Abstract
Objective: China has the highest stroke incidence in the world, with a large percentage of post-stroke depression (PSD). Abdominal acupuncture is used frequently to treat PSD. This research systematically evaluated the clinical efficacy of this treatment for PSD.
Methods: A literature search retrieved randomized controlled trials in English and Chinese on abdominal acupuncture in conjunction with other therapies (experimental groups), compared to conventional therapies (control groups) for treating PSD from January 2000 to November 2020. Literature quality was evaluated with the Cochrane Library bias-risk assessment tool. RevMan5.3 software was used for the meta-analysis.
Results: A total of 10 RCTs involving 708 patients were evaluated. Hamilton Depression Scale scores of the experimental groups were significantly lower than in the control groups (mean difference [MD] = −2.34; 95% confidence interval [CI]: −2.89, −1.78; P < 0.00001). Total effective rates of the experimental groups were significantly higher than in the control groups (odds ratio = 3.90; 95% CI: 2.29, 6.62, P < 0.00001). Barthel index scores in the experimental groups were significantly higher than in the control groups (MD = −11.39; 95% CI: 9.07, 13.72; P < 0.00001). There were no significant differences in National Institutes of Health Stroke Scale (NIHSS) scores between the 2 groups (MD = −0.03; 95% CI: −0.68, 0.62; P = 0.93).
Conclusions: Abdominal acupuncture for treating PSD is generally effective. However, the degree of neurologic improvement needs further investigation.
Keywords: abdominal acupuncture, Traditional Chinese Medicine, post-stroke depression, meta-analysis
Introduction
According to the latest data published by Lancet Neurology, stroke ranked as the predominant cause of death in China. That country had the highest incidence of stroke in the world, with a lifetime risk rate of 39.3% among the general Chinese population.1 Post-stroke depression (PSD) is a depressive disorder secondary to stroke. The clinical manifestations include apathy, sleep disturbances, slow responses, and memory losses. The incidence of PSD occurs in about one-third of stroke survivors.2 It inflicts a considerable amount of physical and psychologic pain in these patients and imposes a serious burden to their families and to society. People who have serious depression might consequently commit suicide. At present, conventional medical treatments for PSD include antidepressant medications and psychotherapy. Unfortunately, pharmaceutical agents have certain side-effects. The cost of psychotherapy is relatively high.
Abdominal acupuncture is a newly developed treatment modality based on the Traditional Chinese Medicine (TCM) theory, which has the advantages of being safe, relatively painless, efficient, and widely applicable.3 Abdominal acupuncture is guided by the belief that the abdominal innate meridian system is where the clinician identifies reaction points corresponding with the body parts around Shenque points. Slight acupuncture stimulation is performed to heal chronic conditions. In recent years, acupuncture has been used increasingly in clinical practice. In this study, the clinical efficacy of abdominal acupuncture therapy for treating PSD in randomized controlled trials (RCTs) was evaluated in meta-analysis to test the following hypothesis: For patients with PSD, abdominal acupuncture has higher efficacy for treating depressive symptoms, compared with conventional regimens.
Methods
Inclusion and Exclusion Criteria
The type of research included in this study was RCTs. With respect to research subjects, there were no restrictions related to age, gender, and sources of cases. For intervention measures, the experimental groups used mono abdominal acupuncture therapy or combination therapy. The latter could include a combination of antidepressants, other acupuncture methods, and rehabilitation. The control groups used conventional interventions for stroke, which included anticoagulation, lipid-lowering, and plaque stabilization medications; and treatments for dehydration, elevated intracranial pressure, blood pressure and blood sugar problems as needed; there could be blank controls as well. The control groups could use any combination of treatment methods, such as antidepressants, or other routes of acupuncture and/or rehabilitation.
Unpublished or duplicate studies, conference presentations, and systematic reviews were excluded. Also excluded were studies without Hamilton Depression Scale (HAMD) scores as the observation indicators, or studies with no available full-texts despite exhaustive retrieval efforts.
Retrieval and Selection of Studies
An online search was conducted in PubMed, the Cochrane Library, Foreign Medical Literature Retrieval Service (FMRS), Chinese Biomedical Literature Database (CBM), ClinicalKey, China National Knowledge Infrastructure (CNKI), and Wanfang databases for RCTs in the English and Chinese languages on the efficacy of abdominal acupuncture alone or in combination with other therapies, compared with conventional therapies for treating PSD. The retrieval time frame was from January 2000 to November 2020. Key words used for search were: depression, stroke, abdominal acupuncture, and post-stroke depression.
As a measure of quality control, 2 graduate students completed the literature search independently. After reading the titles and abstracts and excluding studies obviously not meeting the inclusion criteria, full texts of the articles were downloaded to confirm if they should be included in the review. When there were disagreements or discrepancies, a professor of the Master's program would be consulted.
Efficacy indicators included:
-
(1)
HAMD scores, with lower scores indicating less-severe depressive symptoms
-
(2)
Effective rate as measured by reduction of depressive symptoms
-
(3)
Neurologic rehabilitation indicators as follows:
Barthel Index, the higher the scores, the better the ability to perform activities of daily living (ADLs)
National Institutes of Health Stroke Scale (NIHSS) score, the lower the scores, the better the neurologic function.
Quality Evaluation and Data Management
In the Cochrane Handbook for Systematic Reviews of Interventions,4 quality evaluation consists of random-sequence generation, allocation concealment, blinding of participants and researchers, blinding of outcome assessment, assessments for incomplete outcome data, selective reporting, and other biases. According to the bias-risk evaluation standard set forth by the Handbook, each item would be examined to see if it had any of the three types of bias, that is (1) “low risk,” (2) “risk unknown,” or (3) “high risk.”
Data extraction included author, year of publication, intervention measures of the experimental groups and control groups, numbers of cases from both groups, effective rates, HAMD scores, Barthel indexes, NIHSS scores, and risk-of-bias evaluations.
Data Analysis and Statistical Methods
Review Manager 5.3 for statistical analysis was used. Odds ratio (OR) was used for analysis of binary data. Continuous data were analyzed by mean difference (MD). A χ2 test was used to determine heterogeneity between studies. When the extent of heterogeneity was low or when it was not present (P > 0.05 and I2 < 50%), a fixed-effects model was used to calculate the combined effect value. When the heterogeneity between the studies was P < 0.05 or P > 50%, a random-effects model was used.5 If heterogeneity was high, a subgroup analysis or sensitivity analysis was performed. A P-value of <0.05 was considered statistically significant.
Results
Search Results
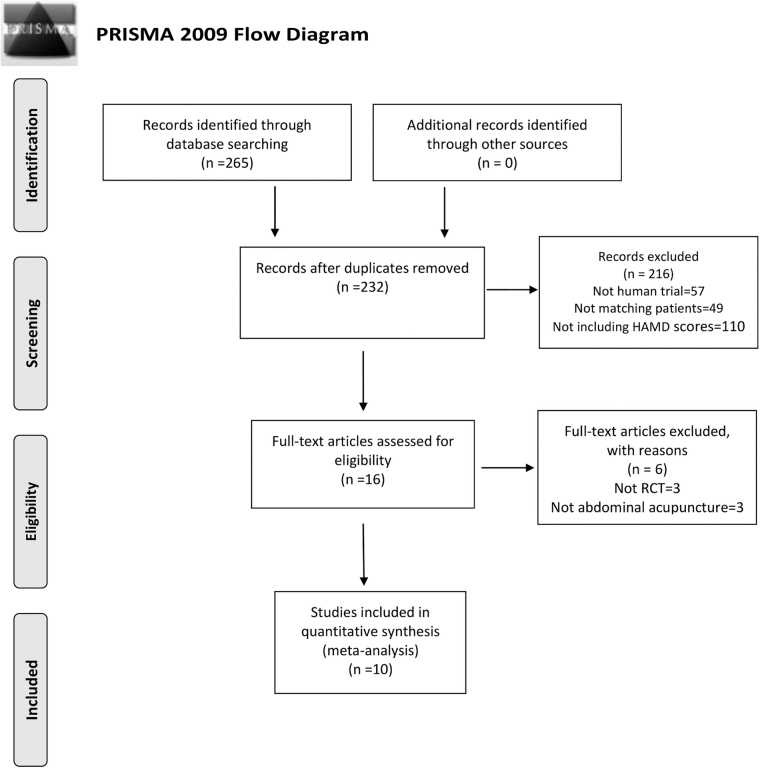
A total of 265 studies was retrieved. After screening the titles and abstracts, 16 records were initially taken into account. After reading the full texts, a total of 10 RCTs were selected strictly in accordance with the inclusion and exclusion criteria (Fig. 1).
FIG. 1.
PRISMA [preferred reporting items for systematic reviews and meta-analyses] flow chart. HAMD, Hamilton Depression Scale.
The Records
A total of 708 subjects (N = 708) in the 10 clinical trials were from hospital wards or outpatient settings, including 353 (n = 353) in the experimental groups and 355 (n = 355) in the control groups. Among them, 1 study did not describe the diagnostic criteria for stroke and depression.6 The rest of the studies all had descriptions that met the TCM or mainstream diagnostic criteria for the disease condition. See Table 1.6–15 All, but 3 trials failed to report adverse effects during treatment.6,7,15 The adverse effects, which could occur in either the experimental groups or the control groups, were believed to be either unremarkable or possibly unrelated to acupuncture treatment. The incidents on record included dizziness, nausea, nasal congestion, dry mouth, constipation, and loss of appetite. Adverse effects related to acupuncture regardless of the route were recorded as follows: local pain and/or bruising; fainting; or stuck or curved needle. No patients discontinued study due to serious adverse effects. Specific characteristics of the included studies are shown in Table 1.
Table 1.
Characteristics of the Included Studies
| 1st author, yr & ref. | Participants |
Duration (wks) | Interventions |
Outcome indicators | Adverse effect |
|||
|---|---|---|---|---|---|---|---|---|
| Experiment | Control | Experiment | Control | Experiment | Control | |||
| Cheng, 20076 | 19 | 20 | 6 | Abdominal acupuncture | Electroacupuncture | 1,2 | Yes | Yes |
| Cheng, 20076 | 19 | 21 | 6 | Abdominal acupuncture | Conventional treatment | 1 | Yes | Yes |
| Feng, 20117 | 33 | 32 | 4 | Abdominal acupuncture | Conventional acupuncture | 1,2 | Yes | Yes |
| Li, 20168 | 30 | 30 | 12 | Abdominal acupuncture+ Prozac® | Prozac | 1,2,3a | N/A | |
| Zhang, 20169 | 28 | 28 | 4 | Abdominal acupuncture+ fluoxetine hydrochloride dispersible tablets | Fluoxetine hydrochloride dispersible tablets | 1,2,3a,3b | N/A | |
| Zeng, 201410 | 50 | 50 | 3 | Abdominal acupuncture + Jiawei Xiaoyao capsules | Doxepin hydrochloride tablets | 1,2 | N/A | |
| Li, 201711 | 30 | 30 | 8 | Abdominal acupuncture+ cephalic acupuncture + psychotherapy | Psychotherapy | 1 | N/A | |
| Bi, 201712 | 20 | 20 | 4 | Abdominal acupuncture+ fluoxetine hydrochloride dispersible tablets | Fluoxetine hydrochloride dispersible tablets | 1,2,3a,3b | N/A | |
| Wang, 202013 | 37 | 37 | 8 | Abdominal acupuncture | Body acupuncture | 1,2 | N/A | |
| Jian, 202014 | 47 | 47 | 6 | Abdominal acupuncture + Bupleurum Decoction plus Os draconis & Oyster Shell | Flupentizone melitroxine tablets | 1,3a | N/A | |
| Chen, 201615 | 40 | 40 | 6 | Abdominal acupuncture + Jiawei Sini powder | Paroxetine hydrochloride tablets | 1,2 | No | Yes |
1 = Hamilton Depression Scale scores; 2 = Effective rate; 3a = Barthel index; 3b = National Institutes of Health Stroke Scale scores.
yr, year; wks, weeks; N/A, not available.
Methodological Quality
Among the 10 included RCTs, 6 trials 6–8,10,13,14 used random-number grouping table and 2 trials9,11 did not describe their specific randomization methods clearly. In 1 trial, the patients were grouped in the order of admissions,12 and another trial did not state its grouping method.15 One trial acknowledged that blinding was not used for intervention and evaluation.6 The remaining trials did not mention the use of blinding at all. Only 2 trials6,13 reported completion and attrition rates, but the rest of the studies simply did not acknowledge this component. None of the trials discussed the bias of selective outcome reporting or other potential biases. The risk of biases in all the included studies is shown in Table 2.
Table 2.
Risk of Biases in the 10 Studies
| Study | Random sequence generation | Allocation concealment | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias |
|---|---|---|---|---|---|---|---|
| Cheng, 20076 | Low | Unknown | Low | Low | low | Low | Unknown |
| Feng, 20117 | Low | Unknown | Unknown | Unknown | Unknown | Low | Unknown |
| Li, 20168 | Low | Unknown | Unknown | Unknown | Unknown | Low | Unknown |
| Zhang, 20169 | Unknown | Unknown | Unknown | Unknown | Unknown | Low | Unknown |
| Zeng, 201410 | Low | Unknown | Unknown | Unknown | Unknown | Low | Unknown |
| Li, 201711 | Unknown | Unknown | Unknown | Unknown | Unknown | Low | Unknown |
| Bi, 201712 | High | Unknown | Unknown | Unknown | Unknown | Low | Unknown |
| Wang, 202013 | Low | Unknown | Unknown | Unknown | Low | Low | Unknown |
| Jian, 202014 | Low | Unknown | Unknown | Unknown | Unknown | Low | Unknown |
| Chen, 201615 | Unknown | Unknown | Unknown | Unknown | Unknown | Low | Unknown |
HAMD Scores
All 10 studies used HAMD scores as an outcome indicator with a high heterogeneity value (P < 0.00001, I2 = 91%). As planned, a subgroup analysis was conducted. Heterogeneity testing between subgroups resulted in either no or low value. The fixed-effects model was then used for analysis. The total effect value of the HAMD scores of the 10 studies was (MD = −2.34, 95% confidence interval [CI]: −2.89, −1.78; P < 0.00001). The results of the subgroup analysis are shown in Figure 2.
FIG. 2.
Subgroup analysis of the Hamilton Depression Scale (HAMD) scores. SD, standard deviation; IV, inverse variance; CI, confidence interval; VS, versus.
Three studies used abdominal acupuncture to compare with other types of acupuncture (i.e., conventional acupuncture, body acupuncture, and electroacupuncture). Heterogeneity testing yielded results of P = 0.48 and I2 = 0%. The results of combined-effect value showed that the experimental groups and the control groups HAMD scores were not statistically significant (MD = −0.32; 95% CI: −1.58, 0.93; P = 0.62).
Three studies used abdominal acupuncture in conjunction with conventional antidepressants to compare with antidepressants only (Prozac® and fluoxetine hydrochloride dispersible tablets). Heterogeneity testing produced a result of P = 0.40; I2 = 0%. The results of combined-effect value indicated that the experimental groups were better than the control groups for reducing the HAMD scores (MD = −4.23; 95% CI: −5.57, −2.90; P < 0.00001).
Three studies used abdominal acupuncture with TCM (Jiawei Xiaoyao capsules, Bupleurum Decoction + Os draconis and Oyster Shell, and Jiawei Sini powder) in comparison with antidepressants (doxepin hydrochloride tablets, flupentizone melitroxine tablets, and paroxetine hydrochloride tablets). Heterogeneity testing resulted in P = 0.32; I2 = 11%. The results of combined-effect value showed that abdominal acupuncture combined with TCM was better than antidepressants alone for reducing the HAMD scores (MD = −1.01, 95% CI: −1.78, −0.25; P = 0.009).
Two studies used abdominal acupuncture or a combination of abdominal acupuncture and cephalic acupuncture to compare with conventional treatment methods. Heterogeneity testing resulted in P = 0.43; I2 = 0%, and the combined-effect value results showed that the experimental groups were noticeably better than the control group for reducing HAMD scores (MD = −9.96; 95% CI: −11.71, 8.21; P < 0.00001).
Effective Rates
Eight studies explored the effective rates, and the heterogeneity among the studies was low (P = 0.11; I2 = 40%). Therefore, the fixed-effects model was used for analysis. The results showed that the effective rates of abdominal acupuncture in the experimental groups were significantly higher than that of the control groups (OR = 3.90; 95% CI: 2.29, 6.62; P < 0.00001). See Figure 3.
FIG. 3.
Meta-analysis of effective rate. M-H, Mantel-Haenszel; CI, confidence interval; df, difference.
Barthel Index and NIHSS Scores
Four studies incorporated the Barthel index. The fixed-effects model was used for analysis because there was no heterogeneity among the studies (P = 0.52; I2 = 0%). The increase in the Barthel index of the experimental groups was remarkable, compared with the control groups after treatment (MD = 11.39; 95% CI: 9.07,13.72; P < 0.00001). See Figure 4.
FIG. 4.
Meta-analysis of Barthel index. SD, standard deviation; IV, inverse variance; CI, confidence interval.
Two studies had NIHSS scores with no heterogeneity between them (P = 1.00; I2 = 0%), and the fixed-effects model was used for analysis. There were no significant differences in the NIHSS scores between the experimental groups and the control groups after abdominal acupuncture (MD = −0.03, 95% CI: −0.68, 0.62; P = 0.93).
Publication Bias
A funnel-chart analysis of the 10 studies using HAMD scores projected a certain degree of publication bias. However, a funnel-chart analysis of 8 studies examining the effective rates showed no publication bias or small publication bias. Only a few studies reported the Barthel index or NIHSS scores; therefore, no analysis for publication bias was performed.
Discussion
TCM views that PSD is a variant syndrome secondary to stroke. In other words, PSD is a mood disorder produced by the insult of the physical disease. Whereas anxiety damages the Liver, causing Qi Stagnation, Blood Stasis, and internal resistance, Stagnation leads to further injuries of the vascular system consuming Qi. Eventually, Qi, Blood, Heart, and Spleen would become Deficient. Abdominal acupuncture is a new treatment technique for addressing chronic and complex diseases proposed by Dr. Z.Y. Bo in 2001.3 The theory of the viscera meridian system stipulates that the internal meridians are associated with the viscera organs (zang-fu) and that the external meridians connect the limbs and bones. This concept is well-applied in the practice of abdominal acupuncture. PSD and other chronic diseases share a common characteristic: they are long-standing with progressive internal invasion. Treatment via abdominal acupuncture, therefore, emphasizes starting with regulating the viscera to reverse the course of the disease.
Abdominal acupuncture has a long history of treatment for diseases. There is a plethora of records regarding abdominal meridian circulation, acupoint positioning, and treatment via the abdominal meridian in the literature of the Internal Classics. At the turn of the twenty-first century, Dr. Bo proposed the abdominal acupuncture system integrating the theory of TCM and modern biomedicine. Since then, this treatment modality has developed rapidly in China with ever-increasing research exploring its efficacy. Currently, abdominal acupuncture has been used to treat cervical spondylosis, insomnia, depression, and sequelae of cerebrovascular disease.16–22 Each abdominal acupuncture point in the records included in this study for treating PSD may each have individual characteristics. The acupoints ranged from Zhongwan, Xiawan, Qihai, Guanyuan, Huaroumen, Wailing, and bilateral upper and lower acupoints for rheumatism, to the large horizontal acupoint.
The meta-analysis revealed that the HAMD scores, effective rates, and Barthel indices of patients receiving abdominal acupuncture treatment for PSD were better than the results of the control groups. Acupuncture therapy has proven to be effective for reducing PSD symptoms in many previous studies.23–26 The subgroup analysis of the HAMD scores in this current study showed that the effect of abdominal acupuncture for treating PSD was comparable to other common acupuncture methods and could achieve the same degree of clinical effect. Compared with traditional acupuncture methods, abdominal acupuncture causes less discomfort to patients.7
It is worth noting that more-rigorous RCTs will be needed to confirm the effect of abdominal acupuncture on PSD, compared with other acupuncture methods, further due to the small number of available studies in the subgroup analysis. In all current subgroup analyses, the efficacy of abdominal acupuncture in the experimental groups was significantly higher than the control groups. The results of combined-effect size also showed that the effective rate of abdominal acupuncture in the experimental groups was higher than the control groups. In terms of neurologic rehabilitation, abdominal acupuncture was effective for improving the ADLs in patients with PSD, but this modality was not statistically significant for reducing NIHSS scores. This finding was consistent with the results of other studies in the literature.5,27 It might be related to the paucity of studies focusing on the examination of outcome index using the NIHSS scores. More research is needed in the future to investigate the reduction of neurologic deficits further in patients with PSD when treated with abdominal acupuncture.
Limitations of the Studies in this Meta-Analysis
Most of the studies had flaws in their research design, as follows:
-
(1)
Given that the majority of the studies had small sample sizes, false–positives might have occurred.
-
(2)
Although many of these researchers stated that they had use the random-number table as the grouping methods, no specific descriptions were provided. A few studies did not even mention their grouping methods.
-
(3)
The blinding application was deficient. Most of the studies did not mention use of blinding.
-
(4)
In some cases, the design of the intervention plans and the control plans could have been more rigorous. For example, sham stimulation as a placebo could have enhanced the credibility of those trials.
-
(5)
Finally, the statistical methods in some studies were not optimal. For instance, a few studies took measurements at different timepoints during the course of treatment. Repetitive-measure analysis of variance should have been used in these studies.28
Conclusions
This meta-analysis shows that abdominal acupuncture therapy has certain benefits for treating PSD. However, further research is needed to explore if this modality is also effective for reducing the neurologic-deficit scores of patients. Since abdominal acupuncture only began to be promoted about 20 years ago, the number of studies included in this meta-analysis was relatively small. In addition, the interventions of the included studies lacked consistency. The current authors hope to see high-quality investigations with more rigorous designs, larger sample sizes, and multicenter RCTs so this treatment method can be truly evidence-based.
Author Disclosure Statement
No financial conflicts of interest exist.
Funding Information
This study did not receive a special grant from any funding agency.
References
- 1.Wu SM, Wu B, Liu M, et al. ; China Stroke Study Collaboration. Stroke in China: Advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18(4):394–405 [DOI] [PubMed] [Google Scholar]
- 2.Hackett ML, Pickles K. Part I: Frequency of depression after stroke. An updated systematic review and meta-analysis of observational studies. Int J Stroke. 2014;9(8):1017–1025 [DOI] [PubMed] [Google Scholar]
- 3.Bo ZY. On abdominal acupuncture therapy [in Chinese]. Chin Acupunct Moxibustion. 2001;21(8):474–476 [Google Scholar]
- 4.Higgins JP, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: John Wiley & Sons, Ltd; 2008 [Google Scholar]
- 5.Zhou X, Ren L, Gao YY, et al. Meta-analysis of effect of acupuncture and antidepressants on depression in patients with post-stroke depression [in Chinese]. Chin Archives Tradit Chin Med. 2018;36(12):2875–2879 [Google Scholar]
- 6.Cheng Y, Tang QS. Abdominal acupuncture in treating Liver-Qi Stagnation and Spleen Deficiency in the elderly with post-stroke depression: A randomized and controlled observation. J Clin Rehabil Tissue Eng Res. 2007;11(39):7791–7794 [Google Scholar]
- 7.Feng Y, Xiao HL, Lin RY, et al. Bo's abdominal acupuncture in the treatment of depression after stroke [in Chinese]. J Clin Acupunct Moxibustion. 2011;27(10):33–35 [Google Scholar]
- 8.Li XN, Wu L, Chi L. Therapeutic observation of abdominal acupuncture “air entraining Guiyuan” with drugs for post stroke depression [in Chinese]. J Clin Acupunct Moxibustion. 2016;32(3):9–12 [Google Scholar]
- 9.Zhang EQ, Wang J, Zhang J. Clinical study on Bo's abdominal acupuncture in the treatment of post stroke depression [in Chinese]. Acta Chin Med. 2016;31(10):1623–1625 [Google Scholar]
- 10.Zeng ZP, Wu SH. Clinical study in Bo's abdominal acupuncture combined with Jiawei Xiaoyao Capsule treating depression after stroke [in Chinese]. Chin Manipulation Rehabil Med. 2014;(7):45–45,46 [Google Scholar]
- 11.Li GZ. Effect observation of psychological rehabilitation with cephalic acupuncture and Bo's abdominal acupuncture therapy in the treatment of post-stroke depression [in Chinese]. Chin J Pract Nerv Dis. 2017;20(13):86–88 [Google Scholar]
- 12.Bi XQ, Xiong Q, Wei M, et al. Application and effect of abdominal acupuncture in the treatment of post-stroke depression [in Chinese]. Chin J Geriatr Care. 2017;15(5):41–42,44 [Google Scholar]
- 13.Wang YM, Zhang XX, Yang XY. Clinical study of Sun's abdominal acupuncture on patients with post stroke depression [in Chinese]. Shandong J Tradit Chin Med. 2020;39(1):26–29 [Google Scholar]
- 14.Jian M, Wen Y, Zhao JH. Observation of the therapeutic effect of Bupleurum Decoction plus Os draconis and Oyster Shell combined with abdominal acupuncture on post-stroke depression [in Chinese]. Henan Tradit Chin Med. 2020;40(2):206–209 [Google Scholar]
- 15.Chen HM, Gao M, Yu T. Therapeutic effect of Jiawei Sini powder combined with abdominal acupuncture on post-stroke depression: An observational study [in Chinese]. Stroke Nerv Dis. 2016;23(5):347–349 [Google Scholar]
- 16.Zhou W, Wang LP. Observation on therapeutic effect of abdominal acupuncture on spastic paralysis after cerebrovascular disorder [in Chinese]. Chin Acupunct Moxibustion. 2005;25(11):757–759 [PubMed] [Google Scholar]
- 17.Guo WG, Ma LR, Gong LF, et al. Observation on the therapeutic effect of abdominal acupuncture on intervertebral disk displacement in 50 cases [in Chinese]. Chin Acupunct Moxibustion. 2003;23(3):145–146 [Google Scholar]
- 18.Guo Y-Q, Chen L-Y, Fu W-B, Xu M-Z, Ou X-M. Clinically randomized controlled study on abdominal acupuncture for treatment of cervical spondylosis [in Chinese]. Chin Acupunct Moxibustion. 2007;27(9):652–656 [PubMed] [Google Scholar]
- 19.Ho LF, Lin ZX, Leung AWN, et al. Efficacy of abdominal acupuncture for neck pain: A randomized controlled trial. PLoS One. 2017;12(7):e0181360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mo X-F, Xuan L-H, Jin Y-B, Cheng X-H, Yu B-Y. Efficacy observation on abdominal acupuncture for adhesion-stage shoulder periarthritis [in Chinese]. Chin Acupunct Moxibustion. 2013;33(9):847–849 [PubMed] [Google Scholar]
- 21.Qin Y, Yi W, Lin S, Yang C, Zhuang Z. Clinical effect of abdominal acupuncture for diarrhea irritable bowel syndrome [in Chinese]. Chin Acupunct Moxibustion. 2017;37(12):1265–1268 [DOI] [PubMed] [Google Scholar]
- 22.Wang YW, Fu WB, Ou AH, Fan L, Huang YF. A systematic review of randomized controlled clinical trials of abdominal acupuncture treatment of cervical spondylosis [in Chinese]. Acupunct Res. 2011;36(2):137–144 [PubMed] [Google Scholar]
- 23.Nie RR, Huang CH. Post-stroke depression treated with acupuncture and moxibustion: An evaluation of therapeutic effect and safety [in Chinese]. Chin Acupunct Moxibustion. 2013;33(6):490–494 [PubMed] [Google Scholar]
- 24.Liu JP, Bourchier S, Cao HJ. Does syndrome differentiation matter? A meta-analysis of randomized controlled trials in Cochrane Reviews of Acupuncture. Med Acupunct. 2012;24(2):68–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cai W, Ma W, Wang GT, Shen WD. Efficacy and safety of electroacupuncture for post stroke depression: Study protocol for a randomized controlled trial. Trials. 2018;19(1)152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang L, Zhong Y, Quan SL, Liu Y, Shi X, Li Z, Wang J. Acupuncture combined with auricular point sticking therapy for post stroke depression: A randomized controlled trial [in Chinese]. Chin Acupunct Moxibustion. 2017,37(6):581–585 [DOI] [PubMed] [Google Scholar]
- 27.Wang Q, Guo Y, Liu Y, et al. Meta-analysis of auricular point sticking in the treatment of post-stroke depression [in Chinese]. China Med Her. 2018;15(4):103–107 [Google Scholar]
- 28.Xie YM, Xu GQ. Longitudinal data analysis methods in the evaluation of clinical efficacy of the application [in Chinese]. J Basic Chin Med. 2007;13(9):711–713 [Google Scholar]