Abstract
Recently cases of vaccine-induced immune thrombotic thrombocytopenia (VITT) and thrombosis following the adenoviral vector vaccine against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were reported. A mechanism similar to heparin-induced thrombocytopenia was proposed with antibodies to platelet factor 4 (PF4). Vaccine related arterial thrombosis in the brain is rare but life-threatening and optimal treatment is not established. We report clinical, laboratory, imaging findings and treatment in a 51-year-old female presenting with acute left middle cerebral artery (MCA) occlusion 7 days after the first dose of ChAdOx1 nCoV-19 vaccine. Due to low platelet count and suspicion of VITT she was not eligible for intravenous thrombolysis (IVT) and proceeded to mechanical thrombectomy (MER) with successful recanalization four hours after onset of symptoms. Treatment with intravenous immunoglobulin (IVIG) and heparin pentasaccharide fondaparinux was initiated. Presence of anti-PF4 antibodies was confirmed. The patient improved clinically with normalization of platelet count. Clinicians should be alert of VITT in patients with acute ischemic stroke after ChAdOx1 nCov-19 vaccination and low platelet counts. MER showed to be feasible and effective. We propose considering MER in patients with VITT and large vessel occlusion despite thrombocytopenia. High-dose IVIG should be started immediately. Alternative anticoagulation to heparin should be started 24 hours after stroke onset unless significant hemorrhagic transformation occurred. Platelet transfusion is contraindicated and should be considered only in severe hemorrhagic complications. Restenosis or reocclusion of the revascularized artery is possible due to the hypercoagulable state in VITT and angiographic surveillance after the procedure is reasonable.
Key Words: Stroke, VITT, Mechanical thrombectomy, Thrombocytopenia
Background and purpose
Recently a rare vaccine-related variant of a prothrombotic disorder that clinically resembles spontaneous heparin-induced thrombocytopenia (HIT) has been identified, referred to as vaccine-induced immune thrombotic thrombocytopenia (VITT).1 , 2 An immune mechanism of thrombotic events following vaccination with ChAdOx1 nCoV-19 was proposed, with the identification of anti-PF4 antibodies without previous heparin exposure.3 Most of the patients with cerebral thrombotic events and thrombocytopenia presented with cerebral venous thrombosis,4 to our knowledge there are eleven cases of patients who suffered an acute ischemic stroke reported.3 , 5, 6, 7, 8, 9 Vaccine related arterial thrombosis in the brain is exceedingly rare but potentially a life-threatening situation and the best choice of treatment is yet to be established.
Methods
We report clinical, laboratory and imaging findings along with choice of treatment in a patient, who presented with left middle cerebral artery (MCA) occlusion and thrombocytopenia 7 days after receiving the first dose of the coronavirus disease-19 (COVID-19) vaccine ChAdOx1 nCoV-19. Patient was urgently treated with mechanical thrombectomy (MER) and high-dose intravenous immunoglobulin (IVIG). We used a standard enzyme-linked immunosorbent assay (ELISA) (HAT45G®, Immucor) to detect anti-PF4 antibodies.
Results
Female patient, age 51, previously treated for hyperlipidemia presented to neurology emergency 2 hours after acute onset of global aphasia, right sided hemiplegia and hemianopsia (National Institutes of Health Stroke Scale – NIHSS 20, modified Rankin Scale – mRS 5). Seven days before she received the first dose of the ChAdOx1 nCoV-19 vaccine. A day before admission she had been experiencing fatigue, chills and mildly increased temperature (37,1 °C). SARS-CoV-2 reverse-transcriptase-polymerase-chain-reaction assay of a nasopharyngeal swab was negative.
Due to high clinical suspicion of acute ischemic stroke in left MCA territory and onset of symptoms within the time window, the protocol for intravenous thrombolysis (IVT) with tissue plasminogen activator was started.
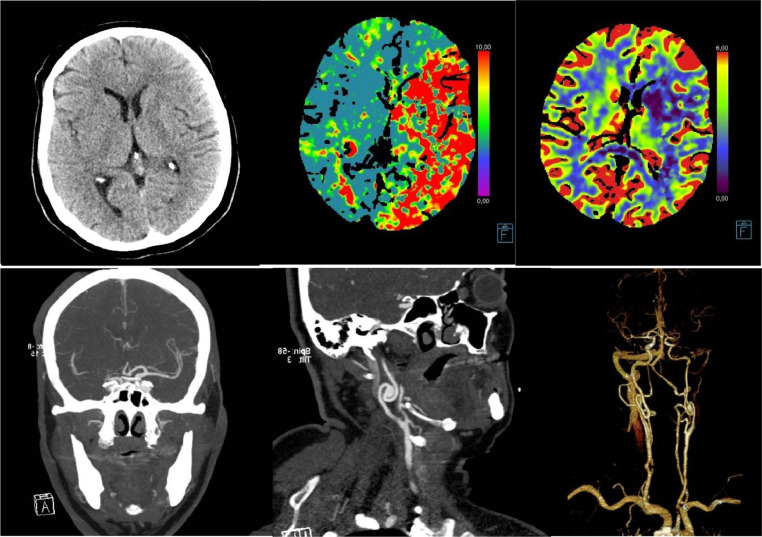
Head computed tomography (CT) showed just minor early ischemic changes in the left basal ganglia and insula, ASPECT (Alberta stroke programme early CT) score of 7. CT perfusion imaging revealed decreased perfusion of most of the left MCA territory with significant mismatch between infarct core and penumbra. Computed tomography angiography (CTA) revealed an occlusion of the proximal left M1 segment of MCA. Additionally, extreme tortuosity and chronic dissection of the proximal left internal carotid artery (ICA) with 10 mm pseudoaneurysm was present (Fig. 1 ).
Fig. 1.
Head CT and CT perfusion – TTP (time to peak) and CBV (cerebral blood volume); CTA – left M1 occlusion and chronic left ICA dissection with pseudoaneurysm.
According to the current guidelines, the patient was eligible for IVT, but laboratory results revealed low platelets (57 × 109/L), highly elevated D-dimer and mildly elevated fibrinogen (Table 1 ). Due to low platelet count IVT was contraindicated. We decided not to correct platelet count by platelet transfusion due to first reports of possible VITT and the risk of worsening the prothrombotic state and progression of cerebral arterial thrombosis. The patient was urgently treated with MER.
Table 1.
Time course table of laboratory characteristics during admission and after 3 months.
| Day | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 12 | 100 |
|---|---|---|---|---|---|---|---|---|---|
| Platelet count (109/L) reference value (150-410) |
57 | 54 | 62 | 65 | 88 | 128 | 165 | 200 | |
| D-dimer (µg/L) reference value (<500) | 31543 | 35603 | 35783 | 25854 | 23839 | 891 | |||
| anti-PF4 antibodies ELISA | positive high titer | positive lower titer | |||||||
| PF4-dependent platelet-activation assay | positive | negative |
The procedure was performed under general anesthesia. The 0.021 inch microcatheter (Haedway 21, Microvention) was advanced past the thrombus over the 0.014 inch microwire (Synchro 14, Stryker) and the large-bore aspiration catheter was advanced close to the proximal aspect of the thrombus. The stent-retriever (Trevo XP 4 × 20 mm) was then deployed across the thrombus and gently pulled into the aspiration catheter. After the first pass of the stent-retriever successful complete reperfusion (Thrombolysis In Cerebral Infarction – TICI 3) was achieved, four hours after symptoms onset (Fig. 2 ).
Fig. 2.
Digital subtraction angiography – left M1 segment occlusion; recanalisation of left M1 segment; chronic left ICA dissection with pseudoaneurysm.
Following the procedure, the patient was considered at very high risk for reperfusion related hemorrhagic complications due to low platelet count and was therefore closely monitored. Blood pressure was held strictly between 100–130/80 mmHg and vigorous intravenous hydration was commenced (0.9% sodium chloride solution 200 mL/h). Four and a half hours after symptoms onset, she received high-dose IVIG (1g/kg for two consecutive days – 90 g/day).
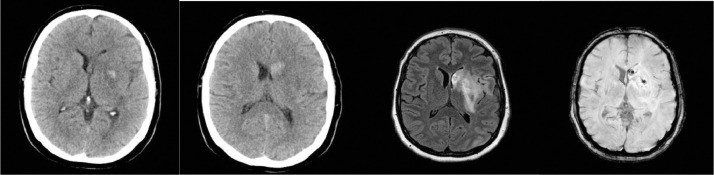
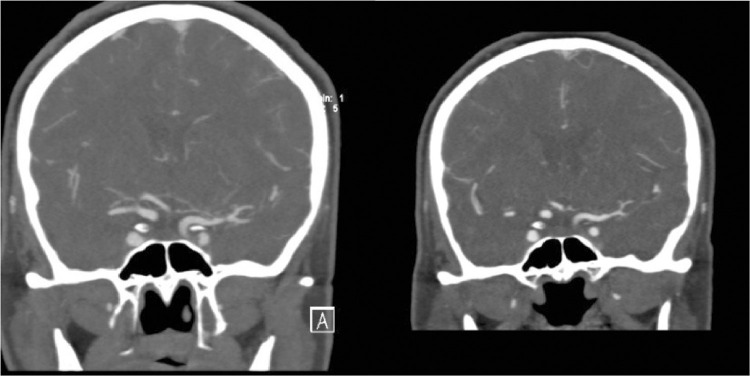
Head CT scan the next day, 24 hours after the treatment, showed small area of MCA territory infarction in basal ganglia and corona radiata with mild hemorrhagic transformation (Fig. 3 ). The patient improved clinically to a moderate motor dysphasia, mild right-sided hemiparesis and partial right-sided hemianopsia. Standard ELISA detected high levels of anti-PF4 antibodies and test for PF4–enhanced platelet-activation showed strong activation. Tests for thrombophilia, antinuclear antibodies, extractable nuclear antigen and antiphospholipid antibodies were negative. Also, holter electrocardiogram, echocardiogram and chest radiograph were unremarkable. Fondaparinux 2,5 mg subcutaneously was introduced 24 hours after MER and continued every 24 hours. On surveillance head magnetic resonance imaging (MRI) nine days after starting anticoagulation treatment no progression of hemorrhagic transformation was noted (Fig. 3). Platelet count gradually increased and normalized after six days and remained stable afterwards (Table 1). On eleventh day surveillance transcranial color duplex sonography (TCCD) and further on intracranial CTA revealed 80–90% restenosis of left M1 segment, which almost completely resolved by the 18th day (Fig. 4 ). After normalization of platelet count, D-dimer levels and regression of stenosis, fondaparinux was discontinued after 17 days and acetylsalicylic acid 100 mg per day was introduced. Moreover, after 2 weeks reduced levels of anti-PF4 antibodies with ELISA were noted and also reduced PF4–enhanced platelet-activation (Table 1). Patient's state improved throughout the hospitalization, she was discharged to a rehabilitation unit with mild motor dysphasia, discrete right arm paresis and partial right hemianopsia (NIHSS 4, mRS 2). Platelet count was monitored every week for the first month and every second week afterwards, values were normal. On surveillance TCCD after one and three months normal flow velocities in proximal left MCA were recorded. After three months on examination only mild difficulties with fine movements of right hand and partial right hemianopsia, less extensive than at discharge, were noted (NIHSS 1, mRS 1), platelet count was normal, D-dimer still mildly elevated (Table 1).
Fig. 3.
Head CT 24 hours after MER – small area of MCA territory infarction with mild hemorrhagic transformation. Surveillance head MRI on day 10, nine days after fondaparinoux was started (fluid attenuated inversion recovery – FLAIR and susceptibility weighted imaging – SWI sequence) shows no progression of hemorrhagic transformation.
Fig. 4.
CTA performed on day 11 shows 80–90% restenosis of left M1 segment and subsequent resolution of stenosis on CTA performed on day 18, 17 days after introducing anticoagulant treatment.
Discussion
VITT usually occurs 1 to 2 weeks after vaccination with ChAdOx1 nCoV-19 and lately reports emerged for other adenoviral COVID-19 vaccines including Ad26.COV2.S.10 The thrombosis is likely caused by platelet-activating antibodies against PF4 produced after vaccination. Whether the adenoviral vector, free DNA or other substances alone or by interaction with platelets or with PF4 play a causative role in antibodies formation is currently not known.1 , 2 Regarding the similarities to HIT alternative anticoagulation to heparin should be used and platelet transfusions given only for lifesaving procedures.
ChAdOx1 nCoV-19 associated VITT usually occurs in the venous system, but as in our patient, can result also in acute ischemic stroke. To our knowledge, eleven patients with ischemic stroke in MCA territory were noted. Two in case series published in The New England Journal of Medicine by Scully M. et al, however no data regarding presentation nor specific treatment was described. Two more cases were published where ischemic stroke was not the initial presentation, in one patient it developed after bilateral superior ophthalmic vein thrombosis and in the other one after bilateral adrenal hemorrhages was diagnosed.5 , 6 Additionally, three cases of younger patients who presented with infarcts in MCA territory.9 However, neither of those five cases received reperfusion therapy. Recently a case of a patient who presented with acute ischemic stroke and was also treated with MER with good clinical outcome was published7 and another two cases who suffered a malignant MCA territory infarction despite thrombectomy.8 One case of a patient with acute MCA occlusion due to embolization of nonocclusive thrombus in ICA was described who was treated successfully with IVT, since platelet count on admission was still normal.11 In our patient pseudoaneurysm of left ICA, with reduced blood flow, could contribute to thrombus formation in arterial system, which then embolized distally.
As in all cases of acute ischemic stroke, time to reperfusion should be as short as possible. In this scenario, it is particularly important to minimize the stroke volume and hemorrhagic transformation, since anticoagulation treatment is essential and must be started as soon as possible to avoid other thrombotic complications. On the other hand, hemorrhagic complications of ischemic stroke can be devastating in patients with low platelets and anticoagulation, especially in circumstances where platelet transfusion is contraindicated. Data on management of patients with acute ischemic stroke and thrombocytopenia are limited, since patients with significant thrombocytopenia (<100 × 109/L) were consistently excluded from all major acute ischemic stroke clinical trials and it is also an absolute contraindication for IVT. By reviewing trials and bringing together the information about patients with significant thrombocytopenia who received IVT the risk for symptomatic intracerebral hemorrhage (sICH) was 7%, compared to the range of 2–7% in patients without thrombocytopenia.12 , 13 Though, the sample size was very small and the cause of thrombocytopenia was mostly not specified. In MER studies lower platelet counts were used (Multi-MERCI <30 × 109/L, MR-CLEAN <40 × 109/L, SWIFT PRIME and EXTEND IA <100 × 109/L, DAWN and DEFUSE-3 <50 × 109/L), but only one study of small subgroup of patients (n=35) with abnormal hemostasis was made and did not show increased risk for sICH, however decreased rates of good outcome were noted.14 There is scarce data on treatment of patients with immune thrombocytopenia (ITP) and acute ischemic stroke. Two cases of patients with ITP and acute ischemic stroke treated with IVT and MER were reported. One had a favorable outcome, with platelet count 48 × 109/L on presentation and the other one had sICH 2 hours after treatment even though his platelet count was 366 × 109/L on admission.12 Our case shows that stroke due to large vessel occlusion in a patient with VITT can be successfully treated with MER and also in concordance with the available data should be the treatment of choice. It should be noted that intravascular catheters used during the procedure should not be flushed with heparin, instead argatroban, bivalirudin or danaparoid could be the alternatives.
Treatment with high-dose IVIG has been shown to inhibit antibody mediated platelet activation, leading to decreased hypercoagulability, a rapid increase in platelet count and has also been proposed as part of VITT therapy.15 , 16 Treatment with IVIG in our patient led to prompt normalization of platelet count and a decrease of D-dimer, representing an improvement in the hypercoagulable state (Table 1).
Platelet transfusion is considered contraindicated because of the risk of additionally sustaining the prothombotic state and thereby worsening symptoms. Due to stable platelet count above 50 × 109/L and no significant hemorrhagic transformation, the patient did not receive platelet transfusion despite anticoagulant treatment with fondaparinux. Reports from patients with HIT receiving platelets show a good safety profile with a low risk of further thrombosis.17 Whether the same is true for patients with VITT is not known, but platelet transfusion should be considered only in lifesaving procedures and in patients with bleeding complications.
Further on, during MER some vascular damage occurs with injury of intimal layer, which in prothrombotic state can lead to rethrombosis with subsequent restenosis or even reocclusion.8 , 18 In our case we documented asymptomatic 80–90% restenosis of left M1 segment of MCA after MER, which regressed completely with anticoagulant treatment. This again illustrates the importance of introducing anticoagulant treatment as soon as possible.
As in autoimmune HIT it is advised to avoid treatment with standard heparin or low-molecular weight heparin, we treated the patient with indirect factor Xa (FXa) inhibitor fondaparinux. Other alternative anticoagulants could be used, namely danaparoid, which is applied in continuous infusion and requires monitoring of anti-activated FXa. Direct thrombin inhibitors can be considered, argatroban, bivalirudin, which are also given intravenously and necessitate monitoring of activated partial thromboplastin time. Their short duration of therapeutic effect can be useful in situations with high bleeding risk, need for surgery or invasive procedures. Recently direct oral anticoagulants, apixaban, rivaroxaban, dabigatran are arising as additional therapeutic option, being easy to administer and require no monitoring, yet data on use in HIT is still limited.19, 20, 21 We decided to use fondaprinux because it is administered once daily, does not need monitoring and danaparoid is not available in our country. After achieving normal platelet count and D-dimer we substituted fondaparinux for acetylsalicylic acid to further reduce the risk for intracranial hemorrhagic complications. Even with antiaggregation therapy no additional thrombosis or worsening of platelet count or D-dimer values were noted.
Conclusion
This case demonstrates that acute stroke due to large vessel occlusion in patient with VITT can be safely and successfully treated with MER. We propose that MER is preferred to IVT where feasible. It is important to avoid using heparin throughout the procedure, since it could worsen the hypercoagulable state. Prompt treatment with high-dose IVIG is essential to achieve platelet stabilization and avoid hemorrhagic complications of stroke. Platelet transfusion should be avoided if possible and considered only in cases of severe hemorrhagic complications. Alternative anticoagulation treatment to heparin in therapeutic doses should be started 24 hours after MER in case of small or medium stroke volume and in the absence of significant hemorrhagic transformation. Restenosis or reocclusion of revascularized artery is possible and could be more frequent due to hypercoagulable state, angiographic surveillance in first two weeks after the procedure is reasonable.
Declarations of interest
None.
References
- 1.Greinacher A, Thiele T, Warkentin TE, et al. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N Engl J Med. 2021;384(22):2092–2101. doi: 10.1056/NEJMoa2104840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schultz NH, Sørvoll IH, Michelsen AE, et al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV-19 vaccination. N Engl J Med. 2021;384(22):2124–2130. doi: 10.1056/NEJMoa2104882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scully M, Singh D, Lown R, et al. Pathologic antibodies to platelet factor 4 after ChAdOx1 nCoV-19 vaccination. N Engl J Med. 2021;384(23):2202–2211. doi: 10.1056/NEJMoa2105385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Franchini M, Testa S, Pezzo M, et al. Cerebral venous thrombosis and thrombocytopenia post-COVID-19 vaccination. Thromb Res. 2021;202:182–183. doi: 10.1016/j.thromres.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blauenfeldt RA, Kristensen SR, Ernstsen SL, et al. Thrombocytopenia with acute ischemic stroke and bleeding in a patient newly vaccinated with an adenoviral vector-based COVID-19 vaccine. J Thromb Haemost JTH. 2021;19(7):1771–1775. doi: 10.1111/jth.15347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bayas A, Menacher M, Christ M, et al. Bilateral superior ophthalmic vein thrombosis, ischaemic stroke, and immune thrombocytopenia after ChAdOx1 nCoV-19 vaccination. Lancet Lond Engl. 2021;397(10285):e11. doi: 10.1016/S0140-6736(21)00872-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costentin G, Ozkul-Wermester O, Triquenot A, et al. Acute Ischemic Stroke Revealing ChAdOx1 nCov-19 Vaccine-Induced Immune Thrombotic Thrombocytopenia: Impact on Recanalization Strategy. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc. 2021;30(9) doi: 10.1016/j.jstrokecerebrovasdis.2021.105942. [DOI] [PubMed] [Google Scholar]
- 8.De Michele M, Iacobucci M, Chistolini A, et al. Malignant cerebral infarction after ChAdOx1 nCov-19 vaccination: a catastrophic variant of vaccine-induced immune thrombotic thrombocytopenia. Nat Commun. 2021;12(1):4663. doi: 10.1038/s41467-021-25010-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Mayhani T, Saber S, Stubbs MJ, et al. Ischaemic stroke as a presenting feature of ChAdOx1 nCoV-19 vaccine-induced immune thrombotic thrombocytopenia. J Neurol Neurosurg Psychiatry. 2021 doi: 10.1136/jnnp-2021-326984. jnnp-2021-326984. [DOI] [PubMed] [Google Scholar]
- 10.Muir K-L, Kallam A, Koepsell SA, Gundabolu K. Thrombotic thrombocytopenia after Ad26.COV2.S vaccination. N Engl J Med. 2021;384(20):1964–1965. doi: 10.1056/NEJMc2105869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walter U, Fuchs M, Grossmann A, et al. Adenovirus-Vectored COVID-19 vaccine-induced immune thrombosis of carotid artery: a case report. Neurology. 2021 doi: 10.1212/WNL.0000000000012576. [DOI] [PubMed] [Google Scholar]
- 12.Alrohimi A, Purdy K, Alqarni M, et al. The clinical conundrum of managing ischemic stroke in patients with immune thrombocytopenia. Can J Neurol Sci J Can Sci Neurol. 2021;48(1):38–46. doi: 10.1017/cjn.2020.138. [DOI] [PubMed] [Google Scholar]
- 13.Seet RCS, Rabinstein AA. Symptomatic intracranial hemorrhage following intravenous thrombolysis for acute ischemic stroke: a critical review of case definitions. Cerebrovasc Dis Basel Switz. 2012;34(2):106–114. doi: 10.1159/000339675. [DOI] [PubMed] [Google Scholar]
- 14.Nogueira RG, Smith WS, MERCI and Multi MERCI Writing Committee Safety and efficacy of endovascular thrombectomy in patients with abnormal hemostasis: pooled analysis of the MERCI and multi MERCI trials. Stroke. 2009;40(2):516–522. doi: 10.1161/STROKEAHA.108.525089. [DOI] [PubMed] [Google Scholar]
- 15.Tsilingiris D, Vallianou NG, Karampela I, Dalamaga M. Vaccine induced thrombotic thrombocytopenia: The shady chapter of a success story. Metab Open. 2021;11 doi: 10.1016/j.metop.2021.100101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arepally GM, Ortel TL. Vaccine-induced immune thrombotic thrombocytopenia: what we know and do not know. Blood. 2021;138(4):293–298. doi: 10.1182/blood.2021012152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Refaai MA, Chuang C, Menegus M, et al. Outcomes after platelet transfusion in patients with heparin-induced thrombocytopenia. J Thromb Haemost JTH. 2010;8(6):1419–1421. doi: 10.1111/j.1538-7836.2010.03861.x. [DOI] [PubMed] [Google Scholar]
- 18.Mereuta OM, Abbasi M, Fitzgerald S, et al. Histological evaluation of acute ischemic stroke thrombi may indicate the occurrence of vessel wall injury during mechanical thrombectomy. J Neurointerventional Surg. 2021 doi: 10.1136/neurintsurg-2021-017310. neurintsurg-2021-017310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hogan M, Berger JS. Heparin-induced thrombocytopenia (HIT): Review of incidence, diagnosis, and management. Vasc Med Lond Engl. 2020;25(2):160–173. doi: 10.1177/1358863X19898253. [DOI] [PubMed] [Google Scholar]
- 20.Greinacher A, Selleng K, Warkentin TE. Autoimmune heparin-induced thrombocytopenia. J Thromb Haemost JTH. 2017;15(11):2099–2114. doi: 10.1111/jth.13813. [DOI] [PubMed] [Google Scholar]
- 21.Jaax ME, Greinacher A. Management of heparin-induced thrombocytopenia. Expert Opin Pharmacother. 2012;13(7):987–1006. doi: 10.1517/14656566.2012.678834. [DOI] [PubMed] [Google Scholar]