Abstract
The number of individuals in the United States who report food insecurity doubled between 2005 and 2012, with little research investigating possible disparities across time in food-insecure populations. The aim of this study was to investigate trends in food insecurity between 2001–2017 by sex, race/ethnicity, income, and age. Adults participating in the National Health Interview Survey (NHIS) between 2011–2017 were included in the study. Food insecurity was dichotomized based on affirmative responses to the Food Security Survey Module. Statistical analysis included logistic regression to investigate trends in food insecurity over time by each demographic variable (age, sex, race/ethnicity, income) adjusted by survey year and demographic variables. After adjustment, those ages ≥65 years were 39% less likely (OR = 0.61, 95% CI [0.57,0.65]) to report food insecurity compared to those ages 18–34; females were 23% more likely to be food insecure than males (OR = 1.23, 95% CI [1.19,1.27]); non-Hispanic blacks were 1.7 times more likely (OR = 1.69, 95% CI [1.62,1.76]) to be food insecure than non-Hispanic whites; and a clear gradient existed by income, with lower incomes more likely to be food insecure. Disparities in food insecurity exist across age, race/ethnicity, sex, and income and were consistent over time. These results suggest that targeted programs may be necessary to decrease food insecurity in particularly vulnerable subpopulations, and barriers to access and use of existing programs need to be investigated.
Keywords: food insecurity, health disparities, soceioeconomic status, race/ethnicity
Introduction
The number of individuals in the United States who report food insecurity doubled from 9% to 18% between 2005 and 2012.1 Declines in levels of food insecurity have since been seen in the overall population; however, some groups continue to experience high levels of food insecurity.2 Defined by the US Department of Agriculture as an inability to or limitation in accessing nutritionally adequate foods, food insecurity has been hypothesized to be a potentially modifiable mechanism that helps explain the influence of poverty on health among individuals of low socioeconomic status.2–7 Significant evidence supports a relationship between food insecurity, mental and physical health, and an individual's ability to manage health conditions.8–10 Food insecurity is associated with overall lower dietary quality, and individuals who are food insecure report concerns that include anxiety surrounding food insufficiency, the need to make food budget adjustments throughout the month, alterations in the types of food obtained, and the need to reduce food intake.2,4,7 Food insecurity also is associated with all-cause mortality in the United States with lifestyle factors explaining much of the relationship.11 Finally, the lack of resources is not limited to the ability to purchase food, with 1 in 3 US adults reporting an inability to afford food, medication, or both.12,13
A better understanding of the social and economic factors influencing health, such as food insecurity, may help direct interventions to address health disparities seen across and within populations.9,14 Generally, individuals who report food insecurity are younger, female, from a racial/ethnic minority group, and have lower educational levels or lower socioeconomic status compared to those reporting food security.3,12,15,16 Minorities and individuals with chronic medical conditions influenced by diet have been shown to report higher levels of food insecurity.1,12,15–18 In addition, there is some indication that women and men respond differentially to food insecurity, which often is seen in a differential influence of combined food insecurity and high obesity in low-income women.8,19 Although some studies have investigated whether trends occur over time, these analyses tend to focus on changes within subpopulations as opposed to differences between these groups.
Because access to different federal and local programs that can assist food-insecure individuals (eg, the Supplemental Nutrition Assistance Program [SNAP], the Women, Infants, and Children [WIC] program) differ by race/ethnicity, sex, and income, investigation of whether specific subpopulations have higher food insecurity over time is important. A recent study showed that structural barriers, such as transportation, obtaining an appointment, child care, and taking off work, impact the number of individuals who are eligible for but do not take part in federal programs.20 The barriers themselves or the way in which these barriers influence individuals' access to programs may differ by demographic factors. For example, in an analysis of women eligible for WIC participation, Hispanics and non-Hispanic blacks were more likely to participate; however, fewer social supports and more structural barriers decreased the likelihood of participation.20 A greater proportion of eligible nonparticipants were noted in income ranges from $20,000-$24,999, which may be because of being unaware of eligibility.20 In addition, although SNAP has been shown to improve caloric, macronutrient, and micronutrient intake, participants continue to struggle with meeting dietary guidelines.21–24 Non-Hispanic blacks, in particular, report a weaker association between food insecurity and diet quality when participating in SNAP.25 Additional factors, such as food deserts, residential segregation, and structural racism, also influence the experiences different demographic groups have with access to and use of programs, necessitating an understanding of differences in food insecurity and whether this varies over time.26–28
Many studies investigate food insecurity, either at a specific point in time or over time in a specific group. To understand if differences noted in levels of food insecurity by sex, race/ethnicity, income, and age across the US population change over time, the research team aimed to investigate trends in the proportion of individuals reporting food insecurity between 2001–2017 across a number of demographic variables. If differences are consistent over time, this information can inform where additional assistance is needed to reduce possible health disparities resulting from food insecurity.
Methods
Data source and study population
This cross-sectional study used data from the National Health Interview Survey (NHIS), which includes information on the health of the civilian, noninstitutionalized population in the United States. NHIS data are used to monitor trends in illness and disability and to track the country's progress in attaining national health goals.29 This study used 7 consecutive years of NHIS data between the years 2011–2017. Family and person files were used for each year.30 Food insecurity questions were first asked in the year 2011, so that was selected as the first year of data. For each family, a single family member serves as the primary respondent for the family, providing information for all children and adult family members. A total of 288,079 families participated in the NHIS survey during 2011–2017. After excluding those without food security measure responses, 287,836 family respondents were used in this analysis.
Because the study used publicly available data, no institutional review board approval was requied.
Food insecurity measure and outcome
During each year of the survey, the same validated scale for food insecurity was used. Ten questions were asked of each family using questions and response options from the US Departement of Agriculture Food Security Survey Module. A 4-level food security status was calculated based on the number of affirmative responses using scoring from Bickel et al4:
-
1.
High Food Security (no affirmative responses)
-
2.
Marginal Food Security (1–2 affirmative responses)
-
3.
Low Food Security (3–5 affirmative responses)
-
4.
Very Low Food Security (6–10 affirmative responses)
These categories were then dichotomized into the outcome: Food Secure (categories 1 & 2) and Food Insecure (categories 3 & 4).
Demographic variables
The demographic variables included: age in years (18–34, 35–49, 50–64, ≥65), sex (male, female), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other minorities), and income measured by the ratio of income to the federal poverty level (<1.00, 1.00–1.99, 2.00–3.99, ≥4.00).
Statistical analysis
Statistical analysis were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC). As NHIS data were collected using a complex multistage design, SAS procedures for survey sampling were used to calculate correct variance estimation. NHIS variance estimation for pooled analyses of adjacent years of the NHIS suverys were followed. To investigate trends over time, a series of logistic regression models were run with food insecurity status as the outcome in each. First, unadjusted models were run for each demographic factor alone (age, sex, race/ethnicity, and income). Second, an adjusted model was run that included all 4 demographic variables and survey year. Variables added to the model were selected a priori and based on important demographic factors noted in the literature to differ by food insecurity status. Statistical significance was considered at the P < 0.05 level.
Results
In total, 287,836 family respondents, representing 124,761,416 US families, had food insecurity data available. The sample demographics are shown in Table 1 to provide an overview of those included in the analysis. Across all years included in the analysis, 10.56% of the sample families reported food insecurity. Of those who were food insecure, more than 11% were aged ≥65 years, slightly more than 65% were female, slightly more than 52% were non-Hispanic white, and more than 41% earned income below the federal poverty level based on the ratio of income to the federal poverty level being below 100%.
Table 1.
Weighted Sample Demographics by Food Security Status for All Participants 2011–2017
| Food secure | Food insecure | P | |
|---|---|---|---|
| Unweighted Sample | n = 254,791 | n = 33,045 | |
| Weighted Sample | N = 111,582,148 | N = 13,179,268 | |
| Mean Age, years | 50.2 | 45.9 | |
| Age Group | <.0001 | ||
| 18–34 | 23.96% | 27.23% | |
| 35–49 | 24.86% | 30.52% | |
| 50–64 | 27.37% | 30.47% | |
| ≥65 | 23.81% | 11.78% | |
| Sex | <.0001 | ||
| Male | 44.11% | 34.85% | |
| Female | 55.89% | 65.15% | |
| Race/Ethnicity | <.0001 | ||
| Non-Hispanic White | 71.18% | 52.19% | |
| Non-Hispanic Black | 11.12% | 23.50% | |
| Hispanic | 11.78% | 20.06% | |
| Other minorities | 5.93% | 4.26% | |
| Ratio of family income to poverty | <.0001 | ||
| <1.00 | 12.25% | 41.49% | |
| 1.00–1.99 | 16.60% | 33.76% | |
| 2.00–3.99 | 33.41% | 20.25% | |
| ≥4.00 | 37.74% | 4.50% |
Table 2 shows the results of the logistic regression models for each demographic variable and food insecurity. For the multivariable logistic models with survey year and demographics, those who were aged ≥65 years were 39% (OR = 0.61, 95% CI [0.57,0.65]) less likely to report food insecurity when compared to their 18- to 34-year-old counterparts. Those aged 35 to 49 and 50 to 64 were more likely to report food insecurity compared to the referent group aged 18 to 34 years (Table 2). Females were more likely to be food insecure than males. When compared to non-Hispanic white individuals, non-Hispanic blacks and Hispanics were more likely to be food insecure, while other minority individuals were less likely to be food insecure (Table 2). In comparison to those who have a ratio of income to the federal poverty level <1.00, those who had a ratio of 1.00–1.99, 2.00–3.99, and ≥4.00 were less likely to be food insecure. The time variable for survey year was statistically significant (P < 0.001) in all logistic models, indicating significant changes over time.
Table 2.
Logistic Models for Relationship Between Food Insecurity and Demographics
| Unadjusted |
Adjusted* |
|
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Age Group | ||
| 18–34 | ref | ref |
| 35–49 | 1.08 (1.04–1.12) | 1.62 (1.55–1.70) |
| 50–64 | 0.98 (0.94–1.02) | 1.66 (1.58–1.75) |
| ≥65 | 0.44 (0.41–0.46) | 0.61 (0.57–0.65) |
| Sex | ||
| Male | ref | ref |
| Female | 1.48 (1.43–1.52) | 1.23 (1.19–1.27) |
| Race/Ethnicity | ||
| Non-Hispanic White | ref | ref |
| Non-Hispanic Black | 2.88 (2.77–3.00) | 1.69 (1.62–1.76) |
| Hispanic | 2.32 (2.22–2.43) | 1.24 (1.18–1.30) |
| Other minorities | 0.98 (0.90–1.06) | 0.78 (0.72–0.85) |
| Ratio of family income to poverty | ||
| <1.00 | ref | ref |
| 1.00–1.99 | 0.60 (0.58–0.63) | 0.64 (0.62–0.67) |
| 2.00–3.99 | 0.18 (0.17–0.19) | 0.19 (0.18–0.20) |
| ≥4.00 | 0.04 (0.03–0.04) | 0.04 (0.03–0.04) |
In adjusted models all variables were included in the same model along with survey year.
CI, confidence interval; OR, odds ratios.
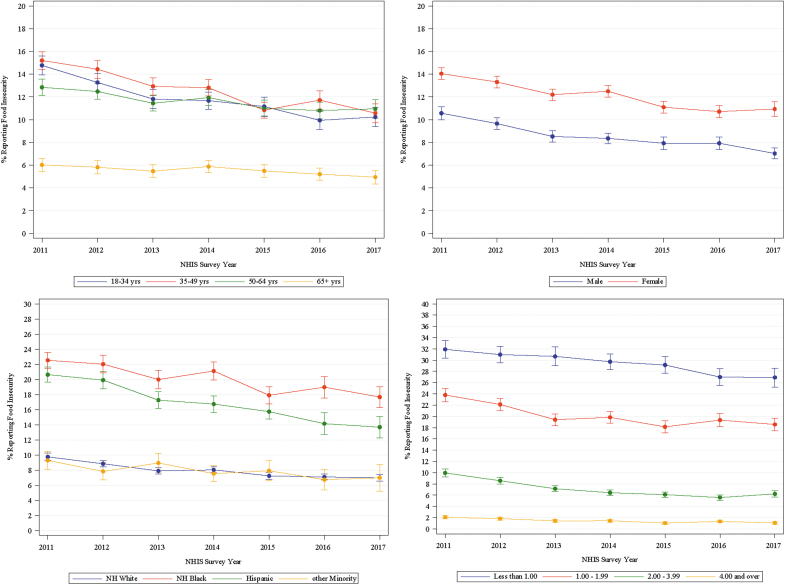
Figure 1 illustrates the percent of people for each demographic variable who report food insecurity. All demographic variables – age, sex, race/ethnicity, and the ratio of income to the federal poverty level – had an overall decreasing trend in reports of food insecurity across the study period. For age, the group aged ≥65 years had the smallest percent reporting food insecurity with slight increases in the years 2014 and 2017. Females reported slightly higher food insecurity percentage than males. Non-Hispanic black individuals had the highest percent of food insecurity followed by Hispanics, with lower proportions of other minorities and non-Hispanic whites reporting food insecurity. There was a clear gradient by income with individuals living at less than 100% of the poverty level reporting significantly higher food insecurity, and individuals living between 100%-150% over the poverty level reporting somewhat lower levels that were consistently higher than groups reporting 200% of the poverty level or higher.
FIG. 1.
Percent of population reporting food insecurity over time, by demographic variable. NH, non-Hispanic; NHIS, National Health Interview Survey.
Discussion
Using a nationally representative sample of US families, this study found that disparities in proportion of food insecurity exist across age, race/ethnicity, sex, and income. Though food insecurity has decreased over time for those aged <65 years, regardless of age group, they reported higher levels of food insecurity than those aged ≥65 years. Similarly, although the overall percentage decreased over time, women consistently reported higher food insecurity compared to men. Compared to non-Hispanic whites, non-Hispanic blacks were 69% more likely, and Hispanics were 24% more likely to report food insecurity, and this disparity persisted across time between 2011–2017. Finally, a gradient existed by income, with trends consistent across time.
This study adds to the literature by helping to understand trends in food insecurity over time by a number of sociodemographic factors. Results suggest important areas for future interventions, and highlight vulnerable populations that may require increased attention to decrease the influence food insecurity has on the US population. A modeling study on the impact of national and targeted dietary policies found that a national 10% fruit and vegetable subsidy would potentially prevent or postpone 150,500 deaths related to cardiovascular disease, while a 30% fruit and vegetable subsidy targeting SNAP participants may save fewer lives but would decrease disparities by approximately 8%.31 Understanding the impact of factors, such as food insecurity, in the context of these kinds of policy trade-offs are necessary to systematically decrease disparities in health. As changes in health policies, such as work requirements for SNAP eligibility, or increases in benefits during the COVID pandemic play out, it is important to monitor social and health conditions over time to ensure disparities are being reduced.32
The consistent disparity over time, despite changes in the overall economic climate and policies targeted at increasing access to resources for vulnerable groups suggests that barriers continue to exist for younger individuals, women, minorities, and those living at a low socioeconomic status. The need to improve understanding of eligibility and decrease barriers to participation in federal programs is therefore warranted. Given the impact social factors, such as discrimination and structural racism, have on accessing programs, it also may be necessary to make it easier for families to access safety net programs through trusted community organizations, and to consider how interactions across different forms of discrimination impact use of programs.27,28 A second factor may be the number of programs available. This study found that all age groups <65 years had higher food insecurity. More support may exist for the elderly, including food pantries and food delivery services specific for elderly populations, in addition to support through programs such as Medicare for transportation and medical costs. For example, the Elderly Nutrition Program conducted by the US Department of Health and Human Services Administration on Aging provides meals to seniors in group settings and in the homes of elderly who are homebound. There are approximately 3 million elderly participants and they receive up to 50% of required nutrients from meals provided by this program.33 Though dedicated programs exist for low-income groups, the lack of specificity to meeting the needs of particular populations, or barriers to accessing the support, may limit the impact of the program.
Limitations
Though this analysis provides nationally representative trends in food insecurity for a variety of vulnerable populations, there are a number of limitations worth noting. First, the data are cross-sectional, and therefore no comments can be made on causality or longitudinal impact on particular individuals over time. Second, sociodemographics are known to interact, and therefore some disparities seen can be a result of multiple areas of vulnerability. Finally, although the research team can speculate on the relationship between disparities and food insecurity, reasons for this relationship cannot be explained fully without data providing finer detail, such as details regarding neighborhood factors.
Conclusion
This study found consistent disparities across age, sex, race/ethnicity, and income in the proportion of food insecurity reported by US adults. Those aged <65 years (regardless of age group), women, non-Hispanic blacks, and Hispanics indicated higher food insecurity. In addition, a clear gradient existed by income with lower incomes reporting higher levels of food insecurity. These differences persisted over time between 2011 and 2017. These results suggest targeted programs may be necessary to decrease food insecurity in particularly vulnerable subpopulations and barriers to access and use of existing programs need to be investigated.
Authors' Note
Data used for this study are publicly available at url: https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm
Author Disclosure Statement
The authors declare that there are no conflicts of interest.
Funding Information
Effort for this study was partially supported by the National Institute of Diabetes and Digestive Kidney Disease (K24DK093699, R01DK118038, R01DK120861, PI: Egede), the National Institute for Minority Health and Health Disparities (R01MD013826, PI: Egede/Walker), and the American Diabetes Association (1-19-JDF-075, PI: Walker).
References
- 1.Berkowitz SA, Berkowitz TSZ, Meigs JB, Wexler DJ. Trends in food insecurity for adults with cardiometabolic disease in the United States: 2005–2012. PLoS One 2017 7;12:e0179172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. 2018. Household Food Security in the United States in 2017, ERR-256, USDepartment of Agriculture, Econogmic Research Service. https://www.ers.usda.gov/publications/pub-details/?pubid=90022 Accessed September11, 2020
- 3.Seligman H, Bindman A, Vittinghoff E, Kanaya A, Kushel M. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med 2007;22:1018–1023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security. Alexandria, VA: U.S. Department of Agriculture, Food and Nutrition Service, 2000 [Google Scholar]
- 5.Seligman HK, Jacobs EA, Lopez A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care 2012;35:233–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved 2010;21:1227–1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med 2014;127:303–310.e3. [DOI] [PubMed] [Google Scholar]
- 8.Gucciardi E, Vahabi M, Norris N, Del Monte JP, Farnum C. The intersection between food insecurity and diabetes: a review. Curr Nutr Rep 2014;3:324–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Essien UR, Shahid NN, Berkowitz SA. Food insecurity and diabetes in developed societies. Obesity 2016;16:79. [DOI] [PubMed] [Google Scholar]
- 10.Vozoris NT, Tarasuk VS. Household food insufficiency is associated with poorer health. J Nutr 2003;133:120–126 [DOI] [PubMed] [Google Scholar]
- 11.Walker RJ, Chawla A, Garacci E, Willaims JS, Mendez C, Ozieh MN, et al. Assessing the relationship between food insecurity and mortality among US adults. Ann Epidemiol 2019;34:33–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berkowitz SA, Meigs JB, DeWalt D, Seligman HK, Barnard LS, Bright OJ, et al. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med 2015;175:257–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Knight CK, Probst JC, Liese AD, Sercye E, Jones SJ. Household food insecurity and medication “scrimping” among US adults with diabetes. Prev Med 2016;83:41–45 [DOI] [PubMed] [Google Scholar]
- 14.Marmot M.Social determinants of health inequities. Lancet 2005; 365:1099–1104 [DOI] [PubMed] [Google Scholar]
- 15.Strings S, Ranchod YK, Laraia B, Nuru-Jeter A. Race and sex differences in association between food insecurity and type 2 diabetes. Ethn Dis 2016; 26: 427–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jernigan VBB, Huyser KR, Valdes J, Simonds VW. Food insecurity among American Indians and Alaska Natives: a national profile using the current population survey-food security supplement. J Hunger Environ Nutr 2017; 12:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walsemann KM, Ro A, Gee GC. Trends in food insecurity among California residents from 2001 to 2011: inequities at the intersection of immigration status and ethnicity. Prev Med 2017; 105: 142–148 [DOI] [PubMed] [Google Scholar]
- 18.Vaccaro JA, Huffman FG. Sex and race/ethnic disparities in food security and chronic disese in US older adults. Gerontol Geriatr Med 2017; 3:2333721417718344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hernandez DC, Reesor LM, Murillo R. Food insecurity and adult overweight/obesity: gender and race/ethnic disparities. Appetite 2017; 1117: 373–378 [DOI] [PubMed] [Google Scholar]
- 20.Liu CH, Liu H. Concerns and structural barriers associated with WIC participation among WIC-eligible women. Public Health Nurs 2016; 33: 395–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mabli J and Ohis J. Supplemental Nutrition Assistance Program participation is associated with an increase in household food security in a national evaluation. J Nutr 2015; 145: 344–351 [DOI] [PubMed] [Google Scholar]
- 22.Mabli J and Worthington J. Supplemental Nutrution Assistance program participation and emergency food pantry use. J Nutr Educ Behav 2017; 49: 647–656 [DOI] [PubMed] [Google Scholar]
- 23.Andreyeva T, Tripp AS, Schwartz MB. Dietary quality of Americans by Supplemental Nutrition Assistance Program participation status: a systematic review. Am J Prev Med 2015; 49: 594–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grummon AH and Taillie LS. Nutritional profiles of Supplemental Nutrition Assistance Program household food and beverage purchases. Am J Clin Nutr 2017; 105: 1433–1442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Allen AJ, Kuczmarski MF, Evans MK, Zonderman AB, Waldstein SR. Race differences in diet quality of urban food-insecure Blacks and Whites reveals resiliency in Blacks. J Racial Ethn Health Disparities 2016; 3: 706–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boyd RW, Lindo EG, Weeks LD, McLemore MR. On racism: a new standard for publishing on racial health inequities. Health Affairs Blog 2020 [Google Scholar]
- 27.Odoms-Young AM.Examining the impact of structural racism on food insecurity: implications for addressing racial/ethnic disparities. Fam Community Health 2018; 41(Suppl 2): S3–S6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017;389:1453–1463 [DOI] [PubMed] [Google Scholar]
- 29.National Center for Health Statistics (NCHS). National Health Interview Survey. https://www.cdc.gov/nchs/nhis/about_nhis.htm Accessed November15, 2017
- 30.National Center for Health Statistics (NCHS). NHIS Data. https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm Accessed November15, 2017
- 31.Pearson-Stuttard J, Bandosz P, Rehm CD, Penalvo J, Whitsel L, et al. Reducing US cardiovascular disease burden and disparities through national and targeted dietary policies: a modelling study. PLoS Med 2017; 14: e1002311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ku L, Brantley E. Widening social and health inequalities during the COVID-19 pandemic. JAMA Health Forum Insights. https://jamanetwork.com/channels/health-forum/fullarticle/2767253 Accessed September11, 2020 [DOI] [PubMed]
- 33.Administration on Aging. (2017). Facts: elderly nutrition program. US Department of Health and Human Services: Washington, DC. http://dhhs.ne.gov/medicaid/Documents/AGS_Elderly_Nutrition_Program.pdf Accessed November28, 2018