Abstract
Cutaneous tuberculosis (CTB), a rare manifestation of tuberculosis is one of the most challenging diagnoses to establish. Metastasic tuberculous abscess is a form of CTB which is characterized by cold abscesses on the patient's extremities or trunk without any involvement of underlying tissue. Here we report a case of 56-year-old Bangladeshi male with no previous history of TB, who presented with multiple abscesses over the body for 3 months. His diagnosis was confirmed on the basis of demonstration of Mycobacterium tuberculosis in the lesions by staining, PCR and culture. But no primary focus was found. After 1 month of anti-tubercular therapy, significant improvement was noted.
Keywords: cutaneous tuberculosis, metastasic tuberculous abscess, tuberculous gumma
Introduction
Tuberculosis (TB) is a global health problem that is not limited to developing countries only. TB has resurfaced in recent decades largely due to the pandemic of HIV infection and the emergence of antimicrobial resistance against Mycobacterium tuberculosis (MTB), posing an increased threat to public health and economic development [1].
Cutaneous tuberculosis (CTB) is a rare manifestation of tuberculosis, accounting for 1–1.5% of all extrapulmonary tuberculosis cases and just 8.4–13.7% of all tuberculosis events [2].
With the rise in tuberculosis cases, CTB has re-emerged in areas of the world where HIV infection and the prevalence of multidrug-resistant tuberculosis remain high [3]. Because of the large variations in clinical presentation, histopathology and treatment response, cutaneous tuberculosis (CTB) remains one of the most difficult diagnoses to establish.
Metastasic tuberculous abscess, also known as tuberculous gumma, is a variety of CTB which is characterized by the development of cold abscesses that form on the patient's extremities or trunk without any underlying tissue involvement [4].
Here, we have reported the case of a patient diagnosed with metastatic tuberculous abscess on the background of immunosuppression due to prolonged corticosteroid use without any previous history of tuberculosis.
Case synopsis
A 56-year-old Bangladeshi male, presented with high grade fever and nodular skin lesions for 3 months. The skin lesions first appeared in the thigh followed by involvement of the trunk. Some of the lesions grew larger and ulcerated over time, releasing pus. He received several courses of antibiotics on suspicion of bacterial abscess without any significant improvement. His co-morbidities include hypertension, ischemic heart disease and chronic kidney disease secondary to long standing hypertension. He has been suffering from inflammatory oligoarthritis involving both knee joints and back for the last 2 years, which was labeled as undifferentiated spondyloarthritis. He took a number of NSAIDs and oral corticosteroids (prednislolone 20 mg daily) irregularly for pain relief. Intra-articular steroid injection was given on one occasion six months back. He had lost about six kilograms over 3 months. There was no previous history of TB or contact with known TB patients.
On examination, his face was puffy with central obesity and relatively thin limbs. Thinning of the skin was also noted. There was neither lymphadenopathy nor organomegaly. Warm, tender, nodular lesions of variable size and shape were found in the abdomen (Fig. 1), back and thigh. Some of them were ulcerated. The largest one was located on the back, measuring about 4 × 3 cm (Fig. 2). Both knee joints were swollen with Grade 2 tenderness and there was restricted movement in all directions with positive patellar tap. Muscle bulk and power were reduced symmetrically and proximally in both lower limbs. Muscle tone was unaltered with normal deep tendon reflexes and flexor plantar responses bilaterally.
Fig. 1.
Multiple skin lesions involving abdomen.
Fig. 2.
Largest skin lesion on the back.
Investigations revealed normal blood counts with high ESR (40 mm in 1st hour) and raised CRP (85.83 mg/L). S. creatinine was raised (1.7 mg/dL) and eGFR was low (30 ml/min/1.73 m2). Urinalysis revealed no abnormality. Microscopy and culture of urine for acid fast bacilli (AFB) were negative. Aspiration of pus from skin lesion revealed numerous AFB on staining (Fig. 3). Skin biopsy revealed perivascular infiltration of chronic inflammatory cells with mild acanthosis and exocytosis of epidermis. MTB-PCR of skin biopsy detected MTB DNA which was susceptible to Rifampicin. Culture of pus in Mycobacteria growth indicator tube (MGIT) revealed growth of MTB (Fig. 4). Sputum smear for acid fast bacilli (AFB) and culture for Mycobacterium tuberculosis were negative. High-resolution computed tomography (HRCT) of the chest and colonoscopy were performed to look for the primary focus of TB, but both were found to be normal. CT scan of abdomen and pelvis were normal as well. Tuberculin skin test was negative. A repeat test was performed after 8 weeks which was negative as well. 24 h urinary free cortisol was well above the normal range, measuring 227.05 mcg/day (Normal range: 50–190 mcg/day). Rheumatoid factor, anti-citrullinated protein antibody (ACPA) and HLA-B27 were negative with normal findings in plain X-ray and MRI of both SI joints. Early osteoarthritic changes were noted in plain X-ray of both knee joints.
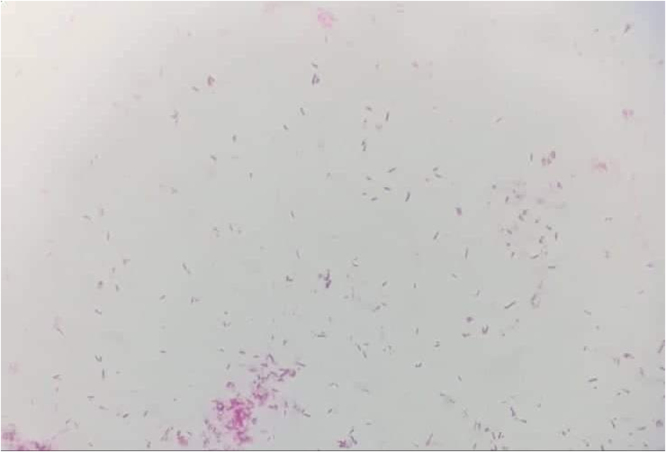
Fig. 3.
ZN staining of pus showing AFB.
Fig. 4.
Growth of MTB in MGIT from pus.
He has been given anti-tubercular therapy comprising isoniazid, rifampicin and pyrazinamide in full dose and ethambutol with renal modification. After one month of taking the anti-tubercular drug, his skin lesions improved significantly.
Discussion
While cutaneous TB remains one of the most difficult diagnoses to make clinically, it should be considered in all cases of chronic skin lesions, especially in HIV-positive patients and those with a history of pulmonary tuberculosis. A wide range of differentials need to be ruled out before reaching definitive diagnosis that include Staphylococcal abscess, atypical mycobacterial infections, sporotrichosis, nocardiosis, cutaneous leishmaniasis, deep fungal infections, syphilitic gumma, leprosy and panniculitis of all forms [5]. In the case of our patient, the chornic non-healing skin lesion, immunocompromised state of the patient, and high prevalence of tuberculosis in this population raised the possibility of cutaneous tuberculosis. Our suspicion was further confirmed by demonstration of bacilli and a good response to anti-tubercular therapy.
Metastatic tuberculous abscess or tuberculous gumma is a multibacillary variant of cutaneous tuberculosis that is caused by the metastatic, hematogenous spread of Mycobacteria. They may remain dormant for an indefinite period until the infection reappears during a period of immunosuppression or malnutrition [4]. In this case, immunosuppression due to prolonged corticosteroid use may have triggered the manifestation of the disease.
The clinical manifestations of metastatic tuberculous abscesses vary widely depending upon the virulence of the organism, route of infection and immunity status of the susceptible host. Single or multiple, tender, cold abscesses with ulceration, fistulae or sporotrichoid pattern are described as the common features. Drainage of pus or caseous material is also frequently observed [6]. Gummas are most commonly found on the limbs, especially the thighs and buttocks. Trunk is also a common site. Presence of abundant fat in these sites may be responsible for this [7]. In the case of our patient, the skin lesions were very much similar to the description in the literature except for increased local temperature that can be explained by secondary bacterial infection.
Other varieties of tuberculosis that can present as ulcers include scrofuloderma, erythema induratum, orificial TB, and occasionally papulonecrotic tuberculid (PNT) [1].
Tuberculous scrofuloderma and orificial TB could not be considered here because there was no clinically evident underlying tuberculous focus. Papulonecrotic tuberculid and erythema induratum, on the other hand, were excluded because they are paucibacillary forms of the disease that are most commonly associated with active tuberculosis infection.
Though tuberculous gumma usually occurs in malnourished people of low socioeconomic status and in patients who are immunosuppressed, several cases in immunocompetent hosts have been reported [6].
A review of 49 case reports of metastatic tuberculous abscess revealed that in almost one fourth of the cases, tuberculous gumma was the sole presentation of tuberculosis and search for a primary location had been given emphasis [7].
Primary focus could not be located in our case in spite of doing a number of investigations. However, some case reports show that it can happen even without any primary focus, as in our case. The reactivation of latent bacilli that were deposited in the skin during a previous subclinical infection may be one possible explanation [8].
Histopathology of a metastatic tuberculous abscess typically reveals suppurative granulomata with nonspecific infiltrates that must be distinguished from non-tuberculous Mycobacteria (NTM). NTM causes a milder form of disease usually resistant to routine anti-tubercular therapy. The history of contaminated wound or surgical procedure is often present in such cases [8].
Though the histopathology report of our patient was somewhat non-specific, numerous AFB on staining, positive MTB-PCR and growth of Mycobacterium tuberculosis in culture confirmed our diagnosis beyond doubt.
The tuberculin skin test usually shows positive result but was found to be negative in 38% of cases in a review of case reports [7]. This test yielded a negative result in our case. As this test can be negative in immunocompromised people and in cases of acute infection, it was repeated after 8 weeks and found to be negative again.
Traditional anti-tubercular therapy or 2RHZE/4RH protocol is highly effective for the treatment of this condition. Less toxic and shorter regimens have been used successfully [7]. In our case, the outcome with ATT was much more satisfactory though ethambutol was given in a modified dose due to renal impairment.
Conclusion
A thorough understanding of the various presentations of tuberculosis is a must-have skill for all clinicians working in countries where the prevalence of TB is very high. Tuberculous Gumma is a rare variety of cutaneous Tuberculosis whereas CTB itself represents a small proportion of all extra-pulmonary TB cases. Diagnosis still remains enigmatic and challenging because of the wide variety of differential diagnoses that must be considered and the difficulty in obtaining microbiological confirmation in a low resource setting. The possibility of this condition should be kept in mind to avoid misdiagnosis and case underreporting in high TB burden countries.
Ethical Approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflict of Interest
The authors declare that they have no conflict of interest and financial disclosure.
Contributor Information
M.A. Alam, Email: adnanulalam01@gmail.com.
Mushfiq Newaz Ahmed, Email: mushfiq_8818@yahoo.com.
Abed Hussain Khan, Email: abedkhan78@gmail.com.
Shohael Mahmud Arafat, Email: arafat2001@gmail.com.
References
- 1.Chen Q., Chen W., Hao F. Cutaneous tuberculosis: a great imitator. Clin Dermatol. 2019;37(3):192–199. doi: 10.1016/j.clindermatol.2019.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Van Zyl L., Du Plessis J., Viljoen J. Cutaneous tuberculosis overview and current treatment regimens. Tuberculosis. 2015;95(6):629–638. doi: 10.1016/j.tube.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 3.Handog E.B., Gabriel T.G., Pineda R.T. Management of cutaneous tuberculosis. Dermatol Ther. 2008;21(3):154–161. doi: 10.1111/j.1529-8019.2008.00186.x. [DOI] [PubMed] [Google Scholar]
- 4.Bravo F.G., Gotuzzo E. Cutaneous tuberculosis. Clin Dermatol. 2007;25(2):173–180. doi: 10.1016/j.clindermatol.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Pacheco C., Silva E., Miranda J., Duarte R. Cutaneous tuberculosis as metastatic tuberculous abscess. J Bras Pneumol. 2015;41(2):200–202. doi: 10.1590/S1806-37132015000004388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Almagro M., Del Pozo J., Rodríguez‐Lozano J., Silva J.G., Yebra‐Pimentel M.T., Fonseca E. Metastatic tuberculous abscesses in an immunocompetent patient. Clin Exp Dermatol: Clin Dermatol. 2005;30(3):247–249. doi: 10.1111/j.1365-2230.2005.01728.x. [DOI] [PubMed] [Google Scholar]
- 7.Machan A., Hanafi T., Hjira N., Boui M. Tuberculous gummas: epidemiological, clinical, bacteriological, immunological, and therapeutic features. Int J Mycobacteriol. 2018;7(3):203–211. doi: 10.4103/ijmy.ijmy_83_18. [DOI] [PubMed] [Google Scholar]
- 8.Suna R., Duttaluri R. Multiple cutaneous tuberculous abscess: a case report. J Clin Diagn Res. 2017;11(10) [Google Scholar]