Abstract
BACKGROUND:
The objective was to assess the prevalence and the associated demographic factors of stress, anxiety, and depression among undergraduate (UG) Indian dental students and determine whether the pattern is different in government-run institutions and those managed by private authorities.
MATERIALS AND METHODS:
A cross-sectional study was conducted among dental UG students from five dental colleges. Snowball sampling was used to approach 776 potential participants, resulting in a complete response from 507 students. The questionnaire consisted of demographic data; year of study; type of college; accommodation; and Depression, Anxiety, and Stress Scale (DASS)-42. Descriptive data and inferential statistics were obtained. Chi-square test was applied for categorical data to test for significance, and higher analysis was done using multiple linear regression.
RESULTS:
Females and males comprised 71.8% (n = 364) and 28.2% (n = 143) of the study population, respectively. The prevalence of anxiety was highest (66.86%, n = 339), followed by depression (57.39%, n = 291) and stress (43.99%, n = 223). In terms of severity also, anxiety was the most prevalent condition as more than one-fourth of the students presented with severe and very severe scores in this aspect (25.43%, n = 129) compared to depression (14.39%, n = 73) and stress (10.09%, n = 51). Regression analysis revealed age as a strong positive predictor for all the three conditions, while staying in the hostel was a positive predictor for anxiety and stress. Being female was also an independent predictor for the high prevalence of stress.
CONCLUSION:
Stress, anxiety, and depression are highly prevalent among Indian dental students. Clinical students and interns have a higher prevalence of stress than preclinical students. Age, being female, and staying in the hostel are positive predictors for the severity of stress. There is no significant difference between government and private colleges, regarding the prevalence of any psychological condition.
Keywords: Anxiety, dental education, depression, stress
Introduction
Stress is a result of the discrepancy between excessive pressure or different types of demands and the individual capacities to deal with these challenges. Persistent stress can lead to psychological disturbance in the form of depression, anxiety, and burnout as well as influence their course. Dental students are expected to put a lot of effort to acquire a wide range of knowledge and mastering the required skills. Existing literature suggests that the prevalence of depression, anxiety, and stress among dental students is very high.[1] Previous data support the observation that dental students have a higher prevalence of negative psychological conditions than their fellow medical students. Some others have reported this level to be comparable to that observed in psychiatric patients.[2,3,4] Such disturbances can hamper the learning ability and academic performance as well as adversely affect patient care. In extreme cases, it can also lead to the tendency of self-harm.[5] Most similar studies have been conducted in the West Asian countries, and very little data are available for dental students in South Asia.[6,7] Because India has the highest number of dental schools in the world, while dentists have limited job prospects, the pattern of psychological issues is expected to be different from that of other countries.[6] The pattern may vary among different regions of India due to the diversity in social and cultural backgrounds, financial status, and future aspirations. Because the social and cultural factors influence the perception of stress, the findings of cross-sectional studies in one region cannot be generalized to other regions, especially when the sources of stress and predisposing factors have continuously evolved over past years.
All the policymakers and other stakeholders in dental education need to know the status of mental health among the students and the possible predisposing factors associated with it. Although it is impossible to eradicate all contributing factors of stress in dental education, identifying them can enable us to prepare the students for their future professional life and contribute toward their personal and psychosomatic well-being.
The Depression, Anxiety, and Stress Scale (DASS)-42 has been used previously in many studies, evaluating the psychological status of medical and dental students in India as well as of those in many other countries.[8,9] This scale has shown excellent reliability, good convergent validity, and acceptable-to-good discriminant validity.[10,11,12]
The present study aims to assess the prevalence of stress, anxiety, and depression and its predictors in undergraduate (UG) dental students in India using the DASS-42.
Materials and Methods
This questionnaire-based, multicentric, cross-sectional study was conducted among UG dental students and interns from five different dental colleges in North India.
Data collection
The study participants were recruited by snowball sampling method. The data were collected from December 2018 to March 2019. To ensure voluntary involvement without any pressure, one of the authors selected one volunteer from each batch of students and trained them about the purpose and methodology of the data collection. Instead of any faculty member, these volunteers approached their classmates and invited them to participate. They explained that participation is entirely voluntary, and no data would be recorded, which could reveal their identity. The students were given a printed copy of the questionnaire and were asked to fill it up at their convenient time and place and return it the next day. Written consent was obtained on a separate sheet at the time of the distribution of the questionnaire. All the participating students were encouraged to approach their friends in other colleges in nearby cities for participation. Those who offered to help were made volunteers and provided with the printed copy of the questionnaire and the pro forma of the informed consent to receive fellow students' responses from other colleges. All the students who refused to participate for any reason were not approached again. The self-administered questionnaire included a brief paragraph on the purpose of the study, followed by two sections. The first section inquired about age, followed by multiple-choice questions related to gender, year of study, type of college (government or private), and accommodation (staying in a hostel or living with the family). The second section included 42 questions from a previously validated and standardized survey instrument, DASS-42. Each of the three parameters (depression, anxiety, and stress) was measured using 14 questions each, scored on a 4-point (0–3) answer scale, where values refer to as 0; did not apply to me at all, 1; applied to me to some degree or some of the time, 2; applied to me to a considerable degree or a good part of the time, and 3; applied to me very much or most of the time. Depression, anxiety, and stress scores were calculated by summing up the responses of each parameter's relevant questions.
Sample size estimation
Considering the prevalence of stress among dental students in a previous study (54.7%, Basudan et al. 2017), absolute precision of 5%, type 1 error of 5%, and confidence interval of 95%, the sample size estimated was 396. However, considering the likelihood of incomplete/incorrect data or refusal to participate due to noncomprehension of questions or stigma attached to such topics among the Indian population, we planned to approach 700 students and interns.
Inclusion and exclusion criteria
All UG students, including interns, were eligible to participate in the study. First-year students who had not completed at least six months in a dental college and those who had to appear in any examination (class test/sessional test/professional examination) in the coming one week were not approached. It was written on the first page of the questionnaire that those who were unable to comprehend the language, suffering from any chronic illness, or undergoing treatment for any psychiatric disorder should not submit their responses.
Data analysis
Statistical analysis was performed using SPSS version 20.0 (IBM Corp. NY, USA). The internal consistency of the questionnaire was assessed by calculating Cronbach's alpha. Descriptive statistics (means, standard deviation, percentage, and frequency) were calculated for demographic as well as the DASS data. Pearson's Chi-square test was used to analyze the data at a significance level of P < 0.05. Multiple linear regression was used to test whether the levels of depression, anxiety, and stress scores could be predicted by any demographic variables recorded in the questionnaire.
Ethical consideration
The study was approved by the Board of Studies, Department of Periodontics and Community Dentistry, and the Institutional Ethics Committee of Faculty of Medicine, Aligarh Muslim University, Aligarh, India, with the code D. No. 8927/Perio/DC/18.
Results
We were able to contact a total of 776 students and interns from five different dental colleges (two managed by the government and three private) in North India, out of which 523 students returned the filled up questionnaire, amounting to a response rate of 67.4%. A total of 16 questionnaire forms had missing data, and therefore only 507 were analyzed. A significant internal consistency of the questionnaire was observed for depression (Cronbach's alpha; 0.87), anxiety (Cronbach's alpha; 0.91), and stress (Cronbach's alpha; 0.89). The mean age of the participants was 22.04 ± 2.20 years (range 17–32 years). The majority of the participants were female (n = 364, 71.8%). Interns were the largest group (n = 224, 44.2%), while the first-year students made up only 3.4% (n = 17) of the study population. Complete demographic data are presented in Table 1. The mean values of depression, anxiety, and stress were found to be 12.07 ± 8.66, 11.05 ± 7.01, and 14.71 ± 7.92, respectively. According to the criteria of DASS, the overall prevalence of abnormal levels of anxiety was 66.86% (n = 339, anxiety scores ≥8), followed by depression at 57.39% (n = 291, depression scores ≥10) and stress at 43.99% (n = 223, stress scores ≥15) [Table 2]. In terms of severity also, anxiety was the most prevalent condition, as more than one-fourth of the students presented with severe and very severe scores in this aspect (25.43%, n = 129, anxiety scores ≥15) compared to that of depression (14.39%, n = 73, depression scores ≥21) and stress (10.09%, n = 51, stress scores ≥26). The distribution of participants according to severity based on DASS scores is depicted in Figure 1. Simple linear regression analysis was performed to predict the levels of depression, anxiety, and stress based on demographic factors [Table 3].
Table 1.
Demographic data of the sample population (n=507)
| Parameter | Variables | n (%) |
|---|---|---|
| Gender | Male | 143 (28.2) |
| Female | 364 (71.8) | |
| Year of study | First-year | 17 (3.4) |
| Second-year | 116 (22.9) | |
| Third-year | 91 (17.9) | |
| Final year | 59 (11.6) | |
| Internship | 224 (44.2) | |
| Type of college | Government | 201 (39.6) |
| Private | 306 (60.4) | |
| Accommodation | Staying in the hostel | 274 (54) |
| Living with the family | 233 (46) |
Table 2.
Prevalence of depression, anxiety, and stress in different sub-groups
| Parameters | Depression | Anxiety | Stress | Row total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||
| Normal, n (%) | Depressed, n (%) | χ 2 | P | Normal, n (%) | Anxious, n (%) | χ2 | P | Normal, n (%) | Stressed, n (%) | P | |||
| Gender | |||||||||||||
| Male | 57 (39.86) | 86 (60.14) | 0.61 | 0.433 | 49 (34.27) | 94 (65.73) | 0.11 | 0.734 | 87 (60.84) | 56 (39.16) | 1.88 | 0.17 | 143 |
| Female | 159 (43.68) | 205 (56.32) | 119 (32.69) | 245 (67.31) | 197 (54.12) | 167 (45.88) | 364 | ||||||
| Type of college | |||||||||||||
| Government | 79 (39.30) | 122 (60.70) | 1.48 | 0.223 | 61 (30.35) | 140 (69.65) | 1.17 | 0.279 | 106 (52.74) | 95 (47.26) | 1.45 | 0.227 | 201 |
| Private | 137 (44.77) | 169 (55.23) | 107 (34.97) | 199 (65.33) | 178 (58.17) | 128 (41.83) | 306 | ||||||
| Year of study | |||||||||||||
| First | 8 (47.06) | 9 (52.94) | 4.06 | 0.397 | 5 (29.41) | 12 (70.59) | 10.66 | 0.030* | 11 (64.71) | 6 (35.29) | 7.87 | 0.096 | 17 |
| Second | 56 (48.28) | 60 (51.72) | 50 (43.10) | 66 (56.70) | 77 (66.38) | 39 (33.62) | 116 | ||||||
| Third | 35 (38.46) | 56 (61.54) | 26 (28.57) | 65 (71.43) | 47 (51.65) | 44 (48.35) | 91 | ||||||
| Final | 26 (35.14) | 48 (64.86) | 16 (21.62) | 58 (78.38) | 37 (50) | 37 (50) | 74 | ||||||
| Internship | 91 (43.54) | 118 (56.46) | 71 (33.97) | 138 (66.03) | 112 (53.59) | 97 (46.41) | 209 | ||||||
| Accommodation | |||||||||||||
| Hostel | 107 (39.05) | 167 (60.95) | 3.08 | 0.079 | 77 (28.10) | 197 (71.90) | 6.82 | 0.009* | 146 (53.28) | 128 (46.71) | 1.8 | 0.179 | 274 |
| Family | 109 (46.78) | 124 (53.22) | 91 (39.06) | 142 (60.94) | 138 (59.23) | 95 (40.77) | 233 | ||||||
| Total | 216 (42.60) | 291 (57.39) | 168 (33.14) | 339 (66.86) | 284 (56.01) | 223 (43.99) | 507 | ||||||
*Statistically significant
Figure 1.
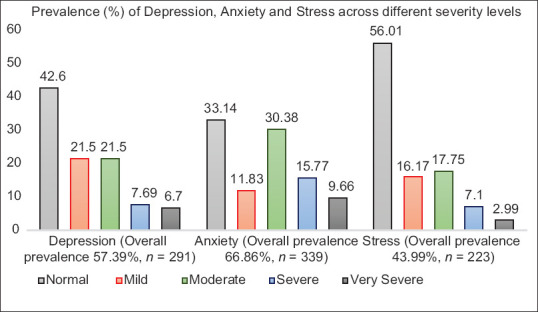
Prevalence (%) of Depression, Anxiety and Stress across different severity levels. Mild: (depression scores 10-13, anxiety scores 8-9, stress scores 15-18), Moderate: (depression scores 14-20, anxiety scores 10-14, stress scores 19-25), Severe: (depression scores 21-27, anxiety scores 15-19, stress scores 26-33), and Very severe: (depression scores ≥28, anxiety scores ≥20, stress scores ≥34)
Table 3.
Multiple linear regression model for the prediction of depression, anxiety, and stress
| Predictor | Outcome (severity of depression/anxiety/stress) | Standardized Coefficients (β) | t | Significance (P) | Collinearity Statistics | |
|---|---|---|---|---|---|---|
|
| ||||||
| Tolerance | Variance Inflation Factor (VIF) | |||||
| Constant | D | −0.540 | 0.590 | |||
| A | 0.148 | 0.882 | ||||
| S | −1.174 | 0.241 | ||||
| Age | D | 0.163 | 3.715 | <0.001* | 1.000 | 1.000 |
| A | 0.122 | 2.754 | 0.006* | 0.985 | 1.015 | |
| S | 0.172 | 3.823 | <0.001* | 0.941 | 1.063 | |
| Gender | D | 0.053 | 1.182 | 0.238 | 0.947 | 1.055 |
| A | 0.050 | 1.099 | 0.272 | 0.918 | 1.090 | |
| S | 0.119 | 2.617 | 0.009* | 0.918 | 1.090 | |
| Type of institute | D | −0.050 | −1.139 | 0.255 | 0.993 | 1.007 |
| A | 0.009 | 0.199 | 0.843 | 0.985 | 1.015 | |
| S | −0.061 | −1.380 | 0.168 | 0.985 | 1.015 | |
| Year of study | D | −0.001 | −0.018 | 0.986 | 0.472 | 2.118 |
| A | 0.000 | 0.006 | 0.995 | 0.461 | 2.168 | |
| S | 0.001 | 0.008 | 0.993 | 0.454 | 2.203 | |
| Accommodation | D | 0.040 | 0.893 | 0.372 | 0.985 | 1.015 |
| A | 0.093 | 2.104 | 0.036* | 0.985 | 1.015 | |
| S | 0.100 | 2.236 | 0.026* | 0.954 | 1.049 | |
*Statistically Significant
Age
A significant regression equation was found between depression and age (F(1,505) = 13.801, P < 0.001), with an R2 of 0.25. Depression score increased by 0.64, anxiety score by 0.39, and stress score by 0.62 for each year of age.
Gender
The prevalence of anxiety and stress was higher among females, but depression was more common among male students [Table 2]. A significant regression equation was found for stress with gender (b = 2.096, t = 2.617, P = 0.009). The severity of stress was also positively correlated with being female (β = 0.119).
Year of study
All the three conditions were most common in final year students, followed by third-year students. Looking at the curve, the prevalence of all the three conditions started on a higher note in the first-year, dropping marginally in the second-year, followed by a continuous increase till the final year and a decrease again in the internship [Figure 2]. On pair-wise comparison, no difference was statistically significant in terms of the prevalence of depression, whereas that of anxiety was significantly higher in both the third- and final years than the second-year students. This parameter was also significantly higher in the final year students than in the interns. In terms of stress, the prevalence was significantly higher among the third-year and final year students, as well as in the interns, when compared to that in second-year students [Table 4]. Pair-wise comparisons were also performed between preclinical students (first- and second-years), clinical students (third- and final years), and interns. No significant difference was observed in the prevalence of depression, whereas anxiety was significantly higher among the clinical students than in the preclinical students. Stress was significantly higher in both clinical students and interns than that in the preclinical students [Table 4].
Figure 2.
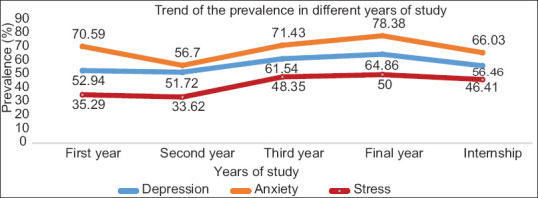
Trend in the prevalence of depression, anxiety, and stress in different years of study
Table 4.
Pair-wise comparison of prevalence among different years of study
| Inter-group comparison | Depression | Anxiety | Stress | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| χ 2 | P | χ 2 | P | χ 2 | P | |
| First versus second | 0.008 | 0.925 | 1.146 | 0.284 | 0.018 | 0.892 |
| First versus third | 0.442 | 0.506 | 0.005 | 0.943 | 0.982 | 0.322 |
| First versus final | 0.839 | 0.359 | 0.472 | 0.492 | 1.199 | 0.273 |
| First versus internship | 0.079 | 0.778 | 0.146 | 0.702 | 0.783 | 0.376 |
| Second versus third | 1.994 | 0.157 | 4.635 | 0.031* | 4.607 | 0.032* |
| Second versus final | 3.180 | 0.074 | 9.198 | 0.002* | 5.05 | 0.025* |
| Second versus internship | 0.675 | 0.411 | 2.662 | 0.103 | 5.015 | 0.025* |
| Third versus final | 0.194 | 0.659 | 1.039 | 0.308 | 0.044 | 0.833 |
| Third versus internship | 0.671 | 0.412 | 0.845 | 0.358 | 0.096 | 0.757 |
| Final versus internship | 1.592 | 0.207 | 3.915 | 0.048 | 0.282 | 0.595 |
| Preclinical versus clinical | 3.76 | 0.052 | 8.48 | 0.003* | 7.023 | 0.008* |
| Preclinical versus internship | 0.687 | 0.407 | 1.903 | 0.168 | 5.295 | 0.021* |
| Clinical versus internship | 1.651 | 0.199 | 3.172 | 0.075 | 0.265 | 0.606 |
| *Statistically Significant | No significant findings | Third, final >second Final >internship Clinical >preclinical |
Third, final and internship >second Clinical >preclinical Internship >preclinical |
|||
Government versus private colleges
Students from government colleges showed a higher prevalence of all the three negative aspects of psychological health than their counterparts from private colleges. However, this difference was not statistically significant.
Accommodation
Students staying in the hostels were found to have a higher prevalence of all the three parameters than those living with the family. However, the difference was statistically significant (P = 0.009) only for the anxiety scores [Table 2]. A significant regression equation was found between anxiety and accommodation (b = 1.310, t = 2.104, P = 0.036) as well as stress and accommodation (b = 1.586, t = 2.236, P = 0.026). Staying in the hostels was associated with higher scores of anxiety (β = 0.093) as well as stress (β = 0.100).
Discussion
The high prevalence of stress, anxiety, and depression in this cross-sectional study is not surprising among Indian dental students. It is important to know that dentistry may not be the first choice for the majority of the UG students in India as reported by multiple studies where more than 60% of the students reported that they joined a BDS program because they had no other option, and 69% of them were forced by their parents to take up this course.[13] Another recent study from a government-run dental college in South India found that 77% of students opted for it because they could not get an MBBS seat.[14] The lack of interest in the profession has been reported as the most common nonacademic reason of stress among BDS students.[6]
On the other hand, job prospects in the dental field are scarce as compared to the increasing number of dentists passing out every year. The situation is not much different now for those with a postgraduate (PG) degree. Jain et al. did a similar survey among UG and PG students as well as teachers.[15] They found an overall high prevalence of depression (31.86%), anxiety (50.44%), and stress (21.24%). Not surprisingly, UG students had a higher prevalence of all the three conditions than their seniors and teachers.
In the current study, a higher number of female respondents reflect the actual demography of dental colleges in India.[6,16,17] A relatively lower response rate than most of the previous studies was mainly because of the minimal participation of first-year students, as the volunteering students from their batches were probably not able to convince them to respond on this sensitive topic. However, we still did not involve teachers or college management for direct interaction with the students to avoid any undue pressure and to keep their participation voluntary and their response anonymous and unbiased. Many final year students did not participate because some examinations were scheduled in the coming week.
Constant stress, if not recognized or left untreated, can lead to depression. The prevalence of depression (57.39%) in the present study was the highest among those reported by UG Indian medical and dental students and much higher than that of the general Indian population (15.9%).[18] Similar high prevalence has been reported among Saudi medical and dental students using DASS-21 and Indian medical students using DASS-42.[8,9,19] The prevalence of stress as high as 57.98%, 48.4%, and 32% had been reported among medical students in the West, South, and North India, respectively.[20,21,22] The differences may be attributed partially to the different indices used in these studies as well as the different social and regional factors.
Anxiety is the psychophysiological signal which indicates that the stress response has been initiated. This potentially debilitating condition is reported to be predictive of reduced performance.[23] A high prevalence of anxiety (66.86%) in our study was in agreement with that of the previous reports from India and Saudi Arabia using DASS-21 or DASS-42 among dental and medical students.[8,9,15,18] Similarly, these studies also reported higher prevalence among females, as found in the current study. Some studies among Indian and Iranian dental students, however, have reported no association between gender and the prevalence of anxiety.[12,24]
We found the maximum prevalence of anxiety and stress in the final year students, similar to the data reported by many previous studies on Indian dental students.[6,13,15,16] Stress was significantly more common among clinical students (third- and final year) and interns, when compared to the preclinical (first- and second-years) group. This finding is consistent with that of many previous studies among Indian dental students.[16,20,25] Clinical students have a very high workload to be completed within a short time, apart from dealing with patients. Students also face more frequent examinations in the final year than during any previous year. Interns were found less vulnerable to anxiety than final year students, as reported previously, although they are concerned about the future, which does not appear very promising to most of them.[12,16] Not everyone can make it through the PG entrance examination for the admission in Master of Dental Surgery (MDS) courses either because of limited seats in the government colleges or due to financial constraints in private colleges. Those planning to start their practice or settling for a private job are not relaxed either. Still, the feeling of accomplishment after clearing all the examinations of the BDS course and receiving stipends during the internship could have some positive effect on their anxiety levels.
Not many studies among Indian dental students have tried to find the association of the type of accommodation with the mental health parameters.[15,16] We found a significantly higher prevalence of anxiety (71.9%) among students staying in the hostels as compared to those staying with their families (60.94%). Similar data have been reported among Indian and Egyptian dental students way back in 2011 and 2012, respectively.[15,26,27] A recent study among the Pakistani medical, nursing, and dental hygiene students also supported these findings. This pattern seems obvious owing to the regional culture, where a firm bond exists among the family members. Not only are younger members guided by their elders, but they can also fall back upon them for emotional, financial, and material support. Although staying in the hostels prepares students for an independent life, many of them could not adjust to the additional responsibilities which otherwise are taken care of by the parents at home. Being alienated by senior students and feeling homesick are other important causes of stress and anxiety among students trying to adjust in a hostel environment.
The prevalence of stress (43.99%) was relatively lower than that of the other two conditions in the present study. Taneja et al. reported similar data (43.8%) using DASS-21 in North Indian medical students.[22] Deshpande and Chari reported an even lower prevalence of 38% among UG students of a South Indian private dental college.[16] However, Saudi and Iranian studies have reported a much higher prevalence of stress.[9,19,24] Stress was also found to be significantly associated with females, as reported previously in medical, dental, and dental hygiene students.[7,8,9,14,28] However, many previous studies have reported higher stress among male dental students, while others have found no correlation of stress with gender among Indian and Iranian dental students.[12,16,17,19,24,25]
Conflict with the previous data from different countries could be due to the difference in curriculum design as well as job prospects. However, the conflicting data from previous Indian studies can be attributed to the continuously widening paradigm of the sources of stress over the past two decades. The sources of stress and anxiety have certainly increased over the past 10–15 years. There has been a continuous decline in job opportunities for dentists over these years, which may be attributed to the opening of new dental colleges, with more dentists passing out every year. Internet access was not common, and social media was not there 15 years ago. Gender-based demography in Indian dental colleges has also changed significantly over these years, with a continuous increase in female: male ratio.[16,29] Female responders comprised 57% of the sample in a similar study published in 2003, while other studies among UG dental students published in 2014, 2015, and 2019 have reported 76%, 78%, and 77% of females responders constituting the sample, respectively.[6,16,29]
A novel finding in the present study was the positive correlation of age with all the three negative affective states, irrespective of any other demographic parameter. As the UG students grow older, they face potentially stressful experiences for the first time, including managing financial concerns, making career decisions, and being in a relationship that may or may not be approved by their parents. They are also expected to show maturity in handling these challenges. By the end of their final year or internship, most of the female students in India who comprise a majority in our sample population are under pressure to get married by their parents. We also observed a wide range in the age reported by the students, with some of them aged over 30 years. Considering these data, the role of the quarter-life crisis in the independent positive correlation of age with depression, anxiety, and stress cannot be ruled out.
The prevalence of all the three negative states was found to be higher among students from government-run colleges as compared to those managed by private bodies. However, the differences were not statistically significant. Admission in a government college in India generally requires higher scores in the qualifying examination, following which dental students avail of a highly subsidized education and hostel fees, with some additional relief to students from the marginal sections of the society. On the other hand, the cost of education is several times higher in the private colleges. As a result, there is a considerable difference in the average socioeconomic status, aptitude, aspirations, and concerns about future prospects among students from these two types of institutions. Shadman et al. recently reported that Iranian students who performed better in the entrance examination and were studying free of charge presented significantly higher levels of severe-to-extremely severe stress and depression than the students who were being charged tuition fees.[24] They attributed this finding to the continued higher competitive approach and consequent worry about the grades among the students who performed better and had their education charges waived off. In another large-scale study involving students from six European countries, subsidized students were found to have 63% reduced odds of reporting performance pressure and 37% reduced odds of reporting faculty and administration as more stressful, reflecting less perceived stress in the academic environment. However, they were still more concerned about self-efficacy beliefs and patient treatment. This finding was attributed to the different profile of students admitted to subsidized dental schools.[30] This may also be applicable in the Indian scenario.
Our study presents a comprehensive evaluation of depression, anxiety, and stress, along with an analysis of correlations with different demographics, in a large sample of students from as many as five dental colleges in North India. This is also the first study to compare the prevalence of depression, anxiety, and stress among UG students from private and government dental colleges in India. Keeping our target population limited to BDS students was another advantage. Students from PG dental courses (MDS) as well as dental auxiliary (dental hygienists and dental mechanics) students have quite different aspirations, curricula, and challenges from those of BDS students. Hence, including them might not have reflected the real picture. However, all of these findings cannot be generalized to students from other regional, social, and cultural backgrounds. Although all attempts were made to encourage unbiased responses by the students, over- and under-reporting cannot be completely ruled out. We did not inquire about the stressors, coping behaviors, socioeconomic status of the family, satisfaction with syllabus and teaching methods, and the availability and utilization of recreational facilities in colleges, which are other significant limitations.
Conclusion
There are high prevalences of depression, anxiety, and stress among UG students of dental colleges situated in North India, with more than two-thirds of respondents having symptoms of anxiety. All the three conditions positively correlated with the increasing age and were most common in final year students. Students staying in hostels have a higher prevalence of anxiety and stress than their fellows living with their family. Females show a higher level of stress irrespective of any other demographic parameters. There is an urgent need to address the factors leading to poor mental health among future dentists. Counseling points may be arranged at every institute for students with symptoms of anxiety or depression, particularly in their third- and final years of study. Dental institutes may also develop a framework with parents to assess the psychological well-being at college, hostel, and home, particularly before and during examinations. Workshops may be organized at regular intervals to foster emotional intelligence, inculcate time management skills, and motivate students to cope with stress in college life.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are thankful to all the participating students and interns for their valuable time and support in the collection of data.
References
- 1.Alzahem AM, van der Molen HT, Alaujan AH, Schmidt HG, Za-makhshary MH. Stress amongst dental students: A systematic review. Eur J Dent Educ. 2011;15:8–18. doi: 10.1111/j.1600-0579.2010.00640.x. [DOI] [PubMed] [Google Scholar]
- 2.Lloyd C, Musser LA. Psychiatric symptoms in dental students. J Nerv Ment Dis. 1989;177:61–9. doi: 10.1097/00005053-198902000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Humphris G, Blinkhorn A, Freeman R, Gorter R, Hoad-Reddick G, Murtomaa H, et al. Psychological stress in undergraduate dental students: Baseline results from seven European dental schools. Eur J Dent Educ. 2002;6:22–9. doi: 10.1034/j.1600-0579.2002.060105.x. [DOI] [PubMed] [Google Scholar]
- 4.Murphy RJ, Gray SA, Sterling G, Reeves K, DuCette J. A comparative study of professional student stress. J Dent Educ. 2009;73:328–37. [PubMed] [Google Scholar]
- 5.Al-Saleh SA, Al-Madi EM, Al-Angari NS, Al-Shehri HA, Shukri MM. Survey of perceived stress-inducing problems among dental students, Saudi Arabia. Saudi Dent J. 2010;22:83–8. doi: 10.1016/j.sdentj.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bathla M, Singh M, Kulhara P, Chandna S, Aneja J. Evaluation of anxiety, depression and suicidal intent in undergraduate dental students: A cross-sectional study. Contemp Clin Dent. 2015;6:215–22. doi: 10.4103/0976-237X.156050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rehmani N, Khan QA, Fatima SS. Stress, anxiety and depression in students of a private medical school in Karachi, Pakistan. Pak J Med Sci. 2018;34:696–701. doi: 10.12669/pjms.343.14664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iqbal S, Gupta S, Venkatarao E. Stress, anxiety and depression among medical undergraduate students and their socio-demographic correlates. Indian J Med Res. 2015;141:354–7. doi: 10.4103/0971-5916.156571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basudan S, Binanzan N, Alhassan A. Depression, anxiety and stress in dental students. Int J Med Educ. 2017;8:179–86. doi: 10.5116/ijme.5910.b961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. second ed. Sydney: Psychology Foundation; 1995. [Google Scholar]
- 11.Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large nonclinical sample. Br J Clin Psychol. 2005;44:227–39. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 12.Madhan B, Barik AK, Patil R, Gayathri H, Reddy MS. Sense of humor and its association with psychological disturbances among dental students in India. J Dent Educ. 2013;77:1338–44. [PubMed] [Google Scholar]
- 13.Tangade PS, Mathur A, Gupta R, Chaudhary S. Assessment of stress level among dental school students: An Indian outlook. Dent Res J (Isfahan) 2011;8:95–101. [PMC free article] [PubMed] [Google Scholar]
- 14.Raghunathan D, Ramakrishnan D, Valsan KI, Ambika S. Prevalence of depression among students of a dental tertiary care center in Kerala. Indian J Community Med. 2019;44(Suppl 1):14. doi: 10.4103/ijcm.IJCM_23_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jain M, Sharma A, Singh S, Jain V, Miglani S. The stress of clinical dental training: A cross-sectional survey among dental students and dentists of a dental college in India. J Indian Assoc Public Health Dent. 2016;14:434–9. [Google Scholar]
- 16.Deshpande A, Chari S. Perceived sources of stress and coping strategies in dental students and interns. J Psychol. 2014;5:133–41. [Google Scholar]
- 17.Sekhon TS, Grewal S, Gambhir RS, Sharma S. Perceived sources of stress among dental college students: An Indian perspective. Eur J Gen Dent. 2015;4:121–6. [Google Scholar]
- 18.Poongothai S, Pradeepa R, Ganesan A, Mohan V. Prevalence of depression in a large urban South Indian population – The Chennai urban rural epidemiology study (CURES70) PLoS One. 2009;4:e7185. doi: 10.1371/journal.pone.0007185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aboalshamat K, Hou XY, Strodl E. Psychological well-being status among medical and dental students in Makkah, Saudi Arabia: A cross-sectional study. Med Teach. 2015;37(Suppl 1):S75–81. doi: 10.3109/0142159X.2015.1006612. [DOI] [PubMed] [Google Scholar]
- 20.Kumar S, Dagli RJ, Mathur A, Jain M, Prabu D, Kulkarni S. Perceived sources of stress amongst Indian dental students. Eur J Dent Educ. 2009;13:39–45. doi: 10.1111/j.1600-0579.2008.00535.x. [DOI] [PubMed] [Google Scholar]
- 21.Hakim A, Tak H, Nagar S, Bhansal S. Assessment of prevalence of depression and anxiety and factors associated with them in undergraduate medical students of Dr. S. N. Medical College, Jodhpur. Int J Community Med Public Health. 2017;4:3267–72. [Google Scholar]
- 22.Taneja N, Sachdeva S, Dwivedi N. Assessment of depression, anxiety, and stress among medical students enrolled in a medical college of New Delhi, India. Indian J Soc Psychiatry. 2018;34:157–62. [Google Scholar]
- 23.Sanders AE, Lushington K. Effect of perceived stress on student performance in dental school. J Dent Educ. 2002;66:75–81. [PubMed] [Google Scholar]
- 24.Shadman N, Raoof M, Amanpour S, Mahdian M, Haghani J, Parizi MT. Stress, anxiety, and depression and their related factors among dental students: A cross-sectional study from southeast of Iran. Strides Dev Med Educ. 2019;16:e74295. [Google Scholar]
- 25.Acharya S. Factors affecting stress among Indian dental students. J Dent Educ. 2003;67:1140–8. [PubMed] [Google Scholar]
- 26.Sedky NA. Perceived sources of stress among junior & mid-senior Egyptian dental students. Int J Health Sci (Qassim) 2012;6:141–57. doi: 10.12816/0005990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Srivastava R, Jyoti B, Pradhan D, Kumar M, Priyadarshi P. Evaluating the stress and its association with stressors among the dental undergraduate students of Kanpur city, India: A cross-sectional study. J Educ Health Promot. 2020;9:56. doi: 10.4103/jehp.jehp_405_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Safaie N, Ketabi S, Kia N, Mirmohammadkhani M, Moonesan MR, Paknazar F. Exploration of mental health problems in association with health-promoting lifestyle profile in Iranian medical students: A cross-sectional study. J Educ Health Promot. 2020;9:84. doi: 10.4103/jehp.jehp_582_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chowdhury CR, Khijmatgar S, Chowdhury A, Harding S, Lynch E, Gootveld M. Dental anxiety in first- and final-year Indian dental students. BDJ Open. 2019;5:15. doi: 10.1038/s41405-019-0017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Polychronopoulou A, Divaris K. Dental students’ perceived sources of stress: A multi-country study. J Dent Educ. 2009;73:631–9. [PubMed] [Google Scholar]


