Abstract
Rapid worldwide decreases in physical activity (PA), an increase in sedentary behaviour (SB) and poorer dietary patterns have been reported during COVID-19 confinement periods. However, as national variability has been observed, this study sought to describe PA, SB and eating patterns, and to explore their gender as well as other socio-demographic correlates and how they interrelate in a representative sample of Portuguese adults during the COVID-19 first mandatory social confinement. The survey was applied online and by telephone to 5856 adults (mean age = 45.8 years; 42.6% women). The majority reported high (46.0%) or moderate (20.5%) PA levels. Men, younger participants, those with higher education levels and a favourable perception of their financial situation reported higher PA levels, with the opposite pattern for SB. Physical fitness activities and household chores were more reported by women, with more strength training and running activities reported by men. Regarding eating behaviours, 45.1% reported changes, positive (58%) and negative (42%), with 18.2% reporting increases in consumption of fruit, vegetables, and fish and other seafood consumption, while 10.8% (most with lower educational level and less comfortable with their income) reported an increase in consumption of ready-to-eat meals, soft drinks, savoury snacks, and take-away and delivered meals. Two clusters—a health-enhancing vs. risky pattern—emerged through multiple correspondence analysis characterized by co-occurrence of high vs. low PA levels, positive vs. negative eating changes, awareness or not of the COVID-19 PA and dietary recommendations, perceived financial situation, higher vs. lower educational level and time in social confinement. In conclusion, while in social confinement, both positive and negative PA and eating behaviours and trends were displayed, highlighting the role of key sociodemographic correlates contributing to healthy vs. risky patterns. Results may inform future health interventions and policies to be more targeted to those at risk, and also advocate the promotion of PA and healthy eating in an integrated fashion.
Keywords: physical activity, sedentary behaviour, eating behaviour, socio-demographic correlates, health and risk patterns, COVID-19 social confinement
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has placed an overwhelming burden on health systems and authorities to respond with effective and appropriate policies, health communication, and interventions [1,2]. To tackle this pandemic, nonpharmacological, behavioural interventions became mandatory to reduce disease transmission and associated morbidity and mortality [1,3,4]. Furthermore, restaurants, gyms, parks, community centres, and other public social and recreational facilities and venues were closed or their access restricted in many countries, depending on the epidemiologic evolution of the disease, whereas several professionals and students transitioned to online work and learning, respectively, during the state of emergency declared in several countries. However, these nonpharmacological interventions, although necessary to curtail the spread of the disease, potentially disrupted many regular aspects of life, including physical activity (PA) and eating habits [5,6,7,8,9], with potentially critical implications for the global burden of disease [10,11,12,13,14].
Several longitudinal studies have documented the association between social isolation and increased risk of chronic illnesses and mortality, independently of other sociodemographic factors or pre-existing health conditions [14,15,16,17,18,19]. One pathway proposed to underpin such relationship is that socially isolated individuals may adopt less favourable lifestyles, such as poor diets or decreased PA levels [20,21,22]. Thus, adequate eating and PA are considered interconnected strategic public health priorities during this pandemic [1,2,14,21,22].
1.1. Social Confinement and Eating Behaviours
Anxiety and boredom evoked by social confinement at home are considered risk factors for dysfunctional eating behaviours, both in terms of “emotional eating”, characterized by overeating of poor-quality foods, and in terms of restricted food access, compared to standard living conditions [6,23]. Furthermore, restricted access to food suppliers due to lockdown and social confinement has placed a burden on regular food-related behaviours [6,24]. This is noteworthy, as maintaining an adequate nutritional status is important for health and well-being, particularly when the immune system is challenged [25]. Malnutrition (both undernutrition and overweight) seems to be a risk factor for poor outcomes in COVID-19 patients [26]. Additionally, limited access to fresh food could negatively affect overall health [24,25]. Thus, it is paramount for researchers and health authorities to identify alterations to dietary patterns during the pandemic, and their socio-demographic correlates [20]. Furthermore, combined with the potential for lower PA levels, impaired dietary habits may lead to a positive energy balance (i.e., weight gain), another critical public health problem [27].
1.2. Social Confinement and Physical Activity
Regular PA is important for the immune system and to counteract many comorbidities, such as obesity, diabetes, hypertension, and heart conditions, that increase susceptibility to severe COVID-19 illness [28,29,30,31], as there is a linear relationship between physical activity levels and immune function/viral defense [32,33]. Recommended amounts of 150 min of moderate-intensity or 75 min of vigorous-intensity PA per week [34,35] are consistent with enhanced immunosurveillance and lowered risk for respiratory illness via effects on the immune, respiratory, cardiovascular, and musculoskeletal systems (for a comprehensive review please see [7]). Thus, PA is a relevant adjuvant to COVID-19 mitigation practices [5,36,37] to be promoted as much as social distancing actions [7,8,9,38,39].
In this line, the World Health Organization encouraged governments to include clear exceptions for PA in nationwide lockdowns, allowing outdoor individual PA, provided that adequate interpersonal distance could be maintained. Furthermore, a wide range of exercises, such as video, or app-guided, equipment free, aerobics or strength training to be performed at home were also encouraged [2,11,40]. Nonetheless, social isolation seems to negatively impact PA and sedentary behaviour (SB) levels and patterns, by limiting participation in usual daily activities, travel and access to other forms of exercise (e.g., gyms, parks, and other recreational facilities) [41,42,43,44,45,46,47]. However, some individuals also show maintained, or even increased, levels of PA while in confinement (e.g., more available time, no other competing tasks, as possible way to enjoy the outdoors) [41,48,49,50].
1.3. The Need for Adequate, Local, and Integrated Monitoring—A Step for Effective Public Health Policies
Overall, epidemiological studies on the COVID-19 pandemic have indicated a decrease in PA levels [6,41,42,44,45,46,47,51] and nutritional quality [6], although highlighting the heterogeneity of results across countries and even within the same country [41,47,51,52]. Indeed, the extent to which lifestyle behaviours are being impacted by the current COVID-19 pandemic is most likely linked to the stringency of individual government confinement policies and contextual and cultural contingencies. Furthermore, it is of the utmost importance to understand the role of gender, especially considering that policy responses have not yet addressed gender impacts of disease outbreaks [53]. Along with gender differences, other socio-economic indicators should also be considered [53]. These include access to specific COVID-19 public health guidelines (including PA and healthy eating) and their perceived usefulness [54,55].
In sum, in spite of population studies on dietary and PA habits already published in response to this much-needed surveillance effort [21], most surveys did not provide a comprehensive analysis of the PA and diet interactions and common determinants. Indeed, a matter worthy of further consideration is the synergetic effect of PA and eating behaviours [20,56]. For example, low PA levels have been suggested to interact with appetite dysregulation, whereas adequate PA levels seem to relate to a better regulation of eating behaviours [57]. Taking all these factors into consideration will allow identifying potential health and risk patterns, facilitating better tailored future public health recommendations.
In this context, The REACT-COVID survey aimed to (i) describe PA, SB and eating habits, and (ii) explore their gender as well as other socio-demographic correlates and how they interrelate, in a representative sample of Portuguese adults during the COVID-19 pandemic initial critical period (national emergency state conductive to mandatory social confinement at home, in 2020).
2. Methods
2.1. Study Design and Participants
The REACT-COVID survey was a cross-sectional observational study. Portuguese adults, aged 16 years and older, living in social confinement (as imposed by national authorities throughout the second trimester of 2020), were invited to participate in the survey. Data were collected between 9 April and 4 May 2020, through a nonprobabilistic sampling procedure. Recruitment of participants followed two strategies: a request to participate in the survey was advertised in institutional websites, media and virtual social networks (snowball sampling) and, complementarily, a telephone survey was conducted with owners of fixed and mobile telephone numbers using a Computer-Assisted Telephone Interviewing (CATI) system. The telephone numbers were randomly generated, ensuring a scattered national geographical distribution. After a maximum of five unsuccessful contact attempts at different times of the day and different days of the week, the telephone numbers were considered as nonresponsive. Specific training regarding interviewing techniques, and focused on the questions of the survey, was given to the health professionals (nutritionists and psychologists) who conducted the telephone interviews. The complementary telephone interviews were conducted to ensure increased response rates for socioeconomic groups that are usually underrepresented in online surveys. The LimeSurvey® platform was used to register the answers to both web-based self-administrated questionnaire and interviewer administrated data collection.
The strategies for survey communication and dissemination were adjusted throughout the fieldwork period, according to the collected sociodemographic database profile, targeting an adequate representation of all sociodemographic subgroups, considering sex, decennial group ages, having or not university-level studies and distribution by residence in the Portuguese regions.
Before data collection, the REACT-COVID protocol was submitted and approved by the Ethics Committee of the Centro Académico de Medicina de Lisboa. The study procedures complied with the Declaration of Helsinki for observational studies. Participants were informed about the aims and procedures before enrolment, either by telephone, or via the online study information sheet that accompanied the survey. There were no financial incentives for participation in the study.
2.2. The Survey
The questionnaire included indicators about PA, food-related behaviours, perceived reasons for changing these behaviours in the context of social confinement, and access to (and perception of the usefulness of) public health guidelines on PA and healthy eating behaviours during the confinement period. Participants were also asked about details of confinement (e.g., duration and reason for confinement—quarantine or prophylactic isolation; self-perceived general health status), as well as about sociodemographic characteristics (gender, age, educational level, residential municipality, having children or not in the household, and subjective financial well-being). The questionnaire was designed to be completed in about 15 min to maximize participation and the quality of the answers.
2.2.1. Eating Behaviours
Regarding eating behaviours, participants were asked whether they had modified their pattern of food intake compared with the pre-confinement period. This was asked for a set of foods: vegetables, fruit, meat, fish and seafood, sweet snacks (e.g., cookies, biscuits, or chocolates), savoury snacks (e.g., crisps), ready meals (e.g., pizza or lasagne), canned seafood, other canned food (not seafood), take-away or delivered meals, fruit juices, soft drinks, water, and alcoholic beverages. For each of these food groups, participants indicated if they diminished, maintained, or increased their intake. The questionnaire included a checklist of possible reasons for the reported changes in food intake. Participants were also asked to indicate their food shopping habits during the confinement period, and an overall perception regarding the quality of their current (during confinement) diet. Finally, two questions addressed food insecurity.
2.2.2. Physical Activity and Sedentary Behaviour
PA and SB were assessed with the International Physical Activity Questionnaire (IPAQ) [58,59]. Participants reported the frequency and duration of total vigorous and moderate PA and walking performed in 10 min bouts over the previous week, as well as the time spent in SB (sitting time) on a usual weekday. Total weekly duration of PA and energy expenditure of PA were calculated according to the IPAQ scoring protocol, by weighting the time reported for each activity intensity with its estimated metabolic equivalent (MET) energy expenditure [59]. Participants were categorized as having a Health-Enhancing PA (HEPA), active and low active, according to IPAQ scoring references [59,60]. Participants were also classified according to three categories of time spent sitting (SB), according to tertiles: 0–180 min a day; 181–419 min a day; ≥420 min a day [61].
2.3. Statistical Analyses
Data cleaning procedures considered the completion time of the questionnaire. For that, the number of answers and completion times were used to calculate mean time of response for the total questionnaire and for the last group of answers of the questionnaire. Five seconds was established as an acceptable minimum completion time average per question. Respondents whose average completion time per question was lower than this were excluded from the analysis.
A minimum sample size of 400 individuals per NUT II region of Portugal (North, Center, Lisbon Metropolitan Area, Alentejo, Algarve, Autonomous Region of the Madeira, and Autonomous Region of the Azores) was estimated to be adequate for the planned analysis. This corresponds to an overall minimum sample size of 2800 individuals.
To verify the representativeness of the sample according to the Portuguese population, we first compared the socioeconomic characteristics of surveyed sample with the Portuguese population distribution. Information of the Census 2011 was used for weighing the sample based on the distributions of sex (men and women), age group (16–34; 35–54; and 55 years or more), level of education (secondary level or lower; and higher education) and NUTS II (North, Center, Lisbon Metropolitan Area, Alentejo, Algarve, Autonomous Region of the Madeira, and Autonomous Region of the Azores) for the Portuguese population. Weighted absolute frequencies (and corresponding proportions) were provided for categorical variables and continuous variables were described by weighted mean values and SDs. Participants who had missing data in variables used for weighing the sample were excluded from analyses.
All statistics were performed using IBM SPSS Statistics® (version 26). The mean time of response for the total questionnaire was calculated, and a cut-off for an acceptable minimum completion time was then established. Responses whose completion time was lower than the established cut-off were excluded from the analyses. Age was categorized in age groups (16–34; 35–54; and 55 years or more) and the level of education was dichotomised in secondary school or below vs. higher education. Participants’ characteristics were described using weighted absolute frequencies (and corresponding percentages). Food intake and PA-related variables were described by main sociodemographic characteristics (gender, age groups, region, financial situation). Tests of independence were performed using the Chi-Square test or Fisher’s Exact Tests (according to the number of cells and variable distribution). To understand how subjects could be nested within clusters of health-enhancing vs. risky patterns of PA and eating behaviours and related variables, Multiple Correspondence Analysis (MCA) was used to explore the data and produce a simplified graphic representation of the information by analysing cases-by-variable categories matrices. Prior to this analysis, which combines patterns of PA and eating behaviours, MCA and Agglomerative Hierarchical Cluster analysis (AHC) were used to identify patterns of changes on food consumption behaviour during the home confinement, compared to before the lockdown.
3. Results
3.1. Participants’ Characteristics
Table 1 depicts participants’ characteristics. The sample comprised 5856 adults aged 16 and older (mean age 45.8 years). Most participants had secondary or higher education (81.5% and 18.5%, respectively). The majority of the participants were employed or studying (82%) and without children (67.8%); 43.6% were in-home social confinement for more than 4 weeks at the time of the survey, and the most common reasons reported for being in social confinement were mandatory teleworking (30.3%) and family support (16.6%).
Table 1.
Participants’ characteristics of the Portuguese REACT COVID-19 survey.
| Participants’ Characteristics | Total | Men | Women | p |
|---|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | ||
| Age | 45.8 (45.4, 46.3) | 45.5 (44.9, 46.1) | 46.2 (45.6, 46.8) | |
| Age-group | <0.001 | |||
| 16–34 years | 27.9 (26.8, 29.1) | 29.5 (27.8, 31.2) | 26.4 (24.8, 27.9) | |
| 35–54 years | 34.9 (33.7, 36.1) | 35.9 (34.2, 37.7) | 34.0 (32.3, 35.7) | |
| ≥55 years | 37.2 (35.9, 38.4) | 34.5 (32.7, 36.3) | 39.6 (37.9, 41.3) | |
| Education | <0.001 | |||
| Secondary school or below | 81.5 (80.5, 82.5) | 83.5 (82.1, 84.9) | 79.9 (78.5, 81.4) | |
| Higher education | 18.5 (17.5, 19.5) | 16.5 (15.1, 17.9) | 20.1 (18.6, 21.5) | |
| Professional situation | <0.001 | |||
| Employee | 57.4 (56.1, 58.8) | 58.7 (56.8, 60.6) | 56.2 (54.4, 58.0) | |
| Student | 15.1 (14.1, 16.0) | 14.9 (13.5, 16.3) | 15.2 (13.8, 16.5) | |
| Retired | 17.4 (16.4, 18.4) | 19.3 (17.8, 20.9) | 15.7 (14.3, 17.0) | |
| Housekeeper | 3.4 (2.9, 3.8) | 0.1 (0.0, 0.2) | 6.4 (5.5, 7.3) | |
| Unemployed | 6.7 (6.1, 7.4) | 6.9 (6.0, 7.9) | 6.6 (5.7, 7.5) | |
| Subjective financial well-being | 0.004 | |||
| Comfortable or very comfortable | 30.1 (28.9, 31.3) | 30.3 (28.6, 32.1) | 29.9 (28.3, 31.6) | |
| Reasonable | 51.3 (50.0, 52.6) | 52.8 (50.9, 54.7) | 49.8 (48.1, 51.6) | |
| Difficult or very difficult | 18.6 (17.6, 19.7) | 16.8 (15.4, 18.3) | 20.2 (18.8, 21.7) | |
| Children | 0.448 | |||
| No | 67.8 (66.6, 69.0) | 67.3 (65.5, 69.1) | 68.2 (66.6, 69.9) | |
| Yes | 32.2 (31.0, 33.4) | 32.7 (30.9, 34.5) | 31.8 (30.1, 33.4) | |
| Social confinement (reasons) | ||||
| Sickness (COVID-19) | 1.2 (1.0, 1.5) | 1.9 (1.4, 2.4) | 0.7 (0.4, 1.0) | <0.001 |
| Sickness (other) | 2.2 (1.8, 2.6) | 1.3 (0.9, 1.8) | 3.0 (2.4, 3.6) | <0.001 |
| Family support | 16.6 (15.6, 17.6) | 14.3 (12.9, 15.6) | 18.7 (17.3, 20.1) | 0.064 |
| Telework | 30.3 (29.1, 31.5) | 31.5 (29.8, 33.2) | 29.3 (27.7, 30.9) | <0.001 |
| Prophylactic isolation | 5.5 (4.9, 6.1) | 7.9 (6.9, 9.0) | 3.3 (2.7, 4.0) | |
| Lockdown (time) | 0.246 | |||
| Up to 3 weeks | 26.0 (24.9, 27.1) | 26.7 (25.0, 28.3) | 25.5 (23.9, 27.0) | |
| Up to 4 weeks | 43.6 (42.3, 44.9) | 44.0 (42.1, 45.8) | 43.2 (41.5, 44.9) | |
| Up to 5 weeks | 30.3 (29.2, 31.5) | 29.4 (27.7, 31.1) | 31.3 (29.7, 33.0) | |
| Self-rated health | <0.001 | |||
| Very good | 37.4 (36.2, 38.7) | 43.0 (41.2, 44.9) | 32.5 (30.8, 34.1) | |
| Good | 37.2 (36.0, 38.4) | 35.6 (33.8, 37.4) | 38.7 (36.9, 40.4) | |
| Reasonable | 25.4 (24.3, 26.5) | 21.4 (19.9, 22.9) | 28.9 (27.3, 30.5) | |
Weighed data: age (n = 5856), education (n = 5856), professional situation (n = 5532), family income perception (n = 5643), children (n = 5856), time of lockdown (n = 5856), self-rated health (n = 5856). Differences between men and women were tested by Chi-Square.
3.2. Physical Activity and Sedentary Behaviour
Table 2 presents the prevalence of PA and SB by gender, age, education, perception of the family financial situation, knowledge and self-rated usefulness of the COVID-19 PA recommendations, and time spent in home social confinement. During social confinement, 46% of the participants (49.9% men and 42.6% women, p > 0.001) were classified as HEPA. As age increased, the number of participants classified as HEPA decreased significantly. Participants with higher education levels were more frequently classified as HEPA.
Table 2.
Prevalence of physical activity and time spent sitting, during the COVID-19 social confinement.
| Participants’ Characteristics | IPAQ Categories | p | Sitting Time (min/day) | p | ||||
|---|---|---|---|---|---|---|---|---|
| % (95% CI) | % (95% CI) | |||||||
| Low Active | Active | HEPA | <180 | 181–419 | ≥420 | |||
| Total | 33.5 (32.3, 34.7) | 20.5 (19.5, 21.5) | 46.0 (44.7, 47.2) | 34.4 (33.2, 35.7) | 28.4 (27.3, 29.6) | 37.1 (35.9, 38.4) | ||
| Gender | <0.001 | <0.001 | ||||||
| Men | 29.4 (27.7, 31.1) | 20.7 (19.2, 22.2) | 49.9 (48.0, 51.7) | 29.8 (28.1, 31.5) | 30.8 (29.1, 32.5) | 39.4 (37.5, 41.2) | ||
| Women | 37.1 (35.4, 38.8) | 20.3 (18.9, 21.7) | 42.6 (40.9, 44.4) | 38.5 (36.7, 40.2) | 26.4 (24.8, 27.9) | 35.2 (33.5, 36.8) | ||
| Age-group | <0.001 | <0.001 | ||||||
| 16–34 years | 27.5 (25.3, 29.6) | 18.6 (16.7, 20.5) | 53.9 (51.5, 56.3) | 24.4 (22.3, 26.4) | 26.1 (24.0, 28.3) | 49.6 (47.1, 52.0) | ||
| 35–54 years | 37.0 (34.9, 39.1) | 16.3 (14.7, 17.9) | 46.6 (44.4, 48.8) | 36.0 (33.9, 38.1) | 29.0 (27.0, 31.0) | 35.0 (32.9, 37.0) | ||
| ≥55 years | 34.8 (32.8, 36.8) | 25.8 (24.0, 27.7) | 39.4 (37.3, 41.4) | 40.6 (38.5, 42.6) | 29.6 (27.7, 31.5) | 29.8 (27.8, 31.7) | ||
| Education | <0.001 | <0.001 | ||||||
| Secondary school or below | 34.6 (33.3, 36.0) | 20.8 (19.7, 22.0) | 44.6 (43.1, 46.0) | 37.4 (36.0, 38.8) | 28.9 (27.6, 30.1) | 33.7 (32.4, 35.1) | ||
| Higher education | 28.7 (26.0, 31.4) | 19.1 (16.8, 21.4) | 52.2 (49.2, 55.2) | 21.4 (19.0, 23.8) | 26.7 (24.0, 29.3) | 52.0 (49.1, 55.0) | ||
| Family income perception | <0.001 | <0.001 | ||||||
| Good | 25.6 (23.5, 27.6) | 21.7 (19.8, 23.7) | 52.7 (50.3, 55.1) | 33.7 (31.5, 36.0) | 26.4 (24.3, 28.5) | 39.9 (37.5, 42.2) | ||
| Reasonable | 34.9 (33.2, 36.6) | 21.7 (20.2, 23.2) | 43.4 (41.6, 45.3) | 31.4 (29.7, 33.1) | 29.1 (27.5, 30.8) | 39.5 (37.7, 41.3) | ||
| Poor | 40.8 (37.8, 43.7) | 16.9 (14.7, 19.2) | 42.3 (39.3, 45.3) | 39.7 (36.8, 42.7) | 29.8 (27.0, 32.5) | 30.5 (27.7, 33.3) | ||
| PA recommendation knowledge | <0.001 | 0.234 | ||||||
| Yes | 34.8 (33.0, 36.6) | 19.5 (18.0, 21.0) | 45.7 (43.8, 47.6) | 37.6 (35.7, 39.4) | 27.5 (25.8, 29.2) | 34.9 (33.1, 36.7) | ||
| No | 32.5 (30.8, 34.1) | 21.3 (19.9, 22.7) | 46.3 (44.5, 48.0) | 31.8 (30.2, 33.4) | 29.2 (27.6, 30.8) | 38.9 (37.2, 40.6) | ||
| PA usefulness of recommendations | <0.001 | <0.001 | ||||||
| Not useful | 36.2 (30.9, 41.5) | 13.7 (9.9, 17.4) | 50.2 (44.6, 55.7) | 24.4 (19.7, 29.2) | 38.1 (32.7, 43.5 | 37.1 (31.8, 42.5) | ||
| I am not sure | 41.7 (35.9, 47.5) | 23.0 (18.1, 28.0) | 35.3 (29.6, 40.9) | 36.3 (30.7, 42.0) | 19.1 (14.4, 23.7) | 45.0 (39.1, 50.8) | ||
| Very useful | 33.7 (31.7, 35.7) | 19.9 (18.2, 21.6) | 46.4 (44.2, 48.5) | 39.7 (37.6, 41.8) | 27.0 (25.1, 28.9) | 33.3 (31.2, 35.3) | ||
| Lockdown (time) | 0.005 | 0.015 | ||||||
| Up to 3 weeks | 35.5 (33.1, 37.9) | 19.0 (17.0, 20.9) | 45.5 (43.0, 48.0) | 37.9 (35.4, 40.3) | 28.1 (25.9, 30.4) | 34.1 (31.7, 36.4) | ||
| Up to 4 weeks | 31.0 (29.2, 32.8) | 21.7 (20.1, 23.3 | 47.3 (45.4, 49.3) | 33.1 (31.3, 34.9) | 28.5 (26.7, 30.2) | 38.4 (36.5, 40.3) | ||
| Up to 5 weeks | 35.6 (33.3, 37.8) | 20.1 (18.2, 22.0) | 44.3 (42.0, 46.7) | 33.4 (31.2, 35.6) | 28.7 (26.6, 30.8) | 37.9 (35.7, 40.2) | ||
Weighed data. Abbreviations: IPAQ, International Physical Activity Questionnaire; PA, physical activity; HEPA—Health-enhancing Physical Activity; CI—Confidence Intervals. Differences among IPAQ categories and sitting time intervals were tested by Chi-Square.
Regarding the time spent sitting, 37.1% of the participants reported spending at least, 420 min per day (7 h) in this behaviour, with men, younger participants, those with higher education levels, those reporting a more favourable perception of the family financial situation, and those who did not know the PA recommendation spending significantly more time sitting in social confinement.
Table 3 summarizes the type of PA and SB engaged during social confinement. Among men and women, the most frequently reported physical activities during social confinement were house cleaning (men: 51.1%; women: 86.7%, p > 0.001), climbing up and down stairs (men: 49.3; women 50.6%), and walking (men: 31.5%; women: 32.9%). Watching television (men: 70.6%; women: 69.5%), using the computer, the tablet or a smartphone (men: 66.5%; women: 55.4%, p < 0.001), and teleworking (men: 39%; women: 34.4%, p > 0.05) were the most frequently reported sedentary activities.
Table 3.
Physical activities and sedentary behaviours, during the COVID-19 social confinement.
| Physical Activities and Sedentary Behaviours |
Men | Women | p |
|---|---|---|---|
| % (95% CI) | % (95% CI) | ||
| Types of physical activities | |||
| House cleaning | 51.1 (49.2, 52.9) | 86.7 (85.5, 87.9) | <0.001 |
| Up and down stairs | 49.3 (47.4, 51.2) | 50.6 (48.9, 52.4) | 0.294 |
| Walking | 31.5 (29.8, 33.3) | 32.9 (31.3, 34.6) | 0.253 |
| Fitness activities | 21.5 (19.9, 23.0) | 28.9 (27.3, 30.5) | <0.001 |
| Gardening | 21.8 (20.2, 23.3) | 23.3 (21.9, 24.8) | 0.147 |
| Bricolage | 24.0 (22.4, 25.6) | 14.2 (13.0, 15.4) | <0.001 |
| Strength training | 23.7 (22.1, 25.3) | 12.9 (11.7, 14.1) | <0.001 |
| Jogging | 22.7 (21.1, 24.2) | 6.5 (5.6, 7.3) | <0.001 |
| Static bicycle | 11.7 (10.5, 12.9) | 5.3 (4.5, 6.0) | <0.001 |
| Dance | 2.2 (1.6, 2.7) | 10.1 (9.1, 11.2) | <0.001 |
| Types of sedentary behaviours | |||
| Watching television | 70.6 (68.9, 72.3) | 69.5 (67.8, 71.1) | 0.359 |
| Computer, tablet, smartphone | 66.5 (64.7, 68.2) | 55.4 (53.7, 57.2) | <0.001 |
| Telework | 39.0 (37.2, 40.8) | 34.4 (32.7, 36.1) | <0.001 |
| Read | 28.6 (26.9, 30.3) | 33.8 (32.2, 35.5) | <0.001 |
| Board games, puzzles, Legos | 8.2 (7.2, 9.2) | 9.2 (8.2, 10.2) | 0.191 |
| Play musical instrument | 3.7 (3.0, 4.4) | 1.2 (0.8, 1.6) | <0.001 |
Weighed data. Men (n = 2743), women (n = 3097). Differences between men and women were tested by Chi-Square.
3.3. Eating Habits
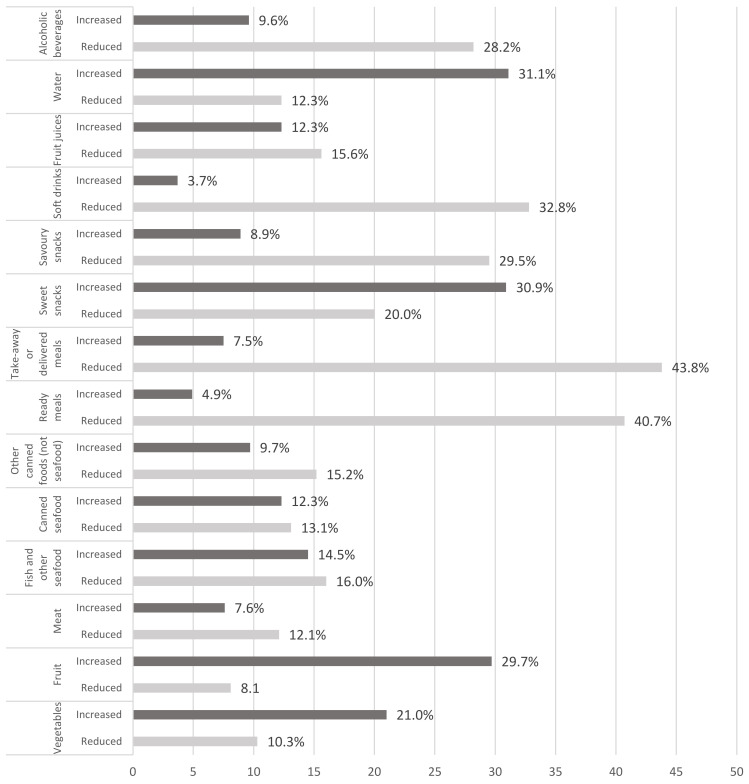
In terms of eating habits, almost half of the participants (45.1%) reported general changes in their eating habits during social confinement and 37.8% reported changes in diet quality (58.1% improved and 41.9% worsened) (Table 4). Women (47.3% vs. 42.6% in men, p < 0.001), young people (57.1% in individuals aged 16–34 years vs. 33.1% in individuals aged more than 55 years, p < 0.001), and those with high educational level (49.1% vs. 44.2%, p < 0.05) were more likely to report changes of eating habits during the COVID-19 confinement. The reported changes in food consumption are presented in Figure 1 and Table 5. Sweet snacks (30.9%), fruit (29.7%), and vegetables (21.0%) were the food categories with the highest proportion of a reported increase in consumption during social confinement, with women reporting the highest increase in vegetables (22.1% vs. 19.9%, p < 0.05) and sweet snacks (32.8% vs. 28.8%, p < 0.05) consumption, and men the highest increase in fruit consumption (32.2% vs. 27.4%, p < 0.001). From the food categories with the highest proportion of a reported decrease in consumption, we highlight takeaway or delivered meals (43.8%), ready meals (40.7%), soft drinks (32.8%), savoury snacks (30.9%), and alcoholic beverages (28.2%). When we combine and analyze together the different food items, two main “dietary patterns” were identified. One “healthy food behaviour pattern” that combines an increase in, at least, two of the following favourable foods (fruit, vegetables, and fish) and an “unhealthy food behaviour pattern” characterized by an increase in ready meals, savoury snacks, soft drinks and take-away consumption, and by a decrease in fruit and vegetable consumption (Table 5). The “unhealthy food behaviour pattern” was more likely to be followed by men (p < 0.001), younger groups (p < 0.001), and by those individuals reporting living with a less comfortable income (p < 0.05) and at risk of food insecurity (p < 0.001). During the analysed period, the estimated proportion of the risk of food insecurity was 33.2%, and 8% reported facing economic difficulties in accessing food.
Table 4.
Self-reported changes of food behaviours, during COVID-19 social confinement.
| Self-Reported Changes of Food Behaviours | Total | Men | Women | p |
|---|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | ||
| Changes in dietary habits | <0.001 | |||
| Yes | 45.1 (43.9, 46.4) | 42.6 (40.8, 44.5) | 47.3 (45.5, 49.0) | |
| No | 54.9 (53.6, 56.1) | 57.4 (55.5, 59.2) | 52.7 (50.9, 54.4) | |
| Changes in diet quality | 0.037 | |||
| No changes/do not know | 62.2 (60.4, 64.0) | 63.8 (61.3, 66.5) | 60.9 (48.5, 63.4) | |
| Yes | 37.8 (36.5, 39.0) | 36.2 (34.4, 38.0) | 39.1 (37.4, 40.8) | |
| Improved (from those who reported changes) | 58.1 (56.1, 60.2) | 59.7 (56.6, 62.7) | 56.9 (54.2, 59.7) | 0.193 |
| Worsened (from those who reported changes) | 41.9 (39.8, 43.9) | 40.3 (37.3, 43.4) | 43.1 (40.3, 45.9) | |
| Cook more often | <0.001 | |||
| Yes | 56.9 (55.6, 58.1) | 51.8 (49.9, 53.6) | 61.4 (59.7, 63.1) | |
| No | 43.1 (41.9, 44.4) | 48.2 (46.4, 50.1) | 38.6 (36.9, 40.3) | |
| Change in the number of meals | 0.007 | |||
| No | 69.8 (68.6, 71.0) | 71.6 (69.9, 73.3) | 68.4 (66.7, 70.0) | |
| Yes | 30.2 (29.0,31.3) | 28.4 (26.7, 30.1) | 31.6 (30.0, 33.3) | |
| Increased (from those who reported changes) | 67.8 (65.6, 69.9) | 66.5 (63.1, 69.7) | 68.8 (65.8, 71.6) | 0.328 |
| Decreased (from those who reported changes) | 32.2 (30.1, 34.4) | 33.5 (30.1, 36.7) | 31.2 (28.4, 34.2) | |
| Snacking more often * | 0.186 | |||
| Yes | 31.4 (30.2, 32.6) | 32.2/30.5, 34.0) | 30.6 (29.0, 32.3) | |
| No | 68.6 (67.4, 69.8) | 67.8 (66.0, 69.5) | 69.4 (67.7, 71.0) | |
| Changes on shopping frequency | <0.001 | |||
| Decreased | 87.3 (86.3, 88.3) | 82.5 (80.7, 84.2) | 91.1 (89.9, 92.3) | |
| Increased | 12.7 (11.7, 13.7) | 17.5 (15.8, 19.3) | 8.9 (7.7, 10.1) | 0.317 |
| Self-reported changes in body weight | ||||
| No changes/do not know | 66.1 (63.8, 68.4) | 63.4 (60.2, 66.7) | 68.4 (65.2, 71.7) | |
| Increased | 21.0 (20.0, 22.0) | 22.3 (20.8, 23.9) | 19.8 (18.5, 21.3) | |
| Decreased | 12.9 (12.1, 13.8) | 14.3 (13.0, 15.6) | 11.7 (10.7, 12.9) | |
| Knowledge about dietary recommendations for lockdown period | <0.001 | |||
| Yes | 45.3 (44.0, 46.6) | 38.5 (36.7, 40.3) | 51.4 (49.6, 53.2) | |
| No | 54.7 (53.4, 56.0) | 61.5 (59.7, 63.3) | 48.6 (46.8, 50.4) | |
| Usefulness of dietary recommendations for lockdown period | <0.001 | |||
| None | 11.9 (10.7, 13.2) | 14.7 (12.7, 17.0) | 10.0 (8.6, 11.5) | |
| I am not sure | 10.5 (9.4, 11.7) | 9.2 (7.6, 11.0) | 11.3 (9.8, 12.9) | |
| Very useful | 77.6 (76.0, 79.2) | 76.0 (73.4, 78.5) | 78.7 (76.6, 80.6) |
Weighed data. Total (n = 5840), men (n = 2743), women (n = 3097); * Snacking is defined as any food eaten between main meals. Differences between men and women were tested by Chi-Square.
Figure 1.
Change in food intake during COVID-19 confinement.
Table 5.
Variation in food intake during COVID-19 social confinement by gender.
| Food Category | Reduced Intake | p | Increased Intake | p | Maintained Intake | |||
|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | |||
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |||
| Take-away or delivered meals | 43.3 (41.5, 45.2) |
44.3 (42.6, 46.1) |
0.459 | 9.8 (8.8, 11.0) |
5.5 (4.7, 6.3) |
<0.001 | 46.9 (45.0, 48.7) |
50.2 (48.4, 52.0) |
| Ready meals | 40.5 (38.7, 42.4) |
40.8 (39.1, 42.6) |
0.831 | 6.7 (5.9, 7.7) |
3.3 (2.7, 3.9) |
<0.001 | 52.7 (50.8, 54.6) |
55.9 (54.1, 57.6) |
| Soft drinks | 33.5 (31.7, 35.2) |
32.2 (30.6, 33.9) |
0.328 | 4.6 (3.8, 5.4) |
3.0 (2.5, 3.7) |
0.003 | 62.0 (60.2, 63.8) |
64.8 (63.0, 66.4) |
| Alcoholic beverages | 30.3 (28.6, 32.0) |
26.4 (24.9, 28.0) |
0.001 | 12.7 (11.6, 14.0) |
6.8 (6.0, 7.7) |
<0.001 | 57.0 (55.2, 58.9) |
66.8 (65.1, 68.4) |
| Savoury snacks | 28.2 (26.6, 29.9) |
30.7 (29.0, 32.3 |
0.044 | 9.3 (8.3, 10.4) |
8.5 (7.6, 9.5) |
0.311 | 62.5 (60.7, 64.3) |
60.8 (59.1, 62.5) |
| Sweet snacks | 19.0 (17.6, 20.5) |
20.9 (19.5, 22.3) |
0.082 | 28.8 (27.2, 30.6) |
32.8 (31.1, 34.4) |
0.001 | 52.2 (50.3, 54.0) |
46.4 (44.6, 48.1) |
| Fish and other seafood | 17.0 (15.7, 18.5) |
15.1 (13.8, 16.3) |
0.041 | 15.5 (14.2, 16.9) |
13.7 (12.5, 14.9) |
0.053 | 67.5 (65.7, 69.2) |
71.2 (69.6, 72.8) |
| Fruit juices | 14.1 (12.8, 15.4) |
17.0 (15.7, 18.3) |
0.003 | 12.6 (11.4, 13.9) |
12.0 (10.9, 13.2) |
0.498 | 73.2 (71.6, 74.9) |
71.0 (69.4, 72.6) |
| Other canned food (not seafood) | 13.8 (12.6, 15.1) |
16.4 (15.1, 17.7) |
0.006 | 9.5 (8.5, 10.7) |
9.9 (8.8, 10.9) |
0.69 | 76.7 (75.1, 78.3) |
73.8 (72.2, 75.3) |
| Meat | 12.5 (11.3, 13.7) |
11.8 (10.7, 13.0) |
0.47 | 8.6 (7.6, 9.7) |
6.8 (5.9, 7.7) |
0.012 | 78.9 (77.4, 80.5) |
81.4 (80.0, 82.7) |
| Canned seafood | 12.0 (10.8, 13.2) |
14.1 (12.9, 15.4) |
0.018 | 13.2 (11.9, 14.5) |
11.6 (10.5, 12.8) |
0.079 | 74.8 (73.2, 76.4) |
74.3 (72.7, 75.8) |
| Vegetables | 10.8 (9.6, 12.0) |
9.9 (8.9, 11.0) |
0.301 | 19.9 (18.4, 21.4) |
22.1 (20.7, 23.6) |
0.04 | 69.4 (67.6, 71.1) |
68.0 (66.3, 69.6) |
| Water | 10.2 (9.1, 11.4) |
14.2 (13.0, 15.5) |
<0.001 | 31.4 (29.7, 33.1) |
30.8 (29.2, 32.4) |
<0.001 | 58.4 (56.6, 60.3) |
55.0 (53.3, 56.8) |
| Fruit | 8.2 (7.2, 9.3) |
8.0 (7.1, 9.0) |
0.773 | 32.2 (30.5, 34.0) |
27.4 (25.9, 29.0) |
<0.001 | 59.6 (57.8, 61.4) |
64.6 (62.9, 66.2) |
| Dietary patterns | Total; % (95% CI) | Men; % (95% CI) | Women; % (95% CI) | p | ||||
| Improved dietary patterns | 18.2 (17.2, 19.2) | 18.1 (16.7, 19.6) | 18.3 (16.9, 19.7) | 0.193 | ||||
| Worsened dietary patterns | 10.8 (10.1, 11.7) | 12.9 (11.7, 14.2) | 9.0 (8.0, 10.1) | |||||
Weighed data. Men (n = 2743), women (n = 3097). Improved dietary patterns represent the increase of consumption of vegetables, fruit and fish. Worsened dietary patterns represent the increase of ready meals, soft drinks, savoury snacks and take-away and delivered meals); Differences between men and women were tested by Chi-Square.
Table 4 presents other changes in food consumption behaviour during the confinement period. Cooking more (56.9%) and a decrease in shopping frequency (87.3%) were the most reported changes. An increase in snacking between meals was also reported by 31.4% of the participants (Table 4).
Weight change was also reported by a significant proportion of participants. In this study, 21.0% and 12.9% of the participants reported an increase and decrease in body weight, respectively (Table 4).
The most frequently reported reasons for changes in food consumption during COVID-19 social confinement can be grouped into four main drivers: the need to reduce the frequency of shopping (34.3%); changes in appetite (changes in appetite in general (19.3%) and changes in appetite caused due to stress (18.6%)); changes in daily routines (different work schedule (17.6%) and changes on regular place for shopping (10.6%)), and changes related with the economic context (10.3%). The main reasons for changes in food consumption during COVID-19 social confinement seemed to be different according to gender. Changes in appetite in general (20.5% vs. 18.0%, p < 0.05) and changes in appetite caused by stress (19.5% vs. 15.9%, p < 0.001) were more frequently reported by women, while changes in daily routines (different work schedule) were more frequently reported by men (19.5% vs. 15.9%, p < 0.001) (Table 6).
Table 6.
Reasons for changes in food intake during COVID-19 social confinement.
| Reasons for Changes in Food Intake | Total | Men | Women | p |
|---|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | ||
| Changes in shopping frequency | 34.3 (33.1, 35.5) | 34.8 (33.0, 36.6) | 33.9 (32.3, 35.6) | 0.469 |
| Changes in appetite | 19.3 (18.3, 20.3) | 18.0 (16.6, 19.4) | 20.5 (19.1, 21.9) | 0.015 |
| Changes in appetite caused by stress | 18.6 (17.6, 19.6) | 14.1 (12.9, 15.5) | 22.6 (21.1, 24.0) | <0.001 |
| Different work schedule | 17.6 (16.6, 18.6) | 19.5 (18.0, 21.0) | 15.9 (14.7, 17.2) | <0.001 |
| Changes in regular place for shopping | 10.6 (9.9, 11.4) | 10.5 (9.4, 11.7) | 10.6 (9.6, 11.7) | 0.91 |
| Concerns with the economic context | 10.3 (9.5, 11.1) | 9.9 (8.8, 11.0) | 10.6 (9.5, 11.7) | 0.391 |
| Different people at meals time | 9.7 (9.0, 10.5) | 9.8 (8.8, 11.0) | 9.7 (8.7, 10.8) | 0.873 |
| Problems with access to usually bought food | 9.1 (8.4, 9.9) | 9.5 (8.5, 10.7) | 8.7 (7.8, 9.8) | 0.311 |
| Because diet can protect against the novel coronavirus | 5.5 (5.0, 6.1) | 6.0 (5.2, 7.0) | 5.1 (4.3, 5.9) | 0.114 |
| Changes on food prices | 4.8 (4.3, 5.4) | 5.3 (4.5, 6.2) | 4.3 (3.7, 5.1) | 0.087 |
| Fear of getting infected with the novel coronavirus through food | 3.8 (3.3, 4.3) | 4.0 (3.4, 4.8) | 3.5 (2.9, 4.2) | 0.264 |
| Concerns with possible stock rupture of food in supermarkets | 2.5 (2.1, 2.9) | 3.5 (2.9, 4.3) | 1.6 (1.2, 2.0) | <0.001 |
Weighed data. Total (n = 5840), men (n = 2743), women (n = 3097). Differences between men and women were tested by Chi-Square.
3.4. Combined Approach: Health and Risk Patterns
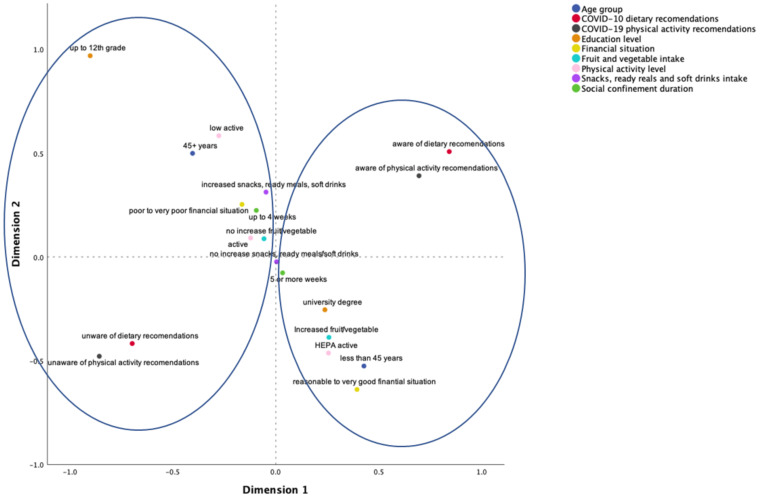
The MCA yielded two dimensions with eigenvalues of 1.715 and 1.344, respectively, and inertia of 0.191 (i.e., explaining 19.1% of the variance) and 0.149 (i.e., explaining 14.9% of the variance). The model explained 34% of the variance (inertia = 0.340, with an Eigenvalue of 3.059). From this analysis, two patterns were identified: a risky pattern and a healthy pattern (herein called clusters). Figure 2 displays the MCA results, showing the two clusters. The first cluster corresponds to a health-enhancing pattern with the co-occurrence of higher PA levels; increased fruit and vegetable consumption; awareness and knowledge of the COVID-19 PA and dietary recommendations; perceived financial situation as reasonable, good, or very good; higher educational level, as well as being for a shorter period of time in social confinement (up to 3 weeks). The second cluster is compatible with a risky pattern, pointing to the co-occurrence of low PA levels; increased consumption of savoury snacks, ready-to-eat meals, soft drinks, takeaways and decreased consumption of fruit and vegetables; not knowing about the COVID-19 PA and dietary recommendations; perceived financial situation as difficult or very difficult; lower educational level, as well as being for a longer period of time in social confinement (4 weeks or more).
Figure 2.
Health vs. risk patterns.
4. Discussion
This study sought to characterize PA and SB levels and changes in food behaviours and explore gender and other socio-demographic correlates, including a combined analysis of the health behaviours surveyed and their common determinants, in Portuguese adults. It was carried out during the first wave of the COVID-19 pandemic after governmental actions imposing social confinement and limiting participation in normal daily activities and routines.
Regarding PA levels, the results of this survey showed that the majority of the population surveyed reported HEPA (46.0% vs. 27.1% in 2017 IAN-AF [62]) and moderate PA levels (33.5% vs. 30.3% in 2017 IAN-AF [62]) during social confinement. Only 20.5% reported low PA levels (vs. 42.6% in 2017 IAN-AF [62]). These results conflict with other international surveys that described decreases in PA levels during confinement periods [41,42,44,45,46,47], and align with the literature pointing to an increase [49,50] and remarkable variations from country to country [51], highlighting the need for specific, comprehensive, national surveillance.
It is important to note that this increase in the prevalence of adequate HEPA levels did not occur homogeneously. Several influences need to be taken into consideration, namely the effects of (i) gender (42.6% of women were classified as HEPA vs. almost 50% men); (ii) age (as age decreased, the number of participants classified as HEPA increased significantly; and (iii) socioeconomic status (those with higher education and good perceived financial situation were more frequently classified as HEPA). Regarding SB, these influences also apply, although in a different direction: men, younger participants, those with higher education levels and with a favourable perception of the family financial situation, reported spending significantly more time sitting. Given these different influences (opposite risk directions), it might be that the promotion of behaviour change may have to follow different strategies and targets when it comes to reducing sitting time or increasing PA, especially in social-confinement contexts.
In this last regard, gender differences were also visible in the type of structured physical activities undertaken. Although walking was the most frequently reported PA in both genders, women significantly reported more physical fitness activities, whereas men reported more frequently being involved in strength training and running activities. For nonstructured PA, domestic activities and climbing up and down the stairs was expressively indicated by all participants inquired. Still, marked gender disparities were observed concerning domestic activities/household chores, with women being the ones that carried out these activities the most. Thus, it would be of paramount importance to further address the role of gender, especially considering that policy responses have not yet addressed the gendered impacts of disease outbreaks [63].
Concerning eating behaviours, this study showed that a high proportion of the population surveyed changed their eating habits during the confinement period of the first wave of the COVID-19 pandemic (45.1%), 58% of those reported an improvement in their diet (main positive changes reported: increase in fruit, vegetables, and water consumption and a decrease in savoury snacks, ready-to-eat meals, soft drinks, and alcoholic beverages intake), while 42% reported a worsening tendency, namely an increased consumption of sweet snacks. This data supports previous findings that both favorable and unfavorable changes in dietary habits were observed during the COVID-19 confinement period [64,65,66,67,68,69]. The confinement period had immediate effects on individuals’ lives, altering daily living routines, imposing food shopping restrictions (lower frequency), and worsening stress load [70]. All these factors seem to have impacted eating habits. However, for 18.2% of the participants, an improvement in eating habits was reported, with a combined increase in fruit, vegetables and fish and other seafood consumption, and more time spent cooking. Contrarily, a worsened dietary pattern was found for 10.8% of the population surveyed in our study, characterized by a combined increase in ready-to-eat meals, soft drinks, savoury snacks, and take-away and delivered meals. These findings are in line with a narrative synthesis [71] of the trajectories of food choices during the COVID-19 confinement periods that included 12 studies and showed an initial decline in diet quality. In general, diet was characterized by an increase in the consumption of carbohydrates sources and snacking. However, the results of this narrative review also found positive eating changes, such as a slightly increased consumption of fruit and vegetables and an important increase in the habit of cooking meals at home.
Moreover, our results also suggest that the COVID-19 pandemic might have increased the social gap in dietary quality. Individuals that live with a less comfortable income tend to have higher adherence to worsened dietary patterns. This survey’s results also allowed a more in-depth understanding of the main reasons pointed out for eating behaviours. Three main triggers were reported: (i) disruption in daily routines and work; (ii) changes in appetite due to anxiety feelings and stress; (iii) the economic uncertainty in terms of future access to food. These triggers were unequally distributed by gender. Disruption of work and daily routines was the most reported driver for men, while changes in appetite due to anxiety feelings and stress were more frequently reported by women.
Regarding the impact of the COVID-19 lockdown on eating habits, it is important to consider the economic damage effects on food insecurity. Data from our study shows a high percentage of individuals at risk of food insecurity (33.2%), and 8% are facing economic difficulties in accessing food. This prevalence is higher when compared to data from 2015/2016 (19.3% of Portuguese households living with food insecurity) [72,73].
Most importantly, and considering the potential interactional nature of the variables under analysis in this study (and that changes in one domain may aggregate with changes in others [56,57]), it is important to note that a combined approach, via MCA, highlighted the emergence of clusters of risk and health protection factors, suggesting, as in previous studies, that health-enhancing spill-over effects may arise when being more physically active and having a healthier eating pattern co-occur [74,75]. Furthermore, our results show that this protective behavioural pattern also clusters with a good perceived financial situation, higher educational level and awareness and knowledge of the COVID-19 PA and dietary recommendations for social confinement, launched by the Portuguese Directorate-General of Health’ Eating and PA National Promotion Programs. These findings are in line with the assertion that, more than a pandemic, COVID-19 may be a syndemic [76], inviting a larger vision, encompassing education, employment, housing, food, and environment, and recognizing how political and social factors drive, perpetuate, or worsen the emergence and clustering of diseases. Indeed, our second cluster further points to the co-occurrence of low PA levels: increased consumption of savoury snacks, soft drinks, take-aways, and decreased consumption of fruit and vegetables; not knowing about the COVID-19 PA and dietary recommendations; perceiving the financial situation as difficult or very difficult; lower educational level, as well as being for a longer period in social confinement (4 weeks or more).
Strengths and Limitations
This cross-sectional survey involved a large sample size that, after being weighted, is similar to the Portuguese residents’ population concerning sociodemographic characteristics. To overcome the constraints of pure online administration (only reaching a certain socio-demographic profile), phone interviews with the same set of questions were also conducted. Survey contents were based on self-report measures. Although device-based measures would be preferred due to their accuracy, the public health measures related to the pandemic precluded their use. Furthermore, device-based measures may not capture domain-and context-specific PA behaviours, essential for this study’s aims. Thus, according to best practices, the survey was based on widely used, validated methods to measure PA and SB [37]. Nonetheless, overestimation of PA may occur when IPAQ is used. In the domain of eating behaviours, an adapted self-report set of questions was also created. Following what has been advocated to conduct studies pertaining to a behavioural epidemiology framework [37], there was an effort in balancing the need for precision vs. feasibility (i.e., necessary adaptations for collecting data during the pandemic). The main analyses conducted in this study allowed us to describe the main PA and eating behaviours during a critical time (first wave of the pandemic-related social confinement), while also exploring their correlates and aggregation patterns, a much needed research endeavor given that, and despite a new burst of studies in this regard, the correlates of lifestyle behaviours (e.g., eating, PA, and SB) and their interactions remain under-researched [22], and international surveys have pointed to national and regional disparities that need to be further explored in the face of national and local public health policies and jurisdiction [6,37,51]. Longitudinal follow-ups will be needed to determine the long-term impact of pandemic-related public health measures on these critical health behaviours.
5. Conclusions
In Portugal, acknowledging the exceptions allowing for outdoor exercise, and also an increased offer of PA guidance and apps and all sorts of exercise classes available on social media, results indicate a positive scenario when compared to previous national surveys: raising the numbers of those in adequate HEPA levels and lowering the ones with low levels. The preferences expressed by the population surveyed may be informative for future health campaigns, highlighting not only the preference for walking and fitness activities, but also the role of informal activities as an intentional way of being active (e.g., house cleaning, climbing up and down stairs).
Concerning eating indicators, an increasing trend in perceived food insecurity was noticed when compared to previous surveys, a finding warranting the attention of public authorities. Changes in dietary habits occurred in positive and negative ways, and two patterns of eating behaviours emerged, suggesting that bad eating habits (e.g., increase savoury snacks, soft drinks, and take-away consumption and decrease in fruit and vegetable consumption) vs. good eating habits foods (e.g., fruit, vegetables, and fish) tend to cluster.
Nonetheless, all results need to be understood considering the role of gender, as significant differences emerged, and overall women tended to show impaired PA levels, stress-induced eating and different PA and eating patterns and preferences which need to be taken in consideration. Furthermore, age, socio-economic status, health literacy and time in social confinement were also correlates of the results, contributing to different health and risk patterns, highlighting: (i) the need for future interventions and public health policies to be more targeted to reach those most in need, in particular the most vulnerable groups, at-risk groups (older adults, socio-economically impaired persons, more time in social confinement); and (ii) the potential advantage, for future interventions and policies, of promoting PA and healthy eating simultaneously and in an integrated fashion, as positive spill-over effects may apply facilitating co-occurrence.
Acknowledgments
The authors wish to thank: (i) all the participants for taking the time to participate in the survey; (ii) the ISAMB team for their support in setting up the survey and data collection, (iii) Diana Mendes and Francisco Mata for their support on dissemination.
Author Contributions
Conceptualization, M.N.S., M.J.G., M.A. and G.F.; formal analysis, M.N.S., M.J.G., R.S., A.M., B.R., C.G. and C.S.S.; investigation, M.N.S., M.J.G., B.R., C.G., C.S.S., R.M., P.G., M.A. and G.F.; methodology, M.N.S., M.J.G., R.S., A.M., B.R., C.G., C.S.S., R.M., P.G., M.A. and G.F.; project administration, M.N.S. and M.J.G.; supervision, M.N.S., M.J.G. and G.F.; validation, C.S.S.; writing—original draft, M.N.S., M.J.G., R.S., A.M. and P.G.; writing—review & editing, M.N.S., M.J.G., R.S., A.M., B.R., C.G., C.S.S., R.M., P.G., M.A. and G.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. The survey was funded by the Portuguese Directorate-General of Health. The following authors are supported by the Portuguese Foundation for Science and Technology: R.S. (CEECIND/01069/2017 and FCT/UIDB/00617/2020), B.R. (UI/BD/150675/2020), and C.S.S. (SFRH/BD/139603/2018).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the Centro Académico de Medicina de Lisboa.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available from the authors upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kluge H.H.P., Wickramasinghe K., Rippin H.L., Mendes R., Peters D.H., Kontsevaya A., Breda J. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet. 2020;395:1678–1680. doi: 10.1016/S0140-6736(20)31067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bas D., Martin M., Pollack C., Venne R. The Impact of COVID-19 on Sport, Physical Activity and Well-Being and Its Effects on Social Development-Policy Brief No. 73. United Nations Department of Economic and Social Affairs; New York, NY, USA: 2020. [Google Scholar]
- 3.World Health Organization Coronavirus Disease (COVID-19) Pandemic. World Health Organization. [(accessed on 3 August 2020)]; Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 4.World Health Organization . COVID-19 Strategy Update-14 April 2020. World Health Organization; Geneva, Switzerland: 2020. [Google Scholar]
- 5.Ainsworth B.A., Li F. Physical activity during the coronavirus disease-19 global pandemic. J. Sport Health Sci. 2020;9:291–292. doi: 10.1016/j.jshs.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., Bouaziz B., Bentlage E., How D., Ahmed M., et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12:1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woods J.A., Hutchinson N.T., Powers S.K., Roberts W.O., CarmenGomez-Cabrera M., Radak Z., Berkes I., Boros A., Boldogh I., Leeuwenburg C., et al. The COVID-19 pandemic and physical activity. Sports Med. Health Sci. 2020;2:55–64. doi: 10.1016/j.smhs.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen P., Mao L., Nassis G.P., Harmer P., Ainsworth B.E., Li F. Coronavirus disease (COVID-19): The need to maintain regular physical activity while taking precautions. J. Sport Health Sci. 2020;9:103–104. doi: 10.1016/j.jshs.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hall G., Laddu D.R., Phillips S.A., Lavie C.J., Arena R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog. Cardiovasc. Dis. 2021;64:108–110. doi: 10.1016/j.pcad.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gakidou E., Afshin A., Abajobir A.A., Abate K.H., Abbafati C., Abbas K.M., Abd-Allah F., Abdulle A.M., Abera S.F., Aboyans V., et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lippi L.G., Henry B.M., Sanchis-Gomar F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19) Eur. J. Prev. Cardiol. 2020;27:906–908. doi: 10.1177/2047487320916823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jakobsson J., Malm C., Furberg M., Ekelund U., Svensson M. Physical activity during the coronavirus (COVID-19) pandemic: Prevention of a decline in metabolic and immunological functions. Front. Sports Act. Living. 2020;2:57. doi: 10.3389/fspor.2020.00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martinez-Ferran M., de la Guía-Galipienso F., Sanchis-Gomar F., Pareja-Galeano H. Metabolic impacts of confinement during the COVID-19 pandemic due to modified diet and physical activity habits. Nutrients. 2020;12:1549. doi: 10.3390/nu12061549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mattioli A.V., Sciomer S., Cocchi C., Maffei S., Gallina S. Quarantine during COVID-19 outbreak: Changes in diet and physical activity increase the risk of cardiovascular disease. Nutr. Metab. Cardiovasc. Dis. 2020;30:1409–1417. doi: 10.1016/j.numecd.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Banerjee S., Burkholder G., Sana B., Szirony G.M. Social Isolation as a predictor for mortality: Implications for COVID-19 prog-nosis. MedRxiv. 2020 (preprint) [Google Scholar]
- 16.Elovainio M., Hakulinen C., Pulkki-Råback L., Virtanen M., Josefsson K., Jokela M., Vahtera J., Kivimäki M. Contribution of risk factors to excess mortality in isolated and lonely individuals: An analysis of data from the UK Biobank cohort study. Lancet Public Health. 2017;2:e260–e266. doi: 10.1016/S2468-2667(17)30075-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sahle B.W., Chen W., Melaku Y.A., Akombi B.J., Rawal L.B., Renzaho A.M.N. Association of psychosocial factors with risk of chronic diseases: A nationwide longitudinal study. Am. J. Prev. Med. 2020;58:e39–e50. doi: 10.1016/j.amepre.2019.09.007. [DOI] [PubMed] [Google Scholar]
- 18.Peçanha T., Goessler K.F., Roschel H., Gualano B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am. J. Physiol. Heart Circ. Physiol. 2020;318:H1441–H1446. doi: 10.1152/ajpheart.00268.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nicholson N.R. A review of social isolation: An important but underassessed condition in older adults. J. Prim. Prev. 2012;33:137–152. doi: 10.1007/s10935-012-0271-2. [DOI] [PubMed] [Google Scholar]
- 20.Arora T., Grey I. Health behaviour changes during COVID-19 and the potential consequences: A mini-review. J. Health Psychol. 2020;25:1155–1163. doi: 10.1177/1359105320937053. [DOI] [PubMed] [Google Scholar]
- 21.Betsch C., Wieler L.H., Habersaat K. Monitoring behavioural insights related to COVID-19. Lancet. 2020;395:1255–1256. doi: 10.1016/S0140-6736(20)30729-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balanzá-Martínez V., Atienza-Carbonell B., Kapczinski F., de Boni R.B. Lifestyle behaviours during the COVID-19-time to connect. Acta Psychiatr. Scand. 2020;141:399–400. doi: 10.1111/acps.13177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.British Dietetic Association Eating Well during Coronavirus/COVID-19. British Dietetic Association. [(accessed on 3 August 2020)]; Available online: https://www.bda.uk.com/resource/eating-well-during-coronavirus-covid-19.html.
- 24.World Health Organization Food and Nutrition during Self-Quarantine: What to Choose and How to Eat Healthily. Geneva, Switzerland: World Health Organization. [(accessed on 3 August 2020)]; Available online: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/news/news/2020/3/food-and-nutrition-during-self-quarantine-what-to-choose-and-how-to-eat-healthily.
- 25.World Health Organization Regional Office for Europe Food and Nutrition Tips during Self-Quarantine. World Health Organization. [(accessed on 4 August 2020)]; Available online: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/novel-coronavirus-2019-ncov-technical-guidance/food-and-nutrition-tips-during-self-quarantine.
- 26.Barazzoni R., Bischoff S.C., Breda J., Wickramasinghe K., Krznaric Z., Nitzan D., Pirlich M., Singer P. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin. Nutr. 2020;39:1631–1638. doi: 10.1016/j.clnu.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hill J.O., Wyatt H.R., Peters J.C. Energy balance and obesity. Circulation. 2012;126:126–132. doi: 10.1161/CIRCULATIONAHA.111.087213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Siordia J.A. Epidemiology and clinical features of COVID-19: A review of current literature. J. Clin. Virol. 2020;127:104357. doi: 10.1016/j.jcv.2020.104357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walsh N.P., Gleeson M., Shephard R.J., Gleeson M., Woods J.A., Bishop N.C., Fleshner M., Green C., Pedersen B.K., Hoffman-Goetz L., et al. Position statement. Part one: Immune function and exercise. Exerc. Immunol. Rev. 2011;17:6–63. [PubMed] [Google Scholar]
- 30.Martin S.A., Pence B.D., Woods J.A. Exercise and respiratory tract viral infections. Exerc. Sport Sci. Rev. 2009;37:157–164. doi: 10.1097/JES.0b013e3181b7b57b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Da Silveira M.P., da Silva Fagundes K.K., Bizuti M.R., Starck É., Rossi R.C., de Resende e Silva D.T. Physical exercise as a tool to help the immune system against COVID-19: An integrative review of the current literature. Clin. Exp. Med. 2021;21:15–28. doi: 10.1007/s10238-020-00650-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nieman D.C. Coronavirus disease-2019: A tocsin to our aging, unfit, corpulent, and immunodeficient society. J. Sport Health Sci. 2020;9:293–301. doi: 10.1016/j.jshs.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nieman D.C., Wentz L.M. The compelling link between physical activity and the body’s defense system. J. Sport Health Sci. 2019;8:201–217. doi: 10.1016/j.jshs.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.U.S. Department of Health and Human Services . Physical Activity Guidelines for Americans. 2nd ed. Department of Health and Human Services; Washington, DC, USA: 2018. [Google Scholar]
- 35.World Health Organization . WHO Guidelines on Physical Activity and Sedentary Behaviour. World Health Organization; Geneva, Switzerland: 2020. [Google Scholar]
- 36.Füzéki E., Groneberg D.A., Banzer W. Physical activity during COVID-19 induced lockdown: Recommendations. J. Occup. Med. Toxicol. 2020;15:25. doi: 10.1186/s12995-020-00278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sallis J.F., Adlakha D., Oyeyemi A., Salvo D. An international physical activity and public health research agenda to inform coronavirus disease-19 policies and practices. J. Sport Health Sci. 2020;9:328–334. doi: 10.1016/j.jshs.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sallis R., Young D.R., Tartof S.Y., Sallis J.F., Sall J., Li Q., Smith G.N., Cohen D.A. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients. Br. J. Sports Med. 2021:1–8. doi: 10.1136/bjsports-2021-104080. [DOI] [PubMed] [Google Scholar]
- 39.Son J.S., Nimrod G., West S.T., Janke M.C., Liechty T., Naar J.J. Promoting older adults’ physical activity and social well-being during COVID-19. Leis. Sci. 2021;43:287–294. doi: 10.1080/01490400.2020.1774015. [DOI] [Google Scholar]
- 40.Dwyer M.J., Pasini M., De Dominicis S., Righi E. Physical activity: Benefits and challenges during the COVID-19 pandemic. Scand. J. Med. Sci. Sports. 2020;30:1291. doi: 10.1111/sms.13710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Deschasaux-Tanguy M., Druesne-Pecollo N., Esseddik Y., de Edelenyi F.S., Allès B., Andreeva V.A., Baudry J., Charreire H., Deschamps V., Egnell M. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March-May 2020): Results from the French NutriNet-Santé cohort study. Am. J. Clin. Nutr. 2021;113:924–938. doi: 10.1093/ajcn/nqaa336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Flanagan E.W., Beyl R.A., Fearnbach S.N., Altazan A.D., Martin C.K., Redman L.M. The impact of COVID-19 stay-at-home orders on health behaviors in adults. Obesity. 2021;29:438–445. doi: 10.1002/oby.23066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hossain M.M., Sultana A., Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: A systematic umbrella review of the global evidence. Epidemiol. Health. 2020;42:e2020038. doi: 10.4178/epih.e2020038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stockwell S., Trott M., Tully M., Shin J., Barnett Y., Butler L., McDermott D., Schuch F., Smith L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021;7:e000960. doi: 10.1136/bmjsem-2020-000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Castañeda-Babarro A., Arbillaga-Etxarri A., Gutiérrez-Santamaría B., Coca A. Physical activity change during COVID-19 con-finement. Int. J. Environ. Res. Public Health. 2020;17:6878. doi: 10.3390/ijerph17186878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McCarthy H., Potts H.W.W., Fisher A. Physical activity behavior before, during, and after COVID-19 restrictions: Longitudinal smartphone-tracking study of adults in the United Kingdom. J. Med. Internet Res. 2021;23:e23701. doi: 10.2196/23701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lesser I.A., Nienhuis C.P. The impact of COVID-19 on physical activity behavior and well-being of Canadians. Int. J. Environ. Res. Public Health. 2020;17:3899. doi: 10.3390/ijerph17113899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spence J.C., Rhodes R.E., McCurdy A., Mangan A., Hopkins D., Mummery W.K. Determinants of physical activity among adults in the United Kingdom during the COVID-19 pandemic: The DUK-COVID study. Br. J. Health Psychol. 2021;26:588–605. doi: 10.1111/bjhp.12497. [DOI] [PubMed] [Google Scholar]
- 49.Faulkner J., O’Brien W.J., McGrane B., Wadsworth D., Batten J., Askew C.D., Badenhorst C., Byrd E., Coulter M., Draper N., et al. Physical activity, mental health and well-being of adults during initial COVID-19 containment strategies: A multi-country cross-sectional analysis. J. Sci. Med. Sport. 2021;24:320–326. doi: 10.1016/j.jsams.2020.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Smith L., Jacob L., Butler L., Schuch F., Barnett Y., Grabovac I., Veronese N., Caperchione C., Lopez-Sanchez G.F., Meyer J., et al. Prevalence and correlates of physical activity in a sample of UK adults observing social distancing during the COVID-19 pandemic. BMJ Open Sport Exerc. Med. 2020;6:e000850. doi: 10.1136/bmjsem-2020-000850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tison G.H., Avram R., Kuhar P., Abreau S., Marcus G.M., Pletcher M.J., Olgin J.E. Worldwide effect of COVID-19 on physical activity: A descriptive study. Ann. Intern. Med. 2020;173:767–770. doi: 10.7326/M20-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maertl T., de Bock F., Huebl L., Oberhauser C., Coenen M., Jung-Sievers C., on behalf of the COSMO Study Team Physical activity during COVID-19 in German adults: Analyses in the COVID-19 Snapshot Monitoring Study (COSMO) Int. J. Environ. Res. Public Health. 2021;18:507. doi: 10.3390/ijerph18020507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Antunes R., Frontini R., Amaro N., Salvador R., Matos R., Morouço P., Rebelo-Gonçalves R. Exploring lifestyle habits, physical activity, anxiety and basic psychological needs in a sample of Portuguese adults during COVID-19. Int. J. Environ. Res. Public Health. 2020;17:4360. doi: 10.3390/ijerph17124360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khoramipour K., Basereh A., Hekmatikar A.A., Castell L., Ruhee R.T., Suzuki K. Physical activity and nutrition guidelines to help with the fight against COVID-19. J. Sports Sci. 2021;39:101–107. doi: 10.1080/02640414.2020.1807089. [DOI] [PubMed] [Google Scholar]
- 55.Polero P., Rebollo-Seco C., Adsuar J.C., Pérez-Gómez J., Rojo-Ramos J., Manzano-Redondo F., Garcia-Gordillo M.Á., Carlos-Vivas J. Physical activity recommen-dations during COVID-19: Narrative review. Int. J. Environ. Res. Public Health. 2020;18:65. doi: 10.3390/ijerph18010065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marks D.F. A General Theory of Behaviour. SAGE Publications Ltd.; London, UK: 2018. [Google Scholar]
- 57.Silva A.M., Júdice P.B., Carraça E.V., King N., Teixeira P.J., Sardinha L.B. What is the effect of diet and/or exercise interventions on behavioural compensation in non-exercise physical activity and related energy expenditure of free-living adults? A systematic review. Br. J. Nutr. 2018;119:1327–1345. doi: 10.1017/S000711451800096X. [DOI] [PubMed] [Google Scholar]
- 58.Bauman A., Bull F., Chey T., Craig C.L., Ainsworth B.E., Sallis J.F., Bowles H.R., Hagstromer M., Sjostrom M., Pratt M., et al. The International Prevalence Study on Physical Activity: Results from 20 countries. Int. J. Behav. Nutr. Phys. Act. 2009;6:21. doi: 10.1186/1479-5868-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Craig C.L., Marshall A.L., Sjostrom M., Bauman A.E., Booth M.L., Ainsworth B.E., Pratt M., Ekelund U., Yngve A., Sallis J.F., et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 60.IPAQ Research Committee Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)-Short and Long Forms. IPAQ Research Committee. [(accessed on 10 August 2020)]; Available online: https://docs.google.com/viewer?a=v&pid=sites&srcid=ZGVmYXVsdGRvbWFpbnx0aGVpcGFxfGd4OjE0NDgxMDk3NDU1YWRlZTM.
- 61.Rezende L.F.M., Sá T.H., Mielke G.I., Viscondi J.Y.K., Rey-López J.P., Garcia L.M.T. All-cause mortality attributable to sitting time: Analysis of 54 countries worldwide. Am. J. Prev. Med. 2016;51:253–263. doi: 10.1016/j.amepre.2016.01.022. [DOI] [PubMed] [Google Scholar]
- 62.Lopes C., Torres D., Oliveira A., Severo M., Guiomar S., Alarcão V., Vilela S., Ramos E., Rodrigues S., Oliveira L., et al. National food, nutrition and physical activity survey of the Portuguese general population. EFSA Supporting Publ. 2017;14:1341E. doi: 10.2903/sp.efsa.2017.EN-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Smith J. Overcoming the ‘tyranny of the urgent’: Integrating gender into disease outbreak preparedness and response. Gend. Dev. 2019;27:355–369. doi: 10.1080/13552074.2019.1615288. [DOI] [Google Scholar]
- 64.Kriaucioniene V., Bagdonaviciene L., Rodríguez-Pérez C., Petkeviciene J. Associations between changes in health behaviours and body weight during the COVID-19 quarantine in Lithuania: The Lithuanian COVIDiet Study. Nutrients. 2020;12:3119. doi: 10.3390/nu12103119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Di Renzo L., Gualtieri P., Pivari F., Soldati L., Attinà A., Cinelli G., Leggeri C., Caparello G., Barrea L., Scerbo F., et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020;18:229. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sidor A., Rzymski P. Dietary choices and habits during COVID-19 lockdown: Experience from Poland. Nutrients. 2020;12:1657. doi: 10.3390/nu12061657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Błaszczyk-Bębenek E., Jagielski P., Bolesławska I., Jagielska A., Nitsch-Osuch A., Kawalec P. Nutrition behaviors in Polish adults before and during COVID-19 lockdown. Nutrients. 2020;12:3084. doi: 10.3390/nu12103084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pellegrini M., Ponzo V., Rosato R., Scumaci E., Goitre I., Benso A., Belcastro S., Crespi C., de Michieli F., Ghigo E., et al. Changes in weight and nutritional habits in adults with obesity during the "lockdown" period caused by the COVID-19 virus emergency. Nutrients. 2020;12:2016. doi: 10.3390/nu12072016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Reyes-Olavarría D., Latorre-Román P., Guzmán-Guzmán I.P., Jerez-Mayorga D., Caamaño-Navarrete F., Delgado-Floody P. Positive and negative changes in food habits, physical activity patterns, and weight status during COVID-19 confinement: Associated factors in the Chilean population. Int. J. Environ. Res. Public Health. 2020;17:5431. doi: 10.3390/ijerph17155431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Abbas A.M., Kamel M.M. Dietary habits in adults during quarantine in the context of COVID-19 pandemic. Obes. Med. 2020;19:100254. doi: 10.1016/j.obmed.2020.100254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zupo R., Castellana F., Sardone R., Sila A., Giagulli V.A., Triggiani V., Cincione R.I., Giannelli G., de Pergola G. Preliminary trajectories in dietary behaviors during the COVID-19 pandemic: A public health call to action to face obesity. Int. J. Environ. Res. Public Health. 2020;17:7073. doi: 10.3390/ijerph17197073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gregório M.J., Rodrigues A.M., Graça P., de Sousa R.D., Dias S.S., Branco J.C., Canhão H. Food insecurity is associated with low adherence to the Mediterranean Diet and adverse health conditions in Portuguese adults. Front. Public Health. 2018;6:38. doi: 10.3389/fpubh.2018.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Huizar M.I., Arena R., Laddu D.R. The global food syndemic: The impact of food insecurity, malnutrition and obesity on the healthspan amid the COVID-19 pandemic. Prog. Cardiovasc. Dis. 2021;64:105–107. doi: 10.1016/j.pcad.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mata J., Silva Marlene N., Vieira Paulo N., Carraça Eliana V., Andrade Ana M., Coutinho Sílvia R., Sardinha Luis B., Teixeira Pedro J. Motivational “spill-over” during weight control: Increased self-determination and exercise intrinsic motivation predict eating self-regulation. Health Psychol. 2009;28:709–716. doi: 10.1037/a0016764. [DOI] [PubMed] [Google Scholar]
- 75.Carraça E.V., Rodrigues B., Teixeira D.S. A motivational pathway linking physical activity to body-related eating cues. J. Nutr. Educ. Behav. 2020;52:1001–1007. doi: 10.1016/j.jneb.2020.08.003. [DOI] [PubMed] [Google Scholar]
- 76.Horton R. Offline: COVID-19 is not a pandemic. Lancet. 2020;396:874. doi: 10.1016/S0140-6736(20)32000-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the authors upon reasonable request.