Highlights
-
•
Child mask behavior is influenced by their parents’ attitudes, accepted norms, and self-efficacy.
-
•
For healthy children, mask behavior is primarily driven by parents’ strong beliefs about mask effectiveness.
-
•
For children with pre-conditions that may make mask-wearing difficult, mask behavior is driven by parents’ strong intentions to enforce mask wearing.
Keywords: COVID-19, Mask use, Protective behaviours, Parent-for-child behaviour, Theory of planned behavior, School
Abstract
Face masks continue to be a necessity until a large proportion of the population, including children, receive immunizations for COVID-19. The aim of this study was to investigate the relationship between parental attitudes and beliefs about masks and parent-for-child mask behavior using the Theory of Planned Behavior. We administered a survey in August 2020 to parents of school-aged children residing in the United States and Canada. Measures included sociodemographic variables for the parent and child, attitudes, norms, perceived control over children’s mask use, intentions and enforcement of mask wearing among children (also titled “parent-for-child mask behavior”). Data were analyzed using structural equation modelling. We collected data from 866 parents and 43.5% had children with pre-existing conditions (e.g., allergies, anxiety, impulsivity, skin sensitivity, asthma) that made extended mask wearing difficult, as per parent’s report. Among the full sample, negative attitudes (β = -0.20, p = .006), norms (β = 0.41, p = .002), and perceived control (β = 0.33, p = .006) predicted intentions. Norms (β = 0.50, p = .004) and intentions (β = 0.28, p = .003) also predicted parent-for-child mask use, while attitudes and perceived control did not. Intentions mediated the associations between attitudes, norms, perceived control, respectively, and mask behavior. Subgroup analyses revealed intentions as the key predictor of parent-for-child mask use among children with pre-conditions and norms as the key predictor among children without pre-conditions (i.e. healthy). Future public health messaging should target parental intentions, attitudes, norms, and perceived control about children’s masks wearing.
1. Background
Despite aggressive COVID-19 vaccination campaigns for teachers in the United States, transmission of the the SARS-Cov-2 virus that causes COVID-19 can still occur in schools. For example, surveillance data from the state of Massachusetts collected from 18 district dashboards in seven counties from 9/1/20 through 2/27/21 shows that community transmission rates among children (3,199 cases in 67,157 children) were similar to those found in the community (28,303 cases in 556,000 adults) at 5% (Personal Communication). This suggests that children can act as vectors for the disease, unlike previously speculated (Vogel, 2020). Absent a COVID-19 vaccine with demonstrated efficacy and safety among children, schools continue to face unprecedented challenges to contain transmission, many of which are dependent on the availability of resources to implement preventive measures (Krishnaratne et al., 2020) and parents willingness’ to adhere to and enforce public health recommendations among their children.
Mask wearing is the most accepted and accessible strategy to mitigate transmission of SARS-Cov-2 (Krishnamachari et al., 2021), even after vaccination. For example, a 2020 meta-analysis found that face masks were associated with a decreased risk of infection of respiratory viruses, including SARS-CoV-2 (Chu et al., 2020). A large population study conducted in the US found that compared to states with mask mandates implemented within 1 month, the states without mask mandates or with masks implemented later had higher infection rates (Krishnamachari et al., 2021). Mask use has also been shown to reduce transmission among children. A cross-sectional study conducted in the US with individuals 13 year of age and older (N = 378,207) found that wearing face masks was associated with reduced community transmission of COVID-19, as measured by the instantaneous reproductive number (Rt) (Rader et al., 2021). A cross-sectional survey conducted in Canada with parents of school-aged children (N = 565) found that increased mask wearing and fewer attended gatherings were associated with lower seropositivity among children aged 8 to 13 years; and for each attended gathering, children wearing masks had a 9.7 increased likelihood of being seropositive compared to 1.02 odds for children not wearing a mask (Manny et al., 2020).
Specific interventions that have been implemented in schools during the COVID-19 pandemic include organizational policies to make contacts safe (e.g., face mask, hand hygiene, physical distancing policies, alternating attendance); environmental measures (e.g., improved ventilation, school yard division, distance between desks); and surveillance approaches (e.g., testing, tracing, symptom screening, isolation, and quarantine) (Krishnaratne et al., 2020). Institutional policies are only effective when used consistently, and resources to implement more costly measures vary across schools. Masks are arguably a low-cost, high-impact strategy to mitigate transmission of SARS-Cov-2 among children both within and outside of school settings. Mask use is mandated in indoor settings including schools, in many jurisdictions across the US (Guzman-Cottrill et al., 2021) and Canada (Government of Canada, 2021), yet children spend a good proportion of their time engaged in activities where health policies cannot easily be enforced, e.g., during sports and leisure activities, recess, play dates, on route to and from school. In such instances, where there is less systematic oversight, wearing masks might be the only reliable strategy to prevent COVID-19 transmission when physical distancing is not possible. For example, a large survey conducted in the US with students aged 13–21, who attended school in person in 2020, found the percentage of students reporting wearing masks “all the time” was highest in classrooms, hallways, and stairwells (65%) compared to school buses (42%), restrooms (40%), and cafeterias (36%) with even lower rates reported during sports and extracurricular activities (28%) or while outside on school property (25%) (Arvelo et al., 2021). Another study showed that among US individuals 13 years and older, 85% were “likely to wear a mask at grocery store”, while only 40% were “likely to wear a mask while visiting with family/friends at home” and 40% were “very likely to wear a mask to the grocery store and when visiting with family/friends” (Rader et al., 2021). A cross-sectional survey conducted in Wuhan, China with children aged 6–13 (N = 8569) found an increased likelihood of wearing a mask in school among grades 5 and 6 compared to grades 1 and 2, whereby roughly over half of all children reported “good mask behavior,” as per health guidelines recommendations (Chen et al., 2020). Lastly, a cross-sectional survey conducted in the US prior to school openings with parents/ guardians of school-aged children (N = 2202) found that parental support for mandatory mask mandates in schools varied as a function of child’s grade: 36.4% supported masks in kindergarten; 40.2% in grades 1–2; 48.0% in grades 3–5; 52.2% in grade >= 6 (Chua et al., 2020).
Pending mass vaccination campaigns for school-aged children, masks remain a key strategy for COVID-19 prevention. With children spending equal amounts of time within controlled school settings and outside of these settings, it is important to determine the individual-level factors that would promote compliance to mask use during activities without direct institutional or parental oversight. Parental attitudes, beliefs, and behaviors in support of children’s health behaviours have been shown to have a direct effect in children’s adoption and enactment of such behaviours, a process termed “parent-for-child” behavior (Hagger and Hamilton, 2019).
1.1. Conceptual model and study objective
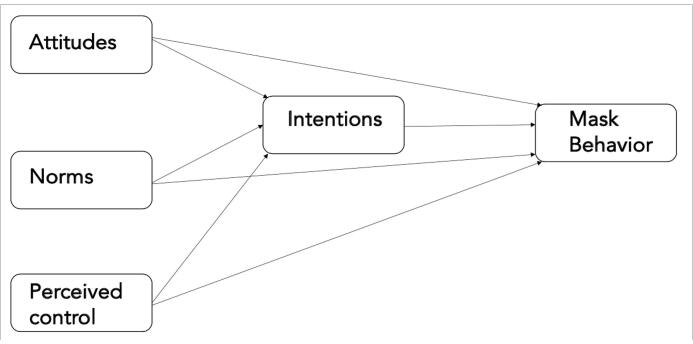
The Theory of Planned Behavior (TPB) (Ajzen, 1985) is a social-psychological theory designed to explain antecedents to behavioral intention and action, with a focus on attitudes (i.e., benefits and consequences of performing or not performing the behavior), subjective norms (i.e., desire to meet common norms regarding the behavior) and perceived control (i.e., personal capacity to perform the behavior and costs/constraints). A 2020 meta-analysis (N = 46 studies) investigating determinants of parent-for-child behaviors using the TPB model found that attitudes, norms and perceived control predicted parental enforcement of health behavior in children and these relationships were mediated by intentions (Hamilton et al., 2020). Few studies have used the TPB model to predict COVID-19 preventive behaviors, including social and physical distancing among general population samples in Bangladesh (Das et al., 2021) and Hong Kong (Yu et al., 2021) and intentions to wear masks among international students (Sun et al., 2021). To our knowledge, there are no studies that applied the TPB model to predict parent-for-child COVID-19 protective behaviors, such as mask wearing.
The objective of this study was to identify modifiable determinants of parent-for-child mask behavior using the Theory of Planned Behavior (Ajzen, 1985) to inform public health messaging about children’s mask wearing throughout the process of immunization against COVID-19.
2. Methods
2.1. Study design and procedures
We used a cross-sectional survey design and collected data online using the Qualtrics platform. The Institutional Research Board of the Harvard TH Chan School of Public Health granted ethics approval for the study (Protocol # IRB20-1140). The reporting of the study followed the STROBE guideline (von Elm et al., 2014) (see Supplementary Materials Table S1). The data are freely accessible at https://osf.io/y5xg9/. The study was advertised online via a paid Facebook advertisement ($100 CAD/day) between July 30, 2020 and August 10, 2020. Study eligibility included being an adult (18 years or older), a parent/caregiver of a school-aged child, and living in Canada or the US. Exclusion criteria included any of the following: being younger than 18 years of age, not being a parent or caregiver of a school-aged child, and not living in the US or Canada. The questionnaire is freely accessible at https://osf.io/y5xg9/.
2.2. Predictor variables
2.2.1. Sociodemographic information
Participants were asked to indicate their age, gender, ethnicity, country of residence, highest level of education completed, household income, work and health status, family size, self-perceived symptoms of COVID-19 over the previous week, and whether they were tested for COVID-19; and the demographic status of their youngest school-aged child, including age, gender, overall health status, and specific health conditions that might interfere with mask wearing (e.g., skin sensitivity).
2.2.2. Attitudes about children’s mask wearing in schools
Attitudes were assessed via three separate items (“I worry that wearing face masks in school could lead to disruptions in my child's daily activities”, “I worry that wearing face masks in school could lead to negative interactions with peers and teachers for my child”, and “I worry that wearing face masks in school could lead to my child having difficulty reading social cues”), which were scored on a 5-point Likert-type scale, ranging from 1 (not at all concerned) to 5 (very concerned). Higher scores indicated more negative attitudes. In the current sample, Cronbach’s alpha was 0.95.
2.2.3. Subjective norms about mask wearing among children
Norms about mask wearing were assessed via three items (e.g., “Masks should be worn all the time when in public and physical distancing is not possible”, “I believe that when used properly, face masks are effective at preventing transmission of the virus that causes COVID-19”, and “I believe the benefits of wearing face masks when in public outweigh the potential concerns”) which were scored on a 5-point Likert-type scale, ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicated increased acceptance of common norms about mask wearing. In the current sample, Cronbach’s alpha was 0.95.
2.2.4. Perceived control over mask wearing by children
Perceived control or self-efficacy for teaching mask wearing to children was assessed via three items (e.g., “I am confident I can teach my child how to wear and adjust a face mask”, “I will be able to provide my child with a face mask to wear to school every day”, and “I am confident I can explain to my child the benefits of wearing a face mask”) which were scored on a 5-point Likert-type scale, ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicated greater perceived control. In the current sample, Cronbach’s alpha was 0.89.
2.3. Outcome variables
2.3.1. Intentions to have children wear masks in schools
Intentions to have children wear masks in schools were assessed via a single item (“I intend to have my child wear a face mask at school”) which was assessed on a 5-point Likert-type scale, ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicated higher intentions.
2.3.2. Parent-for Child Mask behaviour
To assess children’s mask behavior in schools we used a single item (“When I take my child out in public, I insist they wear a face mask”) which was assessed on a 5-point Likert-type scale, ranging from 1 (none of the time) to 5 (all of the time), with an additional option available for those not leaving their homes (6 = I don’t go out). Higher scores indicated more frequent mask use among children. We opted to use this item to approximate children’s mask wearing behaviour in schools, because at the time of data collection, schools were not yet open, so the question could not be asked retrospectively.
2.4. Data analysis plan
Descriptive statistics (mean, standard deviation, percentages) were conducted in SPSS version 27. Structural equation modelling (SEM) analyses with ML bootstrapping with 500 iterations and 95% confidence intervals (CI) were conducted in AMOS version 25 (Arbuckle, 2017) to test the TPB model, including confirmatory factor analyses for the latent multi-item constructs (i.e., attitudes, subjective norms, and perceived control; See Fig. 1). We concurrently estimated 1) the associations between attitudes, subjective norms, perceived control, and intentions, 2) the direct effects of attitudes, subjective norms, perceived control, and intentions on mask behavior, and 3) the indirect effects of attitudes, subjective norms, and perceived control on mask behavior through intentions. A priori, we identified parent’s education and health status, youngest child’s age and health status, and country of residence (Canada versus US), as covariates for the model. The final model excluded country of residence from final model, as it was not associated with the outcomes (Becker, 2005, Spector and Brannick, 2011).
Fig. 1.
Visual Representation of The Theory of Planned Behavior Note. Attitudes (3 items) e.g., “I worry that wearing face masks in school could lead to disruptions in my child's daily activities”. Norms (3 items) e.g., “Masks should be worn all the time when in public and physical distancing is not possible”.Perceived control (3 items) e.g., “I am confident I can teach my child how to wear and adjust a face mask”. Intentions (1 item): “I intend to have my child wear a face mask at school”.Mask Behavior (1 item): “When I take my child out in public, I insist they wear a face mask”.
To assess model fit, we used the chi-square test, which is highly sensitive to sample size and potentially leading to erroneous rejection of the model fit (Reise et al., 1993), in tandem with a combination of other indices, i.e., the Tucker-Lewis Index (TLI; Tucker and Lewis, 1973), the Comparative Fit Index (CFI; Bentler, 1990) and the Root Mean Square Error of Approximation (RMSEA; Steiger, 1990). Good fitting models are indicated by a TLI and CFI ≥ 0.95 and RMSEA ≤ 0.06 (Hu and Bentler, 1999), whereas adequate model fit is indicated by a CFI and TLI ≥ 0.90 or above (Kline, 2005) and a RMSEA ≤ 0.08 (Browne and Cudeck, 1993). The strength of the individual paths (expressed via standardized regression coefficients or β) was reported using Cohen’s guidelines for small (SD ≤ 0.20), moderate (SD ≤ 0.50) and large (SD ≤ 0.80) effect sizes (Cohen, 1988).
2.4.1. Post-hoc Multi-Group Analyses
Given preliminary descriptive analyses that revealed approximately 50% of our participants had children with at least one pre-existing health condition that would make mask wearing difficult, we examined the TPB model among the two subsets of parents. We evaluated the model fit for each subgroup and compared path coefficients between groups using z-tests with a Bonferroni correction (Meyers et al., 2016).
3. Results
3.1. Recruitment and sample characteristics
Data were collected from 869 participants but 170 participants who completed<50% of the survey and/or had missing values for any variables used in the model were excluded. Therefore, analyses were conducted with 699 participants with non-missing data on all variables tested in the model. Among the total sample, 94.7% were females (mothers) with a mean age of 44.4 (+/- 8.4) years old, 84.0% had completed college or university, and 83.7% were married or in a common-law relationship. A total of 54.1% of parents reported having a female youngest child of school age and 43.5% reported their child having a pre-existing condition that might interfere with mask wearing. The most frequently reported pre-conditions included allergies (20.9%), anxiety (20.7%), impulsivity (19.7%), skin sensitivity (16.3%), and asthma (12.7%). Demographic sample characteristics are included in Table 1.
Table 1.
Sample Characteristics.
| Variable | Full sample (N = 699) | Children without pre-conditions (N = 304) | Children withpre-conditions (N = 395) |
|---|---|---|---|
| PARENTS | |||
| Country, n (%) | |||
| USA | 341 (48.8) | 164 (53.9) | 177 (44.8) |
| Canada | 358 (51.2) | 140 (46.1) | 218 (55.2) |
| Age, M (SD) | 44.39 (8.41) | 44.45 (8.31) | 44.34 (8.50) |
| Gender, n (%) | |||
| Male | 28 (4.0) | 15 (4.9) | 13 (3.3) |
| Female | 662 (94.7) | 283 (93.1) | 379 (95.9) |
| Non-binary | 6 (0.8) | 4 (1.3) | 2 (0.5) |
| Other | 1 (0.1) | 0 (0.0) | 1 (0.3) |
| Missing | 2 (0.3) | 2 (0.7) | 0 (0.0) |
| Education, n (%) | |||
| Highschool | 85 (12.2) | 30 (9.9) | 55 (13.9) |
| Trade school | 27 (3.9) | 8 (2.6) | 19 (4.8) |
| College | 229 (32.8) | 100 (32.9) | 129 (32.7) |
| University | 358 (51.2) | 166 (54.6) | 192 (48.6) |
| Marital status, n (%) | |||
| Single | 47 (6.7) | 17 (5.6) | 30 (7.6) |
| In a relationship or common-law | 58 (8.3) | 21 (6.9) | 37 (9.4) |
| Married | 527 (75.4) | 245 (80.6) | 282 (71.4) |
| Separated/divorced | 52 (7.4) | 17 (5.6) | 35 (8.9) |
| Widowed | 13 (1.9) | 3 (1.0) | 10 (2.5) |
| Missing | 2 (0.3) | 1 (0.3) | 1 (0.3) |
| Household income, n (%) | |||
| < $44,999 | 100 (15.1) | 33 (10.9) | 67 (17.0) |
| 45,000-$49,999 | 26 (3.7) | 7 (2.3) | 19 (4.8) |
| $50,000-$54,999 | 31 (4.4) | 9 (3.0) | 22 (5.6) |
| $55,000-$59,999 | 17 (2.4) | 7 (2.3) | 10 (2.5) |
| $60,00-$64,999 | 30 (4.3) | 16 (5.3) | 14 (3.5) |
| $65,000-$69,999 | 17 (2.6) | 9 (3.0) | 8 (2.0) |
| $70,000-$74,999 | 36 (5.2) | 12 (3.9) | 24 (6.1) |
| $75,000-$79,999 | 39 (5.6) | 18 (5.9) | 21 (5.3) |
| >$80,000 | 366 (52.4) | 170 (55.9) | 196 (49.6) |
| Missing | 37 (5.3) | 23 (7.6) | 14 (3.5) |
| Ethnicity, n (%)* | |||
| Asian | 14 (2.0) | 8 (2.6) | 6 (1.5) |
| Black or African American | 3 (0.4) | 3 (1.0) | 0 (0.0) |
| Hispanic | 25 (3.6) | 7 (2.3) | 18 (4.6) |
| Indigenous/Alaskan Native | 16 (2.3) | 5 (1.6) | 11 (2.8) |
| Middle Eastern or North African | 6 (0.9) | 2 (0.7) | 4 (1.0) |
| Pacific Islander | 2 (0.2) | 1 (0.3) | 1 (0.3) |
| White | 636 (91.0) | 295 (97.0) | 359 (90.9) |
| Missing | 26 (3.7) | 11 (3.6) | 15 (3.8) |
| Self-reported health status, n (%) | |||
| Poor | 11 (1.6) | 1 (0.3) | 10 (2.5) |
| Fair | 81 (11.6) | 17 (5.6) | 64 (16.2) |
| Good | 236 (33.8) | 93 (30.6) | 143 (36.2) |
| Very good | 236 (33.8) | 107 (35.2) | 129 (32.7) |
| Excellent | 135 (19.3) | 86 (28.3) | 49 (12.4) |
| YOUNGEST CHILD | |||
| Age, M (SD) | 9.43 (3.80) | 9.19 (3.75) | 9.63 (3.83) |
| Gender, n (%) | |||
| Male | 317 (45.4) | 136 (44.7) | 181 (45.8) |
| Female | 378 (54.1) | 166 (54.6) | 212 (53.7) |
| Non-binary | 2 (0.3) | 1 (0.3) | 1 (0.3) |
| Missing | 2 (0.3) | 1 (0.3) | 1 (0.3) |
| Type of school, n (%) | |||
| Public school | 591 (84.5) | 253 (83.2) | 338 (85.6) |
| Private school | 76 (10.9) | 40 (13.2) | 36 (9.1) |
| Homeschool | 4 (0.6) | 2 (0.7) | 2 (0.4) |
| Missing | 29 (4.0) | 9 (3.0) | 19 (4.8) |
| Parent-reported health status, n (%) | |||
| Poor | 1 (0.1) | 0 (0.0) | 1 (0.3) |
| Fair | 31 (4.4) | 1 (0.3) | 30 (7.6) |
| Good | 131 (18.7) | 28 (9.2) | 103 (26.1) |
| Very good | 238 (34.0) | 92 (30.3) | 146 (37.0) |
| Excellent | 298 (42.6) | 183 (60.2) | 115 (29.1) |
| Pre-existing conditions, n (%)* | |||
| Allergies | 146 (20.9) | – | 146 (20.9) |
| Anxiety | 145 (20.7) | – | 145 (20.7) |
| Impulsivity | 138 (19.7) | – | 138 (19.7) |
| Skin Sensitivity | 114 (16.3) | – | 114 (16.3) |
| Asthma | 89 (12.7) | – | 89 (12.7) |
| Body Image | 35 (5.0) | – | 35 (5.0) |
| Difficulty Breathing | 29 (4.1) | – | 29 (4.1) |
| Difficulty reading facial expressions | 29 (4.1) | – | 29 (4.1) |
| Hearing difficulties | 20 (2.9) | – | 20 (2.9) |
| Difficulty recognizing others | 9 (1.3) | – | 9 (1.3) |
| Immunity disorder | 9 (1.3) | – | 9 (1.3) |
| Mobility Issues | 8 (1.1) | – | 8 (1.1) |
| Autism | 8 (1.1) | – | 8 (1.1) |
| Difficulty reading lips | 7 (1.0) | – | 7 (1.0) |
| Speech Learning Disorder | 7 (1.0) | – | 7 (1.0) |
| Neuro Special Needs | 6 (0.9) | – | 6 (0.9) |
| Depression | 2 (0.3) | – | 2 (0.3) |
Note. *Percentages do not equal 100% because the question asked participants to check all options that apply.
3.2. Predictors of Parent-for-Child mask behavior using the Theory of Planned behaviour
Descriptive statistics for the study measures are included in Table 2. Results of the SEM analysis are included in Table 3. The model fit was acceptable for the analysis conducted across the full sample. Additional model fit indices provided by the software but not included in the model fit evaluation are included in Supplementary Table S2.
Table 2.
Descriptive Statistics for the Study Measures.
| Variable | Full sample(N = 699) | Children without pre-conditions (N = 304) | Children with pre-conditions(N = 395) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| M (SD) | Factor loading | 95% CI | M (SD) | Factor loading | 95% CI | M (SD) | Factor loading | 95% CI | |
| Attitudesa | |||||||||
|
2.75 (1.59) | 0.93 | 0.91, 0.95 | 2.88 (1.64) | 0.94 | 0.91, 0.96 | 2.65 (1.54) | 0.92 | 0.90, 0.94 |
|
2.61 (1.63) | 0.95 | 0.93, 0.96 | 2.76 (1.65) | 0.97 | 0.94, 0.98 | 2.49 (1.60) | 0.94 | 0.91, 0.96 |
|
2.81 (1.52) | 0.90 | 0.88, 0.92 | 2.92 (1.56) | 0.93 | 0.91, 0.95 | 2.73 (1.48) | 0.88 | 0.83, 0.90 |
| Subjective normsb | |||||||||
|
3.64 (1.58) | 0.94 | 0.92, 0.96 | 3.32 (1.68) | 0.95 | 0.93, 0.97 | 3.89 (1.47) | 0.93 | 0.89, 0.95 |
|
3.49 (1.41) | 0.89 | 0.86, 0.91 | 3.23 (1.48) | 0.90 | 0.85, 0.93 | 3.69 (1.32) | 0.88 | 0.83, 0.91 |
|
3.59 (1.57) | 0.95 | 0.93, 0.97 | 3.34 (1.68) | 0.96 | 0.92, 0.98 | 3.77 (1.45) | 0.95 | 0.93, 0.97 |
| Perceived controlb | |||||||||
|
3.99 (1.29) | 0.79 | 0.74, 0.84 | 3.79 (1.34) | 0.78 | 0.71, 0.84 | 4.14 (1.23) | 0.79 | 0.71, 0.84 |
|
3.78 (1.31) | 0.84 | 0.81, 0.87 | 3.63 (1.34) | 0.87 | 0.83, 0.91 | 3.89 (1.27) | 0.82 | 0.75, 0.87 |
|
3.76 (1.45) | 0.93 | 0.91, 0.95 | 3.48 (1.55) | 0.95 | 0.92, 0.97 | 3.98 (1.33) | 0.92 | 0.88, 0.95 |
| Intentions | |||||||||
|
3.52 (1.76) | 3.24 (1.84) | 3.74 (1.67) | ||||||
| Mask Behavior | |||||||||
|
3.46 (1.58) | 3.23 (1.65) | 3.64 (1.51) | ||||||
Note. M = mean; SD = standard deviation; CI = confidence intervals for factor loadings, bootstrapped.
Measured with five-point Likert scale ranging from 1 (not at all) to 5 (very worried)
Measured with five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree)
Measured with a five-point Likert scale ranging from 1 (none of the time) to 5 (all of the time).
Table 3.
Predictors of Parental Intentions to Have Children Wear Masks in Schools and Mask Wearing Behavior.
| Variable | Full sample(N = 699) | Children withoutpre-conditions(N = 304) | Children withpre-conditions(N = 395) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | |
| Predictors of Intentions | |||||||||
| Attitudes | -0.20 | -0.29, -0.11 | 0.006 | -0.23 | -0.38, -0.09 | 0.005 | -0.19 | -0.30, -0.07 | 0.012 |
| Norms | 0.41 | 0.26, 0.57 | 0.002 | 0.40 | 0.17, 0.60 | 0.003 | 0.42 | 0.19, 0.65 | 0.007 |
| Perceived control | 0.33 | 0.17, 0.49 | 0.006 | 0.31 | 0.11, 0.55 | 0.003 | 0.34 | 0.06, 0.56 | 0.015 |
| Direct Effects on Mask Behavior | |||||||||
| Attitudes | -0.07 | -0.21, 0.08 | 0.398 | -0.19 | -0.40, -0.01 | 0.035 | 0.01 | -0.20, 0.18 | 0.970 |
| Norms | 0.50 | 0.32, 0.68 | 0.004 | 0.72 | 0.45, 0.97 | 0.006 | 0.28 | 0.06, 0.54 | 0.019 |
| Perceived control | -0.03 | -0.22, 0.16 | 0.711 | -0.20 | -0.49, 0.04 | 0.095 | 0.12 | -0.15, 0.38 | 0.348 |
| Intentions | 0.28 | 0.14, 0.42 | 0.003 | 0.14 | -0.05, 0.33 | 0.194 | 0.39 | 0.21, 0.56 | 0.003 |
| Indirect Effects on Mask Behavior | |||||||||
| Attitudes | -0.06 | -0.10, -0.02 | 0.003 | -0.04 | -0.12, 0.00 | 0.053 | -0.08 | -0.15, -0.03 | 0.006 |
| Norms | 0.11 | 0.06, 0.19 | 0.001 | 0.07 | 0.00, 0.18 | 0.042 | 0.17 | 0.07, 0.31 | 0.004 |
| Perceived control | 0.09 | 0.04, 0.17 | 0.002 | 0.06 | -0.00, 0.16 | 0.055 | 0.13 | 0.03, 0.25 | 0.016 |
| Overall Model Fit Indices | |||||||||
| X2 (DF), p | 305.01 (61) | < 0.001 | 168.32 (61) | < 0.001 | 227.26 (61) | < 0.001 | |||
| CFI | 0.97 | 0.98 | 0.96 | ||||||
| TLI | 0.95 | 0.96 | 0.94 | ||||||
| RMSEA | 0.08 | 0.08 | 0.08 | ||||||
Note. Analyses included the following covariates: child age, child health status, parent education, parent health status.
β = standardized regression coefficient; CI = confidence intervals; Χ2 = Chi-squared statistic; DF = degrees of freedom; CFI = Comparative Fit Index; TLI = Tucker Lewis Index; RMSEA = Root Mean Square Error of Approximation. Analyses included the following covariates: child age, child health status, parent education, parent health status, parent mask behavior. Direct effects = associations between the 3 predictors and the outcome. Indirect effects = association between the 3 predictors and the outcome through Intentions.
Negative attitudes (β = -0.20, p = .006), norms (β = 0.41, p = .002), and perceived control (β = 0.33, p = .006) were significantly associated with intentions. The magnitude of these associations was “small” for attitudes and “moderate” for norms and perceived control. We found “moderate” direct effects of norms (β = 0.50, p = .004) and intentions (β = 0.28, p = .003) on mask behavior. There was no direct effect of attitudes or perceived control on mask behavior. We also found “small” indirect effects (i.e., mediated by intentions), of attitudes (β = -0.06, p = .003), norms (β = -0.11, p = .001), and perceived control (β = -0.09, p = .002) on mask behavior.
3.3. Subgroup analyses among parents of children without and with Pre-existing conditions
The model fit indices were comparable across both groups (see Table 3). Detailed subgroup analyses are included in Table 3. Among parents of children without pre-conditions (n = 304), attitudes, norms and perceived control were significantly associated with intentions; attitudes and norms had a direct effect on mask behavior, but perceived control and intentions did not; and there were no indirect effects (i.e., through intentions) on mask behavior.
Among parents of children with pre-conditions (n = 395), attitudes, norms and perceived control were significantly associated with intentions; intentions and norms had a direct effect on mask behavior, but attitudes and perceived control did not; attitudes, norms, and perceived control also had a “small” indirect effect (i.e., through intentions) on mask behavior. Post-hoc pairwise comparisons of path coefficients using a Bonferroni corrected α = 0.013 found that the path from norms to mask behavior was significantly stronger in the group without pre-conditions (β = 0.72, p = .006) compared to the group with pre-conditions (β = 0.28, p = .019), z = -2.99, p = .001.
4. Discussion
In the current study we used a theoretical model of health behavior change, i.e., the Theory of Planned Behavior (TPB) (Ajzen, 1985) and structural equation modelling to estimate predictors of parent-for-child mask wearing behavior. We found that positive attitudes about masks, positive beliefs about mask effectiveness (or norms), and higher confidence in modelling mask behavior to children (or perceived control) were associated with higher parental intentions to have children wear masks. Norms and intentions were also associated with parental enforcement of mask wearing among children (or parent-for-child mask behavior), but attitudes and perceived control were not. Lastly the individual relationships between attitudes, norms, perceived control, respectively, and mask behavior were mediated by intentions. This suggests that while holding positive attitudes about mask wearing, positive beliefs about mask effectiveness, and having a sense of efficacy over how to teach children to wear masks are important constructs, ultimately their impact on parent-for-child mask behavior is heavily influenced by parents’ intentions to have children wear masks.
Subgroup analyses of parents with children with pre-conditions that affect mask wearing and parents of children without pre-conditions showed a more nuanced view of the main results. It appears that for parents of children without pre-conditions (i.e., healthy children) norms or holding positive beliefs about mask effectiveness have the largest impact on parent-for-child mask use, as there are arguably fewer foreseeable barriers to their children’s mask use. Conversely, for parents of children with pre-conditions, intentions are the main drivers of parent-for-child mask use, beyond the impact of attitudes, norms, and perceived control. It seems reasonable to assume that enforcing mask use among children with pre-conditions is a more complex and challenging process, which involves the need for intentional planning, in addition to holding positive attitudes, positive norms and having higher perceived control.
Previous studies, which applied the Theory of Planned Behavior Model to predict preventive behaviours during the COVID-19 pandemic, found that attitudes, perceived control and social norms were associated with increased mask wearing among international students enrolled at Chinese universities (Sun et al., 2021); positive attitudes (but not negative), perceived control and social norms were associated with increased social and physical distancing behaviours among general population adults living in Hong Kong (Yu et al., 2021). Another study found that intentions mediated the relationship between attitudes and social distancing behavior and perceived control and behavior, respectively, among an adult general population sample recruited from Bangladesh (Das et al., 2021). Similar to the current project, previous studies used cross-sectional designs and convenience samples primarily recruited on social media. Our study adds to this small body of literature by providing a viewpoint on parents’ approach to children’s mask wearing, most importantly about the mediative role of intention in the link between attitudes, norms, perceived control, and parent-for-child mask wearing.
Prior literature has also shown that parents of school-aged children have concerns about potential harms of mask wearing to the health and socio-emotional development of children (e.g., masks potentially preventing adequate communication in the classroom, blocking emotional signaling between teachers and children) (Spitzer, 2020). Parental concerns about children’s mask use may be magnified among parents of children with pre-existing health conditions (Esposito et al., 2020). Given the large number of parents with children with pre-conditions in our study (44%), we were able to conduct subgroup analyses and uncovered different pathways predicting parental enforcement of mask wearing among two subsets of children.
4.1. Limitations
First, this study used a cross sectional design which limits our ability to make longitudinal or causal predictions. Although we hypothesized the relationships between our variables using the Theory of Planned Behavior and modelled our paths using structural equation modelling, with our design it was not possible to test causal relationships between the variables, as one would with a longitudinal design. Second, we used a convenience sample, composed primarily of women, which included a significant proportion of parents of children with pre-conditions reported by parents as potentially interfering with mask wearing. The characteristics of our sample might limits the generalizability our results. Third, we collected these data in August 2020 prior to the beginning of the 2020 fall semester, when vaccines were not available for adults and there was no foreseeable plan for vaccine trials in children. Despite the time lag between data collection and publication, our results are applicable to the current climate, given the ongoing need to wear masks in public. Last, we assessed our constructs with items created ad-hoc for this study, as there were no COVID-19 specific measures available at the time we started data collection. Real-time rates of children’s mask wearing in schools could not be measured in this study, as schools had not been opened at the time of data collection.
4.2. Future directions and implications
Future research should cross-validate these findings in studies conducted with more diverse samples, particularly individuals from marginalized groups, people of color, and those financially disadvantaged, studies with longitudinal designs that ideally assess real-life mask behaviors among children. The challenge remains on how to improve children’s mask wearing while not directly supervised by parents or when supervised by teachers in classroom settings. Children spend a lot of time unsupervised with many not wearing masks consistently while in school but without close supervision or reminders from adults. This suggests that interventions are needed to boost parental attitudes, beliefs, and behaviors relative to masks, such as those assessed herein, which could act as motivators (or drivers) for children’s mask wearing in multiple settings, not just in the classroom. Last, we suggest that mask-wearing has to be more of a societal, collective decision made by parents so that children’s mask wearing is not limited only to classroom situations.
5. Data availability
Data can be downloaded from the Open Science Framework: https://osf.io/y5xg9/
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. AC is supported by post-doctoral research fellowships from the Canadian Institutes of Health Research (CIHR) and Fonds de Recherche du Quebec – Santé (FRQS). CM is supported by doctoral awards from Vanier Canada, Killam Trusts, and Alberta Innovates, and a Training in Research and Clinical Trials in Integrative Oncology (TRACTION) fellowship from the University of Calgary. BL is supported by a Social Sciences and Humanities Research Council (SSHRC) doctoral scholarship.
CRediT authorship contribution statement
Adina Coroiu: Conceptualization. Chelsea Moran: Conceptualization. Brittany L. Lindsay: . Alan C. Geller: Conceptualization.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2021.101533.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Ajzen I. In: Action control: From cognition to behavior. Kuhl J., Beckmann J., editors. Springer; Berlin Heidelberg, Berlin, Heidelberg: 1985. From intentions to actions: A theory of planned behavior; pp. 11–39. [Google Scholar]
- Arbuckle, J.L., 2017. Amos (version 25.0, spss). IBM, Chicago, IL.
- Arvelo W., Fahrenbruch M., Hast M., Puddy R. Covid-19 stats: Percentage of middle and high school students aged 13–21 years attending in-person classes who reported observing fellow students wearing a mask all the time, by school setting and activity—united states, october 2020. MMWR Morb Mortal Wkly Rep. 2021;70:223. doi: 10.15585/mmwr.mm7006a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker T.E. Potential problems in the statistical control of variables in organizational research: A qualitative analysis with recommendations. Organ Res Methods. 2005;8(3):274–289. doi: 10.1177/1094428105278021. [DOI] [Google Scholar]
- Bentler P.M. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Browne M.W., Cudeck R. In: Testing structural equation models. Bollen K.A., Long J.S., editors. Sage; Newbury Park: 1993. Alternative ways of assessing fit; pp. 136–162. [Google Scholar]
- Chen X., Ran L.i., Liu Q., Hu Q., Du X., Tan X. Hand hygiene, mask-wearing behaviors and its associated factors during the covid-19 epidemic: A cross-sectional study among primary school students in wuhan, china. Int J Environ Res Public Health. 2020;17(8):2893. doi: 10.3390/ijerph17082893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schünemann H.J., Chu D.K., Akl E.A., El-harakeh A., Bognanni A., Lotfi T., Loeb M., Hajizadeh A., Bak A., Izcovich A., Cuello-Garcia C.A., Chen C., Harris D.J., Borowiack E., Chamseddine F., Schünemann F., Morgano G.P., Muti Schünemann G.E.U., Chen G., Zhao H., Neumann I., Chan J., Khabsa J., Hneiny L., Harrison L., Smith M., Rizk N., Giorgi Rossi P., AbiHanna P., El-khoury R., Stalteri R., Baldeh T., Piggott T., Zhang Y., Saad Z., Khamis A., Reinap M., Duda S., Solo K., Yaacoub S., Schünemann H.J. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of sars-cov-2 and covid-19: A systematic review and meta-analysis. The Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua K.-P., DeJonckheere M., Reeves S.L., Tribble A.C., Prosser L.A. Factors associated with school attendance plans and support for covid-19 risk mitigation measures among parents and guardians. Acad Pediatr. 2020;21(4):684–693. doi: 10.1016/j.acap.2020.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Ed. ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. Statistical power analysis for the behavioral sciences 2nd. [Google Scholar]
- Das, A.K., Abdul Kader Jilani, M.M., Uddin, M.S., Uddin, M.A., Ghosh, A.K., 2021. Fighting ahead: Adoption of social distancing in covid-19 outbreak through the lens of theory of planned behavior. Hum Behav Soc Environ:1-21. https://doi.org/10.1080/10911359.2020.1833804.
- Esposito S., Principi N., Leung C.C., Migliori G.B. Universal use of face masks for success against covid-19: Evidence and implications for prevention policies. Eur Respir J:2001260. 2020;55(6):2001260. doi: 10.1183/13993003.01260-202010.1183/13993003.01260-2020.Shareable1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Canada, 2021. Covid-19 guidance for schools kindergarten to grade 12.
- Guzman-Cottrill J.A., Malani A.N., Weber D.J., Babcock H., Haessler S.D., Hayden M.K., Henderson D.K., Murthy R., Rock C., Van Schooneveld T., Wright S.B., Forde C., Logan L.K. Local, state and federal face mask mandates during the covid-19 pandemic. Infect Control Hosp Epidemiol. 2021;42(4):455–456. doi: 10.1017/ice:2020.1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagger M.S., Hamilton K. In: and barriers to parenthood: Existential concerns regarding fertility, pregnancy, and early parenthood. Taubman – Ben-Ari, O. ., editor. Springer International Publishing; Cham: 2019. Health behavior, health promotion, and the transition to parenthood: Insights from research in health psychology and behavior change; pp. 251–269. [Google Scholar]
- Hamilton K., van Dongen A., Hagger M.S. An extended theory of planned behavior for parent-for-child health behaviors: A meta-analysis. Health Psychol. 2020;39(10):863–878. doi: 10.1037/hea0000940. [DOI] [PubMed] [Google Scholar]
- Hu L.-T., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Kline R.B. Ed. ed. Guilford Press; New York: 2005. Principles and practice of structural equation modeling 2nd. [Google Scholar]
- Krishnamachari B., Morris A., Zastrow D., Dsida A., Harper B., Santella A.J. The role of mask mandates, stay at home orders and school closure in curbing the covid-19 pandemic prior to vaccination. Am J Infect. 2021;49(8):1036–1042. doi: 10.1016/j.ajic.2021.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnaratne, S., Pfadenhauer, L.M., Coenen, M., Geffert, K., Jung-Sievers, C., Klinger, C., Kratzer, S., Littlecott, H., Movsisyan, A., et al., 2020. Measures implemented in the school setting to contain the covid‐19 pandemic: A rapid scoping review. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD013812. [DOI] [PMC free article] [PubMed]
- Manny, E., Carroll, A., Charlton, C., Robinson, J., Subbarao, P., Azad, M., Moraes, T., Turvey, S., Chikuma, J., et al., 2020. Increased mask use and fewer gatherings associated with lower sars-cov-2 seropositivity among young school-age children [pre-print]. SSRN. https://doi.org/10.2139/ssrn.3728570.
- Meyers L.S., Gamst G., Guarino A.J. Sage publications; 2016. Applied multivariate research: Design and interpretation. [Google Scholar]
- Rader B., White L.F., Burns M.R., Chen J., Brilliant J., Cohen J., Shaman J., Brilliant L., Kraemer M.U.G., Hawkins J.B., Scarpino S.V., Astley C.M., Brownstein J.S. Mask-wearing and control of sars-cov-2 transmission in the USA: A cross-sectional study. Lancet Digit Health. 2021;3(3):e148–e157. doi: 10.1016/S2589-7500(20)30293-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reise S.P., Widaman K.F., Pugh R.H. Confirmatory factor analysis and item response theory: Two approaches for exploring measurement invariance. Psychol Bull. 1993;114:552–566. doi: 10.1037/0033-2909.114.3.552. [DOI] [PubMed] [Google Scholar]
- Spector P.E., Brannick M.T. Methodological urban legends: The misuse of statistical control variables. Organ Res Methods. 2011;14(2):287–305. doi: 10.1177/1094428110369842. [DOI] [Google Scholar]
- Spitzer M. Masked education? The benefits and burdens of wearing face masks in schools during the current corona pandemic. Trends Neurosci Educ. 2020;20:100138–100238. doi: 10.1016/j.tine.2020.100138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger J.H. Structural model evaluation and modification: An interval estimation approach. Multivariate Behav Res. 1990;25(2):173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Sun Y., Qin B., Hu Z., Li H., Li X., He Y., Huang H. Predicting mask-wearing behavior intention among international students during covid-19 based on the theory of planned behavior. Ann Palliat Med. https:// 2021;10(4):3633–3647. doi: 10.21037/apm10.21037/apm-20-2242. [DOI] [PubMed] [Google Scholar]
- Tucker L.R., Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38(1):1–10. doi: 10.1007/BF02291170. [DOI] [Google Scholar]
- Vogel L. Have we misjudged the role of children in spreading covid-19? Can Med Assoc J. 2020;192(38):E1102–E1103. doi: 10.1503/cmaj.1095897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The strengthening the reporting of observational studies in epidemiology (strobe) statement: Guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- Yu, Y., Lau, J.T.F., Lau, M.M.C., 2021. Levels and factors of social and physical distancing based on the theory of planned behavior during the covid-19 pandemic among chinese adults. Transl Behav Med 146. https://doi.org/10.1093/tbm/ibaa146. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data can be downloaded from the Open Science Framework: https://osf.io/y5xg9/