Abstract
The Amish lead a very simplistic lifestyle free of modern conveniences. They have unique perceptions and beliefs regarding health and illness and generally do not adhere to conventional preventive measures such as immunizations, which can result in un- or under-immunized populations. Populations with low vaccination coverage are at greater risk of outbreaks compared to vaccinated populations as a result of low herd immunity. Over the past two decades, the Delaware Division of Public Health (DPH) has recorded three distinct outbreaks of pertussis in Delaware’s Amish community. The third, and most recent, outbreak was detected in May 2018. DPH conducted an outbreak investigation in the Amish community to identify cases, estimate the burden of disease in the community, and implement control measures including vaccination, treatment, and post-exposure prophylaxis. Through the conduct of active surveillance activities, DPH interviewed 134 families and identified 181 confirmed and probable cases of pertussis. The majority of pertussis cases (77%) occurred among children ≤10 years of age, of which 87% were unvaccinated. DPH engaged the Amish community in meetings, distributed educational materials, and provided medication and vaccines in the community to encourage prevention and implement control measures. DPH officially closed the outbreak investigation on December 20, 2018 following three full incubation periods (63 days) without any new pertussis cases identified in the community.
Introduction
Kent County Delaware, just outside the city limits of Dover, is home to a picturesque and serene Amish community. Numerous buggy signs alert drivers to the presence of the Amish, cautioning vehicles to maintain slow speeds when passing buggies. Children play on traditional Amish scooters while plow teams of the gentle, giant Percheron horses work the fields.
The Amish lead a very simplistic lifestyle free of modern conveniences. Their faith calls for a life of hard work, discipline, humility, and avoidance of any form of self-expression. The family is the foundation of the Amish way of life. Large families are considered a gift from God. When its members live together, work together, worship together, and socialize together, the family is stronger. The wisdom of the elders and grandparents is a treasured asset, and their advice is often sought and followed from one generation to the next.
In Kent County the Amish are involved in a variety of trades including carpentry, masonry, furniture building, blacksmithing, farming, and sawmilling. They also successfully operate a number of community shops for items such as dry goods and quilts. Eleven one-room Amish schools within the community teach students in grades one through eight. After their education, Amish boys typically learn a trade, and girls acquire the skills necessary to raise children and maintain a home.
The Amish have unique perceptions and beliefs regarding health and illness, and pass many customs to their children and grandchildren. They generally do not adhere to conventional preventive measures such as immunizations. The Amish avoid health practices customary to the general population because they view them as actions that put man before God. Many families prefer to take responsibility for their own health by using herbs and natural remedies to mend injuries and care for sick loved ones.
Background
Pertussis is a highly contagious respiratory disease that can cause severe illness in persons of any age; however, children under one year of age are at highest risk of complications or more severe disease.1,2 Primary prevention methods include vaccination of persons of all ages.2,3 Vaccinations protect individuals and populations from the spread of infectious diseases by activating the body’s immune response (i.e., active immunity).4 As the percentage of the vaccinated population increases, herd immunity provides indirect protection to more effectively limit the spread of the disease to susceptible persons.5 To meet the herd immunity threshold for pertussis, or the “minimum proportion to be immunized in a population for elimination of infection,”5 vaccination coverage levels of at least 92% are required. Vaccination coverage in the Amish population has been documented as sub-optimal to provide herd immunity (<10%).6
Delaware reports cases of pertussis to the Centers for Disease Control and Prevention (CDC) annually. Between 2005 and 2018, the median number of reported pertussis cases reported in the state was 17 (see Figure 1). Over the past two decades, the Delaware Division of Public Health (DPH) has recorded three distinct outbreaks of pertussis in Delaware’s Amish community.7 The third and most recent outbreak was detected in May 2018. This report describes the public health investigation of the third outbreak of pertussis in the Amish community and opens the discussion to identify new approaches to increase vaccination and reduce the burden of disease in under- and unimmunized populations.
Figure 1.
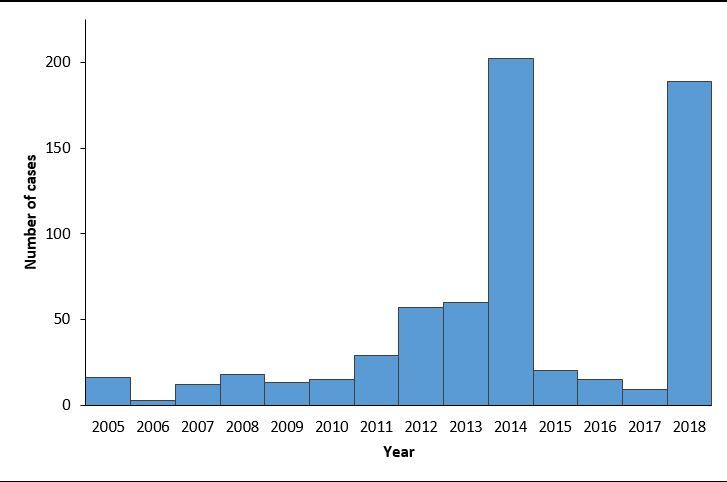
Reported number of pertussis cases, Delaware, 2005 – 2018 (2018 case counts are provisional and subject to change)
Methods
In May 2018, an Amish mother contacted a nurse at the DPH Kent County Health Unit (KCHU). She informed the staff that her child had been coughing for an extended period of time and asked to have her child tested for whooping cough. During her visit, she shared that other families in the community had children who were coughing or had whooping cough. The child tested positive for pertussis. At that time, it became clear that the likelihood of a potential outbreak existed in this population.
Outbreak investigation
To confirm the presence of an outbreak and to quantify the magnitude and spread of the disease throughout the community, DPH initiated active surveillance of pertussis in the Amish community. Active surveillance activities consisted of door-to-door contact investigation. DPH formed two-person field teams that included an epidemiologist and a clinic nurse that investigated reported cases, initiated contact tracing, conducted active case finding among the community, and initiated control measures. The clinic nurse carried nasopharyngeal (NP) swabs during home visits to collect specimens from ill individuals. A state courier transported specimens to the Delaware Public Health Laboratory where they were tested for Bordetella pertussis using polymerase chain reaction (PCR). Additionally, Amish families also directly contacted KCHU regarding ill children. Each family that presented to the clinic with a coughing child and symptoms compatible with pertussis were tested, and an epidemiologic case investigation was initiated.
Case definition and classification
DPH epidemiologists developed a case definition and modified the pertussis investigation questionnaire used in the 2013-2014 Amish outbreak. For this outbreak DPH used the National Notifiable Diseases Surveillance System (NNDSS) 2014 case definition for case classification. The case definition included clinical, laboratory, and epidemiologic linkage criteria. A case was defined a person living in Kent County with cough illness lasting greater than or equal to two weeks with onset between January 2018 and October 2018, and without other apparent cause. A confirmed case was defined as a clinical case of pertussis that: 1) was laboratory confirmed by PCR for B. pertussis; or 2) had an epidemiologic link to a laboratory-confirmed case in the same household residence or Amish community (e.g., school, church) with at least one of the following signs or symptoms: paroxysms of coughing, inspiratory ‘whoop,’ post-tussive emesis, or apnea (with or without cyanosis)(for infants aged <1 year only).8 A probable case was defined as meeting clinical criteria without laboratory confirmation or epidemiologic linkage. A primary case was defined as the first case in a household. A co-primary case was defined as a case with onset of symptoms within six days of a primary case. Secondary household transmission was defined as cough onset seven to 42 days following contact with a primary or co-primary case.
Control measures
In addition to active surveillance activities, DPH instituted control measures. On their visits to Amish homes, DPH field teams carried travel kits with vaccine to provide on-site vaccinations, as well as medications for treatment and/or prophylaxis to deliver to accepting families. Standing orders were written to enable dispensing of azithromycin during field visits for the duration of the outbreak.
Community outreach
In addition to clinic staff, DPH’s Community Health section consists of health educators known as the Community Engagement Team (CET). The CET conducted intensive community outreach and education using epidemiologic data provided by the field team epidemiologists. They distributed educational pamphlets and information sheets to Amish families during home visits. CET members distributed flyers to many businesses within the geographic area of the Amish population in Kent County. The team focused its resources on Amish-owned businesses as well as public and Amish schools to increase knowledge in the community about the current outbreak, treatment, and ways to prevent the disease. To ensure that outreach was conducted in areas where known disease transmission was most prevalent, the team used maps to compare outreach locations with pertussis case locations. Lastly, the lead epidemiologist and a CET member visited each Amish school and delivered flyers for students to take home to their parents about the prevention of, and treatment for, pertussis.
Results
DPH teams interviewed 134 families representing 67 households with confirmed/probable cases (see Table 1). Seventy-four cases were confirmed through laboratory testing (n=21) and epidemiologic linkage (n=53). An additional 107 probable cases were identified. Sixty-nine individuals received azithromycin for treatment or prevention of pertussis. Additionally, 28 individuals were vaccinated at the KCHU due to known exposure or to prevent illness.
Table 1. Characteristics of pertussis cases in an Amish community outbreak, Kent County, Delaware, January 2018 – October 2018.
| Characteristic |
Cases
n(%) |
Primary/Co-Primary cases
n(%) |
Secondary/Second Primary cases
n(%) |
|---|---|---|---|
| Sex | |||
| Male | 88 (49) | 45 (25) | 43 (24) |
| Female | 93 (51) | 47 (26) | 46 (25) |
| Age group (yrs) | |||
| <1 | 9 (5) | 5 (3) | 4 (2) |
| 1-5 | 73 (40) | 41 (23) | 32 (18) |
| 6-10 | 57 (31) | 29 (16) | 28 (16) |
| 11-14 | 18 (10) | 9 (5) | 9 (5) |
| 15-19 | 10 (5.5) | 4 (2) | 6 (3) |
| 20-29 | 8 (4.4) | 2 (1) | 6 (3) |
| >30 | 6 (3.3) | 2 (1) | 4 (2) |
| Vaccination status | |||
| Vaccinated | 19 (10.5) | 11 (6) | 9 (5) |
| Partially vaccinated* | 8 (4.4) | 4 (2) | 3 (1.6) |
| Unvaccinated | 154 (85) | 77 (43) | 77 (43) |
* Partially vaccinated is defined as receipt of ≤ 3 doses of vaccine against pertussis.
Primary and co-primary cases accounted for approximately 51% of all cases. Secondary household transmission and second primary household transmission accounted for approximately 40% and 9% of cases respectively (see Figure 2). Of the five non-Amish cases associated with the outbreak, all had direct, household contact with the Amish. One infant was hospitalized in May 2018 for pneumonia. This child was not tested for pertussis during the hospitalization but had clinically consistent illness and met the case definition for pertussis. No deaths were reported during the outbreak.
Figure 2.
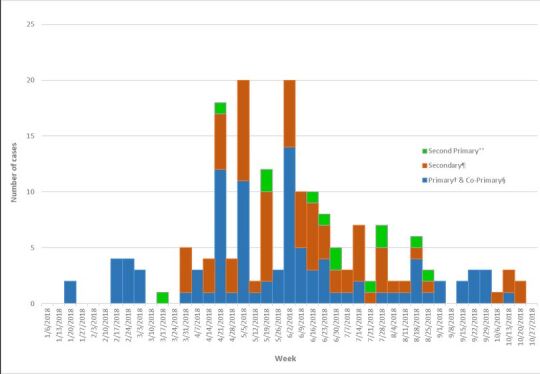
Number of pertussis cases in an Amish community outbreak, Kent County, Delaware, January 2018 – October 2018
Primary - First case in household; Co-Primary - Cough onset within 6 days of Primary case; Secondary - Cough onset 7-42 days after Primary case; Second Primary - Cough onset >42 days after Primary case
Of the 181 confirmed and probable cases, the majority of cases (77%) occurred among children ≤10 years with 40% of cases among children aged 1 to 5 years (see Figure 3). A smaller percentage of cases (14%) were ≥15 years (see Figure 4).
Figure 3.
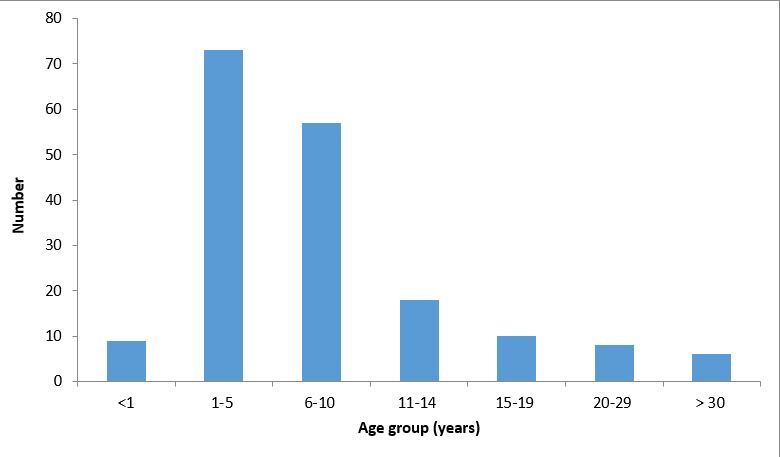
Number of pertussis cases in an Amish community outbreak by age group, Kent County, Delaware, January 2018 – October 2018
Figure 4.
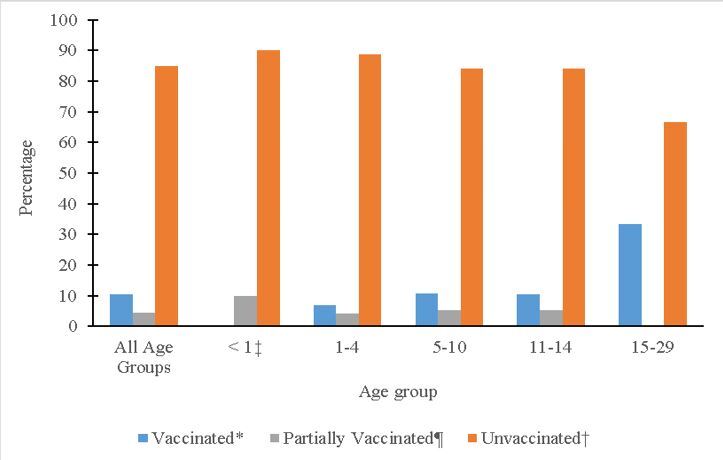
Vaccination status of pertussis cases in an Amish community outbreak by age group, Kent County, Delaware, January 2018 – October 2018
*Received ≥4 doses of vaccine against pertussis; † Received no vaccination against pertussis; Received ≤ 3 doses of vaccine against pertussis; ‡Infants per ACIP recommendations
During epidemiologic interviews, DPH asked family representatives about the vaccination status of all household members. Of the 181 cases, 10.5% reported being fully vaccinated against pertussis (5 doses), 4.4% reported being partially vaccinated (≤3 doses), and 85% reported having never received any pertussis vaccinations. Beginning October 23, 2018, DPH added two additional questions to the outbreak questionnaire to assess attitudes and beliefs regarding the use of antibiotics and vaccinations. Fear of side effects was the most common reason for choosing not to vaccinate or accept antibiotics. The CET distributed educational materials to over 50 businesses, local public schools, and Amish schools.
The last documented cough onset was October 18, 2018. DPH officially closed the outbreak investigation on December 20, 2018 following three full incubation periods (63 days) without any new cough illnesses identified in the community.
Discussion
In general, pertussis outbreaks in under- or unimmunized populations can be difficult to manage. The primary goal of pertussis outbreak control efforts is to decrease morbidity and mortality among infants; a secondary goal is to decrease morbidity among people of all ages. Fortunately, during this outbreak, only one hospitalization and no deaths were reported.
In contrast to the current outbreak, the previous two outbreaks that occurred in 2004 to 2005 and 2014 were defined by increasing numbers of cases during the late fall and winter months. The 2018 outbreak was defined by increasing numbers of cases in the early to late spring months. DPH hypothesized that the outbreak may have peaked in late April to early June of 2018. Similar trends in age groups and vaccination coverage were recorded in the previous outbreaks. Although DPH conducted the outbreak investigation upon identification of the index case, case ascertainment was incomplete despite extensive active surveillance activities in the Amish community. Disease transmission and exposure to unvaccinated children perpetuated the outbreak given the close social interaction of ambulatory children and the general lack of social distancing among the community. There were only five non-Amish pertussis cases documented in this outbreak signifying that spread outside the Amish population was limited to individuals with direct close contact with Amish cases.
During its response, DPH encountered potential barriers to vaccination and treatment. The DPH CET and clinic staff attempted to overcome access barriers by having surveillance teams bring vaccines and antibiotics to the home visits. There was limited uptake of medication. It is unclear whether these same individuals would have visited the local clinic or other healthcare provider to obtain antibiotics. In addition, surveillance teams noted that the Amish community were less receptive to home visits as compared to more positive interactions during previous outbreaks.
To gain further insight, DPH met with leaders within the community and contacted a local health department in Ohio that had experience with outbreaks within Amish communities. The discussion focused on providing accurate information to the Bishops on pertussis, vaccination, and antibiotic therapy. Additionally, the team discussed non-medical activities that the community could do to help decrease disease transmission; most importantly, the idea of social distancing. The Bishops welcomed the conversation and agreed to support DPH by providing education to their church members. In addition to focusing on the current outbreak, the conversation included ways for the DPH team to build and strengthen an ongoing partnership with the Amish community. Suggestions included meeting school officials after classes and contacting leaders directly to disseminate information. An interesting finding during the meeting was that many of their beliefs were not rooted in religion or faith. Residents researched non-evidence-based medical interventions through publications and periodicals, many of which promoted certain diets and avoidance of vaccination.
The local public health department in Ohio provided a similar perspective. It experienced similar challenges related to the community’s concerns and beliefs. It successfully gathered community preferences through surveys and maintained a presence by operating a clinic within the Amish community. Its community clinic strengthened relationships with the residents and improved access to medical care. DPH previously operated a clinic within the Amish community, which may in part weakened DPH’s relationship with the community, leading to some of the present challenges.
Conclusion
The pertussis outbreak investigation closely paralleled the previous pertussis outbreak in this community in 2004-2005. The same challenges and limitations of the previous outbreaks were present in the 2018 outbreak, including low vaccination rates, poor adherence to antibiotic treatment and/or prophylaxis, and poor compliance with social distancing. The current outbreak uncovered an interesting finding that religion is not the primary basis of their health beliefs. Many Amish avoid vaccinations because of their adherence to non-evidence-based medical interventions. These challenges hindered traditional prevention and control efforts. The low vaccination coverage and previous documented pertussis outbreaks in this community suggest that continued periodic circulation of B. pertussis is likely.
DPH recommends ongoing educational outreach to this susceptible community including: those at highest risk for serious illness, vaccination safety, and protective benefits of vaccination during pregnancy and possible complications.
Future considerations for community outreach and education with this community include:
Consistency of DPH’s presence by reinstituting DPH vaccination clinics in the community.
Hosting a health and safety fair to provide health and safety information that is of interest to Amish residents.
Educational outreach through the frequent provision of flyers and other educational information on a variety of health topics.
Acknowledgements
The authors acknowledge the contributions of the Delaware Division of Public Health’s pertussis outbreak team including Camille Moreno-Gorrin, Mamadou Diallo, Andrea Keen, Betty Jo Charles, Amber Scott, Christina Jackson, Odeama Chisholm, Lois Martinez, Yvonne Nelson, Cathy Strouse, Helen Madukwe, Niya Hall, Janet Bordley, Judy Seward, Michelle Broadway-Gardner, Wayne Smith, Shonetesha Quail, Martin Luta, Jim Talbott, and the Delaware Public Health Laboratory.
References
- 1.Kimberlin, David W, Michael T. Brady, Mary A. Jackson, and Sarah S. Long. Red Book: 2018-2021 Report of the Committee on Infectious Diseases, 2018.
- 2.Liang, J. L., Tiwari, T., Moro, P., Messonnier, N. E., Reingold, A., Sawyer, M., & Clark, T. A. (2018, April 27). Prevention of pertussis, tetanus, and diphtheria with vaccines in the United States: Recommendations of the Advisory Committee on Immunization Practices (ACIP).[ [PubMed https://doi.org/]. MMWR Recomm Rep, 67(2), 1–44. 10.15585/mmwr.rr6702a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Pertussis (Whooping Cough). About Pertussis. Pertussis Frequently Asked Questions. https://www.cdc.gov/pertussis/about/faqs.html. Page last reviewed on August 7, 2017. Accessed February 14, 2019.
- 4.Centers for Disease Control and Prevention. Vaccines & Immunizations. https://www.cdc.gov/vaccines/vac-gen/immunity-types.htm. Page last reviewed on March 10, 2017. Accessed February 14, 2019.
- 5.Fine, P. E. (1993). Herd immunity: History, theory, practice. [PubMed https://doi.org/]. Epidemiologic Reviews, 15(2), 265–302. 10.1093/oxfordjournals.epirev.a036121 [DOI] [PubMed] [Google Scholar]
- 6.Williamson, G., Ahmed, B., Kumar, P. S., Ostrov, B. E., & Ericson, J. E. (2017, September). Vaccine-preventable diseases requiring hospitalization. [PubMed]. Pediatrics, 140(3), e20170298. 10.1542/peds.2017-0298 [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) . (2006, August 4). Pertussis outbreak in an Amish community—Kent County, Delaware, September 2004-February 2005. [PubMed]. MMWR. Morbidity and Mortality Weekly Report, 55(30), 817–821. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC). Natonial Notifiable Disease Surveillance System (NNDSS). Surveillance Case Definitions. Pertussis. Pertussis/Whooping Cough (Bordetella pertussis) 2014 Case Definition. https://wwwn.cdc.gov/nndss/conditions/pertussis/case-definition/2014/. Accessed March 5, 2019.


