Abstract
Necrotic enteritis is an important enteric disease in poultry, caused by NetB-producing Clostridium (C.) perfringens strains. As no straight-forward method to assess the NetB activity of C. perfringens was available, we aimed to develop an easy, high-throughput method to measure the NetB activity produced by C. perfringens. First, the appearance of C. perfringens on different avian blood agar plates was assessed. Based on the size of the haemolysis surrounding the C. perfringens colonies, NetB-positive strains could phenotypically be discriminated from NetB-negative strains on both chicken and duck blood agar. Additionally, strains producing the consensus NetB protein induced more pronounced haemolysis on chicken blood agar as compared to the weak outer haemolysis induced by A168T NetB-variant-producing C. perfringens strains. Next, a 96-well plate-based haemolysis assay to screen NetB activity in the C. perfringens culture supernatants was developed. Using this assay, a positive correlation between the in vitro NetB activity and virulence of the C. perfringens strains was shown. The developed activity assay allows us to screen novel C. perfringens isolates for their in vitro NetB activity, which could give valuable information on their disease-inducing potential, or identify molecules and (bacterial) metabolites that affect NetB expression and activity.
Keywords: in vitro activity assay, haemolysis, avian red blood cells, NetB, Clostridium perfringens
1. Introduction
The Gram-positive, spore-forming bacterium Clostridium (C.) perfringens is an anaerobic pathogen, known to cause a variety of histotoxic and enterotoxic diseases in humans and animals. The pathogen can produce more than 20 toxins [1,2]. Not all C. perfringens toxins are produced by all strains. Most of the toxin structural genes are encoded on large plasmids, one of which also includes the necrotic enteritis toxin B (NetB) [2,3]. NetB is the causative toxin for avian necrotic enteritis (NE), a disease that causes significant economic losses in the poultry industry worldwide due to compromised bird performance and increased morbidity and mortality [4,5,6]. To date, no effective non-antibiotic control strategies are available, although different control methods that could potentially prevent NE are being developed and are under investigation. These either intervene in the pathogenesis (e.g., control of predisposing factors, vaccines) or improve the microbiota–host interaction (e.g., dietary additives) [7,8]. While it is well established that the expression of virulence genes of a number of pathogens is affected by environmental factors and molecules, this area of research is under-explored for C. perfringens toxins [9,10,11,12].
To investigate the efficacy of a putative compound that might help controlling NE, time-consuming and expensive animal trials are usually required. These trials are necessary once a possible treatment is discovered. However, if the goal is to test whether a single compound might have a direct effect on NetB activity, a simple, rapid assay could provide a first indication on the efficacy of said compound. Traditionally, detection of NetB toxin activity is performed by an in vitro LMH cell-based toxicity assay [13,14]. This method is labour intensive and time consuming, and the induced cytotoxicity is a result of a combination of cytotoxic compounds secreted in the culture supernatants rather than NetB alone. More recently, Lee et al. described the development of an ELISA to detect the NetB toxin in both culture supernatants and biological samples [15,16]. Although such an ELISA is specific for NetB, no information on the biological activity is obtained. Therefore, there is a clear need for a simple, rapid test that specifically determines the NetB activity. Such an assay would allow us to screen novel C. perfringens isolates for their NetB activity, which could give valuable information on their disease-inducing potential. Additionally, it could be used to identify molecules and (bacterial) metabolites that affect NetB expression and activity.
Haemolysis assays are commonly used for the detection and quantification of C. perfringens alpha toxin (CPA) and perfringolysin O (PFO) production in vitro. The specificity of these assays is linked to differences in the susceptibility of RBCs from various host species towards the respective toxins, with CPA activity being detected using sheep RBCs, whereas PFO is routinely detected using horse RBCs [17,18,19,20,21]. In the current study, we aimed to develop a simple, rapid, and cost-effective activity assay based on the haemolytic properties of NetB, that can be used in a high-throughput format to specifically measure NetB toxin activity in C. perfringens culture supernatants. The NetB activity assay was developed, based on the observation that NetB has haemolytic activity towards red blood cells (RBC) of different avian species, such as chicken, duck and goose [22]. The useability of the developed assay is shown by screening the NetB production of different C. perfringens isolates and comparing the NetB titre with the in vivo virulence of the strains.
2. Materials and Methods
2.1. Bacterial Strains and Growth Conditions
A collection of 9 NetB-positive and 5 NetB-negative C. perfringens strains isolated from broiler chickens was used (Table 1). Additionally, an alpha toxin mutant and a NetB toxin mutant from strain NE 18 were used (Table 1). All C. perfringens strains were grown on Columbia agar (Oxoid, Basingstoke, UK) in an anaerobic chamber with atmosphere containing 10% H2, 10% CO2 and 80% N2 (Jacomex, Dagneux, France). The identity of the NetB protein (consensus NetB or A168T variant NetB, [23,24]) was determined by amplifying a 448 bp region of the netB sequence spanning the region coding for the AA substitution (nucleotide substitution at position 502) using primers netB(186)FW: 5′-TGATACCGCTTCACATAAAGGT-3′ and netB(612)REV: 5′-ACCGTCCTTAGTCTCAACAAAT-3′, and Sanger sequencing of the obtained PCR amplicons by Eurofins Genomics (Ebersberg, Germany). The numbers included in the primer name indicate the 5′ position of the sense strand relative to the start codon (TTG) of the netB gene. C. perfringens strains were cultured anaerobically for 24 h at 37 °C in TGY broth (3% tryptone (Sigma Aldrich, St. Louis, MO, USA), 2% yeast extract (Sigma Aldrich), 0.1% glucose (Sigma Aldrich) and 0.1% L-cysteine (Sigma Aldrich)) unless stated otherwise. To determine the effect of the culture medium on the C. perfringens NetB toxin production, C. perfringens TGY overnight (ON) cultures were diluted 1/1000 in fresh TGY broth, BHI broth (VWR, Belgium) or minimal medium (MM; 50% tryptic soy broth (Sigma Aldrich), 25% nutrient broth (Oxoid) and 25% peptone water (Oxoid)), followed by anaerobic incubation for 24 h at 37 °C. To monitor the bacterial growth and toxin production, samples were taken every hour for seven hours including a last time point after 24 h. Strains remained under anaerobic conditions during the whole time period. Bacterial growth was determined by plating serial dilutions of the cultures on Columbia agar plates, followed by ON incubation at 37 °C under anaerobic conditions (Figure S1). Cell-free supernatants from the C. perfringens cultures were obtained by centrifugation at 4500× g for 5 min at 4 °C, followed by filtration of the supernatants through a 0.2 µm filter, and stored at −20 °C.
Table 1.
C. perfringens strains used in this study.
| Strain ID (Alternative Name) | NetB d | netB Sequence a | Description | Origin | Reference |
|---|---|---|---|---|---|
| JIR4869 (EHE-NE18) | + | Con b | Necrotic enteritis, broiler | Australia | [25] |
| JIR12071 (NE18 Δα, NE18-M1) | + | Con b | Alpha toxin mutant from strain JIR4869 | Australia | [25] |
| JIR12331 (NE18 ΔnetB) | − | NetB toxin mutant from strain JIR4869 | Australia | [13] | |
| JIR4860 (EHE-NE5) | + | Con b | Necrotic enteritis, broiler | Australia | [25] |
| JIR4866 (EHE-NE15) | + | Con b | Necrotic enteritis, broiler | Australia | [25] |
| JIR12058 (UNK-NE30) | + | G502A (A168T) c | Necrotic enteritis, broiler | Australia | [23] |
| JIR4857 | − | Necrotic enteritis, broiler | Australia | [26] | |
| CP3 | − | Healthy broiler | Belgium | [27] | |
| CP4 | − | Healthy broiler | Belgium | [27] | |
| CP23 | + | G502A (A168T) c | Healthy broiler | Belgium | [14] |
| CP56 (JIR12037) | + | Con b | Necrotic enteritis, broiler | Belgium | [27] |
| D3 (99.63206-34) | + | G502A (A168T) b | Necrotic enteritis, broiler | Denmark | [23] |
| S2 | − | Necrotic enteritis, broiler | Denmark | [28] | |
| S36 | + | G502A (A168T) c | Necrotic enteritis, broiler | Denmark | - |
| JGS4100 | + | G502A (A168T) c | Necrotic enteritis, broiler | USA | G. Songer, pers.com. |
| JGS4121 | − | Necrotic enteritis, broiler | USA | G. Songer, pers. com. |
a C. perfringens netB sequence. Con: EHE-NE18 netB consensus sequence (EU143239); G502A (A168T): netB sequence with a nucleotide change at position 502 of the coding sequence (Change from Ala to Thr at amino acid position 168 of the NetB protein). b C. perfringens netB sequence reported by Keyburn et al. 2010 [23]. The nucleotide substitution reported by Keyburn et al. was numbered relative to the start of the sequencing place (i.e., 267 bp upstream of the netB start codon), resulting in G769A. This corresponds to position 502 of the netB gene reported by Abildgaard et al. 2010 and this study [24]. c C. perfringens netB sequence obtained in this study. d Distinction between NetB-positive and NetB-negative C. perfringens strains. +: NetB-positive C. perfringens strain. −: NetB-negative C. perfringens strain.
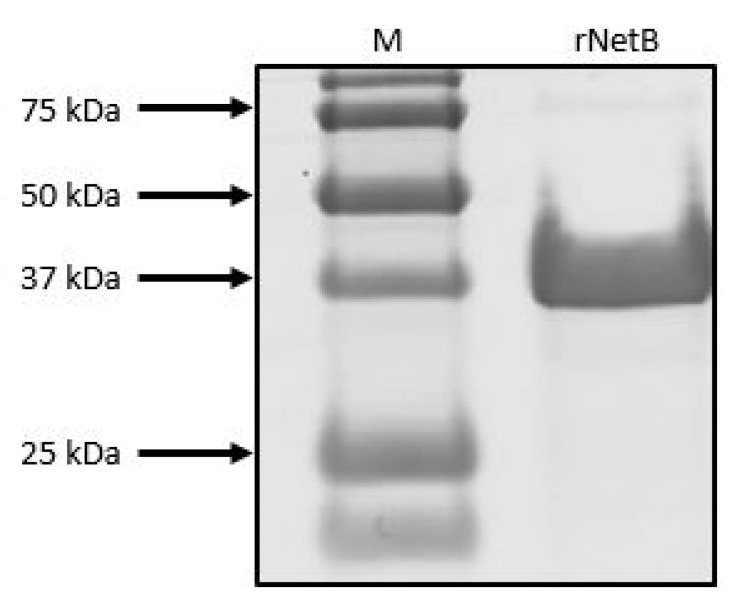
2.2. Recombinant NetB Production
Mature recombinant NetB, without its native signal peptide, was expressed in Escherichia coli using the pBAD TOPO® TA Expression Kit (Invitrogen, Paisley, UK). A fragment encoding the C. perfringens NetB toxin (consensus netB gene; GenBank accession number EU143239.1) was amplified from the DNA of C. perfringens strain CP56 by PCR using a DNA polymerase with proofreading activity (Accuzyme, Bioline, Randolph, MA, USA). The forward primer (5′-GTTCTTGAGGAATAATAAATGAGTGAATTAAATGACATAAAC-3′) contained an in-frame stop codon and translation re-initiation sequence to remove the N-terminal leader and allow native protein expression. The reverse primer (5′-GTTCTTCAGATAATATTCTATTTTATGATCTTGCCAATT-3′) excluded the native netB gene stop codon. The resulting PCR product was incubated with Taq polymerase for 10 min at 72 °C (5 U; Promega, Madison, WI, USA) to add 3′ A-overhangs, cloned into the pBAD-TOPO expression vector and transformed into One Shot TOP10® E. coli. The correct orientation of the netB toxin insert was verified by Sanger sequencing. Recombinant E. coli carrying the pBAD-NetB expression vector was grown at 37 °C and 125 rpm for 3 h until an OD600 of ±0.5 in Terrific Broth supplemented with 100 µg/mL ampicillin. Once the desired OD was reached, protein expression was induced with 0.002% L-arabinose (Sigma Aldrich) and the culture was further incubated ON at 37 °C and 125 rpm. Bacteria were harvested by centrifugation at 100,000 × g, 4 °C for 10 min (Beckman Coulter, Avanti J-E Ultracentrifuge), and pellets were subjected to one freeze–thaw cycle (−20 °C), followed by enzymatic lysis using BugBuster (Invitrogen). NetB protein was purified using a Ni-sepharose column (HisGravisTRap, GE Healthcare, Chicago, IL, USA) according to the manufacturer’s instructions. Finally, the purified protein was dialysed ON at 4 °C in phosphate-buffered saline containing 10% glycerol. Protein concentration was measured using BCA protein assay (Thermo Fisher Scientific, Waltham, MA, USA) and purity was assessed with SDS-PAGE (Figure 1). The produced rNetB was subsequently used to test its activity against chicken RBCs in a 96-well format.
Figure 1.
SDS-PAGE of purified recombinant NetB. The purified protein (rNetB) was separated by 12% SDS-PAGE and Precision Plus Protein™ Standard (BioRad) was used as a size marker (M). SDS-PAGE was stained with Brilliant Blue G; band representing rNetB appears at the expected size of 33 kDa.
2.3. Assessing the Potential of Avian Blood Agar Plates to Discriminate between NetB-Negative and NetB-Positive C. perfringens Strains
To determine whether NetB-positive and NetB-negative C. perfringens strains can be distinguished from each other based on the haemolytic activity towards blood from different avian species, an agar diffusion assay was performed. Therefore, Columbia blood agar (CBA) was prepared using Columbia blood agar base (Oxoid, Basingstoke, UK) supplemented with 5% of either goose, duck or chicken blood. Blood was added after sterilisation of the agar base, followed by dispersing the medium in 120 × 120 mm Petri dishes, air drying at room temperature and storing at 4 °C for maximum 30 days. The haemolytic profile after direct growth of C. perfringens on the CBA agar plates was determined by transferring the C. perfringens strain from an ON culture to the agar plates with a sterile toothpick. Additionally, the haemolytic activity in the supernatants of C. perfringens strains grown ON in TGY was determined. Therefore, small holes were pierced into the agar with the rear end of 20–200 µL pipette tips (diameter 7 mm) which were filled with 20 µL of supernatant per strain. Plates were incubated anaerobically overnight at 37 °C and subsequently scanned with a GS-800 calibrated densitometer (Bio-Rad Laboratories, Hercules, CA, USA). The diameter of the different haemolysis zones was measured using Quantity One software (Bio-Rad Laboratories).
2.4. Determination of the C. perfringens Haemolytic Activity towards Chicken Erythrocytes in a 96-Well Plate-Based Format
Chicken RBCs were obtained from whole blood by centrifugation at 1500× g for 10 min at room temperature (RT), after which the supernatant was removed and RBCs were gently resuspended in Hank’s Balanced Salt Solution (HBSS, Thermo Fisher Scientific). After another two washing steps with HBSS, the RBCs were diluted to a final concentration of 2% RBCs in HBSS (v/v). The haemolytic activity of the rNetB towards chicken RBCs was confirmed by incubating serial two-fold dilutions of the rNetB (starting from 40 µg/mL, diluted in HBSS) with an equal volume of 2% chicken RBCs. To determine whether chicken RBC haemolysis could be used as a measure to discriminate between NetB-positive and NetB-negative C. perfringens strains, equal volumes of chicken RBCs were incubated with 20% culture supernatants. In each assay, RBCs incubated with HBSS were used as a negative control (0% haemolysis), whereas RBCs diluted in distilled water (dH2O) were used as positive control (100% haemolysis). After incubation of the 96-well microtiter plates at 37 °C for 30 min, the plates were centrifuged to pellet intact red blood cells (1 min, 1000× g, RT). The supernatants were transferred to a new 96-well microtiter plate and the OD550nm was determined (Multiskan GO, Thermo Scientific). Haemolytic activity was observed by the increase in absorbance due to the release of haemoglobin from the erythrocytes.
2.5. Assessing the NetB-Specific Haemolytic Activity in C. perfringens Supernatants by Blocking Alpha Toxin and Perfringolysin-Induced Haemolysis
In addition to the NetB toxin, C. perfringens also produces other haemolytic toxins, namely alpha toxin (CPA) and perfringolysin O (PFO). In order to determine the NetB-specific activity in the C. perfringens culture supernatants, the haemolytic activity of CPA and PFO should be neutralised. Therefore, the activity of CPA and PFO was neutralised by incubating the culture supernatants with polyclonal antiserum from calves immunised with a native NetB-negative C. perfringens toxin preparation [29]. The CPA- and PFO-neutralising capacity of the antiserum was previously published [29]. In order to determine the amount of antiserum needed to completely block the CPA- and PFO-induced haemolysis towards chicken RBCs, a two-fold dilution series of the antiserum (20%–0.4% antiserum) was incubated with a constant amount of C. perfringens culture supernatants (20% SN), for 30 min at 37 °C prior to the addition of an equal volume of 2% chicken RBCs. C. perfringens culture supernatants without antiserum were used as a control. All measurements were performed in duplicate (technical replicates), using three independent biological replicates, consisting of supernatants from different ON cultures as well as blood from different birds.
2.6. Final Doubling Dilution Assay Protocol to Determine the NetB Titre in C. perfringens Culture Supernatants
In order to determine the NetB titre in C. perfringens culture supernatants, a doubling dilution assay protocol was established. Therefore, non-NetB haemolytic activities were blocked by incubating a two-fold dilution series of C. perfringens culture supernatants (ranging from 20 to 0.04% SN, diluted in HBSS) with an equal volume of antiserum directed towards both CPA and PFO (0.5% final concentration). This C. perfringens supernatants–antiserum mixture was incubated at 37 °C for 30 min, after which an equal volume of 2% pre-warmed chicken RBCs was added to each well, followed by 30 min incubation at 37 °C. Chicken RBCs diluted in dH20 or HBSS were used as, respectively, a positive control (100% haemolysis), or negative control (0% haemolysis). For the calculation of the NetB titres for all strains, the blank (mean value of all wells containing negative control) was subtracted from all other OD values, after which a Hill curve was fitted to the concentration–response data to calculate the LD50 values for each strain, which represent the supernatant dilution that causes 50% haemolysis. The assay was performed in technical duplicate, for three biological replicates.
A detailed protocol to raise antisera towards C. perfringens CPA and PFO is added in Supplementary File 1. The protocols to determine the concentration of antiserum needed to block non-NetB haemolytic toxins can be found in Supplementary File 2, whereas the final protocol to determine the NetB titre is present in Supplementary File 3.
2.7. Detection of Alpha Toxin Activity
To determine the alpha toxin activity in the supernatants of strains JIR12058, EHE-NE18, CP56, JIR4866 and JIR4860, the lecithinase activity was assayed in an egg yolk agar well diffusion assay [30,31,32]. Therefore, small holes were pierced into Columbia agar supplemented with 2% egg yolk (v/v) with the rear end of a 20–200 µL pipette tip (diameter 7 mm), which were filled with 20 µL of supernatant per tested strain. A standard was included on each plate by preparing a two-fold dilution series of Phospholipase C (Sigma Aldrich) ranging from 1 to 0.0313 U/mL. Plates were incubated anaerobically overnight at 37 °C and scanned with a GS-800 calibrated densitometer (Bio-Rad Laboratories, Hercules, CA, USA). Alpha toxin activity was indicated by the development of turbidity. The area of the opaque zones was measured using ImageJ software (U.S. National Institutes of Health, Bethesda, MD, USA).
2.8. Statistical Analysis
Statistical analysis was performed using GraphPad Prism 8.4.3. For not normally distributed values, a Mann–Whitney U test (2 groups) or Kruskal–Wallis test (>2 groups) was performed to identify significant differences between groups, otherwise an independent t-test (2 groups) or ANOVA (>2 groups) was employed to identify significant differences between groups. For comparison of the NetB titres of different C. perfringens strains grown in different culture media, a two-way ANOVA was preformed, followed by a Tukey’s multiple comparison test. Pearson correlation was applied to assess whether there was a link between the NetB titres and the previously published virulence of the C. perfringens strains [23]. As the alpha toxin activity was not normally distributed, a Spearman correlation was applied to determine the correlation between the alpha toxin activity and either the NetB titre or virulence of the C. perfringens strains. For all analyses, p-values smaller than 0.05 were considered statistically significant.
3. Results
3.1. Assessing the C. perfringens Haemolysis Patterns on Avian Blood Agar Plates
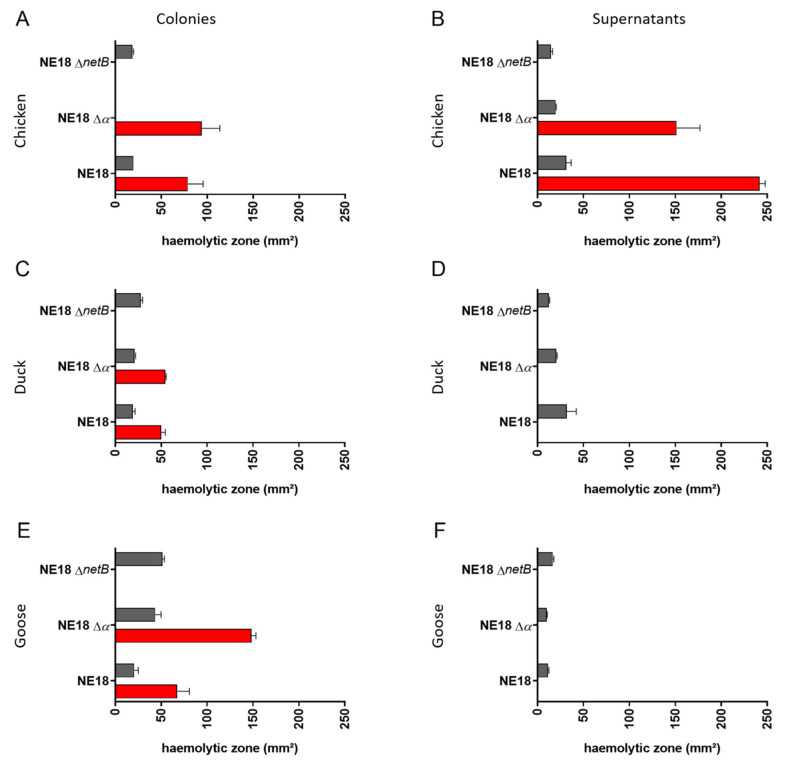
Colonies of a NetB-positive C. perfringens strain (NE18) as well as its NetB mutant (NE18 ΔnetB), and its alpha toxin mutant (NE18 Δα) were grown on Columbia agar supplemented with either chicken, duck or goose blood (Figure 2 and Figure S2A). The wild-type NE18 strain induced a double haemolysis zone on all avian blood types, while the NetB mutant (NE18 ΔnetB) did not induce an outer haemolysis zone on any of the tested avian blood agars (Figure 2A,C,E), indicating that the outer haemolysis zone might be caused by NetB. However, no zone with complete clearing around the colonies was observed, with both the inner and outer haemolysis zone showing only partial haemolysis on all avian blood agar types. This makes it difficult to differentiate between an inner and outer haemolysis zone, an effect that was most pronounced on chicken and duck agar (Figure S2A). When the alpha toxin mutant was grown on CBA supplemented with chicken blood, no boundary between the inner and outer haemolytic zone could be observed, and only the outer haemolysis was measured (Figure 2A). It was, however, possible to measure the inner haemolytic zone against duck and goose blood (Figure 2C,E), indicating that this inner haemolytic zone is likely induced by a combination of other haemolysins, such as perfringolysin O.
Figure 2.
Inner and outer haemolysis induced by C. perfringens strain NE18, its NetB mutant (NE18 ∆netB) and its alpha toxin mutant (NE18 ∆α) on Columbia agar supplemented with blood from different avian species ((A,B): chicken blood; (C,D): duck blood; (E,F): goose blood). Comparison of haemolysis induced from colonies (left column; (A,C,E)) or supernatants (right column; (B,D,F)) was assessed. Grey bars indicate inner haemolysis while red bars represent outer haemolytic zone.
In addition to growing the C. perfringens strains directly on the avian blood agar plates, supernatants from C. perfringens ON cultures grown in TGY were tested on the plates. In contrast to the situation where the C. perfringens colonies were grown on the agar, the culture supernatants did induce a narrow zone of complete haemolysis on all avian blood agar plates (Figure S2B). Additionally, on chicken blood agar, both supernatants from the wild-type NE18 strain, as well as from the alpha toxin mutant strain (NE18 ∆α), were able to induce a subtle, weak outer haemolysis zone. However, supernatants of the NetB mutant strain (NE18 ∆netB) did not induce an outer haemolytic zone on chicken blood agar (Figure 2B), indicating that the outer haemolytic zone is caused by NetB. On plates with duck and goose blood, no outer haemolysis was induced by any of the supernatants (Figure 2D,F), whereas the complete inner haemolytic zones were induced by all strains on all blood types, even by supernatant from the alpha toxin mutant (Figure 2B,D,F and Figure S2B), an observation which further suggests activity of other haemolysins in the supernatant besides alpha toxin.
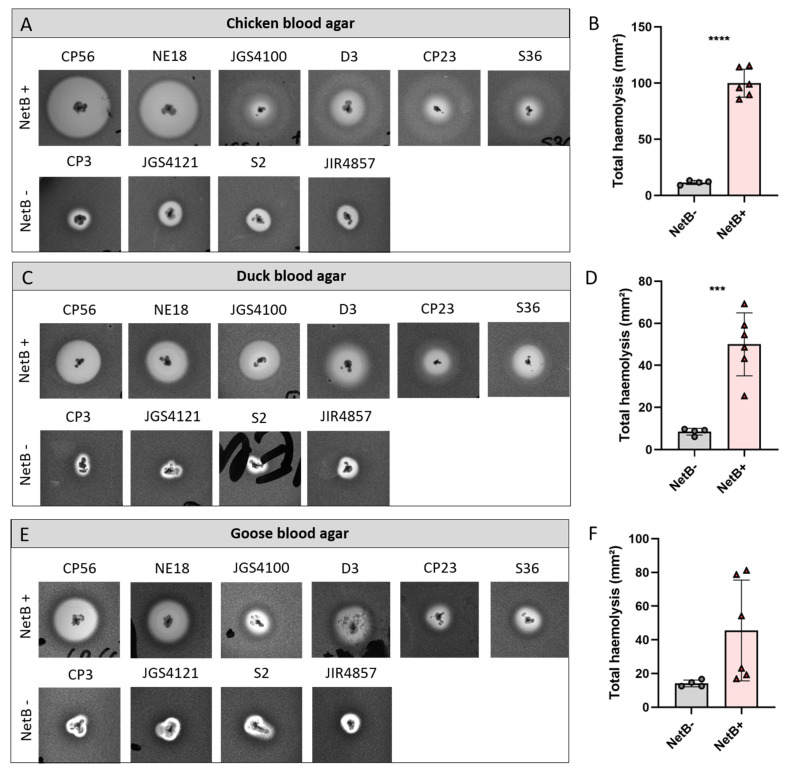
3.2. NetB-Positive Strains Show Stronger Haemolysis on Avian Blood Agar Plates as Compared to NetB-Negative Strains
To further assess the possibility to discriminate NetB-positive from NetB-negative strains based on the haemolysis pattern on avian blood agar, a collection of six NetB-positive and four NetB negative strains was grown on Columbia agar plates supplemented with either chicken, duck or goose blood. Given the above-mentioned difficulty to differentiate the inner and outer haemolysis zone, only the largest haemolysis zone from each strain was measured (Figure 3). For both chicken and duck blood, a significant size difference of the lysis zones between the NetB-positive and NetB-negative strains was observed (chicken blood agar: p < 0.0001, Figure 3A,B; duck blood agar: p = 0.0006, Figure 3C,D). However, on chicken blood agar, a clear variation in haemolysis induced by the NetB-positive strains was observed. The C. perfringens strains CP56 and NE18 (both harbouring the consensus netB gene) induced a pronounced partial outer haemolysis zone, whereas for the NetB-positive strains JGS4100, D3, CP23 and S36 (all harbouring the G502A variant netB sequence), only a weak outer haemolysis zone was observed (Figure 3A). This variability in haemolytic pattern induced by the NetB-positive strains was similar, but less pronounced on duck or goose blood agar (Figure 3C,E). Additionally, on goose blood agar, a large variation in the size of the outer lysis zones caused by NetB-positive strains was observed, which could not be differentiated from the NetB-negative strains (p = 0.074, Figure 3E,F).
Figure 3.
Haemolysis produced by six NetB-positive (CP56, NE18, JGS4100, D3, CP23 and S36) and four NetB-negative C. perfringens strains (CP3, JGS4121, S2 and JIR4857) on Columbia agar supplemented with 5% chicken blood (A,B), duck blood (C,D) or goose blood (E,F). The graph shows the total haemolysis induced by each strain (B,D,F). Grey dots represent a NetB-negative strain, red triangles represent a NetB-positive strain. *** p < 0.001; **** p < 0.0001.
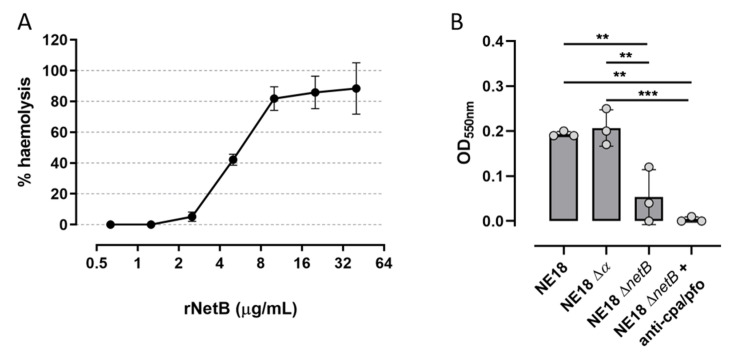
3.3. Assessing the Haemolytic Activity of NetB in C. perfringens Supernatants and rNetB against Chicken RBCs
Based on the results from the avian blood agar experiments, chicken blood was selected to further develop a 96-well plate-based haemolysis assay. The haemolytic activity of NetB towards chicken erythrocytes was confirmed by incubating the chicken RBCs with a doubling dilution series of rNetB (Figure 4A). Haemolysis was observed as an increase in absorbance due to the release of haemoglobin from the RBCs. At the highest concentration (40 µg/mL), the rNetB was able to induce 88.39% ± 16.63% haemolysis of the chicken RBCs, which remained stable up to the concentration of 10 µg/mL rNetB (corresponding to 81.88% ± 7.71% haemolysis). When 5 µg/mL rNetB was incubated with the chicken RBCs, only 42.12% ± 3.58% haemolysis was observed, whereas from the dilution of 1.25 µg/mL rNetB downwards no haemolysis was induced (Figure 4A). Since the goal was to develop an assay where the NetB activity in C. perfringens supernatants could be assessed and compared, the haemolytic activity present in the culture supernatants of the NetB-positive C. perfringens strain (NE18), as well as its NetB mutant (NE18 ΔnetB) and its alpha toxin mutant (NE18 Δα), was assessed. No significant difference could be observed between NE18 WT and NE18 Δα (p = 0.969), an indication that the haemolysis caused by the alpha toxin mutant is comparable with the haemolysis induced by the wild-type strain (Figure 4B). The NetB mutant induced significantly less haemolysis compared to the alpha toxin mutant (p = 0.004) and the NE18 wild-type strain (p = 0.007), suggesting that most haemolysis is indeed caused by NetB. Furthermore, when the alpha toxin and perfringolysin O activity of the NE18 NetB mutant strain was blocked by pre-incubating the culture supernatants with an excess of anti-CPA/PFO, no haemolysis could be observed (Figure 4B).
Figure 4.
(A) Chicken RBC haemolysis induced by a two-fold dilution series of rNetB (starting from 40 µg/mL). The % haemolysis was calculated relative to the negative control (chicken RBCs in HBSS, 0% haemolysis) and positive control (chicken RBCs diluted in dH2O, 100% haemolysis) and plotted on a log2 scale against chicken RBCs. (B) Comparison of haemolysis induced by the wild-type strain NE18, its alpha toxin mutant (NE18 ∆α), the NetB mutant (NE18 ∆netB) or NE18 ∆netB pre-incubated with anti-alpha toxin and perfringolysin antiserum (anti-cpa/pfo). Haemolysis is observed by an increase in OD due to the release of haemoglobin from the RBCs. ** p < 0.01; *** p < 0.001.
3.4. Inhibition of Non-NetB Haemolysins Is Needed to Quantify NetB Activity in C. perfringens Culture Supernatants
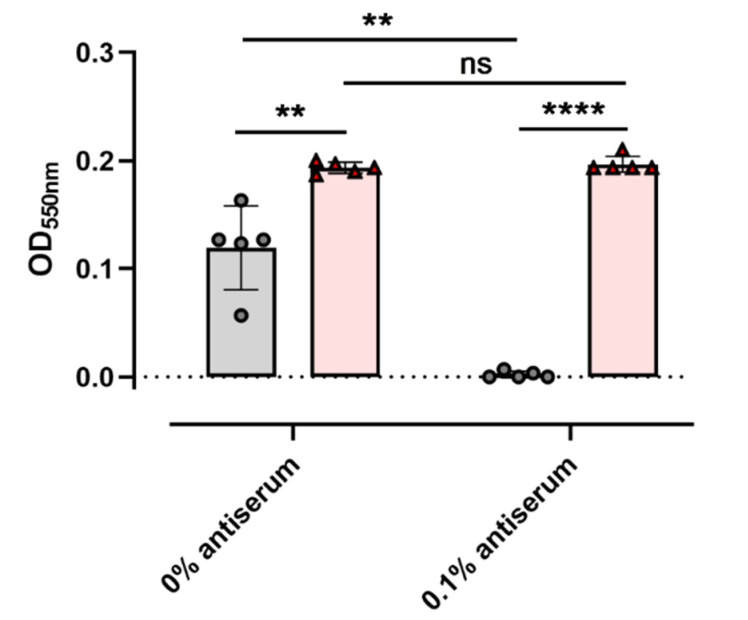
To investigate the possibility to discriminate NetB-positive from NetB-negative C. perfringens strains based on their haemolytic activity towards chicken RBCs in a 96-well plate-based format, the haemolytic activity present in the culture supernatants of the strains was tested (Figure 5). Culture supernatants from the NetB-positive strains showed a significantly higher haemolytic activity towards chicken RBCs as compared to the NetB-negative strains (p = 0.0028). However, quite some variation in haemolysis induced by the NetB-negative strains was observed, making it hard to distinguish between a NetB-positive or NetB-negative isolate solely based on its haemolytic activity towards chicken RBCs. This clearly shows the need to block other haemolytic toxins present in the culture supernatants.
Figure 5.
Haemolysis induced by a selection of NetB-positive (red) and NetB-negative (grey) strains, incubated with and without antiserum directed towards C. perfringens alpha toxin and perfringolysin O. Haemolysis is observed by an increase in optical density due to the release of haemoglobin from the red blood cells. Individual dots represent individual strains. ** p < 0.01, **** p < 0.0001, ns = not significant (p > 0.05).
The optimal concentration of the anti-CPA/PFO antiserum was determined by pre-incubating the C. perfringens culture supernatants with a dilution series of the antiserum prior to performing the haemolysis assay (data not shown). At an antiserum concentration of 0.1%, the haemolytic activity in the culture supernatants from all tested NetB-negative strains was completely blocked (Figure 5, grey), and the difference between the NetB positives and NetB negatives became even more significant (p < 0.0001). While pre-incubation of C. perfringens culture supernatants with anti-CPA/PFO antiserum significantly reduced the haemolysis caused by the NetB-negative strains (p = 0.0022), the antiserum had no effect on the haemolytic activity of the NetB-positive strains (p = 0.4601). Nevertheless, these results clearly show that alpha toxin and perfringolysin O have substantial haemolytic activity towards chicken erythrocytes, which might lead to false results when the goal is to only assess NetB activity. To ensure complete inhibition of CPA/PFO-induced haemolysis, a final serum concentration of 0.5% was therefore included in the final assay protocol (final protocol described in detail in Supplementary File 3).
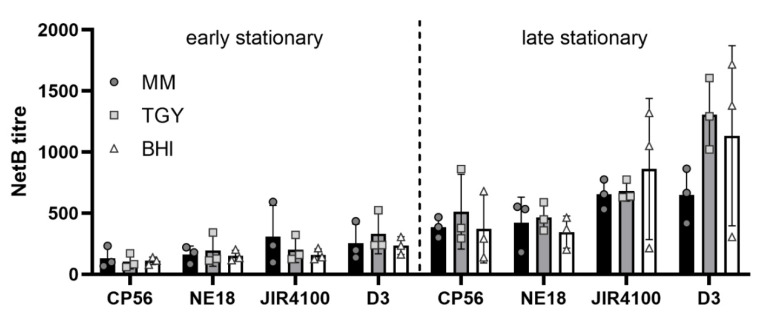
3.5. Maximal NetB Toxin Activity Was Observed in the Late Stationary Phase
As the bacterial growth medium can have an effect on both the growth and toxin production of C. perfringens, the behaviour of four NetB-positive strains (CP56 and NE18 producing the consensus NetB protein; JGS4100 and D3 producing the A168T variant NetB protein) was assessed in three commonly used growth media (MM, TGY and BHI) (Appendix A). Maximal NetB toxin activity was observed in the late stationary phase (overnight culture). The growth medium did not have a significant effect on NetB activity. However, when using BHI medium, a high variability in NetB activity between the different replicates was observed, indicating that this culture medium is less suited to determine the NetB activity (Figure A1). TGY medium was the most sensitive to observe differences in NetB activity between the different C. perfringens strains. Therefore, further experiments were performed using late stationary cultures (overnight cultures) grown in TGY.
3.6. The In Vitro NetB Production Correlates with C. perfringens Virulence
As NetB is essential in the pathogenesis of avian necrotic enteritis, the in vitro NetB production of five C. perfringens strains was compared to the virulence of these strains in an NE in vivo model. The virulence of each strain was previously reported as the average lesion score induced by each strain, compared to the average lesion score induced by strain NE18 in the same in vivo trial (NE18: reference strain included in all trials) [23]. The selected strains were grown in TGY medium for 24 h, after which the NetB titre in the culture supernatants was determined. To obtain a more complete overview of the toxin production by the strains, the in vitro alpha toxin activity was also measured (Table 2).
Table 2.
Overview of the NetB and Alpha toxin production of 5 C. perfringens strains with different virulence. All strains were grown in TGY medium for 24 h, after which both the NetB titre (supernatant dilution that induces 50% of haemolysis) and alpha toxin activity (CPA in units/mL) in the supernatants were determined. The virulence of the strains is expressed as % disease induction in an NE in vivo model, relative to the virulence of strain NE18 [23]. Data are expressed as mean ± standard deviation of the mean.
| Strain ID | NetB Titre | CPA U/mL | % Disease Induction |
|---|---|---|---|
| JIR12058 | 588 ± 54 | 0.048 ± 0.03 | 154 |
| NE18 | 466 ± 115 | 0.102 ± 0.04 | 100 |
| CP56 | 337 ± 60 | 0.119 ± 0.05 | 80 |
| JIR4866 | 436 ± 103 | 0.118 ± 0.03 | 75 |
| JIR4860 | 200 ± 57 | 0.646 ± 0.10 | 47 |
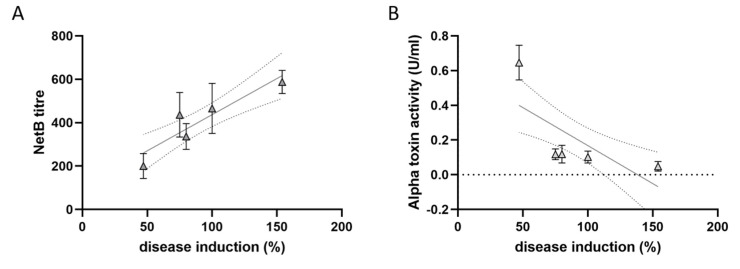
The virulence of the C. perfringens strains was positively correlated with the in vitro NetB titre (Pearson r = 0.92; p = 0.028) but showed a trend towards a negative correlation with the in vitro alpha toxin production (Spearman r = −0.90; p = 0.083) (Figure 6). However, this inverse correlation between the virulence of the strains and in vitro alpha toxin production is mainly due to the high alpha toxin levels of a single, low-virulence strain (JIR4860).
Figure 6.
Correlation between the in vitro NetB (A) or alpha toxin (B) production and the virulence of the C. perfringens strains in an NE in vivo model. All strains were grown in TGY medium for 24 h, after which both the NetB titre (supernatant dilution that induces 50% of haemolysis) and alpha toxin activity in the supernatant was determined. The virulence of the strains was previously assessed by Keyburn et al. and is expressed as % disease induction in the NE in vivo model, relative to the virulence of strain NE18 [23]. Each triangle represents the mean ± standard deviation of triplicate experiments. The linear regression line, together with its 95% confidence interval, are plotted in grey.
4. Discussion
Necrotic enteritis is an important enteric disease in poultry, causing significant economic losses to the livestock industry worldwide. C. perfringens NetB toxin is a major virulence factor in avian necrotic enteritis, and as a consequence, many studies directed towards understanding disease pathogenesis or the development of control strategies are focused on NetB. Identification of NetB-positive strains is routinely performed by amplification of the netB gene using PCR. However, there is no absolute correlation between the presence of the netB gene and the ability to produce NetB [15,24]. Furthermore, detection of the netB gene does not provide information about the NetB activity of the respective strains. In this study, we showed that NetB-positive strains can phenotypically be discriminated from NetB-negative strains based on the induced haemolysis of either chicken blood or duck blood agar plates. Indeed, on chicken or duck blood agar, NetB-positive strains show a large double haemolysis zone, which is in contrast to NetB-negative isolates, which induce a smaller, single haemolysis zone. However, on chicken blood agar, the NetB-positive strains could cause two different types of haemolysis. The C. perfringens strains NE18 and CP56 induced an easy to observe, pronounced partial outer haemolysis zone, whereas the four other tested strains induced a double haemolysis zone, where the outer haemolysis zone was remarkably weaker as compared to the outer haemolysis induced by NE18 or CP56. Remarkably, the strains inducing the stronger outer haemolysis (NE18 and CP56) are known to harbour the consensus netB gene, whereas the four strains showing weak outer haemolysis produce an alternative NetB toxin showing a single amino acid (A168T) difference. Previous research has shown that culture supernatants from different C. perfringens strains producing the A168T NetB variant were equally cytotoxic towards LMH cells as culture supernatants from strain NE18 [23]. However, this LMH cytotoxicity assay has a limited dynamic range and was shown to be less suited to screen the biological activity of NetB mutants [33]. Moreover, previous research from Savva et al. clearly showed that some synthetic AA substitutions (e.g., Y78A, Y187A, H188A) had no effect on the NetB-induced cytotoxicity towards LMH cells, while a significant reduction in haemolysis towards human RBCs was observed [33]. Although the naturally occurring A168T NetB variant is widespread (ranging from 26% (6/23) to 78% (21/27) of tested NetB-positive strains [23,24]), no research on the haemolytic potential of the A168T NetB variant is currently available. However, this AA variation is located in the pre-stem region of the NetB toxin, which is inserted in the lipid bilayer during pore formation, suggesting a possible role during pore formation and subsequent haemolysis [22,33]. Whether or not the NetB A168T variant is responsible for the weaker outer haemolysis zones induced by the NetB-positive strains in our study remains to be elucidated using recombinant protein. Furthermore, it is unclear why this difference in haemolytic profile observed for the strains grown on the chicken blood agar was not linked to a difference in haemolysis induced by the culture supernatants of the same strains towards chicken RBCs in solution. NetB production is positively regulated by the VirS/VirR two-component system [34]. However, it could be that other factors produced by C. perfringens might influence the expression of the netB gene or NetB activity itself, such as “VirR regulated RNA” (VR-RNA), an RNA molecule that has a regulatory function in Clostridia [34]. Therefore, the differences in NetB activity among the pathogenic strains might be the result of a combination of differences in gene expression and other influencing factors.
In this study, we present a rapid and easy 96-well plate-based assay to screen the NetB activity in C. perfringens culture supernatants. The assay is based on the high susceptibility of chicken RBCs towards the haemolytic activity of NetB toxin [22,33]. Although this haemolysis assay has previously been used to characterise the activity of various purified NetB toxin variants, our results clearly indicate that the haemolysis of chicken RBCs induced by C. perfringens culture supernatants is not specific for NetB toxin, and toxin-neutralising antisera are needed to block other haemolytic toxins produced by the C. perfringens strains. As TGY medium was the most sensitive to observe variations in NetB toxin production and the activity of different C. perfringens strains, we propose TGY as a suitable bacterial growth medium to assess NetB toxin production and activity.
Various factors can affect the in vitro toxin production and, therefore, in vitro NetB production and activity cannot be directly linked to in vivo NetB production and subsequent pathogenicity. Therefore, in this study, we used the newly developed NetB assay to screen a selection of NetB-positive strains for their in vitro NetB production and linked this to the previously published pathogenicity of the strains in an NE in vivo model. The in vitro NetB activity was positively correlated with the virulence of the C. perfringens strains, further underscoring the importance of the NetB toxin in NE pathogenesis. This is in accordance with the previously reported observation that NetB-positive strains from NE flocks were able to produce NetB in vitro, whereas for the majority of the NetB-positive strains isolated from healthy broilers, no in vitro NetB production was observed using Western blot [24]. However, as only a limited number of strains with known virulence were available for this study, further research should focus on comparing a larger collection of C. perfringens strains to confirm these results. No link between the in vitro alpha toxin production and in vivo pathogenicity of the strains was observed, thereby confirming the results from previous studies comparing C. perfringens strains isolated from diseased and healthy poultry flocks [27,35,36].
5. Conclusions
The aim of this study was to develop a fast and easy method by which toxin production can be assessed by the measurement of haemolysis induced by NetB in supernatants. This protocol can be very helpful when it comes to further research about different compounds that might inhibit its activity, but also to evaluate which C. perfringens strains produce more active NetB.
Acknowledgments
The authors thank Jackie Cheung (Monash University, Australia) for sharing the initial protocol to determine the C. perfringens perfringolysin O titre using a horse haemolysis assay.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/microorganisms9081708/s1, Figure S1: Growth curves of four NetB-positive and four NetB-negative C. perfringens strains in MM, TGY and BHI medium, Figure S2: Haemolysis induced by the NetB-positive C. perfringens strain NE18, its alpha toxin mutant (NE18 ∆α) or its NetB toxin mutant (NE18 ∆netB) on Columbia agar supplemented with 5% avian blood, File S1: Development of polyclonal antiserum towards non-NetB C. perfringens proteins: Rabbit immunisation protocol, File S2: Determining the optimal antiserum concentration to block non-NetB C. perfringens haemolysins, File S3: NetB doubling dilution assay (haemolysis of chicken red blood cells).
Appendix A
Effect of Culture Medium and Growth Phase on C. perfringens NetB Production
As the bacterial growth medium can have an effect on both the growth and toxin production of C. perfringens, the behaviour of four NetB-positive strains (CP56 and NE18 producing the consensus NetB protein; JGS4100 and D3 producing the A168T variant NetB protein) was assessed in three commonly used growth media (MM, TGY and BHI). For all tested C. perfringens strains, the culture medium did not influence the growth curve, and the end of the logarithmic growth phase was reached after 4–5 h of growth (Figure S1).
To assess the effect of the different growth media on the NetB toxin production, the NetB titre was determined after 7 h (early stationary phase) and 24 h (late stationary phase) growth in the different growth media (Figure A1). At both the 7 h and 24 h timepoint, no effect of the culture media on the NetB titre could be observed. After 7 h growth, all strains showed a similar NetB titre (Figure A1). However, after 24 h incubation in TGY medium, the NetB titre of strain D3 tended to be higher than the NetB titres of strain CP56 (p = 0.099) and NE18 (p = 0.070) (Figure A1, late stationary). When further comparing the 7 h and 24 h timepoints, a significant increase in NetB titre could be observed for all media (MM: p = 0.0006; TGY: p < 0.0001; BHI: p = 0.0102). In both MM and BHI medium, this overall increase in NetB titre over time could be attributed to strain D3 (MM: p = 0.0357; BHI: p = 0.0743), whereas in TGY medium, this increase in NetB titre reached significance for three out of four tested strains (CP56: p = 0.0227; NE18: p = 0.1421; JIR4100: p = 0.0092; D3: p < 0.0001). In contrast to the increase in NetB titre, the bacterial growth did not change between the two timepoints, indicating that bacterial growth stopped but NetB production continued (Figure S1).
Figure A1.
NetB titres after 7 h (early stationary phase) and 24 h (late stationary phase) growth of four NetB-positive strains in different media. The graph shows the NetB titre induced by CP56 and NE18 (both producing the consensus NetB protein), and JIR4100 or D3 (producing the A168T variant NetB protein) grown in either minimal medium (MM, black), tryptose glucose yeast extract medium (TGY, grey) or brain heart infusion broth (BHI, white). The NetB titre of each strain represents the supernatant dilution that induces 50% haemolysis.
Author Contributions
Conceptualisation, R.D., F.V.I. and E.G.; methodology, E.G.; validation, M.H. and E.G.; formal analysis, M.H. and E.G.; investigation, M.H. and E.G.; resources, R.D. and F.V.I.; writing—original draft preparation, M.H., R.D., F.V.I. and E.G.; visualisation, M.H and E.G.; supervision, R.D., F.V.I. and E.G.; funding acquisition, F.V.I. and E.G. All authors have read and agreed to the published version of the manuscript.
Funding
M.H. was funded by the Special Research Fund (BOF, Ghent University, Ghent, Belgium) (grant number BOF24J2015000301). E.G. was funded by the Research Foundation Flanders (FWO) (grant number 12W8919N).
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article and its Supplementary Materials.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kiu R., Brown J., Bedwell H., Leclaire C., Caim S., Pickard D., Dougan G., Dixon R.A., Hall L.J. Genomic analysis on broiler-associated Clostridium perfringens strains and exploratory caecal microbiome investigation reveals key factors linked to poultry necrotic enteritis. Anim. Microbiome. 2019;11:12. doi: 10.1186/s42523-019-0015-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rood J.I., Adams V., Lacey J., Lyras D., McClane B.A., Melville S.B., Moore R.J., Popoff M.R., Sarker M.R., Songer J.G., et al. Expansion of the Clostridium perfringens toxin-based typing scheme. Anaerobe. 2018;53:5–10. doi: 10.1016/j.anaerobe.2018.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parreira V.R., Costa M., Eikmeyer F., Blom J., Prescott J.F. Sequence of Two Plasmids from Clostridium perfringens Chicken Necrotic Enteritis Isolates and Comparison with C. perfringens Conjugative Plasmids. PLoS ONE. 2012;7:e49753. doi: 10.1371/journal.pone.0049753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDevitt R.M., Brooker J.D., Acamovic T., Sparks N.H.C. Necrotic enteritis; a continuing challenge for the poultry industry. Worlds Poult. Sci. J. 2006;62:221–247. doi: 10.1079/WPS200593. [DOI] [Google Scholar]
- 5.Timbermont L., Haesebrouck F., Ducatelle R., van Immerseel F. Necrotic enteritis in broilers: An updated review on the pathogenesis. Avian Pathol. 2011;40:341–347. doi: 10.1080/03079457.2011.590967. [DOI] [PubMed] [Google Scholar]
- 6.To H., Suzuki T., Kawahara F., Uetsuka K., Nagai S., Nunoya T. Experimental induction of necrotic enteritis in chickens by a netB-positive Japanese isolate of Clostridium perfringens. J. Vet. Med. Sci. 2017;79:350–358. doi: 10.1292/jvms.16-0500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.M’Sadeq S.A., Wu S., Swick R.A., Choct M. Towards the control of necrotic enteritis in broiler chickens with in-feed antibiotics phasing-out worldwide. Anim. Nutr. 2015;1:1–11. doi: 10.1016/j.aninu.2015.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adhikari P., Kiess A., Adhikari R., Jha R. An approach to alternative strategies to control avian coccidiosis and necrotic enteritis. J. Appl. Poult. Res. 2020;29:515–534. doi: 10.1016/j.japr.2019.11.005. [DOI] [Google Scholar]
- 9.Gantois I., Ducatelle R., Pasmans F., Haesebrouck F., Hautefort I., Thompson A., Hinton J.C., van Immerseel F. Butyrate Specifically Down-Regulates Salmonella Pathogenicity Island 1 Gene Expression. Appl. Environ. Microbiol. 2006;72:946. doi: 10.1128/AEM.72.1.946-949.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Njoroge J.W., Nguyen Y., Curtis M.M., Moreira C.G., Sperandio V. Virulence meets metabolism: Cra and KdpE gene regulation in enterohemorrhagic Escherichia coli. mBio. 2012;3:5. doi: 10.1128/mBio.00280-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dorman C.J., McKenna S., Beloin C. Regulation of virulence gene expression in Shigella flexneri, a facultative intracellular pathogen. Int. J. Med. Microbiol. 2001;291:89–96. doi: 10.1078/1438-4221-00105. [DOI] [PubMed] [Google Scholar]
- 12.Guiney D.G. Regulation of bacterial virulence gene expression by the host environment. J. Clin. Investig. 1997;99:565. doi: 10.1172/JCI119196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keyburn A.L., Boyce J.D., Vaz P., Bannam T.L., Ford M.E., Parker D., di Rubbo A., Rood J.I., Moore R.J. NetB, a new toxin that is associated with avian necrotic enteritis caused by Clostridium perfringens. PLoS Pathog. 2008;4:e26. doi: 10.1371/journal.ppat.0040026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lanckriet A., Timbermont L., Eeckhaut V., Haesebrouck F., Ducatelle R., van Immerseel F. Variable protection after vaccination of broiler chickens against necrotic enteritis using supernatants of different Clostridium perfringens strains. Vaccine. 2010;28:5920–5923. doi: 10.1016/j.vaccine.2010.06.035. [DOI] [PubMed] [Google Scholar]
- 15.Lee K.-W., Kim W.H., Li C., Lillehoj H.S. Detection of Necrotic Enteritis B–like Toxin Secreted by Clostridium perfringens Using Capture Enzyme-Linked Immunosorbent Assay. Avian Dis. 2020;64:490–495. doi: 10.1637/0005-2086-64.4.490. [DOI] [PubMed] [Google Scholar]
- 16.Lee K.W., Lillehoj H.S., Kim W., Park I., Li C., Lu M., Hofacre C.L. Research Note: First report on the detection of necrotic enteritis (NE) B-like toxin in biological samples from NE-afflicted chickens using capture enzyme-linked immunosorbent assay. Poult. Sci. 2021;100:101190. doi: 10.1016/j.psj.2021.101190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu S., Yang X., Zhang H., Zhang J., Zhou Y., Wang T., Hu N., Deng X., Bai X., Wang J. Amentoflavone Attenuates Clostridium perfringens Gas Gangrene by Targeting Alpha-Toxin and Perfringolysin O. Front. Pharmacol. 2020;11:179. doi: 10.3389/fphar.2020.00179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Awad M.M., Rood J.I. Perfringolysin O Expression in Clostridium perfringens Is Independent of the Upstream pfoR Gene. J. Bacteriol. 2002;184:2034. doi: 10.1128/JB.184.7.2034-2038.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheung J.K., Keyburn A.L., Carter G.P., Lanckriet A.L., van Immerseel F., Moore R.J., Rood J.I. The VirSR two-component signal transduction system regulates NetB toxin production in Clostridium perfringens. Infect. Immun. 2010;78:3064–3072. doi: 10.1128/IAI.00123-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheung J.K., Awad M.M., McGowan S., Rood J.I. Functional Analysis of the VirSR Phosphorelay from Clostridium perfringens. PLoS ONE. 2009;4:e5849. doi: 10.1371/journal.pone.0005849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Awad M.M., Bryant A.E., Stevens D.L., Rood J.I. Virulence studies on chromosomal alpha-toxin and theta-toxin mutants constructed by allelic exchange provide genetic evidence for the essential role of alpha-toxin in Clostridium perfringens-mediated gas gangrene. Mol. Microbiol. 1995;15:191–202. doi: 10.1111/j.1365-2958.1995.tb02234.x. [DOI] [PubMed] [Google Scholar]
- 22.Yan X.X., Porter C.J., Hardy S.P., Steer D., Smith A.I., Quinsey N.S., Hughes V., Cheung J.K., Keyburn A.L., Kaldhusdal M., et al. Structural and functional analysis of the pore-forming toxin NetB from Clostridium perfringens. mBio. 2013;4:e00019-13. doi: 10.1128/mBio.00019-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keyburn A.L., Yan X.X., Bannam T.L., van Immerseel F., Rood J.I., Moore R.J. Association between avian necrotic enteritis and Clostridium perfringens strains expressing NetB toxin. Vet. Res. 2010;41:21. doi: 10.1051/vetres/2009069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abildgaard L., Sondergaard T.E., Engberg R.M., Schramm A., Højberg O. In vitro production of necrotic enteritis toxin B, NetB, by netB-positive and netB-negative Clostridium perfringens originating from healthy and diseased broiler chickens. Vet. Microbiol. 2010;144:231–235. doi: 10.1016/j.vetmic.2009.12.036. [DOI] [PubMed] [Google Scholar]
- 25.Keyburn A.L., Sheedy S.A., Ford M.E., Williamson M.M., Awad M.M., Rood J.I., Moore R.J. Alpha-toxin of Clostridium perfringens is not an essential virulence factor in necrotic enteritis in chickens. Infect. Immun. 2006;74:6496–6500. doi: 10.1128/IAI.00806-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Damme L., Cox N., Callens C., Haesebrouck F., Dargatz M., Ducatelle R., van Immerseel F., Goossens E.C. perfringens challenge reduces matrix metalloproteinase activity in the jejunal mucosa of Eimeria-infected broiler chickens. Vet. Res. 2020;51:100. doi: 10.1186/s13567-020-00825-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gholamiandekhordi A.R., Ducatelle R., Heyndrickx M., Haesebrouck F., van Immerseel F. Molecular and phenotypical characterization of Clostridium perfringens isolates from poultry flocks with different disease status. Vet. Microbiol. 2006;113:143–152. doi: 10.1016/j.vetmic.2005.10.023. [DOI] [PubMed] [Google Scholar]
- 28.van Damme L., Cox N., Callens C., Dargatz M., Flügel M., Hark S., Thiemann F., Pelzer S., Haesebrouck F., Ducatelle R., et al. Protein Truncating Variants of colA in Clostridium perfringens Type G Strains. Front. Cell. Infect. Microbiol. 2021;11:348. doi: 10.3389/fcimb.2021.645248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goossens E., Verherstraeten S., Valgaeren B.R., Pardon B., Timbermont L., Schauvliege S., Rodrigo-Mocholi D., Haesebrouck F., Ducatelle R., Deprez P.R., et al. Toxin-neutralizing antibodies protect against Clostridium perfringens-induced necrosis in an intestinal loop model for bovine necrohemorrhagic enteritis. BMC Vet. Res. 2016;12:101. doi: 10.1186/s12917-016-0730-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rigby G.J. An egg-yolk agar diffusion assay for monitoring phospholipase C in cultures of Clostridium welchii. J. Appl. Bacteriol. 1981;50:11–19. doi: 10.1111/j.1365-2672.1981.tb00866.x. [DOI] [PubMed] [Google Scholar]
- 31.Goossens E., Verherstraeten S., Timbermont L., Valgaeren B.R., Pardon B., Haesebrouck F., Ducatelle R., Deprez P.R., van Immerseel F. Clostridium perfringens strains from bovine enterotoxemia cases are not superior in in vitro production of alpha toxin, perfringolysin O and proteolytic enzymes. BMC Vet. Res. 2014;10:32. doi: 10.1186/1746-6148-10-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stevens D.L., Mitten J., Henry C. Effects of α and θ Toxins from Clostridium perfringens on Human Polymorphonuclear Leukocytes. J. Infect. Dis. 1987;156:324–333. doi: 10.1093/infdis/156.2.324. [DOI] [PubMed] [Google Scholar]
- 33.Savva C.G., Fernandes da Costa S.P., Bokori-Brown M., Naylor C.E., Cole A.R., Moss D.S., Titball R.W., Basak A.K. Molecular architecture and functional analysis of NetB, a pore-forming toxin from Clostridium perfringens. J. Biol. Chem. 2013;288:3512–3522. doi: 10.1074/jbc.M112.430223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ohtani K., Shimizu T. Regulation of Toxin Production in Clostridium perfringens. Toxins. 2016;8:207. doi: 10.3390/toxins8070207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abildgaard L., Engberg R.M., Pedersen K., Schramm A., Hojberg O. Sequence variation in the α-toxin encoding plc gene of Clostridium perfringens strains isolated from diseased and healthy chickens. Vet. Microbiol. 2009;136:293–299. doi: 10.1016/j.vetmic.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 36.Timbermont L., Lanckriet A., Gholamiandehkordi A.R., Pasmans F., Martel A., Haesebrouck F., Ducatelle R., van Immerseel F. Origin of Clostridium perfringens isolates determines the ability to induce necrotic enteritis in broilers. Comp. Immunol. Microbiol. Infect Dis. 2009;32:503–512. doi: 10.1016/j.cimid.2008.07.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article and its Supplementary Materials.