Abstract
Objectives:
People living with HIV (PLWH) have increased risk for cancer and worse cancer-specific survival. We explored the emotional burden of cancer and HIV as a potential driver of cancer mortality.
Research Approach:
Semi-structured qualitative interviews with PLWH and cancer.
Participants:
27 PLWH who had either completed cancer treatment, were currently undergoing treatment, or experienced challenges in completing treatment.
Methodological Approach:
An inductive qualitative approach using the constant comparative method.
Findings:
Participants drew strong parallels between being diagnosed with HIV and cancer. Many described HIV-related stigma that hindered social support. Cancer treatment side effects were a major challenge, impacting treatment adherence for both cancer and HIV.
Implications for Psychosocial Providers:
There is a need for convenient, affordable, and visible services to support PLHIV as they navigate cancer care. Services should be tailored to the unique needs of this population by addressing HIV-related stigma, building social support, and fostering resilience.
Keywords: Dual burden of HIV and Cancer, Health Disparities, HIV-Associated Comorbidities, Qualitative Research, Malignancies, Mental Health, HIV Stigma
BACKGROUND
The life expectancy of people living with HIV (PLWH) has dramatically improved in the last quarter-century, but continues to be lower than the general population (1). One key reason for this disparity is the high prevalence of certain comorbid conditions among PLWH, including cancers (2,3). PLWH have an increased risk for diagnosis of certain cancers and worse cancer-specific survival than the general population for several common cancer types, patterns which hold true for both AIDS-defining and non-AIDS-defining malignancies (4–6). Accordingly, cancer is the number one non-AIDS cause of death among PLWH (7).
The drivers of cancer-specific mortality among PLWH are complex and include system-, provider-, and patient-level factors (8,9). However, one area that has received little attention is the emotional burden of coping with cancer in the context of a pre-existing HIV diagnosis, and the potential negative impact this may have on treatment outcomes. Prior studies focusing on sub-populations of PLWH, namely human papillomavirus (HPV) and anal cancers among men who have sex with men, have identified multiple overlapping stigmas and resulting emotional challenges in managing these comorbid disorders (10,11).
As a result of improved therapeutics for HIV, more than half of all PLWH in the U.S. are now over the age of 50, and this proportion is expected to increase to 70% by the year 2030 (12). The aging of the population of PLWH has placed HIV and noncommunicable diseases such as cancer on an epidemiological “collision course”, with the expectation of steadily rising comorbidity in the years to come (13,14). Further, many older adults living with HIV were diagnosed with the virus during the early years of the epidemic before highly active antiretroviral therapy (HAART) was available, an era marked by mortality, fear, misinformation, and stigma (15). The residual effects of those experiences, including physical and emotional stresses, continue to drive health disparities among PLWH today (16,17). For example, rates of psychiatric disorders are approximately double among PLWH compared to the general population, including substantially higher rates of depression, anxiety, substance use, and traumatic stress (18). Despite broad campaigns seeking to educate the public and reduce misinformation about HIV, stigma remains commonplace and has a direct impact on social support, quality of life, and willingness to engage in care among PLWH (19,20).
The combined burden of HIV and cancer in the United States can be further explained by the syndemic relationship between the two conditions, represented by multiple shared and mutually reinforcing risk factors (21). For example, both HIV and cancer have higher prevalence and poorer outcomes among people with lower education and those living in poverty (22). HIV continues to disproportionately affect people of color, men who have sex with men, and other socially marginalized communities (23). Even among people who do not fit into these categories of risk, both HIV and cancer can lead to social stigma, feelings of self-blame, and emotional turmoil (24). As a result, PLWH and cancer may simultaneously experience historical trauma and the emotional burden of present-day stigma, both of which contribute to inequities in health and well-being (16,17,25).
Thus, among PLWH, the diagnosis of another condition or disease can be devastating and potentially life-threatening (21). The mental health challenges associated with HIV alone or cancer alone are well-established, and emotional distress is associated with poorer care engagement for both conditions (26,27). However, few studies have examined the experiences of patients diagnosed with both HIV and cancer, and the few studies that do exist have focused on specific cancers and sub-populations, such as men who have sex with men. The purpose of this study is to more clearly characterize the dual burden of living with HIV and cancer from the patient’s perspective - including participants who are diverse in their age, sexual orientation, and cancer type - with the goal of guiding future patient-provider interactions and informing interventions to support coping strategies for this vulnerable population.
METHODS
We conducted qualitative in-depth interviews with 27 adult patients who underwent cancer treatment and had a pre-existing HIV diagnosis. Participants were recruited from an academic medical center in the southeastern United States and the demographics of PLWH served by the center largely mirror the demographics of the broader U.S. population of PLWH (28). Participants were eligible to participate if they were 18 years of age, fluent in English, and physically and cognitively capable of completing the informed consent and interview process. We purposively recruited participants into three groups: those who previously completed cancer treatment (n=9), those currently undergoing cancer treatment (n=9), and those who experienced challenges in adhering to or completing cancer treatment, including multiple missed appointments, early discontinuation of treatment, or medication non-adherence (n=9). This recruitment strategy was adopted to ensure that we captured the perspectives of patients with recent experiences to avoid recall bias, and to understand the challenges faced by patients who do not complete cancer treatment. Adult participants with all cancer types were eligible for the study.
Eligible participants were identified using DEDUCE software and the institution’s electronic medical record. Upon preliminary identification of eligible participants, we contacted the patient’s cancer or infectious disease physician to obtain permission to invite the patient to participate in the study. At the patient’s next clinic appointment, we introduced the study to assess the patient’s interest in participating, obtained written informed consent, and scheduled an interview date. Five invited patients declined to participate, citing conflicts with other time commitments and transportation challenges.
Qualitative interviews were conducted at a private office using a semi-structured interview guide and audio-recorded with the participant’s permission. Participants were conducted by a postdoctoral researcher or medical student trained in qualitative research and each interview lasted approximately 60 minutes. Upon completion of the study, a $60 remuneration and parking pass were provided. Interview audio files were uploaded to a secure, password-protected server and transcribed, with all identifying information deleted during transcription. Study findings are reported in accordance with the Standards for Reporting Qualitative Research (SRQR; (29). The study received ethical approval from the institutional review board of the Duke University Health System.
Qualitative Interview Guide
The research team developed the in-depth interview guide using prior literature about the challenges of cancer treatment and cancer outcomes among PLWH (10,11,30), as well as three theoretical frameworks for health care decision-making: the Andersen Healthcare Utilization Model, Health Belief Model, and PEN-3 Model (31–33). These models each highlight factors that promote or hinder access to care, care engagement, and health outcomes. To capture the unique challenges faced by PLWH and cancer, a preliminary version was reviewed and edited by members of the institution’s HIV community advisory board, who also assisted in the interpretation of the study findings. The components of the final qualitative interview guide are detailed in Figure 1.
Figure 1:
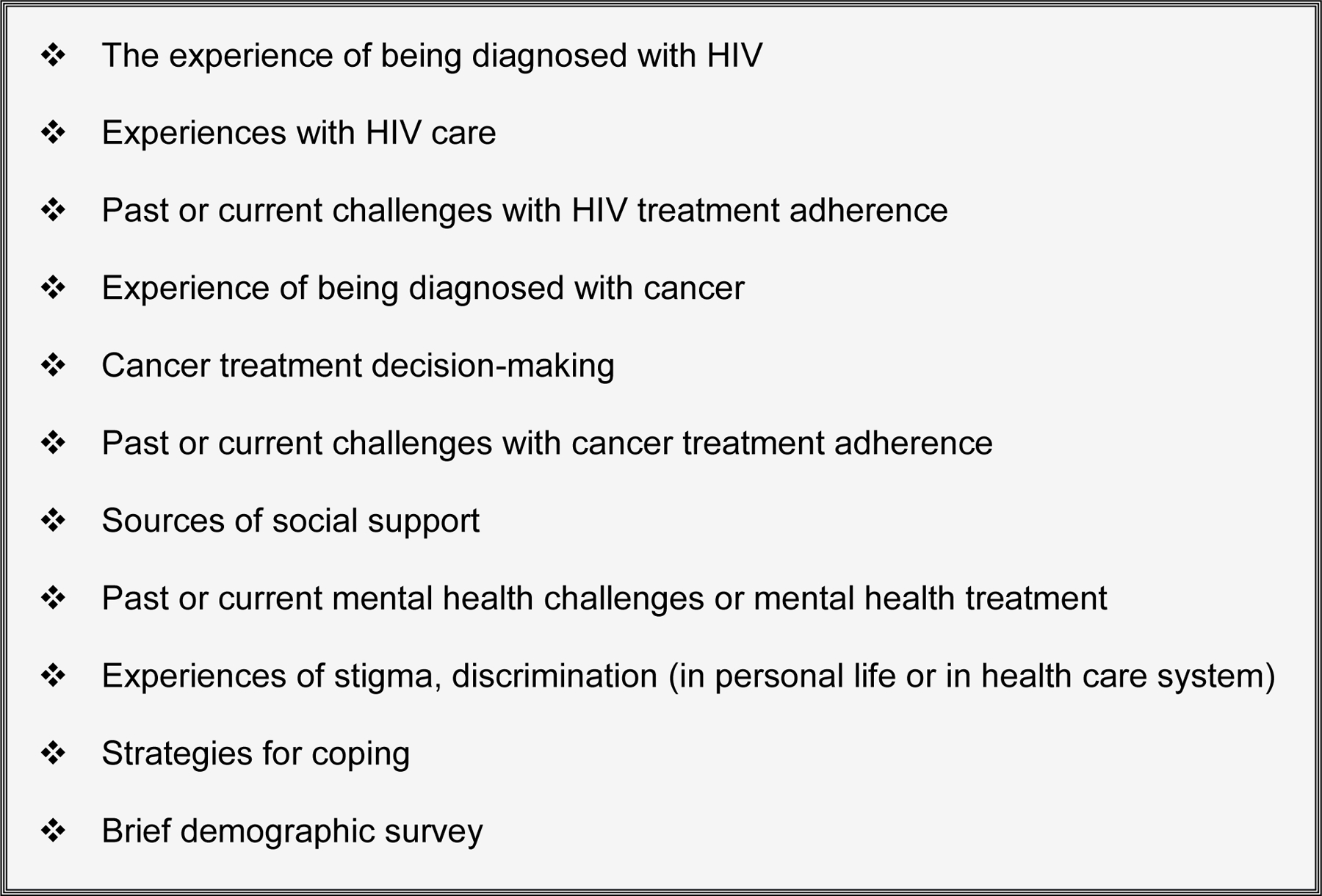
Final domains in the in-depth interview guide
Data Analysis
Broad domains for the data analysis were derived from the theoretically-informed qualitative interview guide. Within each domain, interview data were coded for inductive themes using an applied thematic approach (34) informed by the constant comparative method of qualitative analysis (35). For each transcribed interview, a narrative memo was generated to summarize and organize the content onto the pre-identified domains (36). Each transcript-memo pair was then reviewed for accuracy by a second team member and disagreements were discussed to consensus. Next, two research team members used NVivo software to inductively code the content of the narrative memos within each domain. A subset of 9 interviews, 3 from each participant group, were re-coded by a second team member and assessed for inter-coder agreement using a threshold of 80% agreement (37), which was achieved for all memos. Themes in the data were discussed and finalized in consensus building discussions with the full study team, including topic and method experts, and through feedback from the community advisory board. The final themes were then used to generate frequencies and present the results.
RESULTS
The results are organized around the research domains and describe the inductive themes that emerged during qualitative analysis (see Table 2).
Table 2:
Summary of Qualitative Analysis on Dual Burden of HIV and Cancer (N=27)
| Theme | Frequency (n) | Illustrative Quotation |
|---|---|---|
| Dual burden of HIV and cancer diagnoses | 9 | “It made me feel like, seriously, what next? You have a devastating disease as HIV. And you’re living with that and you’re doing ok. And then after, eight years later down the line, you’re diagnosed with cancer. Now you got two deadly diagnoses…Dealing with both is a double bullet.” |
| Stigma greater for HIV than for cancer | 9 | “You know, the cancer thing, here’s what goes on. ‘Oh God, I can’t believe you had cancer, I’m so sorry.’ Then for HIV. ‘Oh God, you got HIV, what the hell did you do?’ People have sympathy for cancer. They don’t have it for HIV.” |
| Receive support from a Care Coordinator | 9 | Oh man, she’s outstanding. She makes sure I have, like, whatever I might need. She helps me to make a plan so I can keep my heat on in the winter and keep food on the table. And she helps me keep my appointments and set my medicine up so I don’t have to pay any copays.” |
| Disclosed cancer diagnosis and not HIV diagnosis to support system | 8 | “My parents needed to know [about the cancer] but I couldn’t tell them I had HIV. It was better, or easier to say, that I’ve got cancer and not only to them but to everybody else. I can’t tell anyone else I have HIV.” |
| Fear of negative impact of HIV on cancer care | 8 | “My immune system is already suppressed and now, to undergo radiation and chemo, that puts me at a higher risk. There’s more immune suppression because now I gotta take these toxic drugs.” |
| Fear of negative impact of cancer on HIV care | 7 | “The one thing that really bothered me and alarmed me, was that [my viral load] was no longer undetectable after starting my cancer treatment, and I didn’t know what was gonna happen.” |
| Substance abuse as a form of unhealthy coping | 7 | “I was very depressed, you know…HIV was bad enough then I had cancer on top of that and I felt like well I’m going to die so I got into drugs real heavy and I just went on a real emotional rollercoaster. I didn’t care and I thought I was going to die.” |
Note: Frequency refers to the number of interviews where the theme was present.
Participants
Participants predominantly identified as male (n=22, 81.5%) and Black/African American (n=19, 70%), and reported a median annual household income of $24,000 and median age of 56 years. More than one-third of participants (n=10, 37%) were diagnosed with HIV before HAART became available in 1996 (38). On average, participants were diagnosed with their first cancer 13 years after their HIV diagnosis (median: 14, IQR: 7–19). Nine participants (33%) were diagnosed with multiple cancers, including one participant who was diagnosed with three types. Nine participants (33%) meet with a Care Coordinator to assist in navigating their care, with five of these participants describing this person as an important source of support related to care engagement and medication adherence, health education, and social needs. See Table 1 for additional participant demographic and clinical information.
Table 1:
Participant Demographic, HIV, and Cancer Characteristics (N=27)
| Variable | n (%) |
|---|---|
| Gender | |
| Male | 22 (81%) |
| Female | 5 (19%) |
| Race/Ethnicity | |
| Black/African American | 19 (70%) |
| Non-Hispanic White | 7 (26%) |
| Hispanic/Latino | 1 (4%) |
| Education | |
| High school or less | 11 (41%) |
| Some college or college degree | 12 (44%) |
| Graduate of professional degree | 4 (15%) |
| Insurance | |
| Private insurance | 8 (30%) |
| Medicare | 7 (26%) |
| Medicaid | 3 (11%) |
| Uninsured | 1 (4%) |
| Received free ‘charity care’ for cancer | 8 (30%) |
| Work with Care Coordinator | 9 (33%) |
| Cancer Stage at Diagnosis | |
| Stage 1 | 7 (26%) |
| Stage 2 | 3 (11%) |
| Stage 3 | 6 (22%) |
| Stage 4 | 9 (33%) |
| Cancer Type | |
| Anal | 9 (33%) |
| Non-Hodgkins Lymphoma | 5 (19%) |
| Hodgkins Lymphoma | 4 (15%) |
| Head and Neck | 4 (15%) |
| Prostate | 4 (15%) |
| Colorectal | 2 (7%) |
| Liver | 2 (7%) |
| Vulvar | 2 (7%) |
| Lung | 1 (4%) |
| Bladder | 1 (4%) |
| Thyroid | 1 (4%) |
| Penile | 1 (4%) |
| HIV Viral Load at Time of Cancer Diagnosis | |
| > 1,000 copies/mL | 2 (7%) |
| 100–1000 copies/mL | 2 (7%) |
| < 100 copies/mL | 6 (22%) |
| Undetectable | 13 (48%) |
HIV Diagnosis and Treatment
In discussing the HIV diagnosis experience, many participants described an initial period of shock and disbelief, immediately followed by a sense of hopelessness, despair, or fear of death. Several participants shared stories of friends or loved ones who had died of HIV/AIDS, and said these personal experiences contributed to fear that the disease would be fatal.
“[The day I received my HIV diagnosis] was horrible because in those days it was a death sentence. I remember driving home, I felt so hopeless and I didn’t know how to tell my family. I was just choked with emotion and it was the hardest day I think I’ve had in my life, and I’ve had some hard days.”
-male, age 67
Several participants attributed their despair to a lack of information about HIV and said their outlook improved as they learned about the disease and the treatment available to them.
After receiving the HIV diagnosis, about half of participants immediately began antiretroviral therapy (ART) treatment and reported that they have been consistently adherent ever since. Several others delayed in following through with an initial referral, but have since been adherent. Multiple participants described occasionally missing a dose of ART.
“Well, I’m just busy doing other things. I mean, I have other medicines besides the HIV medicine to take at night. I don’t know. You go out, eat, and you get a phone call, and then the next thing you know it’s bedtime so, oh, I forgot to take my medicine.”
– male, age 58
Only a small number of participants described serious challenges with ART adherence, and these tended to be the same participants who experienced cancer treatment challenges. Some described forgetting to take their ART due to alcohol or drug use, while others described apathy, often associated with symptoms of depression: “When I feel depressed, I don’t care [about missing my ART dose], I really don’t. I don’t feel like being bothered. Most of the time I’m in bed.” Participants also frequently connected ART non-adherence to the emotional burden and side effects of cancer treatment. Participants who underwent radiation treatment commonly described the treatment as painful, while those who underwent chemotherapy reported nausea and fatigue that sapped them of energy and motivation to adhere to ART.
“It gets to the point where you miss a lot of [ART] doses. I mean, I had periods where I would be so sick that I’d have to debate am I going to go to the bathroom or am I going to get something to eat. I didn’t have the energy to do both. So I’m sure there were a lot of HIV drugs that were missed because I just didn’t have the energy to do anything.”
– female, age 43, anal cancer
Cancer Diagnosis and Treatment
Participants described their reactions to their cancer diagnosis very similarly to their HIV diagnosis, including feelings of shock, fear, hopelessness, and despair. Many participants drew direct parallels between the two experiences: “So if you want to know how I felt, I was devastated. I felt like I almost died of AIDS and now I’m going to die of cancer.” The time from the cancer diagnosis to the start of treatment was generally short, contributing to feelings that “things were moving really fast.” Themes of fear and uncertainty were particularly common among participants actively receiving treatment at the time of the interview, as they were still unsure about the outcome of treatment.
Participants frequently described a combined or dual burden of HIV and cancer, which had a cumulative impact on health and emotional well-being. For participants who experienced challenges in adhering to cancer treatment, many reported increases in distress and treatment fatigue over time, including the pressures of attending daily treatments, maintaining medication adherence, and treatment side effects. Cancer treatment side effects were the most commonly cited reason for distress, and were a key contributor to cancer treatment non-adherence.
“I stopped everything. I gave up…I took two [chemotherapy] treatments and it wracked my whole body with pain and I said I can’t do this anymore. It takes everything from you, you know? You’re constantly overwhelmed with fatigue.”
– female, age 55, vulvar cancer
For participants who described poor social support or symptoms of mental illness, the challenges of living with HIV and cancer were even more pronounced. As one participant shared, “I have two diseases that are deadly and nobody to talk to.”
A small number of participants acknowledged using drugs and alcohol in an attempt to manage or numb their distress.
“Well, I was really depressed…I was like wow, HIV was bad enough, then I had cancer on top of that and I thought ‘well, I’m going to die’, so I started acting out. I got back into drugs real heavy and I went on an emotional rollercoaster. I mean, I just didn’t care. I thought I was gonna die, so I was gonna go out with a bang.”
– male, age 49, Hodgkins lymphoma
Several participants reported receiving mental health treatment at some point in their lives, and they generally felt it was helpful in coping with their health concerns. Several participants also reported having to discontinue their mental health treatment due to changes in insurance or prohibitive costs.
Differences in Stigma and Support for HIV and Cancer
In discussing differences in support for cancer versus HIV, most patients said they disclosed their cancer diagnosis to loved ones within hours of learning they had cancer. By contrast, participants were extremely cautious with HIV disclosures, which greatly hindered social support. HIV stigma was cited as the key reason for this difference, including experiences of enacted stigma from friends, family, and community members, internalized feelings of shame, and the anticipation of mistreatment or discrimination that might occur if their HIV status became known. Several participants, particularly those in the adherence challenges group, had only disclosed their HIV status to few others, despite carrying the diagnosis for many years (Table 2). As one participant described, “I’m not afraid of telling people about the cancer. What I am [afraid of] is how to tell my parents about my HIV. My partner is the only one who knows.”
HIV stigma also led to difficulties participating in cancer care. Several participants expressed concern about unwanted disclosures of their HIV status by healthcare workers, which prevented them from bringing family members to appointments. There were also rare but impactful instances of perceived stigma by hospital staff. One participant described the following interaction with an oncology nurse: “She was so nice and provided great care, then one day she just stopped coming. I think she went on the computer and saw my [HIV] status and she just never came back.”
Examples of Positive Coping
The dual burden of HIV and cancer was clear for participants; however, many also exemplified resilience, perseverance, and positive coping. As one participant explained, “I don’t let it simmer. I mean, I just move on. I know some people would take a drink, but I don’t do that. I just sit and maybe I get frustrated, take a deep breath, settle down, and move on.” Patients acknowledged the difficult aspects of being treated for HIV and cancer, but several had reached a point of acceptance. Many felt that these experiences had made them stronger, and several reported finding purpose in supporting other patients in treatment.
“I’m much more empathetic now after dealing with HIV and cancer. Every time I come here, I talk to people. You can sometimes see it in their faces that they have fear. When they’re waiting to get CT scans, I go up to them and I share about my positive outlook and about fear and encourage them to look at things in a different light.”
– male, age 67, oral cancer and non-Hodgkins lymphoma
DISCUSSION
This study used qualitative interviews to explore the unique stressors faced by people living with HIV as they navigate a cancer diagnosis and treatment. Patients commonly described a dual or cumulative burden of HIV and cancer, including emotional challenges, side effects, and treatment fatigue. In many cases, coping was complicated by HIV-related stigma, which prevented patients from disclosing their status and seeking social support, supporting findings from earlier studies (16,39). These cumulative challenges created a complex medical and social situation and, in some cases, led to lapses in treatment adherence for HIV and cancer.
Cancer treatment is innately challenging, and side effects can be overwhelming, unpleasant, and negatively impact daily functioning (40). It is unclear whether a pre-existing HIV diagnosis contributes to worsened side effects from cancer treatment (41). However, the cumulative emotional burden of cancer among PLWH can negatively impact motivation to engage in care and may be a driver of disparities in cancer survival among people living with HIV (5,6). Motivation is a critical driver of treatment adherence for both cancer and HIV, particularly in the context of cancer treatment side effects such as fatigue, nausea, and cognitive difficulties. The emotional toll of cancer treatment uniquely affects people with chronic illness, including PLWH, because there is a need to adhere to medication while managing cancer treatments and side effects. Support systems are crucial to mitigate the emotional impact, help patients living with HIV and cancer to complete their cancer treatments, and support adherence to HIV and cancer care (42).
In addition, PLWH commonly express concerns about whether a new cancer diagnosis might influence their HIV treatment and prognosis. Thus, it is important for providers to communicate how/whether cancer treatments may interact with HIV treatment, including viral load or CD4 counts and the efficacy of ART. These concerns may be particularly important for patients whose cancer or cancer treatment has the potential to impact immune processes vital to HIV treatment outcomes (40). Cancer providers can assist PLWH by offering additional information and collaborating with HIV specialists, which may help PLWH cope with potential barriers to mental and physical health. Continued research is necessary to understand how newer cancer treatments may impact HIV and ART, so that providers can provide accurate and helpful information.
Resilience is an important facilitator of treatment adherence for both HIV and cancer, and has been identified as a key factor in predicting positive treatment outcomes (43,44). Resilience can mitigate feelings of hopelessness and fears about death, which may improve cancer care engagement and overall mental health (38,45). It is critically important to develop and assess interventions aimed at fostering resilience, which may improve the experiences of PLWH as they engage in cancer treatments.
Implications for Psychosocial Oncology
There is a need for convenient, affordable, and visible services to support PLWH as they navigate their cancer diagnosis and care. This could include increased access to social work and care navigators, psychotherapy to improve mental health and behavioral health, occupational therapy to improve daily functioning, and support groups sensitive to the issues of PLWH.
Current health insurance programs and charitable care offered in health systems are critical to the ongoing care engagement and associated outcomes among people living with HIV and cancer. Current programs must be sustained or improved and similar efforts should be made to improve low-cost access to mental health care in this vulnerable population.
Additional research is needed to understand the needs of PLWH as they transition from cancer diagnosis to treatment to follow-up for cancer survivorship, as well as the unique needs of PLWH with intersecting marginalized identities, such as LGBTQ and racial minority individuals.
Study Limitations
The results of this study should be interpreted in light of the following limitations. All of the study participants were recruited from a single medical center in the southeastern United States. The medical center has a variety of support services for cancer patients and PLWH, such as the Ryan White HIV/AIDS Program, the Care Coordinator program, a charitable care program for uninsured low-income individuals, and free support groups. It is likely that PLWH undergoing cancer treatment at centers with fewer support services may be in even greater need of auxiliary care. Our study included only qualitative methods, as our goal was to gain a detailed understanding of the experiences of PLWH in their own words; we believe this is an important first step in research on this topic before transitioning to experimental methods, which may be better suited to assess the generalizability of findings in larger and more diverse samples.
Conclusions
This study is among the first to explore the dual emotional burden faced by patients living with HIV and cancer. The research describes the challenges of receiving a cancer diagnosis, cancer treatment side effects, and strategies for coping. For providers, these findings point to the importance of considering this dual burden when assessing barriers to care engagement among PLWH and cancer. It is important for health systems to continue examining strategies to enhance support and foster resilience to maximize cancer and HIV care engagement across healthcare settings.
Acknowledgements:
The authors would like to acknowledge Bijal Shah, MS from the Department of Radiation Oncology, Duke Cancer Institute, for her assistance in study recruitment and the Duke Center for AIDS Research Community Advisory Board (CFAR CAB) for their assistance in developing and piloting the study interview guide and interpreting the findings.
Funding: This project was supported by Duke Cancer Institute’s Cancer Control and Population Sciences Pilot Grant. The authors would also like to acknowledge support received by the Duke University Center for AIDS Research (CFAR; 5P30 AI064518) and the National Cancer Institute (K08 CA228631).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
REFERENCES
- 1.Samji H, Cescon A, Hogg RS, Modur SP, Althoff KN, Buchacz K, et al. Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS ONE 2013;8(12):e81355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coghill AE, Engels EA. Are cancer outcomes worse in the presence of HIV infection? Cancer Epidemiol Biomarkers Prev 2015. August;24(8):1165–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wandeler G, Johnson LF, Egger M. Trends in life expectancy of HIV-positive adults on antiretroviral therapy across the globe: comparisons with general population. Curr Opin HIV AIDS 2016;11(5):492–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coghill AE, Shiels MS, Suneja G, Engels EA. Elevated Cancer-Specific Mortality Among HIV-Infected Patients in the United States. J Clin Oncol 2015. July 20;33(21):2376–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rositch AF, Jiang S, Coghill AE, Suneja G, Engels EA. Disparities and Determinants of Cancer Treatment in Elderly Americans Living With Human Immunodeficiency Virus/AIDS. Clin Infect Dis 2018. 28;67(12):1904–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zucchetto A, Virdone S, Taborelli M, Grande E, Camoni L, Pappagallo M, et al. Non-AIDS-Defining Cancer Mortality: Emerging Patterns in the Late HAART Era. J Acquir Immune Defic Syndr 2016. 01;73(2):190–6. [DOI] [PubMed] [Google Scholar]
- 7.Smith CJ, Ryom L, Weber R, Morlat P, Pradier C, Reiss P, et al. Trends in underlying causes of death in people with HIV from 1999 to 2011 (D:A:D): a multicohort collaboration. Lancet 2014. July 19;384(9939):241–8. [DOI] [PubMed] [Google Scholar]
- 8.Chiu CG, Smith D, Salters KA, Zhang W, Kanters S, Milan D, et al. Overview of cancer incidence and mortality among people living with HIV/AIDS in British Columbia, Canada: Implications for HAART use and NADM development. BMC Cancer 2017. April 14;17(1):270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marcus JL, Chao C, Leyden WA, Xu L, Yu J, Horberg MA, et al. Survival among HIV-infected and HIV-uninfected individuals with common non-AIDS-defining cancers. Cancer Epidemiol Biomarkers Prev 2015. August;24(8):1167–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gaspar M, Grennan T, Salit I, Grace D. Confronting comorbidity risks within HIV biographies: gay men’s integration of HPV-associated anal cancer risk into their narratives of living with HIV. Health, Risk & Society 2018. August 18;20(5–6):276–96. [Google Scholar]
- 11.Gaspar M, Marshall Z, Rodrigues R, Adam BD, Brennan DJ, Hart TA, et al. A tale of two epidemics: gay men’s mental health and the biomedicalisation of HIV prevention and care in Toronto. Sociol Health Illn 2019. July;41(6):1056–70. [DOI] [PubMed] [Google Scholar]
- 12.Wing EJ. HIV and aging. Int J Infect Dis 2016. December;53:61–8. [DOI] [PubMed] [Google Scholar]
- 13.Harris CM, McKenzie R, Nayak S, Kiyatkin D, Baker D, Kisuule F. Graying of the HIV epidemic: a challenge for inpatient medicine providers. J Community Hosp Intern Med Perspect [Internet] 2015. December 11 [cited 2020 Feb 12];5(6). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4677594/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levitt NS, Steyn K, Dave J, Bradshaw D. Chronic noncommunicable diseases and HIV-AIDS on a collision course: relevance for health care delivery, particularly in low-resource settings--insights from South Africa. Am J Clin Nutr 2011. December;94(6):1690S–1696S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991–1999. Am J Public Health 2002. March;92(3):371–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hainsworth EG, Shahmanesh M, Stevenson F. Exploring the views and experiences of HIV positive patients treated for cancer: a systematic review of the literature. AIDS Care 2018;30(5):535–43. [DOI] [PubMed] [Google Scholar]
- 17.Nightingale VR, Sher TG, Mattson M, Thilges S, Hansen NB. The Effects of Traumatic Stressors and HIV-Related Trauma Symptoms on Health and Health Related Quality of Life. AIDS Behav 2011. November;15(8):1870–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.HRSA. HRSA Care Action [Internet] Rockville, MD: Health Resources and Services Administration; 2015. January. Available from: https://hab.hrsa.gov/sites/default/files/hab/Publications/careactionnewsletter/mentalhealth.pdf [Google Scholar]
- 19.Taylor BS, Fornos L, Tarbutton J, Muñoz J, Saber JA, Bullock D, et al. Improving HIV Care Engagement in the South from the Patient and Provider Perspective: The Role of Stigma, Social Support, and Shared Decision-Making. AIDS Patient Care STDS 2018;32(9):368–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tran BX, Phan HT, Latkin CA, Nguyen HLT, Hoang CL, Ho CSH, et al. Understanding Global HIV Stigma and Discrimination: Are Contextual Factors Sufficiently Studied? (GAPRESEARCH). Int J Environ Res Public Health [Internet] 2019. June [cited 2020 Feb 12];16(11). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6603743/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Casper C, Crane H, Menon M, Money D. HIV/AIDS Comorbidities: Impact on Cancer, Noncommunicable Diseases, and Reproductive Health. In: Holmes KK, Bertozzi S, Bloom BR, Jha P, editors. Major Infectious Diseases [Internet] 3rd ed. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017. [cited 2019 Jun 14]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK525185/ [PubMed] [Google Scholar]
- 22.Pellowski JA, Kalichman SC, Matthews KA, Adler N. A pandemic of the poor: social disadvantage and the U.S. HIV epidemic. Am Psychol 2013;68(4):197–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hightow-Weidman L, LeGrand S, Choi SK, Egger J, Hurt CB, Muessig KE. Exploring the HIV continuum of care among young black MSM. PLOS ONE 2017. June 29;12(6):e0179688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nyblade L, Stockton MA, Giger K, Bond V, Ekstrand ML, Lean RM, et al. Stigma in health facilities: why it matters and how we can change it. BMC Medicine 2019. February 15;17(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Turan B, Budhwani H, Fazeli PL, Browning WR, Raper JL, Mugavero MJ, et al. How Does Stigma Affect People Living with HIV? The Mediating Roles of Internalized and Anticipated HIV Stigma in the Effects of Perceived Community Stigma on Health and Psychosocial Outcomes. AIDS Behav 2017. January;21(1):283–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de la Torre-Luque A, Gambara H, López E, Cruzado JA. Psychological treatments to improve quality of life in cancer contexts: A meta-analysis. Int J Clin Health Psychol 2016. May 1;16(2):211–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rooks-Peck CR, Adegbite AH, Wichser ME, Ramshaw R, Mullins MM, Higa D, et al. Mental Health and Retention in HIV Care: A Systematic Review and Meta-Analysis. Health Psychol 2018. June;37(6):574–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.CDC. HIV in the United States and Dependent Areas [Internet] Atlanta, GA: Centers for Disease Control and Prevention; 2019. p. 2. Available from: www.cdc.gov/hiv/pdf/statistics/overview/cdc-hiv-us-ataglance.pdf [Google Scholar]
- 29.O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for Reporting Qualitative Research: A Synthesis of Recommendations. Academic Medicine 2014. September;89(9):1245. [DOI] [PubMed] [Google Scholar]
- 30.Suneja G, Boyer M, Yehia BR, Shiels MS, Engels EA, Bekelman JE, et al. Cancer Treatment in Patients With HIV Infection and Non-AIDS-Defining Cancers: A Survey of US Oncologists. J Oncol Pract 2015. May;11(3):e380–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 1995. March;36(1):1–10. [PubMed] [Google Scholar]
- 32.Iwelunmor J, Newsome V, Airhihenbuwa CO. Framing the impact of culture on health: a systematic review of the PEN-3 cultural model and its application in public health research and interventions. Ethn Health 2014. February;19(1):20–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q 1988;15(2):175–83. [DOI] [PubMed] [Google Scholar]
- 34.Guest G, MacQueen KM, Namey EE. Applied Thematic Analysis Thousand Oaks, CA: SAGE; 2012. [Google Scholar]
- 35.Boeije H A Purposeful Approach to the Constant Comparative Method in the Analysis of Qualitative Interviews. Quality & Quantity 2002. November 1;36(4):391–409. [Google Scholar]
- 36.Birks M, Chapman Y, Francis K. Memoing in qualitative research: Probing data and processes. Journal of Research in Nursing 2008. January 1;13(1):68–75. [Google Scholar]
- 37.Campbell JL, Quincy C, Osserman J, Pedersen OK. Coding In-depth Semistructured Interviews: Problems of Unitization and Intercoder Reliability and Agreement. Sociological Methods & Research 2013. August 1;42(3):294–320. [Google Scholar]
- 38.Harris LM, Emlet CA, Pierpaoli Parker C, Furlotte C. Timing of Diagnosis: Understanding Resilience Narratives of HIV Positive Older Adults Diagnosed Pre- and Post-HAART. Journal of Gerontological Social Work; London 2018. January;61(1):78–103. [DOI] [PubMed] [Google Scholar]
- 39.Hainsworth EG, Shahmanesh M, Stevenson F. HIV positive and treated for cancer: The convergence of pressures “invisible” in HIV and “visible” in cancer. Eur J Cancer Care (Engl) 2020. May;29(3):e13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mayer KH, Torres HA, Mulanovich V. Management of HIV Infection in Patients With Cancer Receiving Chemotherapy. Clin Infect Dis 2014. July 1;59(1):106–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.ASCO. HIV-Infected People With Early-Stage Cancers Are Up to Four Times More Likely to Go Untreated for Cancer - The ASCO Post [Internet] Alexandria, VA: American Society of Clinical Oncologists; 2014. Available from: https://www.ascopost.com/News/17361 [Google Scholar]
- 42.Scheurer D, Choudhry N, Swanton KA, Matlin O, Shrank W. Association between different types of social support and medication adherence. Am J Manag Care 2012. December 1;18(12):e461–467. [PubMed] [Google Scholar]
- 43.Dulin AJ, Dale SK, Earnshaw VA, Fava JL, Mugavero MJ, Napravnik S, et al. Resilience and HIV: a review of the definition and study of resilience. AIDS Care 2018. August 23;30(sup5):S6–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Seiler A, Jenewein J. Resilience in Cancer Patients. Front Psychiatry [Internet] 2019. April 5 [cited 2019 Aug 24];10. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6460045/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Molina Y, Yi JC, Martinez-Gutierrez J, Reding KW, Yi-Frazier JP, Rosenberg AR. Resilience Among Patients Across the Cancer Continuum: Diverse Perspectives. Clin J Oncol Nurs 2014. February;18(1):93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]


