“The Agony and Ecstasy of COVID-19” [1]
The Agony of the COVID-19 pandemic arises from the morbidity and mortality from SARS-CoV-2, including the death of more than four million people worldwide of which about 610,000 were in the United States. For many millions the ecstasy comes from the unprecedented rapid development of multiple vaccines [2,3] with some proving 90% effective in limiting morbidity and mortality [4]. Through this Virtual Special Issue of Sleep Medicine international authors summarize information relevant to sleep researchers and clinicians in hopes of advancing the understanding of the biology and pathology of COVID-19 and the response to its impact and threat.
COVID-19 is a highly contagious, airborne viral disease [5], which can spread by human-to-human transmission from asymptomatic to severe cases [6]. Bill Gates considers Covid-19 as a “Once in-a-Century Pandemic” [7]. This is reminiscent of the great 19th century influenza pandemic [8] with a mortality of 2% of the global population (an estimated >50 million people died), thus placing the current Covid-19 pandemic with about 1% [9] mortality between the 1918–1919 pandemic [8] and the influenza pandemic of 1957 [10] that had a mortality rate of 0.6%.
The ongoing COVID-19 pandemic is proving more dangerous than the epidemics of severe acute respiratory syndrome (SARS-CoV-1) of 2002–2003 [11], the Middle East Repertory Syndrome (MERS) of 2012 [12] or the 2014 Ebola Virus epidemic [13]. An efficient vaccine against COVID-19 [[2], [3], [4]] and an effective specific antiviral therapy are expected to address the SARS-CoV-2 crisis, presuming viral variants do not forestall current progress in disease management. In the meantime, it is essential for all to follow the guidelines recommended by the World Health Organization (WHO) [14] and the Center for Disease Control and Prevention [15], such as properly fitted facial mask, social distancing of a preferred six feet, frequent hand washing, and forgoing unnecessary travel, sizeable indoor gatherings or packed outdoor events [16]. Unfortunately, the conflict between public safety and individual rights has led to political criticisms of these scientifically proven health measures and caused vaccine hesitancy [17]. Without cooperation and collaborations from each of us to contain and defeat this invisible viral enemy, we risk further disruption and potential decay of civilized society.
1. Abbreviated sequence of events of the ongoing pandemic
As highlighted by Li et al. and Peng et al. in this issue, the first case of pneumonia of uncertain etiology occurred sometime in late 2019 in the city of Wuhan, located in the Hubei Province of China. COVID-19 then spread rapidly to Thailand on January 13, 2020 and later to other parts of Southeast Asia. Countries of Europe and the American continents soon followed [18]. The Chinese CDC first reported about infectivity on January 15, 2020. The International Committee on Taxonomy for Viruses (ICTV) named SARS- CoV-2. On January 15, 2020 the WHO declared the spread of viral pneumonia to be of serious international concern. On February 11, 2020 the WHO named the disease caused by SARS-CoV-2 as COVID-19. On March 11, 2020 the WHO labeled the outbreak a pandemic [18]. On March 16, 2020 the confirmed cases outside China surpassed the number of cases reported in China for the first time. Worldwide there are over 190 million reported cases with over 4 Million deaths and of this writing a resurgence of global cases from multiple variants.
The origin of the virus is still under investigation but was thought to have originated from bats, then transmitted to an unknown animal in Wuhan, and then transmitted to humans, followed by human-to-human spread [18]. It is notable that the great influenza pandemic (incorrectly labeled “Spanish Flu”) of the 19th century was thought to have originated in Romania around 1915–1918 then spreading worldwide. There are anecdotal reports that this viral disease may also have originated elsewhere and then spread by World War I soldiers [8,18].
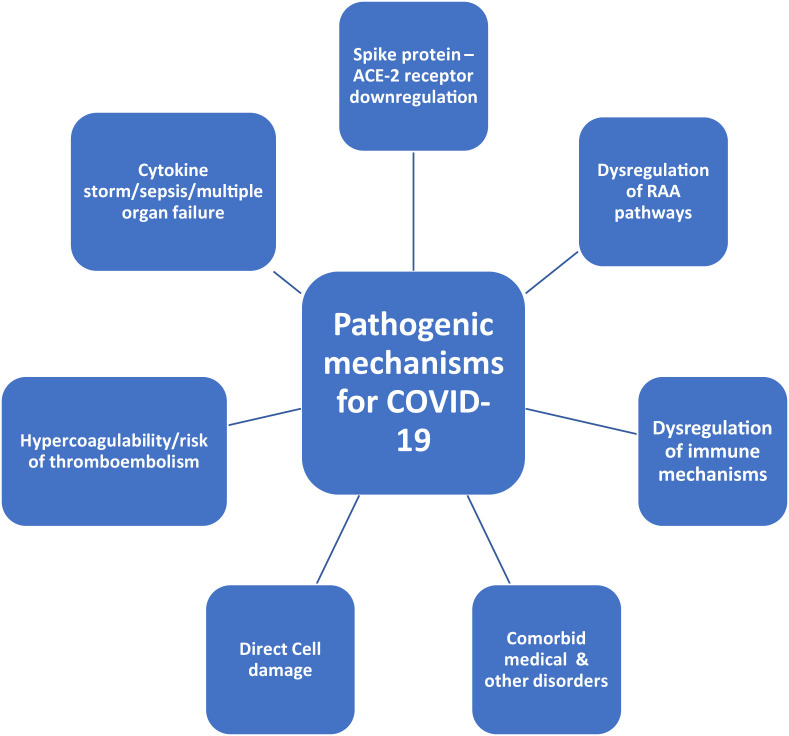
COVID-19 is an emerging disease with many unknown aspects, including the specifics of its invasion of the body and the brain. As highlighted by the articles in this issue, further study is needed on its pathophysiological mechanisms [Fig. 1 ], the long-term natural history, factors of infectivity, the long-term immunity following an infection or vaccination as well as the question of recurrence following an initial infection, and the specificity of the positive reverse transcriptase –polymerase chain reaction (RT-PCR) test, particularly for viral variants [19]. The clinical manifestations in most of the cases are mild but the moderate-severe cases carried an early high mortality, particularly significant for the elderly with comorbidities [[18], [19], [20], [21]]. We know that the virus gains access through the epithelium and vascular endothelium of organs that are rich in angiotensin converting enzyme receptor 2 (ACE-R2), creating controversy about the use of ACE inhibitors and angiotensin receptor blockers [18,[22], [23], [24]]. Another clinical question about the interrelationship between obstructive sleep apnea (OSA) and COVID-19 is discussed in the issue articles by Bhat and Chokroverty, Peng et al. and Labarca as has occurred by authors elsewhere [18,[25], [26], [27]]. In this issue Bruni et al. also describe the disturbed sleep in Italian children and adolescents, even as children seemed to be relatively immune to early variants of the coronavirus. More understanding is needed of the very rare, yet potentially fatal, pediatric multisystem inflammatory syndrome that resembles Kawasaki syndrome [28,29].
Fig. 1.
Pathogenic mechanisms for COVID-19.
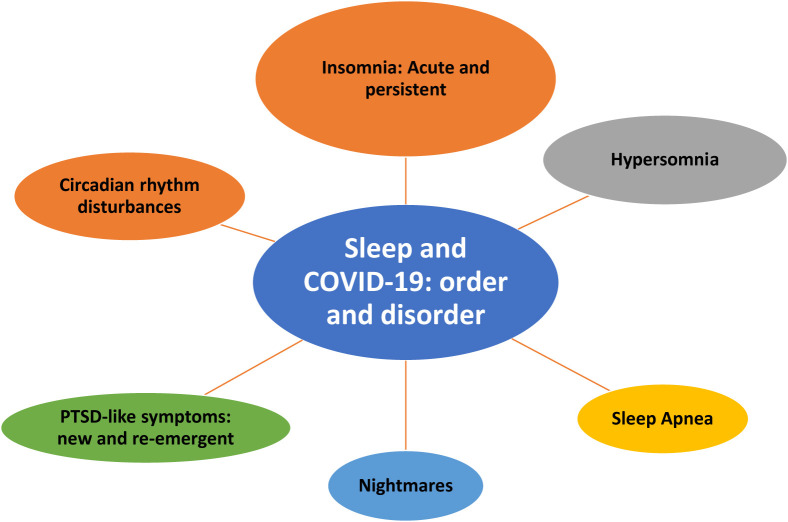
The clinical manifestations of COVID-19 are protean, affecting predominantly the respiratory and gastrointestinal tracts but may involve multiple organs additionally affecting cardiovascular, renal, endocrine and dermatologic systems [30,31] as well as the central, peripheral and autonomic nervous systems as described by Bhat and Chokroverty and Khatoon, Prasad and Kumar in this issue. Barthorpe and Rogers also review neuropsychiatric manifestations from coronavirus infections between 2003 and 2020. Covered by many authors in this issue, sleep dysfunction is prominent in COVID-19 [see Fig. 2 ] and related psychobiological and lifestyle changes from the pandemic that include circadian disruption as discussed by Salehinejad and colleagues. The rates of insomnia symptoms have increased by 2-3-fold with reports of acute insomnia during the pandemic as high as 45% [32]. Frontline health care workers have experienced particularly high rates of sleep, depressive and anxiety symptoms [33] as herein discussed by Poppa et al. There is concern about long-term psychological consequences from COVID-19 and pandemic restrictions, potentially increasing rates of suicide and substance abuse [34]. Although studies are limited, Becker discusses management of sleep dysfunction during COVID-19.
Fig. 2.
Sleep and COVID-19: order and disorder.
In summary, this special issue on COVID-19 includes experts in the field who have investigated this novel coronavirus and its multisystem pathophysiology and diagnosis, including management with special emphasis on sleep and psychological dysfunction. The reader will note overlap among several chapters dealing with sleep, psychological and neurological aspects of COVID-19. The guest editors believe that some overlap is acceptable for this very important topic since different readers will focus on the body systems of interest. It is our hope that the issue proves useful to all clinicians dealing with COVID-19 patients whether sleep specialist, internist, family physician, pediatrician, pulmonologist, neurologist, or psychiatrist. Additionally, paramedical personal who are caring for patients may benefit. In addition to the papers by invited authors and introduction to the topic by the guest editors, we have included in this special issue many original sleep-related articles dealing with COVID-19 across the globe. It is our hope that this issue can be considered a comprehensive review of a cataclysmic pandemic with the hope to see it only once in a lifetime.
Footnotes
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2021.08.019.
Conflict of interest
The following is the supplementary data to this article:
References
- 1.Anonymous.
- 2.Creech C.B., Walker S.C., Samuels R.J. SARS-CoV-2 vaccines. J Am Med Assoc. 2021;325:1318–1320. doi: 10.1001/jama.2021.3199. [DOI] [PubMed] [Google Scholar]
- 3.Coronavirus disease 2019(COVID-19): prevention and treatment. Centers for disease control and prevention; Atlanta: 2020. https://www.cdc.gov/coronavirus/2019-ccing/about/prevention-treatment.html [Google Scholar]
- 4.Thompson M.G., Burgess J.L., Naleway A.L., et al. Interim estimates of vaccine effectiveness of BNT162b2 and mRNA-1273 COVID-19 vaccines in preventing SARS-CoV-2 infection among health care personnel, first responders, and other essential and frontline workers - eight U.S. Locations, december 2020-march 2021. MMWR Morb Mortal Wkly Rep. 2021 Apr 2;70(13):495–500. doi: 10.15585/mmwr.mm7013e3. PMID: 33793460; PMCID: PMC8022879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of COVID-19 : studies. N Engl J Med. 2020;382:1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 6.Gandhi M., Yokoe D.S., Havlir D.S. Asymptomatic transmission, the Achilles' heel of current strategies to control COVID-19. N Engl J Med. 2020;382:2158–2160. doi: 10.1056/NEJMe2009758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gates B. Responding to COVID-19——a once-in-a-century pandemic ? N. Engl J Med. 2020;382:1677–1683. doi: 10.1056/NEJMp2003762. [DOI] [PubMed] [Google Scholar]
- 8.Morens D.M., Taubenberger J.K. Influenza cataclysm, 1918. N Engl J Med. 2018 Dec 13;379(24):2285–2287. doi: 10.1056/NEJMp1814447.PMID30575465. PMCID: PMC6558650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartley D.M., Perencevich E.N. Public health interventions for COVID-19: emerging evidence and implications for an evolving public health crisis. J Am Med Assoc. 2020 May 19;323(19):1908–1909. doi: 10.1001/jama.2020.5910.PMID32275299. [DOI] [PubMed] [Google Scholar]
- 10.Simonsen L., Clarke M.J., Schonberger L.B., et al. Pandemic versus epidemic influenza mortality: a pattern of changing age distribution. J Infect Dis. 1998;178:53–60. doi: 10.1086/515616. [DOI] [PubMed] [Google Scholar]
- 11.Tratner I. Le virus: SARS CoV -1. The virus. Med Sci (Paris ) 2003;19:885–891. doi: 10.1051/medsci/20031989885. [DOI] [PubMed] [Google Scholar]
- 12.Mackay I.M., Arden K.E. Middle East Respiratory syndrome : an emerging coronavirus infection tracked by the crowd. Virus Res. 2015;202:60–88. doi: 10.1016/j.virusres.2015.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zawilinska B., Kosz-Vnenchak M. General introduction into the Ebola virus biology and disease. Folia Med Cracov. 2014;54:57–65. [PubMed] [Google Scholar]
- 14.World Health Organization (Who).www.who.int.
- 15.https://www.cdc.gov/media/releases/2020/s1005-how-spread-covd.html. Updated October 5, 2020.
- 16.Lerner A.M., Folkers G.K., Fauci A.S. Preventing the spread of SARS-CoV-2 with masks and other "Low-tech" interventions. J Am Med Assoc. 2020 Nov 17;324(19):1935–1936. doi: 10.1001/jama.2020.21946.PMID33104157. [DOI] [PubMed] [Google Scholar]
- 17.Rosenbaum L. Escaping catch-22 - overcoming Covid vaccine hesitancy. N Engl J Med. 2021 Apr 8;384(14):1367–1371. doi: 10.1056/NEJMms2101220. Epub 2021 Feb 12. PMID: 33577150. [DOI] [PubMed] [Google Scholar]
- 18.Chokroverty S. The many faces and fangs of COVID-19: an editorial by Sudhansu Chokroverty. Sleep Med. 2020 Aug;vol. 72:164–166. doi: 10.1016/j.sleep.2020.06.006. Epub 2020 Jun 5. Erratum in: sleep med. 2021 Feb;78:203. PMID: 32540212; PMCID: PMC7273139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Omer S.B., Malani P., Del Rio C. The COVID-19 pandemic in the US: a clinical update. J Am Med Assoc. 2020 May 12;323(18):1767–1768. doi: 10.1001/jama.2020.5788.PMID32250388. [DOI] [PubMed] [Google Scholar]
- 20.Chen N., Zhou M., Dong X., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020 Feb 15;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. Epub 2020 Jan 30. PMID: 32007143; PMCID: PMC7135076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guan W.J., Ni Z.Y., Hu Y., et al. China medical treatment expert group for covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Apr 30;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. Epub 2020 Feb 28. PMID: 32109013; PMCID: PMC7092819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patel A.B., Verma A. COVID-19 and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: what is the evidence? J Am Med Assoc. 2020 May 12;323(18):1769–1770. doi: 10.1001/jama.2020.4812.PMID32208485. [DOI] [PubMed] [Google Scholar]
- 23.Mancia G., Rea F., Ludergnani M., et al. Renin-angiotensin-aldosterone system blockers and the risk of covid-19. N Engl J Med. 2020 Jun 18;382(25):2431–2440. doi: 10.1056/NEJMoa2006923. Epub 2020 May 1. PMID: 32356627; PMCID: PMC7206933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoffmann M., Kleine-Weber H., Schroeder S., et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020 Apr 16;181(2):271–280. doi: 10.1016/j.cell.2020.02.052. Epub 2020 Mar 5. PMID: 32142651; PMCID: PMC7102627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller M.A., Cappuccio F.P. A systematic review of COVID-19 and obstructive sleep apnoea. Sleep Med Rev. 2021 Feb;55:101382. doi: 10.1016/j.smrv.2020.101382. Epub 2020 Sep 8. PMID: 32980614; PMCID: PMC7833740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maas M.B., Kim M., Malkani R.G., et al. Obstructive sleep apnea and risk of COVID-19 infection, hospitalization and respiratory failure. Sleep Breath. 2021 Jun;25(2):1155–1157. doi: 10.1007/s11325-020-02203-0. Epub 2020 Sep 29. PMID: 32989673; PMCID: PMC7521948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strausz S., Kiiskinen T., Broberg M., et al. Sleep apnoea is a risk factor for severe COVID-19. BMJ Open Respir Res. 2021 Jan;8(1) doi: 10.1136/bmjresp-2020-000845. PMID: 33436406; PMCID: PMC7804843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levin M. Childhood multisystem inflammatory syndrome - a new challenge in the pandemic. N Engl J Med. 2020 Jul 23;383(4):393–395. doi: 10.1056/NEJMe2023158. Epub 2020 Jun 29. PMID: 32598829; PMCID: PMC7346677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feldstein L.R., Rose E.B., Horwitz S.M., et al. Overcoming COVID-19 investigators; CDC COVID-19 response team. Multisystem inflammatory syndrome in U.S. Children and adolescents. N Engl J Med. 2020 Jul 23;383(4):334–346. doi: 10.1056/NEJMoa2021680. Epub 2020 Jun 29. PMID: 32598831; PMCID: PMC7346765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gupta A., Madhavan M.V., Sehgal K., et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020 Jul;26(7):1017–1032. doi: 10.1038/s41591-020-0968-3. Epub 2020 Jul 10. PMID: 32651579. [DOI] [PubMed] [Google Scholar]
- 31.Wiersinga W.J., Rhodes A., Cheng A.C., et al. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. J Am Med Assoc. 2020 Aug 25;324(8):782–793. doi: 10.1001/jama.2020.12839.PMID32648899. [DOI] [PubMed] [Google Scholar]
- 32.Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatr Res. 2021 Jan;295:113599. doi: 10.1016/j.psychres.2020.113599. Epub 2020 Nov 26. PMID: 33285346; PMCID: PMC7689353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.da Silva F.C.T., Neto M.L.R. Psychological effects caused by the COVID-19 pandemic in health professionals: a systematic review with meta-analysis. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021 Jan 10;104:110062. doi: 10.1016/j.pnpbp.2020.110062. Epub 2020 Aug 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sher L. (2020) The impact of the COVID-19 pandemic on suicide rates. QJM. 2020 Oct 1;113(10):707–712. doi: 10.1093/qjmed/hcaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.