNFR1/2). The transmembrane form (tmTNFα) preferentially binds to TNFR2. Upon tmTNFα cleavage by the TNF-alpha-converting enzyme (TACE), its soluble (sTNFα) form is released with higher affinity for TNFR1. This assortment empowers TNFα with a plethora of opposing roles in the processes of tumor cell survival (and apoptosis) and anti-tumor immune stimulation (and suppression), in addition to angiogenesis and metastases. Its functions and biomarker potential to predict cancer progression and response to immunotherapy are reviewed here, with a focus on lung cancer. By mining existing sequencing data, we further demonstrate that the expression levels of TNF and TACE are significantly decreased in lung adenocarcinoma patients, while the TNFR1/TNFR2 balance are increased. We conclude that the biomarker potential of TNFα alone will most likely not provide conclusive findings, but that TACE could have a key role along with the delicate balance of sTNFα/tmTNFα as well as TNFR1/TNFR2, hence stressing the importance of more research into the potential of rationalized treatments that combine TNFα pathway modulators with immunotherapy for lung cancer patients.
Keywords: TNFα, TNFR1, TNFR2, lung cancer, immunotherapy, immune checkpoint inhibition (Min. 5–Max. 8)
1. The Pleiotropic Immunological Biology of TNFα
About 60 years ago, it was reported that bacterial endotoxin administration to mice resulted in the release of a serological protein with necrotic anti-tumor activity at high concentrations. Due to the latter characteristic, this protein was termed tumor necrosis factor (TNF) [1] and considered a breakthrough for cancer therapy. Today, the TNF superfamily consists of 19 members and 29 TNF receptors [2]. Within this family, functional TNFα is represented by a trimer of 17.35 kDa monomers, folded into a rigid bell-shaped “jelly roll” composed of antiparallel filaments [3]. It exists in two forms: a transmembrane form (tmTNFα) next to a soluble (sTNFα) form. The latter one is cleaved from tmTNFα by the metalloproteinase TNF-alpha-converting enzyme (TACE). Upon X-ray crystallography analysis, TNFα was demonstrated to bind to TNF receptors 1 and 2 (TNFR1 and TNFR2), represented by a 55 and 75 kDa type I and type II transmembrane protein, respectively [4,5]. The structural pleiotropism of TNFα and its receptors endows it with a multifaceted role linked to both anti- and pro-inflammatory assets as well as apoptotic assets. The complexity of these findings tempered the original enthusiasm for TNFα as a breakthrough molecule for cancer therapy.
1.1. The Pro-Inflammatory Character of sTNFα versus tmTNFα
Soluble TNFα is mainly secreted by activated macrophages [6] and to a lesser extent, by T lymphocytes, natural killer (NK) cells, neutrophils, endothelial and cardiac muscle cells, fibroblasts, and osteoclasts [7,8]. By comparison, tmTNFα is expressed constitutively on the surface of a broad range of immune cells such as alveolar and non-alveolar macrophages [9], monocytes [10], lymphocytes [11], dendritic cells (DCs), and NK cells [12]. In addition, its expression has been reported on non-immune cells such as adipocytes [13] and tumor cells [14].
In general, sTNFα is rapidly released upon trauma or infection, as it is bestowed with a determining role in immunoregulatory processes such as immune ontogeny, inflammation, and apoptosis [7]. As a soluble pro-inflammatory cytokine, it primarily acts at sites remote from the TNFα-producing cells to support the production of downstream pro-inflammatory cytokines along with the recruitment, activation, and regulation of inflammatory cells such as macrophages. To illustrate, when macrophages are activated by Toll-like receptors, they secrete sTNFα, which subsequently regulates macrophage differentiation in an autocrine fashion [15]. Hence, TNFα neutralizing antibodies have been shown to reduce the production of several pro-inflammatory cytokines and growth factors such as interleukin-1 (IL-1) and granulocyte-macrophage colony-stimulating factor (GM-CSF) [16]. Of note, sTNFα has an intrinsic pleiotropic activity as it is also involved in anti-inflammatory responses that aim to restore homeostasis [17].
In comparison, tmTNFα is an important mediator of immune-cell crosstalk. To illustrate, when DCs express tmTNFα, the latter can interact with TNFR2 on NK cells, resulting in increased NK cell proliferation and cytotoxic activity [18]. Moreover, tmTNFα can act in a dual manner upon its interaction with TNFR: either as a ligand or as a receptor through an “outside-to-inside” signaling pathway known as “reverse signaling”. There is evidence that, as a ligand, it is mainly involved in host defense mechanisms against infections [19], while the receptor-like form appears to have a role in modulating immune cell activation. To elaborate, tmTNFα expressed by activated T cells can bind to TNFR2, expressed by monocytes, leading to monocyte activation with subsequent secretion of interleukin-10 (IL-10) and sTNFα. Additionally, endogenous IL-10 was shown to downregulate T cell contact-mediated sTNFα production by monocytes, suggestive for an autoregulatory loop involving both sTNFα and tmTNFα [19,20,21]. What is more, T cells can also activate monocytes by expressing TNFR2 that can trigger reverse signaling via tmTNFα, expressed by the monocytes. Hence, both TNFα isoforms are significantly involved in the regulation of the inflammatory response [22].
1.2. Two Distinct Receptors Fine-Tune TNFα’s Biological Effects
TNFR1, also known as tumor necrosis factor receptor superfamily, member 1A (TNFRSF1A) or CD120a, is expressed on almost all host cells including various tumor cell types [23,24,25,26] and tumor-associated endothelial cells [27]. In contrast, TNFR2 (TNFRSF1B or CD120b) is predominantly located on the surface of immune cells, such as NK cells, macrophages [28], regulatory T cells (Tregs), suppressive myeloid cells [29], and endothelial cells [30]. As indicated by "+" in Figure 1, sTNFα shows a significantly higher affinity for TNFR1 than tmTNFα, while the opposite holds true for TNFR2 [31,32].
Figure 1.
Pathways activated by soluble TNFα (sTNFα) and transmembrane TNFα (tmTNFα) upon binding to TNFRs. Downstream signaling via TNFR1 is most effective upon high-affinity (+++) binding to sTNFα. In the case of TNFR1, this can lead to caspase8/3-mediated apoptosis through signaling via its death domain (DD), recruitment of TRADD, and subsequent recruitment of FADD or TRAF2. The latter could also result in activation of pro-inflammatory signals via the "classical NF-κB" pathway, and is primarily activated via TNFR1 (red arrows). Upon high-affinity (+++) binding of tmTNFα to TNFR2, TRAF2 is triggered, which preferentially results in NF-κB activation via the alternative pathway (blue arrows) to activate the expression of proliferation and survival related genes. Both sTNFα and tmTNFα bind with low-affinity (+) to TNFR2 and TNFR1 respectively. TNF-alpha-converting enzyme (TACE), responsible for the conversion of sTNFα from tmTNFα and of soluble TNFRs [56]. For completeness, the alternative TNFR ligand lymphotoxin alpha 3 (LTα3), with its affinity binding profile to TNFR1 and 2, is depicted as well. This figure was created with BioRender.com (accessed on 4 June 2021).
In terms of biological effects, high affinity binding to TNFR1 (and not TNFR2) has been demonstrated to result in DC activation and subsequent stimulation of antigen specific CD8+ T cells [33]. That TNFR1-knockout (ko) mice show resistance to colitis development [34] further confirms its involvement in the differentiation of inflammatory T cells. In comparison, activation of TNFR2 in lymphoid cells leads to inflammatory responses as well as T cell activation, thymocyte proliferation, GM-CSF production [7], and NK cell-mediated IFN-γ production [35]. Yet, its main role seems to be linked to restoration of homeostasis and promotion of an immunosuppressive environment, as TNFR2 gene ko models show elevated inflammatory responses [33,34,36]. To illustrate, TNFR2 signaling has been shown to promote Treg differentiation, proliferation, and suppressive function, while TNFR1 does not affect Treg cell expansion [37,38,39]. Moreover, upon activation of both TNFRs, TNFR2 is more liable to receptor shedding than TNFR1 [40,41,42]. The shedded soluble TNFRs have been shown to serve as decoy receptors for sTNFα to control its innate immune activation threshold. Hence, more pronounced TNFR2 shedding is in line with its immune restorative function [43,44].
Next to their roles in immune cell proliferation and activation, triggered TNFR1 and TNFR2 can also induce apoptotic and necrotic cell death. In the case of TNFR1, this is the result of the interaction between the receptors’ death domain (DD) and the adapter protein TNF receptor-associated death domain (TRADD). Upon interaction of DD-TRADD, the activation of cysteine-aspartyl-specific proteases (caspases) is stimulated [45,46]. Although TNFR2 lacks a DD, it has been reported to cause activation-induced cell death (AICD), e.g., in mature CD8+ T cells [36]. As outlined in Figure 1, the different outcomes upon TNFR1 and 2 triggering result from their distinct downstream signaling [47]. Although both exploit the NF-κB pathway for transcriptional activation of inflammatory and anti-apoptotic genes [48], the “classical” NF-κB pathway is mainly activated upon sTNFα binding to TNFR1 [31], while the “alternative pathway” is preferentially but not exclusively primed upon TNFR2 binding [28,49,50]. Additionally, both TNFRs can regulate gene expression by activating at least two members of the MAP kinase (MAPK) family, such as P38 [51,52] and JNK [53], and this via a series of protein phosphorylations (MEKK). Notably, the TNF superfamily member lymphotoxin alpha can, in its soluble homotrimer form (LTα3), also bind to both TNFRs with an affinity profile comparable to that of sTNFα [54,55]. In terms of biological effects, sTNFα and LTα3 have been reported to show equal mitogenic stimulation capacities upon TNFR binding, yet sTNFα was shown to be more potent to mediate gene regulation and cytotoxicity.
In conclusion, the presence of two functional isoforms (soluble and transmembrane) next to two receptors with specific expression, affinity, and downstream signaling avenues collectively serves the pleiotropic job description of TNFα. As regulator of cytotoxic, pro-, and anti-inflammatory functions, it is evident that TNFα can play a critical role in the development of chronic inflammatory diseases as well as cancer, as outlined below.
2. TNFα Plays Opposing Roles in Cancer
Despite TNFα’s denomination, in vitro reported tumor necrosis after high TNFα concentrations appeared a phenomenon that is not so straightforwardly translated to successful cancer treatments in vivo. The latter is partly explained by TNFα’s multifunctionality as a cytotoxic but also immune modulating cytokine. As the immune system plays a complex role on the tumor microenvironmental (TME) battlefield, TNFα is used as a weapon to modulate and/or kill tumor cells, immune cells, and/or endothelial cells [57].
Previously observed direct anti-tumoral properties of TNFα in vivo are among others based on its capacity to hinder tumor-associated blood vessel formation (angiogenesis) via selective endothelial cytotoxicity and necrotic hemorrhage [58]. This selective endothelial cytotoxicity can subsequently result in hyperpermeability of tumor vessels and increased blood cell extravasation. The exact underlying mechanism remains unknown, yet van Horssen et al. [59] described the noteworthy hypothesis that tumor-residing endothelial cells are more sensitive to TNFα because they upregulate TNFR1 upon cytokine signaling by tumor cells and macrophages. However, external administration of TNFα was shown to occupy TNFR1 expressed by tumor and healthy endothelial cells without toxicity towards the latter, due to the presence of a low number of receptors on healthy cells [60]. Nevertheless, studies in mice and rats further showed a synergistic anti-tumor effect of TNFα in combination with chemotherapeutic drugs, as accumulation of the latter at the tumor site was shown to be improved [61,62,63]. Moreover, persistent high-level stimulation with TNFα in vitro inhibits endothelial cell proliferation in a dose-dependent manner [64], further supporting its anti-angiogenic effects [65,66,67]. However, Fajardo et al. hypothesized that TNFα could show both pro- and anti-angiogenic effects in vivo, depending on its local concentration. When murine TNFα was administered subcutaneously in mice, this was shown to exert opposing effects. At low doses (range: 0.01–1 ng), TNFα induced angiogenesis whereas increasing doses (1 and 5 µg) reduced this effect with complete abolishment at the highest doses [68].
While a high concentration of TNFα has been linked to hemorrhagic necrosis, it is now widely accepted that chronic exposure to TNFα is more likely to promote tumor progression. First, it has been demonstrated repeatedly that chronic inflammation, in which the innate immune system plays a leading role, can promote cancer onset as well as progression and metastasis, typifying the “never-healing-wound” character of solid cancers [69,70]. Indeed, chronic exposure to TNFα can promote cellular transformation via the induction of direct mutations and DNA damage [71] as well as via profound epigenetic changes that modulate the expression level of oncogenes and tumor suppressor genes [72]. In addition, inflammation influences epithelial-to-mesenchymal cell transition (EMT) and subsequent cancer cell invasion. Further, TNFα has been shown to affect expression of EMT-inducing transcription factors, particularly in synergy with TGFβ [73]. Moreover, TNFα associated with chronic inflammation can be held responsible for the observed phenomenon of cancer cell specific resistance to TNFα-induced cell death [74]. Specifically, chronic TNFα/TNFR1 binding increases the expression of anti-apoptotic, angiogenic, and invasive proteins via the TAK-1, MAPKs, Akt, IKK, AP-1, and NF-κB signaling pathways [28,75,76]. Notably, also the ligands and receptors of the LTα family with, among others, affinity for TNFR1 and 2, have been linked to increased carcinogenesis, as extensively reviewed elsewhere [55,77].
Even if chronic inflammation is not involved in the onset of tumor cell transformation, the immune system often becomes a co-worker during cancer progression. Today it is generally accepted that the immune system can identify and control nascent malignancies in a process called cancer immunosurveillance. In contrast, the latter can also promote tumor progression through the selection of poorly immunogenic variants and suppression of anti-tumor immunity. Together, the dual host-protective and tumor-promoting actions of immunity are referred to as cancer immunoediting and comprise three distinct phases: the elimination, equilibrium, and escape phase [78,79,80].
The elimination phase is characterized by an imbalance towards more anti-tumor immunity, installed by adaptive as well as innate immune cells. Characteristic for a potent Th1-oriented tumor-associated antigen (TAA) specific adaptive immune response is the presence of immunogenic TAAs, presented via MHC-I on the surface of tumor cells, together with Fas, TRAIL, and IFN-γ receptors and the presence of perforin, granzymes, IFN-α/β/γ, IL-1, IL-12, and TNFα within the TME. Hence, TNFα can ameliorate this phase through its involvement in activation of T cells, macrophages, and NK cells. For example, it was shown that TNFR1 signaling promotes the accumulation of anti-tumor M1 polarized tumor-associated macrophages (TAMs) by suppressing the M2-polarizing release of IL-13 from eosinophils co-recruited with inflammatory monocytes [81]. On their turn, MHC-IIhigh (M1) TAMs and granulocytes can secrete, among others, TNFα, IL-1, and IL-12 to further ameliorate a Th1-polarized anti-tumor immune profile [82].
During the equilibrium phase, anti- and pro-tumor immunity are in balance and/or immune-mediated tumor dormancy is installed [80]. It was reported that the absence of TNFR or IFN-γ promoted angiogenesis and multistage carcinogenesis in an experimentally induced pancreatic murine tumor model, suggesting that a coordinated interaction between IFN-γ and TNFα was responsible for the activation of TAA-specific cytotoxic T cells [83]. Moreover, the combination of IFN-γ and TNFα drove pancreatic tumor cells into STAT-1 and TNFR1-mediated senescence [82]. Because IFN-γ and TNFα induce senescence in numerous murine and human cancers, this may be a general mechanism for arresting cancer progression.
In the escape phase, TNFα has several effects capable of lowering the antitumor immune response by facilitating the accumulation and/or activation of a wide range of immunosuppressive cells such as Tregs [37], regulatory B cells [84], and suppressive myeloid cells [85]. As stated before, the common factor of these immunosuppressive effects lies within TNFα binding to TNFR2. When secreted by activated CD4+ T-cells, TNFα has been shown to induce myelopoiesis in tumor-bearing mice. Furthermore, cells of the myeloid lineage can be recruited to become immune-suppressive regulatory myeloid cells, which decrease TAA-specific CD8+ T cell mediated tumor cytotoxicity [86]. Moreover, it has been reported that tmTNFα, rather than sTNFα, is able to activate immunosuppressive myeloid cells upon binding to TNFR2. To illustrate, a marked increase in immunosuppressive myeloid cell accumulation was only observed when tmTNFα was constitutively expressed on 4T1 mammary tumor cells, with subsequent promotion of NO, ROS, IL-10, and TGF-β secretion by these myeloid cells and inhibition of lymphocyte proliferation. In contrast, 4T1 overexpression of sTNFα resulted in increased lymphocyte infiltration and tumor regression [87]. TNFα also facilitates the installment of an effector T cell hostile milieu via indoleamine 2,3-dioxygenase 1 (IDO1) accumulation in the TME. To illustrate, while M2b polarized macrophage conditioned medium stimulates tumor cell proliferation and IDO1 expression in vitro, this is reduced upon TNFα neutralization [88]. As IDO1 converts tryptophan into kynurenine, tryptophan is deprived with subsequent installment of TAA-specific T cell anergy, while Treg activity, lymphangiogenesis, and neovascularization are enhanced in vivo. Finally, TNFα has been linked to cancer therapy resistance. To illustrate, in a murine triple-negative breast cancer model, resistance to the anti-angiogenic drug bevacizumab was shown to be accompanied by M2b TAM-mediated secretion of the chemokine CCL1 along with TNFα. Upon TNFα-neutralizing nanobody administration in vivo, this immunosuppressive M2b macrophage-induced resistance was overcome, supporting TNFα’s key role in resistance to bevacizumab [88].
Although both TNFα and its receptors’ precise role within the complex and ever-evolving TME are far from fully understood, substantial evidence has emerged that TNFα signaling has a paradoxical and dual role in cancer progression and the dynamic immunoediting process. While it has been held responsible for key tumor promoting features such as the maintenance of an antigen-ignorant chronic inflammatory state and immunosuppressive effects that hinder TAA-specific effector functions, its documented anti-tumor assets in vitro and in vivo hamper a clear-cut conclusion.
3. Specificities of TNFα in Lung Cancer Progression
Lung cancer remains the leading cause of cancer-related deaths worldwide, responsible for almost 1.8 million deaths in 2020 alone [89]. Lung cancer comprises two key types: non-small cell lung cancer (NSCLC), accounting for 80–85% of cases, and small cell lung cancer (SCLC) [90].
As the human respiratory tract is continuously exposed to air that can potentially contain airborne pathogens, lungs necessitate a unique, fine-tuned, and rapidly acting pulmonary immune system to maintain homeostasis [91]. When the immunohistological expression of TNFα and its receptors was evaluated in healthy human lung tissue, TNFα was shown to be particularly prominent in bronchial epithelial cells, vascular smooth muscle cells, and alveolar macrophages. In addition, TNFR1 was shown to be eminently expressed on bronchial epithelial cells and endothelial cells, while TNFR2 was expressed by nearly all cell types [92]. Therefore, it is not surprising that in the complex process of lung cancer onset, progression, and dissemination, TNFα and its receptors have been reported to play decisive roles, too. Indeed, it was recently described that TNF is one of the co-occurring frequently altered immune genes found within the TCGA pan-cancer lung adenocarcinoma (LUAD) dataset (n = 507) [93]. However, the exact effect seems to be nuanced by contradicting functions governed by their isoforms, signal strength, and downstream signaling pathways. This is illustrated by the finding that specific genetic polymorphisms of the TNF gene region impact lung cancer progression differently. While the 238 G>A polymorphism, found in the promoter region of TNFα, has a favorable prognostic association for NSCLC [94], the 308 G>A polymorphism constitutes an increased risk for lung cancer [95].
Another opposing effect is found for sTNFα and tmTNFα on lung cancer growth [96]. When murine lung tumor lines expressed tmTNFα, their engraftment resulted in the formation of small tumors with reduced tumor-associated myeloid cell infiltration, in contrast to control or sTNFα-overexpressing lines. The observed myeloid cell reduction was found to be a direct effect of tmTNFα on myeloid survival via induction of ROS-mediated cell necrosis. Furthermore, human NSCLC was shown to express varying levels of sTNFα and tmTNFα, and gene expression patterns favoring tmTNFα appeared predictive of improved lung cancer survival [96]. This is in contrast with previous findings using the mammary 4T1 model and, moreover, counterintuitive, as tmTNFα shows a higher affinity than sTNFα for the immunosuppression promoting TNFR2 [87]. The fact that TNFα could have a favorable impact on survival is further supported by a study on citronellol’s ability to induce necroptosis of human lung tumor cells in vitro and in vivo. This study identified a decisive role for TNFα in this necroptosis induction via its activation of RIP1/3 and simultaneous downregulation of caspase 3/8 activity [97].
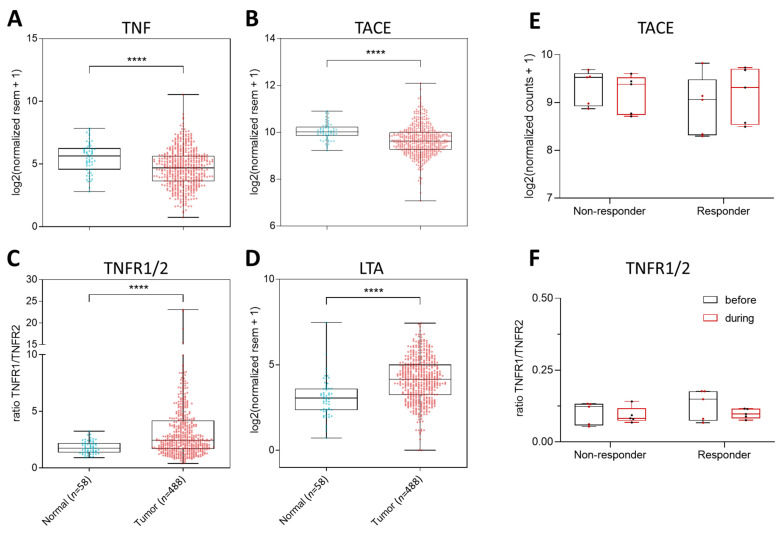
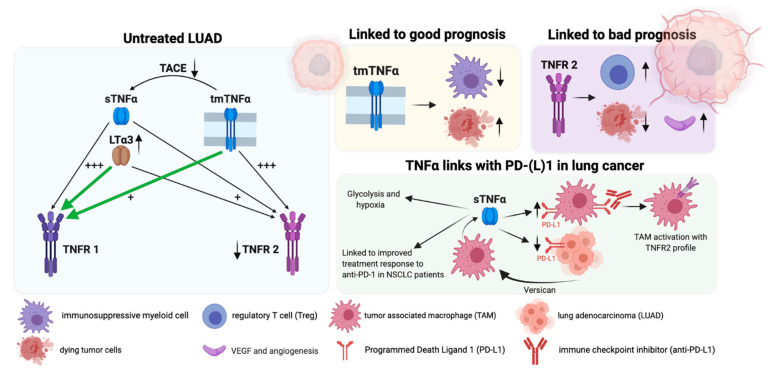
In an attempt to predict the most common interactions between the different TNFα-signaling members within the lung TME, we compared the overall TNF, TACE, TNFR1, and TNFR2 expression profiles within a healthy tissue and TCGA pan-cancer LUAD transcriptomic data set. We found a significant reduction of TNF, TACE, and TNFR2 transcripts within the LUAD cohort (Figure 2A,B), leading to an increased TNFR1/TNFR2 ratio (Figure 2C). These findings imply that LUAD tumors are characterized by reduced numbers of TNFα and especially of sTNFα molecules as TACE is significantly reduced. The specific reduction of TNFR2 and not TNFR1 in LUAD tumors further implies that TNFR1 but not TNFR2 plays a crucial role in tumor progression. As TNFR1 also shows high affinity for LTα3, we used the same LUAD cohort to evaluate the expression profile of the lymphotoxin alpha monomer encoding gene LTA. We found a significant upregulation of LTA in the LUAD cohort compared to healthy controls (Figure 2D). Previous studies linked the expression of at least two LTA-signaling members to a poor clinical outcome in lung cancer patients: the receptor for the heterotrimeric LTαβ (LTβR) and the alternative LTα3 receptor herpes virus entry mediator (HVEM) [98,99]. Overall, these findings suggest that the TNFα pathway will have the highest likelihood to signal within the LUAD TME via TNFR1 through low-affinity binding to tmTNFα or high-affinity binding to LTα3, as graphically visualized with green arrows in Figure 3.
Figure 2.
Gene expression analysis of several TNF family members within lung cancer patients. (A–D) Expression profiles were collected from TCGA for both normal (n = 58) and LUAD tumor tissue (n = 488). Next, we obtained the Log2-transformed normalized RSEM values via Wanderer for TNF (A), TACE (B), TNFR1 and 2 (C), and LTA (D) [100]. For (C), the ratio of the expression values of TNFR1 over TNFR2 is depicted. Statistical analysis was performed using the Mann–Whitney test (****, p < 0.0001). (E,F) Gene expression analysis of TACE, TNFR1, and TNFR2 in CD8+ T cells from NSCLC patients before and during anti-PD-1 mAb treatment. RNAseq dataset obtained from the Gene Expression Omnibus (GEO) database (accession number: GSE111414, accessed on 06/07/2021). Counts were normalized using DESeq2 in R. Counts for TNF were zero for most samples (data not shown). (A) Gene expression profile of TACE in both non-responder and responder groups. (B) Ratio of TNFR1 and TNFR2 normalized expression values. For each group: n = 5.
Figure 3.
Overview of TNFα signaling within LUAD with link to prognosis and checkpoint inhibition. (+++) high-affinity binding, (+) low-affinity binding, green arrows support likeliness of TNFα-signaling pathways in LUAD patients. This figure was created with BioRender.com (accessed on 5 August 2021).
Nevertheless, studies on the lung tumor growth promoting role of TNFα signaling are ample, too. First, several clinical studies have reported on the decisive role of TNFα in lung cancer EMT, invasion, and metastasis [101,102]. Secondly, TNFα has been shown to play an essential role in creating an immunosuppressive lung TME [103], among others, by upregulating MHC-II in alveolar type-II (AT-II) cells responsible for a plethora of functions that support the maintenance and optimal functioning of alveoli. Because AT-II cells’ primary function is not antigen presentation, they lack co-stimulatory signals (CD80/CD86), essential to effectively prime CD4+ T cells. Thus, instead of creating an antitumor immune response, increased AT-II cell-specific MHC-II expression can trigger Treg differentiation [104]. Numerous studies evaluated TNFR2 as a potential biomarker for NSCLC as it has been shown to be crucial for TNFα-mediated immunosuppression [105,106]. High amounts of TNFR2+ Tregs have been found in the TME of murine [39,107] as well as human advanced lung cancers [108,109], suggesting that Tregs are activated through TNFα/TNFR2 signaling. In addition, TNFR2 expression by lung tumor cells and the lung TME has been shown to support tumor cell survival [110], pre- metastatic niche formation [111], and neovascularization via vascular endothelial growth factor (VEGF) release. These findings are further supported by the observation that the levels of TNFR2 expression in human lung cancer patients, which are up to 35% [106], correlate positively to a more advanced clinical stage, immune invasion, progressive metastasis, shorter survival time, and poor prognosis [106,108]. These findings were confirmed in TNFR2-ko mice engrafted with the Lewis lung carcinoma (LLC) model. Compared to wild type and TNFR1/2 double ko mice, tumor growth decreased twofold in TNFR2-ko mice specifically and correlated with reduced VEGF expression and capillary density, along with increased numbers of apoptotic LLC cells. As they further showed that blocking TNFR2 via a short-hairpin RNA in cultured LLCs increased TNFα-mediated apoptosis and expression of several angiogenic factors, they confirmed that TNFR2 directly ameliorates angiogenesis and LLC survival [110]. Moreover, Chopra et al. reported that TNFα or TNFR2 deficiency on immune cells resulted in the reduction of lung metastasis and a decrease in the number of pulmonary Tregs [39].
In conclusion, preclinical evidence suggests that TNFR2 is involved in lung tumor progression while tmTNFα (with high affinity for TNFR2) has been linked to a better prognosis for lung cancer patients. This implies that the biomarker potential of tmTNFα and TNFR2 for lung cancer progression most likely pivots on the delicate balances of sTNFα over tmTNFα as well as TNFR1 over TNFR2.
4. Linking TNFα to Antitumor Immunotherapy in Lung Cancer
The goal of antitumor immunotherapy is to completely and specifically eradicate both primary and metastatic tumor lesions by mobilized cytotoxic effector cells. Hence, immunotherapy can achieve actual cures of advanced lung cancer patients, representing an unprecedented reality [112,113]. Therefore, the first FDA approval of an immunotherapeutic treatment for squamous cell NSCLC benchmarked a revolutionary era for lung cancer patients. This treatment is based on blocking the immune checkpoint programmed death-1 (PD-1) pathway. Under healthy conditions this pathway is used to put an adequate brake on T cell stimulation and return to homeostatic conditions. As tumor cells can express the PD-1 ligand (PD-L1) themselves, they can corrupt this pathway to hinder their execution by PD-1+ TAA-specific cytotoxic effector cells [114,115]. Since 2016, five PD-(L)1 inhibitors (nivolumab, pembrolizumab, atezolizumab, durvalumab, and cemiplimab) have been approved by the FDA as second- and/or first-line treatment options for advanced NSCLC [93]. Notably, for the treatment of SCLC, both nivolumab and pembrolizumab were originally approved [116] yet have been withdrawn from the US market since confirmatory trials failed to evidence improved survival outcomes. Additionally, only ~20% of unselected NSCLC patients benefit from blocking immune checkpoints, and many of the initial responders eventually develop resistance to therapy. Moreover, the growing trend to combine several immune checkpoint inhibitors (ICIs) coincides with a growing occurrence of severe to fatal immune-related adverse effects (irAEs), often related to a local increase in TNFα [117]. Together with the emerging concept of hyperprogression upon ICI [118], these phenomena cast light on the current knowledge gap of immunotherapy hampering mechanisms.
In search for clues, the relationship between TNFα and immune checkpoint signaling in the TME is being explored, hinting towards a lead role for TAMs. While IFN-γ is the main regulator of PD-L1 expression in tumor cells, PD-L1 expression in TAMs seems to be regulated via TNFα [119]. In 2017, Hartley et al. demonstrated that TNFα increases the expression of PD-L1 on bone marrow-derived monocytes and macrophages. They found that this was maintained through the secretion of versican by tumor cells, which stimulated the production of TNFα by monocytes themselves in a TLR2-dependent manner [120]. One year later, the same group provided more evidence on the interactions between the TNFα and PD-L1 pathways, as they demonstrated that PD-L1 blockade increased spontaneous macrophage proliferation, survival, and activation in vitro. Via RNAseq and IPA software analysis of these anti-PD-L1 treated macrophages, they further revealed an activated TNFR2 signaling profile [119]. Furthermore, it was recently shown in NSCLC patients that TNFα-secreting TAMs can enhance hypoxia and aerobic glycolysis and that TAMs dampen PD-L1 expression on murine lung tumor cells specifically [121,122]. The latter does contradict the observation that TAM-secreted TNFα could stabilize PD-L1 expression on 4T1 mammary cancer cells, triggering immunosuppression in vivo [123].
As melanoma remains the textbook example for immunotherapy responsiveness, TNFα targeting studies are most numerous for this cancer type. Overall, preclinical TNFα blockade has been shown to reduce the induction of irAEs upon ICI combinations and even improve therapeutic effectiveness of ICIs [117,124]. Upon adoptive CD8+ T cell transfer, TNFα appeared to be a crucial factor in the incitement of melanoma dedifferentiation, which resulted in immune escape and melanoma relapse [125]. Bertrand et al. partly explained these effects by the observation that TNFα/TNFR1 signaling triggers AICD of tumor-infiltrating CD8+ T cells in melanoma, with subsequent lack of response to anti-PD-1 therapy [126]. Hence, via systemic administration of etanercept, melanoma growth was inhibited in immunocompetent animals specifically. Notably, similar effects were seen in TNFR1-ko, but not TNFR2-ko, mice, suggestive for the decisive role of TNFR1 in this AICD of CD8+ T cells [127]. A few years later, Bertrand et al. further validated these findings by showing that anti-PD-1 therapy can stimulate T-cell expression of the alternative checkpoint T-cell immunoglobulin and mucin domain 3 (TIM-3) via TNFα. Moreover, they could demonstrate that co-blockade of PD-1 and TNFα overcomes resistance to anti-PD-1 monotherapy [124]. Hence, we eagerly await the results from the first Phase Ib, open-label trial [128] that is evaluating the administration of nivolumab (anti-PD-1) and ipilimumab (anti-CTLA-4) in combination with the anti-TNFα drug infliximab or certolizumab in patients with advanced melanoma.
In contrast to melanoma, only a handful of preclinical studies have explored the potential of TNFα pathway modulating strategies to treat lung cancer with rather contradictory findings. For example, anti-TNFα antibody treatment has been tested together with an intrapulmonary IFN-beta immuno-gene therapy (Ad.IFNβ) in an orthotopic mouse model of lung cancer. The rationale for this was that blocking the pro-inflammatory actions of TNFα could reduce the induction of dose-limiting pulmonary inflammation upon Ad.IFNβ delivery. However, upon administration, the anti-TNFα antibody not only significantly reduced the pulmonary inflammation but also the therapeutic effect of Ad.IFNβ delivery. Hence, TNFα proved to be both a dose-limiting factor as well as crucial for the anti-tumor immune stimulatory capacity of Ad.IFNβ [129]. More straightforward was the negative role described for TNFα secretion by TAMs, as this promoted cell glycolysis, tumor hypoxia, and decreased PD-L1 expression. Hence, when the TNFα-secreting TAMs were depleted upon clodronate treatment of LLC-engrafted mice, PD-L1 expression significantly increased in the aerobic cancer cells. Moreover, this treatment increased tumor T cell infiltration and most importantly, its response to anti-PD-L1 therapy, which was otherwise completely ineffective [121]. While the above study suggests that TNFα blockade can increase effectivity of anti-PD-L1 therapy, this seems diametrically opposed to the observation that not reduced but increased serological levels of TNFα were found to be associated with improved anti-PD-1 treatment response and survival in NSCLC (along with IFN-γ, IL-1, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, and IL-12) [130]. Using an online available RNAseq dataset on CD8+ T cells sorted out of NSCLC patients’ peripheral blood mononuclear cells before and during anti-PD-1 mAb therapy [131], we were able to support the notion that increased levels of sTNFα could be linked to improved anti-PD-1 treatment response, as we found a non-significant increase in TACE expression within the responder group specifically, linked to more release of sTNFα from its tmTNFα form (Figure 2E). While the TNFR1/TNFR2 ratio decreased upon anti-PD-1 treatment, this phenomenon was seen in both the responder and non-responder groups (Figure 2F). Finally, the levels of LTA were very similar between the responder and non-responder groups (data not shown), although we were unable to draw any conclusions for TNF due to the lack of representative data, underscoring the current lack of human data on gene expression profiles of the different TNFα family members before, during, and after antitumor immunotherapy.
5. Conclusions and Future Perspectives on TNFα Modulation for Lung Cancer Treatment
The multitude of contradictory findings currently poses a stalemate for TNFα pathway-affecting strategies in combination with immunotherapy to treat lung cancer and suggests the need for additional research into biomarkers to guide rationalized therapy combinations. This conundrum is reflected by the range of preclinical studies that report on the therapeutic efficacy of TNFα upon its administration as well as its inhibition [132]. To illustrate, when a TNF-based Activity-on-Target cytokine (AcTakine) was specifically targeted to the CD13+ neovasculature in vivo, the rapid destruction of the tumor neovasculature and complete regression of large, established tumors was demonstrated. In contrast, selective blockage of sTNFα via INB03 led to a reduced carcinogen-induced tumor incidence and growth rate [133]. Moreover, a detrimental role has been attributed to sTNFα and TNFR1 for melanoma-infiltrated functional CD8+ T cells as well as the onset of irAEs, rationalizing combined TNFα-blockade with immunotherapy to treat melanoma.
By mining existing next-generation sequencing data from LUAD patients, the latter were shown to contain less TNF, and because of the significant reduction in TACE, sTNFα protein is likely to be most decreased. Together with the notion that tmTNFα, and not sTNFα, has been shown to play a key role in Th1-polarized antitumor immunity and improved lung cancer patient survival [18,134], this argues against a tumor promoting role for TNFα in lung cancer, discouraging TNFα-blockage for lung cancer treatment today. Additionally, the role of TNFR2 in lung cancer progression remains undetermined and requires more research. High amounts of TNFR2+ Tregs have been found in the TME of human advanced lung cancers, and TNFR2 has recently been identified as a tumor-promoting oncogene with new biomarker potential for cancer [135,136]. However, upon mining the currently available transcriptomic dataset from a TCGA LUAD patient cohort, we demonstrated that the expression of TNFR2 is markedly decreased in the lung TME. Moreover, pre-clinically, TNFR2 agonists as well as antagonists have been linked to antitumoral effects, arguing against the effectiveness of TNFR2 modulation for lung cancer therapy [137,138,139,140].
To conclude, numerous studies point out that TNFα signaling is extensively involved in lung tumor progression and response to (immuno-)therapy. However, the underlying mechanisms of the different TNFα family members that modulate tumor prognosis and response to treatment remain to be revealed. We summarized our main findings in Figure 3 to highlight that TNFα signaling involves different ligands and receptors in LUAD, which have been linked to prognosis response to PD-(L)1 treatment. To make matters more complicated, all of these components can be expressed, secreted, and sensed by a broad range of malignant, immune, and non-immune cells within the respiratory tract, whereas most (pre-)clinical data have been based on serological values of sTNFα and RNA sequencing data. Therefore, we believe that larger genomic, transcriptomic, and proteomic dataset analysis studies are needed for various disease stages and treatment options on the single cell lung TME level to advance our current understanding of the biomarker and modulatory potential of the TNFα pathway for lung cancer prognosis and therapy.
Funding
K.D.R. and C. Goyvaerts were supported by Kom op tegen Kanker, Fonds Wetenschappelijk Onderzoek (FWO) Vlaanderen, Wetenschappelijk Fonds Willy Gepts, and the BCLAS Fund in honor of Jean René Maisin.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Carswell E.A., Old L.J., Kassel R.L., Green S., Fiore N., Williamson B. An endotoxin-induced serum factor that causes necrosis of tumors. Proc. Natl. Acad. Sci. USA. 1975;72:3666. doi: 10.1073/pnas.72.9.3666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aggarwal B.B., Gupta S.C., Kim J.H. Historical perspectives on tumor necrosis factor and its superfamily: 25 years later, a golden journey. Blood. 2012;119:651. doi: 10.1182/blood-2011-04-325225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baeyens K.J., de Bondt H.L., Raeymaekers A., Fiers W., de Ranter C.J. IUCr the structure of mouse tumour-necrosis factor at 1.4 å resolution: Towards modulation of its -selectivity and trimerization. Acta Crystallogr. 1999;55:772–778. doi: 10.1107/S0907444998018435. [DOI] [PubMed] [Google Scholar]
- 4.Schall T.J., Lewis M., Koller K.J., Lee A., Rice G.C., Wong G.H.W., Gatanaga T., Granger G.A., Lentz R., Raab H., et al. Molecular cloning and expression of a receptor for human tumor necrosis factor. Cell. 1990;61:361–370. doi: 10.1016/0092-8674(90)90816-W. [DOI] [PubMed] [Google Scholar]
- 5.Loetscher H., Pan Y.-C.E., Lahm H.-W., Gentz R., Brockhaus M., Tabuchi H., Lesslauer W. Molecular cloning and expression of the human 55 kd tumor necrosis factor receptor. Cell. 1990;61:351–359. doi: 10.1016/0092-8674(90)90815-V. [DOI] [PubMed] [Google Scholar]
- 6.Parameswaran N., Patial S. Tumor necrosis factor-alpha signaling in macrophages. Crit. Rev. Eukaryot. Gene Expr. 2010;20:87–103. doi: 10.1615/CritRevEukarGeneExpr.v20.i2.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bradley J. TNF-mediated inflammatory disease. J. Pathol. 2008;214:149–160. doi: 10.1002/path.2287. [DOI] [PubMed] [Google Scholar]
- 8.Mehta A.K., Gracias D.T., Croft M. TNF activity and t cells. Cytokine. 2018;101:14. doi: 10.1016/j.cyto.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Armstrong L., Thickett D.R., Christie S.J., Kendall H., Millar A.B. Increased expression of functionally active membrane-associated tumor necrosis factor in acute respiratory distress syndrome. Am. J. Respir. Cell Mol. Biol. 2012;22:68–74. doi: 10.1165/ajrcmb.22.1.3728. [DOI] [PubMed] [Google Scholar]
- 10.Williams M.A., Newland A.C., Kelsey S.M. Cytokine modulated cell-membrane bound tumour necrosis factor expression is associated with enhanced monocyte-mediated killing of human leukaemic targets. Leuk. Res. 2000;24:317–330. doi: 10.1016/S0145-2126(99)00189-7. [DOI] [PubMed] [Google Scholar]
- 11.Horiuchi T., Morita C., Tsukamoto H., Mitoma H., Sawabe T., Harashima S.-I., Kashiwagi Y., Okamura S. Increased expression of membrane tnf-α on activated peripheral cd8+ t cells in systemic lupus erythematosus. Int. J. Mol. Med. 2006;17:875–879. doi: 10.3892/ijmm.17.5.875. [DOI] [PubMed] [Google Scholar]
- 12.Caron G., Delneste Y., Aubry J.-P., Magistrelli G., Herbault N., Blaecke A., Meager A., Bonnefoy J.-Y., Jeannin P. Human NK cells constitutively express membrane tnf-α (mtnfα) and present mtnfα-dependent cytotoxic activity. Eur. J. Immunol. 1999;29:3588–3595. doi: 10.1002/(SICI)1521-4141(199911)29:11<3588::AID-IMMU3588>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 13.Xu H., Sethi J.K., Hotamisligil G.S. Transmembrane tumor necrosis factor (TNF)-α inhibits adipocyte differentiation by selectively activating tnf receptor 1. J. Biol. Chem. 1999;274:26287–26295. doi: 10.1074/jbc.274.37.26287. [DOI] [PubMed] [Google Scholar]
- 14.Qu Y., Zhao G., Li H. Forward and reverse signaling mediated by transmembrane tumor necrosis factor-alpha and tnf receptor 2: Potential roles in an immunosuppressive tumor microenvironment. Front. Immunol. 2017;8:1675. doi: 10.3389/fimmu.2017.01675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Caldwell A.B., Cheng Z., Vargas J.D., Birnbaum H.A., Hoffmann A. Network Dynamics determine the autocrine and paracrine signaling functions of TNF. Genes Dev. 2014;28:2120–2133. doi: 10.1101/gad.244749.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.FionulaM B., Jackson A., Chantry D., Maini R., Feldmann M. Inhibitory effect of tnf alpha antibodies on synovial cell interleukin-1 production in rheumatoid arthritis. Lancet. 1989;334:244–247. doi: 10.1016/S0140-6736(89)90430-3. [DOI] [PubMed] [Google Scholar]
- 17.Marino M.W., Dunn A., Grail D., Inglese M., Noguchi Y., Richards E., Jungbluth A., Wada H., Moore M., Williamson B., et al. Characterization of tumor necrosis factor-deficient mice. Proc. Natl. Acad. Sci. USA. 1997;94:8093–8098. doi: 10.1073/pnas.94.15.8093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu J., Chakrabarti A.K., Tan J.L., Ge L., Gambotto A., Vujanovic N.L. Essential role of the TNF-TNFR2 cognate interaction in mouse dendritic cell–natural killer cell crosstalk. Blood. 2007;109:3333–3341. doi: 10.1182/blood-2006-06-026385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Horiuchi T., Mitoma H., Harashima S., Tsukamoto H., Shimoda T. Transmembrane TNF-α: Structure, function and interaction with anti-tnf agents. Rheumatology. 2010;49:1215–1228. doi: 10.1093/rheumatology/keq031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parry S.L., Sebbag M., Feldmann M., Brennan F.M. Contact with T cells modulates monocyte il-10 production: Role of T cell membrane TNF-Alpha. J. Immunol. 1997;158:3673–3681. [PubMed] [Google Scholar]
- 21.Rossol M., Meusch U., Pierer M., Kaltenhäuser S., Häntzschel H., Hauschildt S., Wagner U. Interaction between transmembrane tnf and tnfr1/2 mediates the activation of monocytes by contact with T cells. J. Immunol. 2007;179:4239–4248. doi: 10.4049/jimmunol.179.6.4239. [DOI] [PubMed] [Google Scholar]
- 22.Eissner G., Kolch W., Scheurich P. Ligands working as receptors: Reverse signaling by members of the TNF superfamily enhance the plasticity of the immune system. Cytokine Growth Factor Rev. 2004;15:353–366. doi: 10.1016/j.cytogfr.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 23.Deng J., Zhao X., Rong L., Li X., Liu X., Qin Z. TNFR-1 on tumor cells contributes to the sensitivity of fibrosarcoma to chemotherapy. Protein Cell. 2013;4:393. doi: 10.1007/s13238-013-3008-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhao Y., Yang F., Li W., Xu C., Li L., Chen L., Liu Y., Sun P. MiR-29a suppresses MCF-7 cell growth by downregulating tumor necrosis factor receptor 1. Tumor Biol. 2017;39:1010428317692264. doi: 10.1177/1010428317692264. [DOI] [PubMed] [Google Scholar]
- 25.Yang Z., Wang Y., Zhang L., Zhao C., Wang D. Phosphorylated form of pyruvate dehydrogenase α1 mediates tumor necrosis factor α induced glioma cell migration. Oncol. Lett. 2021;21:176. doi: 10.3892/ol.2021.12437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hwang H.S., Park Y.-Y., Shin S.-J., Go H., Park J.-M., Yoon S.Y., Lee J.-L., Cho Y.M. Involvement of the TNF-α pathway in TKI resistance and suggestion of TNFR1 as a predictive biomarker for TKI responsiveness in clear cell renal cell carcinoma. J. Korean Med. Sci. 2020;35:e31. doi: 10.3346/jkms.2020.35.e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang P., Rani M.R.S., Ahluwalia M.S., Bae E., Prayson R.A., Weil R.J., Nowacki A.S., Hedayat H., Sloan A.E., Lathia J.D., et al. Endothelial expression of TNF receptor-1 generates a proapoptotic signal inhibited by integrin A6β1 in glioblastoma. Cancer Res. 2012;72:1428–1437. doi: 10.1158/0008-5472.CAN-11-2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wajant H., Siegmund D. TNFR1 and TNFR2 in the control of the life and death balance of macrophages. Front. Cell Dev. Biol. 2019;91 doi: 10.3389/fcell.2019.00091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Polz J., Remke A., Weber S., Schmidt D., Weber-Steffens D., Pietryga-Krieger A., Müller N., Ritter U., Mostböck S., Männel D.N. Myeloid suppressor cells require membrane TNFR2 expression for suppressive activity. Immun. Inflamm. Dis. 2014;2:121–130. doi: 10.1002/iid3.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Faustman D., Davis M. TNF receptor 2 pathway: Drug target for autoimmune diseases. Nat. Rev. Drug Discov. 2010;9:482–493. doi: 10.1038/nrd3030. [DOI] [PubMed] [Google Scholar]
- 31.Grell M., Wajant H., Zimmermann G., Scheurich P. The type 1 receptor (CD120a) is the high-affinity receptor for soluble tumor necrosis factor. Proc. Natl. Acad. Sci. USA. 1998;95:570–575. doi: 10.1073/pnas.95.2.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grell M., Douni E., Wajant H., Löhden M., Clauss M., Maxeiner B., Scheurich P. The transmembrane form of tumor necrosis factor is the prime activating ligand of the 80 KDa tumor necrosis factor receptor. Cell. 1995;83:793–802. doi: 10.1016/0092-8674(95)90192-2. [DOI] [PubMed] [Google Scholar]
- 33.Ding X., Yang W., Shi X., Du P., Su L., Qin Z., Chen J., Deng H. TNF receptor 1 mediates dendritic cell maturation and CD8 T cell response through two distinct mechanisms. J. Immunol. 2011;187:1184–1191. doi: 10.4049/jimmunol.1002902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang S., Xie C., Chen Y., Wang J., Chen X., Lu Z., June R.R., Zheng S.G. Differential roles of TNFα-TNFR1 and TNFα-TNFR2 in the differentiation and function of CD4 + Foxp3 + induced treg cells in vitro and in vivo periphery in auto. Cell Death Dis. 2019;10:27. doi: 10.1038/s41419-018-1266-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Almishri W., Santodomingo-Garzon T., Le T., Stack D., Mody C.H., Swain M.G. TNFα Augments cytokine-induced NK cell IFNγ production through TNFR2. J. Innate Immun. 2016;8:617–629. doi: 10.1159/000448077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zheng L., Fisher G., Miller R.E., Peschon J., Lynch D.H., Lenardo M.J. Induction of apoptosis in mature T cells by tumour necrosis factor. Nature. 1995;377:348–351. doi: 10.1038/377348a0. [DOI] [PubMed] [Google Scholar]
- 37.Chen X., Bäumel M., Männel D.N., Howard O.M.Z., Oppenheim J.J. Interaction of TNF with TNF receptor type 2 promotes expansion and function of mouse CD4+CD25+ T regulatory cells. J. Immunol. 2007;179:154–161. doi: 10.4049/jimmunol.179.1.154. [DOI] [PubMed] [Google Scholar]
- 38.Zhong H., Bussel J., Yazdanbakhsh K. In Vitro TNF blockade enhances Ex vivo expansion of regulatory T cells in patients with immune thrombocytopenia. Br. J. Haematol. 2015;168:274–283. doi: 10.1111/bjh.13126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chopra M., Lang I., Salzmann S., Pachel C., Kraus S., Bäuerlein C.A., Brede C., Garrote A.-L.J., Mattenheimer K., Ritz M., et al. Tumor necrosis factor induces tumor promoting and anti-tumoral effects on pancreatic cancer via TNFR1. PLoS ONE. 2013;8:75737. doi: 10.1371/journal.pone.0075737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Philippe C., Roux-Lombard P., Fouqueray B., Perez J., Dayer J.M., Baud L. Membrane expression and shedding of tumour necrosis factor receptors during activation of human blood monocytes: Regulation by desferrioxamine. Immunology. 1993;80:300. [PMC free article] [PubMed] [Google Scholar]
- 41.Rochemonteix B.G., Nicod L.P., Dayer J.M. Tumor necrosis factor soluble receptor 75: The Principal receptor form released by human alveolar macrophages and monocytes in the presence of interferon gamma. Am. J. Respir. Cell Mol. Biol. 2012;14:279–287. doi: 10.1165/ajrcmb.14.3.8845179. [DOI] [PubMed] [Google Scholar]
- 42.Lainez B., Fernandez-Real J.M., Romero X., Esplugues E., Cañete J.D., Ricart W., Engel P. Identification and characterization of a novel spliced variant that encodes human soluble tumor necrosis factor receptor 2. Int. Immunol. 2004;16:169–177. doi: 10.1093/intimm/dxh014. [DOI] [PubMed] [Google Scholar]
- 43.Mierlo G.J.D.v., Scherer H.U., Hameetman M., Morgan M.E., Flierman R., Huizinga T.W.J., Toes R.E.M. Cutting edge: TNFR-shedding by CD4+CD25+ regulatory T cells inhibits the induction of inflammatory mediators. J. Immunol. 2008;180:2747–2751. doi: 10.4049/jimmunol.180.5.2747. [DOI] [PubMed] [Google Scholar]
- 44.Xanthoulea S., Pasparakis M., Kousteni S., Brakebusch C., Wallach D., Bauer J., Lassmann H., Kollias G. Tumor necrosis factor (TNF) receptor shedding controls thresholds of innate immune activation that balance opposing TNF functions in infectious and inflammatory diseases. J. Exp. Med. 2004;200:367–376. doi: 10.1084/jem.20040435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Naudé P.J.W., Boer J.A.d., Luiten P.G.M., Eisel U.L.M. Tumor necrosis factor receptor cross-talk. FEBS J. 2011;278:888–898. doi: 10.1111/j.1742-4658.2011.08017.x. [DOI] [PubMed] [Google Scholar]
- 46.Varfolomeev E., Vucic D. Intracellular regulation of TNF activity in health and disease. Cytokine. 2018;101:26–32. doi: 10.1016/j.cyto.2016.08.035. [DOI] [PubMed] [Google Scholar]
- 47.Vandenabeele P., Declercq W., Beyaert R., Fiers W. Two tumour necrosis factor receptors: Structure and function. Trends Cell Biol. 1995;5:392–399. doi: 10.1016/S0962-8924(00)89088-1. [DOI] [PubMed] [Google Scholar]
- 48.Hayden M.S., Ghosh S. Regulation of NF-ΚB by TNF family cytokines. Semin. Immunol. 2014;26:253. doi: 10.1016/j.smim.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yang S., Wang J., Brand D.D., Zheng S.G. Role of TNF–TNF receptor 2 signal in regulatory T cells and its therapeutic implications. Front. Immunol. 2018;9:784. doi: 10.3389/fimmu.2018.00784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rauert H., Wicovsky A., Müller N., Siegmund D., Spindler V., Waschke J., Kneitz C., Wajant H. membrane tumor necrosis factor (TNF) induces P100 processing via TNF receptor-2 (TNFR2) J. Biol. Chem. 2010;285:7394–7404. doi: 10.1074/jbc.M109.037341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang W., Liu H.T. MAPK Signal pathways in the regulation of cell proliferation in mammalian cells. Cell Res. 2002;12:9–18. doi: 10.1038/sj.cr.7290105. [DOI] [PubMed] [Google Scholar]
- 52.Ichijo H. From receptors to stress-activated MAP kinases. Oncogene. 1999;18:6087–6093. doi: 10.1038/sj.onc.1203129. [DOI] [PubMed] [Google Scholar]
- 53.Natoli G., Costanzo A., Ianni A., Templeton D.J., Woodgett J.R., Balsano C., Levrero M. Activation of SAPK/JNK by TNF receptor 1 through a noncytotoxic TRAF2-dependent pathway. Science. 1997;275:200–203. doi: 10.1126/science.275.5297.200. [DOI] [PubMed] [Google Scholar]
- 54.Medvedev A.E., Espevik T., Ranges G., Sundan A. Distinct roles of the two tumor necrosis factor (TNF) receptors in modulating TNF and lymphotoxin α effects. J. Biol. Chem. 1996;271:9778–9784. doi: 10.1074/jbc.271.16.9778. [DOI] [PubMed] [Google Scholar]
- 55.Gubernatorova E.O., Polinova A.I., Petropavlovskiy M.M., Namakanova O.A., Medvedovskaya A.D., Zvartsev R.V., Telegin G.B., Drutskaya M.S., Nedospasov S.A. Dual role of TNF and LTα in carcinogenesis as implicated by studies in mice. Cancers. 2021;13:1775. doi: 10.3390/cancers13081775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jiang H., Hampel H., Prvulovic D., Wallin A., Blennow K., Li R., Shen Y. Elevated CSF levels of TACE activity and soluble TNF receptors in subjects with mild cognitive impairment and patients with Alzheimer’s disease. Mol. Neurodegener. 2011;6:69. doi: 10.1186/1750-1326-6-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Waters J.P., Pober J.S., Bradley J.R. Tumour necrosis factor and cancer. J. Pathol. 2013;230:241–248. doi: 10.1002/path.4188. [DOI] [PubMed] [Google Scholar]
- 58.Nooijen P.T., Manusama E.R., Eggermont A.M., Schalkwijk L., Stavast J., Marquet R.L., de Waal R.M., Ruiter D.J. Synergistic effects of TNF-Alpha and melphalan in an isolated limb perfusion model of rat sarcoma: A histopathological, immunohistochemical and electron microscopical study. Br. J. Cancer. 1996;74:1908. doi: 10.1038/bjc.1996.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Van Horssen R., ten Hagen T.L.M., Eggermont A.M.M. TNF-α in Cancer treatment: Molecular insights, antitumor effects, and clinical utility. Oncologist. 2006;11:397–408. doi: 10.1634/theoncologist.11-4-397. [DOI] [PubMed] [Google Scholar]
- 60.Bradley J.R., Thiru S., Pober J.S. Disparate localization of 55-Kd and 75-Kd tumor necrosis factor receptors in human endothelial cells. Am. J. Pathol. 1995;146:27. [PMC free article] [PubMed] [Google Scholar]
- 61.Brouckaert P., Takahashi N., van Tiel S.T., Hostens J., Eggermont A.M.M., Seynhaeve A.L.B., Fiers W., Hagen T.L.M. Ten tumor necrosis factor-α augmented tumor response in B16BL6 melanoma-bearing mice treated with stealth liposomal doxorubicin (Doxil®) correlates with altered Doxil® pharmacokinetics. Int. J. Cancer. 2004;109:442–448. doi: 10.1002/ijc.11703. [DOI] [PubMed] [Google Scholar]
- 62.Ten Hagen T.L.M., van der Veen A.H., Nooijen P.T.G.A., van Tiel S.T., Seynhaeve A.L.B., Eggermont A.M.M. Low-dose tumor necrosis factor-α augments antitumor activity of stealth liposomal doxorubicin (DOXIL®) in soft tissue sarcoma-bearing rats. J. Cancer. 2000;87:829–837. doi: 10.1002/1097-0215(20000915)87:6<829::AID-IJC12>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 63.Veen A.H.v.d., Wilt J.H.W.d., Eggermont A.M.M., Tiel S.T.v., Seynhaeve A.L.B., Hagen T.L.M. Ten TNF- α augments intratumoural concentrations of doxorubicin in TNF- α -based isolated limb perfusion in rat sarcoma models and enhances anti-tumour effects. Br. J. Cancer. 2000;82:973. doi: 10.1054/bjoc.1999.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fràter-Schröder M., Risau W., Hallmann R., Gautschi P., Böhlen P. Tumor necrosis factor type alpha, a potent inhibitor of endothelial cell growth in vitro, is angiogenic in vivo. Proc. Natl. Acad. Sci. USA. 1987;84:5277. doi: 10.1073/pnas.84.15.5277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sainson R.C.A., Johnston D.A., Chu H.C., Holderfield M.T., Nakatsu M.N., Crampton S.P., Davis J., Conn E., Hughes C.C.W. TNF primes endothelial cells for angiogenic sprouting by inducing a tip cell phenotype. Blood. 2008;111:4997–5007. doi: 10.1182/blood-2007-08-108597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Giraudo E., Primo L., Audero E., Gerber H.-P., Koolwijk P., Soker S., Klagsbrun M., Ferrara N., Bussolino F. Tumor necrosis factor-α regulates expression of vascular endothelial growth factor receptor-2 and of its co-receptor neuropilin-1 in human vascular endothelial cells. J. Biol. Chem. 1998;273:22128–22135. doi: 10.1074/jbc.273.34.22128. [DOI] [PubMed] [Google Scholar]
- 67.Patterson C., Perrella M.A., Endege W.O., Yoshizumi M., Lee M.E., Haber E. Downregulation of vascular endothelial growth factor receptors by tumor necrosis factor-alpha in cultured human vascular endothelial cells. J. Clin. Investig. 1996;98:490. doi: 10.1172/JCI118816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fajardo L., Kwan H., Kowalski J., Prionas D., Allison A. Dual role of tumor necrosis factor-alpha in angiogenesis. Am. J. Pathol. 1992;140:539–544. [PMC free article] [PubMed] [Google Scholar]
- 69.Gina L., Tonya C.W., Steven M.D. Chronic inflammation, chronic obstructive pulmonary disease, and lung cancer. Curr. Opin. Pulm. Med. 2009;15:303–307. doi: 10.1097/MCP.0B013E32832C975A. [DOI] [PubMed] [Google Scholar]
- 70.Greten F.R., Grivennikov S.I. Inflammation and cancer: Triggers, mechanisms, and consequences. Immunity. 2019;51:27–41. doi: 10.1016/j.immuni.2019.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yan B., Wang H., Rabbani Z.N., Zhao Y., Li W., Yuan Y., Li F., Dewhirst M.W., Li C.-Y. Tumor necrosis factor-α is a potent endogenous mutagen that promotes cellular transformation. Cancer Res. 2006;66:11565–11570. doi: 10.1158/0008-5472.CAN-06-2540. [DOI] [PubMed] [Google Scholar]
- 72.Grivennikov S.I. Inflammation and colorectal cancer: Colitis-associated neoplasia. Semin. Immunopathol. 2012;35:229–244. doi: 10.1007/s00281-012-0352-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Suarez-Carmona M., Lesage J., Cataldo D., Gilles C. EMT and inflammation: Inseparable actors of cancer progression. Mol. Oncol. 2017;11:805–823. doi: 10.1002/1878-0261.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Balkwill F. TNF-α in promotion and progression of cancer. Cancer Metastasis Rev. 2006;25:409–416. doi: 10.1007/s10555-006-9005-3. [DOI] [PubMed] [Google Scholar]
- 75.Gaur U., Aggarwal B.B. Regulation of proliferation, survival and apoptosis by members of the TNF superfamily. Biochem. Pharmacol. 2003;66:1403–1408. doi: 10.1016/S0006-2952(03)00490-8. [DOI] [PubMed] [Google Scholar]
- 76.Idriss T.H., Naismith H. James TNFα and the TNF receptor superfamily: Structure-function relationship(s) Microsc. Res. Tech. 2000;50:184–195. doi: 10.1002/1097-0029(20000801)50:3<184::AID-JEMT2>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 77.Huang Y., Yu X., Wang L., Zhou S., Sun J., Feng N., Nie S., Wu J., Gao F., Fei B., et al. Four genetic polymorphisms of lymphotoxin-alpha gene and cancer risk: A systematic review and meta-analysis. PLoS ONE. 2013;8:e82519. doi: 10.1371/journal.pone.0082519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Vesely M.D., Schreiber R.D. Cancer immunoediting: Antigens, mechanisms, and implications to cancer immunotherapy. Ann. N. Y. Acad. Sci. 2013;1284:1–5. doi: 10.1111/nyas.12105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McCoach C.E., Bivona T.G. The evolving understanding of immunoediting and the clinical impact of immune escape. J. Thorac. Dis. 2018;10:1248–1252. doi: 10.21037/jtd.2018.03.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mittal D., Gubin M.M., Schreiber R.D., Smyth M.J. New insights into cancer immunoediting and its three component phases —elimination, equilibrium and escape. Curr. Opin. Immunol. 2014;27:16–25. doi: 10.1016/j.coi.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kratochvill F., Neale G., Haverkamp J.M., Van de Velde L.-A., Smith A.M., Kawauchi D., McEvoy J., Roussel M.F., Dyer M.A., Qualls J.E., et al. TNF counterbalances the emergence of M2 tumor macrophages. Cell Rep. 2015;12:1902–1914. doi: 10.1016/j.celrep.2015.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Braumüller H., Wieder T., Brenner E., Aßmann S., Hahn M., Alkhaled M., Schilbach K., Essmann F., Kneilling M., Griessinger C., et al. T-helper-1-cell cytokines drive cancer into senescence. Nature. 2013;494:361–365. doi: 10.1038/nature11824. [DOI] [PubMed] [Google Scholar]
- 83.Müller-Hermelink N., Braumüller H., Pichler B., Wieder T., Mailhammer R., Schaak K., Ghoreschi K., Yazdi A., Haubner R., Sander C.A., et al. TNFR1 signaling and IFN-γ signaling determine whether T cells induce tumor dormancy or promote multistage carcinogenesis. Cancer Cell. 2008;13:507–518. doi: 10.1016/j.ccr.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 84.Schioppa T., Moore R., Thompson R.G., Rosser E.C., Kulbe H., Nedospasov S., Mauri C., Coussens L.M., Balkwill F.R. B regulatory cells and the tumor-promoting actions of TNF-α during squamous carcinogenesis. Proc. Natl. Acad. Sci. USA. 2011;108:10662–10667. doi: 10.1073/pnas.1100994108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhao X., Rong L., Zhao X., Li X., Liu X., Deng J., Wu H., Xu X., Erben U., Wu P., et al. TNF Signaling drives myeloid-derived suppressor cell accumulation. J. Clin. Investig. 2012;122:4094–4104. doi: 10.1172/JCI64115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sayed M.F.a., Amrein M.A., Bührer E.D., Huguenin A.-L., Radpour R., Riether C., Ochsenbein A.F. T-cell–secreted TNFα induces emergency myelopoiesis and myeloid-derived suppressor cell differentiation in cancer. Cancer Res. 2019;79:346–359. doi: 10.1158/0008-5472.CAN-17-3026. [DOI] [PubMed] [Google Scholar]
- 87.Hu X., Li B., Li X., Zhao X., Wan L., Lin G., Yu M., Wang J., Jiang X., Feng W., et al. Transmembrane TNF-α promotes suppressive activities of myeloid-derived suppressor cells via TNFR2. J. Immunol. 2014;192:1320–1331. doi: 10.4049/jimmunol.1203195. [DOI] [PubMed] [Google Scholar]
- 88.Liu Y., Ji X., Kang N., Zhou J., Liang X., Li J., Han T., Zhao C., Yang T. Tumor necrosis factor α inhibition overcomes immunosuppressive M2b macrophage-induced bevacizumab resistance in triple-negative breast cancer. Cell Death Dis. 2020;11:1–13. doi: 10.1038/s41419-020-03161-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lung Statistics, Globocan, Number of New Cases. [(accessed on 1 July 2021)];2020 Available online: https://Gco.Iarc.Fr/Today/Data/Factsheets/Cancers/15-Lung-Fact-Sheet.Pdf.
- 90.Travis W.D., Brambilla E., Nicholson A.G., Yatabe Y., Austin J.H.M., Beasley M.B., Chirieac L.R., Dacic S., Duhig E., Flieder D.B., et al. The 2015 world health organization classification of lung tumors: Impact of genetic, clinical and radiologic advances since the 2004 classification. J. Thorac. Oncol. 2015;10:1243–1260. doi: 10.1097/JTO.0000000000000630. [DOI] [PubMed] [Google Scholar]
- 91.Hartl D., Tirouvanziam R., Laval J., Greene C.M., Habiel D., Sharma L., Yildirim A.Ö., Dela Cruz C.S., Hogaboam C.M. Innate immunity of the lung: From basic mechanisms to translational medicine. J. Innate Immun. 2018;10:487–501. doi: 10.1159/000487057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ermert M., Pantazis C., Duncker H.R., Grimminger F., Seeger W., Ermert L. In situ localization of TNFα/β, tace and TNF Receptors TNF-R1 and TNF-R2 in control and LPS-treated lung tissue. Cytokine. 2003;22:89–100. doi: 10.1016/S1043-4666(03)00117-0. [DOI] [PubMed] [Google Scholar]
- 93.Spella M., Stathopoulos G.T. Immune resistance in lung adenocarcinoma. Cancers. 2021;13:384. doi: 10.3390/cancers13030384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shih C.-M., Lee Y.-L., Chiou H.-L., Chen W., Chang G.-C., Chou M.-C., Lin L.-Y. Association of TNF-α polymorphism with susceptibility to and severity of non-small cell lung cancer. Lung Cancer. 2006;52:15–20. doi: 10.1016/j.lungcan.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 95.Xie H., Yao H., Huo Y., Li N., Cheng Y. Association between TNF-α gene 308G>A polymorphism and lung cancer risk: A meta-analysis. Tumor Biol. 2014;35:9693–9699. doi: 10.1007/s13277-014-2265-6. [DOI] [PubMed] [Google Scholar]
- 96.Ardestani S., Li B., Deskins D.L., Wu H., Massion P.P., Young P.P. Membrane versus soluble isoforms of TNF-α exert opposing effects on tumor growth and survival of tumor-associated myeloid cells. Cancer Res. 2013;73:3938–3950. doi: 10.1158/0008-5472.CAN-13-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yu W.-N., Lai Y.-J., Ma J.-W., Ho C.-T., Hung S.-W., Chen Y.-H., Chen C.-T., Kao J.-Y., Way T.-D. Citronellol induces necroptosis of human lung cancer cells via TNF-α pathway and reactive oxygen species accumulation. In Vivo. 2019;33:1193–1201. doi: 10.21873/invivo.11590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dimitrakopoulos F.-I.D., Kottorou A.E., Antonacopoulou A.G., Panagopoulos N., Scopa C., Kalofonou M., Dougenis D., Koutras A., Makatsoris T., Tzelepi V., et al. Expression of immune system-related membrane receptors CD40, RANK, BAFFR and LTβR Is associated with clinical outcome of operated non-small-cell lung cancer patients. J. Clin. Med. 2019;8:741. doi: 10.3390/jcm8050741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ren S., Tian Q., Amar N., Yu H., Rivard C.J., Caldwell C., Ng T.L., Tu M., Liu Y., Gao D., et al. The immune checkpoint, HVEM may contribute to immune escape in non-small cell lung cancer lacking PD-L1 expression. Lung Cancer. 2018;125:115–120. doi: 10.1016/j.lungcan.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 100.Díez-Villanueva A., Mallona I., Peinado M.A. Wanderer, an interactive viewer to explore DNA methylation and gene expression data in human cancer. Epigenetics Chromatin. 2015;8:1–8. doi: 10.1186/s13072-015-0014-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shang G.-S., Liu L., Qin Y.-W. IL-6 and TNF-α promote metastasis of lung cancer by inducing epithelial-mesenchymal transition. Oncol. Lett. 2017;13:4657. doi: 10.3892/ol.2017.6048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Chae Y., Chang S., Ko T., Anker J., Agte S., Iams W., Choi W., Lee K., Cruz M. Epithelial-mesenchymal transition (EMT) signature is inversely associated with T-cell infiltration in non-small cell lung cancer (NSCLC) Sci. Rep. 2018:8. doi: 10.1038/s41598-018-21061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gong L., Caetano M.d.S., Cumpian A.M., Daliri S., Flores A.G., Chang S.H., Ochoa C.E., Evans C.M., Yu Z., Moghaddam S.J. Tumor necrosis factor links chronic obstructive pulmonary disease and K-ras mutant lung cancer through induction of an immunosuppressive pro-tumor microenvironment. Oncoimmunology. 2016;5:e1229724. doi: 10.1080/2162402X.2016.1229724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Guo N., Wen Y., Wang C., Kang L., Wang X., Liu X., Soulika A.M., Liu B., Zhao M., Han X., et al. Lung adenocarcinoma-related TNF-α-dependent inflammation upregulates MHC-II on alveolar type II cells through CXCR-2 to contribute to treg expansion. FASEB J. 2020;34:12197–12213. doi: 10.1096/fj.202000166RR. [DOI] [PubMed] [Google Scholar]
- 105.Yang Y., Islam M.S., Hu Y., Chen X. TNFR2: Role in cancer immunology and immunotherapy. ImmunoTargets Ther. 2021;10:103–122. doi: 10.2147/ITT.S255224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhang Y.W., Chen Q.Q., Cao J., Xu L.Q., Tang X., Wang J., Zhang J., Dong L.X. Expression of tumor necrosis factor receptor 2 in human non-small cell lung cancer and its role as a potential prognostic biomarker. Thorac. Cancer. 2019;10:437. doi: 10.1111/1759-7714.12948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chen X., Subleski J.J., Kopf H., Howard O.M.Z., Männel D.N., Oppenheim J.J. Cutting edge: Expression of TNFR2 defines a maximally suppressive subset of mouse CD4+ CD25+ FoxP3+ T regulatory cells: Applicability to tumor-infiltrating t regulatory Cells. J. Immunol. 2008;180:6467–6471. doi: 10.4049/jimmunol.180.10.6467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yan F., Du R., Wei F., Zhao H., Yu J., Wang C., Zhan Z., Ding T., Ren X., Chen X., et al. Expression of TNFR2 by regulatory T cells in peripheral blood is correlated with clinical pathology of lung cancer patients. Cancer Immunol. Immunother. 2015;64:1475–1485. doi: 10.1007/s00262-015-1751-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Williams G.S., Mistry B., Guillard S., Ulrichsen J.C., Sandercock A.M., Wang J., González-Muñoz A., Parmentier J., Black C., Soden J., et al. Phenotypic screening reveals TNFR2 as a promising target for cancer immunotherapy. Oncotarget. 2016;7:68278–68291. doi: 10.18632/oncotarget.11943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sasi S.P., Bae S., Song J., Perepletchikov A., Schneider D., Carrozza J., Yan X., Kishore R., Enderling H., Goukassian D.A. Therapeutic non-toxic doses of TNF induce significant regression in TNFR2-P75 knockdown lewis lung carcinoma tumor Implants. PLoS ONE. 2014;9:92373. doi: 10.1371/journal.pone.0092373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ham B., Wang N., D’Costa Z., Fernandez M.C., Bourdeau F., Auguste P., Illemann M., Eefsen R.L., Høyer-Hansen G., Vainer B., et al. TNF receptor-2 facilitates an immunosuppressive microenvironment in the liver to promote the colonization and growth of hepatic metastases. Cancer Res. 2015;75:5235–5247. doi: 10.1158/0008-5472.CAN-14-3173. [DOI] [PubMed] [Google Scholar]
- 112.Remon J., Passiglia F., Ahn M.J., Barlesi F., Forde P.M., Garon E.B., Gettinger S., Goldberg S.B., Herbst R.S., Horn L., et al. Immune checkpoint inhibitors in thoracic malignancies: Review of the existing evidence by an IASLC expert panel and recommendations. J. Thorac. Oncol. 2020;15:914–947. doi: 10.1016/j.jtho.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 113.Ferro S., Huber V., Rivoltini L. Mechanisms of tumor immunotherapy, with a focus on thoracic cancers. J. Thorac. Dis. 2018;10:4619. doi: 10.21037/jtd.2018.07.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Freeman G.J., Long A.J., Iwai Y., Bourque K., Chernova T., Nishimura H., Fitz L.J., Malenkovich N., Okazaki T., Byrne M.C., et al. Engagement of the Pd-1 immunoinhibitory receptor by a Novel B7 family member leads to negative regulation of lymphocyte activation. J. Exp. Med. 2000;192:1027. doi: 10.1084/jem.192.7.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gao Q., Wang X.-Y., Qiu S.-J., Yamato I., Sho M., Nakajima Y., Zhou J., Li B.-Z., Shi Y.-H., Xiao Y.-S., et al. Overexpression of PD-L1 significantly associates with tumor aggressiveness and postoperative recurrence in human hepatocellular carcinoma. Clin. Cancer Res. 2009;15:971–979. doi: 10.1158/1078-0432.CCR-08-1608. [DOI] [PubMed] [Google Scholar]
- 116.Bristol Myers Squibb—Bristol Myers Squibb Statement on Opdivo (Nivolumab) Small Cell Lung Cancer U.S. [(accessed on 9 August 2021)]; Available online: https://news.bms.com/news/details/2020/Bristol-Myers-Squibb-Statement-on-Opdivo-nivolumab-Small-Cell-Lung-Cancer-US-Indication/default.aspx.
- 117.Perez-Ruiz E., Minute L., Otano I., Alvarez M., Ochoa M.C., Belsue V., de Andrea C., Rodriguez-Ruiz M.E., Perez-Gracia J.L., Marquez-Rodas I., et al. Prophylactic TNF blockade uncouples efficacy and toxicity in dual CTLA-4 and PD-1 immunotherapy. Nature. 2019;569:428–432. doi: 10.1038/s41586-019-1162-y. [DOI] [PubMed] [Google Scholar]
- 118.Ferrara R., Mezquita L., Texier M., Lahmar J., Audigier-Valette C., Tessonnier L., Mazieres J., Zalcman G., Brosseau S., Le Moulec S., et al. Hyperprogressive disease in patients with advanced non–small cell lung cancer treated with PD-1/PD-L1 inhibitors or with single-agent chemotherapy. JAMA Oncol. 2018;4:1543–1552. doi: 10.1001/jamaoncol.2018.3676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hartley G.P., Chow L., Ammons D.T., Wheat W.H., Dow S.W. Programmed cell death ligand 1 (PD-L1) signaling regulates macrophage proliferation and activation. Cancer Immunol. Res. 2018;6:1260–1273. doi: 10.1158/2326-6066.CIR-17-0537. [DOI] [PubMed] [Google Scholar]
- 120.Hartley G., Regan D., Guth A., Dow S. Regulation of PD-L1 expression on murine tumor-associated monocytes and macrophages by locally produced TNF-α. Cancer Immunol. Immunother. CII. 2017;66:523. doi: 10.1007/s00262-017-1955-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jeong H., Kim S., Hong B.-J., Lee C.-J., Kim Y.-E., Bok S., Oh J.-M., Gwak S.-H., Yoo M.Y., Lee M.S., et al. Tumor-associated macrophages enhance tumor hypoxia and aerobic glycolysis. Cancer Res. 2019;79:795–806. doi: 10.1158/0008-5472.CAN-18-2545. [DOI] [PubMed] [Google Scholar]
- 122.Westendorf A.M., Skibbe K., Adamczyk A., Buer J., Geffers R., Hansen W., Pastille E., Jendrossek V. Hypoxia enhances immunosuppression by inhibiting CD4+ effector T cell function and promoting treg activity. Cell. Physiol. Biochem. 2017;41:1271–1284. doi: 10.1159/000464429. [DOI] [PubMed] [Google Scholar]
- 123.Lim S.-O., Li C.-W., Xia W., Cha J.-H., Chan L.-C., Wu Y., Chang S.-S., Lin W.-C., Hsu J.-M., Hsu Y.-H., et al. Deubiquitination and stabilization of PD-L1 by CSN5. Cancer Cell. 2016;30:925–939. doi: 10.1016/j.ccell.2016.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bertrand F., Montfort A., Marcheteau E., Imbert C., Gilhodes J., Filleron T., Rochaix P., Andrieu-Abadie N., Levade T., Meyer N., et al. TNFα blockade overcomes resistance to anti-PD-1 in experimental melanoma. Nat. Commun. 2017;8:1–13. doi: 10.1038/s41467-017-02358-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Landsberg J., Kohlmeyer J., Renn M., Bald T., Rogava M., Cron M., Fatho M., Lennerz V., Wölfel T., Hölzel M., et al. Melanomas resist T-cell therapy through inflammation-induced reversible dedifferentiation. Nature. 2012;490:412–416. doi: 10.1038/nature11538. [DOI] [PubMed] [Google Scholar]
- 126.Bertrand F., Rochotte J., Colacios C., Montfort A., Tilkin-Mariamé A.F., Touriol C., Rochaix P., Lajoie-Mazenc I., Andrieu-Abadie N., Levade T., et al. Blocking tumor necrosis factor α enhances CD8 T-cell-dependent immunity in experimental melanoma. Cancer Res. 2015;75:2619–2628. doi: 10.1158/0008-5472.CAN-14-2524. [DOI] [PubMed] [Google Scholar]
- 127.Bertrand F., Colacios C., Ségui B. TNF-R1, an immune checkpoint in melanoma? Genes Cancer. 2015;6:369. doi: 10.18632/genesandcancer.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.TNF-Inhibitor as Immune Checkpoint Inhibitor for Advanced MELanoma—TICIMEL—ClinicalTrials.Gov: NCT03293784. [(accessed on 9 August 2021)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03293784.
- 129.Wilderman M.J., Kim S., Gillespie C.T., Sun J., Kapoor V., Vachani A., Sterman D.H., Kaiser L.R., Albelda S.M. Blockade of TNF-α decreases both inflammation and efficacy of intrapulmonary ad.IFNβ immunotherapy in an orthotopic model of bronchogenic lung cancer. Mol. Ther. 2006;13:910–917. doi: 10.1016/j.ymthe.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 130.Boutsikou E., Domvri K., Hardavella G., Tsiouda D., Zarogoulidis K., Kontakiotis T. Tumour necrosis factor, interferon-gamma and interleukins as predictive markers of antiprogrammed cell-death protein-1 treatment in advanced non-small cell lung cancer: A pragmatic approach in clinical practice. Ther. Adv. Med Oncol. 2018;10:1758835918768238. doi: 10.1177/1758835918768238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Trefny M.P., Rothschild S.I., Uhlenbrock F., Rieder D., Kasenda B., Stanczak M.A., Berner F., Kashyap A.S., Kaiser M., Herzig P., et al. A variant of a killer cell immunoglobulin-like receptor is associated with resistance to PD-1 blockade in lung cancer. Clin. Cancer Res. 2019;25:3026–3034. doi: 10.1158/1078-0432.CCR-18-3041. [DOI] [PubMed] [Google Scholar]
- 132.Mercogliano M.F., Bruni S., Mauro F., Elizalde P.V., Schillaci R. Harnessing tumor necrosis factor alpha to achieve effective cancer immunotherapy. Cancers. 2021;13:564. doi: 10.3390/cancers13030564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sobo-Vujanovic A., Vujanovic L., DeLeo A.B., Concha-Benavente F., Ferris R.L., Lin Y., Vujanovic N.L. Inhibition of soluble tumor necrosis factor prevents chemically-induced carcinogenesis in mice. Cancer Immunol. Res. 2016;4:441. doi: 10.1158/2326-6066.CIR-15-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Vujanovic L., Szymkowski D.E., Alber S., Watkins S.C., Vujanovic N.L., Butterfield L.H. Virally infected and matured human dendritic cells activate natural killer cells via cooperative activity of plasma membrane-bound TNF and IL-15. Blood. 2010;116:575–583. doi: 10.1182/blood-2009-08-240325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Shaikh F., He J., Bhadra P., Chen X., Siu S.W.I. TNF receptor type II as an emerging drug target for the treatment of cancer, autoimmune diseases, and graft-versus-host disease: Current Perspectives and in silico search for small molecule binders. Front. Immunol. 2018;9:1382. doi: 10.3389/fimmu.2018.01382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Sheng Y., Li F., Qin Z. TNF receptor 2 makes tumor necrosis factor a friend of tumors. Front. Immunol. 2018;9:1170. doi: 10.3389/fimmu.2018.01170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fischer R., Kontermann R.E., Pfizenmaier K. Selective targeting of TNF receptors as a novel therapeutic approach. Front. Cell Dev. Biol. 2020;8:401. doi: 10.3389/fcell.2020.00401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Torrey H., Butterworth J., Mera T., Okubo Y., Wang L., Baum D., Defusco A., Plager S., Warden S., Huang D., et al. Targeting TNFR2 with antagonistic antibodies inhibits proliferation of ovarian cancer cells and tumor-associated tregs. Sci. Signal. 2017;10:462. doi: 10.1126/scisignal.aaf8608. [DOI] [PubMed] [Google Scholar]
- 139.Torrey H., Kühtreiber W.M., Okubo Y., Tran L., Case K., Zheng H., Vanamee E., Faustman D.L. A novel TNFR2 agonist antibody expands highly potent regulatory T cells. Sci. Signal. 2020;13:661. doi: 10.1126/scisignal.aba9600. [DOI] [PubMed] [Google Scholar]
- 140.Tam E.M., Fulton R.B., Sampson J.F., Muda M., Camblin A., Richards J., Koshkaryev A., Tang J., Kurella V., Jiao Y., et al. Antibody-mediated targeting of TNFR2 activates CD8+ T cells in mice and promotes antitumor immunity. Sci. Transl. Med. 2019;11:512. doi: 10.1126/scitranslmed.aax0720. [DOI] [PubMed] [Google Scholar]