Abstract
SARS-CoV-2, a betacoronavirus of likely zoonotic origin, was first reported in December 2019. Its rapid worldwide spread precipitated a range of interventions, including by veterinarians, due to impacts on human health and well-being as well as animal health and welfare. We conducted 36 key informant interviews to explore the responses of Australian veterinarians, their engagement in One Health collaboration and cooperation, and their existing and developed insights to the COVID-19 pandemic. Responses were analysed using thematic analysis. Australian veterinarians provided valuable contributions to the national COVID-19 response by protecting animal welfare, maintaining local food security, providing essential veterinary services while mitigating human health risks in clinical settings and providing both key skills and surge capacity to the human health response. This was all guided by skills in scientific literacy and evidence-based communication. Informants identified a clear and urgent need for greater One Health coordination during pandemic prevention, preparedness, and response, even in the case of a disease which largely only affects humans.
Keywords: One Health, Global health security, COVID-19, Veterinarian, Preparedness, Response, Public health
Highlights
-
•
Veterinarians provided key skills and surge capacity in epidemiology and laboratory analysis within the national COVID-19 response.
-
•
Maintenance of veterinary services assisted pet owners, many of whom saw their pets as a source of emotional and physical support during the pandemic.
-
•
Veterinarians identified an urgent need for improved One Health coordination to strengthen preparedness and response to future pandemic.
-
•
Both intra- and inter-professional silos were recognised as perpetual obstacles to operationalising One Health.
1. Introduction
COVID-19, the disease caused by the betacoronavirus SARS-CoV-2, was first reported in Wuhan, China in December 2019 [1]. Worldwide spread was rapid thereafter, with the World Health Organisation (WHO) declaring a pandemic on March 11, 2020 [2]. Initial public health responses were reliant on non-pharmaceutical interventions which were executed with variable stringency and efficacy in different countries [3,4]. Concentrated worldwide efforts in vaccine development resulted in the first vaccination program being launched in Britain in December 2020 [5]. By mid-August 2021, worldwide cases were approaching 210 million with 4.41 million reported deaths [6].
Australia is one of few countries in the world that has – as of the time of writing – been largely effective in limiting the number of cases and deaths caused by COVID-19. This was achieved through a swift and strong public health response early in the pandemic [4] as well as during a ‘second wave’ of infections in the state of Victoria [7]. The first Australian case of COVID-19 was reported on 25 January 2020 [8] with the Australian Prime Minister declaring a pandemic before the WHO, on 27 February [9]. With increasing community transmission, Australian national borders were closed to all non-citizens and non-residents on 20 March 2020 to decrease risk of importation of the virus by international travellers and enable health authorities to contain local outbreaks [10]. Concurrent social distancing and self-isolation requirements were introduced along with strict travel restrictions into remote indigenous communities [11], establishment of border restrictions by most state and territory governments [8] and limitations to all but essential services by federal government [11]. These measures were highly effective in controlling COVID-19 throughout much of the pandemic; following the incursion of the Delta variant in mid-2021, the virus has proved more challenging to contain [12].
While the original source of the virus is yet to be confirmed, most scientists agree that SARS-CoV-2 is of zoonotic origin with bats being the likely reservoir host [13,14]. To date, the existence and species of any intermediate host remains unknown [14]. The first cases of SARS-CoV-2 in domestic animals were detected in a dog in Hong Kong in February 2020 [15], followed by a cat in Belgium in March 2020 [16]; both were assessed to be the result of transmission from humans to animals. Nonetheless, this gave rise to questions regarding the ongoing zoonotic potential of the virus, particularly in species such as cats and ferrets which have ACE2 receptors, the binding site for the spike protein on SARS-CoV-2 [17].
Given the clear links to animal health, the COVID-19 pandemic prompted early actions and reactions by the veterinary profession in many countries. Actions by veterinarians included those taken in response to animal health and welfare concerns [18] as well as public health impacts [19]; leveraging veterinary laboratories to provide extra diagnostic capacity; and redirecting veterinary medical equipment to hospitals [20]. Professional associations and researchers investigated the effects of COVID-19 on veterinary practices [21] and veterinary-related concerns of dog owners [22]. Some veterinarians offered critical opinions of the national response to COVID-19 in their country, suggesting the experience of the profession in population medicine and management of large disease outbreaks gave them insights that should have been drawn on by their local health authorities [23]. Others shared perspectives on the advantages of veterinary engagement in a One Health response to COVID-19 in areas such as food security, comparative medicine and vaccine development, as well as surveillance and epidemiological outbreak modelling [20,[24], [25], [26], [27], [28]].
While some narrative descriptions of veterinary responses to COVID-19 have been published [[18], [19], [20]], as yet no studies have systematically collected data on the contributions and experiences of individual veterinarians, as well as the range of issues faced by the veterinary profession during the pandemic. We conducted key informant interviews of Australian veterinary professionals from both clinical and non-clinical roles in order to: 1) identify the range of contributions, relevant skills and motivations for engaging in the response; 2) characterise the extent of One Health collaboration and cooperation; and 3) discover existing and developed insights into preparedness and response to COVID-19 and future pandemics.
2. Methods
This study utilised qualitative research methods. Data were collected using key informant interviews and research reported using criteria outlined in the COREQ checklist [29]. Approval for the project was granted by the University of Sydney human ethics committee (project number 2020/442).
Interviews were conducted between August and October 2020 by SS, a One Health researcher with qualifications in both veterinary science and public health. SS is a committee member of the Veterinary Public Health (VPH) Special Interest Group (SIG) of the Australian Veterinary Association (AVA) and contributed to the AVA COVID-19 working group. She is also a committee member of the One Health SIG of the Public Health Association of Australia and a co-moderator of the Australian Veterinarians in Public Health (AVPH) Facebook group. Due to both her previous research [[30], [31], [32]] and active involvement in One Health, VPH and clinical veterinary practice in Australia, SS was either known, or known of, by many informants in the study. The other members of the research team, SM and JAT, are veterinary epidemiologists and academics engaged in One Health and VPH who are also known or familiar to a number of study informants.
Informants were selected purposefully by the research team and included Australian-based veterinarians who were known to have taken actions in response to COVID-19, either as an individual or as representative members or employees of stakeholder groups. Some key individuals suggested by interviewees were also approached to participate in the study (snowball sampling).
Informants were from across Australia; more were selected from Victoria and New South Wales (NSW) due to the larger impact of COVID-19 within these states which generated a greater involvement by veterinarians in these locations. We endeavoured to recruit representatives from clinical and non-clinical roles, as well as a range of major stakeholder groups to gain insight into the scope of response made by veterinarians to COVID-19.
Invitations were sent by email to potential informants with an explanation of the interview process and purpose of the study, with a request to contact SS if they wished to participate. Email contact was used initially as a way to standardize communication and minimise coercion in the presence of relationships between the researchers and informants. A second email was sent after two weeks if no response was made, followed up by phone in a small number of cases. Fifty-two invitations were sent and 36 informants agreed to participate in the study; ten people did not respond, three suggested another member of their organisation and three declined to participate. The final sample size was determined by a combination of factors; the desire to explore the breadth of response by a diverse cohort of veterinarians, time constraints in conducting the study, the volume of data generated and finally, recognition of common concepts and ideas recurring during the interviews.
Interviews were semi-structured using 10 open ended questions, with additional prompts to enable clarification where necessary. The interview questions covered the informant's experiences, challenges, motivations and insights from their response to COVID-19. The interview guide can be found in the supplementary material. Three trial interviews with veterinarians from clinical and non-clinical backgrounds were conducted before the study. Audio recordings were reviewed by an experienced medical anthropologist who provided feedback. Minor refinements were made to the questions and interview technique after this review. Interviews were conducted using video teleconferencing software (Zoom Video Communications, Inc.; San Jose, CA) by SS at a time convenient for the participant. An oral consent script was read out loud and agreed to by each participant before proceeding with the interview. Each interview began with the same question, with the order of subsequent questions guided by the flow of conversation. Interviews ranged in length between approximately 30 and 60 minutes. Interviews were recorded, with the audio file being retained and the video file being deleted as per the conditions of the ethics approval. Recordings were reviewed, with one interview being repeated after a partial failure of the recording. Interviews were transcribed using Otter.ai (Otter.ai Inc.; Los Altos, CA), a speech to text application, with accuracy subsequently checked against the audio recording by SS who edited as required. Informants were identified by a unique numerical code and transcripts de-identified to protect their identity. Interview transcripts were sent to all informants for comment and correction and audio recordings deleted once transcripts were reviewed, again as a condition of the ethics approval.
Data were analysed using principles of thematic analysis (TA) using an inductive approach [33,34]. Figure S1 shows the process of analysis and theme development and involvement of the researchers within each stage. Analysis was performed using both manual methods and NVivo V12.2.0 (QSR International; Melbourne, VIC). Initial coding and thematic development were performed in NVivo and then reviewed manually by reading transcripts and highlighting and collating data segments representative of developing themes. At each stage of the analysis the data were re-read by SS to ensure continuing representation of the data content during coding and development and refinement of themes, with regular discussion at team meetings. Agreement on final themes and subthemes was reached by the research team within the context of the aims of the study.
Participant quotations are used in the text, figures and tables to illustrate themes and subthemes. Quotations are in italics, with any alterations or insertions being identified by square brackets; the latter were made to ensure clarity and do not alter the meaning of the text. Quotations are identified by the participant's numerical code (V plus an assigned number based on order of interviews). A draft of the paper was forwarded to informants for comment, endeavouring to protect confidentiality where required and ensuring accurate representation of their comments within the manuscript.
3. Results
3.1. Informant backgrounds
Informants primary employment at the beginning of the COVID-19 pandemic was either in clinical veterinary roles (n = 11) or non-clinical (n = 24) roles, with one informant being retired, having previously been employed in a non-clinical role. Clinical veterinary roles included owners or employees from veterinary practices, corporate veterinary management, shelter medicine and zoo medicine. Non-clinical roles included veterinarians employed by federal and state animal health bodies, state public health departments, other government organisations, non-government organisations (NGO), and universities. Four informants primarily in non-clinical roles also did clinical work on a casual basis or as part of their employment.
3.2. Thematic analysis
Five main themes were identified from the interview data:
-
1.
Indirect impacts of COVID-19 on animal welfare and health;
-
2.
Managing human health in veterinary settings;
-
3.
Providing key skills and support to the public health response;
-
4.
Scientific literacy and communication; and
-
5.
Insights on pandemic preparedness
Within these themes, a number of subthemes further illustrated the diversity of responses and reflections by veterinarians within each area.
Themes 1–3 encapsulate the areas of response to COVID-19 by veterinarians and are reflective of their feelings, motivations, capacity and skills. Supporting this was an overarching requirement for scientific literacy and communication (Theme 4), as veterinarians saw a need to interpret, distil and disseminate the huge amounts of evolving information. Theme 5 describes reflections of veterinarians in response to the pandemic through the unique lens of their training and experience. Within these themes, a number of sub-themes further illustrate the diversity of response and reflections by veterinarians within each area.
3.2.1. Indirect impacts of COVID-19 on animal welfare and health
‘I thinkwe learned early on that the health of animals [is] unlikely to be impacted by [SARS-CoV-2].It's more the reliance animals have on the humans managing them and ensuring their health and safety. And…when you take away the humans from that equation, then you do[end up]with potential animal welfare concerns.’ (V20)
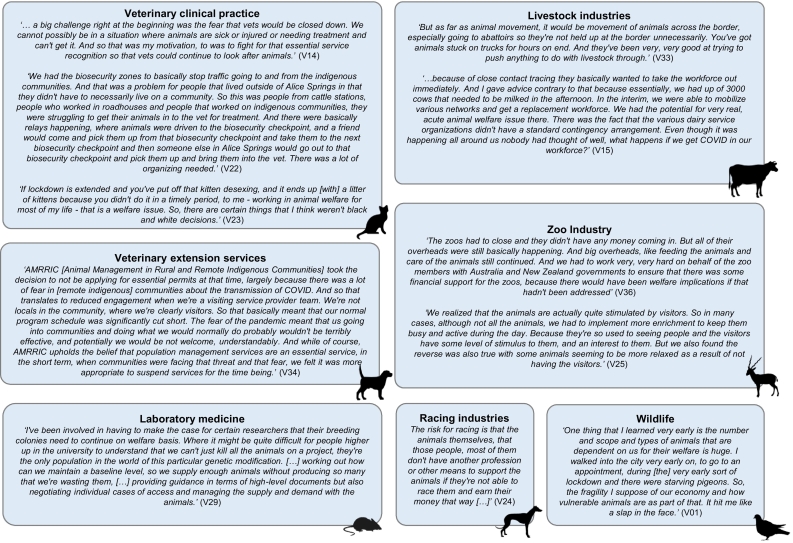
In Australia, lockdowns, state border closures and biosecurity bubbles implemented by the government as part of the public health response had unforeseen impacts on animal health and welfare. These unprecedented restrictions revealed the vulnerability of animals as a consequence of human movement restrictions and poor health. An overview of the impacts on animal industries as described by the informants is shown in Fig. 1.
Fig. 1.
Impacts of public health interventions and human health concerns due to COVID-19 on animal welfare and health as described by veterinary informants in Australia.
Informants rapidly became aware of the repercussions of human movement restrictions on a number of animal industries. Of significant concern was the lack of government clarity regarding the classification of veterinarians as essential services during initial national lockdowns, requiring advocacy by the Royal Society for the Prevention and Cruelty of Animals (RSPCA), AVA and government animal health bodies. The Victorian lockdown in particular produced uncertainty regarding continuity of animal health services including routine veterinary procedures and husbandry as well as management of stray animals. Further, animal welfare officers were forced to negotiate bureaucratic processes to obtain essential service permits to continue their work in universities. Some informants also voiced concerns for companion animals housed with owners under lockdown, particularly in high density housing, describing a lack of consideration of animal toileting, food, exercise and medical needs with no engagement of veterinarians in local health planning for such events.
Border closures restricted movement of many animal industry workers. In response, state-based multi-sectoral committees were rapidly formed, including representatives from livestock and racing industries, police and veterinarians from government and the RSPCA. Veterinarians on these committees provided weight to advocacy efforts facilitating free movement of animal transport workers and animal attendants across borders. This prevented delays in animal transport including horses during the breeding season and livestock such as cattle, sheep, pigs and poultry to abattoirs. Within these committees, stakeholders who are not typically aligned were unified with a common purpose of maintaining animal welfare and health. In addition, veterinarians servicing border communities or those with specialised skills were granted permission to move under public health orders.
Informants employed by the federal government described repercussions on agricultural industries caused by trade disruptions. These stemmed from the impacts of COVID-19 and associated restrictions on human populations overseas as well as trade sanctions imposed by China against Australia during the pandemic. Shortages of inputs such as agricultural chemicals and pharmaceuticals, particularly from manufacturing centres such as Wuhan, raised concerns about possible long-term consequences for animal health. Trade sanctions on exports of high-end perishable commodities left lobsters dying on the tarmac in China. Disruption of meat and dairy exports resulted in product being redirected to domestic markets and culling of animals due to decreased demand. This, alongside disruptions caused by COVID-19 outbreaks in Victorian abattoirs and meat processing facilities, necessitated veterinarians and staff from both federal and state animal health bodies to monitor animal welfare outcomes along the entire food processing chain.
Finally, management of animal disease outbreaks, in particular avian influenza in Victoria, was challenging during the pandemic. This was complicated by both secondment of staff to public health responses (see Theme 3) and hesitancy by other state animal health bodies to assist due to difficulty recalling personnel quickly due to state quarantine requirements. Early investigation and response to the emergence of Ehrlichia canis, a canine disease which was previously considered exotic to Australia, in Western Australia (May 2020) and the Northern Territory (June 2020) was also impacted by decreased availability of resources and engagement by government bodies, alongside restricted access to affected communities.
3.2.2. Managing human health in veterinary settings
‘It became clear to me that in veterinary practices,particularly in the face of a pandemic, we don't [just have to be] concerned about the employees and the clients, we have to be concerned about who lives with the employees and who lives with the clients. Because there might be a colleague that you have who's got elderly parents who are in their 90s, who've both got, you know, [chronic obstructive pulmonary disease] or something like that. If they get COVID they're going to die. And what you do at work can have an indirect but reasonable impact on that.’ (V01)
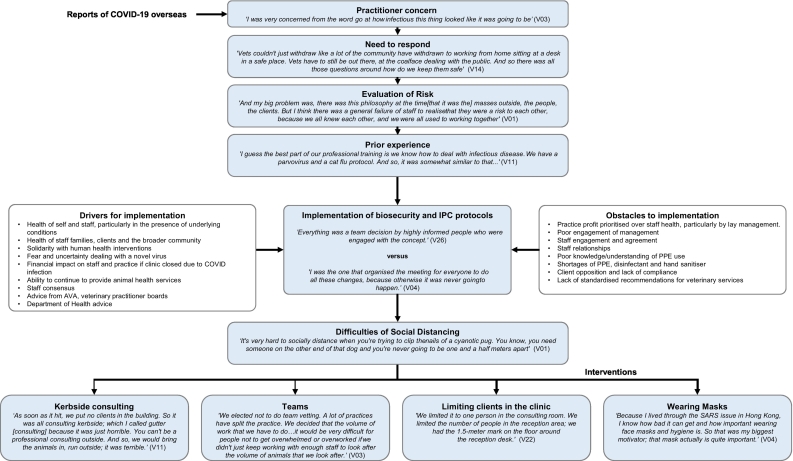
Upon early reports of COVID-19 in January 2020, some informants had immediate concerns of its potential impact worldwide, as well as the possible consequences for them and their veterinary practices. A flow chart summarising sub-themes and implementation of human health interventions as described by practitioners interviewed is shown in Fig. 2.
Fig. 2.
Pathway to implementation of COVID-19 related human health interventions in veterinary clinics as described by veterinary informants in Australia.
As cases were reported in Australia, clinicians identified a need to rapidly implement biosecurity and infection prevention and control (IPC) protocols in veterinary clinics to minimise the risk of human-to-human transmission of COVID-19. Many cited their understanding and experience in management of highly infectious animal diseases, such as canine parvovirus, as foundational for their actions. Others recounted anxiety about their responsibility for human health outcomes and decisions made in the face of a novel virus. They described a need for guidelines specific to veterinary practices in areas such as appropriate use of personal protective equipment (PPE) and implementation of public health recommendations. For some informants, shortages of PPE and hand sanitiser within human health services created ethical dilemmas regarding their use within veterinary settings.
The logistics of veterinary practice made it difficult to enforce public health recommendations. Informants described difficulties with social distancing in small consultation rooms and while restraining animals for examination, treatment and surgery. Management of human contact within clinics was perceived to be in two contexts: contact between staff and clients; and contact between staff members. Strategies to minimise contact with clients included restricting the number of clients in the clinic and ‘kerbside’ consulting, with animals collected by staff from clients outside the clinic. These interventions required flexibility in cases of sensitive procedures such as euthanasia or clients with special circumstances. Despite screening clients using Department of Health (DOH) guidelines regarding illness and travel history, a number of informants reported clients breaking self-isolation requirements or lying about illness in order to seek veterinary care for their animal(s).
Despite concerns being focused on contact with clients, some informants also noted their primary risk was other staff due to prolonged and unavoidable close contact. Many instituted wearing masks within the practice for all staff prior to official public health recommendations. Staff were encouraged to stay home if sick and get tested, which was seen to be contrary to the usual ethos, ‘that before the virus, nobody would dare call in sick because you knew that everyone else would have to pick up the load’ (V09). Many practice owners covered employee wages in these cases, with one informant from corporate management reporting their introduction of COVID-19 leave in addition to employee holiday and sick leave allowances. Splitting the workforce into two ‘teams’ ensured clinics could remain operational if a staff member was infected and others were required to isolate.
All informants described some emotional and physical costs, including time constraints, longer working hours, inflexible rosters and relational difficulties between staff members. Most informants concluded working in teams was difficult to sustain within the structure of most veterinary practices. Kerbside consulting created difficulties, fragmenting communication and removing usual relational cues and interactions with clients. Some informants conveyed struggles to engage staff with interventions or reluctance of lay (non-veterinary) management to implement protocols and procedures necessary to mitigate COVID-19 transmission, leading one informant to consider resigning from their job. Client reactions to health interventions were mixed, ranging from gratefulness to reports of increased verbal abuse to veterinarians and staff.
3.2.3. Providing key skills and support to the public health response
‘We wanted to make a positive contribution to the response.We want to use our skills, because we knew we had skills that could be really made use of. I think that was the main drive.’(V35)
As the threat of the pandemic was realized, state and federal health departments required a surge workforce. Veterinarians with requisite skills were seconded, employed or volunteered in a range of areas (Table 1) including epidemiology (e.g. contact tracing, modelling and diagnostic test validation) and data science. Crucially, veterinary epidemiologists in Victoria provided unique expertise, bringing advanced skills and new approaches to visualising and analysing data, standardising reporting, and modelling that were lacking in the department yet pivotal to the public health response. This included development of the ‘Mystery Case Tracker’ application to aid targeting of surveillance to individuals that are likely to be undetected cases [35].
Table 1.
Selected quotes on the engagement of Australian veterinarians within the public health response to COVID-19.
| Supporting state and federal health department functions | |
|---|---|
| Motivations for engaging |
‘Recruitment calls went out, and all the organisations that had close ties to the department and have collaborated in the past. Heads were approached to provide some of their staff which was wonderful and gave us a huge sort of surge workforce.This is such a unique opportunity.It's been that feeling of:this as an emergency response, we want to help our state and our country, however we can.’ (V16) ‘I think it's a bit cool as a vet to be able to work for the[Department of Health and Human Services].You know, I've always been very, very much a fan of One Health.It seemed like a very good opportunity to jump onto the other, the human side of things and see how that was working. And yeah, sort of see both sides.’ (V31) |
| Recognition of skills | ‘I think there was a recognition that our staff are used to dealing with population level health pandemic type scenarios and had some skills to offer.’ (V21) ‘I think it was preparedness.Because one thing NSW has, well, [Department of Primary Industries] has done a lot, is emergency management. And the interactions that occur during emergency management and drought. COVID is just another way of […] addressing that, using that system that has been in place. Which means pulling in a lot of key players to actually address the problems.’ (V33) |
| Transition to human health response | ‘My attitude was not to try and solve problems. When I was providing advice or commentary on something, I'd be very clear to say, ‘Well, I'm coming at this really differently from you. And so, you know, this may be totally wrong, butthis isthe way I think about this.’ And I think, to some extent some of the ways that we think about population health, about international trade are really quite different. And hopefully, some of those things, some of those approaches were quite useful.’ (V12) ‘Most of the modelling work I did for the department was a multi-level model. So, we're talking about simulation of spread between and within households that parallel identically to spread within and between farms. Soa lot of what we worked on had analogues in veterinary epidemiology. Now, we didn't commonly say that, because sometimes we found that led to people not being as engaged, so better to keep that to ourselves.’ (V35) |
| Acceptance by the public health workforce |
‘I guess it's a really interesting case study of veterinary public health and One Health in action because there's a number of veterinarians involved in the National IncidentRoom, as well as people involved in food safety epidemiology, people from academic roles in epidemiology.It's pretty amazing, really, to think that people could come from across the public sector and academia and work together.’(V12) ‘I say yes, there are challenges in that space. There is a mutual respect issue that I think will not go away. In a lot of senses, we've gained a lot of respect through this outbreak and that's for the benefit of our further One Health work together. Butin other respects there isn't an equal acceptance of our skills and advice because we aren't specifically from the public health or medical domain.’ (V35) |
| Supporting laboratory and research functions | |
| Boosting laboratory capacity | ‘We were very well prepared for high throughput testing for an animal outbreak. And we just used our utterly routine extraction and PCR methods for the COVID-19 testing.That's the beauty of what the laboratory brings is that we are operating in this disease space all the time.And the big achievement I think, which hasn't been sung about, is making the virus transport media. Sowe've made over half a million vials of virus transport media, which doesn't contain nucleases unlike a lot of the commercial virus transport media.So it's more effective than some of the commercially available transport media. So, we supply about half the state's transport media needs’ (V28) |
| Overseeing animal research | ‘We've got really large groups of animals, larger than we ordinarily would, because everything's been runat once.We were running three groups at a time so we can generate the data more quickly.A lot of our work is looking at just stopping your lungs consuming themselves.I guess feeling that I'm involved in some tiny way in facilitating research that will have an impact is really rewarding. But it's also,there's that urgency that we need to do this, we need to do as fast as possible, do it properly.’ (V29) |
| Supporting the international response | |
| Capacity building | ‘And in a number of those projects, we have beenrequested to provide what technical assistance we can to COVID responses for a number of countries,predominantly Indonesia, in ramping up their COVID testing and some of their COVID responses in terms of sequencing bioinformatics. And also, we've been setting up an advisory group to help them with some vaccine platform development.It's not just for this COVID, but so that platform is ready for vaccine development for a future pandemic or a future occurrence.’ (V32) |
| Pivoting existing overseas investments | ‘So where current projects were able to value add to the responses in various countries of the region, [vets were amongst those who provided] some technical assessment of those submissions. If you've got limited resources what do you prioritize fast? What's really practical? Like, training in administering supplementary oxygen is going to be more important than ventilators for some countries.’ (V05) |
Existing structures within state and federal veterinary departments, including emergency management response agreements, along with pre-existing relationships between university academics and health department officials facilitated incorporation of veterinarians into the public health response. This was expedited by previous experience with joint responses, multi-disciplinary epidemiology research projects or desktop exercises conducted during ‘peace time’. However, informants in some jurisdictions reported that available skilled veterinary personnel were not effectively utilized or even kept informed by their local state health bodies, which they attributed to a lack of health planning and joint exercises between human and animal health departments.
Veterinary informants seconded to health departments reported a straightforward transition into the human health response, with any barriers quickly dissipating in the face of the significant need for assistance. Many saw analogues in their work within veterinary epidemiology, population health and animal disease outbreak management, but commented on the need to re-frame ideas and terminology to improve receptivity by human health professionals. Some informants observed limited awareness by health professionals of the high-level epidemiological skills possessed by some veterinarians and a lack of mutual respect and equal acceptance within the human health space. However overall, they felt involvement led to increased regard and understanding of the skills of veterinary professionals and significant gains in bridging barriers to One Health.
Informants in laboratory and research environments also reported leveraging their skills to support the response. In NSW the state veterinary laboratory (Elizabeth Macarthur Agricultural Institute) provided extra COVID-19 testing capacity, aided by their experiences in high throughput PCR testing for animal diseases. They also identified and addressed shortcomings in existing viral transport media, rapidly testing an alternative and moving to produce over half the media used in the state [36]. Veterinarians serving as animal welfare officers in universities also provided advice regarding research design and animal models in conjunction with monitoring animal welfare, as research into COVID-19 pathophysiology was scaled up to rapidly generate data.
Veterinary informants also reported providing assistance to international capacity building efforts. The Australian Centre for Disease Preparedness (ACDP) provided support and advice to veterinary laboratories overseas to aid in scaling up their services to provide high throughput COVID-19 testing, sequencing bioinformatics and vaccine platform development. Informants also provided assistance through their workplaces, assisting partner projects overseas to pivot towards COVID-19 specific responses, including in areas of research, surveillance and education. Additional assistance was provided through provision of resources for frontline health workers.
3.2.4. Scientific literacy and communication
‘The amount of information is unlike any other infectious disease I've ever known […] It's a human-to-human responsibility, making sure that people understood what the potential risks […] are and could be, and are not, but also a sense of duty to my profession and also the animals. […] I think the challenge was actually knowing what the truth is.’(V19)
The early stages of the COVID-19 pandemic were characterised by uncertainty and fear. For many in clinical practice, keeping abreast of information being disseminated by government, media and scientific sources was demanding on top of their normal workload. Yet many informants felt a responsibility to research the evidence and explain health information to their friends and family. The fact that much of the scientific literature was being released as pre-print articles, some of which became the subject of media reports prior to peer review, was noted as generating concerns for both veterinarians and their clients.
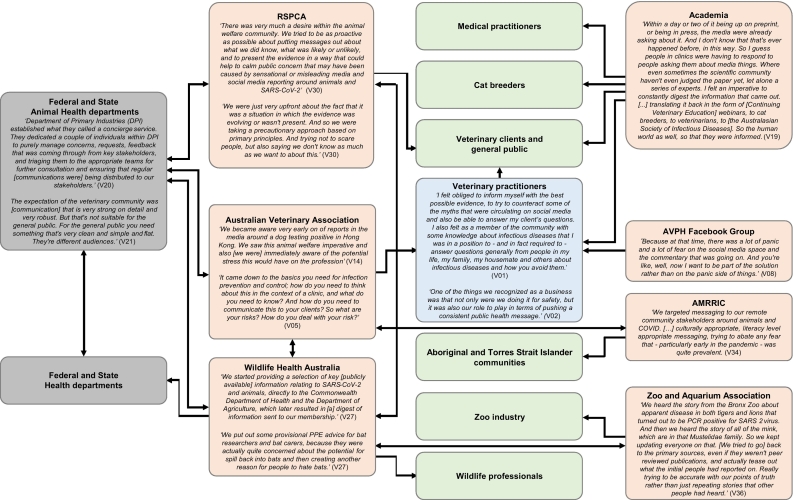
In response, veterinary informants with additional training in microbiology, wildlife medicine, epidemiology and/or public health stated that they felt compelled to use their knowledge and skills to interpret and distil information into clear and concise messages. These were transmitted via existing and new communication networks as illustrated in Fig. 3. Some saw this as a responsibility to help protect their colleagues, driven by prior experience with deadly zoonoses such as Hendra virus. Prompt communication of evolving information to stakeholders was deemed essential to assist and support veterinarian's response to COVID-19 as outlined in the description of the first three themes.
Fig. 3.
Communication network used by veterinarians during the COVID-19 response in Australia. Direction of arrows reflect the nature of the communication (one-way or two-way). Colours indicate the nature of the actors involved (grey = government, red = peak organisations and academia, blue = private sector, green = public and other end-users). Selected quotes are shown in italics, and are statements made by informants from within the relevant organisation. AMRRIC, Animal Management in Rural and Remote Indigenous Communities; AVPH, Australian Veterinarians in Public Health; RSPCA, Royal Society for the Prevention of Cruelty to Animals. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
To address concerns arising within clinical practice, the VPH SIG offered their assistance to the AVA, precipitating the formation of the COVID-19 working group. Members were recruited from the VPH SIG, other AVA SIGs, AVA board, and key stakeholder groups including the Department of Agriculture, Water and Environment (DAWE), NSW Department of Primary Industries (DPI), and Wildlife Health Australia (WHA), creating a collaborative platform to appraise and disseminate evidence as it emerged. Information directed at clinicians was focused on practical implementation of IPC within veterinary settings in the context of human-to-human transmission as well as evolving data regarding zoonotic risk from animals. The AVPH Facebook group provided a forum for distribution and critical discussion of information being reported in media and research literature. In addition, one veterinary microbiologist disseminated information to veterinary and medical practitioners using webinar format to convey key findings from the literature, particularly on the zoonotic potential of SARS-CoV-2.
Within the public sector, NSW DPI established a ‘COVID concierge’ to manage and triage concerns raised by stakeholders. This initiative provided significant benefits by expediting communication, with historical relationships providing both necessary formal and informal communication pathways between different stakeholder groups. WHA provided bespoke summaries of publicly available information concerning the wildlife origin of SARS-CoV-2 and risks to and from native wildlife to state and federal government agencies for health, environment and agriculture. Tailored information was also provided by informants to wildlife professionals, zoos and cat breeders, while DAWE provided specific guidance regarding animal importation and COVID-19 testing of animals, with the Animal Health Committee developing an agreed case definition to progress actions and understandings of COVID-19 in animals.
Information for the general public, particularly regarding companion animals, was provided by the AVA, RSPCA and animal health departments on their websites and by many veterinary clinics on their Facebook pages. Messaging was often aimed at calming the fears of the public, particularly regarding the risk of infection from animals which may have led to harm or abandonment of companion animals. Additional advice regarding management of pets in the case of COVID-19 infection of owners and planning for their care in the case of hospitalisation was also given. Animal Management in Rural and Remote Indigenous Communities (AMRRIC) provided messaging tailored to Aboriginal and Torres Strait Islander communities, sensitive to fear exacerbated by differences in culture, language and literacy.
Most informants recognised the inherent difficulties in providing evidence-based information in the presence of a novel virus. Some felt anxiety about inadvertently giving information that may later be proved incorrect. They were however cognisant of their experience as veterinarians in dealing with the unknown and felt confident in an approach based on first principles and scientific literacy. Failing this, they felt supported by veterinary colleagues who were more experienced in virology and VPH. A number commented on the importance in consistency of messaging across stakeholders to prevent confusion and distrust amongst recipients. All were honest about the limitations of the information they were providing in an evolving disease situation.
3.2.5. Insights on pandemic preparedness
‘I think I've learned that despite a lot of peopletalking about emerging infectious diseases and risks to humans from wildlife and vice versa for[20-25]years, that no one's really been listening.’(V36)
Many of the veterinarians interviewed, particularly those in non-clinical roles, were naturally inclined to view their work within the paradigm of One Health. They saw their professional training and experience equipped them to effectively function in and contribute to this space, stating ‘this is the thing that the profession gives you, that you're multilingual and you're transdisciplinary’ (V29). Most reflections offered by informants were provided through this lens and encapsulated their unique foresight and insight into COVID-19 and events surrounding its emergence and subsequent management. An overview of these reflections is included in Table 2.
Table 2.
Selected quotes on pandemic preparedness and planning in Australia by veterinary informants.
| Over-arching perspectives | |
|---|---|
| Veterinarians within the paradigm of One Health | ‘I think it's that skill of all vets to be constantly comparing.One of the things that differentiates us from quite a few other professions in the health sphere, […], we often don't have all the information on one disease in one species. And soour innate response is always to go through comparative medicine. And I must admit, until maybe about 10, 12 years ago, I thought that everybody thought like that. And I realized that that's actually not the case.Even though I've worked with fantastic people in the medical sphere, they still have a very human-centric focus.’ (V19) |
| Foresight into emerging threats | |
| Horizon scanning | ‘Particularly in recent years with emerging diseases, and particularly a lot of the new emerging diseases in humans originating from animals we had a heightened awareness of these new diseases. At the zoo, infectious diseases are a very, very important part of managing the health of our animals, and we're always considering infectious disease risks and have to keep up to speed with all those issues, in terms of protecting both our animals and our people. So, generally, it's front and centre for us.’ (V25) |
| Recognition of risk factors for emergence | ‘There's so much risk involved in having, particularly wild animals in these kinds of situations.There's wet markets or any kind of wildlife trade where they're stressed, in poor unhygienic conditions, they're mixing with a lot of people, a lot of other species. It's just an absolute disaster from the point of view of potential zoonotic and trans-species infections. And we've known that for a long time.It just actually boggles the mind that we just haven't even really acted on this beforehand, because it is an existential threat to our race and to our societies and our communities.’ (V30) |
| Shortcomings in national preparedness | |
| Lack of multi-agency planning | ‘We did have a pandemic plan, and we've had it many, many years. And it's been practiced a few times, but I think it was very health oriented. Because it didn't really address things like business continuity during pandemics for all areas of society.The original plans […] it has been very, very human oriented and they need to actually broaden that.’ (V33) |
| Failure to heed lessons from previous outbreaks | ‘Someone asked me recently were the lessons from the Callinan enquiry into biosecurity breaches in equine influenza, did that inform anything in the department'sresponse?I would hesitate to say that I don't thinkanyone in public health management would know of that inquiry, or what occurred in that outbreak. And so, the parallels to the breakdown of quarantine in hotels in Victoria that led to the second wave, the shortcomings and cheap skating on how quarantine's managed that leads to a massive event is, the false economy of that, is what is clearly written in the Callinan enquiry.You can have the rules in place, but if they're not followed, or the system managed inappropriately, there's key lessons there.’ (V35) |
| Lack of funding for prevention | ‘But you know, prevention is far more cost effective and far more effective than other methods.But I'm not sure that people want toinvest in prevention. Becauseyou spend a lot of money on something and you can't see a result. And it's very hard to keep governments and funders motivated to keep spending money on something when you can't prove that you're actually achieving anything.’ (V36) |
| Lack of companion animal authority | ‘I mean, companion animals aren't a part of our emergency animal disease responses.How you deal with companion animals, like dogs and cats in the state of an emergency animal disease is just not clear. Because who are the people that make decisions about dogs and cats? And is there any authority that could help make those decisions or access all the owners?We need to find some way to bring that in because certainly my experience was that the [Chief Veterinary Officers] of the states weren't comfortable with making decisions on companion animals or even having their offices deal with companion animal inquiry.’ (V05) |
| Optimising national preparedness | |
| Improving existing systems | ‘I think the big thing is around resource sharing. So even if the systems themselves aren't identical but set up in such a way that you can easily share resources, and not just easily, but quickly share it. And I think that's where practicing exercises in peace-time is really important for things like that.Because […] I don't think this is the last of these sorts of pandemics we're going to see, it's just going to become more frequent.I think the need to work with multiple agencies in responsesis going to become the norm. And I think it's a matter of ensuring that processes, governance systems are all in place to ensure that we can mobilize things quickly and efficiently.’ (V20) |
| Linking scientists and practitioners | ‘I think I've learnt that there is a real need for bridging between the scientists and the practitioners.I think maybe we need some of us to position ourselves as that intermediate bridge.There's so many publications that are coming out, but they just don't make their way to the average practitioner.And what is going to change the behaviour of practitioners?’ (V08) |
| Linking experts and government | ‘What we should learn from this in Australia is that we need better structures in place for collaborations between experts and collaborations into government agencies. We need better surge force plans. Because what has been incredibly challenging in Victoria is just actually getting enough people to be able to work in the response, both in technical roles like epidemiologists, also in contact tracing and some of the other logistics roles.And I think it really underlines nationally how important some type of One Healthagency is to be able to get national coordination for these types of diseases, especially if the next one has ongoing, zoonotic transmission.’ (V16) |
A number of informants remarked that they were unsurprised by the emergence of SARS-CoV-2. Many such informants served in roles where preparedness and response to outbreaks was an integral part of their work. Horizon scanning was seen as fundamental by veterinarians working in wildlife, zoo and some government sectors, where recognition of emerging disease threats is perceived as essential for outbreak and pandemic preparedness. Others conveyed long-standing concerns regarding the consequences of the lack of consideration of the inter-relationships between human, animal and environmental health, particularly in the context of food security. Some conveyed how they took personal actions to reduce their footprint, such as buying locally produced food and limiting their intake of agricultural products known to have more detrimental impacts on the environment. Recognition of risk factors for zoonotic disease emergence such as the wildlife trade, wet markets and damaged ecosystems was accompanied in some cases with prior experience working in areas related to disease emergence and outbreak management.
In addition to anticipating the emergence of a disease like COVID-19, informants also commented on pre-existing shortcomings in preparedness, which they attributed to a lack of formal cross-disciplinary and cross-sectoral structures and planning. This was manifested in insufficient multi-agency pandemic exercises and failure to engage with lessons learnt from previous outbreaks. In particular, some pointed to the need for human health agencies to acknowledge and learn from both human and animal outbreaks, with parallels drawn to the quarantine breakdown seen during the equine influenza outbreak in Australia as well as warnings from Ebola and previous coronavirus outbreaks such as SARS-CoV-1 and Middle East Respiratory Syndrome (MERS) virus. Some saw the lack of national preparedness overall was related to the ongoing difficulties in government funding for disease prevention, where effective interventions show no tangible outcomes aside from an absence of disease. Insufficient national stockpiles of PPE were seen as a lack of government response to anticipated need. Basic technological issues, such as lack of compatibility of information technology (IT) systems, were also noted in a number of sectors and resulted in delayed responses.
Reports of transmission of COVID-19 from humans to pets and the unknown ongoing risk of transmission from animal sources led a number of informants to convey disquiet about the lack of established governance structures nationally for surveillance and management of zoonotic diseases in companion animals. Many were concerned about the potential of serious consequences for animal welfare and spread of disease amongst domestic pets and identified this as an ongoing issue.
Advancement of current One Health structures was deemed highly important by most participants as summarised by one informant: ‘I think also having better structures for multi-sectoral collaboration would be really useful. We're all very good at working in our own domain or sphere of excellence. Someone once called them‘silos of excellence’. But I think having opportunities to collaborateand coordinate on some of these sorts of broader issues is really important from a government perspective, and from a society perspective’ (V12). Many desired a truly One Health multi-disciplinary body, some with a vision for inclusion of disciplines such as social scientists, engineers and economists. Others seemed to prefer retention of current structures, adopting a collaborative governance framework with shared responsibility and knowledge integration to enable priority-based, scalable responses. Some suggested employment of veterinarians within public health departments to act as knowledge brokers, providing insight on animal health and facilitating communication between animal and human health departments.
Federal and state government support of further One Health initiatives was deemed essential. This included injection of funds into local research, developing sustainable pathways for post-graduate VPH and veterinary epidemiology training, and sectorial and stakeholder based after-action reviews based on One Health timeliness metrics. Many commented that funding should be free of political agendas, observing the damage to COVID-19 responses in countries such as the United States as a consequence of political interference. Lack of forthcoming funding was seen likely to significantly impact future national pandemic preparedness.
4. Discussion
In 2004, the Canadian veterinary pathologist, Dr. Fredrick A. Leighton, questioned the social relevance of 21st century veterinarians [37]. Reflecting on the increasingly narrow professional focus on companion animal clinical practice, he noted the diminishing expertise in areas of fundamental public importance such as public health, food security and environmental health. He suggested that most would fail the ‘lifeboat test’; in the face of ‘unanticipated and severe difficulty’ the majority of veterinarians could be deemed desirable, but not essential to society. To the contrary, in the presence of challenges faced by veterinarians during the COVID-19 pandemic, informants in our study firmly established their relevance. This included actions taken by companion animal veterinarians to ably manage extra demands including mitigation of public health risks and increased impacts on animal welfare alongside unexpected demands on companion animal services during the pandemic, with animal shelters emptied and veterinary practices experiencing increased demand [38].
Maintenance of these fundamental skills within the veterinary profession is dependent on continued advocacy worldwide to retain aspects of global health, such as public health and food security, as core competencies within veterinary education in the presence of increased demands on university curricula and veterinary practice [[39], [40], [41], [42], [43], [44], [45], [46]]. However, the rationale for sustaining these skills is complicated by how both governments and society understand and value the work done by the veterinary profession [45]. This was illustrated during the pandemic by the lack of clarity of the status of veterinarians as essential services in many countries, with different restrictions being placed on professional practice during national lockdowns worldwide [[47], [48], [49], [50]]. More critically, in Australia and many other countries, misunderstandings around the societal role of veterinarians has manifested in decreased government funding to public veterinary services [[51], [52], [53]], which in Australia has also contributed to reductions in university offerings for postgraduate study in VPH.
Informants in our study were welcomed into the public health response and seen as valuable contributors. Indeed, as mentioned by the informants, experiences gained by veterinarians through their response to exotic animal disease incursions (such as equine influenza in Australia in 2007), and knowledge and insight of wildlife and zoo veterinarians into conditions predisposing to disease emergence are highly relevant to human health outbreak preparedness and response [[54], [55], [56], [57], [58], [59]]. Veterinarians also need to be mindful of inherent differences in human and animal health management [60], something which our informants did seem heedful of. Nonetheless, some respondents questioned whether their expertise was accepted by human health professionals. Studies have documented difficulties in interprofessional cooperation and communication between medical and allied health professionals [61,62] which may be mirrored in interactions between medical professionals and veterinarians. Following the emergence of West Nile virus (WNV) in the United States, there was widespread discussion regarding the initial dismissal by public health agencies of concerns raised by a veterinary pathologist - who eventually identified WNV as the agent causing neurological signs in both birds and humans [59]. Such historical experiences may lead veterinarians to question how their expertise will be perceived by medical professionals when contributing to a public health response. Understanding different professional roles and responsibilities as well as one's own limitations are seen as key to effective One Health practice [30] and may be strengthened by incorporating opportunities for interprofessional education into undergraduate training of veterinary and human health professionals [63].
While efforts to advocate for One Health approaches tend to focus on zoonotic aspects of disease control, this research shows the importance of One Health approaches to pandemic preparedness and response even when a disease is principally transmitted from human to human. In the United States, for example, attachment to pets was found to be an important influence on health seeking behaviour, with some owners stating they would be inclined to delay testing and treatment for COVID-19 due to pet-related welfare concerns [64]. The lack of consideration of animal health and welfare needs and the repercussions as described in this study and elsewhere [18] were clear indicators of a lack of One Health coordination in the Australian response. A further example was found in the absence of specific health guidelines for veterinary practice where standard workplace recommendations from the DOH were difficult to implement in this context. Instead, veterinarians were left to mobilize relevant information and set guidelines [65] from within the profession with limited medical input. This contrasts with the United States where, for example, the Centers for Disease Control and Prevention (CDC) published a guideline specifically on IPC in companion animal veterinary clinics a month after a pandemic was declared by WHO [66].
The existence of ‘silos’, both intra- and inter-professionally, was recognised by informants as a perpetual obstacle to operationalising One Health. Australia is the only OECD country that does not have a CDC-type national body; responsibilities for disease prevention and control instead fall to federal and/or state agencies associated with (human) health on the one hand and agriculture/primary industries on the other [67]. Critically, companion animal health falls outside this governance structure [68,69]. Establishment of formal One Health structures and systems with appropriate representation of all stakeholders, including in companion animal health, was seen as pivotal to future pandemic preparedness by our respondents. Similar calls have been made by the tripartite (WHO-FAO-OIE) and others [20,[70], [71], [72]] along with the need to strengthen global health security and zoonoses management more broadly [73,74]. Indeed, the Sydney Statement on Global Health Security [75] states “Global health security must embrace a One Health approach, not only to prevent and respond to disease, but also to protect ecosystems that underpin human, animal, and environmental health. All relevant sectors must be meaningfully involved and engaged, including heath, agriculture, environmental, security, and other vital components.” This includes a need for joint simulation exercises in peacetime [72,76,77], something which our informants also called for. Inclusion of environmental scientists within these is essential given potential for significant environmental impacts in the event of an emerging infectious disease with continuing zoonotic potential where mass culling of animals may be considered to protect public health.
This study which used key informant interviews has provided useful insights into the response to COVID-19 by the veterinary profession in Australia. Nonetheless, there are some limitations. Engagement with some of sectors of the profession, in particular government veterinarians in Victoria, including those employed in abattoirs, proved difficult. This was likely due to increased work demands at the time the study was conducted, which coincided with the second wave of COVID-19 and avian influenza outbreaks in this state. We were also unable to interview any clinicians in mixed or equine practice despite a number of invitations. Many clinical veterinarians described increased work pressures due to the required public health interventions, which may have impacted more on rural practitioners, particularly in areas with increased community cases. Despite this, we managed to interview veterinarians covering a broad range of responses. Finally, even though the authors are known to many of the study informants, we do not feel this has biased their responses and perceive the insights gained are perhaps deeper due to their trust.
5. Conclusion
This unique study demonstrates how veterinarians in Australia added value to the national response to COVID-19. Many veterinarians were formally engaged in the national public health response in areas such as epidemiology and laboratory analysis, with others providing support for essential research. Within the agriculture sector, measures taken to secure unimpeded transport of animals and animal workers across closed borders ensured both local food security and animal welfare. Maintenance of veterinary services during the pandemic required clinicians to modify their practice management to protect public health, where modelling ‘COVID safe’ practices was seen as a responsibility, showing solidarity with public health messaging. Continuity of veterinary services assisted pet owners, many of whom saw their pets as a source of emotional and physical support during the pandemic [78,79]. Most responses were guided by scientific literacy and clear, evidence-based communication. Many informants saw their training and experience as veterinarians was foundational to their capacity to respond to the pandemic. In conclusion, this study affirms the relevance of the veterinary profession to 21st century issues and calls for their greater engagement in all areas of disease prevention, preparedness and response. Adoption of a coordinated multi-disciplinary and multi-sectoral response is essential to ensure Australia and the world can meet the continuing challenges of COVID-19 and future pandemics.
Declaration of Competing Interest
The authors declare they have no conflict of interest in relation to this paper.
Acknowledgements
The authors wish to thank Cynthia Hunter for her advice regarding interview development and reviewing trial interviews and Isabel MacPhillamy, Michelle Doré and Emma Davis for taking part in trial interviews. We especially thank our veterinary colleagues who participated in this study, generously sharing their knowledge and insights and particularly their actions which contributed positively to the Australian COVID-19 response.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.onehlt.2021.100314.
Appendix A. Supplementary data
Supplementary material
References
- 1.World Health Organisation Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) 2020. https://www.who.int/publications/i/item/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19) (accessed 11 March 2021)
- 2.World Health Organisation WHO Director-General's Opening Remarks at the Media Briefing on COVID-19 [Press Release] 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed 18 March 2021)
- 3.Haug N., Geyrhofer L., Londei A., Dervic E., Desvars-Larrive A., Loreto V. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat. Hum. Behav. 2020;4(12):1303–1312. doi: 10.1038/s41562-020-01009-0. [DOI] [PubMed] [Google Scholar]
- 4.Lowy Institute Covid Performance Index. 2021. https://interactives.lowyinstitute.org/features/covid-performance/ (accessed 25 March 2021)
- 5.Triggle N. BBC News; 8 December 2020. Covid-19 Vaccine: First Person Receives Pfizer Jab in UK.https://www.bbc.com/news/uk-55227325 (accessed 25 March 2021) [Google Scholar]
- 6.Johns Hopkins University of Medicine Coronavirus Resource Centre. 2021. https://coronavirus.jhu.edu/ (accessed 24 March 2021)
- 7.Department of Health and Human Services State Government of Victoria Premier's Statement on Changes to Regional Restrictions [Press Release] 2 August 2020. https://www.dhhs.vic.gov.au/updates/coronavirus-covid-19/premiers-statement-changes-regional-restrictions (accessed 25 March 2021)
- 8.Parliament of Australia COVID-19: A Chronology of State and Territory Government Announcements (Up Until 30 June 2020) 2020. https://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/pubs/rp/rp2021/Chronologies/COVID-19StateTerritoryGovernmentAnnouncements#_Toc52275792 (accessed 22 March 2020)
- 9.Prime Minister of Australia Press Conference - Australian Parliament House [Press Release] 27 February 2020. https://www.pm.gov.au/media/press-conference-australian-parliament-house-4 (accessed 22 March 2021)
- 10.Prime Minister of Australia Border Restrictions [Press Release] 19 March 2020. https://www.pm.gov.au/media/border-restrictions (accessed 22 March 2021)
- 11.Prime Minister of Australia Update on Coronavirus Measures [press release] 20 March 2020. https://www.pm.gov.au/media/update-coronavirus-measures-0 (accessed 22 March 2020)
- 12.Minister for Health and Aged Care Hon Greg Hunt MP Press Conference in Canberra on 2 August 2021 About the COVID-19 Vaccination Rollout, Queensland Cases, Delta Variant and Phase 1B [Press Release] 2 August 2021. https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/press-conference-in-canberra-on-2-august-2021-about-the-covid-19-vaccination-rollout-queensland-cases-delta-variant-and-phase-1b (accessed 17 August 2021)
- 13.Andersen K.G., Rambaut A., Lipkin W.I., Holmes E.C., Garry R.F. The proximal origin of SARS-CoV-2. Nat. Med. 2020;26(4):450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deng J., Jin Y., Liu Y., Sun J., Hao L., Bai J. Serological survey of SARS-CoV-2 for experimental, domestic, companion and wild animals excludes intermediate hosts of 35 different species of animals. Transbound. Emerg. Dis. 2020;67(4):1745–1749. doi: 10.1111/tbed.13577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sit T.H.C., Brackman C.J., Ip S.M., Tam K.W.S., Law P.Y.T., To E.M.W. Infection of dogs with SARS-CoV-2. Nature. 2020;586(7831):776–778. doi: 10.1038/s41586-020-2334-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garigliany M., Van Laere A.-S., Clercx C., Giet D., Escriou N., Huon C. SARS-CoV-2 natural transmission from human to cat, Belgium, March 2020. Emerg. Infect. Dis. J. 2020;26(12):3069. doi: 10.3201/eid2612.202223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leroy E.M., Ar Gouilh M., Brugere-Picoux J. The risk of SARS-CoV-2 transmission to pets and other wild and domestic animals strongly mandates a one-health strategy to control the COVID-19 pandemic. One Health. 2020;10:100133. doi: 10.1016/j.onehlt.2020.100133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baptista J., Blache D., Cox-Witton K., Craddock N., Dalziel T., de Graaff N. Impact of the COVID-19 pandemic on the welfare of animals in Australia. Front. Vet. Sci. 2021;7(1219) doi: 10.3389/fvets.2020.621843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hasler B., Bazeyo W., Byrne A.W., Hernandez-Jover M., More S.J., Ruegg S.R. Reflecting on One Health in action during the COVID-19 response. Front. Vet. Sci. 2020;7:578649. doi: 10.3389/fvets.2020.578649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferri M., Lloyd-Evans M. The contribution of veterinary public health to the management of the COVID-19 pandemic from a One Health perspective. One Health. 2021;12:100230. doi: 10.1016/j.onehlt.2021.100230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Veterinary Medical Association COVID-19 Impact on Veterinary Practices. 2020. https://www.avma.org/resources-tools/animal-health-and-welfare/covid-19/covid-19-impact-veterinary-practices (accessed 24 March 2020)
- 22.Kogan L.R., Erdman P., Bussolari C., Currin-McCulloch J., Packman W. The initial months of COVID-19: dog owners’ veterinary-related concerns. Front. Vet. Sci. 2021;8:629121. doi: 10.3389/fvets.2021.629121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sibley D., Brownlie J. Vets would not manage Covid-19 this way. Vet. Rec. 2020;186(14):462–463. doi: 10.1136/vr.m3004. [DOI] [PubMed] [Google Scholar]
- 24.Decaro N., Martella V., Saif L.J., Buonavoglia C. COVID-19 from veterinary medicine and One Health perspectives: what animal coronaviruses have taught us. Res. Vet. Sci. 2020;131:21–23. doi: 10.1016/j.rvsc.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun J., He W.-T., Wang L., Lai A., Ji X., Zhai X. COVID-19: epidemiology, evolution, and cross-disciplinary perspectives. Trends Mol. Med. 2020;26(5):483–495. doi: 10.1016/j.molmed.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mardones F.O., Rich K.M., Boden L.A., Moreno-Switt A.I., Caipo M.L., Zimin-Veselkoff N. The COVID-19 pandemic and global food security. Front. Vet. Sci. 2020;7:578508. doi: 10.3389/fvets.2020.578508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mobasheri A. COVID-19, companion animals, comparative medicine, and One Health. Front. Vet. Sci. 2020;7(522) doi: 10.3389/fvets.2020.00522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Halasa T., Graesboll K., Denwood M., Christensen L.E., Kirkeby C. Prediction models in veterinary and human epidemiology: our experience with modeling SARS-CoV-2 spread. Front. Vet. Sci. 2020;7:513. doi: 10.3389/fvets.2020.00513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 30.Steele S.G., Toribio J.-A., Booy R., Mor S.M. What makes an effective One Health clinical practitioner? Opinions of Australian One Health experts. One Health. 2019;8:100108. doi: 10.1016/j.onehlt.2019.100108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steele S.G., Booy R., Mor S.M. Establishing research priorities to improve the One Health efficacy of Australian general practitioners and veterinarians with regard to zoonoses: a modified Delphi survey. One Health. 2018;6:7–15. doi: 10.1016/j.onehlt.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Steele S.G., Booy R., Manocha R., Mor S.M., Toribio J.-A.L.M.L. Towards One Health clinical management of zoonoses: a parallel survey of Australian general medical practitioners and veterinarians. Zoonoses Public Health. 2021;68:88–102. doi: 10.1111/zph.12799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Terry G., Hayfield N., Clarke V., Braun V. In: The SAGE Handbook of Qualitative Research in Psychology. 2 ed. Willig C., Stainton-Rogers W., editors. SAGE Publications Ltd; 55 City Road, London: 2017. Thematic analysis; pp. 17–36. [Google Scholar]
- 34.Green J., Thorogood N. 4th ed. SAGE Publications Ltd.; London: 2018. Qualitative Methods for Health Research. [Google Scholar]
- 35.Premier of Victoria Innovation Boosts Mystery Case Tracking. 2020. https://www.premier.vic.gov.au/innovation-boosts-mystery-case-tracking (accessed 4 May 2021)
- 36.Kirkland P.D., Frost M.J. The impact of viral transport media on PCR assay results for the detection of nucleic acid from SARS-CoV-2 and other viruses. bioRxiv. 2020 doi: 10.1101/2020.06.09.142323. 2020.06.09.142323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leighton F.A. Veterinary medicine and the lifeboat test: a perspective on the social relevance of the veterinary profession in the 21st century. Can. Vet. J. 2004;45(3):259–263. [PMC free article] [PubMed] [Google Scholar]
- 38.CM Research . 2021. COVID-19: Global pandemic impact on the veterinary market. [Google Scholar]
- 39.Wong V., Clavel M., Dehove A. OIE twinning programme for veterinary education. Rev. Sci. Tech. 2017;36(2):691–700. doi: 10.20506/rst.36.2.2686. [DOI] [PubMed] [Google Scholar]
- 40.Soulsby L., Walsh D.A. Global health: setting the agenda for veterinary medical education to enable veterinarians to meet their responsibilities in the field. Rev Sci Tech. 2009;28(2):861–872. doi: 10.20506/rst.28.2.1929. [DOI] [PubMed] [Google Scholar]
- 41.Maccabe A.T. Advancing veterinary medical education worldwide: where do we go from Here? J. Vet. Med. Educ. 2020;47(s1):99–100. doi: 10.3138/jvme-2019-0029. [DOI] [PubMed] [Google Scholar]
- 42.Kelly A.M., Galligan D.T., Salman M.D., Osburn B.I. The epic challenge of global food security: a compelling mission for veterinary medicine. J. Am. Vet. Med. Assoc. 2020;256(6):643–645. doi: 10.2460/javma.256.6.643. [DOI] [PubMed] [Google Scholar]
- 43.Pollard A.E., Rowlison D.L., Kohnen A., McGuffin K., Geldert C., Kramer C. Preparing veterinarians to address the health impacts of climate change: student perceptions, knowledge gaps, and opportunities. J. Vet. Med. Educ. 2021;0(0) doi: 10.3138/jvme-2019-0080. [DOI] [PubMed] [Google Scholar]
- 44.Hollier P.J., Fathke R.L., Brown C.C. The veterinary profession and precarious values. J. Am. Vet. Med. Assoc. 2014;244(10):1130–1132. doi: 10.2460/javma.244.10.1130. [DOI] [PubMed] [Google Scholar]
- 45.Council for Agricultural Science and Technology . 2020. Impact of Recruitment and Retention of Food Animal Veterinarians on the U.S. Food Supply. [Google Scholar]
- 46.World Organisation for Animal Health (OIE) 2012. OIE Competencies of ‘Day 1 Graduates’. OIE Sub-Regional Representation for South-East Asia. [Google Scholar]
- 47.British Veteirnary Association Advice for Veterinary Professionals. 2021. https://www.bva.co.uk/coronavirus/coronavirus-advice-for-veterinary-professionals/ (accessed 30 March 2021)
- 48.Australian Veterinary Association Minister for agriculture – vets an essential service during the COVID-19 crisis. 2020. https://www.ava.com.au/coronavirus/vets-an-essential-service-during-the-covid-19-crisis/ (accessed 22 March 2021)
- 49.American Veterinary Medical Association Veterinary practices are “essential businesses”. 2020. https://www.avma.org/resources-tools/animal-health-and-welfare/covid-19/veterinary-practices-are-essential-businesses (accessed 30 March 2021)
- 50.Veterinary Council of New Zealand COVID-19 general FAQs and resources for vets. 2020. https://www.vetcouncil.org.nz/Web/News/Articles/COVID-19_for_vets.aspx (accessed 30 March 2021)
- 51.Department of Agriculture and Water Resources . 2018. National Animal Health Surveillance and Diagnostics Business Plan 2016–2020. [Google Scholar]
- 52.Schneider H., Batho H., Stemshorn B., Thiermann A. OIE; Paris, France: 2016. PVS Evaluation Report Australia. [Google Scholar]
- 53.National research council (USG committee on achieving sustainable global capacity for surveillance and response to emerging diseases of zoonotic origin) In: Sustaining Global Surveillance and Response to Emerging Zoonotic Diseases. Keusch G.T., Gonzalez M.C., editors. National Academies Press (US); Washington (DC): 2009. Sustainable financing for global disease surveillance and response. [PubMed] [Google Scholar]
- 54.Kahn L.H. Confronting zoonoses, linking human and veterinary medicine. Emerg. Infect. Dis. 2006;12(4):556–561. doi: 10.3201/eid1204.050956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.OIE . 2018. Emergency Preparedness and Response Planning. Paris. [Google Scholar]
- 56.Animal Health Australia AUSVETPLAN Manuals and Documents. 2018. https://www.animalhealthaustralia.com.au/our-publications/ausvetplan-manuals-and-documents/ (accessed 8 September 2020)
- 57.Callinan I. Department of Agriculture, Fisheries and Forestry; Australia: 2008. Equine Influenza Inquiry Report. [Google Scholar]
- 58.Enticott G., Maye D. Missed opportunities? Covid-19, biosecurity and One Health in the United Kingdom. Front. Vet. Sci. 2020;7(577) doi: 10.3389/fvets.2020.00577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wilson J.M., McNamara T. The 1999 West Nile virus warning signal revisited. Intell. Natl. Secur. 2020;35(4):519–526. doi: 10.1080/02684527.2020.1750144. [DOI] [Google Scholar]
- 60.Eussen B.G.M., Schaveling J., Dragt M.J., Blomme R.J. Stimulating collaboration between human and veterinary health care professionals. BMC Vet. Res. 2017;13(1):174. doi: 10.1186/s12917-017-1072-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zwarenstein M., Rice K., Gotlib-Conn L., Kenaszchuk C., Reeves S. Disengaged: a qualitative study of communication and collaboration between physicians and other professions on general internal medicine wards. BMC Health Serv. Res. 2013;13(1):494. doi: 10.1186/1472-6963-13-494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Luetsch K., Scuderi C. Experiences of medical dominance in pharmacist-doctor interactions - an elephant in the room? Res. Soc. Adm. Pharm. 2020;16(9):1177–1182. doi: 10.1016/j.sapharm.2019.12.013. [DOI] [PubMed] [Google Scholar]
- 63.Wilkes M.S., Conrad P.A., Winer J.N. One Health-one education: medical and veterinary inter-professional training. J. Vet. Med. Educ. 2019;46(1):14–20. doi: 10.3138/jvme.1116-171r. [DOI] [PubMed] [Google Scholar]
- 64.Applebaum J.W., Adams B.L., Eliasson M.N., Zsembik B.A., McDonald S.E. How pets factor into healthcare decisions for COVID-19: a One Health perspective. One Health. 2020;11:100176. doi: 10.1016/j.onehlt.2020.100176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Australian Veterinary Association Coronavirus (COVID-19): AVA Updates. 2020. https://www.ava.com.au/coronavirus/ (accessed 24 June 2020)
- 66.Centers for disease control and prevention Interim infection prevention and control guidance for veterinary clinics treating companion animals during the COVID-19 response. 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/veterinarians.html (accessed 4 May 2021)
- 67.Australian Medical Association Australian National Centre for Disease Control (CDC) - 2017. 2017. https://ama.com.au/position-statement/australian-national-centre-disease-control-cdc-2017 (accessed 2 April 2020)
- 68.Australian Veterinary Association Engagement of private veterinary practitioners in national disease surveillance. 2019. https://www.ava.com.au/policy-advocacy/policies/other-services-provided-by-veterinarians/engagement-of-private-veterinary-practitioners-in-national-disease-surveillance/ (accessed 8 September 2020)
- 69.Kelman M., Barrs V.R., Norris J.M., Ward M.P. Canine parvovirus prevention-what influence do socioeconomics, remoteness, caseload and demographics have on veterinarians’ perceptions and behaviors? Prevent. Vet. Med. 2020;181:105065. doi: 10.1016/j.prevetmed.2020.105065. [DOI] [PubMed] [Google Scholar]
- 70.Amuasi J.H., Walzer C., Heymann D., Carabin H., Huong L.T., Haines A. Calling for a COVID-19 One Health research coalition. Lancet. 2020;395(10236):1543–1544. doi: 10.1016/S0140-6736(20)31028-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Waugh C., Lam S., Sonne C. One Health or planetary health for pandemic prevention? Lancet. 2020;396(10266):1882–1883. doi: 10.1016/S0140-6736(20)32392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.World Health Organization, Food and Agriculture Organization of the United Nations, World Organisation for Animal Health . 2019. Taking a multisectoral, One Health approach: A tripartite guide to addressing zoonotic diseases in countries. [Google Scholar]
- 73.Belay E.D., Kile J.C., Hall A.J., Barton-Behravesh C., Parsons M.B., Salyer S. Zoonotic disease programs for enhancing global health security. Emerg. Infect. Dis. 2017;23(13):S65–S70. doi: 10.3201/eid2313.170544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jenkins B. The global health security agenda and the role of the World Organisation for animal health. Rev. Sci. Tech. 2017;36(2):639–645. doi: 10.20506/rst.36.2.2681. [DOI] [PubMed] [Google Scholar]
- 75.Global Health Security 2019 Conference Sydney Statement on Global Health Security. 2019. https://www.ghs2019.com/sydney-statement.php (accessed 4 May 2021)
- 76.McDarby G., Reynolds L., Zibwowa Z., Syed S., Kelley E., Saikat S. The global pool of simulation exercise materials in health emergency preparedness and response: a scoping review with a health system perspective. BMJ Global Health. 2019;4(4) doi: 10.1136/bmjgh-2019-001687. e001687-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Belot G., Caya F., Errecaborde K.M., Traore T., Lafia B., Skrypnyk A. IHR-PVS National Bridging Workshops, a tool to operationalize the collaboration between human and animal health while advancing sector-specific goals in countries. bioRxiv. 2020 doi: 10.1101/2020.12.29.424658. 2020.12.29.424658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shoesmith E., Shahab L., Kale D., Mills D.S., Reeve C., Toner P. The influence of human–animal interactions on mental and physical health during the first COVID-19 lockdown phase in the U.K.: a qualitative exploration. Int. J. Environ. Res. Public Health. 2021;18(3):976. doi: 10.3390/ijerph18030976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ratschen E., Shoesmith E., Shahab L., Silva K., Kale D., Toner P. Human-animal relationships and interactions during the Covid-19 lockdown phase in the UK: Investigating links with mental health and loneliness. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0239397. e0239397-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material