Abstract
Aim
To compare the accuracy of the inverted greyscale CT versus the conventional CT in the assessment of post-operative spinal orthopaedic implants and osseous fusion.
Methods
50 patients who had CT as part of their routine spinal implant follow up were evaluated for the presence of fusion, fracture and loosening with conventional CT and with greyscale inverted CT images. 3 independent observers assessed the images 2 months apart. Diagnostic performance (sensitivity and specificity) of the conventional and greyscale inversion images relative to the reference standard were calculated. Agreement with the reference standard was assessed using Cohen's kappa for conventional and greyscale inversion images.
Results
Correct classifications increased when using the greyscale inverted CT images for each reader compared to conventional CT images (40–46, 39 to 42 and 41 to 44 (out of 50)). Inverted images demonstrated better agreement with the reference standard than conventional grayscale images for assessment of fusion (kappa of 0.588 for inverted CT versus 0.484 for conventional CT) and loosening (kappa 0.386 for inverted versus 0.293 for conventional). Sensitivity was increased for assessment of fusion and loosening. McNemar's test performed for assessment of sensitivity differences showed statistical significance (p = 0.038 for fusion and p = 0.0313 for loosening).
Conclusion
Greyscale inversion CT is a useful adjunct which has advantages (improved sensitivity and better agreement) over conventional CT imaging in cases of fusion and loosening of metallic implants following spinal instrumentation. We recommend the use of both the greyscale inversion CT images and conventional CT imaging when assessing post-operative spinal orthopaedic implants.
Keywords: Inversion, CT, Implant
1. Introduction
Backpain is a common clinical symptom which will affect between one third to one half of the UK population.1 The incidence of surgical intervention in the management of backpain in the UK has doubled from 1997 to 2012.2 Spinal stabilisation and fusion is used to correct spinal instability due to degenerative change, trauma, infection, tumour and congenital deformity e.g. scoliosis. There are a broad range of devices available to achieve stabilisation and fusion of an unstable spinal segment and these include screws, rods, hooks, disc implants and vertebral cages. The internal fixation is required for early stabilisation whist the process of bony fusion occurs.3,4 Post-operative imaging is used to confirm the correct positioning and the integrity of the fixation device, to assess for osseous fusion and to assess for the presence of adjacent segment disease progression.
Radiographs are the most commonly used initial investigation to assess for implant position, implant integrity and the degree of osseous fusion due to its ease of availability, low radiation dose and low cost. Due to advances in CT technology and implant development, the streak artefacts seen with early CT and early spinal hardware are now largely eliminated. Due to its excellent bone detail and 3 dimensional capabilities, CT is now the imaging modality of choice of when assessing hardware position, hardware failure, spinal alignment and the presence of bony fusion.5, 6, 7, 8, 9
CT images are visible on Picture Archiving and Communication system (PACS) as white on black images depending on the attenuation of the tissue imaged. PACS also has the additional functionality to magnify images, change window width and level, adjust the contrast, brightness and also to invert the greyscale. The use of inversion of greyscale has been shown to improve the inter and intraobserver reliability when measuring spinopelvic alignment on radiographs,9 to improve the detection of pulmonary nodules on plain radiographs10 and in the detection of rib fractures on trauma radiographs.11 Anecdotally many skeletal radiologists use inversion greyscale CT images when imaging orthopaedic hardware as it can make loosening, implant failure and the presence of bony fusion appear more conspicuous.
In this study, we aim to compare the accuracy of the inverted greyscale CT versus the conventional CT in the assessment of post-operative spinal orthopaedic implants and osseous fusion.
2. Methods and materials
2.1. Study group
We retrospectively selected 50 consecutive patients over the age of 18 from our spinal orthopaedic database who had history of spinal surgery with implant insertion who underwent post-operative CT imaging as part of their spinal orthopaedic hardware follow up. CT was acquired using the Siemens Somatom Sensation AS (Siemens Medical Systems). The individual scan parameters we used on each patient depended factors such as patient size but for most cases we uses a KV between 120 and 140, an mAs between 200 and 380, a pitch of 0.8, collimation of 40 × 0.6 mm and reconstructed slice thickness of 1–2 mm. Each case was assessed for one of 3 parameters; the presence of fusion, for the fracture of part of the implant or for loosening of the implant. There were 28 cases related to the presence or absence of fusion, 14 cases related to the presence or absence of hardware loosening and 8 cases related to the presence or absence of fracture of the hardware. For each clinician reviewing the case, the specific relevant question was asked e.g. is there fusion, is the screw fractured or is there loosening for example. Responses were documented as yes or no. This work was registered and approved by the hospital research and audit department as a service evaluation project (Reference number 21–015).
2.2. Image evaluation
Image evaluation was performed using a dedicated PACS (GE Centricity™ Universal Viewer v 6.0) on high resolution (1536 × 2048 pixels) LCD greyscale display monitors (Eizo RX340). 2 radiologists and 1 orthopaedic surgeon independently reviewed all the images. 1 of the radiologists had approximately 7 years-experience in reviewing post-operative CT scans, the other radiologist was at the end of a musculoskeletal fellowship programme and had 3 years experience in reviewing post-operative CT scans and the orthopaedic surgeon had 6 years-experience in reviewing post-operative CT scans. The 50 cases were individually reviewed twice over 2 separate reading sessions 2 months apart, one session viewed on the conventional CT bone windows and the other session was viewed with greyscale inversion. A single relevant key image from each study (chosen by the senior author) was viewed and a specific question was asked for each image e.g. is there fusion, is there loosening or is there fracture of the hardware? Answers for each case were scored as 1- no and 2 -yes. A single key image was chosen rather than the entire CT dataset so there was only one abnormality per image. The “reference standard” to which these responses were compared to was the review of the entire data set for the study, along with any previous and subsequent CT scans, radiographs and the patients clinical picture in a multidisciplinary setting attended by a consultant radiologist (senior author of the study) and the orthopaedic surgeon who had overall clinical responsibility for the patient.
2.3. Statistical analysis
Statistical analysis were performed on IBM SPSS Statistics, version 25 (IBM Corp, N.Y., USA), and MedCalc Statistical Software, version 19.6.4 (MedCalc Software Ltd, Ostend, Belgium). Agreement between the answers given for each finding (the presence of fusion, for fracture of part of the implant, or for loosening of the implant) with the reference standard was assessed using Cohen's kappa, calculated separately for conventional and gray scale inversion. The diagnostic performance (sensitivity, and specificity) of the conventional and gray scale inversion images relative to the reference standard were also calculated. McNemar's test was used on cases with positive findings and negative findings separately to assess for statistical significance of differences in sensitivity and specificity, using a statistical methodology validated by Kim and Lee.12
3. Results
The total number of correct and incorrect answers on inversion and conventional images for each reader is summarised in Table 1.
Table 1.
The total of correct and incorrect classifications on greyscale inversion and conventional images for each reader.
| Reader |
Conventional |
Inversion |
||
|---|---|---|---|---|
| Correct | Incorrect | Correct | Incorrect | |
| 1 | 40 | 10 | 46 | 4 |
| 2 | 39 | 11 | 42 | 8 |
| 3 | 41 | 9 | 44 | 6 |
3.1. Agreement with the reference standard
Agreement of inverted and conventional images with the reference standard, assessed with Cohen's kappa, is shown in Table 2. Inverted images demonstrated better agreement with the reference standard than conventional grayscale images for assessment of fusion (kappa of 0.588 for inverted versus 0.484 for conventional) and loosening (kappa 0.386 for inverted versus 0.293 for conventional), when results were pooled between all readers (Fig. 1, Fig. 2. Agreement with the reference standard was perfect (1.00) for the absence or presence of fracture, with either conventional and inverted CT, as there were no incorrect classifications by any of the readers (Fig. 3).
Table 2.
Agreement with reference standard (answers shown per reviewer and overall).
| Agreement (Cohen's Kappa) | Fusion |
Loosening |
Fracture |
|||
|---|---|---|---|---|---|---|
| Conventional | Inverted | Conventional | Inverted | Conventional | Inverted | |
| 1 | 0.449 | 0.825 | 0.323 | 0.440 | 1.000 | 1.000 |
| 2 | 0.606 | 0.475 | 0.143 | 0.440 | 1.000 | 1.000 |
| 3 | 0.411 | 0.484 | 0.632 | 0.000 | 1.000 | 1.000 |
| Overall | 0.484 | 0.588 | 0.293 | 0.386 | 1.000 | 1.000 |
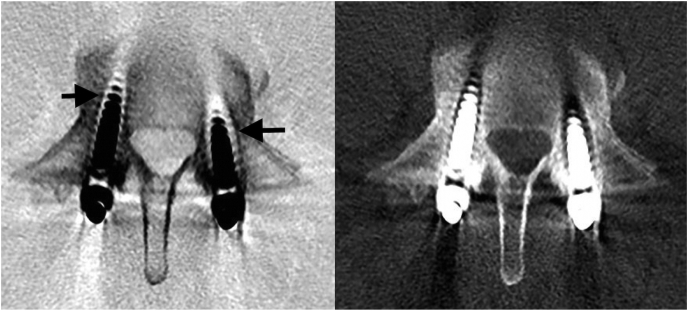
Fig. 1.
Inversion greyscale CT (left) and conventional CT image (right). There is failure of fusion of the posterior elements (black arrow). On the inverted image the number of correct classifications increased.
Fig. 2.
Inversion greyscale CT (left) and conventional CT image (right). There is loosening of both pedicle screws (worse on the right – as you look at the image (black arrows). Again on the inverted images the number of correct classifications increased.
Fig. 3.
Inversion greyscale CT (left) and conventional CT image (right). There is pedicle screw fracture which was correctly classified as a fracture on both the inversion and conventional CT image.
Individual readers’ results were less consistent, with two readers demonstrating improved agreement and one reader worse agreement for fusion (this was the least experienced reader). Two readers demonstrated improved agreement for loosening with one reader showing no change in agreement.
3.2. Diagnostic performance of conventional and grey scale inversion images
The sensitivity and specificity of conventional and greyscale inverted images, when pooled between observers, are summarised in Table 3 and Fig. 4.
Table 3.
Summary of diagnostic performance of the pooled results between conventional CT and greyscale inversion CT when the cases were subdivided into fusion, loosening and fracture cases. Note: Differences in sensitivity for fusion (∗) loosening and (#) were statistically significant (p = 0.0386 and p = 0.0313 respectively). Differences in specificities were not statistically significant.
| Fusion |
Loosening |
Fracture |
||||
|---|---|---|---|---|---|---|
| Conventional | Inversion | Conventional | Inversion | Conventional | Inversion | |
| Sensitivity | 70.0%∗ | 83.3%∗ | 74.4%# | 89.7%# | 100.0% | 100.0% |
| Specificity | 88.9% | 79.2% | 100.0% | 66.7% | 100.0% | 100.0% |
Fig. 4.
Graphical representation of the comparison of diagnostic performance of the pooled results between conventional CT and greyscale inversion CT when the cases were subdivided into fusion, loosening and fracture cases.
Sensitivity was increased for assessment of fusion and loosening. McNemar's test performed for assessment of sensitivity differences showed statistical significance (p = 0.038 for fusion and p = 0.0313 for loosening). There was a trend to decreased specificity with inverted CT compared to conventional images for the same categories, but this did not reach statistical significance (p = 0.687 for fusion and p = 1.000 for loosening).
Sensitivity and specificities were 100% for assessment of orthopaedic implant fracture, both on inverted and conventional CT.
4. Discussion
The concept of using greyscale inversion to view diagnostic images is not novel. A number of studies have looked at using inversion greyscale in the assessment of pulmonary nodules on chest radiographs.10,13 Lungren and colleagues10 showed there was a statistical difference in sensitivity to nodule detection when the inverted greyscale and a combination of the inverted greyscale and conventional radiographs were compared with conventional radiographs. De Boo and colleagues13 also showed there was an increased sensitivity for the detection of pulmonary nodules when the conventional radiograph was compared with the conventional and the inverted greyscale radiographs but this difference was not statistically significant. Both studies showed a slight decrease in specificity when using the inverted greyscale images.
In the field of orthopaedic medicine, Sun and colleagues9 showed that the use of greyscale inversion resulted improved intra and interobserver reliabilities in the measurement of a range of spinopelvic parameters including thoracic kyphosis (TK), lumbar lordosis (LL), sagittal vertical axis (SVA), pelvic incidence (PI), sacral slope (SS) and pelvic tilt (PT) when inverted greyscale radiographs were compared with conventional spinal radiographs. The measurements of PI, PT and SVA reached statistical significance for the 2 readers in the study. More recently Xia and colleagues14 showed that the intraclass correlation coefficients (ICC) were increased in the inverted greyscale radiographs compared to the conventional radiographs when measuring proximal junctional kyphosis in scoliotic patients in both the observers used in their study. They also showed intraclass correlation coefficients of interobserver reliabilities also were greater in the inverted grayscale view.
There is very little in the medical literature regarding the use of inversion of greyscale CT images. In a recent publication from Gadre and colleagues,15 they described the use of greyscale inversion of high resolution CT images of the temporal bone for visualising the stapes foot print in patients with post traumatic dizziness and third window syndrome. They showed the inverted greyscale CT images uncovered defects in the stapes footprint which were not visualised on the conventional CT images.
In our study there was improved sensitivity and agreement with the reference standard for assessment of loosening and fusion with the greyscale inversion CT images when compared with the conventional CT images. Our results suggest that greyscale inversion CT has added value at identifying loosening and fusion when compared to standard CT in pooled results. Interestingly, all 3 raters subjectively remarked that they preferred viewing images with greyscale inversion suggesting that abnormalities were subjectively “more conspicuous” than when compared to the conventional CT images, however this may explain why the false positive rate was increased in the greyscale inversion group for loosening and fusion cases. Is there a physiological reason for this apparent advantage of the inverted greyscale images over the conventional images? In a series of experiments looking at proof reading performance, positive polarity images (viewing dark text on a white background) was shown to have consistently better proofreading performance and contrast perception than with negative polarity (light text on a black background) images.16 Proposed reasons for this difference could be multifactorial, human brains are used to seeing positive polarity images (for example in books, newspapers, journal etc.) from a very early age and therefore the human brain is “trained” to look at images in this presentation state as opposed to the negative polarity presentation state, and therefore may be easier to analyze. Furthermore, positive polarity images are associated with higher luminescence which results in increased pupil constriction which improves depth of field, reduces focusing effort and leads to a higher quality retinal image.16 Finally, reflections on a screen are reduced with a positive polarity image. The inversion greyscale CT image (where images are presented with a white background with black appearing bones and implants) resembles an image with positive polarity and therefore could provide a physiologic basis for the differences seen between the greyscale inverted image and the conventional image (black background and white bones and implants) and the subjective improvement that these images have over the conventional CT images.
Our results show that the greyscale inversion CT has added value over convention CT for identifying loosening and fusion. The technique to convert a conventional CT image to a greyscale inversion image is straightforward and does not require any additional scanning time, hardware or software. It also should not add significant time to the reporting time. It can be performed by a single click of a mouse button on most PACS systems. Our recommendation would be is that it is to be used in conjunction with rather than instead of conventional CT images.
Our study has some limitations, firstly we used a single image to assess the abnormality rather than the whole data set, this therefore does not replicate the clinical scenario in which one would review the whole study and any previous relevant imaging. Our study group also included a select group of patients with a high number of positive findings, reflecting the use of cross sectional imaging in practice when there is high level of clinical suspicion or to further evaluate an abnormality seen on radiographs. This makes it difficult to demonstrate with statistical significance any true differences in specificity between conventional and inverted CT We have only assessed for agreement with the reference standard and diagnostic performance, and not the confidence in the diagnosis with a 5 point Likert scale.
5. Conclusion
Greyscale inversion CT is a useful adjunct which has advantages over conventional CT imaging in cases of fusion and loosening of metallic hardware following spinal instrumentation. A trend of decreased specificity was noted in our cohort, though this was not statistically significant and needs further assessment in future studies. We are not proposing that greyscale inversion CT should be used in isolation but as an adjunct to conventional CT images when assessing post-operative spinal orthopaedic hardware.
Funding
No funding
Declaration of competing interest
No conflicts of interest to declare.
References
- 1.Fayaz A., Croft P., Langford R.M. lPrevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJOpen. 2016;6 doi: 10.1136/bmjopen-2015-010364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weir S., Samnaliev M., Kuo T. The incidence and healthcare costs of persistent postoperative pain following lumbar spine surgery in the UK: a cohort study using the Clinical Practice Research Datalink (CPRD) and Hospital Episode Statistics (HES) BMJ Open. 2017;7 doi: 10.1136/bmjopen-2017-017585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slone R.M., McEnery K.W., Bridwell K.H., Montgomery W.J. Fixation techniques and instrumentation used in the thoracic, lumbar, and lumbosacral spine. Radiol Clin. 1995;33:233–265. [PubMed] [Google Scholar]
- 4.Berquist T.H. Imaging of the postoperative spine. Radiol Clin. 2006;44:407–418. doi: 10.1016/j.rcl.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 5.Peters Marloes J.M., Bastiaenen Carolien H.G., Brans Boudewijn T., Weijers René E., Paul C. Willems the diagnostic accuracy of imaging modalities to detect pseudarthrosis after spinal fusion—a systematic review and meta-analysis of the literature. Skeletal Radiol. 2019;48 doi: 10.1007/s00256-019-03181-5. pages1499–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brodsky A.E., Kovalsky E.S., Khalil M.A. Correlation of radiologic assessment of lumbar spine fusions with surgical exploration. Spine. 1991;16(6):S261–S265. doi: 10.1097/00007632-199106001-00017. [DOI] [PubMed] [Google Scholar]
- 7.Pai V.S., Hodgson B. Assessment of bony union following surgical stabilisation for lumbar spondylolysis: a comparative study between radiography and computed tomography. J Orthop Surg. 2006;14(1):17–20. doi: 10.1177/230949900601400105. [DOI] [PubMed] [Google Scholar]
- 8.Fogel G.R., Toohey J.S., Neidre A., Brantigan J.W. Fusion assessment of posterior lumbar interbody fusion using radiolucent cages: X-ray films and helical computed tomography scans compared with surgical exploration of fusion. Spine J. 2008;8(4):570–577. doi: 10.1016/j.spinee.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 9.Sun Grayscale inversion radiographic view provided improved intra- and inter-observer reliabilities in measuring spinopelvic parameters in asymptomatic adult population. BMC Muscoskel Disord. 2016;17:411. doi: 10.1186/s12891-016-1269-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lungren M.P., Samei E., Barnhart H. Gray-scale inversion radiographic display for the detection of pulmonary nodules on chest radiographs. Clin Imag. 2012;36:515–521. doi: 10.1016/j.clinimag.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 11.Park J.B., Cho Y.S., Choi H.J. Diagnostic accuracy of the inverted grayscale rib series for detection of rib fracture in minor chest trauma. Am J Emerg Med. 2015;33:548–552. doi: 10.1016/j.ajem.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 12.Kim S., Lee W. Does McNemar's test compare the sensitivities and specificities of two diagnostic tests? Stat Methods Med Res. 2017 Feb;26(1):142–154. doi: 10.1177/0962280214541852. Epub 2016 Sep 30. PMID: 24996898. [DOI] [PubMed] [Google Scholar]
- 13.De Boo D.W., Uffmann M., Bipat S. Gray-scale reversal for the detection of pulmonary nodules on a PACS workstation. AJR Am J Roentgenol. 2011;197:1096–1100. doi: 10.2214/AJR.11.6625. [DOI] [PubMed] [Google Scholar]
- 14.Xia C., Xu L., Xue B., Sheng F., Qiu Y., Zhu Z. Grayscale inversion view can improve the reliability for measuring proximal junctional kyphosis in adolescent idiopathic scoliosis. World Neurosurg. 2018 Nov;119:e631–e637. doi: 10.1016/j.wneu.2018.07.224. Epub 2018 Aug 2. PMID: 30077754. [DOI] [PubMed] [Google Scholar]
- 15.Gadre A.K., Edwards I.R., Baker V.M., Roof C.R. Membranous or hypermobile stapes footplate: a new anatomic site resulting in third window syndrome. Front Neurol. 2020 Aug 20;11:871. doi: 10.3389/fneur.2020.00871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buchner A., Baumgartner N. Text - background polarity affects performance irrespective of ambient illumination and colour contrast. Ergonomics. 2007 Jul;50(7):1036–1063. doi: 10.1080/00140130701306413. [DOI] [PubMed] [Google Scholar]