Abstract
Background: While early life exposures such as mode of birth, breastfeeding, and antibiotic use are established regulators of microbiome composition in early childhood, recent research suggests that the social environment may also exert influence. Two recent studies in adults demonstrated associations between socioeconomic factors and microbiome composition. This study expands on this prior work by examining the association between family socioeconomic status (SES) and host genetics with microbiome composition in infants and children. Methods: Family SES was used to predict a latent variable representing six genera abundances generated from whole-genome shotgun sequencing. A polygenic score derived from a microbiome genome-wide association study was included to control for potential genetic associations. Associations between family SES and microbiome diversity were assessed. Results: Anaerostipes, Bacteroides, Eubacterium, Faecalibacterium, and Lachnospiraceae spp. significantly loaded onto a latent factor, which was significantly predicted by SES (p < 0.05) but not the polygenic score (p > 0.05). Our results indicate that SES did not predict alpha diversity but did predict beta diversity (p < 0.001). Conclusions: Our results demonstrate that modifiable environmental factors influence gut microbiome composition at an early age. These results are important as our understanding of gut microbiome influences on health continue to expand.
Keywords: socioeconomic status, infant, childhood, microbiome, stress
1. Introduction
The human gut microbiota play an important role in a broad range of physiological functions, including immune system maturation, metabolic and inflammatory processes, and the central nervous system [1,2,3]. Microbial diversity is influenced by a combination of environmental and host genetic factors and is associated with several complex diseases [4]. Various environmental factors influence inter-individual variation in the gut microbiota structure and function during childhood, including mode of birth (vaginal or caesarean section), initiation and duration of breastfeeding, antibiotic exposure, indoor and outdoor environment, pet exposure, and diet [5,6].
While the human gut microbiome composition is strongly shaped by various environmental factors, there is also evidence for host genetic influence [7]. Early underpowered studies suggested that monozygotic twins were no more similar in gut microbiota than dizygotic twins, suggesting very little, if any, genetic influence [8,9]. However, more recent studies incorporating larger twin samples from the TwinsUK cohort show a small but statistically significant effect of genetics on microbiome composition [10,11]. Studies in mice further demonstrate the role of host genetic influence on microbiome composition [12,13,14]. Importantly, molecular genetic studies [15] and multiple genome-wide association studies (GWAS) have demonstrated that host genetics moderately influence microbial composition in humans [16,17,18,19,20,21]. Together, these studies demonstrate the existence of human genes with alleles that contribute to microbiome composition.
As our understanding of environmental and genetic influences on gut microbiome composition continue to grow, recent research suggests the social environment may also play a role in regulating the gut microbiome [22]. Research linking the social environment to the gut microbiome mostly stems from animal models focused on the impact of social interactions and psychosocial stress. Studies in primates suggest that social relationships influence gut microbiome composition through microbial sharing between individuals [23,24,25,26]. In addition to direct microbial sharing, psychosocial stressors may also affect microbiome structure [27,28]. Animal studies demonstrate that psychological stressors, such as novel housing, social disruption, restraint stress, and early life stress, affect microbial community compositions [29,30,31]. Prenatal maternal stress and interruption of maternal care have also been shown to impact the gut microbiota of offspring in mice [25,30,32,33,34]. Collectively, this body of evidence suggests an association between social factors and the microbiome, encouraging studies of these relations in humans.
Research to date on social factors and the microbiome in humans is limited. Socioeconomic status (SES) is a factor that reflects economic resources such as education, income, and occupation. As SES is related to living conditions, psychosocial stress, and nutrition, it is likely that SES plays a major role in influencing the gut microbiome [35,36]. A study of forty-four healthy adults found that lower neighborhood-level SES in Chicago, Illinois was associated with reduced alpha-diversity, greater abundance of taxa associated with the genus Bacteroides, and lower abundance of taxa associated with the genus Prevotella in the gut microbiota [37]. Bowyer et al. (2019) extended this work using a large sample of adult twins in the United Kingdom. This study found associations between individual and area-level income and relative abundance of operational taxonomic units (OTUs) in the gut microbiome [38]. They also found individual and area-level incomes were linked to microbial composition and lower alpha diversity [38]. However, much less research has investigated the relationships between SES and gut microbiome composition in children.
These two studies are an important first step in describing associations of SES and the microbiome. The current study extends this work by testing the associations between family SES with relative abundance of genera and diversity in the gut microbiome of infants and children while controlling for potential genetic associations. We use genera previously associated with SES in adults [38] in a structural equation model framework. Genetic associations were controlled for with polygenetic scores (PGS) generated from the most recent and largest microbiome GWAS findings [20]. Although cross-sectional data cannot be used to demonstrate causality, structural models yield fit indices that represent the fit of the data to the hypothesized model.
2. Materials and Methods
2.1. Demographics and Family SES
Demographic and socioeconomic characteristics (child age, child sex, parental education, and birth type) were collected by parental-report. Family SES was measured by averaging paternal and maternal education [39]. Education levels were coded as follows: Less Than Seventh Grade = 1; Junior High School = 2; Partial High School = 3; High School Graduate = 4; Partial College or Specialized Training = 5; College Graduate = 6; Graduate Training = 7. Written consent was obtained from parents or legal guardians in accordance with ethics approval from the host institution’s Institutional Review Board.
2.2. SNP Microarray and Polygenic Scores (PGS)
Saliva was collected from participants in the lab using Oragene (DNA Genotek, Ottawa, ON, Canada) saliva collection kits. DNA was extracted with a standard isolation kit (DNA Genotek’s PT-L2P-5). Sample yield and purity were assessed spectrophotometrically using NanoDrop ND-1000 (ThermoScientific, Wilmington, DE, USA) methods. Genotyping of the Multi-Ethnic Global Array (MEGA, >1.7 million markers) run on an Illumina iScanSystem (Illumina, San Diego, CA, USA) was conducted at the Translational Genomics Research Institution (TGen, Phoenix, AZ, USA). Initial genotype definitions were based on auto-clustering all samples that had call rate >0.98 using the GenomeStudio software (2.0). Following genotype calling on all samples, VCF files were imported to the TOPMed Imputation Server [40] and built with the hg38 reference for whole genome imputation followed by a liftover to build hg19 for PGS.
PGS were generated according to standardized, published methods [41]. In summary, using the ‘’P/A’’ variants discovered by Hughes et al. (2020), the count of each effect allele was multiplied by the natural log of the odds ratio for that allele and then summed across all SNPs for each individual. The sum of all allelic effects represents the PGS.
2.3. Stool Sample Collection and Handling
Stool samples were collected by parents in OMR-200 tubes (OMNIgene GUT, DNA Genotek, Ottawa, Ontario, CA, USA), stored on ice, and brought within 24 h to the laboratory in RI where they were immediately frozen at −80 °C. Stool samples were not collected if the infant had taken antibiotics within the last two weeks. Samples were transported to Wellesley College (Wellesley, MA, USA) on dry ice for further processing.
2.4. DNA Extraction and Sequencing of Metagenomes
Nucleic acids were extracted from 200 µL of each stool sample using the RNeasy PowerMicrobiome kit automated on the QIAcube (Qiagen, Germantown, MD, USA), excluding the DNA degradation steps. Cell lysing steps were performed using the Qiagen PowerLyzer 24 Homogenizer (Qiagen, Germantown, MD, USA) at 2500 speed for 45 s, then samples were transferred to the QIAcube to complete the protocol, and extracted DNA was eluted in a final volume of 100 µL. Extracted DNA was sequenced at the Integrated Microbiome Resource (IMR, Dalhousie University, NS, Canada) [42]. To sequence metagenomes, a pooled library (max. 96 samples per run) was prepared using the Illumina Nextera Flex Kit for MiSeq and NextSeq (a PCR-based library preparation procedure) from 1 ng of each sample where samples were enzymatically sheared and tagged with adaptors, PCR amplified while adding barcodes, purified using columns or beads, and normalized either using Illumina beads or manually. Samples were then pooled onto a plate and sequenced on the Illumina NextSeq 550 platform using 150 + 150 bp paired-end “high output” chemistry, generating ~400 million raw reads and ~120 Gb of sequence. The average sequencing depth per sample was 7,738,479. Samples were deposited in NCBI Genbank under Bioproject PRJNA695570.
2.5. Analyzing Metagenomes
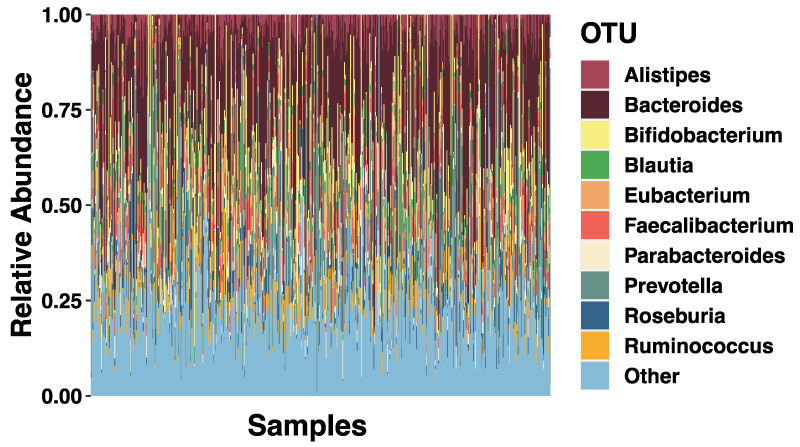
Metagenomic data were analyzed using bioBakery workflows with all necessary dependencies and default parameters [43]. Briefly, KneadData (v0.7.10) was used to trim and filter raw sequence reads, and to separate human and 16S ribosomal gene reads from bacterial sequences in fecal samples. Samples that passed quality control were taxonomically profiled to the genus level using MetaPhlAn (v3.0.7) [44]. Full taxonomic breakdown at the genus level showing top ten microorganisms can be found in Figure 1.
Figure 1.
Full Sample Taxonomic Summaries. Stacked bar plots showing the average relative abundance of the top ten. Different colored bars represent different genus (indicated by the key). Any other genus are classified as ‘’Other’’.
2.6. Structural Equation Modeling
Using the lavaan [45] package in R [46], a latent variable path model within the structural equation modeling (SEM) framework was used to investigate relationships between family SES and the gut microbiome in infants and young children. SEM is a multivariate method where complex relationships between exposures and outcome variables can be estimated simultaneously in a single model, with error measured separately. A latent variable path model is a statistical model of hypothesized relationships among a set of latent and observed variables. In statistics, latent variables are variables that are not directly observed but are rather inferred from other directly measured variables. Latent variables represent “shared” variance, or the degree to which variables “move” together, therefore, variables that have no correlation cannot result in a latent construct. The use of latent variables can serve to reduce the dimensionality of data since many observable variables can be aggregated into a single latent variable.
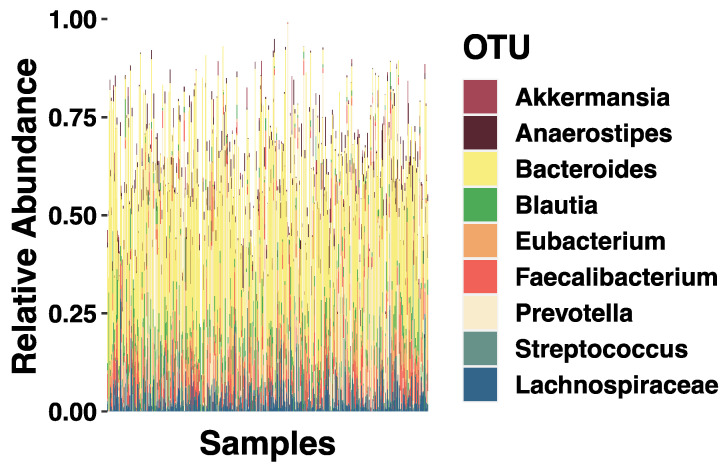
The underlying theoretical framework includes assumptions about the causality of relationships suggested by the literature such that early environmental exposures influence microbiome structure. The latent variable SEM can easily incorporate covariates such as sex, age, birth type, and sequencing depth to examine their influences on the underlying microbiome composition. Relationships are estimated by solving regression-style equations based on a variance-covariance matrix and all correlations between variables are modeled [47]. This is an advantage in handling microbiota relative abundance data since profiles derived from sequencing data are inherently relative and correlated [48,49]. While SEM is still a relatively novel statistical approach with microbiome data, others have had success with it [50,51]. Taxonomic breakdown of the genera assessed in this study can be found in Figure 2.
Figure 2.
SEM Model Taxonomic Summaries. Stacked bar plots showing the average relative abundance of the genera assessed with socioeconomic status (SES). Different colored bars represent different genus (indicated by the key).
Participant data were chosen based on available microbiome data. For SEM, all other variables were subjected to full information maximum likelihood (FIML) estimation, which has been shown to be superior compared to listwise deletion, pairwise deletion, and similar response pattern imputation [52]. The basic premise of FIML is that instead of imputing the values of missing data, we estimate missing values by determining the value that maximizes the likelihood function based on the sample data that we have.
Model goodness of fit (GOF) was evaluated jointly by two commonly used fit indices, root mean square error of approximation (RMSEA) and the standardized root mean square residual (SRMR). GOF was considered acceptable if the RMSEA and SRMR were less than 0.08 [53,54].
2.7. Microbiome Diversity
Alpha diversity measure (Shannon index) was calculated for each individual using the R package vegan. Bray–Curtis dissimilarities, the distances to group centroids, were used as measures of beta diversity, using the function vegdist within vegan. Permutational multivariate analysis of variance (PERMANOVA) was performed with the family SES variable (9999 permutations) within vegan to test associations.
3. Results
3.1. Sample Characteristics
A summary of sample descriptive statistics can be found in Table 1.
Table 1.
Sample descriptive statistics.
| Variable | N | Mean (SD) or % | Range |
|---|---|---|---|
| Metagenomics | 588 | - | - |
| Age (years) | 315 | 4.5 (3.63) | 1 m–15 y |
| Sex (Female) | 547 | 45% | - |
| Socioeconomic status (SES) | 434 | 4.2 (1.87) | 1–7 |
| PGS | 358 | 0.36 (1.42) | −2.72–2.79 |
| Birth type | 370 | 69% (Vaginal) | - |
| Race | 406 | 60.6% White; 26.8% Mixed; 7.6% African American; 1.2% Asian; 1.2% Native American; 2.5% Declined | - |
| --Alpha-Diversity (Shannon) | 588 | 2.05 (0.56) | 0.09–3.02 |
3.2. SES and Relative Abundance
The primary aim of the present study was to examine the relations between SES with childhood microbiome abundance and diversity. To test these predictions, we used the lavaan package in R, a structural equation modeling program. As a first step in our analyses, we tested a measurement model with one latent variable, indicated by the relative abundance of the genera Akkermansia, Anaerostipes, Bacteroides, Blautia, Eubacterium, Faecalibacterium, Lachnospiraceae, Prevotella, and Streptococcus. The initial model was based on the predefined theoretical framework and then trimmed by dropping indicators that were not statistically significant, specifically Akkermansia, Prevotella, Streptococcus, and Blautia from the model to improve model fit. The revised model fit the data well (RMSEA = 0.068, SRMR = 0.036), was a significant improvement from the first model (χ2Δ[22] = 332.43, p < 0.00001), and provided a basis for further model testing. All loadings were significant (all p’s < 0.01).
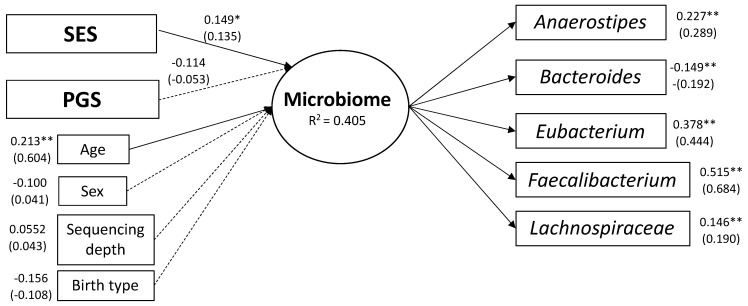
Next, we added SES, PGS, child sex, child age, birth type, and sequencing depth as predictors of the microbiome latent variable. The hypothesized model fit the data well (CFI = 0.811; RMSEA = 0.062, SRMR = 0.047; Figure 1). SES was a significant predictor of the latent microbiome factor (β = 0.135, p < 0.05). PGS was not a significant predictor of the microbiome latent factor (p > 0.05). Of all the covariates, only child age was a significant predictor (β = 0.604, p < 0.001). The full model and results can be found in Figure 3.
Figure 3.
Latent Variable Path Model-Socioeconomic Status (SES) and Microbiome. Gut microbiome genera previously associated with SES in adulthood load onto a single latent variable which is predicted by SES and age in young children. The shapes in the graph represent variables where squares are observed variables and circles are latent variables. The single headed arrows are regression effects, solid lines indicates a significant path and dashed line indicates non-significance. Unstandardized estimates are above the standardized estimates, which are in parentheses. * p < 0.05, ** p < 0.001. RMSEA = 0.062; SRMR = 0.047.
3.3. Alpha Diversity
Using a linear regression model, we tested if Shannon index (alpha diversity) was predicted by SES with the covariates of child’s age, child’s sex, birth type, and sequencing depth. SES was not a significant predictor of the Shannon index (p > 0.05). Of all the covariates, as expected, only child age was a significant predictor of alpha diversity ((β = 0.061, p < 0.001).
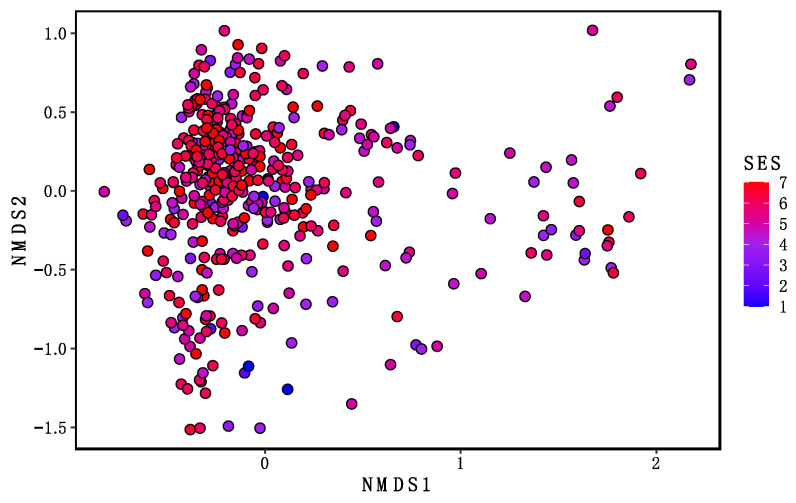
3.4. Beta Diversity
Examining intra-individual (beta) microbiome diversity, we found significant differences across SES for Bray–Curtis dissimilarity (F(1, 432) = 8.46, p = 0.0001; R2 = 0.0192; Figure 4). This suggests a difference in microbiota community composition across SES levels.
Figure 4.
Socioeconomic Status (SES) and Beta Diversity. Beta diversity was calculated based on Bray-Curtis Dissimilarity Distances and visualized using a Non-metric Multidimensional Scaling (NMDS) plot. The NMDS plot projects dissimilarity onto a plane with the two axes representing the largest variance. Data points represent individual beta-diversity values and have been colored by SES score to visualize the relationship between SES and beta-diversity. F(1, 432) = 8.46, p = 0.0001; R2 = 0.0192; Stress value = 0.17.
4. Discussion
Although studies have investigated the relation between SES and gut microbiome in adults and many studies have investigated different lifestyle factors and the gut microbiome in early infancy [5,6,55,56,57], knowledge on the associations between SES and gut microbiome in young children is lacking. This study focused on evaluating the associations between family SES and child genetics with the bacterial community structure of the gut microbiome in a cohort of infants and children. Using SEM, we found similar relationships between SES and composition of the gut microbiome at the genera level to the composition reported in previous studies of adults [37,38].
Using genera associated with SES in adulthood, we tested the association between nine microorganisms and SES in a latent variable path model. We found Anaerostipes, Bacteroides, Eubacterium, Faecalibacterium, and Lachnospiraceae all significantly load onto a single latent factor that was predicted by SES and by child’s age. The average relation across our sample between SES and microbiome was 0.15 (Figure 3). Parents with higher years of education had children who scored higher on the latent microbiome factor. That is, they were higher on Faecalibacterium, Eubacterium, Anaerostipes, and Lachnospiraceae, and lower on Bacteroides. These results align well with previous studies that found associations with adult individual—or area—SES with relative abundance of these genera.
Of note, the genera Faecalibacterium had the highest factor loading (0.68). The genus Faecalibacterium belongs to the family of Ruminococcaceae. F. prausnitzii, a species belonging to this genera, is considered a key marker for a healthy gut and has the ability to produce butyrate, a short chain fatty acid, by consuming acetate [58,59]. Butyrate is an energy source for the colonic epithelium and plays a major role in gut physiology and has several beneficial effects for health including protection against pathogens, modulation of immune system, and reduction of cancer progression [60]. One study in six-year-olds found non-smoking mothers, vaginal birth, and high family SES were all associated with increased relative abundance of Faecalibacterium [61]. Together, with the findings of this study, this suggests that Faecalibacterium abundance may be susceptible to a wide range of environmental factors. Therefore, Faecalibacterium abundance may be one biological pathway in which early environmental influences shape disease vulnerability through life.
Alpha diversity captures the diversity of species, or the evenness and richness of microbial composition [62]. Reduced alpha diversity has been associated with brain-based disorders in adulthood such as Alzheimer’s disease and major depressive disorder, and in children with attention-deficit/hyperactivity disorder (ADHD) [63,64,65]. We found that alpha diversity increases with age, as has been shown in other studies [66,67]. However, our results showed no association between family SES and the overall composition of the gut microbiome in infants and young children (alpha diversity). This is consistent with another study that reported no association between family SES and alpha diversity in six-year-olds [61]. These findings depart from two studies in adults that found family and neighborhood-level SES were associated with alpha diversity in adults [37,38]. Interestingly, this pattern of findings suggests that microbiome alpha diversity may not be sensitive to the impact of SES until a later developmental stage. However, we did find that SES significantly predicts beta-diversity, as measured by Bray–Curtis dissimilarity, suggesting gut microbiome diversity is influenced by family SES in childhood to some degree. These findings may have important implications for understanding how interventions in childhood could help prevent the eventual impact of SES on microbiome diversity and subsequent health.
Interest in the interplay between host genetics and the gut microbiome is increasing, with many GWAS studies to date [16,17,18,19,20,21]. Polygenic scores are calculated by summing the number of risk alleles, which are weighted by effect sizes derived from GWAS results [41]. Polygenic studies have demonstrated modest prediction for many complex phenotypes including blood pressure [68,69], height [70], diabetes [71], obesity [72], ADHD [73], depression [74], and schizophrenia [75]. A recent study found the polygenic score for arthritis was associated with the presence of Prevotella spp. in the microbiome [76]. Using the most recent and largest-to-date microbiome GWAS study [20], we calculated individual PGSs. We did not find an association between the PGS and microbiome composition in children, suggesting that SES may have more impact than genetics at this age. However, there are multiple explanations for this null finding. One of the major reasons may be the limited number of microorganisms assessed in this study, perhaps the PGS may be associated with genera not included here. Another interesting possibility is that the genetic influence on microbiome composition may have a specific developmental window. In other words, a PGS based on a GWAS conducted in adults may not be associated with microbiome composition in childhood. In addition, other factors such as ethnic differences between studies, gene-environment interactions, and dissimilarity in sequencing methods, might also make it difficult to detect a genetic association with microbiome composition in this study.
There are some limitations of the current study to address. As we only had two indicators of family SES, we used a manifest composite variable rather than a latent factor in the model. Use of a manifest variable representing family SES likely underestimated the association with microbiome, as it included measurement error. Using maternal and paternal education as a measure of SES may have imperfect representation of this complex variable. Future studies should consider incorporating other indicators of family SES such as income, occupation, and area-level metrics. Further, we did not have access to diet variables such as food quantity/quality or diversity, which could be driving the associations observed with SES. Since SES is associated with a variety of lifestyle factors such as medication use, pet ownership [5], psychosocial stress [77], and host environment [9,78], we are unable to determine which of these factors is driving associations with microbiome metrics. Associations found with SES in this study were small in magnitude. This may be due to the restricted SES range in our volunteer longitudinal cohort which are known to be biased towards higher SES households. While detailed information on the history of antibiotic use is missing in this study, we did exclude any participants who reported antibiotic use within two weeks prior to collection.
5. Conclusions
Our results demonstrate that modifiable environmental factors, such as SES, may influence gut microbiome composition at an early age. Further, our results suggest that host genetics are not associated with the taxa tested in early life. These results are important as the understanding of gut microbiome-host health relationships continue to expand. Our future research will explore if children’s microbiome mediates the well-established relationships between SES and children’s academic and health functioning.
Author Contributions
Conceptualization, C.R.L., K.S.B., K.L.-C., S.K.H. and V.K.-C.; methodology, C.R.L., K.S.B., K.L.-C. and V.K.-C.; validation, K.S.B. and S.H.M.; formal analysis, C.R.L., K.S.B., M.D.D.B. and M.N.; investigation, C.R.L., K.S.B., M.J.H., S.H.M., A.R.V., V.D., M.J.H. and S.C.L.D.; resources, C.R.L., S.C.L.D. and V.K.-C.; data curation, C.R.L. and K.S.B.; writing—original draft preparation, C.R.L.; writing—review and editing, C.R.L., K.S.B., K.L.-C., S.K.H. and V.K.-C.; visualization, C.R.L. and K.L.-C.; supervision, M.J.H., K.L.-C., S.K.H., S.C.L.D. and V.K.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Environmental Influences on Child Health Outcomes (ECHO), National Institutes of Health, grant number UG3OD023313; National Institutes of Health, grant number R34-DA050284; NICHD NIH, grant number 1K99HD099307-01A1.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Brown University (IRB#: 1500991 approval renewed 09/09/2020).
Informed Consent Statement
Informed consent was obtained from all subjects and/or guardians involved in the study.
Data Availability Statement
Samples were deposited in NCBI Genbank under Bioproject PRJNA695570.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cryan J.F., O’Riordan K.J., Sandhu K., Peterson V., Dinan T.G. The gut microbiome in neurological disorders. Lancet Neurol. 2020;19:179–194. doi: 10.1016/S1474-4422(19)30356-4. [DOI] [PubMed] [Google Scholar]
- 2.Singhvi N., Gupta V., Gaur M., Sharma V., Puri A., Singh Y., Dubey G.P., Lal R. Interplay of Human Gut Microbiome in Health and Wellness. Indian J. Microbiol. 2019;60:26–36. doi: 10.1007/s12088-019-00825-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shreiner A.B., Kao J.Y., Young V.B. The gut microbiome in health and in disease. Curr. Opin. Gastroenterol. 2015;31:69–75. doi: 10.1097/MOG.0000000000000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gilbert J.A., Blaser M.J., Caporaso J.G., Jansson J., Lynch S.V., Knight R. Current understanding of the human microbiome. Nat. Med. 2018;24:392–400. doi: 10.1038/nm.4517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim H., Sitarik A.R., Woodcroft K., Johnson C.C., Zoratti E. Birth Mode, Breastfeeding, Pet Exposure, and Antibiotic Use: Associations with the Gut Microbiome and Sensitization in Children. Curr. Allergy Asthma Rep. 2019;19:1–9. doi: 10.1007/s11882-019-0851-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sbihi H., Boutin R., Cutler C., Suen M., Finlay B.B., Turvey S.E. Thinking bigger: How early-life environmental exposures shape the gut microbiome and influence the development of asthma and allergic disease. Allergy. 2019;74:2103–2115. doi: 10.1111/all.13812. [DOI] [PubMed] [Google Scholar]
- 7.Rothschild D., Weissbrod O., Barkan E., Kurilshikov A., Korem T., Zeevi D., Costea P.I., Godneva A., Kalka I.N., Bar N., et al. Environment dominates over host genetics in shaping human gut microbiota. Nat. Cell Biol. 2018;555:210–215. doi: 10.1038/nature25973. [DOI] [PubMed] [Google Scholar]
- 8.Turnbaugh P., Hamady M., Yatsunenko T., Cantarel B.L., Duncan A., Ley R., Sogin M.L., Jones W.J., Roe B.A., Affourtit J.P., et al. A core gut microbiome in obese and lean twins. Nat. Cell Biol. 2008;457:480–484. doi: 10.1038/nature07540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yatsunenko T., Rey F.E., Manary M., Trehan I., Dominguez-Bello M.G., Contreras M., Magris M., Hidalgo G., Baldassano R.N., Anokhin A., et al. Human gut microbiome viewed across age and geography. Nat. Cell Biol. 2012;486:222–227. doi: 10.1038/nature11053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodrich J.K., Davenport E., Beaumont M., Jackson M., Knight R., Ober C., Spector T.D., Bell J., Clark A., Ley R.E. Genetic Determinants of the Gut Microbiome in UK Twins. Cell Host Microbe. 2016;19:731–743. doi: 10.1016/j.chom.2016.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goodrich J.K., Waters J.L., Poole A., Sutter J.L., Koren O., Blekhman R., Beaumont M., Van Treuren W., Knight R., Bell J., et al. Human Genetics Shape the Gut Microbiome. Cell. 2014;159:789–799. doi: 10.1016/j.cell.2014.09.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Benson A.K., Kelly S.A., Legge R., Ma F., Low S.J., Kim J., Zhang M., Oh P.L., Nehrenberg D., Hua K., et al. Individuality in gut microbiota composition is a complex polygenic trait shaped by multiple environmental and host genetic factors. Proc. Natl. Acad. Sci. USA. 2010;107:18933–18938. doi: 10.1073/pnas.1007028107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKnite A., Perez-Munoz M.E., Lu L., Williams E., Brewer S., Andreux P.A., Bastiaansen J., Wang X., Kachman S., Auwerx J., et al. Murine Gut Microbiota Is Defined by Host Genetics and Modulates Variation of Metabolic Traits. PLoS ONE. 2012;7:e39191. doi: 10.1371/journal.pone.0039191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leamy L.J., Kelly S.A., Nietfeldt J., Legge R.M., Ma F., Hua K., Sinha R., Peterson D.A., Walter J., Benson A.K., et al. Host genetics and diet, but not immunoglobulin A expression, converge to shape compositional features of the gut microbiome in an advanced intercross population of mice. Genome Biol. 2014;15:552. doi: 10.1186/s13059-014-0552-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blekhman R., Goodrich J.K., Huang K., Sun Q., Bukowski R., Bell J.T., Spector T.D., Keinan A., Ley R.E., Gevers D., et al. Host genetic variation impacts microbiome composition across human body sites. Genome Biol. 2015;16:1–12. doi: 10.1186/s13059-015-0759-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davenport E., Cusanovich D., Michelini K., Barreiro L., Ober C., Gilad Y. Genome-Wide Association Studies of the Human Gut Microbiota. PLoS ONE. 2015;10:e0140301. doi: 10.1371/journal.pone.0140301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bonder M.J., Kurilshikov A., Tigchelaar E.F., Mujagic Z., Imhann F., Vila A.V., Deelen P., Vatanen T., Schirmer M., Smeekens S.P., et al. The effect of host genetics on the gut microbiome. Nat. Genet. 2016;48:1407–1412. doi: 10.1038/ng.3663. [DOI] [PubMed] [Google Scholar]
- 18.Wang J., Thingholm L.B., Skiecevičienė J., Rausch P., Kummen M., Hov J.R., Degenhardt F., Heinsen F.-A., Rühlemann M.C., Szymczak S., et al. Genome-wide association analysis identifies variation in vitamin D receptor and other host factors influencing the gut microbiota. Nat. Genet. 2016;48:1396–1406. doi: 10.1038/ng.3695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Turpin W., GEM Project Research Consortium. Espin-Garcia O., Xu W., Silverberg M.S., Kevans D., Smith M.I., Guttman D.S., Griffiths A., Panaccione R., et al. Association of host genome with intestinal microbial composition in a large healthy cohort. Nat. Genet. 2016;48:1413–1417. doi: 10.1038/ng.3693. [DOI] [PubMed] [Google Scholar]
- 20.Hughes D.A., Bacigalupe R., Wang J., Rühlemann M.C., Tito R.Y., Falony G., Joossens M., Vieira-Silva S., Henckaerts L., Rymenans L., et al. Genome-wide associations of human gut microbiome variation and implications for causal inference analyses. Nat. Microbiol. 2020;5:1079–1087. doi: 10.1038/s41564-020-0743-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu F., Fu Y., Sun T.-Y., Jiang Z., Miao Z., Shuai M., Gou W., Ling C.-W., Yang J., Wang J., et al. The interplay between host genetics and the gut microbiome reveals common and distinct microbiome features for complex human diseases. Microbiome. 2020;8:1–14. doi: 10.1186/s40168-020-00923-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Foster J.A., Rinaman L., Cryan J.F. Stress & the gut-brain axis: Regulation by the microbiome. Neurobiol. Stress. 2017;7:124–136. doi: 10.1016/j.ynstr.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moeller A.H., Foerster S., Wilson M.L., Pusey A.E., Hahn B.H., Ochman H. Social behavior shapes the chimpanzee pan-microbiome. Sci. Adv. 2016;2:e1500997. doi: 10.1126/sciadv.1500997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amato K.R., Van Belle S., Di Fiore A., Estrada A., Stumpf R., White B., Nelson K.E., Knight R., Leigh S. Patterns in Gut Microbiota Similarity Associated with Degree of Sociality among Sex Classes of a Neotropical Primate. Microb. Ecol. 2017;74:250–258. doi: 10.1007/s00248-017-0938-6. [DOI] [PubMed] [Google Scholar]
- 25.Amaral W.Z., Lubach G.R., Proctor A., Lyte M., Phillips G.J., Coe C.L. Social Influences on Prevotella and the Gut Microbiome of Young Monkeys. Psychosom. Med. 2017;79:888–897. doi: 10.1097/PSY.0000000000000454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tung J., Barreiro L., Burns M., Grenier J.-C., Lynch J., Grieneisen L.E., Altmann J., Alberts S.C., Blekhman R., Archie E.A. Social networks predict gut microbiome composition in wild baboons. eLife. 2015;4:e05224. doi: 10.7554/eLife.05224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bailey M.T. Psychological Stress, Immunity, and the Effects on Indigenous Microflora. Microb. Endocrinol. Interkingdom Signal. Infect. Dis. Health. 2016;874:225–246. doi: 10.1007/978-3-319-20215-0_11. [DOI] [PubMed] [Google Scholar]
- 28.Grzywacz J., Almeida D.M., Neupert S.D., Ettner S.L. Socioeconomic Status and Health: A Micro-level Analysis o Exposure and Vulnerability to Daily Stressors. J. Health Soc. Behav. 2004;45:1–16. doi: 10.1177/002214650404500101. [DOI] [PubMed] [Google Scholar]
- 29.Tannock G.W., Savage D.C. Influences of dietary and environmental stress on microbial populations in the murine gastrointestinal tract. Infect. Immun. 1974;9:591–598. doi: 10.1128/iai.9.3.591-598.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bailey M.T., Dowd S., Galley J.D., Hufnagle A.R., Allen R.G., Lyte M. Exposure to a social stressor alters the structure of the intestinal microbiota: Implications for stressor-induced immunomodulation. Brain, Behav. Immun. 2011;25:397–407. doi: 10.1016/j.bbi.2010.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sudo N., Chida Y., Aiba Y., Sonoda J., Oyama N., Yu X.-N., Kubo C., Koga Y. Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J. Physiol. 2004;558:263–275. doi: 10.1113/jphysiol.2004.063388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O’Mahony S.M., Marchesi J., Scully P., Codling C., Ceolho A.-M., Quigley E.M., Cryan J., Dinan T. Early Life Stress Alters Behavior, Immunity, and Microbiota in Rats: Implications for Irritable Bowel Syndrome and Psychiatric Illnesses. Biol. Psychiatry. 2009;65:263–267. doi: 10.1016/j.biopsych.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 33.Jašarević E., Howerton C.L., Howard C.D., Bale T.L. Alterations in the Vaginal Microbiome by Maternal Stress Are Associated With Metabolic Reprogramming of the Offspring Gut and Brain. Endocrinol. 2015;156:3265–3276. doi: 10.1210/en.2015-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bailey M.T., Coe C.L. Maternal separation disrupts the integrity of the intestinal microflora in infant rhesus monkeys. Dev. Psychobiol. 1999 doi: 10.1002/(SICI)1098-2302(199909)35:2<146::AID-DEV7>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 35.Dowd J.B., Renson A. “Under the Skin” and into the Gut: Social Epidemiology of the Microbiome. Curr. Epidemiology Rep. 2018;5:432–441. doi: 10.1007/s40471-018-0167-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Herd P., Palloni A., Rey F., Dowd J. Social and population health science approaches to understand the human microbiome. Nat. Hum. Behav. 2018;2:808–815. doi: 10.1038/s41562-018-0452-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miller G.E., Engen P.A., Gillevet P.M., Shaikh M., Sikaroodi M., Forsyth C.B., Mutlu E., Keshavarzian A. Lower Neighborhood Socioeconomic Status Associated with Reduced Diversity of the Colonic Microbiota in Healthy Adults. PLoS ONE. 2016;11:e0148952. doi: 10.1371/journal.pone.0148952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bowyer R.C.E., Jackson M.A., Le Roy C.I., Ni Lochlainn M., Spector T.D., Dowd J.B., Steves C.J. Socioeconomic Status and the Gut Microbiome: A TwinsUK Cohort Study. Microorg. 2019;7:17. doi: 10.3390/microorganisms7010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jankovic J., Stojisavljević D., Erić M., Marinković J. Association of socioeconomic status measured by education, and cardiovascular health: A population-based cross-sectional study. BMJ Open. 2014;4:e005222. doi: 10.1136/bmjopen-2014-005222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taliun D., NHLBI Trans-Omics for Precision Medicine (TOPMed) Consortium. Harris D.N., Kessler M.D., Carlson J., Szpiech Z.A., Torres R., Taliun S.A.G., Corvelo A., Gogarten S.M., et al. Sequencing of 53,831 diverse genomes from the NHLBI TOPMed Program. Nat. Cell Biol. 2021;590:290–299. doi: 10.1038/s41586-021-03205-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marees A.T., De Kluiver H., Stringer S., Vorspan F., Curis E., Marie-Claire C., Derks E. A tutorial on conducting genome-wide association studies: Quality control and statistical analysis. Int. J. Methods Psychiatr. Res. 2018;27:e1608. doi: 10.1002/mpr.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Comeau A.M., Douglas G.M., Langille M.G.I. Microbiome Helper: A Custom and Streamlined Workflow for Microbiome Research. mSystems. 2017;2:e00127-16. doi: 10.1128/mSystems.00127-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McIver L.J., Abu-Ali G., Franzosa E.A., Schwager R., Morgan X.C., Waldron L., Segata N., Huttenhower C. bioBakery: A meta’omic analysis environment. Bioinform. 2017;34:1235–1237. doi: 10.1093/bioinformatics/btx754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Beghini F., McIver L.J., Blanco-Míguez A., Dubois L., Asnicar F., Maharjan S., Mailyan A., Manghi P., Scholz M., Thomas A.M., et al. Integrating taxonomic, functional, and strain-level profiling of diverse microbial communities with bioBakery 3. eLife. 2021;10 doi: 10.7554/eLife.65088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rosseel Y. lavaan: AnRPackage for Structural Equation Modeling. J. Stat. Softw. 2012;48:1–36. doi: 10.18637/jss.v048.i02. [DOI] [Google Scholar]
- 46.R Core Team . R: A Language and Environment for Statistical Computing. R Core Team; Vienna, Austria: 2020. [Google Scholar]
- 47.Weston R., Gore P.A. A Brief Guide to Structural Equation Modeling. Couns. Psychol. 2006;34:719–751. doi: 10.1177/0011000006286345. [DOI] [Google Scholar]
- 48.Lovén J., Orlando D.A., Sigova A.A., Lin C.Y., Rahl P.B., Burge C.B., Levens D.L., Lee T.I., Young R.A. Revisiting Global Gene Expression Analysis. Cell. 2012;151:476–482. doi: 10.1016/j.cell.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gloor G.B., Macklaim J.M., Pawlowsky-Glahn V., Egozcue J.J. Microbiome Datasets Are Compositional: And This Is Not Optional. Front. Microbiol. 2017;8:2224. doi: 10.3389/fmicb.2017.02224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wu X., Berkow K., Frank D.N., Li E., Gulati A.S., Zhu W. Comparative analysis of microbiome measurement platforms using latent variable structural equation modeling. BMC Bioinform. 2013;14:79. doi: 10.1186/1471-2105-14-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vu K., Lou W., Tun H.M., Konya T.B., Morales-Lizcano N., Chari R.S., Field C.J., Guttman D.S., Mandal R., Wishart D.S., et al. From Birth to Overweight and Atopic Disease: Multiple and Common Pathways of the Infant Gut Microbiome. Gastroenterol. 2021;160:128–144.e10. doi: 10.1053/j.gastro.2020.08.053. [DOI] [PubMed] [Google Scholar]
- 52.Enders C., Bandalos D. The Relative Performance of Full Information Maximum Likelihood Estimation for Missing Data in Structural Equation Models. Struct. Equ. Model. A Multidiscip. J. 2001;8:430–457. doi: 10.1207/S15328007SEM0803_5. [DOI] [Google Scholar]
- 53.McDonald R.P., Ho M.-H.R. Principles and practice in reporting structural equation analyses. Psychol. Methods. 2002;7:64–82. doi: 10.1037/1082-989X.7.1.64. [DOI] [PubMed] [Google Scholar]
- 54.Hu L., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 55.Bäckhed F., Roswall J., Peng Y., Feng Q., Jia H., Kovatcheva-Datchary P., Li Y., Xia Y., Xie H., Zhong H., et al. Dynamics and Stabilization of the Human Gut Microbiome during the First Year of Life. Cell Host Microbe. 2015;17:690–703. doi: 10.1016/j.chom.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 56.Fernández L., Langa S., Martin V., Maldonado A., Jiménez E., Martín R., Rodríguez J.M. The human milk microbiota: Origin and potential roles in health and disease. Pharmacol. Res. 2013;69:1–10. doi: 10.1016/j.phrs.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 57.Vangay P., Ward T., Gerber J.S., Knights D. Antibiotics, Pediatric Dysbiosis, and Disease. Cell Host Microbe. 2015;17:553–564. doi: 10.1016/j.chom.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Martin R., Miquel S., Benevides L., Bridonneau C., Robert V., Hudault S., Chain F., Berteau O., Azevedo V., Chatel J.M., et al. Functional Characterization of Novel Faecalibacterium prausnitzii Strains Isolated from Healthy Volunteers: A Step Forward in the Use of F. prausnitzii as a Next-Generation Probiotic. Front. Microbiol. 2017;8:1226. doi: 10.3389/fmicb.2017.01226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fitzgerald C.B., Shkoporov A.N., Sutton T.D.S., Chaplin A.V., Velayudhan V., Ross R.P., Hill C. Comparative analysis of Faecalibacterium prausnitzii genomes shows a high level of genome plasticity and warrants separation into new species-level taxa. BMC Genom. 2018;19:1–20. doi: 10.1186/s12864-018-5313-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Miquel S., Martin R., Rossi O., Humaran L.G.B., Chatel J., Sokol H., Thomas M., Wells J., Langella P. Faecalibacterium prausnitzii and human intestinal health. Curr. Opin. Microbiol. 2013;16:255–261. doi: 10.1016/j.mib.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 61.Gschwendtner S., Kang H., Thiering E., Kublik S., Foesel B., Schulz H., Krauss-Etschmann S., Heinrich J., Schöler A., Schloter M., et al. Early life determinants induce sustainable changes in the gut microbiome of six-year-old children. Sci. Rep. 2019;9:1–9. doi: 10.1038/s41598-019-49160-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hagerty S.L., Hutchison K.E., Lowry C.A., Bryan A.D. An empirically derived method for measuring human gut microbiome alpha diversity: Demonstrated utility in predicting health-related outcomes among a human clinical sample. PLoS ONE. 2020;15:e0229204. doi: 10.1371/journal.pone.0229204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vogt N.M., Kerby R.L., Dill-McFarland K.A., Harding S.J., Merluzzi A.P., Johnson S.C., Carlsson C.M., Asthana S., Zetterberg H., Blennow K., et al. Gut microbiome alterations in Alzheimer’s disease. Sci. Rep. 2017;7:1–11. doi: 10.1038/s41598-017-13601-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Prehn-Kristensen A., Zimmermann A., Tittmann L., Lieb W., Schreiber S., Baving L., Fischer A. Reduced microbiome alpha diversity in young patients with ADHD. PLoS ONE. 2018;13:e0200728. doi: 10.1371/journal.pone.0200728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jiang H., Ling Z., Zhang Y., Mao H., Ma Z., Yin Y., Wang W., Tang W., Tan Z., Shi J., et al. Altered fecal microbiota composition in patients with major depressive disorder. Brain, Behav. Immun. 2015;48:186–194. doi: 10.1016/j.bbi.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 66.Laursen M.F., Andersen L.B.B., Michaelsen K.F., Mølgaard C., Trolle E., Bahl M.I., Licht T.R. Infant Gut Microbiota Development Is Driven by Transition to Family Foods Independent of Maternal Obesity. mSphere. 2016;1:e00069-15. doi: 10.1128/mSphere.00069-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Odamaki T., Kato K., Sugahara H., Hashikura N., Takahashi S., Xiao J.-Z., Abe F., Osawa R. Age-related changes in gut microbiota composition from newborn to centenarian: A cross-sectional study. BMC Microbiol. 2016;16:1–12. doi: 10.1186/s12866-016-0708-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hoffmann T.J., Ehret G.B., Nandakumar P., Ranatunga D., Schaefer C., Kwok P.-Y., Iribarren C., Chakravarti G.B.E.P.N.A., Risch D.R.C.S.C.I.N. Genome-wide association analyses using electronic health records identify new loci influencing blood pressure variation. Nat. Genet. 2016;49:54–64. doi: 10.1038/ng.3715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ehret G.B., CHARGE-EchoGen Consortium. Ferreira T., Chasman D.I., Jackson A.U., Schmidt E., Johnson T., Thorleifsson G., Luan J., Donnelly L.A., et al. The genetics of blood pressure regulation and its target organs from association studies in 342,415 individuals. Nat. Genet. 2016;48:1171–1184. doi: 10.1038/ng.3667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wood A.R., The Electronic Medical Records and Genomics (eMERGE) Consortium. Esko T., Yang J., Vedantam S., Pers T., Gustafsson S., Chu A.Y., Estrada K., Luan J., et al. Defining the role of common variation in the genomic and biological architecture of adult human height. Nat. Genet. 2014;46:1173–1186. doi: 10.1038/ng.3097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Barrett J.C., Clayton D.G., Concannon P., Akolkar B., Cooper J.D., Erlich H.A., Julier C., Morahan G., Nerup J., Nierras C., et al. Genome-wide association study and meta-analysis find that over 40 loci affect risk of type 1 diabetes. Nat. Genet. 2009;41:703–707. doi: 10.1038/ng.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Torkamani A., Topol E. Polygenic Risk Scores Expand to Obesity. Cell. 2019;177:518–520. doi: 10.1016/j.cell.2019.03.051. [DOI] [PubMed] [Google Scholar]
- 73.Ronald A., de Bode N., Polderman T.J. Systematic Review: How the Attention-Deficit/Hyperactivity Disorder Polygenic Risk Score Adds to Our Understanding of ADHD and Associated Traits. J. Am. Acad. Child Adolesc. Psychiatry. 2021 doi: 10.1016/j.jaac.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wray N.R., Ripke S., Mattheisen M., Trzaskowski M., Byrne E.M., Abdellaoui A., Adams M.J., Agerbo E., Air T.M., Andlauer T., et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat. Genet. 2018;50:668–681. doi: 10.1038/s41588-018-0090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Adolfsson R. Biological insights from 108 schizophrenia-associated genetic loci. Nat. Cell Biol. 2014;511:421–427. doi: 10.1038/nature13595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wells P., Adebayo A., Bowyer R.C.E., Freidin M.B., Finckh A., Strowig T., Lesker T.R., Alpízar-Rodríguez D., Gilbert B., Kirkham B., et al. Associations between gut microbiota and genetic risk for rheumatoid arthritis in the absence of disease: A cross-sectional study. Lancet Rheumatol. 2020;2:e418–e427. doi: 10.1016/S2665-9913(20)30064-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tobin C.S.T., Erving C.L., Barve A. Race and SES Differences in Psychosocial Resources: Implications for Social Stress Theory. Soc. Psychol. Q. 2020;84:1–25. doi: 10.1177/0190272520961379. [DOI] [Google Scholar]
- 78.Flies E.J., Skelly C., Negi S.S., Prabhakaran P., Liu Q., Liu K., Goldizen F.C., Lease C., Weinstein P. Biodiverse green spaces: A prescription for global urban health. Front. Ecol. Environ. 2017;15:510–516. doi: 10.1002/fee.1630. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Samples were deposited in NCBI Genbank under Bioproject PRJNA695570.