Abstract
BACKGROUND:
Lecturing (didactic) has been the key teaching-learning method for a long time. As per competency-based medical education, an Indian medical graduate should be competent in recommended skills. In the subject of Community Medicine of medical undergraduation, “Biostatistics” is one of the components of the curriculum. Often the students find the statistics challenging to understand and thus neglect it or prefer rote learning. In the recent era, many newer teaching-learning modalities have come up, namely problem-based learning (PBL), small group teaching, community-based learning, etc. The objective was to compare the utility and effectiveness of PBL versus traditional teaching techniques (didactic) for Biostatistics.
MATERIALS AND METHODS:
The study was conducted in the department of Community Medicine, Government Medical College, Azamgarh (Uttar Pradesh) from March to November 2019. A total of 96 medical students of the final year were randomly divided into two groups. 'Group A' underwent didactic lecturing whereas “Group B” had problem-based learning for identified topics in Biostatistics. The teaching material and instructors were the same for both groups. Two weeks after completion of sessions, students' assessment was carried out for both groups.
RESULTS:
The study demonstrated that the PBL method was a more effective way of teaching-learning statistics compared to didactic lecturing. A significant difference (P < 0.05) was observed between the mean examination score of Group A (traditional teaching technique) and Group B (PBL). Group B had higher scores than group A in all assessment heads (Objective, Descriptive, and Viva-voce). PBL was perceived to be a student-centric Teaching-learning method promoting analytical skills, critical thinking & overall self-directed learning.
CONCLUSION:
PBL teaching method was found to be effective in improving the students' performance in Statistics in comparison to didactic lecturing.
Keywords: Performance, problem-based learning, statistics
Introduction
In medical education, the most commonly practiced teaching-learning method is Didactic lecturing, which is also referred to as, conventional or traditional teaching technique (TTT). Although it is the most feasible method for teaching a large number of students, it is often known for the passive transfer of knowledge from teacher to student and limited opportunity for feedback leading to low receptivity.[1] The academic satisfaction among students is a major concern to different departments of the university and also to the educational planner.[2] In the recent era, many newer teaching-learning modalities have come up like problem-based learning (PBL), team-based learning,[3] project-based, and case-based learning[4] .
As per competency-based medical education, an Indian medical graduate should be competent in recommended skills.[5] In the subject Community Medicine of medical under graduation, “Biostatistics” is one of the key areas of the curriculum to be taught. Even during postgraduation and while working as a faculty in a teaching institute, basic knowledge of statistics is essential for carrying out research. Biostatistics is a branch of applied statistics and it must be taught with the focus being on its various applications in biomedical research.[6] It is an essential tool for medical research, clinical decision making, and health management.[7]
Still today, the medical students often find the statistics part as difficult to understand and thus neglect it or prefer for rote learning. The biostatistical literacy of medical students is a problem all over the world.[6] Many students fail to make the connection between statistical reasoning and scientific inquiry[8] and this deficit in basic biostatistical knowledge adversely affects research quality. It may be because of its conceptual and mathematical nature wherein the students need to have analytical and problem-solving skills. As for the other topics, the Didactic lecture is the commonly used method for teaching Biostatistics too, which may be failing short because of its inbuilt limitations, namely herein the focus is on learning statistical concepts, not on the process of using statistics to solve problems. Not using an integrated approach is detrimental to statistics and research methods teaching, which is of particular concern in the age of evidence-based medicine.[9]
Writing on the teaching and learning of medical statistics remarked that medical practitioners were totally intimidated by the idea of statistics.[10] Surveys on this issue are uncommon in the literature.[7]
Considering this, in the present study, the PBL approach was explored and evaluated against the TTT for its utility and efficacy in facilitating the teaching-learning of biostatistics.
Materials and Methods
This comparative cross-sectional analytical study was conducted in the Department of Community Medicine, Government Medical College, Azamgarh (Uttar Pradesh), India from March to November 2019. The study was conducted after receiving IEC approval (1662/GMCA/IEC/2019) and informed consent from study participants. A total of 96 medical students of final year (Part-I) participated in the study and were randomly divided into two groups (Group A and Group B). Group A underwent traditional teaching technique (didactic lecturing) whereas Group B had a PBL approach for teaching-learning identified topics in Biostatistics. The teaching material and instructors were the same for both the groups. Two weeks after the completion of sessions, students' assessment was carried out using descriptive, objective, and viva-voce for both groups, and results were compared. At the end, the perception of students was sought by taking their feedback. For ethical reasons, after the completion of the study, the control group was also taught using the PBL approach; however, it was not included as a part of the present study [Figure 1].
Figure 1.
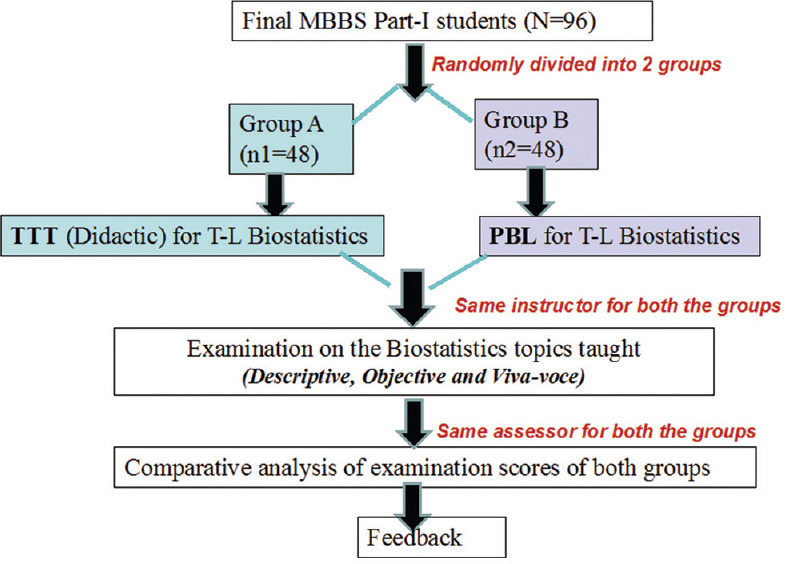
Plan of action of study
Following two study tools were used:
-
Examination Question paper-It had the following three components:
- Objective (MCQs) - 20 questions (each one mark)
- Viva voce - 10 questions (each two marks)
- Descriptive - 10 questions (2 LAQs- 15 Marks each and 5 SAQs -6 Marks each)
Total score - 100
Table 1 : Feedback form: Students' perception about the teaching-learning method for biostatistics
Table 1.
Feedback form: Students’ perception about the teaching-learning method for Biostatistics
| Items | 1 (SD) | 2 (D) | 3 (N) | 4 (A) | 5 (SA) |
|---|---|---|---|---|---|
| Gaining statistical reasoning skills (GCRS) | |||||
| Facilitation of problem-solving skills (FPSS) | |||||
| Facilitation of communication skills (FCS) | |||||
| Facilitation of self-directed learning (FSDL) | |||||
| Gaining robust retrievable knowledge (GRRK) | |||||
| Gaining basic science knowledge (GBSK) | |||||
| Facilitation of integration of basic and statistical science knowledge (FCSK) | |||||
| Increasing intrinsic motivation of student (IIMS) | |||||
| Facilitation of development of Self-assessment and peer assessment skills (SAPS) | |||||
| Overall effectiveness of Traditional teaching technique and Problem based learning (OE) |
1=SD, 2=D, 3=N, 4=A, 5=SA, SD=Strongly disagree, D=Disagree, N=Neutral, A=Agree, SA=Strongly agree,
Data analysis
Data entry and analysis were done using the IBM SPSS statistics for health care version 16. Descriptive analysis and t-test were used to test association. P ≤ 0.05 was taken as a statistically significant association.
Results
The age and gender-wise profile of both Group A and Group B, depicted that, there was no statistically significant difference in the mean age of study participants, and the male to female proportion was also similar with male students outnumbering the female. Thus, both the groups were similar with regard to age and gender [Table 2].
Table 2.
Distribution of students in Group A (traditional teaching techniques) and Group B (problem-based learning) according to age and gender
| Variables | Group A (TTT) (n1=48) | Group B (PBL) (n2=48) | P |
|---|---|---|---|
| Age, mean±SD | 23.44±1.90 | 24.40±2.28 | 0.5 |
| Male, n (%) | 35 (72.92) | 30 (62.50) | 0.32 |
| Female, n (%) | 13 (27.08) | 18 (37.50) |
*Unpaired t-test. TTT=Traditional teaching techniques, PBL=Problem-based learning, SD=Standard deviation
The students of Group A and B appeared for the examination and their scores were analyzed. It was found that the students in Group A who had the teaching-learning of Biostatistics through Traditional Teaching technique (didactic lecture) received mean marks as 30.67, 13.54, and 12.98 in descriptive (Out of 60 marks), objective (out of 20 marks), and viva-voce (Out of 20 marks) assessment heads respectively [Figure 2].
Figure 2.
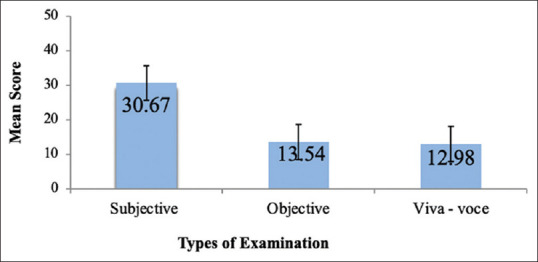
Mean score of students of Group A (Traditional teaching technique) in examination/assessment heads
In contrast, the students in Group B who had the teaching-learning of Biostatistics through the PBL method received mean marks as 41.06, 17.29, and 16.83 in descriptive (out of 60 marks), objective (out of 20 marks), and viva-voce (out of 20 marks) assessment heads, respectively [Figure 3].
Figure 3.
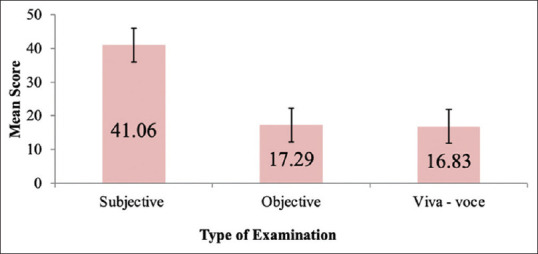
Mean score of students of Group B (Problem-based learning) in examination/assessment heads
The examination scores of both Group A and B were compared wherein a significant difference (P < 0.05) was observed between the mean examination score of Group A (TTT) and Group B (PBL) for all heads such as objective, descriptive, and viva voce in Statistics. The mean score was higher in Group B (PBL) for all assessment components [Table 3].
Table 3.
Comparison of examination score of students in Group A (traditional teaching technique) and Group B (problem-based learning)
| Exam questions | Mean±SD | P | |
|---|---|---|---|
|
| |||
| Group TTT (n=48) | Group PBL (n=48) | ||
| Objective (MCQs) (out of 20 marks) | 13.54±5.05 | 17.29±1.87 | 0.03 |
| Descriptive (out of 60 marks) | 30.67±2.10 | 41.06±1.34 | 0.01 |
| Viva voce (out of 20 marks) | 12.98±2.10 | 16.83±1.17 | 0.034 |
| Total (out of 100 marks) | 57.19±6.83 | 75.18±4.36 | 0.01 |
*Unpaired t-test. TTT = Traditional teaching technique, PBL = Problem-based learning, SD = Standard deviation, MCQs = Multiple Choice Questions
Figure 4 shows that for almost all feedback parameters the students in Group B (PBL) expressed a greater satisfaction than Group A (TTT). The maximum score on the five-point Likert scale was for Facilitation of integration of basic and statistical science knowledge and gaining basic science knowledge.
Figure 4.
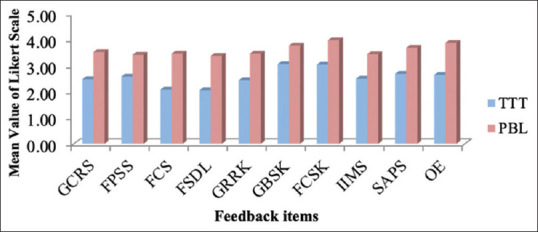
Distribution of students in Group A (Traditional teaching technique) and Group B (Problem-based learning) based on the feedback
Discussion
In the present study, a total of 96 participants (48 in each group) participated and were exposed to TTT and PBL approaches for teaching-learning Biostatistics. The mean examination score was statistically greater in Group B (PBL) than in Group A (TTT).
In PBL the self-study and group discussions develop self-directed learning, interdisciplinary knowledge creation, and collaborative skills. The entire process is very interactive, achieving the goal of student engagement in learning, which has been shown to improve retention and satisfaction.[11]
In conformity with the findings of the study, Shahabudin[12] demonstrated that students taught using PBL showed better factual recall than traditionally educated students. Kaufman et al. too reported that PBL students scored higher on the final professional Part-I.[13] The findings of the present study supported the hypothesis that statistics knowledge is certainly better retained if learnt using the PBL method compared with the traditional lecture method. Hwang and Kim[14] and McParland Monica et al.[15] found that the level of knowledge in the PBL group was significantly higher than that of students in the lecture group and a PBL curriculum resulted in significantly better examination performance than did the traditional teaching. A meta-analysis[16] on all 15 published studies to obtain an overall estimate of the effectiveness of PBL on learning outcomes of preventive medicine education was conducted in China. Seven of the studies tested the effectiveness of PBL for teaching-learning Medical statistics. The result showed that PBL in preventive medicine education appeared to be more effective than lecture-based learning in improving knowledge, attitude, and skills.
However, the findings of the present study are in contrast to certain studies that reported that undergraduate students in a PBL group had lower knowledge acquisition compared with those who received the lecture method.[17,18,19]
The students' feedback about the satisfaction level for PBL as well as TTT method based on ten parameters was undertaken. The mean score of all the items was more for PBL in comparison to TTT, indicating that the PBL was more acceptable than TTT for teaching-learning Statistics. The present study indicated that students were highly motivated to learning in problem-based approach and they expressed that the PBL approach help in developing better problem-solving skills, formulate evidence-based decisions, and enhance their communication skills.
It was found that in comparison to TTT, PBL facilitates better learning abilities, deeper comprehension of the concepts by students. PBL can help learners develop broader perspectives of case scenarios in developing their curiosity and lifelong learning habits.
This is in conformity with the study by Gibbon,[20] which found that PBL can help the students to become more effective in identifying, seeking out, and assimilating knowledge and it also helps to foster the development of their analytical and creative skills. Several studies have reported the improvement of other aspects of learning such as developing communication skills, autonomy, motivation development, and increasing the capacity of remembering the information as advantages of the PBL method.[21,22,23] Boyle[8] stated that by using statistics in real-life situations, PBL methods help life sciences students develop a strategy for dealing with problems, give them a mental framework for evaluating alternative methods of analysis, and motivate them to take responsibility for their own learning.
The study results are also in agreement with Claramita et al.[24] in which PBL was found to provoke the interest of medical students in participating in academic research related to Statistics in their future professional careers. Some of the unsatisfied elements for TTT are lack of supervision on students, intrinsic motivation, and course organization.
But there are studies wherein, the acceptance of PBL among the surveyed medical students was found to be low and that more rigorous and practical training is recommended to tutors and students to understand the philosophy of PBL.[1]
Overall the findings of this study showed a definite advantage of PBL when compared to lecture-based learning in equipping the learner with factual recall, analytical and critical thinking in addition to problem-solving skills for Biostatistics. The active participation of the students in group discussions, their independent and collective thinking related to practical scenarios, the triggers by different individuals in the group discussion with the facilitator during the consolidation phase have been the major factors for superior scores obtained.
Since the apical council is aiming for a curriculum focusing on competency-based medical education, it will be worthy and beneficial to incorporate the PBL approach for Statistics as well. The application of PBL for the medical statistics, a subject of mathematical nature adds to the novelty of the study. The learning objectives and trigger points as emerged from each case scenario/problem discussion in statistics will facilitate self-directed learning by students. A module or logbook consisting of case problem covering various topics in statistics can also be developed for a smooth transition from the traditional to the PBL approach.
Conclusion
PBL method was found to be an effective way of delivering statistics knowledge in medical education in comparison to the conventional didactic method. The examination score showed that PBL has a definite advantage in equipping the learner with factual recall, development of analytical and critical thinking in addition to problem-solving skills.
Limitations
Although the current study puts light on comparison between TTT and PBL method, it had some limitations such as small sample size that restricts the generalization of the results. Future research should examine the perception of the academic staff and faculty towards the utility of PBL for Biostatistics. Learning in a traditional environment is dependent on the interaction between the lecturer and the students. PBL emphasizes a more social constructivist model and therefore a single factor such as the teacher cannot be isolated in the same way. Therefore, future research may be undertaken to determine the effectiveness of PBL across different faculty.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Al-Naggar RA, Bobryshev YV. Acceptance of problem based learning among medical students. J Community Med Health Educ. 2012;2:146. [Google Scholar]
- 2.Coles CR, Grant JG. Curriculum evaluation in medical and health-care education. Med Educ. 1985;19:405–22. doi: 10.1111/j.1365-2923.1985.tb01345.x. [DOI] [PubMed] [Google Scholar]
- 3.Paes ÂT. IASE Satellite Paper. Federal University of São Paulo, Brazil; 2015. [Last accessed on 2020 Jul 17]. Perspectives on Teaching Biostatistics for Undergraduate Medical Students using Team-Based Learning. Available from: http://atpaes@unifesp.br . [Google Scholar]
- 4.Ishtiaq M, Iqbal N, Malik N, Rubab H, Hashim M. Project-based and case-based learning of statistics in undergraduate nursing students-Islamabad: A mixed method study. Ann Pak Inst Med Sci. 2017;13:61–7. [Google Scholar]
- 5.Competency Based Undergraduate Curriculum For The Indian Medical Graduate. Medical Council of India, Pocket-14, Sector- 8, Dwarka New Delhi 110 077; 2018. [Google Scholar]
- 6.Sami W. Biostatistics education for undergraduate medical students. Biomedica. 2010;26 Jan.-Jun. 26:6. [Google Scholar]
- 7.Adeleye OA, Ofili AN. Difficulty in understanding statistics: Medical students' perspectives in a Nigerian University. Int J Health Res. 2009;2:233–42. [Google Scholar]
- 8.Boyle CR. A problem based learning approach to teaching biostatistics. Mississippi State University. J Statistics Educ. 1999;7:N–1. [Google Scholar]
- 9.Bland JM. Teaching statistics to medical students using problem-based learning: The Australian experience. BMC Med Educ. 2004;4:31. doi: 10.1186/1472-6920-4-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stander I. Teaching conceptual vs. theoretical statistics to medical students. International Statistical Institute, 52nd Session. 1999. [Last accessed on 2011 Dec 29]. Available from: http://www.stat.auckland.ac.nz/~iase/publications/5/stan0219.pdf .
- 11.Berry W. Surviving lecture: A pedagogical alternative. Coll Teach. 2008;56:102–6. [Google Scholar]
- 12.Shahabudin SH. Content coverage in problem-based learning. Med Educ. 1987;21:310–4. doi: 10.1111/j.1365-2923.1987.tb00369.x. [DOI] [PubMed] [Google Scholar]
- 13.Kaufman A, Mennin S, Waterman R, Duban S, Hansbarger C, Silverblatt H, et al. The new Mexico experiment: Educational innovation and institutional change. Acad Med. 1989;64:285–94. doi: 10.1097/00001888-198906000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Hwang SY, Kim MJ. A comparison of problem-based learning and lecture-based learning in an adult health nursing course. Nurse Educ Today. 2006;26:315–21. doi: 10.1016/j.nedt.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 15.McParland M, Noble LM, Livingston G. The effectiveness of problem-based learning compared to traditional teaching in undergraduate psychiatry. Med Educ. 2004;38:859–67. doi: 10.1111/j.1365-2929.2004.01818.x. [DOI] [PubMed] [Google Scholar]
- 16.Ding XJ, Zhao L, Chu H, Tong N, Ni C, Hu Z, et al. Assessing the effectiveness of problem-based learning of preventive medicine education in China. Sci Rep. 2014;4:5126. doi: 10.1038/srep05126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andrews M, Jones PR. Problem-based learning in an undergraduate nursing programme: A case study. J Adv Nurs. 1996;23:357–65. doi: 10.1111/j.1365-2648.1996.tb02679.x. [DOI] [PubMed] [Google Scholar]
- 18.Frost M. An analysis of the scope and value of problem-based learning in the education of health care professionals. J Adv Nurs. 1996;24:1047–53. doi: 10.1111/j.1365-2648.1996.tb02942.x. [DOI] [PubMed] [Google Scholar]
- 19.Kim SA, Kang IA, Kim S, Nam KA, Park JH. Development of a problem-based learning program in nursing education curriculum. J Korean Psychiatr Nurs. 2000;9:559–70. [Google Scholar]
- 20.Gibbon C. Problem Based Learning & Nursing. 2011. [Last accessed on 2020 Aug 10]. Available from: http://www.ljmu.ac.uk/lid/ltweb .
- 21.Tseng HC, Chou FH, Wang HH, Ko HK, Jian SY, Weng WC. The effectiveness of problem-based learning and concept mapping among Taiwanese registered nursing students. Nurse Educ Today. 2011;31:e41–6. doi: 10.1016/j.nedt.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 22.Williams B. Self direction in a problem based learning program. Nurse Educ Today. 2004;24:277–85. doi: 10.1016/j.nedt.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 23.Li G, Zhang L. The exploration of PBL teaching method applied in medical statistics teaching. J Educ Jilin. 2013;29:53–5. [Google Scholar]
- 24.Claramita M, Budiharjo S, Suryadi E. Profile of the integrated clinical skills competencies (ICSC) on students with and without problem-based learning exposure. 2nd Asia-Pacific Conference on Problem- Based Learning in Health Science. 2001:FP 25. [Google Scholar]


