Abstract
Vaccination currently appears to be the only strategy to contain the spread of COVID-19. At the same time, vaccine hesitancy (VH) could limit its efficacy and has, therefore, attracted the attention of Public Health Systems. This systematic review aimed at assessing anti-COVID-19 vaccine acceptance rates worldwide and at identifying populations more prone to vaccine hesitancy, for which specific interventions should be planned. PubMed database was searched using a purposely formulated string. One hundred out of the 9243 studies retrieved were considered pertinent and thus included in the analyses. VH rate was analyzed according to patient geographical origin, ethnicity, age, study setting, and method used for data collection; data from specific populations were separately analyzed. Overall, this study demonstrated significant differences in terms of VH in the general population and in the specific subgroups examined according to geographical, demographic factors, as well as associated comorbidities, underlining the need for purposely designed studies in specific populations from the different countries, to design targeted programs aimed at increasing awareness for confidence and complacency toward COVID-19 vaccines.
Keywords: coronavirus, COVID-19, global vaccination, healthcare workers, SARS-CoV-2, vaccination attitude, vaccine acceptance rate, vaccine hesitancy, vaccine intention, vaccine rejection
1. Introduction
Vaccine hesitancy (VH), defined by the SAGE working group as “delay in acceptance or refusal of vaccination despite availability of vaccination services” [1], has been recognized as a major threat to the effectiveness of this public health strategy aimed at containing and eradicating infectious diseases, deserving inclusion among major health concerns by the World Health Organization (WHO) in 2019 [2].
The potential consequences of VH are currently considered even more alarming because of the ongoing COVID-19 pandemic, against which vaccination appears to be the most efficacious strategy. Indeed, in addition to the considerable logistic and financial challenges implied in the organization of mass vaccination campaigns, VH could significantly limit or delay vaccination spread, thus preventing the rapid achievement of immunization rates required in the population (estimated at around 70% for COVID-19) [3] to fight the pandemic.
Many studies have investigated the distribution and determinants of VH, and highlighted geographical differences, with high income European countries struggling with overall high rates [4]. At the same time, other groups at a higher risk for VH have been identified, including countries with low income and education [5,6].
In this context, this study aims to systematically review literature on vaccine acceptance, to define more precisely the extent of VH associated with the ongoing vaccination campaign against COVID-19, and thus try to identify subpopulations at increased risk for VH, deserving target strategies.
2. Materials and Methods
The study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [7]. Article search was performed using the search string: (COVID-19 OR COVID 19 OR COVID* OR Coronavirus* OR coronavirus* OR SARS-CoV-2) AND (vaccin* accept* OR vaccin* hesitanc* OR vaccin* resistance OR intent* vaccine OR vaccin* confidence OR hesitanc* OR vaccin* rejection OR vaccin*) on PubMed database. Asterisks were used to include any desinence of the most relevant words in our search.
Original articles written in English, performed in adults of both genders, containing sufficient data of interest, and published from November 2019 to March 2021 were considered. Reviews, metanalysis, commentaries, editorials, and original studies not reporting the rate of vaccine acceptance/hesitancy toward COVID-19 vaccination were not included. Information on publication date, time period of data collection date, study design and setting, country, sample, gender and ethnicity of respondents and acceptance/hesitancy rate were collected from studies of interest. “Acceptance rate” was calculated considering both positive and uncertain answers showing willingness to be vaccinated (e.g., “probably yes”, “somewhat likely”, or “somewhat agree”).
Geographical distribution was defined according to the 6 regions identified by the WHO (i.e., Africa, Americas, South-East Asia, Europe, Eastern Mediterranean, and Western Pacific) [8]. After customized analyses, worldwide distribution of VH/vaccine acceptance rate was obtained. Age was collected as mean, otherwise as interval. According to the setting, studies were divided between studies performed in a hospital, and/or in an extra-hospital context. Finally, the method used to collect patient data (i.e., during patient access to healthcare services, online, telephone or email) was recorded. Data were collected and analyzed using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA).
3. Results
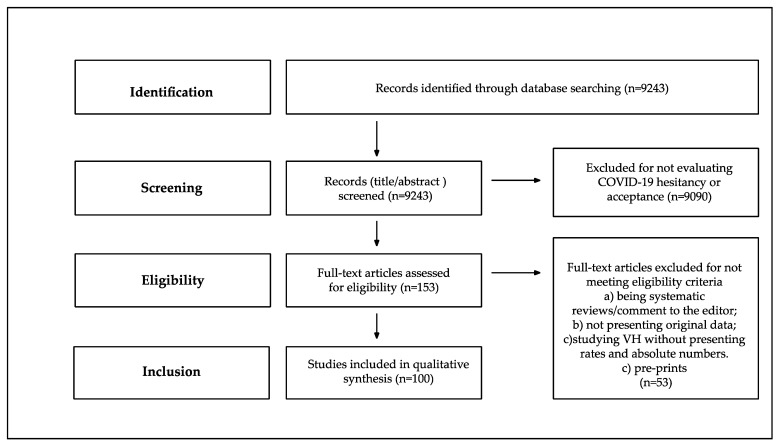
One hundred of the 9243 identified records were considered of interest and, thus, included in the analyses (Figure 1). All studies were performed in 2020, except for five for which the period of data collection was not reported. Among the studies included in our review, 86 (86%) were cross-sectional, and 8 (8%) longitudinal, while the study type was not reported for 6 (6%) of the studies.
Figure 1.
Flow chart of the study selection process.
A sensitivity analysis was performed in a representative sample of the studies selected in order to test heterogeneity in the groups using I2 Statistics. Due to the high heterogeneity that emerged (>50%), the meta-analyses was not conducted.
A time-lead stratification analysis was not conducted since samples between pre- and post- approval of vaccination were not equally distributed. The vast majority of the studies 47/49 (96%) were, in fact, conducted in 2020 before approval of the vaccine and beginning of the vaccination programs.
3.1. Study Sample Characteristics
Main sample features of the studies included in the analysis are shown in Table 1 [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108]. Patient numerosity varied widely among the studies (87–28,629 [32,45]).
Table 1.
COVID-19 confidence rates by included studies and sorted according to WHO global regional area definitions between November 2019 and March 2021.
| WHO Region | Author | State | Data Collection | Study Design | Age (Mean or Most Represented Age Group) | Participants (n) | Males (%) | Ethnicity | Target Population | Setting | Confidence Rate |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Americas | |||||||||||
| Fisher KA et al. [9] | US | 16–20 April 2020 | CS | 48 | 991 | 48.5 | Yes | Adults | Panelist | 57.6 | |
| Guidry JPD et al. [10] | US | July 2020 | CS | 46 | 788 | 50.0 | Yes | Adults | Online | 59.9 | |
| Ruiz JB et al. [11] | US | 15–16 June 2020 | CS | n.a. | 804 | 46.4 | Yes | Adults | Panelist | 62.2 | |
| Callaghan T et al. [12] | US | 28 May–8 June 2020 | CS | 45 | 5009 | 49.5 | Yes | Adults | Survey Platform | 67.7 | |
| Meyer MN et al. [13] | US | December 2020 | CS | 43 | 16,292 | n.a. | No | HCWs | 55.3 | ||
| Kreps S et al. [14] | US | July 2020 | CS | 43 | 1971 | 49.3 | No | Adults | Online | 56.0 | |
| Bogart LM et al. [15] | US | May–July 2020 | CS | 50 | 101 | 87.0 | Yes | Black americans; HIV+ | Online | 46.0 | |
| Reiter PL et al. [16] | US | May 2020 | CS | n.a. | 2006 | 43.3 | Yes | Adults | Online | 69.0 | |
| Khubchandani J et al. [17] | US | June 2020 | CS | n.a. | 1878 | 48.5 | Yes | Adults | Online | 79 | |
| Meier BP et al. [18] | US | 28–30 October 2020 | CS | 45 | 1072 | 47.9 | No | Adults | Online | 70.0 | |
| Graupensperger S et al. [19] | US | 2–13 November 2020 | CS | 20 | 647 | 35.2 | Yes | Students | Online | 91.6 | |
| Salmon DA et al. [20] | US | n.a. | CS | n.a. | 2525 | 48.2 | Yes | Adults | Online | 50.0 | |
| Ehde DM et al. [21] | US | 10 April–6 May 2020 | CS | n.a. | 486 | 17.3 | Yes | Adults with Multiple Sclerosis | Online | 84.5 | |
| Pogue K et al. [22] | US | n.a. | CS | n.a. | 316 | 50.3 | Yes | Adults | Online | 68.6 | |
| Daly M et al. [23] | US | 1 April–31 October 2020 | LS | 47 | 7547 | 47.9 | Yes | Adults | Online | 71.0 (April 2020); 53.6 (October 2020) | |
| Allen JD et al. [24] | US | 13 April–8 June 2020 | CS | 27–45 | 396 | 0 | Yes | Women aged 27–45 | Online | 56.8 | |
| Latkin C et al. [25] | US | 1st survey 24–27 March 2020, 2nd survey 5–14 May 2020, 3rd survey 22–23 July 2020 | LS | n.a. | 592 | 44.0 | Yes | Adults | Online | 59.1 | |
| Malik AA et al. [26] | US | May 2020 | CS | n.a. | 672 | 43.0 | Yes | Adults | Online | 67.0 | |
| Manning ML et al. [27] | US | 10 August–14 September 2020 | CS | n.a. | 1212 | 28.0 | Yes | Nurses; Nursing Students | Online | 60.0 (Full-time faculty); 45.0 (Adjunct faculty and students) | |
| Schrading WA et al. [28] | US | 4 January 2021 | LS | 30–39 | 1398 | 35.0 | Yes | HCWs | Hospital | 86.0 | |
| Caban-Martinez AJ et al. [29] | US | 1–31 October 2020 | CS | 40–49 | 3169 | 91.3 | Yes | Firefighters; HCWs | Online | 48.2 | |
| Shekhar R et al. [30] | US | 7 October–9 November 2020 | CS | 31–40 | 3479 | 24.8 | Yes | HCWs | Online | 36.0 | |
| Rungkitwattanakul D et al. [31] | US | n.a. | n.a. | n.a. | 90 | 60.0 | Yes | Adults on dyalisis | Hospital | 49.0 | |
| Mellis AM et al. [32] | US | 10–27 September 2020 | n.a. | 43 | 87 | 46.0 | No | Adults with Substance Use Disorders | Telephone; Video-conferencing | 45.0 (Immediate readiness); 8.0 (Readiness after a delay) | |
| Amin DP et al. [33] | US | 11–23 January 2021 | CS | 41–50 | 240 | 43.0 | Yes | HCWs | Online | 92.0 | |
| Kuter BJ et al. [34] | US | November–December 2020 | CS | na. | 12,034 | 21.0 | Yes | HCWs | 63.7 | ||
| Unroe KT et al. [35] | US | 14–17 November 2020 | CS | 41–60 | 8243 | 12.6 | Yes | HCWs | Text message; E-mail | 45.0 | |
| Gatwood J et al. [36] | US | 3–8 June 2020 | CS | 25–44 | 1000 | 49.0 | Yes | Adults | Online | 54.1 | |
| Lucia VC et al. [37] | US | n.a. | CS | n.a. | 168 | 43 | No | Medical students | Online | 98.0 | |
| Pamplona G et al. [38] | US | 13–21 January 2021 | n.a. | n.a. | 157 | n.a. | No | HCWs | Hospital and Home-care | 96.2 | |
| Kociolek LK et al. [39] | US | 21 December 2020–13 January 2021 | CS | ≤40 | 4448 | 17.0 | Yes | HCWs | 59.8 | ||
| Gadoth A et al. [40] | US | 24 September–16 October 2020 | CS | 30–49 | 540 | 28.3 | Yes | HCWs | Hospital | 33.2 (Immediately); 65.5 (After a delay) | |
| Shaw J et al. [41] | US | 23 November–5 December | CS | 42 | 5287 | 27.2 | Yes | Adults | Hospital | 57.5 | |
| CastañedaasVasquez DE et al. [42] | Mexico | October–December 2020 | CS | 21 (median age) | 543 | 32.8 | Yes | HCWs | Online | 94.5 | |
| Taylor S et al. [43] | US; Canada | 6–19 May 2020 | CS | 53 | 3674 | 57.0 | Yes | Adults | Online | 80.0 (Canadians); 75.0 (U.S.) | |
| Europe | |||||||||||
| Williams L et al. [44] | UK | April 2020 | CS | 70 (older adults), 43 (participants with chronic respiratory patologies) | 527 | 43.3 | No | Elderly with chronic respiratory diseases | Online | 85.6 | |
| Jackson SE et al. [45] | UK | 7 September–5 October 2020 | CS | n.a. | 28,629 | n.a. | No | Adults | Online | 65.8 (Non-smokers); 66.0 (Ex-smokers) e 50.9 (Smokers) | |
| Williams L et al. [46] | UK | 1st survey: 20 May 12 June 2020, 2nd survey: August 2020 | LS | n.a. | 3436 (1); 2016 (2) | 19.4 (1); 17.6 (2) | Yes | Adults | Online | 74.0 (1); 78.0 (2) | |
| Sherman SM et al. [47] | UK | 14–17 July 2020 | CS | 46 | 1,5 | 49.0 | Yes | Adults | Online | 64.0 | |
| Freeman D et al. [48] | UK | 24 September–17 October | CS | 47 | 5114 | 50.3 | Yes | n.a. | Online | 71.7 | |
| Batty GD et al. [49] | UK | 4 November 2020 | LS | 53 | 11,955 | n.a. | No | n.a. | Outpatient | 82.8 | |
| Robertson E et al. [50] | UK | 24 November–1 December 2020 | LS | 55–64 | 12,035 | 38.8 | Yes | Households | Online | 82 | |
| Gagneux-Brunon A et al. [51] | France | 26 March–2 July 2020 | CS | 30–49 | 2047 | 26.0 | No | HCWs | Social Media; E-mail; Hospital Website and Written Surveys | 76.9 | |
| Ward JK et al. [52] | France | April 2020 | CS | 35–64 | 5018 | 56.6 | No | Adults | Panelist | 76.0 | |
| Detoc M et al. [53] | France | 26 March–20 April 2020 | CS | 30–49 | 3656 | 32.6 | No | Adults | Social Media; E-mail; Hospital Website and Written Surveys | 77.6 | |
| Montagni I et al. [54] | France | 8–11 May 2020 | CS | 28 | 1644 | 21.5 | No | Adults | Online | 70.5 | |
| Barrière J et al. [55] | France | 11 November–12 December 2020 | CS | 67 (median) | 536 | 44.0 | No | Oncological patients | Outpatient | 53.7 | |
| Green MS et al. [56] | Israel | October 2020 | CS | n.a. | 957 | 45.0 | Yes | Adults older than 30 | Panelist | 59.0–92.3 | |
| Dror AA et al. [57] | Israel | March 2020 | CS | n.a. | 1941 | n.a. | No | HCWs; Adults | Online | 75.0 | |
| Zigron A et al. [58] | Israel | March–April 2020 | CS | n.a. | 506 | 43.0 | No | Dentists | Online | 85.0 | |
| La Vecchia C et al. [59] | Italy | 16–28 September 2020 | CS | ≥55 | 1055 | 48.2 | No | Adults | Panelist | 53.7 | |
| Prati G et al. [60] | Italy | April 2020 | CS | 32 | 624 | 46.0 | Yes | Adults | E-mail; Online; Social Media | 75.8 | |
| Barello S et al. [61] | Italy | n.a. | CS | 23 | 934 | 20.4 | No | University students | 86.1 | ||
| Di Gennaro F et al. [62] | Italy | October 2020 | CS | 36 | 1723 | 47.0 | No | HCWs | Online | 67.0 | |
| Graffigna G et al. [63] | Italy | n.a. | CS | 44 | 1004 | 49.0 | No | Adults | Online | 58.6 | |
| Gerussi V et al. [64] | Italy | September–November 2020 | CS | 53 | 599 | 46.6 | No | Adults SARS-CoV-2 positive | Telephone | 40.9 | |
| Pastorino R et al. [65] | Italy | 8 June–2 July 2020 | CS | n.a. | 436 | n.a. | No | University students | Online | 95.1 | |
| Priori R et al. [66] | Italy | n.a. | CS | n.a. | 626 (Rheumatological Patient); 345 (Control Group) | n.a. | No | Adults with rheumatological diseases | Online | 54.9 | |
| Barello S et al. [67] | Italy | 27 November–3 December 2020 | n.a. | n.a. | 1005 | n.a. | No | Adults | Online | 58.0 | |
| Karlsson LC et al. [68] | Finland | 1st survey: May 2020–June 2020, 2nd survey: 30 March 2020–14 April 2020 3rd survey: 3–17 April 2020 | CS | n.a. | 825 (S1); 205 (S2); 1325 (S3) | 21.2 (S1); 30.7 (S2); 19.0 (S3) | Yes | Parents/Guardiands | Online | 73.9 (S1); 77.8 (S2); 72.9 (S3) | |
| Szmyd B et al. [69] | Poland | 22–25 December 2020 | CS | 20 (median) | 1971 | 12.3 (Medical students); 36.9 (Non-medical students) | Yes | University students | Online | 92.0 (Medical students); 59.4 (Non-medical students) | |
| Feleszko W et al. [70] | Poland | 2–9 June 2020 | CS | n.a. | 1066 | n.a. | No | Adults | Online | 72.0 | |
| Papagiannis D et al. [71] | Greece | 15–22 December 2020 | CS | 48 | 340 | 51.2 | No | HCWs | Hospital | 78.5 | |
| Serrazina F et al. [72] | Portugal | 21 December 2020–3 January 2021 | CS | 45 | 256 | 27.0 | No | Adults with Multiple Sclerosis | Hospital; Online | 80.9 | |
| Eguia H et al. [73] | Spain | 10 September–23 November 2020 | CS | 51 | 731 | 44.0 | No | Adults | Social Media | 77.6 | |
| Yigit M et al. [74] | Turkey | n.a. | CS | 40 | 428 | 36.4 | No | Parents/Guardians | Social Media; In-person | 62.6 (National vaccine); 33.9 (International) | |
| African Region | |||||||||||
| Ditekemena JD et al. [75] | DRC | 24 August–8 September 2020 | CS | 35 | 4131 | 31.6 | No | n.a. | Online | 55.9 | |
| Dinga JN et al. [76] | DRC | 5 August 2021 | CS | n.a. | 2512 | 45.1 | No | Adults | Online; In-person | 15.4 | |
| Kabamba Nzaji M et al. [77] | DRC | March–April 2020 | CS | 40 | 613 | 50.9 | No | HCWs | Hospital; Online | 27.7 | |
| Eastern Mediterranean Region | |||||||||||
| Saied SM et al. [78] | Egypt | 08–15 January 2021 | CS | 20 | 2133 | 34.8 | Medical students | Online | 34.9 | ||
| Al-Qerem WA et al. [79] | Jordan | October 2020 | CS | 18–29 | 1141 | 33.5 | No | Adults | Social Media | 36.8 | |
| Sallam M et al. [80] | Jordan; Kuwait | 14–18 December 2020 | CS | 24 (Jordan), 30 (Kuwait) | Giordania, 2173; Kuwait 771; Saudi Arabia 154 | 30.6 (Jordan); 36.1 (Kuwait); 23.4 (Saudi Arabia) | Yes | Adults | Online | 29.4 | |
| Qattan AMN et al. [81] | Saudi Arabia | 08–14 December 2020 | CS | n.a. | 673 | n.a. | No | Adults | Online | 50.5 | |
| Al-Mohaithef M et al. [82] | Saudi Arabia | n.a. | CS | n.a. | 992 | 34.2 | No | Adults | Online | 64.7 | |
| Alqudeimat Y et al. [83] | Kuwait | 26 August–1 September 2020 | CS | n.a. | 2368 | 31.8 | No | Adults | Online | 53.1 | |
| Alabdulla M et al. [84] | Quatar | 15 October–15 November 2020 | CS | 36–45 | 7821 | 59.43 | No | n.a. | Online | 60.5 | |
| Western Pacific Region | |||||||||||
| Dodd RH et al. [85] | Australia | 17–21 April | CS | 56–90 | 4362 | n.a. | No | Adults | Online | 85.8 | |
| Edwards B et al. [86] | Australia | August 2020 | LS | n.a. | 3061 | n.a. | No | Adults | Online, Telephone | 58.5 | |
| Faasse K et al. [87] | Australia | 2–9 March 2020 | CS | 30–49 | 2174 | 23.1 | Yes | Adults | Online; Social Media | 81.1 | |
| Rhodes A et al. [88] | Australia | 15–23 June 2020 | n.a. | n.a. | 2018 | n.a. | No | Parents/Guardians | Hospital; Online | 75.8 | |
| Wang K et al. [89] | Hong Kong SAR | February–March 2020 | CS | 30–39 | 806 | 19.3 | No | Nurses | 40.0 | ||
| Yu Y et al. [90] | Hong Kong SAR | 16–30 September 2020 | CS | n.a. | 450 | 31.0 | No | Adults | Telephone | 4.2–38 | |
| Gan L et al. [91] | China | October–November 2020 | CS | 18–29 | 1009 | 37.9 | No | Adults | Online | 60.4 | |
| Lin Y et al. [92] | China | May 2020 | CS | 26–35 | 3541 | 48.1 | No | Adults | Social Media | 83.3 | |
| Wang J et al. [93] | China | March 2020 | CS | n.a. | 2058 | 45.8 | No | Adults | Online | 91.3 | |
| Wang J et al. [94] | China | 1st survey March 2020, 2nd survey November–December 2020 | LS | n.a. | 791 | 46.9 | No | Adults | Online | 91.9 (1); 88.6 (2) | |
| Zhang KC et al. [95] | China | 1–7 September2020 | CS | n.a. | 2053 | 42.6 | No | Factory workers | Online | 80.6 (If 80.0% vaccine efficacy and free of charge) | |
| Mo PK et al. [96] | China | 01–28 November 2020 | CS | 19 | 6922 | 36.4 | Yes | University students | Online | 78.9 (Vaccine for free); 60.2 (Vaccine fee-based) | |
| Zhang KC et al. [97] | China | 1–7 September 2020 | CS | n.a. | 2053 | 37.5 | No | Factory workers; Parents/Guardians | Online | 72.6 | |
| Yoda T et al. [98] | Japan | September 2020 | n.a. | 45 | 1100 | 53.0 | No | Adults | Panelist | 65.7 | |
| Wong LP et al. [99] | Malaysia | 3–12 April 2020 | CS | 31–40 | 1159 | 44.0 | Yes | Adults | Social Media | 94.3 | |
| South-East Asia Region | |||||||||||
| Parajuli J et al. [100] | Nepal | April–May 2020 | CS | 20–29 | 230 | 50.4 | No | HCWs | Hospital | 94.3 | |
| Harapan H et al. [101] | Indonesia | 25 March–6 April 2020 | CS | n.a. | 1359 | 34.3 | No | Adults | Online | 93.3 | |
| More than one Region | |||||||||||
| Chew NWS et al. [102] | China; India; Indonesia; Singapore; Vietnam and Bhutan | 12–31 December 2020 | CS | 33 | 1,72 | 39.0 | No | HCWs | Online; Telephone | 96.2 | |
| Lazarus JV et al. [103] | China; Brazil; South Africa; South Korea; Mexico; US; India; Spain; Ecuador; UK; Italy; Canada; Germany; Singapore; Sweden; Nigeria; France; Poland; Russia | 16–20 June 2020 | CS | 25–54 | 13,426 | 45.8 | No | Adults | Online; Telephone | 71.5 Overall; China 88.6; Brazil 85.4; South Africa 81.6; South Korea 79.8; Mexico 76.3; US 75.4; India 74.5; Spain 74.3; Ecuador 71.9; UK 71.5; Italy 70.8; Canada 68.7; Germany 67.9; Singapore 67.9; Sweden 65.2; Nigeria 65.2; France 58.9; Poland 56.3; Russia 54.9 | |
| Skjefte M et al. [104] | Worldwide | 28 October–18 November 2020 | CS | 34 | 17,871 | 0 | No | Pregnant women; Mothers | Online | 52.0 (Pregnant women); 73.4 (Non-pregnant women) | |
| Goldman RD et al. [105] | US; Canada; Japan; Spain; Switzerland | 26 March–31 May 2020 | CS | 40 | 1552 | 25.5 | No | Caregivers | Online | 65.2 | |
| Neumann-Böhme S et al. [106] | Denmark; UK; Italy; Portugal; Netherland; Germany; France | April 2020 | CS | n.a. | 1000 | n.a. | No | Adults | Online | 80.0 Denmark; 79.0 UK; 77.3 Italy; 75.0 Portugal; 73.0 Netherlands; 70.0 Germany; 62.0 France. | |
| Verger P et al. [107] | France; Belgium; Canada | October–November 2020 | CS | 40–59 | 2678 | 30.8 | No | HCWs | Online; Telephone; E-mail | 71.6 Overall; France 46.5 (Certainly), 28.8 (Probably); Belgium 39.5 (Certainly), 36.5 (Probably); Canada 42.9 (Certainly), 27.6 (Probably) | |
| Murphy J et al. [108] | Ireland; UK | n.a. | CS | n.a. | 1041 (Ireland); 2025 (UK) | 48.2 (Ireland); 48.3 (UK) | Yes | Adults | n.a. | Ireland 65.0; UK 69.0 |
US: United States of America; UK: United Kingdom; DRC: Democratic Republic of Congo; CS: Cross Sectional study; LS: Longitudinal Study; HCWs: Health Care Workers.
Regarding gender distribution, female predominance was observed in 87 studies (n = 87) [10], and male predominance in 12, being the highest male prevalence (91.3%) observed in the study by Caban-Martinez et al. performed in US firefighters and health care workers (HCWs) [29]. Males and females were equally distributed in the study by Guidry et al. [10].
Mean sample age was reported as interval in 25 (25%) studies, and as mean in 38 (38%) studies, while this information was not given in 37 (37%). Ethnicity was reported in 43 (43%) studies.
3.2. Anti-COVID19 Vaccine Acceptance Rate in the General Population and in Specific Target Populations
Forty-nine (49%) studies were performed in the general adult population; 22 (22%) included HCWs, 9 (9%) patients with chronic diseases (i.e., HIV, multiple sclerosis, chronic respiratory diseases, kidney insufficiency requiring dialytic treatment, neoplasia, rheumatological diseases, and conditions induced by substance use) and their caregivers, 8 (8%) university students, 4 (4%) parents/guardians, 2 (2%) factory workers, 1 (1%) pregnant women and 1 (1%) SARS-CoV-2 positive patient. Five studies (5%) did not target any specific population. Results regarding the vaccine confidence rate for each study are shown in Table 1.
3.2.1. General Population
According to the analysis performed in the general population, the lowest rates of vaccine confidence were found in Hong Kong (4.2–38%), Middle East Area (Jordan and Kuwait, 29.4% and 36.8%, respectively [79,80]) followed by the Democratic Republic of Congo (15.4%) [76,90]. On the other hand, the highest acceptance rate (94.3%) was reported in Malaysia [99].
3.2.2. Specific Populations
In the group of HCWs, the lowest confidence rate (27.7%) was reported in the Democratic Republic of Congo [77], followed by the US (36%) [30], while the highest rate (96.2%) was reported in Asia (China, India, Republic of Indonesia, Singapore, Vietnam and Bhutan) [102].
When considering patients affected by chronic diseases and caregivers, the lowest confidence rate was found among American adults affected by substance use diseases (45%) [32], while the highest (85.6%) was reported in elderly affected by chronic respiratory diseases [44].
Among university students, the lowest acceptance rate (34.9%) was found in Egypt [37], and the highest in the US (98%) [78].
Gender distribution was analyzed in 84 (84%) studies, while 2 (2%) studies analyzed vaccine acceptance in the female population and 14 (14%) studies did not report this data.
Finally, Skjefte et al. reported a confidence rate of 52% among pregnant women and of 75.8% among parents/guardians in Australia [104].
3.3. Differences among WHO Regional Areas: General Population and HCWs
Most of the studies were conducted in the Region of the Americas (n = 35, 35%; 33 in the US; one in the US and Canada, and one in Mexico), followed by the European Region (n = 31; 31%), the Western Pacific Region (n = 15; 15%), the Eastern Mediterranean Region (n = 7; 7%), the African Region (n = 3; 3%) and the Southeastern Asian Region (n = 2; 2%). Finally, seven studies included patients from more than one region (Table 1).
In the European Region, the confidence rate varied from 40.9% to 92.3% in the general population, and from 54.9% to 95.1% in HCWs [56,64,65,66].
In the Region of the Americas, vaccine confidence varied between 36% and 98% in the general population and HCWs [30,37].
For the African Region, it was only identified by a study by Dinga et al. showing a confidence rate of 15.4% in the general population [76], and another by Kabamba Nzaji et al. reporting an acceptance rate of 27.7% in HCWs [77].
In the Eastern Mediterranean Region, confidence rate in the general population varied from 29.4% to 64.7% [80,82]; no study focused on HCWs.
In the Western Pacific Region, the various studies reported confidence rates from 4.2% to 94.3% in the general population [90,99]; a single study focusing on nurses showed a confidence rate of 40% [89].
According to the two studies available for the South Eastern Asian Region, confidence rates were 94.3% in HCWs and 93.3% for the general population [100,101].
Studies including more than one Region showed confidence rates of 71.6–96.2% for HCWs, and of 71.5–80% for the general population [102,103,106,107].
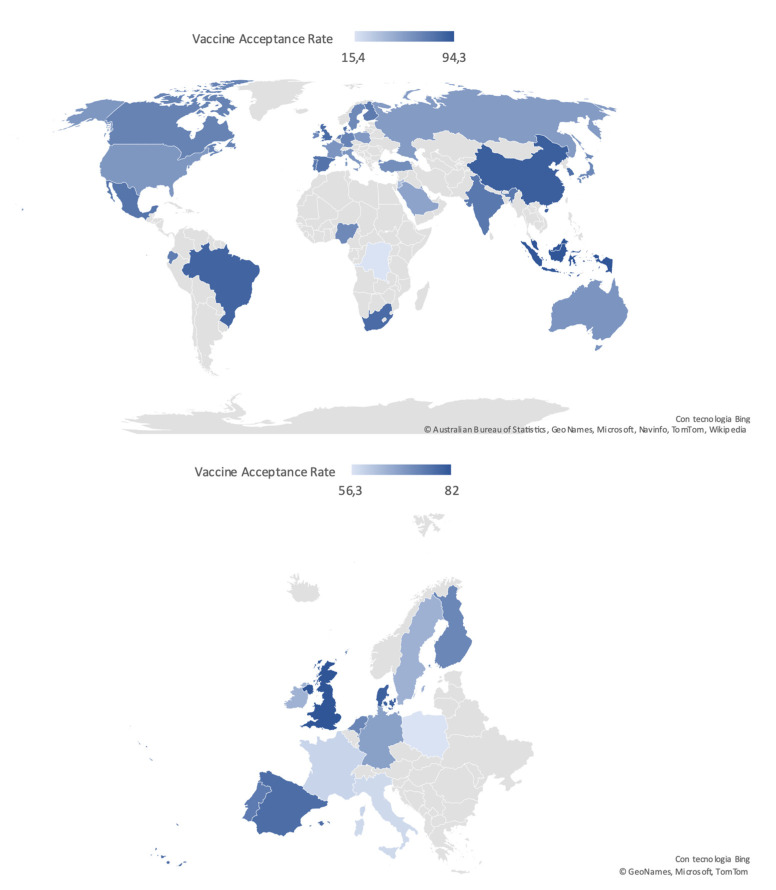
Acceptance rate distribution reported in the general population worldwide and in the European Countries is depicted in Figure 2.
Figure 2.
Worldwide and European distribution of COVID-19 vaccine acceptance rates in the general population, defined according to the most recent available data.
4. Discussion
COVID-19 infection has represented a major health plague worldwide since 2020, for which vaccination currently appears to be the only efficacious strategy to achieve disease control. In this context, vaccine hesitancy (VH), responsible for outbreaks and epidemics of other infectious diseases (i.e., measles) secondary to the drop of immunized people under the herd immunity threshold [109], represents a major threat, deserving rapid identification of predisposing factors, and targeted countermeasures. This systematic review demonstrated largely variable rates of vaccine acceptance worldwide, in the general population, as well as in specific sub-populations.
4.1. Gender Distribution
In most of the selected studies females were more represented than males. A higher prevalence of VH for the different vaccines has been widely reported in literature [110], and it has been hypothesized that this may be due to a lower trust in the Institutions and in the scientific community, an important driver of VH, in women [111]. With regards to COVID-19, the higher prevalence of severe infections and death among males [112] could have increased male risk perception and, subsequently, vaccine acceptance. At the same time, it has to be remarked that this study did not show a clear correlation between the number of males included in the studies surveys and vaccine acceptance. Therefore, several other factors might have influenced this relation.
4.2. Health Care Workers
Extremely variable vaccine confidence rates were reported among health care workers (HCWs). Following the geographical distribution, the lowest rates were observed in the Democratic Republic of Congo (27.7%) and the US (36.0%), and the highest (96.2%) in Eastern Asian countries (China, India, Republic of Indonesia, Singapore, Vietnam, and Bhutan) [30,77,102]. High rates of VH among HCWs are particularly alarming for their crucial role during the SARS-CoV-2 pandemic, in terms of daily patient care but also health literacy promotion for the general population. The wide range of confidence rates towards the COVID-19 vaccination found globally could be explained considering the different roles and relation to the patients played by the different HCWs (e.g., physician, nurse, pharmacist or clerical worker) [113]. Indeed, HCWs involved in direct patient care were found to be more confident, suggesting that an increased vaccine hesitancy could be related to a less direct contact with the patient and, consequently, a reduced risk perception of COVID-19 associated morbidity [34]. At the same time, the high rates of VH reported even in HCWs directly involved in patient care [30] underlines the need of interventions specifically addressed to this category of workers to increase their awareness towards the risk of unsuccessful vaccine campaigns [114].
4.3. Patients Affected by Specific Diseases
Some studies showed a higher vaccine confidence rate in patients with chronic diseases as compared to the general population, as might be expected (i.e., 80.9% and 84.5% in patients with multiple sclerosis from Portugal and the US, respectively; or 85.6% in those with chronic respiratory diseases from UK), possibly secondary to the perception of frailty towards severe disease and death [115,116], which is true especially for respiratory diseases [117] and MS [118].
Other studies, focusing on oncologic (53.7%) and rheumatologic patients (54.9%), showed acceptance rates similar to the general population living in the same countries. Remarkably, some subpopulations showed particularly low acceptance rates, i.e., black adults with HIV (46%), people with drug addiction (45%), adults undergoing chronic dialysis (49%), and, finally, SARS-CoV-2 positives. Patients who had already been infected by the virus could possibly perceive themselves as immunized against COVID-19, independently from its variants, thus reducing the perceived advantages associated with vaccination and the willingness to be vaccinated. In the remaining categories, reluctance to accept a vaccine against COVID-19 might be due to the confounding effect of low income and education, which have been shown to be risk factors for chronic kidney disease, substance abuse, and HIV infection [119,120,121], or, finally, to the possible wariness of frail patients towards potential side effects of the vaccines.
4.4. Surveys Administration Setting
Almost all surveys were conducted online, sending questionnaires via e-mail or using other social media. The dissemination of these versatile information tools has undoubtedly facilitated and speeded up the data collection process, especially during COVID-19 pandemics, in the targeted populations. On the other hand, their use could be responsible for population selection bias, e.g., exclusion of the elderly, and problems in questionnaire filling/misunderstandings, due to the lack/difficulty of interaction with researchers.
Finally, online platforms (in particular the new social media) are considered by some recent studies as carriers of disbelief and skepticism about vaccines [122,123,124], potentially leading to higher rates of hesitancy in the average users of these online platforms.
All these aspects could contribute to the variability of vaccine confidence rates.
4.5. Geographical Distribution
The prevalence of vaccine acceptance/refusal widely varied across countries and WHO Regions, supporting the definition of VH given by the SAGE Group as “complex and context specific, varying across time, place and vaccines” [1]. This could be explained by the complex and unpredictable interaction of demographic, cultural, and social factors, including previously mentioned demographic and educational ones, but also people’s confidence in health and other governmental institutions, and, on the other hand, the tightness of governmental control on social and information media.
The lowest acceptance rates among the general population were observed in Hong Kong, ranging from 4.2% to 38% depending on the type of vaccine evaluated in the study, and in the Democratic Republic of the Congo, corresponding to 15.4%. These two countries present vastly different cultures and demographic features, but share a recent history of political instability that should be considered while examining VH rate under a socio-political perspective.
Conversely, the highest rates were found in China (91.9%), Malaysia (94.3%), and Indonesia (93.3%). These results could reflect a higher awareness toward the terrible consequences of SARS-CoV-2 virus diffusion, as these Asian countries were among the first to be hit by the COVID-19 pandemic, and have consequent confidence in vaccines.
The European Region was characterized by a very broad variability of vaccine acceptance rates, with the highest rates reported in United Kingdom (82%), and the lowest in Italy (40.9%) and in France (53.7%), reflecting once again the impact of cultural and sociodemographic heterogeneity of the examined geographical area on VH [12].
4.6. Limitations and Strengths
As previously mentioned, the main limitation of the study is represented by the great heterogeneity of the studies included, despite the selection performed. Moreover, some of them lack important methodological/patient information. For these reasons it was opted for a systematic review instead of a metanalysis.
On the other hand, this work presents some strengths. First, the use of a very inclusive search string aiming to be as sensitive as possible. Thanks to this strategy the analysis started from a considerable pool of articles (more than 9000) reducing the risk of losing important data, that were then carefully analyzed to remove preprints or studies not presenting original data, thus increasing the study sensitivity while refining the research. Finally, data collected from studies of interest were analyzed according to some demographic, geographic, clinical, and social factors, to try to highlight major determinants of vaccine hesitancy.
5. Conclusions
VH is a global and increasingly wide-spreading phenomenon. Nonetheless, remarkable differences in vaccine acceptance rates can be observed across countries and subpopulations, supporting the underlying complex and unpredictable interplay among demographic, geopolitical and cultural aspects, which are hard to be understood and discriminated. At the same time, focused research aimed at formulating targeted strategies to improve vaccine awareness, confidence and acceptance prevalence is of utmost importance.
Since communication, especially via social media, has been clearly demonstrated to play a pivotal role in determining adherence to vaccination, these instruments should be better exploited by the governmental institutions and the scientific community to increase people trust in the evidence-based rationale and rigorous production process, as well as expected short and long-term benefits of universal vaccination for the ongoing COVID-19 and potential future pandemics.
Author Contributions
Conceptualization and methodology, all the authors equally contributed; formal analysis, M.G.S. and E.G.; investigation and data curation, M.G.S., Z.D.V., E.G. and M.M.; writing—original draft preparation, M.G.S. and E.G.; writing—review and editing, Z.D.V., M.M., D.T. and F.G.; supervision, D.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.MacDonald N.E. SAGE Working Group on Vaccine Hesitancy Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 2.Ten Health Issues WHO Will Tackle This Year. [(accessed on 20 July 2021)]; Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 3.Britton T., Ball F., Trapman P. A Mathematical Model Reveals the Influence of Population Heterogeneity on Herd Immunity to SARS-CoV-2. Science. 2020;369:846–849. doi: 10.1126/science.abc6810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines. 2021;9:160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bocquier A., Cortaredona S., Fressard L., Galtier F., Verger P. Seasonal influenza vaccination among people with diabetes: Influence of patients’ characteristics and healthcare use on behavioral changes. Hum. Vaccin. Immunother. 2020;16:2565–2572. doi: 10.1080/21645515.2020.1729628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paul E., Steptoe A., Fancourt D. Attitudes towards Vaccines and Intention to Vaccinate against COVID-19: Implications for Public Health Communications. Lancet Reg. Health Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Countries Overview, World Health Organization. [(accessed on 20 July 2021)]; Available online: https://www.who.int/countries.
- 9.Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine: A Survey of U.S. Adults. Ann. Intern. Med. 2020;173:964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guidry J.P.D., Laestadius L.I., Vraga E.K., Miller C.A., Perrin P.B., Burton C.W., Ryan M., Fuemmeler B.F., Carlyle K.E. Willingness to Get the COVID-19 Vaccine with and without Emergency Use Authorization. Am. J. Infect. Control. 2021;49:137–142. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruiz J.B., Bell R.A. Predictors of Intention to Vaccinate against COVID-19: Results of a Nationwide Survey. Vaccine. 2021;39:1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Callaghan T., Moghtaderi A., Lueck J.A., Hotez P., Strych U., Dor A., Fowler E.F., Motta M. Correlates and Disparities of Intention to Vaccinate against COVID-19. Soc. Sci. Med. 2021;272:113638. doi: 10.1016/j.socscimed.2020.113638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meyer M.N., Gjorgjieva T., Rosica D. Trends in Health Care Worker Intentions to Receive a COVID-19 Vaccine and Reasons for Hesitancy. JAMA Netw. Open. 2021;4:e215344. doi: 10.1001/jamanetworkopen.2021.5344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kreps S., Prasad S., Brownstein J.S., Hswen Y., Garibaldi B.T., Zhang B., Kriner D.L. Factors Associated With US Adults’ Likelihood of Accepting COVID-19 Vaccination. JAMA Netw. Open. 2020;3:e2025594. doi: 10.1001/jamanetworkopen.2020.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bogart L.M., Ojikutu B.O., Tyagi K., Klein D.J., Mutchler M.G., Dong L., Lawrence S.J., Thomas D.R., Kellman S. COVID-19 Related Medical Mistrust, Health Impacts, and Potential Vaccine Hesitancy Among Black Americans Living With HIV. J Acquir. Immune Defic. Syndr. 2021;86:200–207. doi: 10.1097/QAI.0000000000002570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 Vaccine among Adults in the United States: How Many People Would Get Vaccinated? Vaccine. 2020;38:6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J Community Health. 2021;46:270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meier B.P., Dillard A.J., Lappas C.M. Predictors of the Intention to Receive a SARS-CoV-2 Vaccine. J. Public Health. 2021:fdab013. doi: 10.1093/pubmed/fdab013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graupensperger S., Abdallah D.A., Lee C.M. Social Norms and Vaccine Uptake: College Students’ COVID Vaccination Intentions, Attitudes, and Estimated Peer Norms and Comparisons with Influenza Vaccine. Vaccine. 2021;39:2060–2067. doi: 10.1016/j.vaccine.2021.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salmon D.A., Dudley M.Z., Brewer J., Kan L., Gerber J.E., Budigan H., Proveaux T.M., Bernier R., Rimal R., Schwartz B. COVID-19 Vaccination Attitudes, Values and Intentions among United States Adults Prior to Emergency Use Authorization. Vaccine. 2021;39:2698–2711. doi: 10.1016/j.vaccine.2021.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ehde D.M., Roberts M.K., Herring T.E., Alschuler K.N. Willingness to Obtain COVID-19 Vaccination in Adults with Multiple Sclerosis in the United States. Mult. Scler. Relat. Disord. 2021;49:102788. doi: 10.1016/j.msard.2021.102788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pogue K., Jensen J.L., Stancil C.K., Ferguson D.G., Hughes S.J., Mello E.J., Burgess R., Berges B.K., Quaye A., Poole B.D. Influences on Attitudes Regarding Potential COVID-19 Vaccination in the United States. Vaccines. 2020;8:582. doi: 10.3390/vaccines8040582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daly M., Robinson E. Willingness to Vaccinate Against COVID-19 in the U.S.: Representative Longitudinal Evidence from April to October 2020. Am. J. Prev. Med. 2021;60:766–773. doi: 10.1016/j.amepre.2021.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Allen J.D., Abuelezam N.N., Rose R., Fontenot H.B. Factors Associated with the Intention to Obtain a COVID-19 Vaccine among a Racially/Ethnically Diverse Sample of Women in the USA. Transl. Behav. Med. 2021;11:785–792. doi: 10.1093/tbm/ibab014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Latkin C., Dayton L.A., Yi G., Konstantopoulos A., Park J., Maulsby C., Kong X. COVID-19 Vaccine Intentions in the United States, a Social-Ecological Framework. Vaccine. 2021;39:2288–2294. doi: 10.1016/j.vaccine.2021.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 Vaccine Acceptance in the US. E. Clin. Med. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Manning M.L., Gerolamo A.M., Marino M.A., Hanson-Zalot M.E., Pogorzelska-Maziarz M. COVID-19 Vaccination Readiness among Nurse Faculty and Student Nurses. Nurs. Outlook. 2021:S0029655421000233. doi: 10.1016/j.outlook.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schrading W.A., Trent S.A., Paxton J.H., Rodriguez R.M., Swanson M.B., Mohr N.M., Talan D.A., Project COVERED Emergency Department Network. Bahamon M., Carlson J.N., et al. Vaccination Rates and Acceptance of SARS-CoV-2 Vaccination among U.S. Emergency Department Health Care Personnel. Acad. Emerg. Med. 2021;28:455–458. doi: 10.1111/acem.14236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Caban-Martinez A.J., Silvera C.A., Santiago K.M., Louzado-Feliciano P., Burgess J.L., Smith D.L., Jahnke S., Horn G.P., Graber J.M. COVID-19 Vaccine Acceptability Among US Firefighters and Emergency Medical Services Workers: A Cross-Sectional Study. J. Occup. Environ. Med. 2021;63:369–373. doi: 10.1097/JOM.0000000000002152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shekhar R., Sheikh A.B., Upadhyay S., Singh M., Kottewar S., Mir H., Barrett E., Pal S. COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines. 2021;9:119. doi: 10.3390/vaccines9020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rungkitwattanakul D., Yabusaki A., Singh D., Lawson P., Nwaogwugwu U., Iheagwara O.S., Mere C. COVID-19 Vaccine Hesitancy among African American Hemodialysis Patients: A Single-center Experience. Hemodial. Int. 2021;25:410–412. doi: 10.1111/hdi.12922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mellis A.M., Kelly B.C., Potenza M.N., Hulsey J.N. Trust in a COVID-19 Vaccine among People with Substance Use Disorders. Drug Alcohol Depend. 2021;220:108519. doi: 10.1016/j.drugalcdep.2021.108519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Amin D.P., Palter J.S. COVID-19 Vaccination Hesitancy among Healthcare Personnel in the Emergency Department Deserves Continued Attention. Am. J. Emerg. Med. 2021:S0735675721001005. doi: 10.1016/j.ajem.2021.01.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kuter B.J., Browne S., Momplaisir F.M., Feemster K.A., Shen A.K., Green-McKenzie J., Faig W., Offit P.A. Perspectives on the Receipt of a COVID-19 Vaccine: A Survey of Employees in Two Large Hospitals in Philadelphia. Vaccine. 2021;39:1693–1700. doi: 10.1016/j.vaccine.2021.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Unroe K.T., Evans R., Weaver L., Rusyniak D., Blackburn J. Willingness of Long-Term Care Staff to Receive a COVID-19 Vaccine: A Single State Survey. J. Am. Geriatr. Soc. 2021;69:593–599. doi: 10.1111/jgs.17022. [DOI] [PubMed] [Google Scholar]
- 36.Gatwood J., McKnight M., Fiscus M., Hohmeier K.C., Chisholm-Burns M. Factors Influencing Likelihood of COVID-19 Vaccination: A Survey of Tennessee Adults. Am. J. Health Syst. Pharm. 2021;78:879–889. doi: 10.1093/ajhp/zxab099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lucia V.C., Kelekar A., Afonso N.M. COVID-19 Vaccine Hesitancy among Medical Students. J. Public Health. 2020:fdaa230. doi: 10.1093/pubmed/fdaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pamplona G.M., Sullivan T., Kotanko P. COVID-19 Vaccination Acceptance and Hesitancy in Dialysis Staff: First Results from New York City. Kidney Int. Rep. 2021;6:1192–1193. doi: 10.1016/j.ekir.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kociolek L.K., Elhadary J., Jhaveri R., Patel A.B., Stahulak B., Cartland J. Coronavirus Disease 2019 Vaccine Hesitancy among Children’s Hospital Staff: A Single-Center Survey. Infect. Control. Hosp. Epidemiol. 2021;42:775–777. doi: 10.1017/ice.2021.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gadoth A., Halbrook M., Martin-Blais R., Gray A., Tobin N.H., Ferbas K.G., Aldrovandi G.M., Rimoin A.W. Cross-Sectional Assessment of COVID-19 Vaccine Acceptance Among Health Care Workers in Los Angeles. Ann. Intern. Med. 2021;174:882–885. doi: 10.7326/M20-7580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shaw J., Stewart T., Anderson K.B., Hanley S., Thomas S.J., Salmon D.A., Morley C. Assessment of US Healthcare Personnel Attitudes Towards Coronavirus Disease 2019 (COVID-19) Vaccination in a Large University Healthcare System. Clin. Infect. Dis. 2021:ciab054. doi: 10.1093/cid/ciab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Castañeda-Vasquez D.E., Ruiz-Padilla J.P., Botello-Hernandez E. Vaccine Hesitancy against SARS-CoV-2 in Health Personnel of Northeastern Mexico and Its Determinants. J. Occup. Environ. Med. 2021;63:633–637. doi: 10.1097/JOM.0000000000002205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Taylor S., Landry C.A., Paluszek M.M., Groenewoud R., Rachor G.S., Asmundson G.J.G. A Proactive Approach for Managing COVID-19: The Importance of Understanding the Motivational Roots of Vaccination Hesitancy for SARS-CoV2. Front. Psychol. 2020;11:575950. doi: 10.3389/fpsyg.2020.575950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams L., Gallant A.J., Rasmussen S., Brown Nicholls L.A., Cogan N., Deakin K., Young D., Flowers P. Towards Intervention Development to Increase the Uptake of COVID-19 Vaccination among Those at High Risk: Outlining Evidence-based and Theoretically Informed Future Intervention Content. Br. J. Health Psychol. 2020;25:1039–1054. doi: 10.1111/bjhp.12468. [DOI] [PubMed] [Google Scholar]
- 45.Jackson S.E., Paul E., Brown J., Steptoe A., Fancourt D. Negative Vaccine Attitudes and Intentions to Vaccinate Against Covid-19 in Relation to Smoking Status: A Population Survey of UK Adults. Nicotine Tob. Res. 2021:ntab039. doi: 10.1093/ntr/ntab039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Williams L., Flowers P., McLeod J., Young D., Rollins L., The CATALYST Project Team the CATALYST Project Team Social Patterning and Stability of Intention to Accept a COVID-19 Vaccine in Scotland: Will Those Most at Risk Accept a Vaccine? Vaccines. 2021;9:17. doi: 10.3390/vaccines9010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sherman S.M., Smith L.E., Sim J., Amlôt R., Cutts M., Dasch H., Rubin G.J., Sevdalis N. COVID-19 Vaccination Intention in the UK: Results from the COVID-19 Vaccination Acceptability Study (CoVAccS), a Nationally Representative Cross-Sectional Survey. Hum. Vaccines Immunother. 2021;17:1612–1621. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Freeman D., Loe B.S., Chadwick A., Vaccari C., Waite F., Rosebrock L., Jenner L., Petit A., Lewandowsky S., Vanderslott S., et al. COVID-19 Vaccine Hesitancy in the UK: The Oxford Coronavirus Explanations, Attitudes, and Narratives Survey (Oceans) II. Psychol. Med. 2020:1–15. doi: 10.1093/pubmed/fdab028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Batty G.D., Deary I.J., Fawns-Ritchie C., Gale C.R., Altschul D. Pre-Pandemic Cognitive Function and COVID-19 Vaccine Hesitancy: Cohort Study. Brain Behav. Immun. 2021;96:S0889159121001975. doi: 10.1016/j.bbi.2021.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Robertson E., Reeve K.S., Niedzwiedz C.L., Moore J., Blake M., Green M., Katikireddi S.V., Benzeval M.J. Predictors of COVID-19 Vaccine Hesitancy in the UK Household Longitudinal Study. Brain Behav. Immun. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gagneux-Brunon A., Detoc M., Bruel S., Tardy B., Rozaire O., Frappe P., Botelho- Nevers E. Intention to Get Vaccinations against COVID-19 in French Healthcare Workers during the First Pandemic Wave: A Cross-Sectional Survey. J. Hosp. Infect. 2021;108:168–173. doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ward J.K., Alleaume C., Peretti-Watel P., Peretti-Watel P., Seror V., Cortaredona S., Launay O., Raude J., Verger P., Beck F., et al. The French Public’s Attitudes to a Future COVID-19 Vaccine: The Politicization of a Public Health Issue. Soc. Sci. Med. 2020;265:113414. doi: 10.1016/j.socscimed.2020.113414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Detoc M., Bruel S., Frappe P., Tardy B., Botelho-Nevers E., Gagneux-Brunon A. Intention to Participate in a COVID-19 Vaccine Clinical Trial and to Get Vaccinated against COVID-19 in France during the Pandemic. Vaccine. 2020;38:7002–7006. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Montagni I., Ouazzani-Touhami K., Mebarki A., Texier N., Schück S., Tzourio C., The CONFINS Group Acceptance of a Covid-19 Vaccine Is Associated with Ability to Detect Fake News and Health Literacy. J. Public Health. 2021:fdab028. doi: 10.1093/pubmed/fdab028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Barrière J., Gal J., Hoch B., Cassuto O., Leysalle A., Chamorey E., Borchiellini D. Acceptance of SARS-CoV-2 Vaccination among French Patients with Cancer: A Cross—Sectional Survey. Ann. Oncol. 2021;32:673–674. doi: 10.1016/j.annonc.2021.01.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Green M.S., Abdullah R., Vered S., Nitzan D. A Study of Ethnic, Gender and Educational Differences in Attitudes toward COVID-19 Vaccines in Israel—Implications for Vaccination Implementation Policies. Isr. J. Health Policy Res. 2021;10:26. doi: 10.1186/s13584-021-00458-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A., Srouji S., Sela E. Vaccine Hesitancy: The next Challenge in the Fight against COVID-19. Eur. J. Epidemiol. 2020;35:775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zigron A., Dror A.A., Morozov N.G., Shani T., Haj Khalil T., Eisenbach N., Rayan D., Daoud A., Kablan F., Marei H., et al. COVID-19 Vaccine Acceptance Among Dental Professionals Based on Employment Status During the Pandemic. Front. Med. 2021;8:618403. doi: 10.3389/fmed.2021.618403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.La Vecchia C., Negri E., Alicandro G., Scarpino V. Attitudes towards Influenza Vaccine and a Potential COVID-19 Vaccine in Italy and Differences across Occupational Groups, September 2020: Attitudes towards Influenza Vaccine and a Potential COVID-19 Vaccine in Italy. La Med. Del Lav. Work. Environ. Health. 2020;111:445–448. doi: 10.23749/mdl.v111i6.10813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Prati G. Intention to Receive a Vaccine against SARS-CoV-2 in Italy and Its Association with Trust, Worry and Beliefs about the Origin of the Virus. Health Educ. Res. 2020;35:505–511. doi: 10.1093/her/cyaa043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Barello S., Nania T., Dellafiore F., Graffigna G., Caruso R. ‘Vaccine Hesitancy’ among University Students in Italy during the COVID-19 Pandemic. Eur. J. Epidemiol. 2020;35:781–783. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Di Gennaro F., Murri R., Segala F.V., Cerruti L., Abdulle A., Saracino A., Bavaro D.F., Fantoni M. Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses. 2021;13:371. doi: 10.3390/v13030371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Graffigna G., Palamenghi L., Boccia S., Barello S. Relationship between Citizens’ Health Engagement and Intention to Take the COVID-19 Vaccine in Italy: A Mediation Analysis. Vaccines. 2020;8:576. doi: 10.3390/vaccines8040576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gerussi V., Peghin M., Palese A., Bressan V., Visintini E., Bontempo G., Graziano E., De Martino M., Isola M., Tascini C. Vaccine Hesitancy among Italian Patients Recovered from COVID-19 Infection towards Influenza and Sars-Cov-2 Vaccination. Vaccines. 2021;9:172. doi: 10.3390/vaccines9020172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pastorino R., Villani L., Mariani M., Ricciardi W., Graffigna G., Boccia S. Impact of COVID-19 Pandemic on Flu and COVID-19 Vaccination Intentions among University Students. Vaccines. 2021;9:70. doi: 10.3390/vaccines9020070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Priori R., Pellegrino G., Colafrancesco S., Alessandri C., Ceccarelli F., Di Franco M., Riccieri V., Scrivo R., Sili Scavalli A., Spinelli F.R., et al. SARS-CoV-2 Vaccine Hesitancy among Patients with Rheumatic and Musculoskeletal Diseases: A Message for Rheumatologists. Ann. Rheum. Dis. 2021;80:953–954. doi: 10.1136/annrheumdis-2021-220059. [DOI] [PubMed] [Google Scholar]
- 67.Barello S., Palamenghi L., Graffigna G. Looking inside the ‘Black Box’ of Vaccine Hesitancy: Unlocking the Effect of Psychological Attitudes and Beliefs on COVID-19 Vaccine Acceptance and Implications for Public Health Communication. Psychol. Med. 2021:1–2. doi: 10.1017/S003329172100101X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Karlsson L.C., Soveri A., Lewandowsky S., Karlsson L., Karlsson H., Nolvi S., Karukivi M., Lindfelt M., Antfolk J. Fearing the Disease or the Vaccine: The Case of COVID-19. Personal. Individ. Differ. 2021;172:110590. doi: 10.1016/j.paid.2020.110590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Szmyd B., Bartoszek A., Karuga F.F., Staniecka K., Błaszczyk M., Radek M. Medical Students and SARS-CoV-2 Vaccination: Attitude and Behaviors. Vaccines. 2021;9:128. doi: 10.3390/vaccines9020128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Feleszko W., Lewulis P., Czarnecki A., Waszkiewicz P. Flattening the Curve of COVID-19 Vaccine Rejection—An International Overview. Vaccines. 2021;9:44. doi: 10.3390/vaccines9010044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Papagiannis D., Rachiotis G., Malli F., Papathanasiou I.V., Kotsiou O., Fradelos E.C., Giannakopoulos K., Gourgoulianis K.I. Acceptability of COVID-19 Vaccination among Greek Health Professionals. Vaccines. 2021;9:200. doi: 10.3390/vaccines9030200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Serrazina F., Sobral Pinho A., Cabral G., Salavisa M., Correia A.S. Willingness to Be Vaccinated against COVID-19: An Exploratory Online Survey in a Portuguese Cohort of Multiple Sclerosis Patients. Mult. Scler. Relat. Disord. 2021;51:102880. doi: 10.1016/j.msard.2021.102880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Eguia H., Vinciarelli F., Bosque-Prous M., Kristensen T., Saigí-Rubió F. Spain’s Hesitation at the Gates of a COVID-19 Vaccine. Vaccines. 2021;9:170. doi: 10.3390/vaccines9020170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yigit M., Ozkaya-Parlakay A., Senel E. Evaluation of COVID-19 Vaccine Refusal in Parents. Pediatric Infect. Dis. J. 2021;40:e134–e136. doi: 10.1097/INF.0000000000003042. [DOI] [PubMed] [Google Scholar]
- 75.Ditekemena J.D., Nkamba D.M., Mutwadi A., Mavoko H.M., Siewe Fodjo J.N., Luhata C., Obimpeh M., Van Hees S., Nachega J.B., Colebunders R. COVID-19 Vaccine Acceptance in the Democratic Republic of Congo: A Cross-Sectional Survey. Vaccines. 2021;9:153. doi: 10.3390/vaccines9020153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dinga J.N., Sinda L.K., Titanji V.P.K. Assessment of Vaccine Hesitancy to a COVID-19 Vaccine in Cameroonian Adults and Its Global Implication. Vaccines. 2021;9:175. doi: 10.3390/vaccines9020175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kabamba Nzaji M., Kabamba Ngombe L., Ngoie Mwamba G., Banza Ndala D.B., Mbidi Miema J., Luhata Lungoyo C., Lora Mwimba B., Cikomola Mwana Bene A., Mukamba Musenga E. Acceptability of Vaccination Against COVID-19 Among Healthcare Workers in the Democratic Republic of the Congo. POR. 2020;11:103–109. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Saied S.M., Saied E.M., Kabbash I.A., Abdo S.A.E. Vaccine Hesitancy: Beliefs and Barriers Associated with COVID-19 Vaccination among Egyptian Medical Students. J. Med. Virol. 2021;93:4280–4291. doi: 10.1002/jmv.26910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Al-Qerem W.A., Jarab A.S. COVID-19 Vaccination Acceptance and Its Associated Factors among a Middle Eastern Population. Front. Public Health. 2021;9:632914. doi: 10.3389/fpubh.2021.632914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sallam M., Dababseh D., Eid H., Al-Mahzoum K., Al-Haidar A., Taim D., Yaseen A., Ababneh N.A., Bakri F.G., Mahafzah A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines. 2021;9:42. doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Qattan A.M.N., Alshareef N., Alsharqi O., Al Rahahleh N., Chirwa G.C., Al-Hanawi M.K. Acceptability of a COVID-19 Vaccine Among Healthcare Workers in the Kingdom of Saudi Arabia. Front. Med. 2021;8:644300. doi: 10.3389/fmed.2021.644300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Al-Mohaithef M., Padhi B.K. Determinants of COVID-19 Vaccine Acceptance in Saudi Arabia: A Web-Based National Survey. J. Multidiscip. Healthc. 2020;13:1657–1663. doi: 10.2147/JMDH.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Alqudeimat Y., Alenezi D., AlHajri B., Alfouzan H., Almokhaizeem Z., Altamimi S., Almansouri W., Alzalzalah S., Ziyab A. Acceptance of a COVID-19 Vaccine and Its Related Determinants among the General Adult Population in Kuwait. Med. Princ. Pract. 2021;30:262–271. doi: 10.1159/000514636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Alabdulla M., Reagu S.M., Al-Khal A., Elzain M., Jones R.M. COVID-19 Vaccine Hesitancy and Attitudes in Qatar: A National Cross-sectional Survey of a Migrant-majority Population. Influenza Other Respi. Viruses. 2021;15:361–370. doi: 10.1111/irv.12847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dodd R.H., Cvejic E., Bonner C., Pickles K., McCaffery K.J., Ayre J., Batcup C., Copp T., Cornell S., Dakin T., et al. Willingness to Vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021;21:318–319. doi: 10.1016/S1473-3099(20)30559-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Edwards B., Biddle N., Gray M., Sollis K. COVID-19 Vaccine Hesitancy and Resistance: Correlates in a Nationally Representative Longitudinal Survey of the Australian Population. PLoS ONE. 2021;16:e0248892. doi: 10.1371/journal.pone.0248892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Faasse K., Newby J. Public Perceptions of COVID-19 in Australia: Perceived Risk, Knowledge, Health-Protective Behaviors, and Vaccine Intentions. Front. Psychol. 2020;11:551004. doi: 10.3389/fpsyg.2020.551004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rhodes A., Hoq M., Measey M.-A., Danchin M. Intention to Vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021;21:e110. doi: 10.1016/S1473-3099(20)30724-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wang K., Wong E.L.Y., Ho K.F., Cheung A.W.L., Chan E.Y.Y., Yeoh E.K., Wong S.Y.S. Intention of Nurses to Accept Coronavirus Disease 2019 Vaccination and Change of Intention to Accept Seasonal Influenza Vaccination during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Survey. Vaccine. 2020;38:7049–7056. doi: 10.1016/j.vaccine.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yu Y., Lau J.T.F., Lau M.M.C., Wong M.C.S., Chan P.K.S. Understanding the Prevalence and Associated Factors of Behavioral Intention of COVID-19 Vaccination Under Specific Scenarios Combining Effectiveness, Safety, and Cost in the Hong Kong Chinese General Population. Int. J. Health Policy Manag. 2021:1–12. doi: 10.34172/ijhpm.2021.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gan L., Chen Y., Hu P., Wu D., Zhu Y., Tan J., Li Y., Zhang D. Willingness to Receive SARS-CoV-2 Vaccination and Associated Factors among Chinese Adults: A Cross Sectional Survey. Int. J. Environ. Res. Public Health. 2021;18:1993. doi: 10.3390/ijerph18041993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lin Y., Hu Z., Zhao Q., Alias H., Danaee M., Wong L.P. Understanding COVID-19 Vaccine Demand and Hesitancy: A Nationwide Online Survey in China. PLoS Negl. Trop. Dis. 2020;14:e000896. doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang J., Jing R., Lai X., Zhang H., Lyu Y., Knoll M.D., Fang H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines. 2020;8:482. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang J., Lu X., Lai X., Lyu Y., Zhang H., Fenghuang Y., Jing R., Li L., Yu W., Fang H. The Changing Acceptance of COVID-19 Vaccination in Different Epidemic Phases in China: A Longitudinal Study. Vaccines. 2021;9:191. doi: 10.3390/vaccines9030191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhang K.C., Fang Y., Cao H., Chen H., Hu T., Chen Y., Zhou X., Wang Z. Behavioral Intention to Receive a COVID-19 Vaccination Among Chinese Factory Workers: Cross- Sectional Online Survey. J. Med. Internet Res. 2021;23:e24673. doi: 10.2196/24673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mo P.K., Luo S., Wang S., Zhao J., Zhang G., Li L., Li L., Xie L., Lau J.T.F. Intention to Receive the COVID-19 Vaccination in China: Application of the Diffusion of Innovations Theory and the Moderating Role of Openness to Experience. Vaccines. 2021;9:129. doi: 10.3390/vaccines9020129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang K.C., Fang Y., Cao H., Chen H., Hu T., Chen Y.Q., Zhou X., Wang Z. Parental Acceptability of COVID-19 Vaccination for Children Under the Age of 18 Years: Cross- Sectional Online Survey. JMIR Pediatr. Parent. 2020;3:e24827. doi: 10.2196/24827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yoda T., Katsuyama H. Willingness to Receive COVID-19 Vaccination in Japan. Vaccines. 2021;9:48. doi: 10.3390/vaccines9010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wong L.P., Alias H., Wong P.-F., Lee H.Y., AbuBakar S. The Use of the Health Belief Model to Assess Predictors of Intent to Receive the COVID-19 Vaccine and Willingness to Pay. Hum. Vaccines Immunother. 2020;16:2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Parajuli J., Mishra P., Sharma S., Bohora K.B., Rathour P.S., Joshi J., Kamar S.B., Pandey H., Chaudhary A. Knowledge and Attitude about COVID 19 among Health Care Workers Working in Seti Provincial Hospital. J. Nepal Health Res. Counc. 2020;18:466–471. doi: 10.33314/jnhrc.v18i3.2816. [DOI] [PubMed] [Google Scholar]
- 101.Harapan H., Wagner A.L., Yufika A., Winardi W., Anwar S., Gan A.K., Setiawan A.M., Rajamoorthy Y., Sofyan H., Mudatsir M. Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Front. Public Health. 2020;8:381. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Chew N.W.S., Cheong C., Kong G., Phua K., Ngiam J.N., Tan B.Y.Q., Wang B., Hao F., Tan W., Han X., et al. An Asia-Pacific Study on Healthcare Workers’ Perceptions of, and Willingness to Receive, the COVID-19 Vaccination. Int. J. Infect. Dis. 2021;106:52–60. doi: 10.1016/j.ijid.2021.03.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., Kimball S., El-Mohandes A. Author Correction: A Global Survey of Potential Acceptance of a COVID-19 Vaccine. Nat. Med. 2021;27:354. doi: 10.1038/s41591-020-01226-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Skjefte M., Ngirbabul M., Akeju O., Escudero D., Hernandez-Diaz S., Wyszynski D.F., Wu J.W. COVID-19 Vaccine Acceptance among Pregnant Women and Mothers of Young Children: Results of a Survey in 16 Countries. Eur. J. Epidemiol. 2021;36:197–211. doi: 10.1007/s10654-021-00728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Goldman R.D., Yan T.D., Seiler M., Parra Cotanda C., Brown J.C., Klein E.J., Hoeffe J., Gelernter R., Hall J.E., Davis A.L., et al. Caregiver Willingness to Vaccinate Their Children against COVID-19: Cross Sectional Survey. Vaccine. 2020;38:7668–7673. doi: 10.1016/j.vaccine.2020.09.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel J., Schreyögg J., Stargardt T. Once We Have It, Will We Use It? A European Survey on Willingness to Be Vaccinated against COVID-19. Eur. J. Health Econ. 2020;21:977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Verger P., Scronias D., Dauby N., Adedzi K.A., Gobert C., Bergeat M., Gagneur A., Dubé E. Attitudes of Healthcare Workers towards COVID-19 Vaccination: A Survey in France and French-Speaking Parts of Belgium and Canada, 2020. Eurosurveillance. 2021;26:2002047. doi: 10.2807/1560-7917.ES.2021.26.3.2002047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Murphy J., Vallières F., Bentall R.P., Shevlin M., McBride O., Hartman T.K., McKay R., Bennett K., Mason L., Gibson-Miller J., et al. Psychological Characteristics Associated with COVID-19 Vaccine Hesitancy and Resistance in Ireland and the United Kingdom. Nat. Commun. 2021;12:29. doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Plans-Rubió P. Evaluation of the Establishment of Herd Immunity in the Population by Means of Serological Surveys and Vaccination Coverage. Hum. Vaccines Immunother. 2012;8:184–188. doi: 10.4161/hv.18444. [DOI] [PubMed] [Google Scholar]
- 110.Razai M.S., Chaudhry U.A.R., Doerholt K., Bauld L., Majeed A. Covid-19 Vaccination Hesitancy. BMJ. 2021;373:n1138. doi: 10.1136/bmj.n1138. [DOI] [PubMed] [Google Scholar]
- 111.Larson H.J., Clarke R.M., Jarrett C., Eckersberger E., Levine Z., Schulz W.S., Paterson P. Measuring Trust in Vaccination: A Systematic Review. Hum. Vaccin Immunother. 2018;14:1599–1609. doi: 10.1080/21645515.2018.1459252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Peckham H., de Gruijter N.M., Raine C., Radziszewska A., Ciurtin C., Wedderburn L.R., Rosser E.C., Webb K., Deakin C.T. Male Sex Identified by Global COVID-19 Meta-Analysis as a Risk Factor for Death and ITU Admission. Nat. Commun. 2020;11:6317. doi: 10.1038/s41467-020-19741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Paris C., Bénézit F., Geslin M., Polard E., Baldeyrou M., Turmel V., Tadié É., Garlantezec R., Tattevin P. COVID-19 Vaccine Hesitancy among Healthcare Workers. Infect. Dis. Now. 2021;51:484–487. doi: 10.1016/j.idnow.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Talbot T.R., Bradley S.E., Cosgrove S.E., Ruef C., Siegel J.D., Weber D.J. Influenza Vaccination of Healthcare Workers and Vaccine Allocation for Healthcare Workers during Vaccine Shortages. Infect. Control. Hosp. Epidemiol. 2005;26:882–890. doi: 10.1086/502512. [DOI] [PubMed] [Google Scholar]
- 115.Jordan R.E., Adab P., Cheng K.K. Covid-19: Risk Factors for Severe Disease and Death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 116.McGurnaghan S.J., Weir A., Bishop J., Kennedy S., Blackbourn L.A.K., McAllister D.A., Hutchinson S., Caparrotta T.M., Mellor J., Jeyam A., et al. Risks of and Risk Factors for COVID-19 Disease in People with Diabetes: A Cohort Study of the Total Population of Scotland. Lancet Diabetes Endocrinol. 2021;9:82–93. doi: 10.1016/S2213-8587(20)30405-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gerayeli F.V., Milne S., Cheung C., Li X., Yang C.W.T., Tam A., Choi L.H., Bae A., Sin D.D. COPD and the Risk of Poor Outcomes in COVID-19: A Systematic Review and Meta-Analysis. EClinicalMedicine. 2021;33:100789. doi: 10.1016/j.eclinm.2021.100789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Louapre C., Collongues N., Stankoff B., Giannesini C., Papeix C., Bensa C., Deschamps R., Créange A., Wahab A., Pelletier J., et al. Clinical Characteristics and Outcomes in Patients with Coronavirus Disease 2019 and Multiple Sclerosis. JAMA Neurol. 2020;77:1079. doi: 10.1001/jamaneurol.2020.2581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bello A.K., Peters J., Rigby J., Rahman A.A., El Nahas M. Socioeconomic Status and Chronic Kidney Disease at Presentation to a Renal Service in the United Kingdom. Clin. J. Am. Soc. Nephrol. 2008;3:1316–1323. doi: 10.2215/CJN.00680208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Patrick M.E., Wightman P., Schoeni R.F., Schulenberg J.E. Socioeconomic Status and Substance Use among Young Adults: A Comparison across Constructs and Drugs. J. Stud. Alcohol Drugs. 2012;73:772–782. doi: 10.15288/jsad.2012.73.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Economically Disadvantaged, HIV by Group, HIV/AIDS, CDC. [(accessed on 20 July 2021)]; Available online: https://www.cdc.gov/hiv/group/poverty.html.
- 122.Gori D., Reno C., Remondini D., Durazzi F., Fantini M.P. Are We Ready for the Arrival of the New COVID-19 Vaccinations? Great Promises and Unknown Challenges Still to Come. Vaccines. 2021;9:173. doi: 10.3390/vaccines9020173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Gori D., Montalti M., Guaraldi F. Mass Immunization and Vaccine Hesitancy in Children and Their Families: A Long and Winding Road Ahead to Address without a Second Thought. Vaccines. 2021;9:752. doi: 10.3390/vaccines9070752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Piltch-Loeb R., Savoia E., Goldberg B., Hughes B., Verhey T., Kayyem J., Miller-Idriss C., Testa M. Examining the Effect of Information Channel on COVID-19 Vaccine Acceptance. PLoS ONE. 2021;16:e0251095. doi: 10.1371/journal.pone.0251095. [DOI] [PMC free article] [PubMed] [Google Scholar]