Abstract
Background
COVID-19 is a lung disease, and there is medical evidence that air pollution is one of the external causes of lung diseases. Fine particulate matter is one of the air pollutants that damages pulmonary tissue. The combination of the coronavirus and fine particulate matter air pollution may exacerbate the coronavirus’ effect on human health.
Research question
This paper considers whether the long-term concentration of fine particulate matter of different sizes changes the number of detected coronavirus infections and the number of COVID-19 fatalities in Germany.
Study design
Data from 400 German counties for fine particulate air pollution from 2002 to 2020 are used to measure the long-term impact of air pollution. Kriging interpolation is applied to complement data gaps. With an ecological study, the correlation between average particulate matter air pollution and COVID-19 cases, as well as fatalities, are estimated with OLS regressions. Thereby, socioeconomic and demographic covariates are included.
Main findings
An increase in the average long-term air pollution of 1 μg/m3 particulate matter PM2.5 is correlated with 199.46 (SD = 29.66) more COVID-19 cases per 100,000 inhabitants in Germany. For PM10 the respective increase is 52.38 (SD = 12.99) more cases per 100,000 inhabitants. The number of COVID-19 deaths were also positively correlated with PM2.5 and PM10 (6.18, SD = 1.44, respectively 2.11, SD = 0.71, additional COVID-19 deaths per 100,000 inhabitants).
Conclusion
Long-term fine particulate air pollution is suspected as causing higher numbers of COVID-19 cases. Higher long-term air pollution may even increase COVID-19 death rates. We find that the results of the correlation analysis without controls are retained in a regression analysis with controls for relevant confounding factors. Nevertheless, additional epidemiological investigations are required to test the causality of particulate matter air pollution for COVID-19 cases and the severity.
Keywords: COVID-19 cases, COVID-19 mortality, Particulate matter PM10 and PM2.5, Long-term air pollution, County-level data Germany
1. Introduction
Environmental effects, in particular air pollution, are well-known for their health-relevance (Cohen et al., 2017). For this reason, statutory thresholds and permissible limits for pollutants are defined. The World Health Organization (WHO, 2006), as well as the European Union (European Commission n. y.) recommend or even prescribe the respective thresholds. Among others, air pollution with fine particulate matter is considered dangerous to health. In this respect, is known that long-term exposure to air pollution, especially to particulate matter with a diameter of 10 μm and less, PM10, as well as particulate matter with a diameter of less than 2.5 μm, PM2.5, may cause inflammation and many other changes in the body that are linked to a large number of medical conditions, especially lung diseases (Ciencewicki and Jaspers, 2007; Anderson et al., 2012; WHO, 2016; Cohen et al., 2017; Stockfelt et al., 2017; Guo et al., 2018; Guo et al., 2019; Lelieveld et al., 2019). Moreover, air pollution has evidentely increased the risk of dying by SARS (severe acute respiratory syndrome) in China, for short-term as well as long-term exposure to particulate matter, sulphur dioxide, nitrogen dioxide, carbon monoxide and ozone (Cui et al., 2003).
The new coronavirus SARS-CoV-2 is a respiratory and lung disease that can have severe and deadly consequences. This supports the assumption that the disease activated by SARS-CoV-2, COVID-19, might be connected in some way or other with fine particulate matter exposure (Woodby et al., 2020; Zhu et al., 2021; Bourdrel et al., 2021). In particular, long-term exposure to this air pollution seems to be the cause of the negative health effects.
There are two different mechanisms that may create a causal relationship between fine particulate air pollution and SARS-CoV-2 infections. The first is that particulate matter might carry the airborne virus, transmitting it into the human respiratory system (Copat et al., 2020; Martelletti and Martelletti, 2020; Di Girolamo, 2021; Nor et al., 2021). The second is that fine particulate matter could increase the severity of the Covid-19 disease by delaying or complicating recovering (Domingo and Rovira, 2020; Leifer et al., 2021). However, it is difficult to distinguish between these two mechanisms, due to a lack of individual-related longitudinal data that are not available in the midst of a pandemic (Villeneuve and Goldberg, 2020). In a review paper, Comunian et al. (2020) analyzed the role played by ACE2 (angiotensin-converting enzyme 2) in the inflammation of lung cells and the intrusion of the coronavirus into these cells in connection with daily PM-concentrations, especially in Italian cities. According to Comunian et al. (2020), PM may therefore play a role in the transportation of the virus in the environment and thus in susceptibility to the virus, as well as the severity of the COVID-19 disease.
In this paper, we contribute to the literature on the connection between long-term exposure to fine matter particulate air pollution and COVID-19, by studying this relationship empirically with county-level data from Germany. In this context, fine matter air pollution is measured in terms of long-term exposure to PM10 and PM2.5. In particular, the effect of long-term exposure to fine particulate matter on the number of COVID-19 infections and the number of COVID-19 fatalities per 100,000 inhabitants is investigated. A short-term analysis of these effects for Germany was presented by Isphording and Pestel (2021). In another study with German data, Huang and Brown (2021) provided evidence of an increasing COVID-19 incidence due to long-term air pollution with nitrogen dioxide (NO2). To the best of our knowledge, this present study is the first on the suspected long-term effect of PM on COVID-19 in Germany.
Although the COVID-19 pandemic is a recent phenomenon, research related to this issue consists of a large number of papers that investigate the relation between COVID-19 and air pollution, and especially particulate matter pollution. The ecological studies concerning this impact are available for cities, regions, countries and groups of countries, as well as the world as a whole. However, a number of these studies appeared early in the pandemic when the number of observations was quite small. Papers on the relevance of environmental factors, including air pollution, for COVID-19 up to May 2020, were critically reviewed by Shakil et al. (2020) and up to the end of September 2020 by Ali and Islam (2020). Ali et al. (2021) reviewed papers on air pollution and COVID-19 infections and mortality from January to December 2020. An even more comprehensive review of papers on environmental aspects of COVID-19 was undertaken by Sharma et al. (2021). The conclusion of these reviews presented ecological and observational evidence of increasing effects of short-term and long-term air pollution, in particular PM2.5, PM10, and NO2, on COVID-19 infections and fatalities.
Pozzer et al. (2020) studied air pollution by means of satellite data worldwide as a cofactor of COVID-19 mortality. The mortality data were obtained from epidemiologic data relating to China and the USA. In addition, they calculated the anthropogenic share of pollution with a model from atmospheric chemistry. According to this paper, about 15% of COVID-19 mortality globally may be attributed to air pollution in general. However, the range of the 95% confidence interval was large (7–33%) and the epidemiologic data were from the early wave of the disease. These results were qualitatively confirmed by Barnett-Itzhaki and Levi (2021) in a linear regression study on the impact of the PM2.5 concentration on COVID-19 morbidity and mortality in 36 OECD countries. With Pearson correlation analysis, Lembo et al. (2021) found, in 33 European countries, positive connections between diverse air pollutants and the number of infections with and deaths from the disease. Coccia (2021) concluded from a global analysis with more than 160 countries that beside higher health care expenditures and GDPs, lower exposure to ultrafine particulate matter, PM2.5, was correlated with lower COVID-19 infection and death rates. In order to obtain more precise results for a country that is much smaller, but more densely populated than China and the USA, we investigate PM air pollution and COVID-19 cases and fatalities in Germany.
At the country level, ecological studies on the effects of fine and ultrafine particulate matter air pollution, PM10 and PM2.5, are available for several countries and regions. In this respect, China, Italy and the USA were studied intensely. Two Chinese studies concentrated on the epicenter of the outbreak of the pandemic, Wuhan, as well as Wuhan and Xiaogan. Yao et al. (2020a) found a positive correlation between PM10 and PM2.5 on the CFR of COVID-19 in Wuhan on a day-by-day basis. Li et al. (2020) also reported positive correlations between PM10, PM2.5, NO2 and CO, an air quality index and COVID-19 incidence in Wuhan and Xiaogan for the period January 26 to February 29, 2020. Moreover, they also included five meteorological variables (four temperature variables and one for sunshine duration), whereby only temperature had an influence. In an empirical analysis with 49 Chinese cities, Yao et al. (2020b) referred to positive correlations between both PM10 and PM2.5 and the CFR of COVID-19. According to their results, PM2.5 (PM10) increases by 10 μm/m3 enhanced the CFR by 0.24% (0.26%). Zhu et al. (2020) found, for 120 Chinese cities, positive short-term associations concerning confirmed COVID-19 cases by considering six air pollutants. An increase of 10 μm/m3 of PM2.5 (PM10) was accompanied by a 2.24% (1.76%) increase in the number of daily cases. These results show that particulate matter air pollution seemingly increased both the number of COVID-19 cases and the CFR of the disease. With generalized additive models (GAMs), controlling for confounding, Zhang et al. (2021) analyzed the short-term impact of air pollution, in particular PM10 and PM2.5, on daily new confirmed cases in 235 Chinese cities. The result was that not only the number of new daily COVID-19 cases had been positively correlated with lagged short-term air pollution, but also the velocity of coronavirus propagation. By contrast, in our investigation, data include the large second wave of COVID-19 infections in Germany, which yields a more advanced picture of the pandemic situation in Germany.
Conticini et al. (2020) clarified the medical connections between chronic respiratory diseases, including COVID-19, and air pollution. Since the provinces of Lombardy and Emilia Romagna in Northern Italy were heavily polluted areas and exhibit high COVID-19 lethality, air pollution may be a contributing factor for the latter. This was confirmed for Northern Italy by Martelletti and Martelletti (2020) for high levels of PM10 and P2.5 pollution. Moreover, Frontera et al. (2020) reported correlations between PM2.5 and NO2 concentrations and intensive-care admissions and deaths of COVID-19 patients in Italian regions. Fattorini and Regoli (2020) emphasized the importance of long-term air quality for respiratory diseases like COVID-19. With data for the last four years, they found evidence of positive correlations of high concentrations of PM10, PM2.5, NO2 and O3 on COVID-19 cases in 71 Italian provinces. Indications of particulate matter pollution as a carrier of the SARS-CoV-2 virus was found by Di Girolamo (2021) for Northern Italy using satellite data and a microphysical model. The latter was applied to model the transmission of the virus by air. Again, high levels of correlation (larger than 0.80) prevailed between the concentration of PM10 with COVID-19 cases and CFR. However, in a systematic literature review, Maleki et al. (2021) did not confirm that particulate matter pollution reinforces the transmission of SARS-CoV-2. The role of meteorological variables in the transmission of the virus is still unclear; and their potential effects were studied by Zhao et al. (2021).
Investigating the relationship between air pollution with nitrogen dioxide and COVID-19 mortality in the northern Italian regions of Veneto and Emilia-Romagna, Filippini et al. (2021) detected a positive correlation. By considering Italian cities with high daily levels of PM concentration during the months before the virus spread, Comunian et al. (2020) demonstrated a positive correlation between PM concentration and an enzyme receptor that was related to the lung inflammation process with the virus. They used satellite data for the nitrogen dioxide (NO2) concentration and applied a multivariate negative binomial regression model as, for instance, recommended by Villeneuve and Goldberg (2020) for such ecological studies. For the same pollutant, NO2, Ogen (2020) analyzed the impact on COVID-19 fatality in 66 regions from Italy, Spain, France and Germany. The results showed that 78% of the fatality cases were found in only five regions in Italy and Spain with the highest concentration levels of the pollutant and with an airflow that prevented its dispersion. In our study, we do not concentrate on specific German regions, but include data from the entire country, at the level of counties. This is the smallest administrative unit for which data are available in Germany.
Hospitalization risks among COVID-19 infected persons, in combination with individual-level health characteristics and local exposure to PM2.5 over a year, were considered in a U.S. study by Bowe et al. (2021). An increase of PM2.5 by 1.9 μg/m3 correlated with a 10% higher risk of hospitalization. In a comprehensive study with more than 3000 counties in the USA, Wu et al. (2020) investigated the connection between the long-term average PM2.5 exposure and COVID-19 deaths with county-level data. In their empirical ecological regression analysis, they included 20 potential confounding variables. According to the results, even an increase of 1 μg/m3 in the PM2.5 concentration brought about an 8% increase in the COVID-19 death rate. Also applying an ecological regression analysis with a zero-inflated negative binomial model and by controlling for spatial trends and potential confounders, Liang et al. (2020) detected a positive relationship between U.S. county-level NO2 long-term exposure and COVID-19 CFR and the mortality rate, but only a marginal effect of PM2.5 and O3 (ozone). The studies of Wu et al. (2020) and Liang et al. (2020) are not only interesting because of their results, but also because of the methods they apply. The studies employed (zero-inflated) negative binomial regression analysis and control for potential confounders with several variables. The paper of Persico and Johnson (2021) is also interesting from a methodological point of view. They applied difference-in-differences estimations based on a change in the U.S. Environmental Protection Agency (EPA) enforcement policy. The roll-back of enforcement increased pollution and this effect was used to estimate its effect on the number of COVID-19 cases and deaths. An 11.8% increase in pollution was followed by an increase of COVID-19 cases (deaths) by 53% (10.6%). Another aspect of the connection between air pollution and COVID-19 was shown for the USA by Chakraborty (2021). A multivariate regression analysis demonstrated that air pollution was positively correlated in counties with higher population proportions of socioeconomically deprived and non-Hispanic black people, as were COVID-19 cases and deaths. In a study with data from San Francisco, California, the air pollutants from wildfires were used by Meo et al. (2020) to estimate the effects of PM2.5 and carbon monoxide (CO) on daily cases and deaths, as well as cumulative cases and deaths. For PM2.5, a positive effect on daily and cumulative cases of COVID-19 and on cumulative deaths was indeed found. In contrast, a study with 1128 COVID-19 patients of the hospitals and clinics of the University of Cincinnati, USA, Mendy et al. (2021) applied logistic regression to investigate the association between PM2.5 pollution and patient hospitalization. Thereby, they used local exposure to PM2.5 and controlled for comorbidities and socioeconomic factors. As a result, only those patients who suffered from asthma or chronic obstructive pulmonary disease (COPD) yielded hospitalization probabilities that were 62% higher with 1 μg/m3 in long-term average PM2.5 exposure. This result stresses the need for individual-based studies to find clear causal evidence of the effects of air pollution in COVID-19 patients. Since Germany is much smaller than the USA, the number of counties is also much smaller. This may be an advantage over the USA regarding ecological studies at the county level, as the counties themselves are smaller, and therefore, the within-county variability is also smaller. In addition, in our investigation we control for spillover-effects that exceed the county level by state-level fixed effects.
Travaglio et al. (2020) studied the relationship between air pollution in England, and COVID-19 cases and deaths at regional and subregional levels. They found evidence of correlation between poor air quality and both cases and deaths rates of COVID-19, adjusted by population density. Especially fine particulate matter was linked to increased infectivity. Stieb et al. (2020) documented a positive relation between long-term exposure to PM2.5 and COVID-19 incidence in 111 Canadian health regions. They used negative binomial regression models and controlled for health-related and sociodemographic variables at the level of the respective regions. Their ecological approach was criticized by Villeneuve and Goldberg (2020, 2021), but justified by Stieb et al. (2021). As stated above, in contrast to studies from very large countries such as the USA, China and Canada, the smaller Germany and its counties are exploited in our study.
Marquès et al. (2021) studied air pollution effects on COVID-19 in the Tarragona province in Catalonia (Spain). They divided the province into an urban/industrial and an agricultural/rural part. Infections and mortality had been higher in the urban/industrial area than in the other part of the province, which was probably related to the respective exposure to PM10, NO2 and O3. Further ecological evidence for the association between fine particulate matter air pollution and COVID-19 was documented for Latin America and the Caribbean (Bolaño-Ortiz et al., 2020).
In a study with German county-level data, Isphording and Pestel (2021) investigated the short-term impact of air pollution due to PM10 and O3 on COVID-19 cases and deaths. In their empirical analysis, they controlled for local weather conditions, as well as for other confounding variables. They found short-term significant air quality effects on the fatality of COVID-19 patients, in particular for those older than 80. Moreover, air pollution was also correlated with the confirmed COVID-19 cases. By contrast, our study is about the long-term effects of PM air pollution on cases and fatalities related to COVID-19. Our investigation can be seen as a complement to the short-term study of Isphording and Pestel (2021).
To sum up, air pollution and particulate matter concentration in particular, evidently increased the number of COVID-19 infections, as well as the fatality rate. In a recent review of relevant papers, Becchetti et al. (2021) concluded that there was “huge”, as well as strong and robust evidence of air quality playing a role in COVID-19 outcomes. Although the short-term variation of the pollutant concentration may play a certain role, long-term exposure to the pollutants seems to be more important, particularly from a public health and public policy perspective. The short-term concentration of particulate matter depends on the weather conditions and on other rather random effects. Long-term exposure to pollutants may be much more damaging to health as they put particular stress on the human body. Therefore, the focus of this paper is on long-term exposure to particulate matter and the associated number of COVID-19 cases and mortality in Germany. It complements the short-term empirical analysis of Isphording and Pestel (2021). Since this paper is also an ecological regression study, the limitations of such studies documented above must be taken into consideration when interpreting the results.
2. Materials and methods
2.1. Data and data preparation
The analysis is based on German data at the county level. From the available site data, the so-called background concentration was chosen. Particulate matter data is available from the German Federal Environmental Agency (Umweltbundesamt, 2021). The number of counties with measured concentration values was restricted by the measuring station network organized by the states (Bundesländer). Whereas PM10 data were available for the years 2002–2020, PM2.5 concentration was measured for 2010 to 2020 only. The average concentration in micrograms per cubic meter, μg/m3, over this period was the main independent variable in the estimations below.
As dependent variables, the number of confirmed COVID-19 cases per 100,000 inhabitants and the number COVID-19 deaths per 100,000 inhabitants, both as of February 22, 2021, were used. They were also available at the county-level, provided daily by the Robert Koch Institute (RKI 2021).
As confounding variables, the distances to several locations seem worth considering. The distance in kilometers from a county to Ischgl in Austria, where one of the greatest outbreaks of the virus was observed (Felbermayr et al., 2020), defined the respective variable. In addition, there were three virus hotspots in Germany when COVID-19 broke out in 2020: the city of Hamburg in Northern Germany, the county of Starnberg in Southern Bavaria and the counties of Heinsberg in North Rhine Westphalia (Felbermayr et al., 2020). The distance in kilometers of the nearest respective county to one of these German hotspots defined the hotspot variable.
As demographic variables, the population density (RKI 2021), the proportion of people over 75 years of age (Statistische Ämter, 2021 a) and the (net) commuter flow (Statistische Ämter, 2021 a) were applied in the estimations below (see e.g. Sarmadi et al., 2021 for sociodemographic variables in ecological studies on air quality and COVID-19). The proportion of one over 75 years of age was measured as decimal values, and the population density as inhabitants per square kilometers. The net commuter flow (the number of ingoing commuters minus outgoing commuters) accounted for the transmission of the virus between homes and workplaces. Since commuter flow (cf) and population density (pd) are highly correlated, the variable commuter flow (cf) was represented in the estimations below by the residuals of the auxiliary regression: cf = constant + beta∙cf, to avoid multicollinearity.
In addition, the number of nursing home spots per 100,000 people older than 75 years (Statistische Ämter, 2021 a), long-term available income per inhabitant in 1000 Euros, based on the years 2002–2018 (Statistische Ämter, 2021 b), a dummy variable for East Germany and a dummy variable for counties bordering on the Czech Republic were included as confounding variables (for border regulations between Czechia and Saxony, see ElbeLabe, 2021).
2.2. Statistical analysis
Considering counties with particulate matter recording stations only, would yield 248 counties with PM10 long-term concentration and 109 counties with PM2.5 long-term concentration. To expand the data basis, a so-called Kriging-interpolation (see Oliver, 1990, for this method) was used to calculate concentrations for counties without particulate matter recording stations. With this method, nearby measured weighted values were used to predict values at locations with no recording station. To determine the weighting, the distance to the measured points, as well as their autocorrelations, were applied (ArcGIS, 2021). With this method, 400 counties were included in the estimations below.1
Firstly, we applied OLS regressions for both PM10 and PM2.5. Secondly, we used a fixed effect model, in which the fixed effects are the German states (Bundesländer). Finally, we calculated standardized estimation coefficients. All estimations are run with heteroscedasticity robust standard errors.
3. Results
3.1. Particulate matter concentration and COVID-19 cases
Applying the Kriging-interpolation, Fig. 1, Fig. 2 show the PM10 or PM2.5 concentration with data including interpolated values.
Fig. 1.
Concentration of PM 10 in Germany (2010–2020). Source: Umweltbundesamt (2021), own calculations.
Fig. 2.
Concentration of PM 2.5 in Germany (2010–2020). Source: Umweltbundesamt (2021), own calculations.
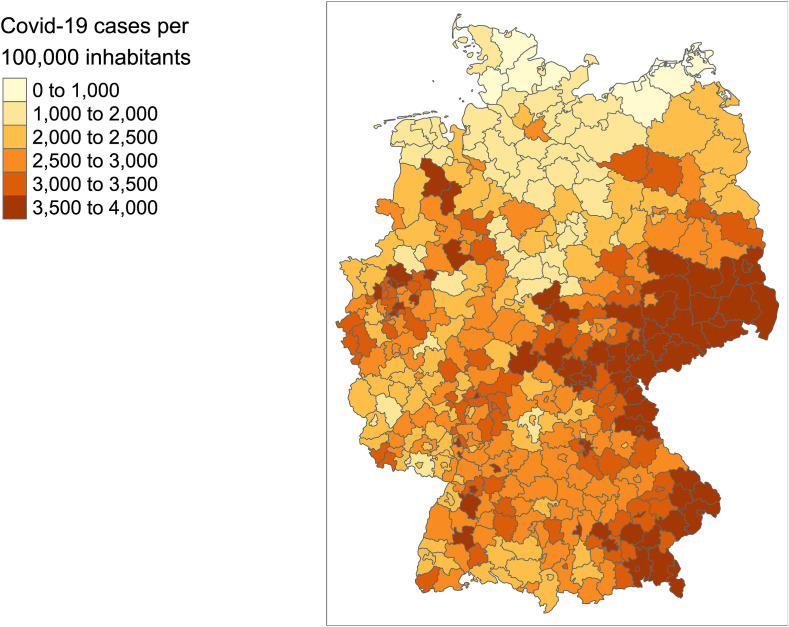
The first part of the investigation is about the potential impact of PM10 and PM2.5 concentration on the number of confirmed COVID-19 cases, shown in Fig. 3 . The results of the OLS-regressions are presented in Table 1 for PM10 and Table 2 for PM2.5. All regressions were run including the confounding variables, presented in Section 2.1. In the first column, both tables contain the regressors, and in the second column the results of the basic model without fixed effects. In the third column, the standardized coefficients of the estimation of the basic model are shown. Similarly, in the fourth column, the estimation results for the model with state (Bundesländer) fixed effects are presented. The respective standardized coefficients for this estimation are shown in the fifth column of the tables. Note that for both particulate matter concentrations, the values for the respective particulate matter concentration are Kriging-interpolated for those counties without their own PM-recording stations. The same estimations as in Table 1, Table 2, but without Kriging-Interpolation, are presented in the Appendix, Tables A1 and A2.
Fig. 3.
Confirmed COVID-19 cases per 100,000 inhabitants in Germany. Source: Data from Robert Koch Institute, RKI 2021.
Table 1.
COVID-19 cases per 100,000 inhabitants and Kriging-interpolated PM10 pollution.
| Variable | Basic Model | Standardized Coefficients | State Fixed Effects Model | Standardized Coefficients |
|---|---|---|---|---|
| Distance to Ischgl | −1.892*** (0.212) |
−0.4349298 | −1.802*** (0.465) |
−0.4141894 |
| Distance to nearest German hotspot | 1.782*** (0.534) |
0.1530381 | 1.955*** (0.806) |
0.1679186 |
| Nursing home places per 100 k inhabitants at 75 and older | 0.017 (0.022) |
0.03517896 | 0.047** (0.021) |
0.09850678 |
| Share of people >75 years | 3709.915 (3662.871) |
0.0668369 | 1551.690 (6706.982) |
0.02795485 |
| Population density | 0.275*** (0.049) |
0.2033308 | 0.167*** (0.056) |
0.1234201 |
| Commuter flow (modified) | −0.004*** (0.001) |
−0.09751138 | −0.003** (0.001) |
−0.0743129 |
| Avg. PM10, 2002 to 2020 | 52.381*** (12.999) |
0.1689943 | 36.080*** (8.643) |
0.1164028 |
| Avg. Income 2002 to 2018 | 4.772 (20.297) |
0.01166486 | 10.994 (26.832) |
0.02687409 |
| East Germany | 544.945*** (166.363) |
0.2241532 | ||
| Border with Czech Republic | 1900.803*** (262.786) |
0.3644518 | 1422.722*** (94.377) |
0.2727866 |
| Constant | 1600.346** (709.202) |
|||
| Fixed effects | No | Yes | ||
| Observations | 400 | 400 | ||
| Adj. R2 | 0.463 | 0.145 | ||
| F Statistic | 35.406*** (df = 10; 389) |
10.166*** (df = 9; 375) |
*, **, ***: p < 0.1, 0.05, 0.01, respectively. -
Source: Own calculations.
Table 2.
COVID-19 cases per 100,000 inhabitants and Kriging-interpolated PM2.5 pollution.
| Variable | Basic Model | Standardized Coefficients | State Fixed Effects Model | Standardized Coefficients |
|---|---|---|---|---|
| Distance to Ischgl | −2.019 *** (0.198) |
−0.4642156 | −1.756*** (0.386) |
−0.4035886 |
| Distance to nearest German hotspot | 1.961*** (0.503) |
0.1683947 | 2.023 *** (0.696) |
0.1737094 |
| Nursing home places per 100 k inhabitants at 75 and older | 0.023 (0.020) |
0.04905546 | 0.043** (0.017) |
0.09084879 |
| Share of people >75 years | 2410.773 (3279.293) |
0.04343189 | 1230.704 (6004.623) |
0.02217206 |
| Population density | 0.253*** (0.049) |
0.1868741 | 0.164*** (0.063) |
0.1216532 |
| Commuter flow (modified) | −0.003** (0.002) |
−0.0796416 | −0.003** (0.001) |
−0.07579911 |
| Avg. PM2.5, 2010 to 2020 | 199.455*** (29.657) |
0.275265 | 130.951** (62.119) |
0.1807226 |
| Avg. Income 2002 to 2018 | 9.131 (19.392) |
0.02232083 | 7.857 (26.119) |
0.01920682 |
| East Germany | 491.772*** (157.385) |
0.2022812 | ||
| Border with Czech Republic | 1724.710*** (227.283) |
0.3306886 | 1343.385*** (90.305) |
0.2575749 |
| Constant | 351.632 (701.009) | |||
| Fixed effects | No | Yes | ||
| Observations | 400 | 400 | ||
| Adj. R2 | 0.505 | 0.166 | ||
| F Statistic | 41.674*** (df = 10; 389) |
11.502 (df = 9; 375) |
*, **, ***: p < 0.1, 0.05, 0.01, respectively. -
Source: Own calculations.
According to Table 1, Table 2, the fine particulate matter concentration PM10 and PM2.5 were statistically highly significantly positively correlated with COVID-19 cases in German counties. The standardized coefficient of the estimations showed that the correlation is relatively strong. For instance, for both particulate matter concentrations, the standardized effect was of comparable size with the effect of population density: 0.1690 for PM10, in comparison to 0.2033 for population density, and 0.2753 for PM2.5, in comparison to 0.1869 for population density. These results were robust, as shown by the estimations with state fixed effects in Table 1, Table 2 They were also robust if a negative binomial model (not shown here) is applied. Interestingly, the population share of people older than 75 years did not correlate statistically significantly with COVID-19 cases in Germany. By contrast, the relative number of nursing home places for the respective age group was significantly and positively correlated with German COVID-19 cases, but only in the model with state fixed effects. Moreover, the positive (and statistically significant) correlations of the distance to the nearest German hotspot, population density and border region with the Czech Republic with the number of German COVID-19 cases was straightforward and depends on the characteristics of this highly contagious virus. Moreover, in the basic model, people living in East Germany – in comparison to West Germany – had a higher risk of infection by the virus.
The negative (and statistically significant) correlation of the distance to the first Austrian COVID-19 skiing hotspot Ischgl, seems to result from the fact that it was one of the first origins of COVID-19 cases in Germany. In addition, its effect on the number of cases declined over time, so that the effect became negative in the end when other regions caught up. Although the commuter flow was expected to have a positive correlation with the COVID-19 cases, the effect was statistically significantly negative, but small. The county-level income, averaged over 2002 to 2018, was not statistically significantly correlated with COVID-19 cases. These results indicate that there may be a connection between long-term exposure to fine particulate matter, PM10 and PM2.5, and the number of COVID-19 cases.
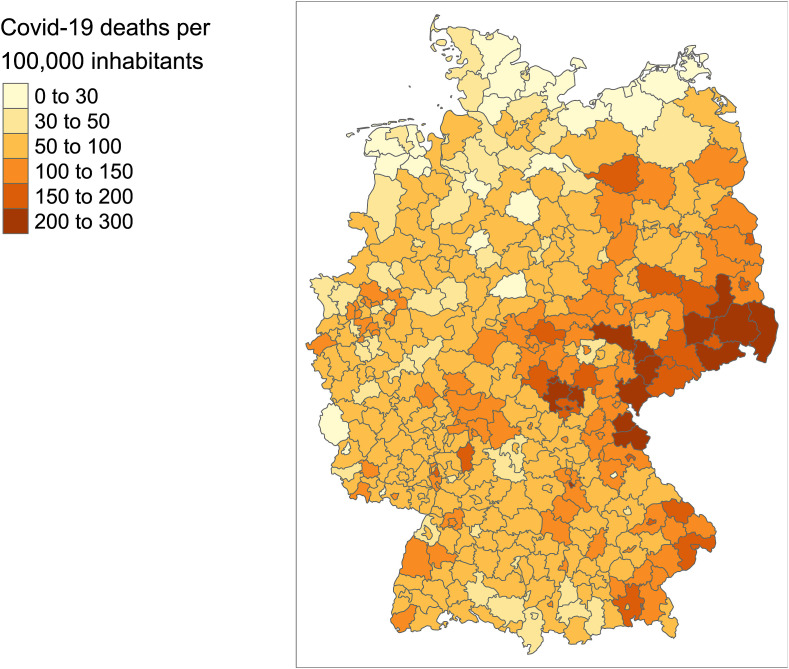
3.2. Particulate matter concentration and COVID-19 mortality
Although the number of COVID-19 cases and the number of COVID-19-related deaths correlated with each other, a specific analysis of the relationship between long-term exposure to particulate matter and the COVID-19 death rate was required, as the severity of the disease might be more sensitive to long-term PM10 and PM2.5 concentration than the number of infections. COVID-19-related deaths are shown in Fig. 4 .
Fig. 4.
COVID-19 deaths per 100,000 inhabitants in Germany. Source: Data from Robert Koch Institute, RKI 2021.
The estimation results are presented in Table 3 for PM10 and in Table 4 for PM2.5. All regressions were run including the confounding variables, presented in Section 2.1. The structure of Table 3, Table 4 is the same as in Table 1, Table 2. Columns 2 and 3 contain the estimated and standardized values of the basic model, Columns 4 and 5 the respective values for the estimation with state fixed effects. Note that Table 3, Table 4 encompass all counties, whereby missing values of fine particulate matter are Kriging-interpolated. Estimations with recorded values only are presented in Tables A3 and A4 in the Appendix.
Table 3.
COVID-19 mortality per 100,000 inhabitants and Kriging-interpolated PM10 pollution.
| Variable | Basic Model | Standardized Coefficients | State Fixed Effects Model | Standardized Coefficients |
|---|---|---|---|---|
| Distance to Ischgl | −0.071*** (0.009) |
−0.316617 | −0.042 (0.030) |
−0.1883841 |
| Distance to nearest German hotspot | 0.139*** (0.026) |
0.2328296 | 0.130*** (0.037) |
0.2178253 |
| Nursing home places per 100 k inhabitants at 75 and older | 0.003*** (0.001) |
0.133083 | 0.004*** (0.001) |
0.1687632 |
| Share of people >75 years | 753.997*** (156.552) |
0.2647978 | 706.861*** (213.657) |
0.2482438 |
| Population density | 0.006** (0.003) |
0.09350062 | 0.004* (0.002) |
0.059609 |
| Commuter flow (modified) | −0.0002** (0.0001) |
−0.1037025 | −0.0002*** (0.0001) |
−0.1017682 |
| Avg. PM10, 2002 to 2020 | 2.108*** (0.714) |
0.1325954 | 1.211 (1.037) |
0.07614606 |
| Avg. Income 2002 to 2018 | 0.324 (0.958) |
0.01543386 | 0.360 (1.059 |
0.01717202 |
| East Germany | 23.729*** (7.973) |
0.1902687 | ||
| Border with Czech Republic | 81.108*** (18.424) |
0.3031498 | 63.000*** (9.778) |
0.2354696 |
| Constant | −75.135** (34.165) |
|||
| Fixed effects | No | Yes | ||
| Observations | 400 | 400 | ||
| Adj. R2 | 0.477 | 0.204 | ||
| F Statistic | 37.443*** (df = 10; 389) |
14.026*** (df = 9; 375) |
*, **, ***: p < 0.1, 0.05, 0.01, respectively. -
Source: Own calculations.
Table 4.
COVID-19 mortality per 100,000 inhabitants and Kriging-interpolated PM2.5 pollution.
| Variable | Basic Model | Standardized Coefficients | State Fixed Effects Model | Standardized Coefficients |
|---|---|---|---|---|
| Distance to Ischgl | −0.074*** (0.009) |
−0.3329968 | −0.038 (0.031) |
−0.1701805 |
| Distance to nearest German hotspot | 0.147*** (0.0256) |
0.2459477 | 0.133*** (0.041) |
0.2226709 |
| Nursing home places per 100 k inhabitants at 75 and older | 0.003*** (0.001) |
0.1405996 | 0.004*** (0.001) |
0.1639519 |
| Share of people >75 years | 693.680*** (153.798) |
0.2436149 | 688.833*** (209.357) |
0.2419125 |
| Population density | 0.006** (0.002) |
0.09066316 | 0.004* (0.002) |
0.06479335 |
| Commuter flow (modified) | −0.0002* (0.0001) |
−0.0940145 | −0.0002** (0.0001) |
−0.1027767 |
| Avg. PM2.5, 2010 to 2020 | 6.177*** (1.439) |
0.1661786 | 2.929 (2.361) |
0.07879814 |
| Avg. Income 2002 to 2018 | 0.418 (1.015) |
0.01992261 | 0.229 (1.255) |
0.0109199 |
| East Germany | 22.477*** (7.853) |
0.1802286 | ||
| Border with Czech Republic | 74.894*** (19.248) |
0.2832652 | 58.734*** (19.248) |
0.2277068 |
| Constant | −102.044*** (36.664) |
|||
| Fixed effects | No | Yes | ||
| Observations | 400 | 400 | ||
| Adj. R2 | 0.486 | 0.203 | ||
| F Statistic | 38.736*** (df = 10; 389) |
131.428*** (df = 9; 375) |
*, **, ***: p < 0.1, 0.05, 0.01, respectively. -
Source: Own calculations.
According to the basic model in Table 3, Table 4, PM10 and PM2.5 were statistically significantly and positively correlated with the number of COVID-19 mortality in Germany. As with COVID-19 cases, East Germany suffered from a higher burden of COVID-19 fatalities than the western part of the country. However, the particulate matter correlation with COVID-19 mortality was not robust to controlling for state-level fixed effects. In addition to the variables that already correlated with COVID-19 cases, the number of nursing home places for elderly people statistically significantly and positively correlated with the number of COVID-19 fatalities. The effect sizes of these determinants was substantial.
An issue with these estimations was that the number of COVID-19 cases and fatalities correlated. Therefore, in the estimations of Table 5, Table 6 , the number of COVID-19 cases was included as a regressor. Note that Table 5, Table 6 encompass all counties, whereby missing values of fine particulate matter concentration are Kriging-interpolated. Estimations with recorded values only are presented in Tables A5 and A6 in the Appendix.
Table 5.
COVID-19 mortality per 100,000 inhabitants and Kriging-interpolated PM10 pollution (including COVID-19 cases).
| Variable | Basic Model | Standardized Coefficients | State Fixed Effects Model | Standardized Coefficients |
|---|---|---|---|---|
| Covid-19 cases per 100 k inhabitants | 0.036*** (0.002) |
0.7038624 | 0.036*** (0.003) |
0.7074111 |
| Distance to Ischgl | −0.002 (0.008) |
−0.01048626 | 0.023 (0.031) |
0.1046181 |
| Distance to nearest German hotspot | 0.075*** (0.019) |
0.1251119 | 0.059 (0.037) |
0.09903778 |
| Nursing home places per 100 k inhabitants at 75 and older | 0.003*** (0.001) |
0.1083218 | 0.002*** (0.004) |
0.09907837 |
| Share of people >75 years | 620.042*** (107.581) |
0.2177538 | 650.551*** (120.058) |
0.2284682 |
| Population density | −0.003** (0.002) |
−0.04961626 | −0.002 (0.001) |
−0.02769972 |
| Commuter flow (modified) | −0.0001 (0.00005) |
−0.03506787 | −0.0001** (0.00004) |
−0.04919842 |
| Avg. PM10, 2002 to 2020 | 0.217 (0.550) |
0.01364661 | −0.099 (0.924) |
−0.006198567 |
| Avg. Income 2002 to 2018 | 0.152 (0.925) |
0.007223405 | −0.039 (1.173) |
−0.00183901 |
| East Germany | 4.053 (5.231) |
0.03249576 | ||
| Border with Czech Republic | 12.475 (13.439) |
0.04662592 | 11.370 (8.967) |
0.04249736 |
| Constant | −132.919*** (28.727) |
|||
| Fixed effects | No | Yes | ||
| Observations | 400 | 400 | ||
| Adj. R2 | 0.743 | 0.569 | ||
| F Statistic | 105.713*** (df = 11; 388) |
55.165*** (df = 10; 374) |
*, **, ***: p < 0.1, 0.05, 0.01, respectively. -
Source: Own calculations.
Table 6.
COVID-19 mortality per 100,000 inhabitants and Kriging-interpolated PM2.5 pollution (including COVID-19 cases).
| Variable | Basic Model | Standardized Coefficients | State Fixed Effects Model | Standardized Coefficients |
|---|---|---|---|---|
| Covid-19 cases per 100 k inhabitants | 0.037*** (0.002) |
0.7217954 | 0.037*** (0.003) |
0.7201644 |
| Distance to Ischgl | 0.0005 (0.008) |
0.002071874 | 0.027 (0.029) |
0.1204697 |
| Distance to nearest German hotspot | 0.074*** (0.019) |
0.1244012 | 0.058* (0.035) |
0.09757158 |
| Nursing home places per 100 k inhabitants at 75 and older | 0.003*** (0.001) |
0.1051916 | 0.002*** (0.0005) |
0.09852581 |
| Share of people >75 years | 604.416*** (106.596) |
0.212266 | 643.366*** (117.721) |
0.2259449 |
| Population density | −0.003** (0.002) |
−0.04422172 | −0.002 (0.001) |
−0.02281696 |
| Commuter flow (modified) | −0.0001 (0.00004) |
−0.03652956 | −0.0001** (0.00004) |
−0.04818884 |
| Avg. PM2.5, 2010 to 2020 | −1.208 (1.032) |
−0.03250641 | −1.909* (0.924) |
−0.05135185 |
| Avg. Income 2002 to 2018 | 0.080 (0.910) |
0.003811532 | −0.061 (1.104) |
−0.00291217 |
| East Germany | 4.268 (5.201) |
0.03422297 | ||
| Border with Czech Republic | 11.926 (13.431) |
0.04457573 | 11.293 (8.684) |
0.04221049 |
| Constant | −115.064*** (28.727) |
|||
| Fixed effects | No | Yes | ||
| Observations | 400 | 400 | ||
| Adj. R2 | 0.743 | 0.572 | ||
| F Statistic | 106.082*** (df = 11; 388) |
55.773*** (df = 10; 374) |
*, **, ***: p < 0.1, 0.05, 0.01, respectively. -
Source: Own calculations.
Although the number of COVID-19 cases and the concentration of fine particulate matter had been correlated, the correlation (about 0.21) did not disturb the estimation. The latter also held true for the remaining regressors. The estimations demonstrate that there was no correlation between the concentration of PM10 and PM2.5 (there was only one estimated PM2.5 value that was statistically significant at the 10% error level in Table 6, but it had a negative sign) and COVID-19 fatalities over and above the effect of fine particulate matter concentration on the number of COVID-19 cases.
4. Discussion
This paper is essentially ecological in approach. There is a mechanism that combines the SARS-CoV-2 virus with detrimental effects for the human respiratory system and the immune system at the microscopic-level of the human body. The same applies to particulate matter air pollution, although it cannot be stated that these effects are also observable in events at the macroscopic level (Anjum and Mumford, 2018, p. 110), but the known mechanism renders such effects at least plausible.
As with all ecological studies, the criticism of Villeneuve and Goldberg (2020) is relevant for this paper too. They draw attention to the methodological shortcomings and constraints of ecological studies on the connection between fine particulate matter and COVID-19. As they pointed out, the main shortcomings are (see also Goldberg and Villeneuve, 2021):
-
(a)
cross-level bias (ecological fallacy) due to using regional-level fine particulate matter (PM) pollution data as proxies for unavailable individual-level exposures to PM,
-
(b)
underreporting health outcomes, i.e., COVID-19 cases and deaths,
-
(c)
lack of highly-resolution measurements of spatial air pollution,
-
(d)
inadequate control for confounding,
-
(e)
ignorance of the regional variation in the timing and temporal changes of the pandemic with respect to at-risk populations.
Although some of these shortcomings may be eliminated or alleviated (for instance, control for confounding or the resolution of spatial air pollution), it is not possible to provide clear-cut evidence of the causality of PM in the transmission of the coronavirus and the severity of COVID-19. In the meantime, ecological studies using regression analysis may be the only sources of empirical evidence of these effects (Wu et al., 2020). Ecological studies cannot prove their case, but they can nevertheless provide exploratory evidence of the hypothesis that the respective effects do indeed exist (Stieb et al., 2021). Of course, individual studies are indispensable for deciding whether the hypothesis can be confirmed. Robotto et al. (2021) proposed standardized methods for indoor and outdoor air sampling that could be applied by respective studies. However, data for such studies is not currently available, and probably will not be for a long time. Moreover, potential underreporting of health outcomes is also an unsolvable issue for this paper.
Nevertheless, criticisms (c), (d) and (e) were accounted for in this study. Although satellite data was not at our disposal, Kriging interpolation, a widely used approach in geographical information systems, was used to extend the available air pollution data to cover all of Germany. In addition, averaging data over a longer period is considered as a proxy variable for long-term exposure to air pollution for the respective population. However, this is no substitute for individual-level exposure data that is required for causal analysis.
Air pollution with fine and ultrafine particulate matter was found in a correlation analysis, as related to COVID-19 cases and fatalities in Germany. To test this connection more thoroughly, we incorporated several relevant covariates into the regression analysis to control for confounding. The selection of data was driven by an attempt to control for long-term, as well as short-term confounding variables.
First of all, three coronavirus-related variables were included as covariates in the estimations:
-
•
the distance to the Austrian ski resort, Ischgl, that was one of the first hotspots of German COVID-19 cases when holiday makers returned from skiing holidays there (Felbermayr et al., 2020),
-
•
the distances to German COVID-19 hotspots, for instance Heinsberg, where carnival celebrations had been superspreader events (Felbermayr et al., 2020) and
-
•
dummy variables for counties at the border to the Czech Republic that was heavily hit by SARS-CoV-2 (ElbeLabe, 2021).
In estimations for Germany, two variables are important indicators of socioeconomic differences:
-
•
a dummy variable for East Germany, as this part of the country still lags behind West Germany with respect to its socioeconomic development and
-
•
disposable income at the county-level. As with the air pollution variable, disposable income was averaged over 2002 to 2008, in order to control for long-term income.
As soon became clear just after the beginning of the COVID-19 pandemic, older people had a considerably higher risk of coming down with COVID-19 and to dying from the disease, in particular because more of this age cohort live in nursing homes and suffer from comorbidities (Barnett and Grabowski, 2020). To control for this specific situation, the following covariates (all at the county-level) were included in the estimations:
-
•
the share of people 75 years and older and
-
•
the number of nursing home places per 100,000 inhabitants for people 75 years and older.
As further demographic variables.
-
•
population density and
-
•
commuter flows
were included in the estimations. A higher population density correlates with higher infection risks (Wong and Li, 2020) and commuter flows may propagate the virus between counties (Mitze and Kosfeld, 2021).
Nevertheless, due to unavailability, health variables at the county-level are missing, although they are potentially confounding variables (Sarmadi et al., 2021). Since we controlled for the population share of older people, the morbidity of these people was indirectly included in the estimations.
A further limitation that restricts the explanatory power of all ecological studies concerning COVID-19 is the unknown number of asymptomatic cases. Those who are asymptomatically infected are generally younger, but may show CT abnormalities, and are contagious (Kronbichler et al., 2020). Therefore, estimations of the relationship between air pollution and COVID-19 may be biased by the unknown county-distribution of asymptomatic cases.
In an alternative estimation model in Section 3, state-level fixed effects were included. Germany consists of 16 federal states (called ‘Bundesländer’), that are further subdivided into counties. To control for potential air pollution and COVID-19 externalities between counties in a federal state, a state-level fixed effects model was estimated. With both air pollution variables PM2.5 and PM10, the estimated coefficients with respect to COVID-19 infection cases became smaller, but remained statistically significant. This means that the correlation between fine particulate matter air pollution and infections was robust for these controls. However, this was different for estimations of the correlation between fine particulate matter air pollution and COVID-19 deaths. Controlling for state-level fixed effects, the estimated coefficients lost their statistical significance. Hence, the latter effect was not robust to state-level controls. Therefore, it is difficult to say whether particulate matter pollution increased COVID-19 fatalities. Further investigations are required to resolve this issue.
To include all German counties (with one exception) in the empirical analysis, Kriging interpolation was used. Missing air pollution values were interpolated with this method because satellite data were not available. To determine whether this may create bias in the estimations, estimations only for those counties with measuring stations are shown in the Appendix. The outcome was that the results with Kriging interpolations did not differ much from those with only original data (and, hence, a smaller number of included counties). The only exception was the estimation of long-term PM2.5 air pollution on COVID-19 fatalities. These estimations were statistically insignificant, probably due to the relatively small number of measuring stations.
To render the interpretation of the estimated coefficient more convenient, standardized coefficients were calculated and presented in the tables in Section 3. Standardized coefficients reveal the strength of an effect in relation to the standard deviation of the variable. In multiple regression analysis, this renders it possible to compare effect sizes among the estimated coefficients.
Of course, the results presented in this paper cannot be interpreted as causal effects. As indicated above, there are also some limitations of this paper from an ecological viewpoint:
-
•
there are data gaps, as not all German counties have measuring stations for particulate matter air pollution and
-
•
there is no data on the distribution of other diseases in the counties.
Nevertheless, the results of the empirical analysis in this paper provide some exploratory indications of a connection between fine particulate air pollution and COVID-19 infections and – to a lesser extent – COVID-19 fatalities in Germany. Nevertheless, there might be an indirect effect of fine particulate matter concentration on COVID-19 fatalities via the number of COVID-19 cases. Accordingly, one could argue that COVID-19 cases are a mediator variable for the transmission of fine particulate matter pollution on COVID-19 fatalities.
5. Conclusion
Long-term exposure to fine particulate air pollution correlates with COVID-19 infections and – to a lesser extent – to COVID-19 fatalities in Germany. These results for Germany provide a further piece in the global puzzle of the connections of air pollution and diseases in general, as well as COVID-19 in particular. The county-level seems to be internationally the lowest administrative level for which data is available. The next small step in ecological research may be to apply satellite data to measure air pollution much more precisely than with data from measuring stations. The next big step, however, would entail investigations with data at the individual exposure with fine particulate matter and other sources of air pollution, in order to explore whether and to what extent air pollution is a causal factor for diseases like COVID-19.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
The county of Göttingen was not included in the estimations, due to a local government reform in 2016, when the former counties of Göttingen and Osterode am Harz merged. The new county was named Göttingen.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2021.111948.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Ali N., Islam F. The effects of air pollution on COVID-19 infection and mortality – a review on recent evidence. Front. Public Health. 2020;8:580057. doi: 10.3389/fpubh.2020.580057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali N., Fariha K.A., Islam F., Mishu M.A., Mohanto N.C., Hosen M.J., Hossain K. Exposure to air pollution and COVID-19 severity: a review of current insights, management, and challenges. Integrated Environ. Assess. Manag. 2021;2021:1–9. doi: 10.1002/ieam.4435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson J.O., Thundiyil J.G., Stolbach A. Clearing the air: a review of the effects of particulate matter air pollution on human health. J. Med. Toxicol. 2012;8:166–175. doi: 10.1007/s13181-011-0203-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anjum R.L., Mumford S. Oxford University Press; Oxford: 2018. Causation in Science and the Methods of Scientific Discovery. [Google Scholar]
- ArcGIS . 2021. How Kriging Works.https://help.arcgis.com/en/arcgisdesktop/10.0/help/index.html#//009z00000076000000.htm ArcGIS Resource Center at. [Google Scholar]
- Barnett M.L., Grabowski D.C. Nursing homes are ground zero for COVID-19 pandemic. JAMA Health Forum. 2020;1(3) doi: 10.1001/jamahealthforum.2020.0369. [DOI] [PubMed] [Google Scholar]
- Barnett-Itzhaki Z., Levi A. Effects of chronic exposure to ambient air pollutants on COVID-19 morbidity and mortality – a lesson from OECD countries. Environ. Res. 2021;195:110723. doi: 10.1016/j.envres.2021.110723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becchetti L., Beccari G., Conzo G., Conzo P., De Santis D., Salustri F. Air quality and COVID-19 adverse outcomes: divergent views and experimental findings. Environ. Res. 2021;193:110556. doi: 10.1016/j.envres.2020.110556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolaño-Ortiz T.R., Caramargo-Caicedo Y., Puliafito S.E., Ruggeri M.F., Bolaño-Diaz S., Pascual-Flores R., Saturno J., Ibarra-Espinosa S., Mayol-Bracero O.L., Torres-Delgado E., Cereceda-Balic F. Spread of SARS-CoV-2 through Latin America and the Caribbean region: a look from its economic conditions, climate and air pollution indicators. Environ. Res. 2020;191 doi: 10.1016/j.envres.2020.109938. doi:109938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourdrel T., Annesi-Maesano I., Alahmad B., Maesano C.N., Bind M.-A. The impact of outdoor air pollution on COVID-19: a review of evidence from in vitro, animal, and human studies. Eur. Respir. Rev. 2021;30:200242. doi: 10.1183/16000617.0242-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowe B., Xie Y., Gibson A.K., Cai M., van Donkelaar A., Martin R.V., Burnett R., Al-Aly Z. Ambient fine particulate matter air pollution and the risk of hospitalization among COVID-19 positive individuals: cohort study. Environ. Int. 2021;154:106564. doi: 10.1016/j.envint.2021.106564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborty J. Convergence of COVID-19 and chronic air pollution risks: racial/ethnic and socioeconomic inequities in the U.S. Environ. Res. 2021;193:110586. doi: 10.1016/j.envres.2020.110586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciencewicki J., Jaspers I. Air pollution and respiratory viral infection. Inhal. Toxicol. 2007;19:1135–1146. doi: 10.1080/08958370701665434. [DOI] [PubMed] [Google Scholar]
- Coccia M. High health expenditures and low exposure of population to air pollution as critical factors that can reduce fatality rate in COVID-19 pandemic crisis: a global analysis. Environ. Res. 2021;199:111339. doi: 10.1016/j.envres.2021.111339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen A.J., Brauer M., Burnett R., et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389:1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comunian S., Dongo D., Milani C., Palestini P. Air pollution and COVID-19: the role of particulate matter in the spread and increase of COVID-19’s morbidity and mortality. Int. J. Environ. Res. Publ. Health. 2020;17 doi: 10.3390/ijerph17124487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020;261:114465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copat C., Cristaldi A., Fiore M., Grasso A., Zuccarello P., Signorelli S.S., Conti G.O., Ferrante M. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: a systematic review. Environ. Res. 2020;191:110129. doi: 10.1016/j.envres.2020.110129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y., Zhang Z.-F., Froines J., Zhao J., Wang H., Yu S.-Z., Detels R. Air pollution and case fatality of SARS in the People's Republic of China: an ecologic study. Environ. Health. 2003:2. doi: 10.1186/1476-069X-2-15. 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domingo J.L., Rovira J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ. Res. 2020;187:109650. doi: 10.1016/j.envres.2020.109650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Girolamo P. Assessment of the potential role of atmospheric particulate pollution and airborne transmission in intensifying the first wave pandemic impact of SARS-CoV-2/COVID-19 in northern Italy. Bull. Atmos. Sci. Technol. 2021 doi: 10.1007/s42865-020-00024-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ElbeLabe . 2021. Current Regulations on Covid-19 in Saxony and Czechia.https://www.elbelabe.eu/en/current-regulations-on-covid-19/ Internet URL: [Google Scholar]
- European Commission, n.y. Air Quality Standards. https://ec.europa.eu/environment/air/quality/standards.htm (accessed 30 March 2021).
- Fattorini D., Regoli F. Role of the chronic air pollution levels in the COVID-19 outbreak risk in Italy. Environ. Pollut. 2020;264:114732. doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felbermayr G., Hinz J., Chowdhry S. Kiel Institut for the World Economy and Kiel Centre for Globalization; 2020. Après Ski: The Spread of Coronavirus from Ischgl through Germany. [Google Scholar]
- Filippini T., Rothman K.J., Cocchio S., Narne E., Mantoan D., Saia M., Goffi A., Ferrari F., Maffeis G., Orsini N., Baldo V., Vinceti M. Associations between mortality from COVID-19 in two Italian regions and outdoor air pollution as assessed through tropospheric nitrogen dioxide. Sci. Total Environ. 2021;760:143355. doi: 10.1016/j.scitotenv.2020.143355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera A., Cianfanelli L., Vlachos K., Landoni G., Cremona G. Severe air pollution links to higher mortality in COVID-19 patients: the “double hit” hypothesis. J. Infect. 2020 doi: 10.1016/j.jinf.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg M.S., Villeneuve P.J. Re: an ecological analysis of long-term exposure to PM2.5 and incidence of COVID-19 in Canadian health regions. Environ. Res. 2021;194:110610. doi: 10.1016/j.envres.2020.110610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo C., Zhang Z., Lau A.K.H., Lin C.Q., Chuang Y.C., Chan J., Jiang W.K., Tam T., Yeoh E.-K., Chan T.-C., Chang L.-Y., Lao X.Q. Effect of long-term exposure to fine particulate matter on lung function decline and risk of chronic obstructive pulmonary disease in Taiwan: a longitudinal, cohort study. Lancet Planet. Health. 2018;2:e114–125. doi: 10.1016/S2542-5196(18)30028-7. [DOI] [PubMed] [Google Scholar]
- Guo C., Hoek G., Chang L.-Y., Bo Y., Lin C., Huang B., Chan T.-C., Tam T., Lau A.K.H., Lao X.Q. Long-term exposure to ambient fine particulate matter (PM2.5) and lung function in children, adolescent, and young adults: a longitudinal cohort study. Environ. Health Perspect. 2019;127(12) doi: 10.1289/EHP5220. 127008-1-127008-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang G., Brown P.E. Population-weighted exposure to air pollution and COVID-19 incidence in Germany. Spat. Stat. 2021;41:100480. doi: 10.1016/j.spasta.2020.100480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isphording I.E., Pestel N. Pandemic meets pollution: poor air quality increases deaths by COVID-19. J. Environ. Econ. Manag. 2021;108:102448. doi: 10.1016/j.jeem.2021.102448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronbichler A., Kresse D., Yoon S., Leed K.W., Effenberger M., Shin J.I. Asymptomatic patients as a source of COVID-19 infections: a systematic review and meta-analysis. Int. J. Infect. Dis. 2020;98:180–186. doi: 10.1016/j.ijid.2020.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leifer I., Kleinman M.T., Blake D., Tratt D., Marston C. Wildfire smoke exposure: Covid-19 comorbidity? J. Respiration. 2021;1:74–79. [Google Scholar]
- Lelieveld J., Klingmüller K., Pozzer A., Pöschl U., Fnais M., Daiber A., Münzel T. Cardiovasular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur. Heart J. 2019;40(20):1590–1596. doi: 10.1093/eurheart/ehz135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lembo R., Landoni G., Cianfanelli L., Frontera A. Air pollutants and SARS-CoV-2 in 33 European countries. Acta Biomed. 2021;92(1) doi: 10.23750/abm.v92i1.11155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Xu X.-L., Dai D.-W., Huang Z.-Y., Yan-Jun Z.M. Air pollution and temperature are associated with increased COVID-19 incidence: a time series study. Int. J. Infect. Dis. 2020;97:278–282. doi: 10.1016/j.ijid.2020.05.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang D., Shi L., Zhao J., Liu P., Sarnat J.A., Gao S., Schwartz J., Liu Y., Ebelt S.T., Scovronick N., Chang H.H. Urban air pollution may enhance COVID-19 case-fatality and mortality rates in the United States. Innovation. 2020;1(3):100047. doi: 10.1016/j.xinn.2020.100047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maleki M., Anvari E., Hopke P.K., Noorimotlagh Z., Mirzaee S.A. An updated systematic review on the association between atmospheric particulate matter pollution and prevalence of SARS-CoV-2. Environ. Res. 2021;195:110898. doi: 10.1016/j.envres.2021.110898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquès M., Rovira J., Nadal M., Domingo J.L. Effects of air pollution on the potential transmission and mortality of COVID-19: a preliminary case-study in Tarragona province (Catalonia, Spain) Environ. Res. 2021;192:110315. doi: 10.1016/j.envres.2020.110315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martelletti L., Martelletti P. Air pollution and the novel COVID-19 disease: a putative disease risk factor. SN Compr. Clin. Med. 2020 doi: 10.1007/s42399-020-00274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendy A., Wu X., Keller J.L., Fassler C.S., Apewokin S., Mersha T.B., Xie C., Pinney S.M. Long-term exposure to fine particulate matter and hospitalization in COVID-19 patients. Respir. Med. 2021;178:106313. doi: 10.1016/j.rmed.2021.106313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meo S.A., Abukhalaf A.A., Alomar A.A., Alessa O.M. Wildfire and COVID-19 pandemic: effect of environmental pollution PM-2.5 and carbon monoxide on the dynamics of daily cases and deaths due to SARS-CoV-2 infection in San-Francisco USA. Eur. Rev. Med. Pharmacol. Sci. 2020;12:10286–10292. doi: 10.26355/eurrev_202010_23253. [DOI] [PubMed] [Google Scholar]
- Mitze T., Kosfeld R. The propagation effect of commuting to work in the spatial transmission of COVID-19. J. Geogr. Syst. 2021 doi: 10.1007/s10109-021-00349-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nor N.S.M., Yip C.W., Ibrahim N., Jaafar M.H., Rashid Z.Z., Mustafa N., Hamid H.H.A., Chandru K., Latif M.T., Saw P.E., Lin C.Y., Alhasa K.M., Hashim J.H., Nadzir M.S.M. Particulate matter (PM2.5) as a potential SARS-CoV-2 carrier. Nature Sci. Rep. 2021;11:2508. doi: 10.1038/s41598-021-81935-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver M.A. Kriging: a method of interpolation for geographical information systems. Int. J. Geogr. Inf. Syst. 1990;4:313–332. [Google Scholar]
- Persico C.L., Johnson K.R. The effects of increased pollution on COVID-19 cases and deaths. J. Environ. Econ. Manag. 2021;107:102431. doi: 10.1016/j.jeem.2021.102431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pozzer A., Dominici F., Haines A., Witt C., Münzel T., Lelieveld J. Regional and global contributions of air pollution to risk of death from COVID-19. Cardiovasc. Res. 2020;116:2247–2253. doi: 10.1093/cvr/cvaa288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert Koch Institute (RKI) RKI; 2021. COVID-19 Cases and Death Rates Germany.https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Fallzahlen.html [Google Scholar]
- Robotto A., Quaglino P., Lembo D., Morello M., Brizio E., Bardi L., Civra A. SARS-CoV-2 and indoor/outdoor air samples: a methodological approach to have consistent and comparable results. Environ. Res. 2021;195:110847. doi: 10.1016/j.envres.2021.110847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarmadi M., Moghanddam V.K., Dickerson A.S., Martelletti L. Association of COVID-19 distribution with air quality, sociodemographic factors, and comorbidities: an ecological study of US states. Air Qual. Atmos. Health. 2021;14:455–465. doi: 10.1007/s11869-020-00949-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakil M.H., Munim Z.H., Tasnia M., Sarowar S. COVID-19 and the environment: a critical review and research agenda. Sci. Total Environ. 2020;745:141022. doi: 10.1016/j.scitotenv.2020.141022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma G.D., Tiwari A.K., Jain M., Yadav A., Srivastava M. COVID-19 and environmental concerns: a rapid review. Renew. Sustain. Energy Rev. 2021;148:111239. doi: 10.1016/j.rser.2021.111239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistische Ämter . 2021. Indikatoren und Karten zur Raum- und Stadtentwicklung.https://www.inkar.de [Google Scholar]
- Statistische Ämter . 2021. Volkswirtschaftliche Gesamtrechnung der Länder, Reihe 2. Kreisergebnisse Band 3. Einkommen der privaten Haushalte in den kreisfreien Städten und Landkreisen der Bundesrepublik Deutschland 1995 bis 2018.https://www.statistikportal.de/de/vgrdl/ergebnisse-kreisebene/einkommen-kreise [Google Scholar]
- Stieb D.M., Evans G.J., To T.M., Brook J.R., Burnett R.T. An ecological analysis of long-term exposure to PM2.5 and incidence of COVID-19 in Canadian health regions. Environ. Res. 2020;191:110052. doi: 10.1016/j.envres.2020.110052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stieb D.M., Evans G.J., To T.M., Brook J.R., Burnett R.T. Response to Goldberg and Villeneuve re: an ecological analysis of long-term exposure to PM2.5 and incidence of COVID-19 in Canadian health regions. Environ. Res. 2021;194:110623. doi: 10.1016/j.envres.2020.110623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockfelt L., Andersson E.M., Molnár P., Gidhagen L., Segersson D., Rosengren A., Barregard L., Sallsten G. Long-term effects of total and source-specific particulate air pollution on incident cardiovascular disease in Gothenburg, Sweden. Environ. Res. 2017;158:61–71. doi: 10.1016/j.envres.2017.05.036. [DOI] [PubMed] [Google Scholar]
- Travaglio M., Yu Y., Popovic R., Selley L., Leal N.S., Martins L.M. 2020. Links between Air Pollution and COVID-19 in England.https://www.medrxiv.org/content/10.1101/2020.04.16.20067405v5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umweltbundesamt . 2021. Feinstaubmesswerte der Jahre 2002 bis 2020.https://www.umweltbundesamt.de/themen/luft/luftschadstoffe/feinstaub [Google Scholar]
- Villeneuve P.J., Goldberg M.S. Methodological considerations for epidemiological studies of air pollution and the SARS and COVID-19 coronavirus outbreaks. Environ. Health Perspect. 2020;128(9) doi: 10.1289/EHP7411. 095001-1-095001-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Who . World Health Organization; Geneva: 2006. Air Quality Guidelines Global Update 2005. [Google Scholar]
- Who . WHO; Geneva: 2016. Ambient Air Pollution: A Global Assessment of Exposure and Burden of Disease. [Google Scholar]
- Wong D.W.S., Li Y. Spreading of COVID-19: density matters. PLoS One. 2020;15(12) doi: 10.1371/journal.pone.0242398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodby B., Arnold M.M., Valacchi G. SARS-CoV-2 infection, COVID-19 pathogenesis, and exposure to air pollution: what is the connection? Ann. N. Y. Acad. Sci. 2020 doi: 10.1111/nyas.14512. 2020 Oct 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Nethery R.C., Sabath M.B., Braun D., Dominici F. Air pollution and COVID-19 mortality in the United States: strengths and limitations of an ecological regression analysis. Sci. Adv. 2020;6 doi: 10.1126/sciadv.abd4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y., Pan J., Liu Z., Meng X., Wang W., Kan H., Wang W. Temporal association between particulate matter pollution and case fatality rate of COVID-19 in Wuhan. Environ. Res. 2020;189:109941. doi: 10.1016/j.envres.2020.109941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y., Pan J., Wang W., Liu Z., Kan H., Qiu Y. Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chines cities. Sci. Total Environ. 2020;741:140396. doi: 10.1016/j.scitotenv.2020.140396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Tang M., Guo F., Wei F., Yu Z., Gao K., Jin M., Wang J., Chen K. Associations between air pollution and COVID-19 epidemic during quarantine period in China. Environ. Pollut. 2021;268:115897. doi: 10.1016/j.envpol.2020.115897. Part A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao C., Fang X., Feng Y., Fang X., He Y., Pan H. Emerging role of air pollution and meteorological parameters in COVID-19. J. Evid. Based Med. 2021;14:123–138. doi: 10.1111/jebm.12430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu C., Maharajan K., Liu K., Zhang Y. Role of atmospheric particulate matter exposure in COVID-19 and other health risks in human: a review. Environ. Res. 2021;198:111281. doi: 10.1016/j.envres.2021.111281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.