Abstract
High sodium and low potassium intakes are associated with increased levels of blood pressure and risk of cardiovascular diseases. Assessment of habitual dietary habits are helpful to evaluate their intake and adherence to healthy dietary recommendations. In this study, we determined sodium and potassium food-specific content and intake in a Northern Italy community, focusing on the role and contribution of adherence to Mediterranean diet patterns. We collected a total of 908 food samples and measured sodium and potassium content using inductively coupled plasma mass spectrometry. Using a validated semi-quantitative food frequency questionnaire, we assessed habitual dietary intake of 719 adult individuals of the Emilia-Romagna region. We then estimated sodium and potassium daily intake for each food based on their relative contribution to the overall diet, and their link to Mediterranean diet patterns. The estimated mean sodium intake was 2.15 g/day, while potassium mean intake was 3.37 g/day. The foods contributing most to sodium intake were cereals (33.2%), meat products (24.5%, especially processed meat), and dairy products (13.6%), and for potassium they were meat (17.1%, especially red and white meat), fresh fruits (15.7%), and vegetables (15.1%). Adherence to a Mediterranean diet had little influence on sodium intake, whereas potassium intake was greatly increased in subjects with higher scores, resulting in a lower sodium/potassium ratio. Although we may have underestimated dietary sodium intake by not including discretionary salt use and there may be some degree of exposure misclassification as a result of changes in food sodium content and dietary habits over time, our study provides an overview of the contribution of a wide range of foods to the sodium and potassium intake in a Northern Italy community and of the impact of a Mediterranean diet on intake. The mean sodium intake was above the dietary recommendations for adults of 1.5–2 g/day, whilst potassium intake was only slightly lower than the recommended 3.5 g/day. Our findings suggest that higher adherence to Mediterranean diet patterns has limited effect on restricting sodium intake, but may facilitate a higher potassium intake, thereby aiding the achievement of healthy dietary recommendations.
Keywords: dietary intake, Mediterranean diet, potassium, public health, salt, sodium, sodium-to-potassium ratio
1. Introduction
Non-communicable diseases (NCDs) are the leading causes of death worldwide [1]. In particular, cardiovascular diseases (CVD) still represent the leading cause of death and disability [2], being responsible for more than 35% of all deaths in Italy [3]. Although effective preventive measures can be implemented; i.e., by controlling behavioral and metabolic factors, nutritional determinants represent the most significant risk factors, preceded exclusively by blood pressure [4,5,6,7].
The effect of dietary intakes of sodium and potassium on the regulation of blood pressure levels has been widely investigated [8]. Sodium and potassium have a fundamental role in the distribution of fluids inside and outside cells, and in osmolarity regulation. Differences in sodium and potassium concentrations are maintained by the specific permeability of cell membranes and by activity of transmembrane transporters such as Na/K-ATPase. In particular, potassium is an essential mineral that plays a primary role in several physiological mechanisms including transmission of electrical activity in muscle cells and nerve fibers [1,9]. In humans, an increase in potassium intake has been linked to decreasing blood pressure levels and stroke incidence, with an indication of a possible U-shape relationship with minimum risk at 3.5 g/day (i.e., 90 mmol/day) of potassium excretion [10,11]. Conversely, a decrease in sodium intake showed an approximately linear association with blood pressure levels [12], cardiovascular diseases [13], and stroke [14], with beneficial effects of sodium reduction in both subjects with and without hypertension [12,15,16].
In addition to CVD, blood pressure lowering has also been associated with a reduced risk of mild cognitive impairment [17]. There is growing evidence that a high salt intake is detrimental for cognition [18,19], thus a reduction in sodium together with an increase in potassium intake, plus other dietary interventions, may be helpful for dementia prevention [19,20,21]. For these reasons, the World Health Organization (WHO) has approved an action plan for reducing the costs of public health, one of which is to lower salt consumption by the population [22].
In Italy, few studies have estimated dietary sodium and potassium intakes at the population level. Findings from the Italian Total Diet Study 2001–2002 using a 7 day diary recall reported an average intake of 3.8 and 2.9 g/day for sodium and potassium, respectively [23]. More recently, a lower sodium intake has been reported, namely 2.3 and 1.9 g/day for men and women, respectively [24]. Nonetheless, these values are still higher than the recommended dietary intake (DRI) of 1.5 and 2.0 g/day, respectively, suggested by the Italian Society of Human Nutrition (SINU) [25] and the safe and adequate intake of 2.0 g/day for adults suggested by the European Food Safety Authority (EFSA) [26]. As regards potassium, a slight increase in its intake was seen in the past years, from 3.2 g/day and 2.8 g/day in men and women, respectively, during the Third Italian National Consumption Survey in 2005–2006 using a 3-day semi-structured diary [27], to 3.3 g/day and 3.0 g/day in men and women, respectively, during the Cardiovascular Epidemiology Observatory/Health Examination Survey (CUORE) in 2008–2012 using 24 h urine collection carried out by the Italian National Institute of Health [24]. However, the latest 2018–2019 data from the CUORE project conducted by the Italian National Institute of Health highlighted that the potassium intake of the Italian general adult population has fallen to 3.043 g/day for men and 2.561 g/day for women [28]. This highlights the importance of increasing potassium intake in order to meet the adequate intakes of 3.5 g/day or 3.9 g/day suggested by the EFSA and SINU, respectively [9,25].
The primary aim of the present study was to assess dietary intakes of sodium and potassium in a sample population from the Emilia-Romagna region in Northern Italy, and to evaluate how such intakes may be influenced by adherence to dietary patterns widely known to be beneficial to human health, namely those related to the Mediterranean diet.
2. Materials and Methods
2.1. Food Collection and Analysis
We measured the sodium and potassium content in food samples collected from markets and stores in Northern Italy, as previously described [29,30]. Briefly, we identified foods most frequently consumed in a typical Italian diet [31,32]. We selected relevant food items characterizing the Italian diet [33], with particular reference to the Emilia-Romagna Region using previous population-based studies addressing the dietary habits of subjects of this Northern Italy community [34,35].
We purchased selected food and beverages in two provinces of the Emilia-Romagna region, namely Modena and Reggio Emilia in the period of October 2016–February 2017. During sample handling, we tried to avoid metal cross-contamination using plastic food containers and plastic and stainless cutlery. We also used a food blender equipped with a stainless-steel blade. After homogenisation, we aliquoted 0.5 g portion (wet weight) into quartz containers previously washed with MilliQ water (MilliQPlus, Millipore, MA, USA) and HNO3. Sample digestion was performed using 10 mL solution (5 mL HNO3 + 5 mL H2O) in a microwave system (Discover SP-D, CEM Corporation, NC, USA). Digested material was stored in plastic tubes and diluted to 50 mL with deionised water before analysis. We measured the sodium and potassium concentration using an inductively coupled plasma-mass spectrometer (Agilent 7500ce, Agilent Technologies, Santa Clara, CA, USA). All analyses were performed in duplicate, implementing standard quality controls as previously described [36,37]. A total of 908 food study samples were analyzed. Limits of quantification were 0.02 and 0.10 mg/kg for sodium and potassium, respectively, with corresponding limits of detection (LOD) of 0.01 and 0.05 mg/kg. Values for 35 and 9 samples for sodium and potassium, respectively, were below the LOD and were set equal to LOD/2 [38].
2.2. Study Population and Assessment of Dietary Habits
We assessed habitual dietary intakes of a Northern Italy community in the period 2005–2006. We identified a large population sample from the databases of the Emilia-Romagna Region–National Health Service directories of five provinces (Bologna, Ferrara, Modena, Parma and Reggio Emilia). Inclusion criteria were age > 18 years, and residence in one of the studied provinces. From the random sample of 2825 eligible subjects invited to participate, a total of 747 subjects accepted (response rate of 26.4%), and were therefore recruited. The study was authorized by the Modena Ethics Committee (approval no. 71.11/2011). All participants provided written informed consent and returned study material for collection of individual characteristics.
To estimate dietary habits, we administrated the food frequency questionnaires (FFQ) implemented within the ‘European Prospective Investigation into Cancer and Nutrition’ project. The EPIC-FFQ is a validated semi-quantitative FFQ, and we used the version specifically developed for the population of Northern Italy [39]. Frequency and amount of consumption of 188 food items were estimated over the previous year. Accurate completion by participants was ensured through photos of foods and serving sizes. For quality data control, we excluded incomplete FFQs or those reporting extreme and implausible values of energy intake; i.e., <0.5th or >99.5th percentile, based on the ratio of total energy intake to calculated basal metabolic rate, which excluded 28 subjects [40]. The final study sample was 719 adult participants, including 319 men and 400 women, none of whom reported ‘special’ dietary requirements or habits such as weight control or vegetarian/vegan diet during the survey. We eventually estimated daily dietary intake (mg/day) as previously reported by multiplying the quantity of sodium and potassium in foods (mg/kg food as consumed) with the corresponding food intake determined from the FFQ (in g/day) [41] and we calculated the sodium-to-potassium (Na/K) ratio. For daily dietary intakes, we also performed stratified analysis by sex and by adherence to the Italian Mediterranean Index (IMI) [42], and to the Mediterranean–DASH Intervention for Neurodegenerative Delay (MIND) pattern, which combines the Dietary Approach to Stop Hypertension (DASH) and the Mediterranean diet, with the aim of reducing the risk of dementia [43,44]. We used frequency and quantity of food and beverage intake as assessed through the EPIC-FFQ to evaluate the adherence to the investigated dietary patterns. In particular, we implemented specifically developed routines for the scoring system of both the IMI and MIND diets.
The Italian Mediterranean Index (IMI) was developed by the Epidemiology and Prevention Unit of the Milan National Cancer Institute [45] by adapting the Greek Mediterranean Index to typical Italian eating behavior. The score is based on intake of 11 items: 6 typical Mediterranean foods or food groups (pasta; typical Mediterranean vegetables such as raw tomatoes, leafy vegetables, onion and garlic, salad, and fruiting vegetables; fruit; legumes; olive oil; and fish), 4 non-Mediterranean foods (soft drinks, butter, red meat, and potatoes), and alcohol consumption. One point was given for consumption of each typical Mediterranean food in the upper tertile of the distribution, and for consumption of each non-Mediterranean food in the bottom tertile; all other dietary components received 0 points. Alcohol received 1 point for intake up to 12 g/day; abstainers and persons who consumed >12 g/day did not receive any points. The range of possible scores was 0–11. Similarly, the MIND pattern has 15 components, including 10 brain-healthy food groups (green leafy vegetables, other vegetables, nuts, berries, beans, whole grains, white meat (fish and poultry), olive oil instead of other oil, and wine-intake limitation), as well as a decrease in 5 unhealthy food groups, including red meats, butter and stick margarine, cheese, pastries and sweets, and fried/fast food. Scores range from 0 to 15, with higher values meaning greater adherence [46]. Additional general guidelines for the MIND diet are consuming at least three servings of whole grains, a salad and one other vegetable, and a glass of wine each day. In addition, nuts are used as a snack on most days and beans every other day. Poultry and berries are recommended at least twice a week and fish at least once a week. It is essential to limit the intake of the MIND diet’s “unhealthy food groups”, especially butter (less than 1 tablespoon a day), cheese, and fried or fast food (less than a serving a week for any of the three) [46]. For both diets, we used the mean value as cutpoint for identification of poor and high adherence.
We checked the normal distribution of variables using the Shapiro–Wilk test, and we used a t-test for independent samples to compare differences between means. We used linear regression analysis to investigate the relation between the Na/K ratio and adherence score to both IMI and MIND patterns, adjusting for age, sex, body mass index, and energy intake. We reported beta regression coefficients and values of the predicted Na/K ratio together with their 95% confidence intervals (CI). We used Stata statistical package (v17.1 Stata Corp., College Station, TX, USA, 2021) for all statistical analyses.
3. Results
Characteristics of the study participants are reported in Table 1. Out of the total 719 included participants, there were 319 men, median age 60 (interquartile range-IQR: 50–69) years and 400 women, median age 53 (IQR: 41–63) years. Nearly half of the participants had educational attainment of high school or more, and the vast majority lived with partners (married or unmarried). Body mass index distribution showed a general tendency to overweight with a median value of 25.1. The median energy intake was 1907 kcal/day, higher in men (2025 kcal/day) than in women (1801 kcal/day). Adherence to the Italian Mediterranean Index was moderate with approximately 60% of subjects having a score equal or above the median value of 4, and a similar higher proportion of subjects appeared to adhere to MIND pattern, with a mean score of 7.5. Mean intake of specific food categories demonstrated comparable dietary habits in both sexes, except for a slightly lower consumption of cereal products (206.4 g/day vs. 174.2 g/day), meat (142.4 g/day vs. 117.2 g/day) and beverages (mainly due to wine: 191.4 g/day vs. 73.9 g/day) in women, while men had a lower consumption of milk and yogurt (159.4 g/day vs. 212.5 g/day), coffee and tea (120.6 g/day vs. 170.6 g/day) and a slightly lower intake of vegetables (154.1 g/day vs. 161.4 g/day) and citrus fruits (207.0 g/day vs. 223.8 g/day) (Supplementary Table S1).
Table 1.
Characteristics of study participants. Number (percentage-%) reported when not otherwise indicated and median and interquartile range (IQR).
| All Subjects | Men | Women | ||||
|---|---|---|---|---|---|---|
| Characteristics | N | (%) | N | (%) | N | (%) |
| Overall | 719 | (100) | 319 | (44.4) | 400 | (55.6) |
| Age (years) | ||||||
| Median (IQR) | 57 | (43–67) | 60 | (50–69) | 53 | (41–63) |
| <65 years | 499 | (69.4) | 190 | (59.6) | 309 | (77.2) |
| ≥65 years | 220 | (30.6) | 129 | (40.4) | 91 | (22.8) |
| Education (years) | ||||||
| ≤5, primary school or less | 170 | (23.6) | 86 | (27.0) | 84 | (21.0) |
| 6–8, middle school | 178 | (24.8) | 86 | (27.0) | 92 | (23.0) |
| 9–13, high school | 268 | (37.3) | 101 | (31.7) | 167 | (41.7) |
| ≥14, college or more | 103 | (14.3) | 46 | (14.4) | 57 | (14.3) |
| Marital status | ||||||
| Married/unmarried partner | 493 | (68.6) | 239 | (74.9) | 254 | (63.5) |
| Unmarried/single | 104 | (14.5) | 42 | (13.2) | 62 | (15.5) |
| Divorced | 48 | (6.7) | 18 | (5.6) | 40 | (7.5) |
| Widowed | 74 | (10.3) | 20 | (6.3) | 54 | (13.5) |
| Body mass index (kg/m2) | ||||||
| Median (IQR) | 25.1 | (22.7–27.8) | 26.1 | (24.2–28.7) | 24.1 | (21.6–27.0) |
| ≤19 | 45 | (6.3) | 3 | (0.9) | 42 | (10.5) |
| 20–24 | 306 | (42.6) | 116 | (36.4) | 190 | (47.5) |
| 25–29 | 287 | (39.9) | 162 | (50.8) | 125 | (31.2) |
| ≥30 | 81 | (11.3) | 38 | (11.9) | 43 | (10.8) |
| Energy (kcal/day) Median (IQR) | 1907 | (1538–2364) | 2025 | (1650–2463) | 1801 | (1456–2296) |
| Italian Mediterranean Index | ||||||
| Median (IQR) | 4 | (3–5) | 4 | (3–5) | 4 | (3–5) |
| <4 | 275 | (38.2) | 129 | (40.4) | 146 | (36.5) |
| ≥4 | 444 | (61.8) | 190 | (59.6) | 254 | (63.5) |
| MIND pattern | ||||||
| Median (IQR) | 7.5 | (6.5–8.5) | 7.5 | (6.5–8.5) | 7.5 | (7.0–8.5) |
| <7.5 | 288 | (40.1) | 144 | (45.1) | 144 | (36.0) |
| ≥7.5 | 431 | (59.9) | 175 | (54.9) | 256 | (64.0) |
The average sodium and potassium content of food is reported in Table 2. The highest sodium levels were found in processed meat (12.0 g/kg); fish and seafood, especially preserved and tinned fish (13.0 g/kg); followed by bread, rolls, and other prepackaged cereals and salty snacks (5.4 and 6.2 g/kg, respectively). In addition, cheese (5.2 g/kg), butter, and other animal fats (3.7 g/kg) showed a higher sodium content compared to milk (4.4 g/day) and vegetable/olive oils (<0.3 g/kg), respectively. Conversely, the highest potassium levels were found in legumes (10.0 g/kg); dry fruits (7.2 g/kg); followed by meat, especially white meat (5.3 g/kg); mushrooms (5.1 g/kg); vegetables (3.1 g/kg); and potatoes (4.1 g/kg). Food containing lower sodium levels were fresh fruits (14.8 mg/kg), followed by almost all beverages (35.4 mg/kg), while rice demonstrated the lowest value (8.0 mg/kg) compared to other cereal products. Lower levels of potassium were found in almost all dairy products (1.2 g/kg), beverages (0.5 g/kg), and oils and fats (0.1 g/kg).
Table 2.
Average content (mg/kg wet weight) of sodium (Na) and potassium (K) in foods and number (%) of samples below the limit of detection (LOD).
| Sodium | Potassium | |||||||
|---|---|---|---|---|---|---|---|---|
| Food 1 | N | Mean Na | <LOD (N) |
<LOD (%) | Mean K | <LOD (N) |
<LOD (%) |
Na/K Ratio |
| Cereals and cereal products | 112 | 3397.4 | 2 | 1.8 | 2094.8 | 0 | 0.0 | 1.62 |
| Pasta and other grains | 41 | 551.4 | 1 | 2.4 | 2544.2 | 0 | 0.0 | 0.22 |
| Rice | 8 | 8.0 | 1 | 12.5 | 1443.9 | 0 | 0.0 | 0.01 |
| Bread and rolls | 42 | 5409.8 | 0 | 0.0 | 1888.7 | 0 | 0.0 | 2.86 |
| Pizza, crackers, and other salty snacks | 21 | 6220.2 | 0 | 0.0 | 1877.3 | 0 | 0.0 | 3.31 |
| Meat and meat products | 86 | 6037.9 | 0 | 0.0 | 4275.9 | 0 | 0.0 | 1.41 |
| Red meat | 28 | 1715.9 | 0 | 0.0 | 4020.9 | 0 | 0.0 | 0.43 |
| White meat | 12 | 1637.6 | 0 | 0.0 | 5258.2 | 0 | 0.0 | 0.31 |
| Processed meat | 36 | 12,000.0 | 0 | 0.0 | 4329.0 | 0 | 0.0 | 2.77 |
| Offal | 10 | 843.4 | 0 | 0.0 | 3620.1 | 0 | 0.0 | 0.23 |
| Milk and dairy products | 72 | 4356.2 | 0 | 0.0 | 1178.1 | 0 | 0.0 | 3.70 |
| Milk and yogurt | 13 | 416.5 | 0 | 0.0 | 1726.4 | 0 | 0.0 | 0.24 |
| Cheese | 59 | 5224.2 | 0 | 0.0 | 1057.3 | 0 | 0.0 | 4.94 |
| Fresh cheese | 17 | 4002.5 | 0 | 0.0 | 1241.9 | 0 | 0.0 | 3.22 |
| Aged cheese | 42 | 5718.8 | 0 | 0.0 | 982.6 | 0 | 0.0 | 5.82 |
| Eggs | 9 | 1110.8 | 0 | 0.0 | 1192.7 | 0 | 0.0 | 0.93 |
| Fish and seafood | 62 | 4271.7 | 0 | 0.0 | 2789.1 | 0 | 0.0 | 1.53 |
| Fish | 41 | 4251.5 | 0 | 0.0 | 3407.6 | 0 | 0.0 | 1.25 |
| Preserved and tinned fish | 9 | 13,000.0 | 0 | 0.0 | 3572.0 | 0 | 0.0 | 3.64 |
| Non-piscivorous fish | 15 | 1430.8 | 0 | 0.0 | 3541.6 | 0 | 0.0 | 0.40 |
| Piscivorous fish | 17 | 2079.5 | 0 | 0.0 | 3202.4 | 0 | 0.0 | 0.65 |
| Crustaceans and mollusks | 21 | 4311.3 | 0 | 0.0 | 1581.5 | 0 | 0.0 | 2.73 |
| All vegetables | 196 | 1846.7 | 2 | 1.0 | 3056.9 | 0 | 0.0 | 0.60 |
| Leafy vegetables | 40 | 908.9 | 0 | 0.0 | 3307.6 | 0 | 0.0 | 0.27 |
| Tomatoes | 19 | 2285.4 | 0 | 0.0 | 4244.1 | 0 | 0.0 | 0.54 |
| Root vegetables | 14 | 435.6 | 1 | 7.1 | 2662.1 | 0 | 0.0 | 0.16 |
| Cabbage | 28 | 579.2 | 0 | 0.0 | 3140.3 | 0 | 0.0 | 0.18 |
| Other vegetables | 63 | 3903.5 | 1 | 1.6 | 2790.8 | 0 | 0.0 | 1.40 |
| Mushrooms | 5 | 218.2 | 0 | 0.0 | 5093.9 | 0 | 0.0 | 0.04 |
| Legumes | 43 | 725.9 | 11 | 25.6 | 10,062.5 | 0 | 0.0 | 0.07 |
| Potatoes | 14 | 1543.8 | 0 | 0.0 | 4054.7 | 0 | 0.0 | 0.38 |
| Fresh fruit | 60 | 14.8 | 3 | 5.0 | 1902.6 | 0 | 0.0 | 0.01 |
| Citrus fruit | 12 | 24.7 | 1 | 8.3 | 1712.9 | 0 | 0.0 | 0.01 |
| All other fruit | 48 | 12.3 | 2 | 4.2 | 1950.0 | 0 | 0.0 | 0.01 |
| Dry fruit, nuts and seeds | 45 | 1138.4 | 7 | 15.6 | 7189.2 | 0 | 0.0 | 0.16 |
| Dry fruit | 8 | 1149.8 | 0 | 0.0 | 8351.2 | 0 | 0.0 | 0.14 |
| Nuts and seeds | 37 | 1135.9 | 7 | 18.9 | 6938.0 | 0 | 0.0 | 0.16 |
| Sweets products | 79 | 1408.0 | 1 | 1.3 | 3271.8 | 0 | 0.0 | 0.43 |
| Sugar, non-chocolate confectionery | 8 | 128.6 | 0 | 0.0 | 2078.2 | 0 | 0.0 | 0.06 |
| Chocolate, candy bars, etc. | 21 | 392.2 | 1 | 4.8 | 7529.2 | 0 | 0.0 | 0.05 |
| Ice-cream | 5 | 297.0 | 0 | 0.0 | 1490.8 | 0 | 0.0 | 0.20 |
| Cakes, pies and pastries | 30 | 2108.8 | 0 | 0.0 | 1515.8 | 0 | 0.0 | 1.39 |
| Biscuits, dry cakes | 15 | 2481.4 | 0 | 0.0 | 2053.5 | 0 | 0.0 | 1.21 |
| Oils and fats | 23 | 1305.4 | 8 | 34.8 | 121.8 | 0 | 0.0 | 10.72 |
| Vegetables fats and oils (non-olive) | 12 | 332.2 | 5 | 41.7 | 24.2 | 7 | 58.3 | 13.73 |
| Olive oil | 4 | 1.3 | 3 | 75.0 | 6.1 | 1 | 25.0 | 0.21 |
| Butter and other animal fats | 7 | 3718.9 | 0 | 0.0 | 355.3 | 0 | 0.0 | 10.47 |
| Beverages | 102 | 35.4 | 1 | 0.9 | 534.2 | 1 | 0.9 | 0.07 |
| Coffee and tea | 8 | 21.4 | 0 | 0.0 | 1236.5 | 0 | 0.0 | 0.02 |
| Wine | 50 | 14.7 | 0 | 0.0 | 566.1 | 0 | 0.0 | 0.03 |
| Red wine | 27 | 14.3 | 0 | 0.0 | 708.2 | 0 | 0.0 | 0.02 |
| White wine | 23 | 15.1 | 0 | 0.0 | 399.3 | 0 | 0.0 | 0.04 |
| Aperitif wines and beers | 8 | 53.3 | 1 | 12.5 | 493.3 | 0 | 0.0 | 0.11 |
| Spirits and liqueurs | 21 | 45.8 | 0 | 0.0 | 60.9 | 1 | 4.8 | 0.75 |
| Fruit juices | 8 | 52.2 | 0 | 0.0 | 1229.5 | 0 | 0.0 | 0.04 |
| Soft drinks | 7 | 128.6 | 0 | 0.0 | 175.5 | 0 | 0.0 | 0.73 |
1 Bold characters relate to main food categories.
The dietary intakes of sodium and potassium in the study population are reported in Table 3 and Table 4. Overall mean intakes were 2.2 g/day and 3.4 g/day for sodium and potassium, respectively. Foods contributing the most to sodium intake were cereals (33.2%); meat products (24.5%), mainly processed meats; followed by dairy products (13.6%) and vegetables (12.6%). For potassium, they were meat (17.1%), fresh fruits (15.7%), and vegetables (15.1%), and with relevant contributions from cereals and dairy products (11.6% each) and beverages (10.8%). Men had overall intakes that were only slightly higher than women for both sodium (2.2 vs. 2.1 g/day) (Supplementary Tables S2 and S3) and potassium (3.4 vs. 3.3 g/day) (Supplementary Tables S4 and S5).
Table 3.
Distribution of sodium daily dietary intake in all subjects (in mg/day) and percentage contribution (%) of each food to total intake.
| Food 1 | Mean | SD | P5 | P25 | P50 | P75 | P95 | % |
|---|---|---|---|---|---|---|---|---|
| Total intake | 2151.8 | 867.9 | 1019.9 | 1563.1 | 2025.9 | 2569.0 | 3785.1 | 100 |
| Cereals and cereal products | 714.3 | 453.5 | 110.2 | 396.7 | 661.7 | 943.2 | 1487.9 | 33.20 |
| Pasta and other grains | 31.5 | 22.4 | 2.3 | 15.9 | 27.6 | 42.8 | 74.5 | 1.46 |
| Rice | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.00 |
| Bread and rolls | 423.8 | 389.3 | 0.0 | 107.7 | 324.6 | 587.5 | 1112.8 | 19.70 |
| Pizza, crackers, and other salty snacks | 259.0 | 191.4 | 31.2 | 128.6 | 219.1 | 354.0 | 581.7 | 12.04 |
| Meat and meat products | 526.5 | 349.8 | 125.6 | 290.9 | 455.1 | 670.1 | 1222.3 | 24.47 |
| Red meat | 113.9 | 79.0 | 14.0 | 57.6 | 100.0 | 153.5 | 267.7 | 5.29 |
| White meat | 48.1 | 42.7 | 0.7 | 18.9 | 38.8 | 67.0 | 131.6 | 2.24 |
| Processed meat | 363.0 | 306.5 | 32.0 | 151.4 | 284.3 | 478.8 | 957.7 | 16.87 |
| Offal | 1.5 | 3.9 | 0.0 | 0.0 | 0.0 | 1.3 | 6.7 | 0.07 |
| Milk and dairy products | 291.6 | 206.8 | 66.1 | 155.8 | 246.9 | 366.5 | 677.8 | 13.55 |
| Milk and yogurt | 85.0 | 99.3 | 0.0 | 20.8 | 68.3 | 114.7 | 252.1 | 3.95 |
| Cheese | 206.6 | 171.6 | 22.9 | 88.9 | 167.4 | 275.6 | 530.6 | 9.60 |
| Fresh cheese | 58.5 | 76.0 | 0.0 | 12.0 | 36.0 | 72.0 | 188.9 | 2.72 |
| Aged cheese | 148.1 | 137.4 | 5.7 | 55.5 | 112.1 | 203.6 | 390.0 | 6.88 |
| Eggs | 16.7 | 12.6 | 1.6 | 8.1 | 15.0 | 23.5 | 36.9 | 0.78 |
| Fish and seafood | 129.8 | 160.6 | 14.7 | 55.2 | 100.9 | 159.9 | 344.5 | 6.03 |
| Fish | 98.6 | 149.7 | 11.6 | 38.0 | 70.3 | 118.7 | 270.1 | 4.58 |
| Preserved and tinned fish | 72.2 | 143.3 | 0.0 | 21.3 | 47.2 | 78.4 | 215.6 | 3.36 |
| Non-piscivorous fish | 14.6 | 17.9 | 0.0 | 2.1 | 9.0 | 20.3 | 51.1 | 0.68 |
| Piscivorous fish | 11.8 | 20.5 | 0.0 | 0.3 | 4.1 | 14.4 | 46.3 | 0.55 |
| Crustaceans and mollusks | 31.2 | 43.3 | 0.0 | 2.9 | 15.4 | 47.1 | 105.3 | 1.45 |
| All vegetables | 270.7 | 164.7 | 66.9 | 152.7 | 243 | 348.1 | 590.6 | 12.58 |
| Leafy vegetables | 31.7 | 27.5 | 4.2 | 13.1 | 24.7 | 41.6 | 84.0 | 1.47 |
| Tomatoes | 101.9 | 110.3 | 2.9 | 25.4 | 66.0 | 143.4 | 304.6 | 4.74 |
| Root vegetables | 17.8 | 21.5 | 0.9 | 4.2 | 10.4 | 23.1 | 60.0 | 0.83 |
| Cabbage | 2.4 | 4.1 | 0.0 | 0.0 | 1.0 | 3.2 | 10.1 | 0.11 |
| Other vegetables | 116.9 | 85.6 | 21.5 | 54.9 | 96.4 | 160.9 | 275.3 | 5.43 |
| Mushrooms | 0.6 | 0.9 | 0.0 | 0.1 | 0.3 | 0.9 | 1.9 | 0.03 |
| Legumes | 13.6 | 13.5 | 0.4 | 4.6 | 9.9 | 18.4 | 38.9 | 0.63 |
| Potatoes | 37.9 | 37.4 | 2.8 | 16.5 | 27.8 | 49.4 | 108.1 | 1.76 |
| Fresh fruit | 4.2 | 2.5 | 0.7 | 2.5 | 3.9 | 5.4 | 8.8 | 0.20 |
| Citrus fruit | 2.7 | 1.7 | 0.5 | 1.5 | 2.4 | 3.5 | 5.7 | 0.13 |
| All other fruit | 1.6 | 1.2 | 0.0 | 0.7 | 1.4 | 2.0 | 3.8 | 0.07 |
| Dry fruit, nuts and seeds | 1.9 | 3.4 | 0.0 | 0.2 | 0.3 | 1.8 | 9.4 | 0.09 |
| Dry fruit | 0.4 | 1.3 | 0.0 | 0.0 | 0.1 | 0.1 | 2.8 | 0.02 |
| Nuts and seeds | 1.5 | 2.9 | 0.0 | 0.2 | 0.2 | 1.5 | 8.1 | 0.07 |
| Sweets products | 114.7 | 131.5 | 1.1 | 31.1 | 77.4 | 152.8 | 332.7 | 5.33 |
| Sugar, non-chocolate confectionery | 0.4 | 0.7 | 0.0 | 0.0 | 0.2 | 0.4 | 1.5 | 0.02 |
| Chocolate, candy bars, etc. | 2.1 | 3.4 | 0.0 | 0.0 | 0.7 | 2.2 | 8.8 | 0.10 |
| Ice-cream | 4.1 | 4.6 | 0.0 | 0.7 | 3.1 | 5.9 | 12.7 | 0.19 |
| Cakes, pies and pastries | 74.0 | 114.4 | 0.0 | 7.0 | 30.2 | 110.3 | 253.1 | 3.44 |
| Biscuits, dry cakes | 34.1 | 42.5 | 0.0 | 0.0 | 15.6 | 59.6 | 119.6 | 1.58 |
| Oils and fats | 9.7 | 11.5 | 0.1 | 1.4 | 5.9 | 14.5 | 29.5 | 0.45 |
| Vegetables fats and oils (non-olive) | 0.7 | 1.6 | 0.0 | 0.2 | 0.4 | 0.8 | 2.4 | 0.03 |
| Olive oil | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.00 |
| Butter and other animal fats | 9.0 | 11.2 | 0.0 | 0.6 | 5.3 | 13.4 | 28.0 | 0.42 |
| Beverages | 19.7 | 25.1 | 2.1 | 5.9 | 11.5 | 22.8 | 64.3 | 0.92 |
| Coffee and tea | 3.2 | 2.8 | 0.2 | 1.6 | 2.6 | 4.0 | 7.0 | 0.15 |
| Wine | 1.8 | 2.4 | 0.0 | 0.0 | 0.8 | 3.6 | 7.2 | 0.08 |
| Red wine | 1.1 | 1.7 | 0.0 | 0.0 | 0.2 | 1.6 | 4.8 | 0.05 |
| White wine | 0.8 | 1.5 | 0.0 | 0.0 | 0.0 | 0.7 | 3.8 | 0.04 |
| Aperitif wines and beers | 4.0 | 11.6 | 0.0 | 0.0 | 0.6 | 3.4 | 19.0 | 0.19 |
| Spirits and liqueurs | 0.1 | 0.5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.8 | 0.00 |
| Fruit juices | 4.9 | 12.3 | 0.0 | 0.0 | 0.7 | 4.8 | 22.4 | 0.23 |
| Soft drinks | 5.7 | 15.2 | 0.0 | 0.0 | 0.0 | 4.3 | 25.7 | 0.26 |
1 Bold characters relate to main food categories.
Table 4.
Distribution of potassium daily dietary intake in all subjects (in mg/day) and percentage contribution (%) of each food to total intake.
| Food 1 | Mean | SD | P5 | P25 | P50 | P75 | P95 | % |
|---|---|---|---|---|---|---|---|---|
| Total intake | 3367.3 | 1127.9 | 1887.4 | 2611.8 | 3238.8 | 3862.6 | 5508.4 | 100 |
| Cereals and cereal products | 390.6 | 203.3 | 108.4 | 252.9 | 362.0 | 505.2 | 751.0 | 11.60 |
| Pasta and other grains | 145.3 | 103.6 | 10.4 | 73.3 | 127.5 | 197.7 | 344.0 | 4.31 |
| Rice | 8.0 | 11.0 | 0.0 | 1.6 | 5.1 | 8.8 | 28.0 | 0.24 |
| Bread and rolls | 148.0 | 135.9 | 0..0 | 37.6 | 113.3 | 205.1 | 388.5 | 4.39 |
| Pizza, crackers, and other salty snacks | 89.3 | 64.8 | 9.5 | 43.0 | 80.9 | 117.5 | 197.4 | 2.65 |
| Meat and meat products | 574.9 | 316.6 | 140.4 | 355.5 | 531.1 | 735.6 | 1219.4 | 17.07 |
| Red meat | 286.7 | 192.1 | 36.5 | 143.8 | 256.1 | 389.7 | 674.0 | 8.52 |
| White meat | 153.9 | 137.4 | 2.3 | 59.2 | 124.8 | 211.2 | 420.2 | 4.57 |
| Processed meat | 127.6 | 107.8 | 11.3 | 53.2 | 100.0 | 168.4 | 337.0 | 3.79 |
| Offal | 6.6 | 16.6 | 0.0 | 0.0 | 0.0 | 5.8 | 27.0 | 0.20 |
| Milk and dairy products | 391.9 | 409.8 | 21.3 | 123.9 | 318.5 | 508.1 | 1046.4 | 11.64 |
| Milk and yogurt | 348.3 | 402.9 | 0.0 | 82.5 | 281.7 | 472.8 | 1031.5 | 10.34 |
| Cheese | 43.6 | 37.0 | 4.7 | 19.1 | 34.9 | 56.1 | 109.0 | 1.29 |
| Fresh cheese | 18.1 | 23.6 | 0.0 | 3.7 | 11.2 | 22.4 | 58.6 | 0.54 |
| Aged cheese | 25.4 | 23.6 | 1.0 | 9.5 | 19.3 | 35.0 | 67.0 | 0.76 |
| Eggs | 18.0 | 13.6 | 1.7 | 8.7 | 16.1 | 25.3 | 39.6 | 0.53 |
| Fish and seafood | 107.3 | 86.2 | 13.7 | 49.7 | 87.5 | 136.4 | 280.0 | 3.19 |
| Fish | 95.7 | 80.0 | 9.3 | 42.1 | 78.5 | 122.4 | 243.4 | 2.84 |
| Preserved and tinned fish | 31.5 | 37.7 | 0.0 | 9.3 | 23.4 | 40.0 | 86.8 | 0.94 |
| Non-piscivorous fish | 37.7 | 45.0 | 0.0 | 5.6 | 23.8 | 53.0 | 143.4 | 1.12 |
| Piscivorous fish | 26.5 | 37.7 | 0.0 | 1.6 | 13.2 | 39.9 | 92.2 | 0.79 |
| Crustaceans and mollusks | 11.6 | 16.2 | 0.0 | 1.1 | 5.7 | 17.8 | 38.2 | 0.35 |
| All vegetables | 506.8 | 291.2 | 143.3 | 308.2 | 453.8 | 639.7 | 1118.6 | 15.05 |
| Leafy vegetables | 102.8 | 86.0 | 9.7 | 40.8 | 78.1 | 140.2 | 284.0 | 3.05 |
| Tomatoes | 234.2 | 180.4 | 20.2 | 105.1 | 198.4 | 315.0 | 572.0 | 6.95 |
| Root vegetables | 87.2 | 89.4 | 10.0 | 30.8 | 61.2 | 105.1 | 254.2 | 2.59 |
| Cabbage | 13.1 | 22.2 | 0.0 | 0.0 | 5.7 | 17.3 | 55.0 | 0.39 |
| Other vegetables | 69.6 | 53.1 | 10.1 | 31.1 | 56.4 | 97.0 | 173.7 | 2.07 |
| Mushrooms | 12.9 | 20.2 | 0.0 | 1.5 | 6.1 | 20.4 | 43.8 | 0.38 |
| Legumes | 188.5 | 187.5 | 5.0 | 63.4 | 136.9 | 254.6 | 539.3 | 5.60 |
| Potatoes | 99.5 | 98.2 | 7.3 | 43.4 | 73.0 | 129.7 | 283.8 | 2.95 |
| Fresh fruit | 529.9 | 314.9 | 91.5 | 315.2 | 494.3 | 696.4 | 1117.6 | 15.74 |
| Citrus fruit | 421.8 | 264.4 | 76.6 | 236.5 | 383.4 | 555.7 | 909.7 | 12.53 |
| All other fruit | 108.1 | 85.7 | 1.5 | 46.4 | 97.1 | 139.3 | 260.0 | 3.21 |
| Dry fruit, nuts and seeds | 12.2 | 21.5 | 0.0 | 1.4 | 2.2 | 11.9 | 60.5 | 0.36 |
| Dry fruit | 3.3 | 9.2 | 0.0 | 0.0 | 0.8 | 0.8 | 20.0 | 0.10 |
| Nuts and seeds | 8.9 | 17.7 | 0.0 | 1.4 | 1.4 | 9.0 | 49.3 | 0.27 |
| Sweets products | 169.4 | 147.5 | 15.0 | 71.9 | 133.5 | 221.9 | 429.5 | 5.03 |
| Sugar, non-chocolate confectionery | 27.6 | 33.4 | 0.0 | 6.2 | 18.6 | 41.4 | 80.0 | 0.82 |
| Chocolate, candy bars, etc. | 39.6 | 65.8 | 0.0 | 0.0 | 12.8 | 42.9 | 169.4 | 1.18 |
| Ice-cream | 20.8 | 23.3 | 0.0 | 3.7 | 15.5 | 29.5 | 64.0 | 0.62 |
| Cakes, pies and pastries | 53.2 | 82.2 | 0.0 | 5.0 | 21.7 | 79.3 | 181.9 | 1.58 |
| Biscuits, dry cakes | 28.2 | 35.2 | 0.0 | 0.0 | 12.9 | 49.3 | 99.0 | 0.84 |
| Oils and fats | 1.1 | 1.1 | 0.1 | 0.4 | 0.8 | 1.6 | 3.1 | 0.03 |
| Vegetables fats and oils (non-olive) | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 0.1 | 0.2 | 0.002 |
| Olive oil | 0.1 | 0.1 | 0.0 | 0.1 | 0.1 | 0.2 | 0.3 | 0.004 |
| Butter and other animal fats | 0.9 | 1.1 | 0.0 | 0.2 | 0.6 | 1.4 | 2.8 | 0.03 |
| Beverages | 364.4 | 274.9 | 67.8 | 193.8 | 310.8 | 473.0 | 799.5 | 10.82 |
| Coffee and tea | 180.8 | 162.2 | 4.0 | 83.4 | 162.5 | 231.6 | 394.3 | 5.37 |
| Wine | 73.3 | 97.1 | 0.0 | 0.8 | 29.7 | 108.4 | 265.6 | 2.18 |
| Red wine | 52.8 | 84.3 | 0.0 | 0.0 | 11.3 | 80.4 | 236.0 | 1.57 |
| White wine | 20.6 | 40.7 | 0.0 | 0.0 | 0.8 | 19.2 | 99.8 | 0.61 |
| Aperitif wines and beers | 27.2 | 78.7 | 0.0 | 0.0 | 3.7 | 26.7 | 127.8 | 0.81 |
| Spirits and liqueurs | 0.2 | 0.7 | 0.0 | 0.0 | 0.0 | 0.0 | 1.0 | 0.01 |
| Fruit juices | 75.1 | 153.6 | 0.0 | 0.0 | 17.5 | 81.1 | 351.0 | 2.23 |
| Soft drinks | 7.8 | 20.8 | 0.0 | 0.0 | 0.0 | 5.8 | 35.1 | 0.23 |
1 Bold characters relate to main food categories.
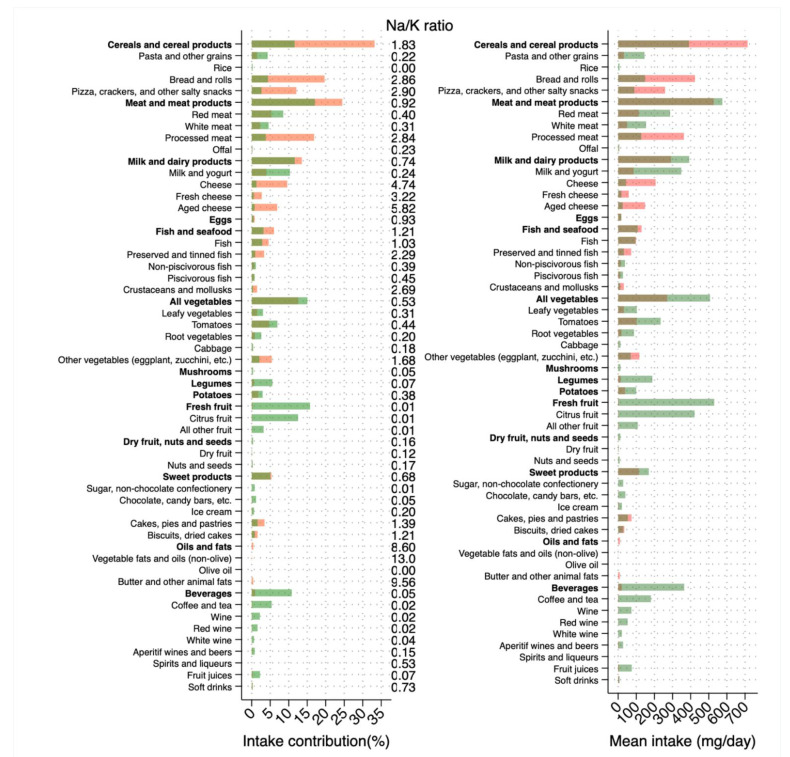
In Figure 1, we present a comparison between sodium and potassium intake from all food categories, their contribution to the overall intake, and the food-specific Na/K ratio. Cereals overall had a higher Na/K ratio, although pasta and rice had a lower Na/K ratio. Similarly, fish and seafood favored sodium with high Na/K ratios for preserved/tinned fish and crustaceans/mollusks, while other types of fish showed the opposite relationship. Similar patterns were noted for dairy products with Na/K ratio in favor of potassium for milk and yogurt, but not for cheese. Interestingly, legumes, potatoes and particularly fresh fruits intakes were in favor of potassium and the same for beverages, mainly driven by coffee, tea and wine. It is noteworthy that amongst oils and fats, olive oil only showed a Na/K ratio in favor of potassium whereas the intake of both animal fats and other vegetable oils greatly increased sodium intake.
Figure 1.
Average level of intake (in mg/day) of sodium and potassium according to food categories, their percentage contribution (in %) and sodium-to-potassium (Na/K) ratio. Light and dark orange bars indicate sodium and light and dark green bars indicate potassium, respectively.
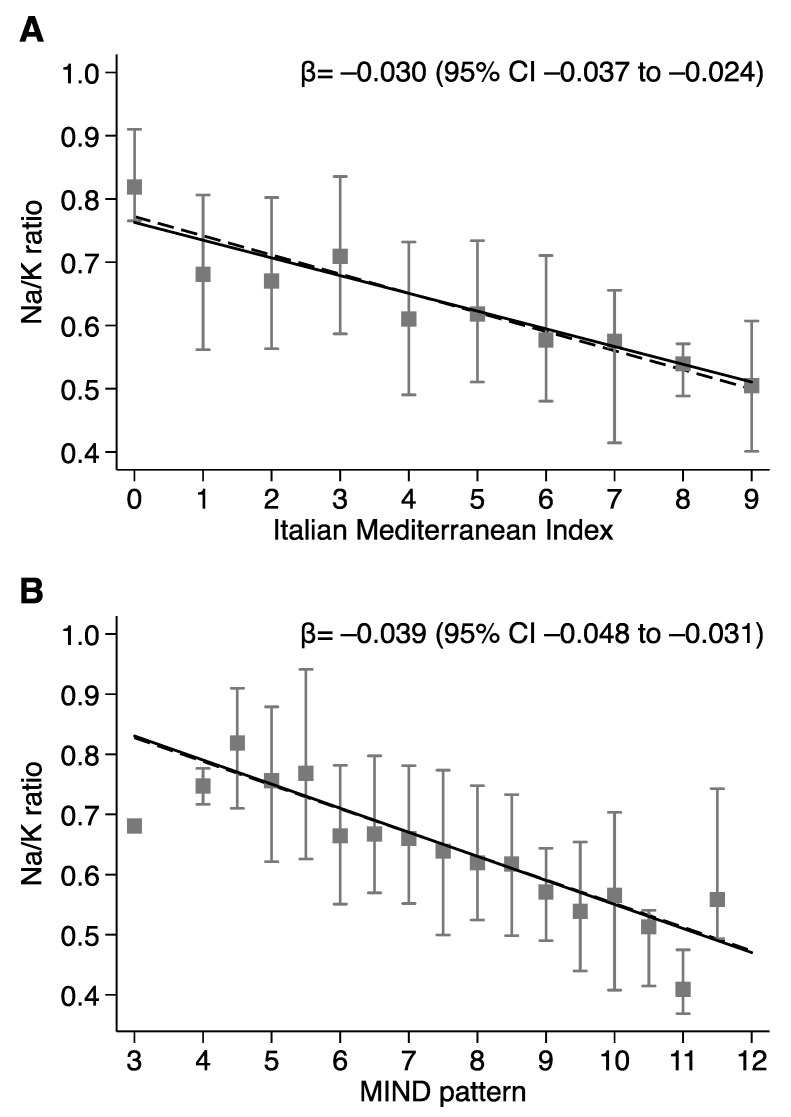
The distribution of sodium and potassium intake divided below (<4) and above (≥4) the median adherence to the Italian Mediterranean Index showed no substantial influence on sodium intake (2.2 vs. 2.1 g/day for low and high adherence, respectively) (Table 5). Conversely, subjects with adherence above the median score of the Italian Mediterranean Index demonstrated substantial higher potassium intake (3.1 vs. 3.6 g/day). Substantially identical findings were observed when dividing below (<7.5) and above (≥7.5) the median adherence to the MIND pattern (Table 6). Finally, the increase in adherence to Mediterranean and MIND patterns was linearly associated with a decrease in the Na/K ratio, from a predicted value based on linear regression analysis of 0.77 (95% CI 0.74–0.80) in the subjects with lowest adherence to the predicted value of 0.50 (95% CI 0.47–0.53) in the highest-adherent ones (Figure 2). Similar relationships were noted with the MIND pattern, with a predicted Na/K ratio of 0.83 (95% CI 0.79–0.87) in the lowest-adherence subjects and 0.47 (95% CI 0.43–0.51) in the highest ones (Figure 2).
Table 5.
Distribution of sodium and potassium daily dietary intake below (<4) and above (≥4) the median adherence to the Italian Mediterranean Index (IMI) (in mg/day). Mean, standard deviation and p values form the t-test of difference between means are reported.
| Sodium | Potassium | |||||
|---|---|---|---|---|---|---|
| Food 1 | IMI < 4 N = 275 |
IMI ≥ 4 N = 444 |
p Value | IMI < 4 N = 275 |
IMI ≥ 4 N = 444 |
p Value |
| Total intake | 2164.7 (849.5) | 2143.8 (880.0) | 0.755 | 3049.6 (901.6) | 3564.1 (1207.3) | <0.001 |
| Cereals and cereal products | 731.5 (465.3) | 703.7 (446.2) | 0.424 | 384.7 (202.9) | 394.2 (203.6) | 0.542 |
| Pasta and other grains | 28.6 (21.0) | 33.3 (23.1) | 0.006 | 131.8 (96.8) | 153.6 (106.8) | 0.006 |
| Rice | 0.04 (0.05) | 0.05 (0.07) | 0.046 | 7.0 (9.3) | 8.7 (12.0) | 0.046 |
| Bread and rolls | 444.4 (415.6) | 411.1 (372.1) | 0.265 | 155.1 (145.1) | 143.5 (129.9) | 0.265 |
| Pizza, crackers, and other salty snacks | 258.5 (173.7) | 259.3 (201.7) | 0.959 | 90.7 (60.1) | 88.4 (67.6) | 0.645 |
| Meat and meat products | 601.8 (361.9) | 479.8 (334.1) | <0.001 | 624.3 (294.0) | 544.4 (326.5) | 0.001 |
| Red meat | 130.4 (78.8) | 103.7 (77.4) | <0.001 | 327.9 (191.3) | 261.2 (188.4) | <0.001 |
| White meat | 44.1 (38.6) | 50.5 (44.9) | 0.049 | 141.0 (123.2) | 162.0 (145.0) | 0.046 |
| Processed meat | 426.0 (335.2) | 323.9 (280.7) | <0.001 | 149.8 (117.9) | 113.9 (98.7) | <0.001 |
| Offal | 1.3 (3.4) | 1.7 (4.1) | 0.180 | 5.6 (14.7) | 7.3 (17.7) | 0.180 |
| Milk and dairy products | 281.2 (195.8) | 298.1 (213.4) | 0.289 | 345.2 (397.5) | 420.8 (415.1) | 0.016 |
| Milk and yogurt | 73.5 (96.7) | 92.1 (100.3) | 0.015 | 301.3 (392.1) | 377.4 (407.1) | 0.014 |
| Cheese | 207.7 (163.8) | 205.9 (176.4) | 0.896 | 43.9 (35.0) | 43.4 (38.2) | 0.856 |
| Fresh cheese | 59.5 (67.3) | 57.9 (80.9) | 0.787 | 18.4 (20.9) | 18.0 (25.1) | 0.787 |
| Aged cheese | 148.2 (129.6) | 148.1 (142.2) | 0.989 | 25.5 (22.3) | 25.4 (24.4) | 0.989 |
| Eggs | 16.2 (11.3) | 17.0 (13.4) | 0.393 | 17.4 (12.1) | 18.3 (14.4) | 0.393 |
| Fish and seafood | 117.6 (211.0) | 137.3 (119.0) | 0.110 | 87.8 (72.2) | 119.3 (91.8) | <0.001 |
| Fish | 89.5 (204.4) | 104.2 (102.1) | 0.202 | 77.3 (66.9) | 107.0 (85.2) | <0.001 |
| Preserved and tinned fish | 69.7 (201.6) | 73.8 (90.3) | 0.713 | 28.9 (43.1) | 33.1 (33.8) | 0.141 |
| Non-piscivorous fish | 11.3 (13.3) | 16.6 (20.0) | <0.001 | 28.2 (30.8) | 43.5 (51.1) | <0.001 |
| Piscivorous fish | 8.4 (13.9) | 13.8 (23.5) | <0.001 | 20.2 (29.7) | 30.4 (41.5) | <0.001 |
| Crustaceans and mollusks | 28.1 (35.5) | 33.1 (47.3) | 0.127 | 10.5 (13.5) | 12.3 (17.6) | <0.001 |
| All vegetables | 204.7 (104.5) | 311.6 (181.3) | <0.001 | 358.6 (168.8) | 598.5 (312.6) | <0.001 |
| Leafy vegetables | 23.0 (17.7) | 37.1 (30.9) | <0.001 | 68.8 (56.0) | 123.8 (94.2) | <0.001 |
| Tomatoes | 80.2 (76.4) | 115.4 (125.0) | <0.001 | 174.4 (119.3) | 271.2 (200.8) | <0.001 |
| Root vegetables | 10.7 (11.3) | 22.2 (24.9) | <0.001 | 56.9 (49.8) | 105.9 (102.4) | <0.001 |
| Cabbage | 1.5 (2.5) | 3.0 (4.7) | <0.001 | 8.3 (13.7) | 16.0 (25.7) | <0.001 |
| Other vegetables | 89.3 (59.4) | 133.9 (94.5) | <0.001 | 50.3 (35.9) | 81.5 (58.3) | <0.001 |
| Mushrooms | 0.5 (0.6) | 0.6 (1.0) | 0.073 | 11.2 (14.2) | 13.9 (23.1) | 0.073 |
| Legumes | 9.9 (9.4) | 15.9 (15.1) | <0.001 | 136.5 (130.8) | 220.7 (209.0) | <0.001 |
| Potatoes | 38.4 (26.3) | 37.5 (42.9) | 0.756 | 100.9 (69.1) | 98.6 (112.6) | 0.756 |
| Fresh fruit | 3.3 (1.9) | 4.8 (2.6) | <0.001 | 407.7 (234.6) | 605.6 (334.2) | <0.001 |
| Citrus fruit | 2.0 (1.2) | 3.0 (1.8) | <0.001 | 320.7 (192.8) | 484.5 (283.0) | <0.001 |
| All other fruit | 1.3 (1.1) | 1.7 (1.3) | <0.001 | 87.0 (73.6) | 121.1 (90.0) | <0.001 |
| Dry fruit, nuts and seeds | 1.9 (3.7) | 1.9 (3.2) | 0.861 | 12.0 (23.2) | 12.3 (20.5) | 0.844 |
| Dry fruit | 0.4 (1.2) | 0.5 (1.3) | 0.674 | 3.1 (8.4) | 3.4 (9.7) | 0.674 |
| Nuts and seeds | 1.5 (3.2) | 1.5 (2.7) | 0.983 | 8.9 (19.7) | 8.9 (16.4) | 0.983 |
| Sweets products | 123.7 (142.2) | 109.1 (124.2) | 0.149 | 181.1 (151.4) | 162.2 (144.8) | 0.095 |
| Sugar, non-chocolate confectionery | 0.4 (0.7) | 0.3 (0.8) | 0.338 | 29.2 (33.2) | 26.6 (33.6) | 0.320 |
| Chocolate, candy bars, etc. | 2.2 (3.6) | 2.0 (3.3) | 0.322 | 42.7 (69.5) | 37.7 (63.5) | 0.322 |
| Ice-cream | 4.3 (4.4) | 4.0 (4.8) | 0.380 | 21.7 (21.9) | 20.1 (24.1) | 0.380 |
| Cakes, pies and pastries | 84.2 (125.8) | 67.7 (106.4) | 0.060 | 60.5 (90.5) | 48.7 (76.5) | 0.060 |
| Biscuits, dry cakes | 32.5 (42.1) | 35.1 (42.8) | 0.436 | 26.9 (34.8) | 29.0 (35.4) | 0.436 |
| Oils and fats | 11.6 (13.0) | 8.6 (10.2) | <0.001 | 1.3 (1.3) | 1.0 (1.0) | <0.001 |
| Vegetables fats and oils (non-olive) | 0.8 (1.6) | 0.7 (1.6) | 0.658 | 0.1 (0.1) | 0.1 (0.1) | 0.709 |
| Olive oil | 0.02 (0.01) | 0.02 (0.02) | <0.001 | 0.1 (0.0) | 0.2 (0.1) | <0.001 |
| Butter and other animal fats | 10.8 (12.9) | 7.9 (9.8) | <0.001 | 1.2 (1.3) | 0.8 (0.9) | <0.001 |
| Beverages | 22.6 (24.0) | 17.9 (25.7) | 0.016 | 380.8 (269.1) | 354.2 (278.3) | 0.208 |
| Coffee and tea | 3.2 (2.7) | 3.2 (2.8) | 0.993 | 181.5 (183.0) | 180.3 (148.0) | 0.924 |
| Wine | 2.3 (2.5) | 1.6 (2.3) | <0.001 | 87.2 (99.7) | 64.7 (94.5) | 0.003 |
| Red wine | 1.2 (1.7) | 1.0 (1.7) | 0.087 | 59.6 (86.5) | 48.5 (82.8) | 0.087 |
| White wine | 1.0 (1.8) | 0.6 (1.3) | <0.001 | 27.6 (48.1) | 16.2 (34.8) | <0.001 |
| Aperitif wines and beers | 4.4 (9.8) | 3.7 (12.6) | 0.465 | 30.1 (66.4) | 25.5 (85.4) | 0.449 |
| Spirits and liqueurs | 0.2 (0.7) | 0.1 (0.4) | 0.001 | 0.3 (0.9) | 0.1 (0.5) | 0.001 |
| Fruit juices | 4.3 (8.1) | 5.3 (14.3) | 0.297 | 70.4 (129.6) | 78.0 (166.9) | 0.521 |
| Soft drinks | 8.3 (16.2) | 4.1 (14.3) | <0.001 | 11.3 (22.1) | 5.6 (19.6) | <0.001 |
1 Bold characters relate to main food categories.
Table 6.
Distribution of sodium and potassium daily dietary intake below (<7.5) and above (≥7.5) the median adherence to the Mediterranean–DASH Diet Intervention for Neurodegenerative Delay (MIND) (in mg/day). Mean, standard deviation, and p values from the t-test of differences between means are reported.
| Sodium | Potassium | |||||
|---|---|---|---|---|---|---|
| Food 1 | MIND < 7.5 N = 288 |
MIND ≥ 7.5 N = 431 |
p Value | MIND < 7.5 N = 288 |
MIND ≥ 7.5 N = 431 |
p Value |
| Total intake | 2121.5 (841.8) | 2172.1 (885.4) | 0.444 | 3058.1 (993.1) | 3573.9 (1165.8) | <0.001 |
| Cereals and cereal products | 687.3 (440.1) | 732.3 (461.9) | 0.193 | 390.3 (194.9) | 390.7 (208.9) | 0.981 |
| Pasta and other grains | 33.4 (22.9) | 30.2 (22.1) | 0.057 | 154.3 (105.6) | 139.3 (101.8) | 0.057 |
| Rice | 0.04 (0.06) | 0.05 (0.06) | 0.160 | 7.3 (10.1) | 8.5 (11.6) | 0.160 |
| Bread and rolls | 406.9 (375.3) | 435.1 (398.5) | 0.341 | 142.0 (131.0) | 151.9 (139.1) | 0.341 |
| Pizza, crackers, and other salty snacks | 247.0 (190.8) | 267.0 (191.5) | 0.170 | 86.7 (67.6) | 91.1 (62.9) | 0.380 |
| Meat and meat products | 595.0 (354.1) | 480.7 (339.6) | <0.001 | 607.0 (298.2) | 553.5 (327.0) | 0.026 |
| Red meat | 123.6 (77.8) | 107.4 (79.2) | 0.007 | 321.2 (193.7) | 263.7 (187.8) | <0.001 |
| White meat | 39.5 (38.1) | 53.8 (44.7) | <0.001 | 127.0 (123.5) | 171.9 (143.2) | <0.001 |
| Processed meat | 430.1 (326.9) | 318.1 (283.7) | <0.001 | 151.3 (115.0) | 111.9 (99.8) | <0.001 |
| Offal | 1.8 (4.6) | 1.4 (3.3) | 0.202 | 7.6 (19.7) | 6.0 (14.2) | 0.202 |
| Milk and dairy products | 281.8 (189.9) | 298.2 (217.4) | 0.299 | 342.1 (376.8) | 425.2 (427.7) | 0.008 |
| Milk and yogurt | 72.9 (92.1) | 93.1 (103.1) | 0.007 | 298.3 (372.1) | 381.7 (419.3) | 0.007 |
| Cheese | 208.9 (162.7) | 205.1 (177.4) | 0.769 | 43.7 (34.2) | 43.5 (38.8) | 0.927 |
| Fresh cheese | 56.7 (66.3) | 59.6 (81.8) | 0.616 | 17.6 (20.6) | 18.5 (25.4) | 0.616 |
| Aged cheese | 152.2 (134.7) | 145.4 (139.3) | 0.520 | 26.1 (23.1) | 25.0 (23.9) | 0.520 |
| Eggs | 16.0 (12.4) | 17.2 (12.8) | 0.210 | 17.2 (13.3) | 18.5 (13.7) | 0.210 |
| Fish and seafood | 100.8 (96.8) | 149.1 (189.5) | <0.001 | 81.4 (66.9) | 124.6 (93.1) | <0.001 |
| Fish | 75.3 (84.5) | 114.1 (179.1) | 0.001 | 71.8 (62.3) | 111.6 (86.4) | <0.001 |
| Preserved and tinned fish | 55.2 (75.9) | 83.6 (173.6) | 0.009 | 24.4 (24.1) | 36.3 (43.8) | <0.001 |
| Non-piscivorous fish | 11.1 (14.1) | 16.9 (19.8) | <0.001 | 28.1 (35.8) | 44.0 (49.3) | <0.001 |
| Piscivorous fish | 9.0 (16.3) | 13.6 (22.8) | 0.003 | 19.3 (28.2) | 31.3 (42.3) | <0.001 |
| Crustaceans and mollusks | 25.6 (32.9) | 35.0 (48.6) | 0.004 | 9.6 (12.5) | 13.0 (18.1) | 0.006 |
| All vegetables | 222.0 (146.2) | 303.2 (168.5) | <0.001 | 405.1 (262.6) | 574.7 (289.8) | <0.001 |
| Leafy vegetables | 22.4 (21.1) | 37.9 (29.5) | <0.001 | 72.1 (73.7) | 123.2 (87.6) | <0.001 |
| Tomatoes | 95.0 (99.9) | 106.6 (116.6) | 0.169 | 208.0 (168.8) | 251.7 (185.9) | 0.001 |
| Root vegetables | 12.4 (16.6) | 21.4 (23.6) | <0.001 | 66.5 (72.3) | 101.0 (96.8) | <0.001 |
| Cabbage | 1.4 (2.3) | 3.1 (4.8) | <0.001 | 7.6 (12.3) | 16.7 (26.3) | <0.001 |
| Other vegetables | 90.8 (74.2) | 134.3 (88.3) | <0.001 | 50.9 (45.1) | 82.1 (54.4) | <0.001 |
| Mushrooms | 0.4 (0.7) | 0.6 (1.0) | 0.002 | 10.0 (15.7) | 14.8 (22.5) | 0.002 |
| Legumes | 9.4 (10.6) | 16.4 (14.5) | <0.001 | 130.9 (147.4) | 227.0 (201.2) | <0.001 |
| Potatoes | 35.0 (34.5) | 39.8 (39.1) | 0.093 | 91.9 (90.5) | 104.5 (102.8) | 0.093 |
| Fresh fruit | 3.4 (2.1) | 4.8 (2.6) | <0.001 | 423.7 (260.7) | 600.9 (328.1) | <0.001 |
| Citrus fruit | 2.1 (1.3) | 3.0 (1.8) | <0.001 | 332.8 (211.2) | 481.3 (279.5) | <0.001 |
| All other fruit | 1.3 (1.1) | 1.7 (1.3) | <0.001 | 90.9 (77.7) | 119.6 (88.9) | <0.001 |
| Dry fruit, nuts and seeds | 1.1 (2.2) | 2.4 (3.9) | <0.001 | 7.3 (13.9) | 15.5 (24.9) | <0.001 |
| Dry fruit | 0.2 (0.8) | 0.6 (1.5) | <0.001 | 1.7 (5.9) | 4.3 (10.7) | <0.001 |
| Nuts and seeds | 0.9 (1.9) | 1.8 (3.3) | <0.001 | 5.6 (11.9) | 11.2 (20.4) | <0.001 |
| Sweets products | 137.3 (149.3) | 99.6 (115.8) | <0.001 | 186.6 (152) | 157.9 (143.5) | 0.011 |
| Sugar, non-chocolate confectionery | 0.4 (1.0) | 0.3 (0.5) | <0.010 | 26.9 (25.6) | 28.1 (37.8) | 0.636 |
| Chocolate, candy bars, etc. | 2.1 (3.5) | 2.1 (3.4) | 0.996 | 39.6 (67.4) | 39.6 (64.9) | 0.996 |
| Ice-cream | 4.4 (5.1) | 3.9 (4.3) | 0.180 | 22.2 (25.5) | 19.8 (21.6) | 0.180 |
| Cakes, pies and pastries | 91.5 (137.2) | 62.4 (94.6) | <0.001 | 65.8 (98.6) | 44.8 (68.0) | 0.001 |
| Biscuits, dry cakes | 38.9 (41.9) | 30.9 (42.7) | 0.014 | 32.2 (34.6) | 25.6 (35.3) | 0.014 |
| Oils and fats | 11.2 (11) | 8.8 (11.7) | 0.006 | 1.3 (1.1) | 1.0 (1.1) | 0.004 |
| Vegetables fats and oils (non-olive) | 0.9 (2.1) | 0.6 (1.1) | 0.029 | 0.06 (0.14) | 0.05 (0.08) | 0.035 |
| Olive oil | 0.02 (0.01) | 0.03 (0.02) | <0.001 | 0.11 (0.07) | 0.14 (0.08) | <0.001 |
| Butter and other animal fats | 10.2 (10.7) | 8.1 (11.5) | 0.012 | 1.1 (1.1) | 0.8 (1.1) | 0.001 |
| Beverages | 20.6 (23.0) | 19.1 (26.4) | 0.410 | 363.3 (252.6) | 365.2 (289.2) | 0.930 |
| Coffee and tea | 3.0 (2.2) | 3.3 (3.1) | 0.108 | 160.4 (124.9) | 194.4 (181.8) | 0.006 |
| Wine | 2.4 (2.8) | 1.5 (2.1) | <0.001 | 92.9 (112.9) | 60.3 (82.5) | <0.001 |
| Red wine | 1.3 (2.0) | 0.9 (1.4) | 0.001 | 65.9 (100.9) | 44.0 (69.9) | 0.001 |
| White wine | 1.0 (1.8) | 0.6 (1.3) | 0.001 | 27.0 (47.9) | 16.3 (34.6) | 0.001 |
| Aperitif wines and beers | 4.4 (10.6) | 3.7 (12.3) | 0.423 | 30.3 (72.3) | 25.2 (82.7) | 0.400 |
| Spirits and liqueurs | 0.2 (0.6) | 0.1 (0.4) | 0.041 | 0.2 (0.8) | 0.1 (0.6) | 0.041 |
| Fruit juices | 4.2 (7.9) | 5.3 (14.6) | 0.212 | 70.6 (131.9) | 78.2 (166.7) | 0.516 |
| Soft drinks | 6.6 (14.1) | 5.1 (15.9) | 0.210 | 8.9 (19.3) | 7.0 (21.6) | 0.210 |
1 Bold characters relate to main food categories.
Figure 2.
Linear regression between sodium-to-potassium (Na/K) ratio and Italian Mediterranean Index-IMI (A) or MIND pattern (B). Squares and spikes indicate median and interquartile range, respectively. Solid and dashed lines indicate crude and adjusted linear fitting, respectively.
4. Discussion
In this Northern Italy community, we found that the mean sodium intake was above the current internationally recognized dietary recommendations of 1.5–2 g/day for adult populations [26], while the mean potassium intake was slightly lower than the dietary recommendation of 3.5 g/day [9]. Compared to previous Italian surveys, we found a small decrease in the average sodium intake when compared to the 3.8 g/day reported by the Italian Total Diet Study (TDS) 2001–2002 [23]. The most recent 2008–2012 CUORE survey showed substantially similar intakes with values of 2.3 and 1.9 g/day for men and women, respectively [24]. As regards potassium, our results were similar to intakes reported in the recent surveys which generally reported a potassium intake >3 g/day [24,27,47], although differences between sexes were less marked compared to other surveys, without an appreciably higher intake in men compared to women [27,28]. As a consequence, it is not surprising that higher adherence to the Mediterranean and MIND diets is associated with a general decrease of Na/K ratio. That lowering effect seemed mainly driven by an increase in potassium intake, since sodium intake was only slightly affected while potassium increased at higher levels of adherence to the investigated dietary patterns.
Despite the fact that there is no single definition of Mediterranean diet, it usually describes the traditional diet of populations residing in areas bordering the Mediterranean Sea, and is characterized by a high consumption of plant-based foods (such as vegetable, legumes, fruits, and nuts), preference for whole-grain cereals, fish and dairy products instead of other sources of refined carbohydrates and animal proteins [48,49]. Other features include the daily consumption of olive oil and moderate intake of alcohol (mostly red wine) during meals [49]. However in recent decades, there has been a gradual decline in adherence to the traditional Mediterranean diet in favor of Western dietary habits characterized by an unbalanced intake of foods that may lead to micronutrient deficiencies [50].
In spite of the general assumption of high adherence of Italians to a Mediterranean dietary pattern, this is unfortunately not true, since a gap still exists between the recommendations and the real dietary pattern, especially in most recent years [51,52]. Habitual salt intake in Europe is approximately 10 g per day [53] of which unprocessed foods represented approximately 12% of total salt intake but the majority (over 75%) occurred from processed food consumption [53,54,55] rather than from discretionary salt. The assessment of dietary sodium intake in free-living individuals is challenging due to high day-to-day variation, diversity in sources (naturally present, added during food processing, and discretionary use of salt at home) and the general trend for an overall reduction in salt concentrations of processed foods in recent years.
Our findings suggest that increased adherence to IMI and MIND patterns has limited effects on sodium intake, but it leads to an almost adequate potassium intake. For individuals, WHO recommend a sodium intake <2 g/day and a potassium intake >3.5 g/day [56,57] which would yield a Na/K ≤0.6, a ratio of intake considered beneficial for health in order to decrease blood pressure and generally improve cardiovascular health [52,58]. Foods showing the lowest Na/K ratio were fresh and dry fruits, most vegetables, legumes, and beverages, in accordance with previous surveys [47,59]. Conversely, among other categories, processed and prepackaged cereals (particularly salty and sweet snacks), processed meat, cheese, and non-olive oils and fats demonstrated higher values according to our findings and those reported previously [59,60]. In addition, efforts to decrease Na/K ratio could include specific indications supporting the use of low-sodium products, the gradual reduction of added salt to allow progressive adaptation towards a more sensitive taste, and the use of salt substitutes rich in potassium [61,62].
Our study population is generally characterized by good adherence to the Mediterranean diet [63]. However, more than a third of subjects (38%) in the study population had scores between 0–3 out of a maximum score of 11 points, indicating that improvement in dietary habits is both possible and definitely needed. Various longitudinal studies have analyzed the benefits of a Mediterranean diet in comparison with other types of diet [64,65,66,67]. These studies have shown that people with good adherence to a Mediterranean diet have a better quality of life and greater life expectancy, along with a decreased prevalence of chronic diseases [68,69]. Evidence has been accumulating that the Mediterranean diet may provide a substantial benefit by reducing the risk of many chronic diseases such as CVD disease, e.g., through maintenance of blood pressure and endothelial function [70,71].
Our study has some limitations. We did not include the quantity of drinking water in the intake of beverages, but it is considered a trivial source of both sodium and potassium [55,72,73]. In addition, we did not account for discretionary salt use since the EPIC questionnaire only assessed the habit to add salt when subjects do not eat at home. Moreover, we recruited only healthy adult subjects, and the results cannot be generalized to other populations e.g., children and the elderly, the latter being potentially more vulnerable to adverse effects in relation to excess sodium intake. In addition, since the recruitment period was carried out during 2005–2006, dietary habits of the population may have changed over time, although recent results from 2008–2012 showed similar values of intake of sodium and potassium [24], suggesting a relatively stable intake in a population without intervention specifically aimed at improving dietary habits. Finally, considering the ten-year gap between the time of population sampling and food analysis, we cannot entirely rule out that some changes over time may have occurred towards a sodium reduction and thus partially biased our estimates, especially due to a decrease in salt in processed foods [74]. Small, though still limited, changes in the sodium content of processed and restaurant foods appear to have occurred in more recent years [75,76,77]. However, the relatively low intake of processed and prepackaged foods in the study population, and the evidence that high sodium levels are still found in these products, despite efforts by the food industry in lowering its concentrations [78] suggests that our assessments are likely still currently valid.
One strength of our study is that we measured the sodium and potassium content of a large number of food samples and beverages that represent habitual dietary patterns of Northern Italy, and were therefore able to assess sodium and potassium dietary intakes with a high degree of accuracy. In addition, we estimated dietary intakes in a randomly selected large population sample from the Emilia-Romagna region. Although its dietary characteristics could be generally similar to those of other Italian populations [45,79], some peculiarities may be present due to the regional differences in plant growing and animal husbandry. However, the 2008–2012 survey was carried out with recruitment of participants from 21 municipalities across the country [24], among which Modena municipality only has been considered, and in addition no specific data about sodium and potassium was made available [80].
Finally, as regards the assessment of dietary habits, we estimated both sodium and potassium intake along with adherence to Mediterranean diet in our study community through implementation of the EPIC-validated semi-quantitative FFQ in the version tailored for dietary habits of the population of Northern Italy [81]. Although there is a European consensus that two non-consecutive 24 h dietary recalls are the preferred methods for the estimation of sodium intake when using a dietary survey at the population or group level [82], the implementation of the EPIC-FFQ should be considered a strength of the study. The EPIC-FFQ assesses frequency and quantity of consumption over an entire year, and takes into account intakes of seasonal food, supporting its substantial validity and reproducibility for the assessment of dietary habits in the adult population [83].
5. Conclusions
Our study provides an updated assessment of foods that contribute to sodium and potassium intake in a Northern Italy community. We found a mean sodium intake of 2.2 g/day, which exceeds the dietary recommendation for adults of 1.5–2 g/day, whereas the mean potassium intake was 3.4 g/day, which was slightly lower than the recommended 3.5 g/day. Our findings suggest that higher adherence to Mediterranean diet and MIND patterns has no effect on sodium intake, but may have a beneficial influence on potassium, favoring the achievement of the recommended dietary intake though a decrease in the Na/K ratio, notably by higher intakes of fresh and dry fruits, most vegetables, legumes, and beverages, as well as a reduction in processed and prepackaged foods.
Acknowledgments
The authors are grateful to subjects who participated in the study and made it possible.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/nu13082681/s1, Table S1: Food intake (g/day) according to different categories for the whole study population and by sex. Mean and standard deviation (SD) along with p values from t-test for independent samples for the difference between men and women are reported. Table S2: Distribution of sodium daily dietary intake in men (in mg/day) and percentage contribution (%) of each food to total intake. Table S3: Distribution of sodium daily dietary intake in women (in mg/day) and percentage contribution (%) of each food to total intake. Table S4: Distribution of potassium daily dietary intake in men (in mg/day) and percentage contribution (%) of each food to total intake. Supplemental Table S5: Distribution of potassium daily dietary intake in women (in mg/day) and percentage contribution (%) of each food to total intake.
Author Contributions
Conceptualization, M.V. and T.F.; data curation, C.M. (Carlotta Malagoli), L.V., M.M., and T.F.; formal analysis, L.V., M.M., and T.F.; funding acquisition, C.M. (Cristina Marchesi) and M.V.; investigation/methodology, A.N., C.M. (Carlotta Malagoli), L.V., and S.J.F.-T.; roles/writing—original draft, A.N., M.M., M.V., S.J.F.-T., and T.F.; writing—review and editing, all authors. All authors have read and agreed to the published version of the manuscript.
Funding
Filippini, Malavolti, and Vinceti were supported by the ‘Dipartimenti di Eccellenza 2018–2022’ grant to the UNIMORE Department of Biomedical, Metabolic, and Neural Sciences from the Italian Ministry of Education, University, and Research. Filippini was supported by grant ‘UNIMORE FAR IMPULSO 2020′ (no. 494/2020) from the University of Modena and Reggio Emilia. Vinceti was supported by the Reggio Emilia Health Authority of the National Health Service.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki after the approval of the Modena Ethics Committee (project no. 71.11/2011).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on reasonable request from the corresponding author. The data are not publicly available due to privacy reasons.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vos T., Allen C., Arora M., Barber R.M., Bhutta Z.A., Brown A., Carter A., Casey D.C., Charlson F.J., Chen A.Z., et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roth G.A., Mensah G.A., Johnson C.O., Addolorato G., Ammirati E., Baddour L.M., Barengo N.C., Beaton A.Z., Benjamin E.J., Benziger C.P., et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ISTAT . Main Causes of Death in Italy—2012. National Institute of Statitics; Rome, Italy: 2014. [(accessed on 19 July 2021)]. Available online: https://www.istat.it/it/files//2014/12/Principali_cause_morte_2012.pdf. [Google Scholar]
- 4.Filippini T., Violi F., D’Amico R., Vinceti M. The effect of potassium supplementation on blood pressure in hypertensive subjects: A systematic review and meta-analysis. Int. J. Cardiol. 2017;230:127–135. doi: 10.1016/j.ijcard.2016.12.048. [DOI] [PubMed] [Google Scholar]
- 5.Fuchs F.D., Whelton P.K. High Blood Pressure and Cardiovascular Disease. Hypertension. 2020;75:285–292. doi: 10.1161/HYPERTENSIONAHA.119.14240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Committee to Review the Dietary Reference Intakes for Sodium and Potassium. Board F.A.N. Dietary Reference Intakes for Sodium and Potassium. National Academies Press; Washington, DC, USA: 2019. Health and Medicine Division Dietary Reference Intakes for Sodium and Potassium. [PubMed] [Google Scholar]
- 7.Whelton P.K. Sodium, Blood Pressure, and Cardiovascular Disease. Hypertension. 2021;77:2138–2139. doi: 10.1161/HYPERTENSIONAHA.121.17223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whelton P.K. Sodium and Potassium Intake in US Adults. Circulation. 2018;137:247–249. doi: 10.1161/CIRCULATIONAHA.117.031371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.EFSA Panel on Dietetic Products. Nutrition and Allergies (NDA) Turck D., Bresson J.-L., Burlingame B., Dean T., Fairweather-Tait S., Heinonen M., Hirsch-Ernst K.I., Mangelsdorf I., et al. Dietary reference values for potassium. EFSA J. 2016;14:e04592. doi: 10.2903/j.efsa.2016.4592. [DOI] [Google Scholar]
- 10.Filippini T., Naska A., Kasdagli M., Torres D., Lopes C., Carvalho C., Moreira P., Malavolti M., Orsini N., Whelton P.K., et al. Potassium Intake and Blood Pressure: A Dose-Response Meta-Analysis of Randomized Controlled Trials. J. Am. Hear. Assoc. 2020;9:e015719. doi: 10.1161/JAHA.119.015719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vinceti M., Filippini T., Crippa A., de Sesmaisons A., Wise L., Orsini N. Meta-Analysis of Potassium Intake and the Risk of Stroke. J. Am. Hear. Assoc. 2016;5:e004210. doi: 10.1161/JAHA.116.004210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Filippini T., Malavolti M., Whelton P.K., Naska A., Orsini N., Vinceti M. Blood Pressure Effects of Sodium Reduction. Circulation. 2021;143:1542–1567. doi: 10.1161/CIRCULATIONAHA.120.050371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Y.-J., Yeh T.-L., Shih M.-C., Tu Y.-K., Chien K.-L. Dietary Sodium Intake and Risk of Cardiovascular Disease: A Systematic Review and Dose-Response Meta-Analysis. Nutrients. 2020;12:2934. doi: 10.3390/nu12102934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jayedi A., Ghomashi F., Zargar M.S., Shab-Bidar S. Dietary sodium, sodium-to-potassium ratio, and risk of stroke: A systematic review and nonlinear dose-response meta-analysis. Clin. Nutr. 2019;38:1092–1100. doi: 10.1016/j.clnu.2018.05.017. [DOI] [PubMed] [Google Scholar]
- 15.Whelton P.K., Campbell N.R.C., Lackland D.T., Parati G., Ram C.V.S., Weber M.A., Zhang X. Strategies for prevention of cardiovascular disease in adults with hypertension. J. Clin. Hypertens. 2020;22:132–134. doi: 10.1111/jch.13797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whelton S.P., McEvoy J.W., Shaw L., Psaty B.M., Lima J.A.C., Budoff M., Nasir K., Szklo M., Blumenthal R.S., Blaha M.J. Association of Normal Systolic Blood Pressure Level with Cardiovascular Disease in the Absence of Risk Factors. JAMA Cardiol. 2020;5:1011–1018. doi: 10.1001/jamacardio.2020.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carey R.M., Whelton P.K. New findings bearing on the prevention, detection and management of high blood pressure. Curr. Opin. Cardiol. 2021;36:429–435. doi: 10.1097/HCO.0000000000000864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Faraco G., Hochrainer K., Segarra S.G., Schaeffer S., Santisteban M.M., Menon A., Jiang H., Holtzman D.M., Anrather J., Iadecola C. Dietary salt promotes cognitive impairment through tau phosphorylation. Nat. Cell Biol. 2019;574:686–690. doi: 10.1038/s41586-019-1688-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohan D., Yap K.H., Reidpath D., Soh Y.C., McGrattan A., Stephan B.C., Robinson L., Chaiyakunapruk N., Siervo M. Link Between Dietary Sodium Intake, Cognitive Function, and Dementia Risk in Middle-Aged and Older Adults: A Systematic Review. J. Alzheimer’s Dis. 2020;76:1347–1373. doi: 10.3233/JAD-191339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu X., Morris M.C., Dhana K., Ventrelle J., Johnson K., Bishop L., Hollings C.S., Boulin A., Laranjo N., Stubbs B.J., et al. Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) study: Rationale, design and baseline characteristics of a randomized control trial of the MIND diet on cognitive decline. Contemp. Clin. Trials. 2021;102:106270. doi: 10.1016/j.cct.2021.106270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nowak K.L., Fried L., Jovanovich A., Ix J., Yaffe K., You Z., Chonchol M. Dietary Sodium/Potassium Intake Does Not Affect Cognitive Function or Brain Imaging Indices. Am. J. Nephrol. 2018;47:57–65. doi: 10.1159/000486580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.WHO . Tackling NCDs: ‘Best Buys’ and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases. World Health Organization; Geneva, Switzerland: [(accessed on 19 July 2021)]. WHO/NMH/NVI/17.9. Available online: https://apps.who.int/iris/handle/10665/259232. [Google Scholar]
- 23.Lombardi-Boccia G., Aguzzi A., Cappelloni M., Di Lullo G., Lucarini M. Total-diet study: Dietary intakes of macro elements and trace elements in Italy. Br. J. Nutr. 2003;90:1117–1121. doi: 10.1079/BJN2003997. [DOI] [PubMed] [Google Scholar]
- 24.Guastadisegni C., Donfrancesco C., Palmieri L., Grioni S., Krogh V., Vanuzzo D., Strazzullo P., Vannucchi S., Onder G., Giampaoli S. Nutrients Intake in Individuals with Hypertension, Dyslipidemia, and Diabetes: An Italian Survey. Nutrients. 2020;12:923. doi: 10.3390/nu12040923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.SINU . Livelli di Assunzione di Riferimento di Nutrienti ed Energia per la Popolazione Italiana (LARN) 4th ed. SICS Editore; Milan, Italy: 2014. [Google Scholar]
- 26.EFSA Panel on Nutrition. Novel Foods and Food Allergens (NDA) Turck D., Castenmiller J., De Henauw S., Hirsch-Ernst K., Kearney J., Knutsen H.K., Maciuk A., Mangelsdorf I., et al. Dietary reference values for sodium. EFSA J. 2019;17:e05778. doi: 10.2903/j.efsa.2019.5778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sette S., Le Donne C., Piccinelli R., Mistura L., Ferrari M., Leclercq C. The third National Food Consumption Survey, INRAN-SCAI 2005–06: Major dietary sources of nutrients in Italy. Int. J. Food Sci. Nutr. 2013;64:1014–1021. doi: 10.3109/09637486.2013.816937. [DOI] [PubMed] [Google Scholar]
- 28.Donfrancesco C., Noce C.L., Russo O., Buttari B., Profumo E., Minutoli D., Di Lonardo A., Iacone R., Vespasiano F., Vannucchi S., et al. Trend in potassium intake and Na/K ratio in the Italian adult population between the 2008 and 2018 CUORE project surveys. Nutr. Metab. Cardiovasc. Dis. 2021;31:814–826. doi: 10.1016/j.numecd.2020.11.015. [DOI] [PubMed] [Google Scholar]
- 29.Filippini T., Tancredi S., Malagoli C., Malavolti M., Bargellini A., Vescovi L., Nicolini F., Vinceti M. Dietary Estimated Intake of Trace Elements: Risk Assessment in an Italian Population. Expo. Health. 2020;12:641–655. doi: 10.1007/s12403-019-00324-w. [DOI] [Google Scholar]
- 30.Malavolti M., Fairweather-Tait S.J., Malagoli C., Vescovi L., Vinceti M., Filippini T. Lead exposure in an Italian population: Food content, dietary intake and risk assessment. Food Res. Int. 2020;137:109370. doi: 10.1016/j.foodres.2020.109370. [DOI] [PubMed] [Google Scholar]
- 31.Filippini T., Cilloni S., Malavolti M., Violi F., Malagoli C., Tesauro M., Bottecchi I., Ferrari A., Vescovi L., Vinceti M. Dietary intake of cadmium, chromium, copper, manganese, selenium and zinc in a Northern Italy community. J. Trace Elem. Med. Biol. 2018;50:508–517. doi: 10.1016/j.jtemb.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 32.Malagoli C., Malavolti M., Farnetani F., Longo C., Filippini T., Pellacani G., Vinceti M. Food and Beverage Consumption and Melanoma Risk: A Population-Based Case-Control Study in Northern Italy. Nutrients. 2019;11:2206. doi: 10.3390/nu11092206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Turrini A., Lombardi-Boccia G., Aureli F., Cubadda F., D’Addezio L., D’Amato M., D’Evoli L., Darnerud P., Devlin N., Dias M.G., et al. A conceptual framework for the collection of food products in a Total Diet Study. Food Addit. Contam. Part A. 2017;35:171–190. doi: 10.1080/19440049.2017.1384577. [DOI] [PubMed] [Google Scholar]
- 34.Bottecchi I., Vinceti M. Master’s Thesis. University of Modena and Reggio Emilia; Modena, Italy: 2012. Trace Elements in Foods: Analysis of Diet of Reggio Emilia and Modena. [Google Scholar]
- 35.Filippini T., Ferrari A., Michalke B., Grill P., Vescovi L., Salvia C., Malagoli C., Malavolti M., Sieri S., Krogh V., et al. Toenail selenium as an indicator of environmental exposure: A cross-sectional study. Mol. Med. Rep. 2017;15:3405–3412. doi: 10.3892/mmr.2017.6388. [DOI] [PubMed] [Google Scholar]
- 36.Filippini T., Malavolti M., Cilloni S., Wise L., Violi F., Malagoli C., Vescovi L., Vinceti M. Intake of arsenic and mercury from fish and seafood in a Northern Italy community. Food Chem. Toxicol. 2018;116:20–26. doi: 10.1016/j.fct.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 37.Filippini T., Tancredi S., Malagoli C., Cilloni S., Malavolti M., Violi F., Vescovi L., Bargellini A., Vinceti M. Aluminum and tin: Food contamination and dietary intake in an Italian population. J. Trace Elements Med. Biol. 2019;52:293–301. doi: 10.1016/j.jtemb.2019.01.012. [DOI] [PubMed] [Google Scholar]
- 38.Whitcomb B.W., Schisterman E. Assays with lower detection limits: Implications for epidemiological investigations. Paediatr. Peérinat. Epidemiol. 2008;22:597–602. doi: 10.1111/j.1365-3016.2008.00969.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pasanisi P., Berrino F., Bellati C., Sieri S., Krogh V. Validity of the Italian EPIC questionnaire to assess past diet. IARC Sci. Publ. 2002;156:41–44. [PubMed] [Google Scholar]
- 40.Vinceti M., Malagoli C., Fiorentini C., Longo C., Crespi C.M., Albertini G., Ricci C., Lanzoni A., Reggiani M., Virgili A., et al. Inverse Association Between Dietary Vitamin D and Risk of Cutaneous Melanoma in a Northern Italy Population. Nutr. Cancer. 2011;63:506–513. doi: 10.1080/01635581.2011.539314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Filippini T., Malagoli C., Wise L.A., Malavolti M., Pellacani G., Vinceti M. Dietary cadmium intake and risk of cutaneous melanoma: An Italian population-based case-control study. J. Trace Elem. Med. Biol. 2019;56:100–106. doi: 10.1016/j.jtemb.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 42.Malagoli C., Malavolti M., Agnoli C., Crespi C., Fiorentini C., Farnetani F., Longo C., Ricci C., Albertini G., Lanzoni A., et al. Diet Quality and Risk of Melanoma in an Italian Population. J. Nutr. 2015;145:1800–1807. doi: 10.3945/jn.114.209320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Filippini T., Adani G., Malavolti M., Garuti C., Cilloni S., Vinceti G., Zamboni G., Tondelli M., Galli C., Costa M., et al. Dietary Habits and Risk of Early-Onset Dementia in an Italian Case-Control Study. Nutrients. 2020;12:3682. doi: 10.3390/nu12123682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Morris M.C., Tangney C., Wang Y., Sacks F.M., Barnes L.L., Bennett D.A., Aggarwal N.T. MIND diet slows cognitive decline with aging. Alzheimer’s Dement. 2015;11:1015–1022. doi: 10.1016/j.jalz.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Agnoli C., Krogh V., Grioni S., Sieri S., Palli D., Masala G., Sacerdote C., Vineis P., Tumino R., Frasca G., et al. A Priori–Defined Dietary Patterns Are Associated with Reduced Risk of Stroke in a Large Italian Cohort. J. Nutr. 2011;141:1552–1558. doi: 10.3945/jn.111.140061. [DOI] [PubMed] [Google Scholar]
- 46.Morris M.C., Tangney C.C., Wang Y., Sacks F.M., Bennett D.A., Aggarwal N.T. MIND diet associated with reduced incidence of Alzheimer’s disease. Alzheimer’s Dement. 2015;11:1007–1014. doi: 10.1016/j.jalz.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Welch A.A., Fransen H., Jenab M., Boutron-Ruault M.C., Tumino R., Agnoli C., Ericson U., Johansson I., Ferrari P., Engeset D., et al. Variation in intakes of calcium, phosphorus, magnesium, iron and potassium in 10 countries in the European Prospective Investigation into Cancer and Nutrition study. Eur. J. Clin. Nutr. 2009;63:S101–S121. doi: 10.1038/ejcn.2009.77. [DOI] [PubMed] [Google Scholar]
- 48.Naska A., Trichopoulou A. Back to the future: The Mediterranean diet paradigm. Nutr. Metab. Cardiovasc. Dis. 2014;24:216–219. doi: 10.1016/j.numecd.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 49.Villani A., Sultana J., Doecke J., Mantzioris E. Differences in the interpretation of a modernized Mediterranean diet prescribed in intervention studies for the management of type 2 diabetes: How closely does this align with a traditional Mediterranean diet? Eur. J. Nutr. 2018;58:1369–1380. doi: 10.1007/s00394-018-1757-3. [DOI] [PubMed] [Google Scholar]
- 50.Stamler J. Toward a Modern Mediterranean Diet for the 21st Century. Nutr. Metab. Cardiovasc. Dis. 2013;23:1159–1162. doi: 10.1016/j.numecd.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 51.Idelson P.I., D’Elia L., Cairella G., Sabino P., Scalfi L., Fabbri A., Galletti F., Garbagnati F., Lionetti L., Paolella G., et al. Salt and Health: Survey on Knowledge and Salt Intake Related Behaviour in Italy. Nutrients. 2020;12:279. doi: 10.3390/nu12020279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lasalvia P., Gianfagna F., Veronesi G., Franchin M., Tozzi M., Castelli P., Grandi A.M., Zambon A., Iacoviello L., Ferrario M.M. Identification of dietary patterns in a general population of North Italian adults and their association with arterial stiffness. The RoCAV study. Nutr. Metab. Cardiovasc. Dis. 2021;31:44–51. doi: 10.1016/j.numecd.2020.08.001. [DOI] [PubMed] [Google Scholar]
- 53.Strazzullo P., D’Elia L., Kandala N.-B., Cappuccio F.P. Salt intake, stroke, and cardiovascular disease: Meta-analysis of prospective studies. BMJ. 2009;339:b4567. doi: 10.1136/bmj.b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown I.J., Tzoulaki I., Candeias V., Elliott P. Salt intakes around the world: Implications for public health. Int. J. Epidemiol. 2009;38:791–813. doi: 10.1093/ije/dyp139. [DOI] [PubMed] [Google Scholar]
- 55.Mattes R.D., Donnelly D. Relative contributions of dietary sodium sources. J. Am. Coll. Nutr. 1991;10:383–393. doi: 10.1080/07315724.1991.10718167. [DOI] [PubMed] [Google Scholar]
- 56.WHO . Guideline: Sodium Intake for Adults and Children. World Health Organization; Geneva, Switzerland: 2012. [(accessed on 19 July 2021)]. Available online: https://www.who.int/publications/i/item/9789241504836. [PubMed] [Google Scholar]
- 57.WHO . Guideline: Potassium Intake for Adults and Children. World Health Organization; Geneva, Switzerland: 2012. [(accessed on 19 July 2021)]. Available online: https://www.who.int/publications/i/item/9789241504829. [PubMed] [Google Scholar]
- 58.Vinceti M., Filippini T., Wise L.A., Rothman K.J. A systematic review and dose-response meta-analysis of exposure to environmental selenium and the risk of type 2 diabetes in nonexperimental studies. Environ. Res. 2021;197:111210. doi: 10.1016/j.envres.2021.111210. [DOI] [PubMed] [Google Scholar]
- 59.Turrini A., Saba A., Perrone D., Cialfa E., D’Amicis A. Food consumption patterns in Italy: The INN-CA Study 1994–1996. Eur. J. Clin. Nutr. 2001;55:571–588. doi: 10.1038/sj.ejcn.1601185. [DOI] [PubMed] [Google Scholar]
- 60.Leite M.L.C., Nicolosi A., Cristina S., A Hauser W., Pugliese P., Nappi G. Dietary and nutritional patterns in an elderly rural population in Northern and Southern Italy: (I). A cluster analysis of food consumption. Eur. J. Clin. Nutr. 2003;57:1514–1521. doi: 10.1038/sj.ejcn.1601719. [DOI] [PubMed] [Google Scholar]
- 61.Donfrancesco C., Ippolito R., Noce C.L., Palmieri L., Iacone R., Russo O., Vanuzzo D., Galletti F., Galeone D., Giampaoli S., et al. Excess dietary sodium and inadequate potassium intake in Italy: Results of the MINISAL study. Nutr. Metab. Cardiovasc. Dis. 2013;23:850–856. doi: 10.1016/j.numecd.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 62.Ponzo V., Pellegrini M., Costelli P., Vázquez-Araújo L., Gayoso L., D’Eusebio C., Ghigo E., Bo S. Strategies for Reducing Salt and Sugar Intakes in Individuals at Increased Cardiometabolic Risk. Nutrients. 2021;13:279. doi: 10.3390/nu13010279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Agnoli C., Grioni S., Sieri S., Palli D., Masala G., Sacerdote C., Vineis P., Tumino R., Giurdanella M.C., Pala V., et al. Italian mediterranean index and risk of colorectal cancer in the Italian section of the EPIC cohort. Int. J. Cancer. 2012;132:1404–1411. doi: 10.1002/ijc.27740. [DOI] [PubMed] [Google Scholar]
- 64.Knoops K.T.B., de Groot L., Kromhout D., Perrin A.-E., Moreiras-Varela O., Menotti A., Van Staveren W.A. Mediterranean Diet, Lifestyle Factors, and 10-Year Mortality in Elderly European Men and Women. JAMA. 2004;292:1433–1439. doi: 10.1001/jama.292.12.1433. [DOI] [PubMed] [Google Scholar]
- 65.Russo G.L., Siani A., Fogliano V., Geleijnse J.M., Giacco R., Giampaoli S., Iacoviello L., Kromhout D., Lionetti L., Naska A., et al. The Mediterranean diet from past to future: Key concepts from the second “Ancel Keys” International Seminar. Nutr. Metab. Cardiovasc. Dis. 2021;31:717–732. doi: 10.1016/j.numecd.2020.12.020. [DOI] [PubMed] [Google Scholar]
- 66.Tessari S., Casazza M., De Boni G., Bertoncello C., Fonzo M., Di Pieri M., Russo F. Promoting health and preventing non-communicable diseases: Evaluation of the adherence of the Italian population to the Mediterranean Diet by using the PREDIMED questionnaire. Ann Ig. 2020;33:337–346. doi: 10.7416/ai.2020.2393. [DOI] [PubMed] [Google Scholar]
- 67.Tyrovolas S., Polychronopoulos E., Bountziouka V., Zeimbekis A., Tsiligiani I., Papoutsou S., Gotsis E., Metallinos G., Lionis C., Panagiotakos D.B. Level of Adherence to the Mediterranean Diet Among Elderly Individuals Living in Mediterranean Islands: Nutritional Report from the Medis Study. Ecol. Food Nutr. 2009;48:76–87. doi: 10.1080/03670240802577390. [DOI] [PubMed] [Google Scholar]
- 68.Buckland G., Agudo A., Travier N., Huerta J.M., Cirera L., Tormo M.-J., Navarro C., Chirlaque M.D., Moreno-Iribas C., Ardanaz E., et al. Adherence to the Mediterranean diet reduces mortality in the Spanish cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC-Spain) Br. J. Nutr. 2011;106:1581–1591. doi: 10.1017/S0007114511002078. [DOI] [PubMed] [Google Scholar]
- 69.Sofi F., Cesari F., Abbate R., Gensini G.F., Casini A. Adherence to Mediterranean diet and health status: Meta-analysis. BMJ. 2008;337:a1344. doi: 10.1136/bmj.a1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Davis C.R., Bryan J., Hodgson J.M., Murphy K.J. Definition of the Mediterranean Diet; A Literature Review. Nutrients. 2015;7:9139–9153. doi: 10.3390/nu7115459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rees K., Takeda A., Martin N., Ellis L., Wijesekara D., Vepa A., Das A., Hartley L., Stranges S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2019;2019:CD009825. doi: 10.1002/14651858.CD009825.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ministry of Health . Know the Water from Your Tap. Ministry of Health; Rome, Italy: 2021. [(accessed on 19 July 2021)]. Available online: http://www.salute.gov.it/portale/temi/p2_6.jsp?lingua=italiano&id=4528&area=acque_potabili&menu=dieta. [Google Scholar]
- 73.Stoots S.J., Geraghty R., Kamphuis G.M., Jamnadass E., Henderickx M.M., Ventimiglia E., Traxer O., Keller E.X., De Coninck V., Talso M., et al. Variations in the mineral content of bottled ‘carbonated or sparkling’ water across Europe: A comparison of 126 brands across 10 countries. Central Eur. J. Urol. 2021;74:71–75. doi: 10.5173/ceju.2021.0331.r1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pravst I., Lavriša Ž., Kušar A., Miklavec K., Žmitek K. Changes in Average Sodium Content of Prepacked Foods in Slovenia during 2011–2015. Nutrients. 2017;9:952. doi: 10.3390/nu9090952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ahuja J.K.C., Li Y., Haytowitz D.B., Bahadur R., Pehrsson P.R., Cogswell M.E. Assessing Changes in Sodium Content of Selected Popular Commercially Processed and Restaurant Foods: Results from the USDA: CDC Sentinel Foods Surveillance Program. Nutrients. 2019;11:1754. doi: 10.3390/nu11081754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Santos J.A., Sparks E., Thout S.R., McKenzie B., Trieu K., Hoek A., Johnson C., McLean R., Arcand J., Campbell N.R.C., et al. The Science of Salt: A global review on changes in sodium levels in foods. J. Clin. Hypertens. 2019;21:1043–1056. doi: 10.1111/jch.13628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Urban L.E., Roberts S.B., Fierstein J.L., Gary C.E., Lichtenstein A.H. Sodium, Saturated Fat, andTransFat Content Per 1,000 Kilocalories: Temporal Trends in Fast-Food Restaurants, United States, 2000–2013. Prev. Chronic Dis. 2014;11:E228. doi: 10.5888/pcd11.140335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Orlando E.A., Rebellato A.P., Silva J.G.S., Andrade G.C., Pallone J.A.L. Sodium in different processed and packaged foods: Method validation and an estimative on the consumption. Food Res. Int. 2020;129:108836. doi: 10.1016/j.foodres.2019.108836. [DOI] [PubMed] [Google Scholar]
- 79.Filippini T., Michalke B., Wise L., Malagoli C., Malavolti M., Vescovi L., Salvia C., Bargellini A., Sieri S., Krogh V., et al. Diet composition and serum levels of selenium species: A cross-sectional study. Food Chem. Toxicol. 2018;115:482–490. doi: 10.1016/j.fct.2018.03.048. [DOI] [PubMed] [Google Scholar]
- 80.Salvia C., Donfrancesco C., Palmieri L., Noce C.L., Vanuzzo D., Vinceti M., Bargellini A., Borella P., Giampaoli S. The Health Examination Survey at regional level: The Emilia-Romagna Region (Northern Italy) example. Epidemiol Prev. 2020;44:40–47. doi: 10.19191/EP20.1.P040.016. [DOI] [PubMed] [Google Scholar]
- 81.Pala V., Sieri S., Palli D., Salvini S., Berrino F., Bellegotti M., Frasca G., Tumino R., Sacerdote C., Fiorini L., et al. Diet in the Italian Epic Cohorts: Presentation of Data and Methodological Issues. Tumori J. 2003;89:594–607. doi: 10.1177/030089160308900603. [DOI] [PubMed] [Google Scholar]
- 82.Brussaard J.H., for the EFCOSUM Group. Löwik M.R.H., Steingrímsdóttir L., Møller A., Kearney J., De Henauw S., Becker W. A European food consumption survey method–conclusions and recommendations. Eur. J. Clin. Nutr. 2002;56:S89–S94. doi: 10.1038/sj.ejcn.1601432. [DOI] [PubMed] [Google Scholar]
- 83.Pisani P., Faggiano F., Krogh V., Palli D., Vineis P., Berrino F. Relative validity and reproducibility of a food frequency dietary questionnaire for use in the Italian EPIC centres. Int. J. Epidemiol. 1997;26:S152–S160. doi: 10.1093/ije/26.suppl_1.S152. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on reasonable request from the corresponding author. The data are not publicly available due to privacy reasons.