Abstract
To date, several cases of thrombosis have been confirmed to be related to Sars-CoV-2 infection. Multiple attempts detected the prolonged occurrence of Sars-CoV-2 viral RNA (long COVID) in whole blood suggesting that virus byproducts may remain within cells and tissues well over the disease has finished. Patients may develop severe thrombocytopenia, acute anemia of inflammation and, systemic thrombosis with the fatal course of disease, which is suggestive of further interferences of Sars-CoV-2 on hematopoietic stem cells (HSCs) within the differentiation process towards erythroid and megakaryocytic cells. Therefore, we speculated whether Sars-CoV-2 propagates in or compartmentalizes with hematopoietic progenitor, erythroid, and megakaryocytic cells as the main cause of thrombotic events in either COVID-19 patients or vaccinated individuals. Results: The Sars-CoV-2 RNA replication, protein translation and infectious particle formation as the spike proteins in hematopoietic cell lines take place via the angiotensin-converting enzyme 2 (ACE2) entry pathway within primary CD34+ HSCs inducing, ex vivo, the formation of defected erythroid and megakaryocytic cells that eventually become targets of humoral and adaptive immune cells. Conclusions: Viral particles from affected CD34+ HSCs or the cellular component of RBC units and eventually platelets, present the greatest risk for sever thrombosis-transmitted Sars-CoV-2 infections.
Keywords: COVID-19, Sars-CoV-2, CD34+ hematopoietic stem cell (HSCs), thrombosis, thrombophilia, angiotensin-converting enzyme 2 (ACE2)
1. The CD-34+ Hematopoietic Stem Cells and the Risk of Thrombocytopenia and Thrombotic Events in COVID-19 Infection, the Hypotheses of the Disturbances in the Myeloid Trait
Sars-CoV-2 virus, a member of the Coronavirus family, was recently isolated in 2019 in the city of Wuhan in Hubei province, People’s Republic of China, as the etiologic agent of coronavirus disease 2019 (COVID-19). The Sars-CoV-2 virus caused several large outbreaks in Asia before it spread through Europe, the Americas and India [1,2]. The majority of infected people remain asymptomatic or develop mild symptoms such as fever, cough, conjunctivitis, myalgia, fatigue and, minor neuropathies [3]. However, more severe complications such as Guillain-Barré syndrome in adults and elderly have been associated with Sars-CoV-2 infection and led to the declaration of COVID-19 as a Public Health Emergency of International Concern by the World Health Organization (WHO) in 2020 [4,5,6].
Data from different studies confirmed a drastic drop in platelet count (thrombocytopenia), microcytic anemia, low iron, and a fatal outcome for a patient with sickle cell anemia. These observations raised the question whether Sars-CoV-2 has the capability to infect hematopoietic stem cells interfering in the myeloid differentiation process and particularly those cells belonging to the erythroid and megakaryocytic lineage [7].
During hematopoiesis, multipotent human HSCs and progenitor cells, characterized by the expression of a cluster of differentiation 34 (CD34), are able to differentiate into several lineages, including common myeloid cells and lymphoid progenitors (Figure 1). Myeloid progenitor cells differentiate to megakaryocyte/erythroid lineage or granulocyte/macrophage progenitor phenotypes.
Figure 1.
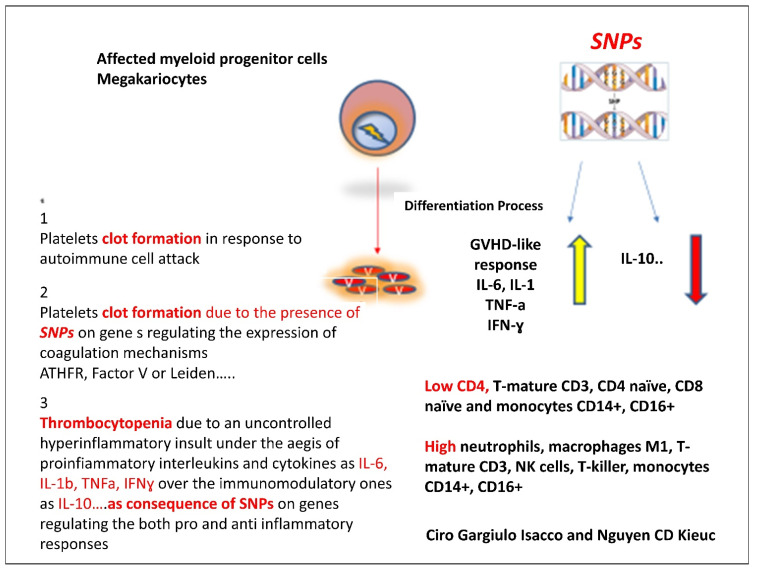
The etiopathogenesis of thrombotic event caused by the S proteins released by the Sars-CoV-2 virus. The current hypothesis is substantially based on three momenta: (i) The subversive activity perpetrated by the virus at the very beginning of the initial differentiation phase of CD34+ HSCs towards the myeloid lineage. (ii) The presence of SNPs at various level of the immune system’s both inflammatory and modulatory response. (iii) SNPs present of gene controlling the coagulation system (MTHFR and Leiden).
The entire process of differentiation to erythrocytes, megakaryocytes, and megakaryocyte-derived platelets is mainly driven by erythropoietin (EPO) and thrombopoietin (TPO) [8,9]. During the differentiation process, the HSCs lose the distinctive CD34+ marker; instead, the erythroid and megakaryocytic differentiation is characterized by the appearance of CD71/Glycophorin A (GLYA) or CD41/CD42b (Figure 1) on erythrocytes and megakaryocytes/platelets, respectively [10,11,12].
Sars-CoV-2 was reported to infect leukocytes—mainly monocytes and macrophages—and B and T cells subtypes—mainly CD4, CD4 naïve, CD8 naïve, T suppressor (CD8-CD57) and T regs (CD4+CD25+high) [13]. However, so far, little is known about the infection of CD34+ HSCs or platelets phenotype by Sars-CoV-2.
Nevertheless, the mechanism of Sars-CoV-2 infection is well understood and could presumably work for any types of cells. The binding between the viral surface spike glycoprotein (S) and target cell surface takes place via the angiotensin-converting enzyme-2 (ACE2), followed by the cleavage of S by the transmembrane protease serine 2 (TMPRSS2). Several research teams observed that this mechanism via ACE2 could also be observed in intestinal epithelial cells, hepatocytes, and neurons, which explains the multiplicity of symptoms that characterize COVID-19 disease [13,14]. Since recently, an aberrant increase in erythroid progenitors together with an aberrant decrease in platelets circulation has been showed either in critical hospitalized cases or after receiving the vaccine shot. Indeed, these observations together with hypoxia, hypocapnia, alkalosis, iron anemia, and coagulopathies were seen highly correlated with an alarming grade of death risk [15,16,17]. Of note, progenitors of the erythroid and myeloid lineage appear to be the only cell types expressing both ACE2 and TMPRSS2 among the cells present in bone marrow. Medical reports from COVID-19 patients showed an increased mean platelet volume (MPV) and platelet hyperactivity, which were occasionally associated with a decrease in the overall platelet count. In our experience, detectable Sars-CoV-2 RNA in the blood stream was associated with platelet hyperactivity in critically ill patients.
Zhang and colleagues clearly demonstrated that platelets are able to express ACE2 and TMPRSS2; they also described the mechanism by which Sars-CoV-2 spike proteins induce platelet hyper-activation and super-aggregation via PAC-1 binding, CD62P expression, α granule secretion and dense granule release, thereby enhancing thrombosis formation [18].
Although they provided clear evidence suggesting the role of the MAPK pathway, downstream of ACE2, enhancing the magnitude of Sars-CoV-2 on platelet activation, in releasing coagulation factors, inflammatory factors, and in the formation of leukocyte–platelet aggregates, we assume otherwise that this is not comprehensive. In fact, the coagulation process was well described by Di Castelnuovo and colleagues referring to the hypercoagulable condition as a possible pathogenic mechanism contributing to disease progression and lethality in COVID-19 hospitalized patients [18]. The insurgence of rare thrombosis events either in COVID-19 affected patients or in post-vaccinated individuals needs further consideration. In our opinion, four factors should be considered: (i) the formation of the “abnormal” platelet progenies from Sars-CoV-2-infected myeloid megakaryocytes which become targets of host immunity (T cells, Th1, NK cells, macrophage M-1); (ii) the presence of single nucleotide polymorphisms (SNPs) on genes regulating the coagulation cascade such as MTHFR and Leiden-factor V; (iii) SNPs at the level of genes regulating the expression of both pro-inflammatory responses (IL-6, TNFα, IFNγ) and immune-modulatory responses (IL-10); (iv) fast platelets turnover with an average lifespan of 8–10 days (Figure 1 and Figure 2).
Figure 2.
The capacity of the Sars-CoV-2 of interfering the differentiation process from CD34+ to megakaryocytes tend to generate a lineage of affected platelets that become target of autoimmune response via macrophages-M1, neutrophils, T-killers that in turn increase the production of pro-inflammatory cytokines and interleukins IL-6, IL-1β, TNFα and INFγ. The impossibility of reversing the process is probably due to two main factors; first, the presence of SNPs on genes regulate the expression of coagulative factors such as MTHFR and Leiden factor; second, the SNPs present on genes regulate the inflammatory responses (IL-6, IL-1β, TNFα and INFγ) and genes conversely regulate the immunomodulatory responses (IL-10, TGF-β).
Several viruses showed this capability of interfering during the myeloid differentiation process to platelets or erythrocytes mainly in consequence of their fast turnover and due to their short half-life. The example may come from idiopathic thrombocytopenic purpura (acute or chronic) that may follow a viral illness, such as chickenpox or Zika virus. In Zika infection, authors observed that cell contagion started from the granulocyte/macrophage lineage, by which patients developed severe thrombocytopenia and microcytic anemia, stressing that the death risk may have followed in complications due to the interference of Zika virus with erythroid and megakaryocytic cells. According to the authors, the hematopoiesis phase is a crucial moment for the Zika virus to execute its opportunistic attack. This is the most critical phase as multipotent human hematopoietic stem and progenitor cells (HSPCs-CD34) start differentiating into several lineages, including common myeloid (CMP) and lymphoid (CLP) progenitors [19,20,21].
The contaminated platelet progenies become an easy and highly vulnerable target of the host immune cells. In addition, in response to an acute infectious phase, such as sepsis, platelets tend to be hyper-reactive promoting the formation of disseminated intravascular coagulation (DIC), which obstructs vessels leading to the formation of systemic ischemic blood clots and multiple organ failure [22,23]. In this scenario, platelets will be both the target and promoter of an uncontrolled pro-inflammatory cytokine storm and bind to neutrophils and release NETs, which in COVID-19 terminal patient promotes lung collapse and failure [22,23,24,25].
The presence of SNPs in cytokine and interleukin genes promotes a further aggravation of the symptoms. The variants not only could be related to the disease susceptibility and cytokine storm, but to COVID-19 complications as well. For instance, variants in ACE2 and TMPRSS2 have been associated to irreversible thrombotic risk condition, while variants in both IL-6 and IL-10, which regulate the level of inflammatory and immune modulatory response, may compromise the correct balance between the two phases leading to an uncontrolled irreversible inflammatory process. The low or total lack of the expression of IL-10 together with an overexpression of IL-6, TNFα and IFNγ as a consequence of polymorphisms attracts great attention especially in diseases following metabolic dysfunctions and in aging-related diseases, typical features of COVID-19-affected individuals. All this information open up a new discussion on COVID-19, especially if one considers the long COVID disease manifestation as it may exhibit different patterns with permanent organ damages and persistent post-COVID symptoms [26,27,28,29].
2. Validating the Premises
Albeit, it is yet scientifically to be demonstrated, there are raising concerns toward a possible association between SARS-CoV-2 and the potential breakdown of the hematopoietic stem cells differentiation process which causes thrombocytopenia, thrombolytic events and acute anemia. We proposed here in accordance with recent immunological advancements in COVID-19 research a new model of pathogenesis. This means that COVID-19 is a complex condition consequent of multiple local, systemic and genetic factors that worsen an individual’s correct response.
Several results and findings have validated this hypothesis. The analysis and measurement of serum CD34+ HSCs, affected megakaryocytes and platelets, the polymorphism on cytokines and interleukins, the over-expression of T-cells, neutrophils NET and M1 macrophages are all features that have been routinely found and assessed which eventually explain those death cases of devastating thrombosis as a consequence of Sars-CoV-2 and vaccine-released S proteins.
In addition, due to its close relation to Zika and Dengue virus present in the Asia Pacific region, the Americas and the Caribbean, the Sars-CoV-2 virus similarly showed its association with significant clinical manifestations such as neural damages and the Guillain-Barré Syndrome, a tropism that has been seen in the context of hematopoietic stem cells activity [30]. We also speculated that Sars-CoV-2-induced impairment of blood vessel integrity or development is mainly related to the high degree of inflammation due to the presence of specific polymorphisms (SNPs) on genes in charge of regulating inflammatory and immune-modulatory responses such as IL-6, IL-1a;b, TNF-α, IFN-γ and IL-10. However, further investigations are crucial to unravel the connection of Sars-CoV-2 pathogenicity and symptom manifestation towards prevention and therapy.
Author Contributions
Conceptualization, C.G.I., K.C.D.N., A.M.I., F.I., G.D., F.L., A.S., S.T., G.M., A.M., M.E.M. and P.D.; Methodology, M.G.B., C.G.I., R.L. (Rita Lazzaro), A.D.I., G.D. and R.L. (Rita Laforgia); Software, T.C.T., P.D., A.M.I., S.K.A., D.T., F.I., F.L., A.S., A.D.I., S.T., G.M. A.P., R.L. (Rita Laforgia) and A.C.; Validation, A.M., M.G.B., G.M., P.D., A.P., R.L. (Rita Lazzaro), L.V., D.I. and V.H.P.; Formal Analysis, F.I., G.D., C.G.I. and D.T., A.D.I.; Investigation, C.G.I., K.C.D.N., A.P., D.I., M.G.B., F.I., V.H.P. and L.V.; Resources, M.G.B. and P.D.; Data Curation, C.G.I., A.C., G.D. and P.D.; Writing—Original Draft Preparation, C.G.I., A.D.I. and A.P.; Writing—Review and Editing, F.I., A.S., F.L., A.S. and C.G.I.; Visualization, A.M.I., M.E.M., T.C.T., S.T., F.L., A.D.I. and P.D.; Supervision, A.S., G.M., C.G.I., F.L., L.V., S.T., M.E.M., A.M., G.D., F.I. and M.G.B.; Project Administration, F.I., G.D., L.V., S.K.A. and A.M.I.; Funding Acquisition, F.I., D.T. and A.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All experimental data to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhou P., Yang X.-L., Wang X.-G., Hu B., Zhang L., Zhang W., Si H.-R., Zhu Y., Li B., Huang C.-L., et al. A Pneumonia Outbreak Associated with a New Coronavirus of Probable Bat Origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu F., Zhao S., Yu B., Chen Y.-M., Wang W., Song Z.-G., Hu Y., Tao Z.-W., Tian J.-H., Pei Y.-Y., et al. A New Coronavirus Associated with Human Respiratory Disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ratajczak M.Z., Kucia M. SARS-CoV-2 Infection and Overactivation of Nlrp3 Inflammasome as a Trigger of Cytokine “Storm” and Risk Factor for Damage of Hematopoietic Stem Cells. Leukemia. 2020;34:1726–1729. doi: 10.1038/s41375-020-0887-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mantefardo B., Gube A.A., Awlachew E., Sisay G. Novel Coronavirus (COVID-19)-Associated Guillain–Barre’ Syndrome: Case Report. IMCRJ. 2021;14:251–253. doi: 10.2147/IMCRJ.S305693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caress J.B., Castoro R.J., Simmons Z., Scelsa S.N., Lewis R.A., Ahlawat A., Narayanaswami P. COVID-19-Associated Guillain-Barré Syndrome: The Early Pandemic Experience. Muscle Nerve. 2020;62:485–491. doi: 10.1002/mus.27024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coronavirus Disease (COVID-19) Situation Reports. [(accessed on 23 July 2021)]; Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 7.Nur E., Gaartman A.E., Tuijn C.F.J., Tang M.W., Biemond B.J. Vaso-occlusive Crisis and Acute Chest Syndrome in Sickle Cell Disease Due to 2019 Novel Coronavirus Disease (COVID-19) Am. J. Hematol. 2020;95:725–726. doi: 10.1002/ajh.25821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bieber E. Erythropoietin, the Biology of Erythropoiesis and Epoetin Alfa. An Overview. J. Reprod. Med. 2001;46:521–530. [PubMed] [Google Scholar]
- 9.Kaushansky K. The Molecular Mechanisms That Control Thrombopoiesis. J. Clin. Investig. 2005;115:3339–3347. doi: 10.1172/JCI26674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luck L., Zeng L., Hiti A.L., Weinberg K.I., Malik P. Human CD34+ and CD34+CD38− Hematopoietic Progenitors in Sickle Cell Disease Differ Phenotypically and Functionally from Normal and Suggest Distinct Subpopulations That Generate F Cells. Exp. Hematol. 2004;32:483–493. doi: 10.1016/j.exphem.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Kratz-Albers K., Scheding S., Möhle R., Bühring H.J., Baum C.M., Mc Kearn J.P., Büchner T., Kanz L., Brugger W. Effective Ex Vivo Generation of Megakaryocytic Cells from Mobilized Peripheral Blood CD34+ Cells with Stem Cell Factor and Promegapoietin. Exp. Hematol. 2000;28:335–346. doi: 10.1016/S0301-472X(99)00152-6. [DOI] [PubMed] [Google Scholar]
- 12.Attar A. Changes in the Cell Surface Markers during Normal Hematopoiesis: A Guide to Cell Isolation. Glob. J. Hematol. Blood Transfus. 2014;1:20–28. doi: 10.15379/2408-9877.2014.01.01.4. [DOI] [Google Scholar]
- 13.Huerga Encabo H., Grey W., Garcia-Albornoz M., Wood H., Ulferts R., Aramburu I.V., Kulasekararaj A.G., Mufti G., Papayannopoulos V., Beale R., et al. Human Erythroid Progenitors Are Directly Infected by SARS-CoV-2: Implications for Emerging Erythropoiesis in Severe COVID-19 Patients. Stem Cell Rep. 2021;16:428–436. doi: 10.1016/j.stemcr.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Odak I., Barros-Martins J., Bošnjak B., Stahl K., David S., Wiesner O., Busch M., Hoeper M.M., Pink I., Welte T., et al. Reappearance of Effector T Cells Is Associated with Recovery from COVID-19. EBioMedicine. 2020;57:102885. doi: 10.1016/j.ebiom.2020.102885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shahbaz S., Xu L., Osman M., Sligl W., Shields J., Joyce M., Tyrrell L., Oyegbami O., Elahi S. Erythroid Precursors and Progenitors Suppress Adaptive Immunity and Get Invaded by SARS-CoV-2. Stem Cell Rep. 2021;16:1165–1181. doi: 10.1016/j.stemcr.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Balzanelli M., Distratis P., Catucci O., Amatulli F., Cefalo A., Lazzaro R., Aityan K.S., Dalagni G., Nico A., De Michele A., et al. Clinical and Diagnostic Findings in COVID-19 Patients: An Original Research from SG Moscati Hospital in Taranto Italy. J. Biol. Regul. Homeost. Agents. 2021;35:171–183. doi: 10.23812/20-605-A. [DOI] [PubMed] [Google Scholar]
- 17.Cavezzi A., Troiani E., Corrao S. COVID-19: Hemoglobin, Iron, and Hypoxia beyond Inflammation. A Narrative Review. Clin. Pract. 2020;10:24–30. doi: 10.4081/cp.2020.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Di Castelnuovo A., Costanzo S., Antinori A., Berselli N., Blandi L., Bonaccio M., Cauda R., Guaraldi G., Menicanti L., Mennuni M., et al. Heparin in COVID-19 Patients Is Associated with Reduced In-Hospital Mortality: The Multicenter Italian CORIST Study. Thromb. Haemost. 2021;121:1054–1065. doi: 10.1055/a-1347-6070. [DOI] [PubMed] [Google Scholar]
- 19.Zhang S., Liu Y., Wang X., Yang L., Li H., Wang Y., Liu M., Zhao X., Xie Y., Yang Y., et al. SARS-CoV-2 Binds Platelet ACE2 to Enhance Thrombosis in COVID-19. J. Hematol. Oncol. 2020;13:120. doi: 10.1186/s13045-020-00954-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roth H., Schneider L., Eberle R., Lausen J., Modlich U., Blümel J., Baylis S.A. Zika Virus Infection Studies with CD34+ Hematopoietic and Megakaryocyte-Erythroid Progenitors, Red Blood Cells and Platelets. Transfusion. 2020;60:561–574. doi: 10.1111/trf.15692. [DOI] [PubMed] [Google Scholar]
- 21.Balzanelli G.M., Distratis P., Amatulli F., Lazzaro R., Cefalo A., Dangela G., Catucci O., Palazzo D., Tomassone D., Pham S.A., et al. Would The End Of COVID-19 Infection As A Chronic Disease? J. Stem Cells Res. Dev. Ther. 2020;6:1–3. doi: 10.24966/SRDT-2060/100057. [DOI] [Google Scholar]
- 22.Balzanelli M.G., Distratis P., Aityan S.K., Amatulli F., Catucci O., Cefalo A., De Michele A., Dipalma G., Inchingolo F., Lazzaro R., et al. An Alternative “Trojan Horse” Hypothesis for COVID-19: Immune Deficiency of IL-10 and SARS-CoV-2 Biology. Endocr. Metab. Immune Disord. Drug Targets. 2021;21:1. doi: 10.2174/1871530321666210127141945. [DOI] [PubMed] [Google Scholar]
- 23.Balzanelli G.M., Distratis P., Amatulli F., Catucci O., Cefalo A., Lazzaro R., Palazzo D., Aityan K.S., Dipalma G., Inchingolo F. Clinical Features in Predicting COVID-19. Biomed. J. Sci. Tech. Res. 2020;29:22921–22926. [Google Scholar]
- 24.Greco E., Lupia E., Bosco O., Vizio B., Montrucchio G. Platelets and Multi-Organ Failure in Sepsis. Int. J. Mol. Sci. 2017;18:2200. doi: 10.3390/ijms18102200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vardon-Bounes F., Ruiz S., Gratacap M.-P., Garcia C., Payrastre B., Minville V. Platelets Are Critical Key Players in Sepsis. Int. J. Mol. Sci. 2019;20:3494. doi: 10.3390/ijms20143494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ballini A., Dipalma G., Isacco C.G., Boccellino M., Di Domenico M., Santacroce L., Nguyễn K.C.D., Scacco S., Calvani M., Boddi A., et al. Oral Microbiota and Immune System Crosstalk: A Translational Research. Biology. 2020;9:131. doi: 10.3390/biology9060131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cazzolla A.P., Lovero R., Lo Muzio L., Testa N.F., Schirinzi A., Palmieri G., Pozzessere P., Procacci V., Di Comite M., Ciavarella D. Taste and Smell Disorders in COVID-19 Patients: Role of Interleukin-6. ACS Chem. Neurosci. 2020;11:2774–2781. doi: 10.1021/acschemneuro.0c00447. [DOI] [PubMed] [Google Scholar]
- 28.Fernández-de-Las-Peñas C., Palacios-Ceña D., Gómez-Mayordomo V., Cuadrado M.L., Florencio L.L. Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): An Integrative Classification. Int. J. Environ. Res. Public Health. 2021;18:2621. doi: 10.3390/ijerph18052621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nejad J.H., Heiat M., Hosseini M.J., Allahyari F., Lashkari A., Torabi R., Ranjbar R. Guillain-Barré Syndrome Associated with COVID-19: A Case Report Study. J. Neurovirol. 2021 doi: 10.1007/s13365-021-00984-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gargiulo C., Hai N.T., Nguyen K.C., Kim N.D., Van T.N., Tuan A.L., Abe K., Flores V., Shiffman M. Autologous Peripheral Blood Stem Cells and γ/δ T Cells May Improve Immunity in Treating Secondary Bacteremic Infection in HIV Infected Patient. Stem Cell Discov. 2015;5:48. doi: 10.4236/scd.2015.54006. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All experimental data to support the findings of this study are available from the corresponding author upon request.