Abstract
The association between malignancy and readmission after Takotsubo syndrome (TTS) hospitalization has not been fully described. We sought to examine the rates, cause, and cost of 30-day readmissions of TTS, with or without malignancy, by utilizing Nationwide Readmissions Databases from 2010 to 2014. We identified 61,588 index hospitalizations for TTS. TTS patients with malignancy tended to be older (70.6 ± 0.2 vs. 66.1 ± 0.1, p < 0.001), and the overall burden of comorbidities was higher than in those without malignancy. TTS patients with malignancy had significantly higher 30-day readmission rates than those without malignancy (15.9% vs. 11.0%; odds ratio (OR), 1.35; 95% confidence interval (CI), 1.18–1.56). Non-cardiac causes were the most common causes of readmission for TTS patients with malignancy versus without malignancy (75.5% vs. 68.1%, p < 0.001). The 30-day readmission rate due to recurrent TTS was very low in both groups (0.4% and 0.5%; p = 0.47). The total costs were higher by 25% (p < 0.001) in TTS patients with vs. without malignancy. In summary, among patients hospitalized with TTS, the presence of malignancy was associated with increased risk of 30-day readmission and increased costs. These findings highlight the importance of optimized management for TTS patients with malignancy.
Keywords: Takotsubo syndrome, malignancy, readmission, cardio-oncology
1. Introduction
The Takotsubo syndrome (TTS), also known as stress-induced cardiomyopathy, can mimic acute coronary syndrome (ACS) and is an increasingly recognized cause of heart failure [1,2]. There are multiple theories regarding the pathophysiology of TTS, though the exact mechanisms remain uncertain [3]. The association between malignancy/chemotherapy and TTS has been reported in multiple studies [4,5,6]. Cancer patients who undergo systemic chemotherapy and/or radiation therapy often develop endothelial dysfunction in their epicardial and microvascular coronary vasculatures, which may play an important role in the high frequency of TTS observed in this cohort.
A recent study demonstrated a high prevalence of malignancy among TTS patients with an increased long-term mortality in TTS patients with concomitant malignancy [4,5]. Although TTS has been shown to be associated with frequent (12%) 30-day readmission, the clinical impact of readmission on TTS patients with malignancy and its associated economic burden on the US healthcare system is less evident [6,7]. Using the Nationwide Readmission Database (NRD), we sought to delineate the incidence, etiology, clinical impact, and costs of 30-day readmission in TTS patients with versus without malignancy.
2. Methods
2.1. Data Source
Data were obtained from the Agency for Healthcare Research and Quality, which administers the Healthcare Cost and Utilization Project (HCUP) [8,9]. We used the NRD from 2010 to 2014. The NRD is a large, administrative database constructed using discharge data from HCUP State Inpatient Databases. It has verified patient linkage numbers used to track the patients across hospitals within a state during a given year. The NRD is designed to support national readmission analyses and is a publicly available and nationally representative healthcare database. From 2010 to 2014, the NRD contained deidentified information for a total of 70,501,787 index hospitalizations from 1715–2048 hospitals in 18–20 states, representing a national estimate of 181,545,077 discharges. Each patient record in the NRD contains information on the patient’s diagnoses and procedures performed during the hospitalization, based on International Classification of Diseases, Ninth Revision-Clinical Modification (ICD-9-CM) codes and Clinical Classification Software (CCS) codes that groups multiple ICD-9-CM codes for facilitated statistical analyses. We identified our study population, comorbidities, causes of readmissions and in-hospital outcomes using a combination of ICD-9-CM codes and CCS codes. Institutional Review Board approval and informed consent were not required for the current study because all of the data collection derived from a publicly open and deidentified administrative database.
2.2. Study Population and Variables
From 2010 to 2014, all index hospitalizations for TTS were selected using ICD-9-CM code 429.83. To ensure that cases were TTS and not ACS, only those who underwent diagnostic coronary angiography (CCS 47) and no revascularization (Procedural CCS 44, 45 and ICD-9-CM procedure codes 36.06 and 36.07) were included in the analysis. Malignancy was identified by CCS code 11–45 [10]. Patients were categorized into 2 groups based on the presence or absence of malignancy.
Patient- and hospital-level variables were included as baseline characteristics. Patients with a concomitant diagnosis of cardiogenic shock and cardiac arrest were identified using ICM-9-CM codes 785.51 and 427.5, respectively. Concurrent use of intra-aortic balloon pump and percutaneous left ventricular assist devices were identified with ICD-9-CM procedure codes 37.61 and 37.68, respectively. Since NRD prohibits linking patients across years, patients whose index hospitalization was in December were excluded in order to allow for completeness of data on 30 days of follow-up after discharge, similarly to other prior studies examining the NRD [11,12,13].
2.3. Study Outcomes
The primary outcome of interest was 30-day readmission rates after index hospitalization for TTS. For 30-day readmissions, only the first readmission within 30 days of the discharge was included, and transfer to another hospital was not counted as a readmission. The primary cause of 30-day readmission was identified based on CCS code in the first diagnosis field of each readmission record and dichotomized into non-cardiac and cardiac causes [9]. Non-cardiac causes included respiratory, infectious, gastrointestinal, neuropsychiatric/substance, stroke/transient ischemic attack, endocrine/metabolic, genitourinary, hematologic/oncologic, peripheral vascular disease, trauma, complication of medical procedure, and other non-cardiac causes. Cardiac causes included angina and chronic ischemic heart disease, heart failure, acute myocardial infarction, nonspecific chest pain, arrhythmia, and other cardiac causes. Furthermore, 30-day mortality rates, along with breakdown of mortality rates during index hospitalization and during readmission, were identified. Finally, total cumulative hospital charges and costs for index hospitalization and readmissions were examined according to the presence of malignancy.
2.4. Statistical Analyses
All statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, NC, USA), and R statistical software, version 3.5.1 (www.R-project.org (accessed on 1 May 2021)), with its package “survey”. Discharge weight and stratum provided by NRD were used for all analyses and thus all of the reported numbers are weighted national estimates [14]. Domain analysis was used for accurate variance calculations for subgroup analyses [15]. All analyses accounted for NRD sampling design by including hospital-year fixed effects based on hospital identification number [8]. We compared baseline patient- and hospital-level characteristics with TTS, stratified by the presence of malignancy. Categorical variables are presented as frequencies and analyzed by the Rao-Scott chi-square test. Continuous variables are shown as mean or median and are tested by either the Mann-Whitney-Wilcoxon test or a survey-specific linear regression test. To evaluate the predictive value of malignancy and other covariates for primary and secondary outcomes, survey-specific univariate and multivariable generalized linear models were applied. Variables with p < 0.1 were included as initial covariates. Final parsimonious models were created by manual removal of each covariate, based on Akaike information criterion, while ensuring each removal did not result in >10% change in the measure of association for the primary predictor variable. Adjusted risks are presented in odds ratio (OR), together with 95% confidence interval (CI) and p value. The estimated cost for each hospitalization was calculated by the validated method of using cost-to-charge ratio provided by HCUP. The total cost was defined as the summation of the cost of readmission and the cost of the index admission. We examined the predictors of total cost by survey-specific multivariate linear regression test for log-transformed costs. All tests were two-sided with p value < 0.05 considered statistically significant.
3. Results
3.1. Baseline Characteristics
A total of 61,583 TTS admissions were included in the analysis, with 7542 patients (12.2%) with malignancy. The baseline patient-level and hospital-level characteristics, according to the presence of malignancy, are presented in Table 1. TTS patients with malignancy were more likely to be female and have a smoking history, known coronary artery disease, congestive heart failure, chronic pulmonary disease, anemia, atrial fibrillation, coagulopathy, fluid/electrolyte disorders, pulmonary circulatory disease and valvular heart disease. TTS with concomitant cardiogenic shock was observed more frequently among those with malignancy. In addition, TTS patients with malignancy were admitted more frequently to teaching hospitals and discharged to facilities more often (such as skilled nursing facility, intermediate care facility, and inpatient rehabilitation facility). There was no significant difference in the prevalence of psychiatric disorders, such as mood disorders, delirium/dementia, personality disorder between TTS patients with malignancy and those without malignancy.
Table 1.
Baseline characteristics of Takotsubo Syndrome Patients with or without Malignancy.
| Characteristics | ||||
|---|---|---|---|---|
| All | Malignancy | No Malignancy | p Value | |
| Number of admissions | 61,583 | 7542 (12.2) * | 54,041 (87.8) | |
| Patient characteristics | ||||
| Age, mean (SE), y | 66.7 (0.1) | 70.6 (0.2) | 66.1 (0.1) | <0.001 † |
| Age ≥ 70 yrs | 27,109 (44.0) | 4328 (57.4) | 22,781 (42.2) | <0.001 ‡ |
| Female | 54,708 (88.8) | 6499 (86.2) | 48,209 (89.2) | <0.001 |
| Smoking history | 21,834 (35.5) | 2864 (38.0) | 18,970 (35.1) | 0.005 |
| Hypertension | 40,597 (65.9) | 4900 (65.0) | 35,697 (66.1) | 0.350 |
| Diabetes mellitus | 11,701 (19.0) | 1405 (18.6) | 10,296 (19.1) | 0.620 |
| Dyslipidemia | 26,830 (43.6) | 3102 (41.1) | 23,728 (43.9) | 0.014 |
| Known coronary artery disease | 25,910 (42.1) | 3495 (46.3) | 22,415 (41.5) | <0.001 |
| Previous myocardial infarction | 3833 (6.2) | 444 (5.9) | 3389 (6.3) | 0.463 |
| Previous PCI | 2988 (4.9) | 341 (4.5) | 2647 (4.9) | 0.458 |
| Previous CABG | 933 (1.5) | 91 (1.2) | 842 (1.6) | 0.177 |
| Family history of coronary artery disease | 5249 (8.5) | 448 (5.9) | 4801 (8.9) | <0.001 |
| Congestive heart failure | 18,531 (30.1) | 2552 (33.8) | 15,979 (29.6) | <0.001 |
| Peripheral vascular disease | 4544 (7.4) | 608 (8.1) | 3936 (7.3) | 0.156 |
| Chronic pulmonary disease | 17,732 (28.8) | 2396 (31.8) | 15,336 (28.4) | <0.001 |
| Chronic kidney disease | 4862 (7.9) | 670 (8.9) | 4192 (7.8) | 0.075 |
| Liver disease | 1238 (2.0) | 116 (1.5) | 1122 (2.1) | 0.070 |
| Anemia | 9425 (15.3) | 1456 (19.3) | 7969 (14.7) | <0.001 |
| Atrial fibrillation | 8744 (14.2) | 1338 (17.7) | 7406 (13.7) | <0.001 |
| Coagulopathy | 2699 (4.4) | 485 (6.4) | 2214 (4.1) | <0.001 |
| Collagen vascular disease | 2683 (4.4) | 282 (3.7) | 2401 (4.4) | 0.117 |
| Fluid/electrolyte disorders | 18,576 (30.2) | 2658 (35.2) | 15,918 (29.5) | <0.001 |
| Obesity | 6554 (10.6) | 537 (7.1) | 6017 (11.1) | <0.001 |
| Other neurological disorders | 5196 (8.4) | 599 (7.9) | 4597 (8.5) | 0.429 |
| Pulmonary circulatory disease | 1243 (2.0) | 252 (3.3) | 991 (1.8) | <0.001 |
| Valvular heart disease | 1592 (2.6) | 296 (3.9) | 1296 (2.4) | <0.001 |
| Median household income | <0.001 | |||
| First quartile | 16,024 (26.4) | 1739 (23.3) | 14,285 (26.8) | |
| Second quartile | 15,865 (26.1) | 1957 (26.2) | 13,908 (26.1) | |
| Third quartile | 14,949 (24.6) | 1816 (24.3) | 13,133 (24.7) | |
| Fourth quartile | 13,849 (22.8) | 1953 (26.2) | 11,896 (22.4) | |
| Primary payer | <0.001 | |||
| Medicare | 37,851 (61.5) | 5462 (72.4) | 32,389 (59.9) | |
| Medicaid | 4028 (6.5) | 389 (5.2) | 3639 (6.7) | |
| Private including HMO | 15,388 (25.0) | 1435 (19.0) | 13,953 (25.8) | |
| Self-pay/no charge/other | 4315 (7.0) | 256 (3.4) | 4059 (7.5) | |
| Hospital characteristics | ||||
| Hospital teaching status | <0.001 | |||
| Teaching | 35,931 (58.3) | 4799 (63.6) | 31,132 (57.6) | |
| Nonteaching | 25,652 (41.7) | 2743 (36.4) | 22,909 (42.4) | |
| Hospital location | 0.149 | |||
| Rural | 212 (0.3) | 13 (0.2) | 199 (0.4) | |
| Urban | 61,371 (99.7) | 7529 (99.8) | 53,842 (99.6) | |
| Hospital bed size | 0.240 | |||
| Small | 4612 (7.5) | 503 (6.7) | 4109 (7.6) | |
| Medium | 13,769 (22.4) | 1643 (21.8) | 12,126 (22.4) | |
| Large | 43,203 (70.2) | 5396 (71.5) | 37,807 (70.0) | |
| Length of stay > 5 days | 18,588 (30.2 | 3134 (41.6) | 15,454(28.6) | <0.001 |
| Disposition | <0.001 | |||
| Home | 44,092 (71.6) | 4552 (60.4) | 39,540 (73.2) | |
| Facility § | 15,710 (25.5) | 2632 (34.9) | 13,078 (24.2) | |
| AMA/unknown | 1777 (2.9) | 358 (4.7) | 1419 (2.6) | |
| Mood disorders | 11,502 (18.7) | 11,354 (18.0) | 10,148 (18.8) | 0.378 |
| Substance abuse | 2676 (4.3) | 165 (2.2) | 2511 (4.6) | <0.001 |
| Delirium/Dementia | 2667 (4.3) | 365 (4.8) | 2302 (4.3) | 0.213 |
| Personality disorder | 103 (0.2) | 0 (0) | 103 (0.2) | 0.061 |
| Acute decompensated heart failure | 10,571 (17.2) | 1472 (19.5) | 9099 (16.8) | 0.003 |
| Cardiogenic shock | 3564 (5.8) | 582 (7.7) | 2982 (5.5) | <0.001 |
| Cardiac arrest | 1663 (2.7) | 221 (2.9) | 1442 (2.7) | 0.544 |
| Postop stroke (complication) | 792 (1.3) | 103 (1.4) | 689 (1.3) | 0.704 |
| Arrhythmia | 16,868 (27.4) | 2394 (31.7) | 14,474 (26.8) | <0.001 |
Abbreviations: SE, standard error; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; HMO, health maintenance organization; AMA, against medical advice. * Values are presented as number (percentage) of patients unless otherwise indicated. † Survey-specific linear regression was performed. ‡ Rao-Scott χ2 test was used for all statistical tests unless stated otherwise. § Facility includes skilled nursing facility, intermediate care facility, and inpatient rehabilitation facility.
3.2. Clinical Outcomes of TTS Patients with or without Malignancy
In-hospital mortality in TTS patients with malignancy was significantly higher by ~2-fold when compared to those without malignancy (4.2% vs. 2.1%, p < 0.001) (Table 2). There was more than a 90% increase in the 30-day total mortality rates in the malignancy group, which was mostly driven by mortality during index-hospitalization. Multivariate analysis, after adjusting for clinical and hospital characteristics, demonstrated a 68% increase in the risk of index-hospitalization mortality (OR, 1.68; 95% CI, 1.29–2.17; p < 0.01) and a 62% increase in the risk of 30-day total mortality (OR, 1.62; 95% CI, 1.25–2.10; p < 0.01) in TTS patients with vs. without malignancy (Table 2, Tables S1 and S2). There was no difference in 30-day readmission mortality between TTS patients with and without malignancy (0.6% vs. 0.4%, p = 0.110).
Table 2.
In-hospital and 30-day Outcomes of Takotsubo Syndrome.
| Unadjusted | Adjusted * | ||||
|---|---|---|---|---|---|
| Outcomes | N (%) | OR (95% CI) | p Value | OR (95% CI) | p Value |
| Number of patients | 7542 (12.2) | ||||
| Inhospital mortality | |||||
| Overall | 1472 (2.4) | ||||
| No malignancy | 1161 (2.1) | 1 (Ref) | 1 (Ref) | ||
| Malignancy | 311 (4.1) | 1.96 (1.56–2.46) | <0.001 | 1.68 (1.29–2.17) | <0.001 |
| 30-day readmission mortality | |||||
| Overall | 254 (0.4) | ||||
| No malignancy | 205 (0.4) | 1 (Ref) | |||
| Malignancy | 49 (0.6) | 1.73 (0.88–3.42) | 0.114 | - | |
| 30-day total mortality † | |||||
| Overall | 1726 (2.8) | ||||
| No malignancy | 1366 (2.5) | 1 (Ref) | 1 (Ref) | ||
| Malignancy | 360 (4.8) | 1.96 (1.56–2.46) | <0.001 | 1.62 (1.25–2.10) | <0.001 |
| 30-day readmission | |||||
| Overall | 7173 (11.6) | ||||
| No malignancy | 5971 (11.0) | 1 (Ref) | 1 (Ref) | ||
| Malignancy | 1202 (15.9) | 1.53 (1.34–1.75) | <0.001 | 1.33 (1.15–1.53) | <0.001 |
Abbreviations: OR, odds ratio; CI, confidence interval; Ref, reference. * Survey-specific multivariate generalized linear model was created with each outcome including all predictors with p values < 0.1 in the univariate analysis. Covariates for in-hospital mortality and 30-day total mortality are available in the Tables S1 and S2. † Thirty-day total mortality included in-hospital mortality and 30-day readmission mortality together.
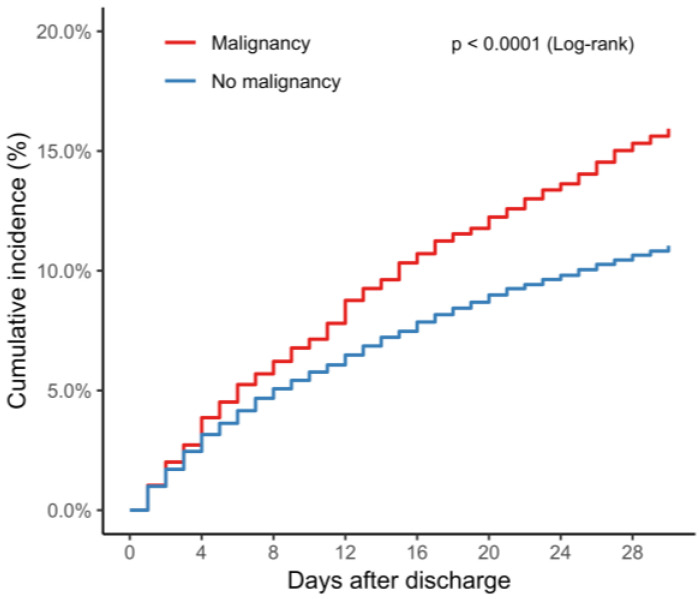
The 30-day readmission rate was significantly higher in TTS patients with malignancy than those without malignancy (15.9% vs. 11.0%, p < 0.001) (Figure 1). After adjusting for clinical and hospital characteristics, there was a 33% increase in the risk of 30-day readmission in TTS patients with malignancy (OR, 1.33; 95% CI, 1.15–1.53; p < 0.01) (Table 3). Other significant predictors for 30-day readmission included a longer (>5 days) length of stay during index admission, chronic pulmonary disease, chronic kidney disease, anemia, atrial fibrillation, fluid/electrolyte disturbance, diabetes mellitus, low household income, and disposition to facility (Table 3).
Figure 1.
Cumulative rates of 30-day readmissions according to the presence of malignancy. Data show unadjusted 30-day readmission rate in TTS patients with malignancy (red) and in those without malignancy (blue). Abbreviations: TTS, Takotsubo syndrome.
Table 3.
Independent Predictors of 30-Day Readmission After Index Hospitalization with Takotsubo Syndrome.
| Variables | Unadjusted OR | Lower CI | Higher CI | p Value | Adjusted OR * | Lower CI | Higher CI | p Value |
|---|---|---|---|---|---|---|---|---|
| Malignancy | 1.53 | 1.34 | 1.75 | <0.001 | 1.33 | 1.15 | 1.53 | <0.001 |
| Length of stay > 5 days | 2.45 | 2.23 | 2.69 | <0.001 | 1.48 | 1.31 | 1.68 | <0.001 |
| Age ≥ 70 yrs | 1.34 | 1.22 | 1.46 | <0.001 | 0.95 | 0.84 | 1.07 | 0.378 |
| Diabetes mellitus | 1.27 | 1.13 | 1.42 | <0.001 | 1.14 | 1.01 | 1.28 | 0.035 |
| Family hx of CAD | 0.56 | 0.46 | 0.69 | <0.001 | 0.78 | 0.63 | 0.97 | 0.024 |
| Chronic pulmonary disease | 1.69 | 1.54 | 1.86 | <0.001 | 1.40 | 1.27 | 1.55 | <0.001 |
| Chronic Kidney disease | 1.88 | 1.64 | 2.16 | <0.001 | 1.36 | 1.17 | 1.59 | <0.001 |
| Anemia | 1.90 | 1.70 | 2.12 | <0.001 | 1.26 | 1.12 | 1.42 | <0.001 |
| Atrial fibrillation | 1.61 | 1.43 | 1.81 | <0.001 | 1.24 | 1.08 | 1.41 | 0.002 |
| Fluid and electrolyte disturbance | 1.75 | 1.58 | 1.92 | <0.001 | 1.20 | 1.07 | 1.34 | 0.001 |
| Median household income (Ref: 1st quartile) | ||||||||
| Second quartile | 0.92 | 0.80 | 1.04 | 0.188 | 0.97 | 0.85 | 1.11 | 0.689 |
| Third quartile | 0.83 | 0.72 | 0.94 | 0.004 | 0.90 | 0.79 | 1.03 | 0.10 |
| Fourth quartile | 0.75 | 0.66 | 0.85 | <0.001 | 0.85 | 0.74 | 0.97 | 0.01 |
| Primary payer (Ref: Medicare) | ||||||||
| Medicaid | 1.11 | 0.93 | 1.31 | 0.250 | 1.25 | 1.02 | 1.53 | 0.032 |
| Private including HMO | 0.53 | 0.46 | 0.60 | <0.001 | 0.75 | 0.64 | 0.88 | <0.001 |
| Self-pay/no charge/other | 0.61 | 0.50 | 0.74 | <0.001 | 0.82 | 0.66 | 1.00 | 0.054 |
| Disposition (Ref: Home) | ||||||||
| Facility | 2.60 | 2.35 | 2.87 | <0.001 | 1.65 | 1.46 | 1.87 | <0.001 |
| AMA/unknown | 0.37 | 0.22 | 0.62 | <0.001 | 0.25 | 0.15 | 0.41 | <0.001 |
Abbreviations: OR, odds ratio; CI, confidence interval; CAD, coronary artery disease; HMO, health maintenance organization; AMA, against medical advice. * A survey-specific multivariate generalized linear model was created with an outcome of 30-day readmission including all predictors with p values < 0.1 in the univariate analysis. Covariates for in hospital mortality and 30-day total mortality are available in the Tables S1 and S2.
3.3. Timing and Cause of Readmission
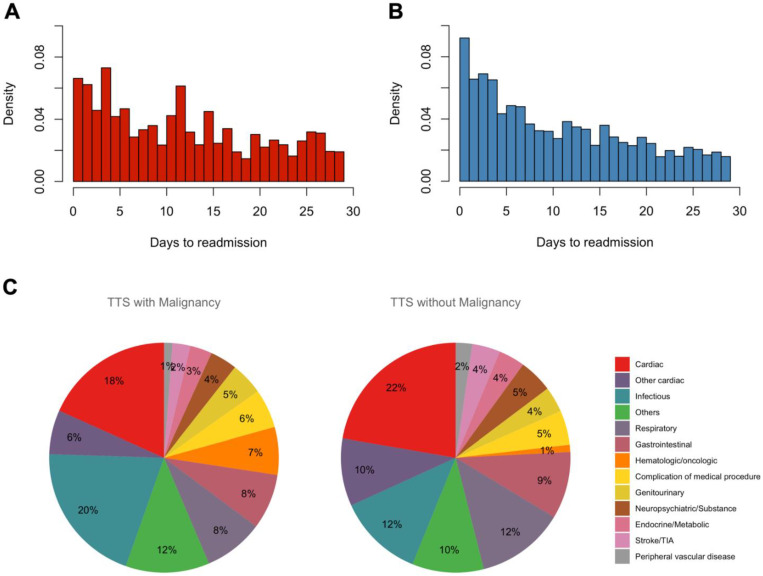
Figure 2 and Figure S1 demonstrate the timing of a 30-day readmission stratified by the presence of malignancy. The median time to readmission was longer in TTS patients with malignancy vs. without malignancy (12 days, interquartile range (IQR) 5–19 days vs. 9 days, IQR 4–17 days, respectively; p = 0.027). A sum of 34% of TTS patients with malignancy and 43% without malignancy were readmitted within 7 days of discharge. A sum of 38% of TTS patients with malignancy and 33% without malignancy were readmitted after 14 days of discharge. Non-cardiac causes were more common causes of readmission for TTS patients with malignancy versus without malignancy (75.5% vs. 68.1%, p < 0.001) (Figure 2C, Tables S3–S5). Among cardiac causes, heart failure was the most prevalent in both TTS patients with and without malignancy (8.1% vs. 11.1%, p = 0.002), followed by arrhythmia (4.9% vs. 3.3%, p = 0.006, and angina (1.8% vs. 2.4%, p = 0.234). Among non-cardiac causes, infectious (20.1% vs. 12.0%, p = <0.001), respiratory (8.4% vs. 12.4%, p < 0.001), and gastrointestinal (7.8% vs. 9.5%, p = 0.075) causes were most prevalent in both groups. The 30-day readmission rate due to recurrent TTS was similarly low in both groups (0.4% vs. 0.5%, respectively; p = 0.47).
Figure 2.
Timing and Causes of 30-day Readmissions for Takotsubo Syndrome with or without malignancy. (A) Time to readmission in TTS patients with malignancy. (B) Time to readmission in TTS patients without malignancy. (C) Histograms representing different causes of 30-day readmissions in TTS patients with malignancy and without malignancy. Abbreviations: TTS, Takotsubo syndrome.
3.4. Specific Cancer Type and Readmission
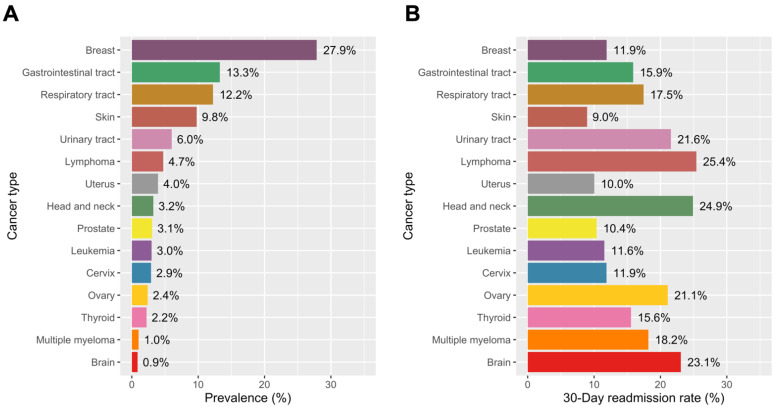
The prevalence of specific cancer types is shown in Figure 3A. The most frequent type of malignancy was breast cancer (27.9%), followed by gastrointestinal tract cancer (13.3%) and respiratory tract cancer (12.2%). The 30-day readmission rate was the highest in patients with lymphoma (25.4%), head and neck cancer (24.9%), brain cancer (23.1%), urinary tract cancer (21.6%), and ovarian cancer (21.1%) (Figure 3B). TTS patients with skin (9.0%), uterus (10.0%), and prostate (10.4%) cancer had the lowest 30-day readmission rates compared to patients with other cancer.
Figure 3.
Thirty-day Readmission Rates of Takotsubo Syndrome by Cancer Types. (A) Prevalence of each type of cancer in TTS patients with malignancy. (B) 30-day readmission rates according to the cancer type in TTS patients with malignancy. Abbreviations: TTS, Takotsubo syndrome.
3.5. Total Charges and Costs by the Presence of Malignancy and Predictors of Total Cost
Hospital charges and costs over 30 days after index hospitalization for TTS stratified by the presence of malignancy are shown in Table S6. The median total charge (index hospitalization + readmissions) was $10,201 higher in TTS patients with malignancy ($50,936; IQR, $29,819–$97,989) than in those without malignancy ($40,735; IQR, $26,160–$72,619) (p < 0.001). The median total cost (index hospitalization + readmissions) was $2982 higher in TTS patients with malignancy ($14,686; IQR, $9294–$27,337) than in those without malignancy ($11,704; IQR, $8065–$19,630) (p < 0.001). After multivariate adjustment, 30-day readmission was independently associated with a 22.3% increase in the 30-day total cost (Table 4). Furthermore, the presence of malignancy was independently associated with a 1.3% increase in the 30-day total cost. Other significant predictors for the increased total costs included length of stay > 5 days, cardiogenic shock, and cardiac arrest.
Table 4.
Independent Predictors of Higher 30-Day Total Cost of Hospitalization in Patients with Takotsubo syndrome.
| Unadjusted | Adjusted * | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Beta | Lower CI | Higher CI | p Value | Beta | Lower CI | Higher CI | p Value |
| Malignancy | 0.093 | 0.078 | 0.108 | <0.001 | 0.013 | 0.005 | 0.022 | 0.003 |
| 30-day readmission | 0.327 | 0.312 | 0.341 | <0.001 | 0.223 | 0.212 | 0.234 | <0.001 |
| Length of stay > 5 days | 0.459 | 0.449 | 0.469 | <0.001 | 0.31 | 0.301 | 0.318 | <0.001 |
| Age ≥ 70 yrs | 0.033 | 0.023 | 0.042 | <0.001 | −0.026 | −0.033 | −0.018 | <0.001 |
| Female (Ref: male) | −0.109 | −0.130 | −0.089 | <0.001 | −0.048 | −0.061 | −0.036 | <0.001 |
| Diabetes mellitus | 0.041 | 0.029 | 0.052 | <0.001 | 0.015 | 0.007 | 0.022 | <0.001 |
| Dyslipidemia | −0.070 | −0.080 | −0.061 | <0.001 | −0.014 | −0.02 | −0.008 | <0.001 |
| Previous PCI | −0.024 | −0.043 | −0.005 | 0.015 | −0.02 | −0.034 | −0.006 | 0.005 |
| Family history of CAD | −0.125 | −0.138 | −0.112 | <0.001 | −0.013 | −0.024 | −0.003 | 0.009 |
| Congestive heart failure | 0.184 | 0.173 | 0.194 | <0.001 | 0.027 | 0.019 | 0.034 | <0.001 |
| Peripheral vascular disease | 0.121 | 0.102 | 0..139 | <0.001 | 0.028 | 0.016 | 0.04 | <0.001 |
| Chronic pulmonary disease | 0.107 | 0.096 | 0.118 | <0.001 | 0.019 | 0.012 | 0.026 | <0.001 |
| Chronic kidney disease | 0.169 | 0.150 | 0.188 | <0.001 | 0.03 | 0.017 | 0.044 | <0.001 |
| Chronic liver disease | 0.200 | 0.157 | 0.242 | <0.001 | 0.04 | 0.012 | 0.068 | 0.005 |
| Anemia | 0.217 | 0.203 | 0.231 | <0.001 | 0.031 | 0.022 | 0.041 | <0.001 |
| Atrial fibrillation | 0.140 | 0.124 | 0.156 | <0.001 | 0.018 | 0.008 | 0.028 | <0.001 |
| Coagulopathy | 0.339 | 0.309 | 0.368 | <0.001 | 0.097 | 0.078 | 0.115 | <0.001 |
| Drug abuse | 0.114 | 0.089 | 0.140 | <0.001 | 0.027 | 0.01 | 0.043 | 0.001 |
| Fluid/electrolyte disorders | 0.257 | 0.246 | 0.269 | <0.001 | 0.059 | 0.051 | 0.068 | <0.001 |
| Other neurological disorders | 0.132 | 0.112 | 0.152 | <0.001 | 0.027 | 0.014 | 0.04 | <0.001 |
| Pulmonary circulatory disease | 0.407 | 0.369 | 0.444 | <0.001 | 0.096 | 0.065 | 0.127 | <0.001 |
| Valvular heart disease | 0.323 | 0.293 | 0.353 | <0.001 | 0.06 | 0.038 | 0.083 | <0.001 |
| Cardiogenic shock | 0.418 | 0.396 | 0.440 | <0.001 | 0.122 | 0.102 | 0.142 | <0.001 |
| Cardiac arrest | 0.403 | 0.372 | 0.434 | <0.001 | 0.147 | 0.122 | 0.173 | <0.001 |
| Intraaortic balloon pump | 0.415 | 0.383 | 0.448 | <0.001 | 0.086 | 0.058 | 0.114 | <0.001 |
| Median household income (Ref: first quartile) | ||||||||
| Second quartile | 0.007 | −0.008 | 0.023 | 0.339 | 0.027 | 0.018 | 0.036 | <0.001 |
| Third quartile | 0.025 | 0.010 | 0.040 | 0.001 | 0.051 | 0.042 | 0.061 | <0.001 |
| Fourth quartile | 0.037 | 0.022 | 0.053 | <0.001 | 0.077 | 0.067 | 0.088 | <0.001 |
| Primary payer (Ref: medicare) | ||||||||
| Medicaid | 0.041 | 0.020 | 0.062 | <0.001 | 0.033 | 0.019 | 0.047 | <0.001 |
| Private | −0.083 | −0.094 | −0.072 | <0.001 | −0.003 | −0.011 | 0.006 | 0.506 |
| Self-pay/no charge/others | −0.069 | −0.087 | −0.050 | <0.001 | −0.001 | −0.014 | 0.012 | 0.897 |
| Disposition (Ref: home) | ||||||||
| Facility | 0.316 | 0.304 | 0.327 | <0.001 | 0.077 | 0.069 | 0.086 | <0.001 |
| AMA/unknown | 0.346 | 0.311 | 0.380 | <0.001 | 0.116 | 0.091 | 0.141 | <0.001 |
| Year (per year) | 0.009 | 0.004 | 0.014 | <0.001 | 0.006 | −0.000 | 0.011 | 0.060 |
Abbreviations: TTS, Takotsubo syndrome; PCI, percutaneous coronary intervention; CAD, coronary artery disease. * A survey-specific multivariate linear regression model was created with an outcome of log-transformed cumulative cost including all predictors with p values < 0.1 in the univariate analysis. Hospital ID was also included as a covariable for consideration of hospital fixed-year effect (insignificant contribution, not shown).
4. Discussion
Using the NRD between 2010 and 2014 to delineate 30-day clinical outcomes in patients hospitalized for TTS with or without malignancy, we identified several key findings. First, there was a high prevalence of malignancy (12.2%) among TTS patients. Second, 30-day readmission rates, all-cause mortality, and total costs (index hospitalization + readmissions) were higher in TTS patients with malignancy compared to those without malignancy. Third, malignancy was independently associated with an increase in 30-day total charges and costs in patients hospitalized for TTS. The implications of these findings underscore the importance of optimal treatment strategy and close follow-up in patients with TTS and malignancy.
The 30-day readmission rate of TTS patients was 11.6%, similar to previous reports [7,16]. Our study demonstrates that malignancy is associated with a significant risk of readmission after index hospitalization for TTS. It is noteworthy that the median time to readmission is longer in TTS patients with malignancy (12 days) than in those without malignancy (9 days). A significant portion (34%) of TTS patients with malignancy were readmitted >14 days after discharge. These findings highlight the need for optimal initial treatment strategy and vigilant attention beyond the initial 1–2 weeks follow-up visit, especially for patients with malignancy. Our study demonstrates that heart failure is the most common cardiac cause of readmission, which is unsurprising given the pathophysiology and clinical manifestation of TTS. Therefore, treatment strategies to optimize heart failure regimen and to minimize readmission after TTS are warranted [17]. Supportive discharge interventions, such as telephone-facilitated post-discharge support program, computer-based education sessions, or nurse-driven protocol-based management program, have shown to be effective in reducing the risk of early readmissions in the heart failure population [18,19,20,21,22]. Furthermore, developing comprehensive programs for heart failure patients with patient-specific interventions based on risk profile and focus on both inpatient and outpatient interventions with cross-site communications have shown to significantly reduce early readmissions [23]. However, efforts in reducing 30-day readmissions after TTS should also consider the fact that the majority of readmissions are due to non-cardiac causes. TTS is a complex disorder with variable clinical manifestations, and malignancy certainly presents an added layer of complexity to the management of TTS. Infectious etiologies were the most frequent cause of readmission among TTS patients with malignancy in our study. Patients with malignancy are at increased risk of infections directly related to their cancer or due to their immunocompromised state from systemic chemotherapy [24]. Interdisciplinary approaches in coordinating outpatient programs focused on reducing readmissions by providing a continuity of care in the inpatient and outpatient setting by both oncologists and cardiologists should be encouraged.
In the present study, the presence of malignancy is not associated with an increased risk in 30-day readmission from recurrent TTS. Reported recurrence rates of TTS are variable, ranging from 1% to 11.4% [25,26,27]. Analysis of the multicenter GEIST (German Italian Stress Cardiomyopathy) Registry data failed to identify any independent predictors of TTS recurrence [28]. The presence of malignancy has been shown to be associated with a higher risk of TTS in numerous studies [29,30,31], and there are numerous reports of TTS associated with chemotherapy or immunotherapy [32,33,34,35,36]. It is plausible that interruption in chemotherapy after initial episode of TTS may play a role in explaining the lack of difference in TTS recurrence rate in those with malignancy. Post-TTS cancer treatment strategy, especially decisions regarding continuation of potentially life-saving chemotherapy, still remains a challenge. Future, longer-term studies are necessary to detect whether TTS patients with malignancy are at risk of developing recurrent TTS.
Our study demonstrated that malignancy was associated with ~70% increase in in-hospital mortality risk during index hospitalization and ~60% increase in overall 30-day mortality risk in patients with TTS. A previous study from National Inpatient Sample 2007 to 2013 showed that solid cancer was associated with 3.4 times increase in in-hospital mortality among TTS patients [37]. Our analysis included all types of cancer (solid or hematologic cancer), which may explain slightly lower in-hospital mortality. Recent data from the International Takotsubo Registry have shown that long-term mortality increased in TTS patients with malignancy while 30-day mortality was not significantly different in TTS patients (n = 1604) with or without malignancy (7% vs. 4%, p = 0.17) [29]. Our larger administrative data (n = 61,583), however, demonstrates that total 30-day mortality rates in TTS patients with malignancy were significantly higher compared to those without malignancy. This result requires a cautious interpretation since the NRD does not include out-of-hospital mortality data. Further studies with a more extensive examination of out-of-hospital mortality are needed to examine this discrepancy.
Cost analysis of our study demonstrates that TTS is responsible for annual cost of ~$148 million for index admission and 30-day readmission in the US (during the years from 2010 to 2014). Readmission within 30-days accounted for 22% increase in the total costs among TTS patients. Furthermore, the presence of malignancy increased the cumulative costs by 1.3% after index hospitalization for TTS. Although 30-day readmission is one of the most significant contributors to an increased overall cost, the presence of malignancy was an independent predictor of increased cost, likely due to longer length of stay and higher frequency of cardiogenic shock. Our findings highlight the impact of TTS in patients with malignancy beyond just short- and long-term mortality. TTS in patients with malignancy pose a significant economic burden on hospital resources and the overall healthcare system, and our study supports the need for increased effort in reducing readmissions in this cohort.
This study has limitations that are largely due to its observational nature. Firstly, the NRD is the administrative data, designed to estimate the national distribution of representative hospital characteristics, which is subject to coding bias or missing variables. Nevertheless, there have been numerous publications which have validated the sampling design of NRD and the utilization of NRD databases for risk-adjusted outcome evaluation [11,16,38]. Secondly, the NRD does not include detailed clinical characteristics, such as coronary anatomy, heart failure class, left ventricular ejection fraction, cardiac enzyme data or medications. Thirdly, our analysis of the 30-day total mortality rate does not include out-of-hospital deaths, which may underestimate the overall incidence of mortality. Fourthly, we used ICD-9-CM codes and CCS codes for defining clinical diagnoses and procedures, which may lead to a misclassification bias. Finally, the result from the overall malignant population may not be generalizable to specific cancer types, stages, or treatment strategies. Nevertheless, the prevalence and 30-day readmission rates according to cancer types were addressed throughout this study.
In summary, malignancy is associated with an increased risk of 30-day readmission, all-cause mortality, and costs in TTS patients. The majority of hospital readmissions in TTS patients were caused by non-cardiac causes. Our findings highlight the importance of tailored and multidisciplinary patient-specific treatment approaches, along with careful coordination of outpatient follow-up care, particularly in TTS patients with malignancy.
Acknowledgments
We thanks to members of Weill Cornell Cardiovascular Outcomes Research Group (CORG) and house staffs of Yale New Haven Health Bridgeport Hospital for their stimulating discussion and supports.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm10163701/s1, Figure S1: Cumulative Density Function for Readmissions within 30 Days in Takotsubo syndrome, Table S1: Independent Predictors of In-hospital Mortality After Index Hospitalization With Takotsubo Syndrome, Table S2: Independent Predictors of 30-Day Total Mortality After Index Hospitalization With Takotsubo Syndrome, Table S3: Causes of Readmission in all Takotsubo Syndrome Patients, Table S4: Causes of Readmission in Takotsubo Syndrome Patients With Malignancy, Table S5: Causes of Readmission in Takotsubo Syndrome Patients Without Malignancy, Table S6: Costs and Charges over 30 Days After Index Hospitalization for Takotsubo syndrome With or Without Malignancy.
Author Contributions
S.-J.J., I.Y. and L.K.K. collected data from the Nationwide Readmission Database regarding the Takotsubo syndrome and cancer and performed statistical analysis. S.-J.J., C.J. and L.K.K. were a major contributor in writing the manuscript. P.G., J.W.C., D.N.F., S.A.M., U.K., D.L.N., H.S.S., R.M.M., G.B. and S.C.W. contributed to clinical and statistical discussion on the results providing constructive suggestions. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by grants from the Michael Wolk Heart Foundation, the New York Cardiac Center, Inc. (MWHFI 17081089-01), and the Weill Cornell Medical Center Alumni Council. The Michael Wolk Heart Foundation, the New York Cardiac Center, Inc., and the Weill Cornell Medical Center Alumni Council had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Institutional Review Board Statement
Ethical review and approval were waived for this study because all data collection was derived from a publicly open and deidentified administrative database.
Informed Consent Statement
Patient consent was waived because all data collection was derived from a publicly open and deidentified administrative database.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. Original United States Nationwide Readmissions Database used for this study is available at https://www.hcup-us.ahrq.gov/db/nation/nrd/nrddbdocumentation.jsp (accessed on 1 May 2021).
Conflicts of Interest
There is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Akashi Y.J., Goldstein D.S., Barbaro G., Ueyama T. Takotsubo cardiomyopathy: A new form of acute, reversible heart failure. Circulation. 2008;118:2754–2762. doi: 10.1161/CIRCULATIONAHA.108.767012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ghadri J.R., Wittstein I.S., Prasad A., Sharkey S., Dote K., Akashi Y.J., Cammann V.L., Crea F., Galiuto L., Desmet W., et al. International expert consensus document on takotsubo syndrome (part i): Clinical characteristics, diagnostic criteria, and pathophysiology. Eur. Heart J. 2018;39:2032–2046. doi: 10.1093/eurheartj/ehy076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghadri J.R., Ruschitzka F., Luscher T.F., Templin C. Takotsubo cardiomyopathy: Still much more to learn. Heart. 2014;100:1804–1812. doi: 10.1136/heartjnl-2013-304691. [DOI] [PubMed] [Google Scholar]
- 4.Templin C., Ghadri J.R., Diekmann J., Napp L.C., Bataiosu D.R., Jaguszewski M., Cammann V.L., Sarcon A., Geyer V., Neumann C.A., et al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N. Engl. J. Med. 2015;373:929–938. doi: 10.1056/NEJMoa1406761. [DOI] [PubMed] [Google Scholar]
- 5.Ghadri J.R., Kato K., Cammann V.L., Gili S., Jurisic S., Di Vece D., Candreva A., Ding K.J., Micek J., Szawan K.A., et al. Long-term prognosis of patients with takotsubo syndrome. J. Am. Coll. Cardiol. 2018;72:874–882. doi: 10.1016/j.jacc.2018.06.016. [DOI] [PubMed] [Google Scholar]
- 6.Fingar K., Washington R. Trends in Hospital Readmissions for Four High-Volume Conditions, 2009–2013. HCUP Statistical Brief # 196. Published November 2015. [(accessed on 11 September 2019)]; Available online: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb196-Readmissions-Trends-High-Volume-Conditions.pdf.
- 7.Smilowitz N.R., Hausvater A., Reynolds H.R. Hospital readmission following takotsubo syndrome. Eur. Heart J. Qual Care Clin. Outcomes. 2019;5:114–120. doi: 10.1093/ehjqcco/qcy045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McIntyre E., Saliba A., McKenzie K. Subjective wellbeing in the Indian general population: A validation study of the personal wellbeing index. Qual Life Res. 2020;29:1073–1081. doi: 10.1007/s11136-019-02375-7. [DOI] [PubMed] [Google Scholar]
- 9.Agency for Healthcare Research and Quality Overview of hospital stays in the United States. [(accessed on 1 May 2021)];2012 Available online: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb180-Hospitalizations-United-States-2012.pdf. [PubMed]
- 10.Rivera D.R., Gallicchio L., Brown J., Liu B., Kyriacou D.N., Shelburne N. Trends in adult cancer-related emergency department utilization: An analysis of data from the nationwide emergency department sample. JAMA Oncol. 2017;3:e172450. doi: 10.1001/jamaoncol.2017.2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim L.K., Yeo I., Cheung J.W., Swaminathan R.V., Wong S.C., Charitakis K., Adejumo O., Chae J., Minutello R.M., Bergman G., et al. Thirty-Day readmission rates, timing, causes, and costs after st-segment-elevation myocardial infarction in the United States: A national readmission database analysis 2010-2014. J. Am. Heart Assoc. 2018;7:e009863. doi: 10.1161/JAHA.118.009863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng E.P., Liu C.F., Yeo I., Markowitz S.M., Thomas G., Ip J.E., Kim L.K., Lerman B.B., Cheung J.W. Risk of mortality following catheter ablation of atrial fibrillation. J. Am. Coll. Cardiol. 2019;74:2254–2264. doi: 10.1016/j.jacc.2019.08.1036. [DOI] [PubMed] [Google Scholar]
- 13.Cheung J.W., Cheng E.P., Wu X., Yeo I., Christos P.J., Kamel H., Markowitz S.M., Liu C.F., Thomas G., Ip J.E., et al. Sex-based differences in outcomes, 30-day readmissions, and costs following catheter ablation of atrial fibrillation: The United States Nationwide Readmissions Database 2010-14. Eur. Heart J. 2019;40:3035–3043. doi: 10.1093/eurheartj/ehz151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agency for Healthcare Research and Quality Introduction to the HCUP Nationwide Readmissions Database (NRD) [(accessed on 1 September 2019)]; Available online: https://www.hcupus.ahrq.gov/db/nation/nrd/Introduction_NRD_2010-2014.pdf.
- 15.Lohr S.L. Sampling: Design and Analysis. Duxbury Press; Pacific Grove, CA, USA: 1999. [Google Scholar]
- 16.Shah M., Ram P., Lo K.B.U., Sirinvaravong N., Patel B., Tripathi B., Patil S., Figueredo V.M. Etiologies, predictors, and economic impact of readmission within 1 month among patients with takotsubo cardiomyopathy. Clin. Cardiol. 2018;41:916–923. doi: 10.1002/clc.22974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arora S., Patel P., Lahewala S., Patel N., Patel N.J., Thakore K., Amin A., Tripathi B., Kumar V., Shah H., et al. Etiologies, trends, and predictors of 30-day readmission in patients with heart failure. Am. J. Cardiol. 2017;119:760–769. doi: 10.1016/j.amjcard.2016.11.022. [DOI] [PubMed] [Google Scholar]
- 18.Leppin A.L., Gionfriddo M.R., Kessler M., Brito J.P., Mair F.S., Gallacher K., Wang Z., Erwin P.J., Sylvester T., Boehmer K., et al. Preventing 30-day hospital readmissions: A systematic review and meta-analysis of randomized trials. JAMA Intern. Med. 2014;174:1095–1107. doi: 10.1001/jamainternmed.2014.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stromberg A., Martensson J., Fridlund B., Levin L.A., Karlsson J.E., Dahlstrom U. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure: Results from a prospective, randomised trial. Eur. Heart J. 2003;24:1014–1023. doi: 10.1016/S0195-668X(03)00112-X. [DOI] [PubMed] [Google Scholar]
- 20.Wakefield B.J., Ward M.M., Holman J.E., Ray A., Scherubel M., Burns T.L., Kienzle M.G., Rosenthal G.E. Evaluation of home telehealth following hospitalization for heart failure: A randomized trial. Telemed J. E Health. 2008;14:753–761. doi: 10.1089/tmj.2007.0131. [DOI] [PubMed] [Google Scholar]
- 21.Linne A.B., Liedholm H. Effects of an interactive CD-program on 6 months readmission rate in patients with heart failure—A randomised, controlled trial [ NCT00311194] BMC Cardiovasc. Disord. 2006;6:30. doi: 10.1186/1471-2261-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rich M.W., Beckham V., Wittenberg C., Leven C.L., Freedland K.E., Carney R.M. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N. Engl. J. Med. 1995;333:1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 23.Coleman E.A., Parry C., Chalmers S., Min S.J. The care transitions intervention: Results of a randomized controlled trial. Arch. Intern. Med. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 24.Vento S., Cainelli F. Infections in patients with cancer undergoing chemotherapy: Aetiology, prevention, and treatment. Lancet Oncol. 2003;4:595–604. doi: 10.1016/S1470-2045(03)01218-X. [DOI] [PubMed] [Google Scholar]
- 25.Elesber A.A., Prasad A., Lennon R.J., Wright R.S., Lerman A., Rihal C.S. Four-year recurrence rate and prognosis of the apical ballooning syndrome. J. Am. Coll. Cardiol. 2007;50:448–452. doi: 10.1016/j.jacc.2007.03.050. [DOI] [PubMed] [Google Scholar]
- 26.Singh K., Carson K., Usmani Z., Sawhney G., Shah R., Horowitz J. Systematic review and meta-analysis of incidence and correlates of recurrence of takotsubo cardiomyopathy. Int. J. Cardiol. 2014;174:696–701. doi: 10.1016/j.ijcard.2014.04.221. [DOI] [PubMed] [Google Scholar]
- 27.Gianni M., Dentali F., Grandi A.M., Sumner G., Hiralal R., Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: A systematic review. Eur. Heart J. 2006;27:1523–1529. doi: 10.1093/eurheartj/ehl032. [DOI] [PubMed] [Google Scholar]
- 28.El-Battrawy I., Santoro F., Stiermaier T., Moller C., Guastafierro F., Novo G., Novo S., Mariano E., Romeo F., Romeo F., et al. Incidence and clinical impact of recurrent takotsubo syndrome: Results from the GEIST registry. J. Am. Heart Assoc. 2019;8:e010753. doi: 10.1161/JAHA.118.010753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cammann V.L., Sarcon A., Ding K.J., Seifert B., Kato K., Di Vece D., Szawan K.A., Gili S., Jurisic S., Bacchi B., et al. Clinical features and outcomes of patients with malignancy and takotsubo syndrome: Observations from the international takotsubo registry. J. Am. Heart Assoc. 2019;8:e010881. doi: 10.1161/JAHA.118.010881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Desai A., Noor A., Joshi S., Kim A.S. Takotsubo cardiomyopathy in cancer patients. Cardiooncology. 2019;5:7. doi: 10.1186/s40959-019-0042-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tornvall P., Collste O., Ehrenborg E., Jarnbert-Petterson H. A case-control study of risk markers and mortality in takotsubo stress cardiomyopathy. J. Am. Coll. Cardiol. 2016;67:1931–1936. doi: 10.1016/j.jacc.2016.02.029. [DOI] [PubMed] [Google Scholar]
- 32.Curigliano G., Cardinale D., Dent S., Criscitiello C., Aseyev O., Lenihan D., Cipolla C.M. Cardiotoxicity of anticancer treatments: Epidemiology, detection, and management. CA Cancer J. Clin. 2016;66:309–325. doi: 10.3322/caac.21341. [DOI] [PubMed] [Google Scholar]
- 33.Ewer M.S., Ewer S.M. Cardiotoxicity of anticancer treatments. Nat. Rev. Cardiol. 2015;12:620. doi: 10.1038/nrcardio.2015.133. [DOI] [PubMed] [Google Scholar]
- 34.Desai R., Abbas S.A., Goyal H., Durairaj A., Fong H.K., Hung O., Sachdeva R., Barac A., Yusuf S.W., Kumar G. Frequency of takotsubo cardiomyopathy in adult patients receiving chemotherapy (from a 5-year nationwide inpatient study) Am. J. Cardiol. 2019;123:667–673. doi: 10.1016/j.amjcard.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 35.Ederhy S., Cautela J., Ancedy Y., Escudier M., Thuny F., Cohen A. Takotsubo-like syndrome in cancer patients treated with immune checkpoint inhibitors. JACC Cardiovasc. Imaging. 2018;11:1187–1190. doi: 10.1016/j.jcmg.2017.11.036. [DOI] [PubMed] [Google Scholar]
- 36.Anderson R.D., Brooks M. Apical takotsubo syndrome in a patient with metastatic breast carcinoma on novel immunotherapy. Int. J. Cardiol. 2016;222:760–761. doi: 10.1016/j.ijcard.2016.07.291. [DOI] [PubMed] [Google Scholar]
- 37.Joy P.S., Guddati A.K., Shapira I. Outcomes of takotsubo cardiomyopathy in hospitalized cancer patients. J. Cancer Res. Clin. Oncol. 2018;144:1539–1545. doi: 10.1007/s00432-018-2661-1. [DOI] [PubMed] [Google Scholar]
- 38.Dharmarajan K., Wang Y., Lin Z., Normand S.T., Ross J.S., Horwitz L.I., Desai N.R., Suter L.G., Drye E.E., Bernheim S.M., et al. Association of changing hospital readmission rates with mortality rates after hospital discharge. JAMA. 2017;318:270–278. doi: 10.1001/jama.2017.8444. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author. Original United States Nationwide Readmissions Database used for this study is available at https://www.hcup-us.ahrq.gov/db/nation/nrd/nrddbdocumentation.jsp (accessed on 1 May 2021).