Abstract
Background: Cardiology divisions reshaped their activities during the coronavirus disease 2019 (COVID-19) pandemic. This study aimed to analyze the organization of echocardiographic laboratories and echocardiography practice during the second wave of the COVID-19 pandemic in Italy, and the expectations for the post-COVID era. Methods: We analyzed two different time periods: the month of November during the second wave of the COVID-19 pandemic (2020) and the identical month during 2019 (November 2019). Results: During the second wave of the COVID-19 pandemic, the hospital activity was partially reduced in 42 (60%) and wholly interrupted in 3 (4%) echocardiographic laboratories, whereas outpatient echocardiographic activity was partially reduced in 41 (59%) and completely interrupted in 7 (10%) laboratories. We observed an important change in the organization of activities in the echocardiography laboratory which reduced the operator-risk and improved self-protection of operators by using appropriate personal protection equipment. Operators wore FFP2 in 58 centers (83%) during trans-thoracic echocardiography (TTE), in 65 centers (93%) during transesophageal echocardiography (TEE) and 63 centers (90%) during stress echocardiography. The second wave caused a significant reduction in number of echocardiographic exams, compared to November 2019 (from 513 ± 539 to 341 ± 299 exams per center, −34%, p < 0.001). On average, there was a significant increase in the outpatient waiting list for elective echocardiographic exams (from 32.0 ± 28.1 to 45.5 ± 44.9 days, +41%, p < 0.001), with a reduction of in-hospital waiting list (2.9 ± 2.4 to 2.4 ± 2.0 days, −17%, p < 0.001). We observed a large diffusion of point-of-care cardiac ultrasound (88%), with a significant increase of lung ultrasound usage in 30 centers (43%) during 2019, extended to all centers in 2020. Carbon dioxide production by examination is an indicator of the environmental impact of technology (100-fold less with echocardiography compared to other cardiac imaging techniques). It was ignored in 2019 by 100% of centers, and currently it is considered potentially crucial for decision-making in cardiac imaging by 65 centers (93%). Conclusions: In one year, major changes occurred in echocardiography practice and culture. The examination structure changed with extensive usage of point-of-care cardiac ultrasound and with lung ultrasound embedded by default in the TTE examination, as well as the COVID-19 testing.
Keywords: COVID-19, point-of-care cardiac ultrasound, lung ultrasound
1. Introduction
Cardiologists were engaged in an important way in the coronavirus disease 2019 (COVID-19) pandemic, with an important tribute in terms of infected and passed away professionals involved in clinical management and diagnostic screening with cardiac and lung ultrasound. During the first lockdown period (March/April 2020) in Italy, as previously reported worldwide, there was an unexpected drop in emergency cardiology admissions [1,2]. The reshaping of cardiology activities caused an important impact on echocardiographic laboratories [3]. In fact, in a previous survey, we observed a significant reduction in every echocardiographic exam during the lockdown period [4].
A new intriguing hypothesis was proposed about the cardio-protective benefits of lockdown, which induced air cleaning from pollution [5]. However, the awareness on the potential environmental impact of medical imaging is still poorly defined. Therefore, we sought to provide an instant survey of the echocardiography practice during the second wave of the COVID-19 pandemic in Italy, with high expectations for the post-COVID era regarding the echocardiographic activity and the perceived role of carbon dioxide production by cardiac imaging modalities in decision-making and its importance in the future development of imaging.
This study aimed to analyze the organization of echocardiographic laboratories and echocardiography practice during the second wave of the COVID-19 pandemic in Italy, and the expectations for the post-COVID era.
2. Methods
We analyzed two different time periods: the month of November during the second wave of the COVID-19 pandemic (2020) and the identical month during 2019 (November 2019).
A list of accredited echocardiographic laboratories was obtained from the Italian Society of Echocardiography and Cardiovascular Imaging (SIECVI). Each member of SIECVI was contacted by mail.
Data were retrieved via an electronic survey based on a structured questionnaire that was uploaded on the SIECVI website (www.siec.it, accessed on 14 December 2020)
For allocation of the response, the questionnaire required general information, such as the name of the hospital, the investigator and the interviewed person’s name:
General information: date, hospital’s name, department, name of the interviewed physician, and city and region of Italy.
Hospital activity and outpatient echocardiographic activity during the second wave of the COVID-19 pandemic.
The number of echocardiographic exams and the duration of waiting in-hospital lists and for outpatients in the two analyzed periods.
Types of activities organization in the echocardiography laboratory to reduce the operator risk: social distancing in the waiting room, limit to accompanying visitors, wearing of masks, reducing the number of exams, improvement of operators’ self-protection and nasopharyngeal swab required for patients before echocardiographic exams.
Usage of point-of-care cardiac ultrasound by cardiologists with a joint reading assessment with other physicians.
Use of lung ultrasound.
Modality of analysis of echocardiographic imaging.
Expectations for the post-COVID era regarding the echocardiographic activity.
Role of carbon dioxide production by cardiac imaging modalities in decision-making and its importance in the future development of imaging.
Statistical Analysis
Data were expressed as a mean ± standard deviations for continuous variables and as numbers (percentage) for categorical variables. Continuous variables were compared by using the Student’s unpaired test, while differences of categorical variables were assessed by the chi-square test.
A probability value of <0.05 was considered statistically significant.
All statistical calculations were performed by using SPSS for Windows, release 18.0 (Chicago, IL, USA).
3. Results
Data were obtained from 70 echocardiographic laboratories: 39 centers (56%) were in the northern regions of Italy (Lombardy, Veneto, Piedmont, Liguria, Friuli-Venezia-Giulia, Trentino-Alto-Adige and Emilia Romagna), 11 centers (16%) were in the central regions (Abruzzo, Latium, Tuscany and Umbria) and 21 (30%) were in southern regions (Campania, Sicily, Apulia and Calabria).
All centers had COVID-divisions, and six centers (9%) were COVID-dedicated hospitals, with three centers in the northern regions and three in the central and southern regions.
The cardiologists of the involved centers in the survey showed a relevant impact of COVID disease (138/991, 13.9%). Moreover, the cardiologists dedicated to the echocardiographic laboratories presented the same incidence of SARS-COVID disease, compared to other cardiologists (48/284, 16.9% vs. 90/707, 12.7%, p = 0.264).
During the second wave of the COVID-19 pandemic, the hospital activity proceeded normally in 25 centers (36%), partially reduced in 42 (60%) and wholly interrupted in 3 (4%), whereas outpatient echocardiographic activity was normal in 22 centers (31%), partially reduced in 41 (59%) and completely interrupted in 7 (10%).
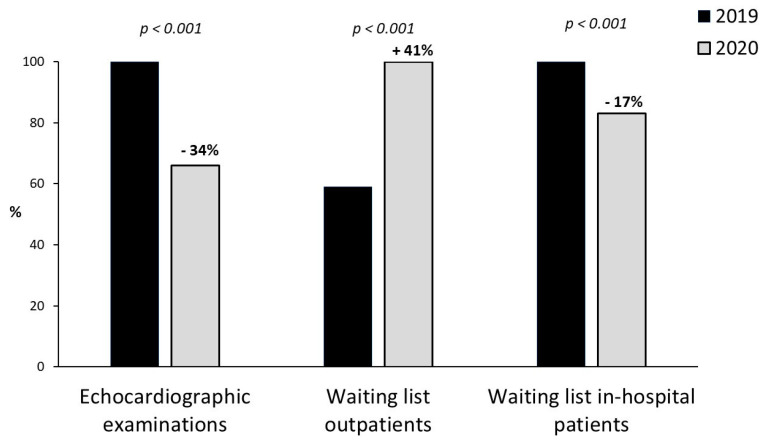
The effect of the second wave caused a significant reduction in the echocardiographic exams, compared to November 2019 (from 513 ± 539 to 341 ± 299 exams per center, −34%, p < 0.001, Figure 1). On average, there was a significant increase in outpatient waiting lists for elective echocardiographic exams (from 32.0 ± 28.1 to 45.5 ± 44.9 days, +41%, p < 0.001, Figure 1), with reduction of in-hospital waiting lists (2.9 ± 2.4 to 2.4 ± 2.0 days, −17%, p < 0.001, Figure 1).
Figure 1.
Percentage difference from November 2019 (black bar) to November 2020 (gray bars) in echocardiographic examinations, waiting list outpatients and waiting list in-hospital patients.
We did not find a difference in the centers with COVID-dedicated hospitals compared to centers without being involved in the number of echocardiographic exams (350 ± 228 vs. 341 ± 286 exams, p = 0.946) in outpatient waiting list for elective echocardiographic exams (75.8 ± 52.3 vs. 40.7 ± 42.0 days, p = 0.100) and in-hospital waiting list (2.8 ± 1.9 to 2.4 ± 2.0 days, p = 0.214).
We observed an important change in the activities’ organization in the echocardiography laboratory to reduce the operator risk: social distancing in waiting rooms (65 centers, 93%), limit to accompanying visitors (69, 99%), wearing of masks (all centers, 100%) and reducing the number of exams (59, 84%). improvement of self-protection of operators using appropriate personal protection equipment: FFP2 in 58 centers (83%) during trans-thoracic echocardiography (TTE), 65 (93%) during transesophageal echocardiography (TEE) and 63 (90%) during stress echocardiography (SE).
A nasopharyngeal swab was required for patients before echocardiographic exams in 46 centers (66%): only before TEE in 25 centers (54%), before TEE and SE in 14 centers (31%) and before all echocardiographic exams in 7 centers (15%). A nasopharyngeal swab was organized directly by the hospital into 46 centers (67%). On balance of test safety with specific reference to contagion risk, 87% of centers considered TTE safer than TEE or SE.
About SE, pharmacological SE was considered safer than exercise in 57 centers (81%).
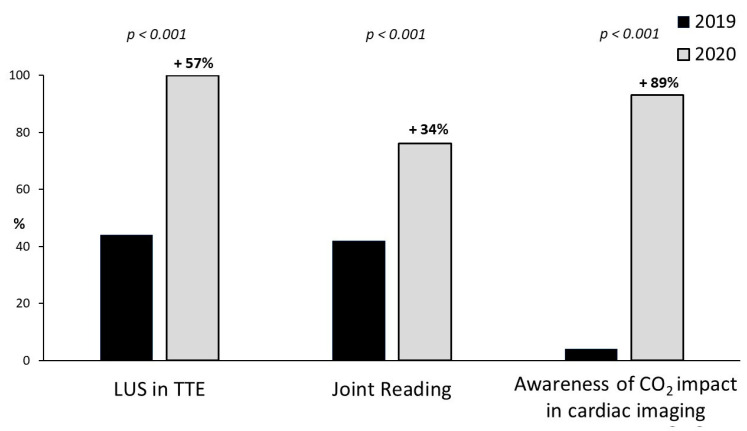
We observed a large and significant diffusion of point-of-care cardiac ultrasound (88%). It was performed by cardiologists with joint reading assessment with anesthesiologists (41%) or intensivists (36%) (Figure 2). Imaging analysis was mainly online (42 centers, 59%), but also offline (26, 38%) or by teleconsulting (2, 3%).
Figure 2.
Percentage difference from November 2019 (black bar) to November 2020 (gray bars) in lung ultrasound evaluation in resting TTE, joint reading assessment with intensivists and awareness of carbon dioxide (CO2) impact in cardiac imaging.
In 2019, the usage of lung ultrasound was a routine in 30 centers (43%); in 2020, all centers integrated lung ultrasound in the standard TTE evaluation of every patient, with or without suspicion of COVID-19 infection (Figure 2).
We also analyzed the expectations for the post-COVID era: participant centers felt that there should be a stable reduction of inappropriate echocardiographic exams (16 centers, 23%), no change in activity in the next year (23, 33%) or project a rebound of activity to take care of the follow-up examinations skipped during the pandemic (30, 43%).
Moreover, 65 centers (93%) believe that diagnostic imaging significantly contributes to the production of carbon dioxide, which is an indicator of the environmental impact of technology, and it should be incorporated in an integrated decision-making between alternative cardiac imaging modalities (Figure 2).
4. Discussion
In this manuscript, we demonstrated that echocardiographic laboratories in Italy were readily highly prepared for the second wave of the COVID-19 pandemic. In fact, we encountered an important change in the organization of echocardiographic activities to reduce patients’ risks: reduction of the exams’ number, social distancing in waiting rooms, limitation of accompanying visitors, wearing of masks and prescribing nasopharyngeal swab. Operators improved self-protection with the systematic de facto obligatory usage of appropriate personal protection equipment during echocardiographic exams.
This new organization of echocardiographic laboratories agreed with the previous papers [6,7] and the position papers of SIECVI [3] that identified these measures as the most important elements to reduce COVID-related risks. Our survey is focused on the Italian Echocardiography community, but similar precautions, recommendations and protection policies were encouraged and applied by single institutions [8], European Association of Echocardiography and Cardiovascular Imaging [9] and American Society of Echocardiography [7].
One more important point was the reduction of the exams’ number: deferring echocardiography studies deemed elective and non-urgent (or inappropriate), greatly reducing volumes in an effort to protect patients and echocardiography laboratory staff [10].
There was a profound remodeling also in the use of stress modalities in the Echocardiography laboratories, since exercise is considered a high-risk procedure because of aerosolization, and pharmacological stress became, by far, the test of choice in most laboratories [6].
The COVID pandemic has paradoxically produced an opportunity to help improve both sustainability and equity in the healthcare field and to reduce unnecessary and/or inappropriate tests, and deferring elective procedures [11].
TTE plays a prominent role in identifying cardiac complications related to COVID-19, but during TTE, the distance physician–patient is so reduced, getting in the droplets’ area. In addition to the preventive measures listed above, cardiac point-of-care ultrasound offers irreplaceable benefits to reduce the duration of TTE and, consequently, the time of exposure. Cardiac point-of-care ultrasound allows for rapid focused diagnostic assessment by providers already at the bedside [12,13]. Accordingly, in this survey, we observed a large diffusion of point-of-care cardiac ultrasound (88% of the centers) with the possibility to perform the examination not only by cardiologists but also with joint reading assessments with anesthesiologists or intensivists.
We have taken notice of a significant increase in the usage of lung ultrasound associated to TTE in all patients during COVID’s second wave (+57%) compared to the same period in 2019. Lung ultrasound is a useful diagnostic tool in different clinical conditions [14], as well as in the COVID-19 pandemic: in the first triage of symptomatic patients, in the emergency department, in the prognostic stratification and monitoring of patients with pneumonia, and in the management of patients in the intensive care unit, with low-cost and radiation-free approach. Another additional application of lung ultrasound is in pre-hospital diagnosis and, also, home monitoring of COVID patients [15,16]
Moreover, “bedside” lung ultrasound can reduce the number of physicians exposed to the virus during patients’ assessment and treatment.
The increase in the usage of lung ultrasound should be considered as the common language and meeting point between cardiologists and intensivist non-cardiology physicians aware of the importance and clinical role of lung ultrasound in critical healthcare [14].
A large portion of the centers (95%) believes that cardiological imaging played a role into the production of carbon dioxide. Indeed, the healthcare industry contributes 5 to 10% of the global carbon dioxide emission, and medical imaging for about 1%. Carbon dioxide emissions are the primary factor for global climate change. It is widely recognized that reducing carbon dioxide emissions is important to attenuate the impacts of climate change. The worsening of air quality induced by pollution acutely increases the admission rates for acute coronary syndromes, acute decompensated heart failure and atrial fibrillation [5]. Conversely, the improvement of air quality reduces the admission rates for the same conditions, as proven during the COVID-19 pandemic, due to the tumble of air pollution due to the lockdown [17,18]. Changes in hospital admission are only the tip of the iceberg of cardiovascular toxic effects of pollution, since, in patients with chronic conditions, coronary artery diseases or heart failure may show an increased vulnerability in coronary flow reserve or pulmonary congestion in the presence of increased air pollution levels [19]. Up until now, prescriptions in cardiac imaging have completely neglected the environmental dimension, yet we know that the environmental impact expressed as the emission of CO2 equivalents varies by a factor of 100 or 1000 between different cardiac imaging techniques, with an echocardiographic examination associated with 2 kg of carbon dioxide emissions and a cardiac resonance imaging or cardiac computed tomography associated with at least 100-fold higher level of emissions [20,21]. The variable of environmental impact of cardiac imaging is now increasingly perceived as being significant by the Italian echocardiographic community. There is a diffuse sentiment that scientific societies may play a major role in disseminating the culture of environmental sustainability in cardiac imaging, eventually promoting climate-neutral choices from industries, doctors and patients also in this important sector of economy [22].
5. Conclusions
In one year, major changes occurred in echocardiography practice and culture, triggered by the adaptive response to the COVID-19 pandemic. Fewer exams are performed per day, with a significant increase of outpatient waiting list for elective echocardiographic exams. Echocardiographic laboratories in Italy minimized the contagion risk by adequate protection policies, and the risk of infection is now included by prescribers and practitioners in the risk–benefit assessment of testing.
The perspective of the study offers a selection of important echocardiographic exams, a better and stricter adherence to the criteria of appropriateness, building the application of a flowchart for the selection of important exams and contributing to the setting aside of clearly inappropriate examinations.
The perceived risk of contagion is higher with TEE than with TTE. The exams structure changed, and lung ultrasounds for B-lines and pleural effusions are now embedded by default in the TTE examination also outside the COVID-19 testing. It is now an almost unanimous sentiment that the environmental impact of cardiac imaging should be incorporated into the risk–benefit assessment of cardiac imaging, with preferential steering towards climate-neutral choices. Carbon dioxide production by cardiac imaging examination is important to be aware of and consider its effect in environmental impact assessment in healthcare, and it should be disseminated by scientific imaging societies.
Acknowledgments
The SIECVI secretariat and staff for excellent administrative and technical support.
Author Contributions
Conceptualization, Q.C., F.A.-C. and A.B. (Andrea Barbieri); methodology, I.M., A.B. (Agata Barchitta) and G.T. (Giuseppe Trocino); validation, F.B. (Frank Benedetto), L.P. and A.C., formal analysis, Q.C. and S.M. (Sofia Miceli); investigation, I.A., G.B. (Giovanni Barbati), V.B., D.B., M.B., G.B. (Gianluigi Bergandi), G.B. (Giovanni Biliardo), A.B. (Amedeo Borganzoni), F.E.B., F.B. (Francesca Bursi), V.C., M.C., G.C. (Grazia Casavecchia), S.C. (Sebastiano Cicco), G.C. (Giovanni Cioffi), R.C., L.C., U.C., M.G.D., A.D., L.D., I.D., M.D.P., P.D.S., W.D., M.D.F., G.D.G., D.D.L., C.D.N., I.F., R.E., F.F., L.F., G.F., D.F., M.G., E.G., C.A.G., G.L.I., A.I., A.M.L., A.M., F.M., V.M., S.M. (Simona Mega), E.M., M.M., D.M., L.N., G.P., C.P. (Chiara Pedone), E.P. (Enrica Petruccelli), M.V.P., V.P., (C.P. Costantina Prota), F.R., D.E.R., S.S. (Silvio Saponara), C.S., V.S., W.S., S.S. (Sergio Severino), L.S., G.T. (Gloria Tamborini) and A.T.; writing—original draft preparation, Q.C.; writing—review and editing, E.P. (Eugenio Picano), A.B. (Andrea Barbieri), C.N., M.P. and P.C.; supervision, B.V., S.C. (Scipione Carerj), G.B. (Giuseppe Boriani), E.B., C.N. and A.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.De Filippo O., D’Ascenzo F., Angelini F., Bocchino P.P., Conrotto F., Saglietto A., Secco G.G., Campo G., Gallone G., Verardi R., et al. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N. Engl, J. Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Rosa S., Spaccarotella C., Basso C., Calabrò M.P., Curcio A., Filardi P.P., Mancone M., Mercuro G., Muscoli S., Nodari S., et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Antonini-Canterin F., Pepi M., Monte I. Document addressed to cardiovascular echography operators at the time of COVID-19: A Document by the “Società Italiana di Ecocardiografia e CardioVascular Imaging” Board 2019–2021. J. Cardiovascular Echo. 2020;30:2–4. doi: 10.4103/jcecho.jcecho_27_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ciampi Q., Antonini-Canterin F., Barbieri A., Barchitta A., Benedetto F., Cresti A., Miceli S., Monte I., Picano E., Pepi M. Remodeling of Activities of Italian Echocardiographic laboratories during COVID-19 Lockdown: The SIECoVId study. J. Cardiovasc. Med. 2021;22:600–602. doi: 10.2459/JCM.0000000000001143. [DOI] [PubMed] [Google Scholar]
- 5.Picano E. Where have all myocardial infarctions gone? The answer is blowing in the less polluted wind. Eur. Heart J. 2020;41:2146–2147. doi: 10.1093/eurheartj/ehaa411. [DOI] [PubMed] [Google Scholar]
- 6.Zoghbi W.A., DiCarli M.F., Blankstein R., Choi A.D., Dilsizian V., Flachskampf F.A., Geske J.B., Grayburn P.A., Jaffer F.A., Kwong R.Y., et al. Multimodality Cardiovascular Imaging in the Midst of the COVID-19 Pandemic: Ramping Up Safely to a New Normal. JACC Cardiovasc. Imaging. 2020;13:1615–1626. doi: 10.1016/j.jcmg.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirkpatrick J.N., Mitchell C., Taub C., Kort S., Hung J., Swaminathan M.J. ASE Statement on Protection of Patients and Echocardiography Service Providers During the 2019 Novel Coronavirus Outbreak: Endorsed by the American College of Cardiology. J. Am. Soc. Echocardiogr. 2020;33:648–653. doi: 10.1016/j.echo.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flórez J.M.V., Barrios Alonso V., Gofin C.F. The day after tomorrow: Echocardiography laboratories after the COVID-19 outbreak. Eur. Heart J. Cardiovasc. Imaging. 2020;21:1057. doi: 10.1093/ehjci/jeaa207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Skulstad H., Cosyns B., Popescu B.A., Galderisi M., Salvo G.D., Donal E., Petersen S., Gimelli A., Haugaa K.H., Muraru D., et al. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur Heart J. Cardiovasc. Imaging. 2020;21:592–598. doi: 10.1093/ehjci/jeaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ward R.P., Lee L., Ward T.J., Lang R.M. Utilization and Appropriateness of Transthoracic Echocardiography in Response to the COVID-19 Pandemic. J. Am. Soc. Echocardiogr. 2020;33:690–691. doi: 10.1016/j.echo.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moynihan R., Johansson M., Maybee A., Lang E., Légaré F. Covid-19: An opportunity to reduce unnecessary healthcare. Recovering health systems can prioritise genuine need. BMJ. 2020;370:m2752. doi: 10.1136/bmj.m2752. [DOI] [PubMed] [Google Scholar]
- 12.Kameda T., Mizuma Y., Taniguchi H., Fujita M., Taniguchi N. Point-of-care lung ultrasound for the assessment of pneumonia: A narrative review in the COVID-19 era. J. Med. Ultrason. 2021;13:1–13. doi: 10.1007/s10396-020-01074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kirkpatrick J.N., Grimm R., Johri A.M., Kimura B.J., Kort S., Labovitz A.J., Lanspa M., Phillip S., Raza S., Thorson K., et al. Recommendations for echocardiography laboratories participating in cardiac point of care cardiac ultrasound (POCUS) and critical care echocardiography training: Report from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2020;33:409–422. doi: 10.1016/j.echo.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Picano E., Scali M.C., Ciampi Q., Lichtenstein D. Lung Ultrasound for the Cardiologist. JACC Cardiovasc. Imaging. 2018;11:1692–1705. doi: 10.1016/j.jcmg.2018.06.023. [DOI] [PubMed] [Google Scholar]
- 15.Barchitta A., Pepi M., Monte I.P., Trocino G., Barbieri A., Ciampi Q., Cresti A., Miceli S., Petrella L., Benedetto F., et al. Lung Semiotics Ultrasound in COVID-19 Infection. J. Cardiovasc. Echogr. 2020;30:S1–S5. doi: 10.4103/jcecho.jcecho_53_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gargani L., Soliman-Aboumarie H., Volpicelli G., Corradi F., Pastore M.C., Cameli M. Why, when, and how to use lung ultrasound during the COVID-19 pandemic: Enthusiasm and cautio. Eur. Heart J. Cardiovasc. Imaging. 2020;21:941–948. doi: 10.1093/ehjci/jeaa163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Collart P., Dubourg D., Levêque A., Sierra N.B., Coppieters Y. Short-term effects of nitrogen dioxide on hospital admissions for cardiovascular disease in Wallonia, Belgium. Int. J. Cardiol. 2018;255:231–236. doi: 10.1016/j.ijcard.2017.12.058. [DOI] [PubMed] [Google Scholar]
- 18.Picano E. Air cardiology is now on air. Eur. Heart J. 2021;42:961–962. doi: 10.1093/eurheartj/ehaa962. [DOI] [PubMed] [Google Scholar]
- 19.D‘Andrea A., Ciampi Q., Russo A., Forni A., Mangia C., Picano E. The effects of lockdown-induced air quality changes on the results of cardiac functional stress testing in coronary artery disease and heart failure patient. Environ. Sci. Pollut. Res. Int. 2021;30:1–8. doi: 10.1007/s11356-021-13622-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marwick T.H., Buonocore J. Environmental impact of cardiac imaging tests for the diagnosis of coronary artery disease. Heart. 2011;97:1128–1131. doi: 10.1136/hrt.2011.227884. [DOI] [PubMed] [Google Scholar]
- 21.Martin M., Mohnke A., Lewis G.M., Dunnick N.R., Keoleian G., Maturen K.E. Environmental Impacts of Abdominal Imaging: A Pilot Investigation. J. Am. Coll. Radiol. 2018;15:1385–1393. doi: 10.1016/j.jacr.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 22.Cano-Aguilar I., Vice-President European Economic and Social Committee. Sustainability must be at the heart of Europe’s future. Open Access Government. [(accessed on 20 January 2020)]; Available online: https://www.openaccessgovernment.org/sustainability-must-be-at-the-heart-of-europes-future/80930/