Abstract
Eating disorder symptoms and suicidal ideation are relatively common, and often begin to emerge in adolescence. Interoceptive deficits, or the inability to perceive and accurately identify the physiological condition of the body, is an established risk factor for both eating disorders and suicidal thoughts and behaviors. Despite this, longitudinal research examining the temporal dynamics between these variables is scarce, especially within adolescent samples. Using a three-wave longitudinal design, the present study tested bidirectional relationships between interoceptive deficits, eating disorder symptoms, and suicidal ideation to examine whether interoceptive deficits predicted eating disorder symptoms and suicidal ideation over the course of a year among a sample of adolescents. Participants were 436 community adolescents recruited from local middle- and high-schools. Data were collected at baseline, 6-month follow-up, and 12-month follow-up. Study measures assessed current suicidal ideation, eating disorder symptom severity, and interoceptive deficits. Autoregressive cross-lagged modeling was conducted in MPlus. We found baseline eating disorder symptoms significantly predicted suicidal ideation at 6-month follow-up when controlling for baseline suicidal ideation. Baseline interoceptive deficits significantly predicted eating disorder symptoms 6-months later, while 6-month follow-up interoceptive deficits significantly predicted 12-month follow-up suicidal ideation. Our findings highlight the need for early and regular assessment of suicidal ideation and eating disorder symptoms in adolescents. Given that interoceptive deficits was a shared risk factor for both conditions within this sample, these results underscore the need for targeted interventions aimed at improving interoception.
Keywords: suicidal ideation, interoceptive deficits, interoception, eating disorders, adolescents
Adolescents with eating disorders (EDs) experience thoughts of suicide at a significantly higher rate than the general population (Franko & Keel, 2006; Obeid et al., 2020). While past research has continually demonstrated a robust cross-sectional relationship between ED symptoms and suicide ideation (Eichen et al., 2016), work examining the longitudinal association between these conditions in adolescents is limited (Crow et al., 2008a; Kim & Kim, 2009; Perkins & Brausch, 2019). Of the few studies that do exist, several found evidence supporting a unidirectional relationship with ED symptoms predicting future suicidal ideation in adolescents (Crow et al., 2008a; Kim & Kim, 2009; Perkins & Brausch, 2019). Yet, other work has suggested that this association may be bidirectional, as in some cases, suicidal ideation has been shown to either precede (Forrest et al., 2016) or predict (Ortiz & Smith, 2020) ED symptoms in adults. As both EDs and suicidal ideation typically onset in middle to late adolescence (Mustelin et al., 2016; Rueter & Kwon, 2005; Stice et al., 1998), examining the course of ED symptom engagement and suicidal ideation experiences together during this developmental period may provide insight into how these conditions influence each other over time. Additionally, examining risk factors associated with both EDs and suicidality, such as the inability to accurately identify bodily and emotional signals (i.e. interoceptive deficits; Brown et al., 2018; Forrest et al., 2015; Jenkinson et al., 2018; Rogers et al., 2018), during this period could significantly improve treatment and prevention efforts by allowing mental health professionals to more directly address risk and maintenance factors.
Many adolescents with EDs experience suicidal ideation over the course of their disorder with estimates of those experiencing thoughts about suicide in bulimia nervosa and binge eating disorder ranging from 34–53% (Crow et al., 2014). Cross-sectionally, greater ED symptom severity is associated with more frequent and severe thoughts of suicide in both adolescents (Crow et al., 2008b) and adults (Eichen et al., 2016). In addition, a recent meta-analysis found that ED diagnoses and symptomology were significant, albeit weak, risk factors for suicide attempts (Smith et al., 2019b). Among the limited research examining the ED-suicidal ideation pathway in adolescence, a recent study found that body dissatisfaction and purging behaviors, but not restricting behaviors, predicted suicidal ideation at 6- and 12-month follow-ups in a community sample of adolescents (Perkins & Brausch, 2019). Another study using a community sample of adolescents found that body dissatisfaction predicted suicidal ideation at a 2-year follow-up (Kim & Kim, 2009). Beyond these two studies, additional work has found that in adolescents, ED symptoms at baseline predict suicide attempts at follow-up (Crow et al., 2008a; Rodríguez-Cano et al., 2006). However, many of these studies had long periods of time between their baseline and follow-up assessments (i.e., 2 to 5 years) and as such, could not capture the more short-term variation in these behaviors (e.g., Bryan & Rudd, 2016; Smyth et al., 2007). As suicidal ideation and ED symptoms fluctuate greatly over weeks and months (Bryan & Rudd, 2016; Smyth et al., 2007), future work should utilize methodological approaches that can capture these dynamic changes.
While past work demonstrates EDs may predict suicidal ideation, other work suggests that the reverse may also be true. Suicidal ideation is often used as a way to escape from and cope with the experience of negative emotional states and experiences (Anestis & Joiner, 2011). Individuals who think about suicide may engage in alternative coping strategies to alleviate these emotions and escape from thoughts of suicide (Paxton & Diggens, 1997; Wildes et al., 2010). Although ED behaviors primarily serve the purpose of temporarily calming concerns about weight and shape (Fox et al., 2019), individuals frequently report engaging in ED behaviors in order to relieve negative affect (Anestis et al., 2007; Berg et al., 2015). Thus, it follows that individuals who think about suicide may turn to ED behaviors as additional coping mechanisms. In fact, one such study found that in a sample of adult patients of EDs, suicidal ideation predicted global ED symptoms at a one-week follow-up (Ortiz & Smith, 2020). Relatedly, Trujillo and colleagues (2019) found that perceived burdensomeness, a facet of suicide desire as defined by the Interpersonal-Psychological Theory of Suicide (IPTS; Joiner, 2005), predicted an increase in ED symptoms over an 8-week period, but ED symptoms did not predict changes in perceived burdensomeness. Further, Forrest and colleagues (2015) found that in a large, nationally representative sample of adults, the onset of suicidal ideation, plans, and attempts generally preceded the onset of binge-eating disorder. However, this pattern was reversed for adolescents; binge-eating disorder onset most often preceded the occurrence of suicidal ideation, plans, and attempts (Forrest et al., 2015). Despite preliminary evidence supporting bidirectional relations between suicidal ideation and ED symptoms, additional work is needed to replicate and extend these findings, particularly in adolescents.
Few studies, especially in adolescents, have comprehensively tested for both bidirectional relations between suicidal ideation and EDs, as well as possible shared risk factors. The current study tested one such shared risk factors for both conditions—interoceptive deficits (Smith et al., 2018b). Interoception, or the ability to accurately and effectively perceive the physiological condition of the body (Craig, 2002), has been implicated in both suicidal thoughts and behaviors (Forrest et al., 2015; Rogers et al., 2018) and ED symptoms (Dodd et al., 2017; Khalsa et al., 2015). The ability to connect to and interpret bodily sensations is crucial to maintaining healthy emotional awareness and regulating emotions (Critchley & Garfinkel, 2017; Zamariola et al., 2019). By contrast, interoceptive deficits have been conceptualized as leading to disconnect from the body (Ainley & Tsakiris, 2013; Brausch & Muehlenkamp, 2014). This bodily disconnect is thought to facilitate the ability to harm the body, including both direct (e.g., suicide attempts) and indirect (e.g., ED behaviors) forms of self-injury, as it is easier to harm an object that is separate from the self (Ainley & Tsakiris, 2013; Brausch & Muehlenkamp, 2014; Muehlenkamp, 2012). Specifically, facets of interoceptive awareness such as a decreased ability to attend to and regulate bodily sensations compounded with poor trust in bodily sensations may create significant distress and thus increase suicidal ideation (Duffy et al., 2020; Duffy et al., in press; Hielscher & Zopf, 2020). Supporting this, several recent studies have demonstrated decreased interoceptive awareness in those that have thought about suicide, made a plan, and attempted suicide in adults (Forrest et al., 2015; Rogers et al., 2018). Furthermore, Smith and colleagues (2019a) found that interoceptive deficits were more pronounced in military members who had thought about suicide compared to those with no suicide history. Related to the current study, multiple studies using adult samples with elevated ED symptoms have found more severe interoceptive deficits are associated with greater suicide risk (Dodd et al., 2017; Duffy et al., 2020; Smith et al., 2018a). However, as the majority of the research on interoception and suicidal ideation is cross-sectional, future work may benefit from including interoceptive deficits as a longitudinal predictor.
Similarly, individuals with EDs commonly report greater interoceptive deficits compared to healthy controls and interoceptive deficits are theorized to facilitate the ability to engage in ED symptoms (Jenkinson et al., 2018; Pollatos et al., 2008). Cross-sectionally, ED symptom severity in adults as assessed by the Eating Disorder Examination Questionnaire (Fairburn & Beglin, 1994) is associated with deficits in multiple facets of interoception (Brown et al., 2018). Adults with elevated ED symptoms often report a diminished ability to detect gastrointestinal sensations such as hunger and fullness (Tylka, 2006). Several other studies have found that ED symptom severity is negatively associated with interoceptive awareness (Jenkinson et al., 2018; Merwin et al., 2010). These findings are supported by neuroimaging studies showing altered functioning in brain areas responsible for recognizing and integrating interoceptive signals both in patients with anorexia nervosa (Kerr et al., 2016; Strigo et al., 2013). Thus, interoceptive deficits may allow individuals to engage in ED behaviors more readily.
Although previous work has identified interoception as a trait-like construct, there is some evidence to suggest that interoception may fluctuate over the course of minutes to several weeks (Wittkamp et al., 2018). For example, participants that completed body scan and breathing mediations reported improved interoceptive awareness after completing these meditations (Kok & Singer, 2017). In addition, Schulz and colleagues (2013) examined whether or not stress might impact objectively assessed interoceptive awareness using the heartbeat discrimination task, in which participants are instructed to determine whether external stimuli (ex., flashing lights, tones, tactile stimuli) are synchronized with their own heartbeat or delayed. Participants completed the heartbeat discrimination task twice and were subjected to either a cold-pressor stress task or a control task in between the two. In the cold-pressor stress condition, participants were asked to submerge their right hand in cold water for three minutes without removing it. Participants that completed the cold-pressor task reported decreased interoceptive accuracy on the heartbeat discrimination task compared to those that completed the control task (i.e,, submerging their right hand in warm water for 3 minutes). Thus, it appears that interoceptive deficits may be responsive to external stimuli and in particular, stress.
Present Study
Overall, it is clear that a robust association between ED symptoms and suicidal ideation exists, and that interoceptive deficits may facilitate and maintain both conditions. However, there is a significant need to better understand exactly how these conditions are related and how they may influence each other over time, particularly over shorter time frames. Furthermore, as both ED symptoms and suicidal ideation often begin and are common in adolescence (Mustelin et al., 2016; Rueter & Kwon, 2005; Stice et al., 1998), understanding their co-occurrence in this developmental period is crucial. Thus, the current study tested if ED symptoms, suicidal ideation, and interoceptive deficits related to each other over the course of a year in a sample of adolescent students using the following time points: baseline, 6-month follow-up, and 12-month follow-up. Based on the existing cross-sectional literature on these variables, we expected to find a significant correlation between suicidal ideation severity, ED symptom severity, and interoceptive deficits at each time point across the duration of the study. Furthermore, given the mixed findings on the directionality of ED symptoms and suicidal ideation, we hypothesized that ED symptoms and suicidal ideation would predict each other bidirectionally over the course of the study. Finally, given research supporting interoceptive deficits as a risk factor for both ED symptoms and suicidality, we hypothesized that interoceptive deficits would predict both follow-up ED symptoms and follow-up suicidal ideation at each time point.
Method
The current study is a secondary data analysis of data collected as a part of a larger longitudinal study examining the temporal relations between nonsuicidal self-injury and suicidal thoughts and behaviors in adolescents. All study procedures received approval from the University’s Institutional Review Board.
Participants
Data were collected from community adolescents (N=436) enrolled in local middle (n=233) and high schools (n=203) in the Southeastern United States. The sample was primarily female (52.8%), Caucasian/White (85.4%), and heterosexual (88.5%) with a mean age of 13.19 (SD=1.089). No inclusion criteria were required in order to participate in the study beyond parental consent and participant assent. At the 6-month follow-up, 389 adolescents completed the protocol, for a retention rate of 85.3%. At the 12-month follow-up, 387 adolescents completed the protocol, for a retention rate of 84.9%. Attrition was partly due to adolescents being out of school on the assessment days or moving out of the school district between assessments.
Procedure
Local middle and high schools were contacted by the PI (AB) to gain consent to conduct research within their school. After determining school consent, all 7th grade students from two middle schools (~700 students) and all 9th grade students at two high schools (~476 students) were sent home with parental consent forms. Approximately 42.7% of the 7th grade students (n=299, 257 positive consent, 42 negative) and 47.5% of the 9th grade students (n=226, 221 positive consent, 5 negative) returned signed consent forms. Those who returned signed, positive parental consent forms were enrolled in the study. Of those who returned positively signed parental consent forms (n=478), 91.2% of the students participated in the study (n=436). These adolescents also signed a written assent form at the time of data collection. During separate school visits, researchers administered the study protocol to adolescents in a group setting. Self-report measures were completed on paper and pencil in a large space within each school (e.g., a school cafeteria), with adolescents spaced at least two seats apart to ensure participant privacy. The entire protocol took approximately 30–45 minutes to complete and participants were compensated $10 at each assessment, for a possible total of $30 for those who completed each of the three assessments. Baseline data were collected at the initial school visit and proceeded by two follow-up visits that were each spaced six months apart (6-month and 12-month).
Data were screened for risk by either the PhD-level researcher (AB) or a master’s level graduate student. Immediately prior to data collection, participants were informed that their responses would be screened and that they may be referred to speak with the school counselor if their responses indicated that they may be a risk. Critical items on several measures indicating either elevated depression or suicide risk were identified prior to data collection. Participants who were deemed at risk on any of the measures were disclosed to the school counselor who followed up with them later that same day. An intervention record was completed for each participant to classify risk severity (i.e., low, moderate, or high) and make recommendations to the school counselor for follow-up (ranging from monitor/review to immediate interview/follow-up). Completed records were left with the school counselors at each school to facilitate follow-up. At baseline, 6.4% (n=28) of participants were referred. At the 6-month follow-up, 5.6% (n=21) were referred. At the 12-month follow-up, 5.2% (n=19) were referred. School counselors followed established policies at their respective school for working with at-risk students according to their determined risk level.
Measures
All measures included were collected at baseline and both follow-ups.
ED symptoms.
The Eating Disorder Inventory (EDI-3; Garner, 2004) was used to assess ED symptom severity. The EDI-3 is a 90-item instrument assessing a broad range of ED-related behaviors and cognitions and includes items such as I eat when I am upset and I am terrified of gaining weight. It includes 12 subscales; however, only the drive for thinness, bulimia, and body dissatisfaction, which together make up an ED composite score, were used to provide an index of ED symptom severity. Items are rated on a 6-point Likert scale from 1 (Never) to 6 (Always). Before scoring, positively-valenced items are reverse-coded and all item response options are recoded so that the two response options in the asymptomatic direction are coded as 0 and the four response options in the symptomatic direction are coded as 1–4 to increase the variance of item scores (Clausen et al., 2011; Garner, 2004). Subscale scores are obtained by averaging responses to all completed items with higher scores indicating greater pathology. An ED composite score is then obtained by averaging the drive for thinness, bulimia, and body dissatisfaction subscale scores. The EDI-3 and the ED composite subscale have demonstrated strong validity and reliability (α=0.87–0.93) in a community sample (Clausen et al., 2011) and good to strong reliability in the current sample across all three time points (α=0.79–0.91).
Interoceptive deficits.
Interoceptive deficits were assessed using the interoceptive deficits subscale of the EDI-3 (Garner, 2004). This subscale assesses deficits in both emotional and physiological signals and consists of ten items such as I don’t know what’s going on inside me and I get confused as to whether or not I am hungry. The interoceptive deficits subscale has demonstrated strong validity and reliability in a community sample (α=0.85) and good reliability in the current study across all three time points (α=0.81–0.88). Although interoceptive deficits and ED symptoms were assessed using the same scale, these scales have been shown to load onto different factors in several validation studies in both community and clinical samples (Brookings et al., in press; Clausen et al., 2011).
Suicidal ideation.
Suicidal ideation severity was assessed using the Suicide Ideation Questionnaire-Junior (SIQ-JR; Reynolds, 1987). The SIQ-JR is a 15-item instrument assessing the frequency of various thoughts about death and suicide over the past month. Items are rated on a 7-point Likert scale from 0 (I never had this thought) to 6 (Almost every day). A total score is obtained by summing responses for all completed items with higher scores indicating more severe and frequent suicidal ideation (range=0–90). In the current sample, 2.8% (n=15) scored at or above the clinical cut-off score (31) at baseline, 3.6% (n=15) at 6-month follow-up, and 3.0% (n=12) at 12-month follow-up. The SIQ-JR has demonstrated strong validity and reliability (α=0.93) in validation studies (Reynolds, 1987) as well as in the current sample across all three timepoints (α=0.93–0.94).
Analytic Strategy
Data were analyzed using SPSS version 24.0 and Mplus version 7.3 (Muthén & Muthén, 1998–2012).
Missing data.
Full-information maximum likelihood (FIML) was used in Mplus to handle missing data as data were missing completely at random at each time point (Little’s missing completely at random tests: χ2 = .78–2.70, p = .26-.94). Pairwise deletion was used to present and examine the bivariate correlations between study variables, see Table 1.
Table 1.
Correlations and descriptive statistics for suicidal ideation, interoceptive deficits, and eating disorder symptom variables
| N=436 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Time 1 SI | – | ||||||||
| 2. Time 1 ID | .59** | – | |||||||
| 3. Time 1 ED | .44** | .52* | – | ||||||
| 4. Time 2 SI | .43** | .42** | .36** | _ | |||||
| 5. Time 2 ID | .45** | .65** | .49** | .48** | – | ||||
| 6. Time 2 ED | .31** | .47** | .68** | .40** | .66** | – | |||
| 7. Time 3 SI | .40** | .40* | .38** | .56** | .54** | .48* | – | ||
| 8. Time 3 ID | .33* | .55** | .43* | .40** | .71** | .54** | .60* | – | |
| 9. Time 3 ED | .24** | .43* | .63** | .37** | .56** | .80** | .46** | .62** | – |
|
| |||||||||
| Mean | 4.85 | 4.43 | 12.64 | 4.98 | 4.41 | 17.05 | 4.23 | 3.91 | 14.75 |
| Standard deviation | 9.96 | 5.54 | 9.67 | 10.74 | 6.19 | 16.16 | 9.46 | 6.03 | 15.18 |
| Skew | 3.57 | 1.70 | .79 | 3.67 | 2.08 | 1.42 | 4.32 | 2.10 | 1.51 |
| Kurtosis | 15.63 | 2.66 | .39 | 15.66 | 4.42 | 2.21 | 25.20 | 5.48 | 2.14 |
| Missing (%) | 5.50 | 5.3 | 5.0 | 15.6 | 14.7 | 14.7 | 18.4 | 18.9 | 18.6 |
Note.
p<.05
p < .01;
p < .001; SI = suicidal ideation; ID = interoceptive deficits; ED = eating disorder composite variable
Data screening.
The interoceptive deficits and ED composite variables had acceptable levels of skew > |2.5|. Log transformation was applied to the suicidal ideation variables to handle skew.
Path analyses.
When we conducted a power analysis using an anticipated effect size of .3, setting the statistical power level to .8, and entering our number of variables, the recommended minimum sample size for model structure was 400 participants (Soper, 2020). Thus, our sample size of 436 participants meets recommendations for testing our hypothesized model described below. Three autoregressive paths were considered: (1) ED symptoms at one time point (T) predicting ED symptoms at the next time point (T + 1), (2) interoceptive deficits at T predicting interoceptive deficits at T+1, and (3) suicidal ideation at T predicting suicidal ideation at T+1. The following cross-lagged paths were considered: (1) ED symptoms at T predicting interoceptive deficits at T + 1 (2) ED symptoms at T predicting suicidal ideation at T + 1, (3) interoceptive deficits at T predicting ED symptoms at T + 1, (4) interoceptive deficits at T predicting suicidal ideation at T + 1 (5) suicidal ideation at T predicting ED symptoms at T + 1, and (6) suicidal ideation at T predicting interoceptive deficits at T + 1. Finally, our variables were allowed to covary with each other at each time point. See Figure 1 for full model. The relative strengths of the relationships were determined through comparison of standardized betas. Model fit was assessed using comparative fit index (CFI; Bentler, 1990), root mean square error of approximation (RMSEA; Browne & Cudeck, 1993), and standardized root mean square residual (SRMR; Hu & Bentler, 1999). Effect sizes for each path are reported in Table 2.
Figure 1. Significant standardized path coefficients for autoregressive cross-lag model tested.
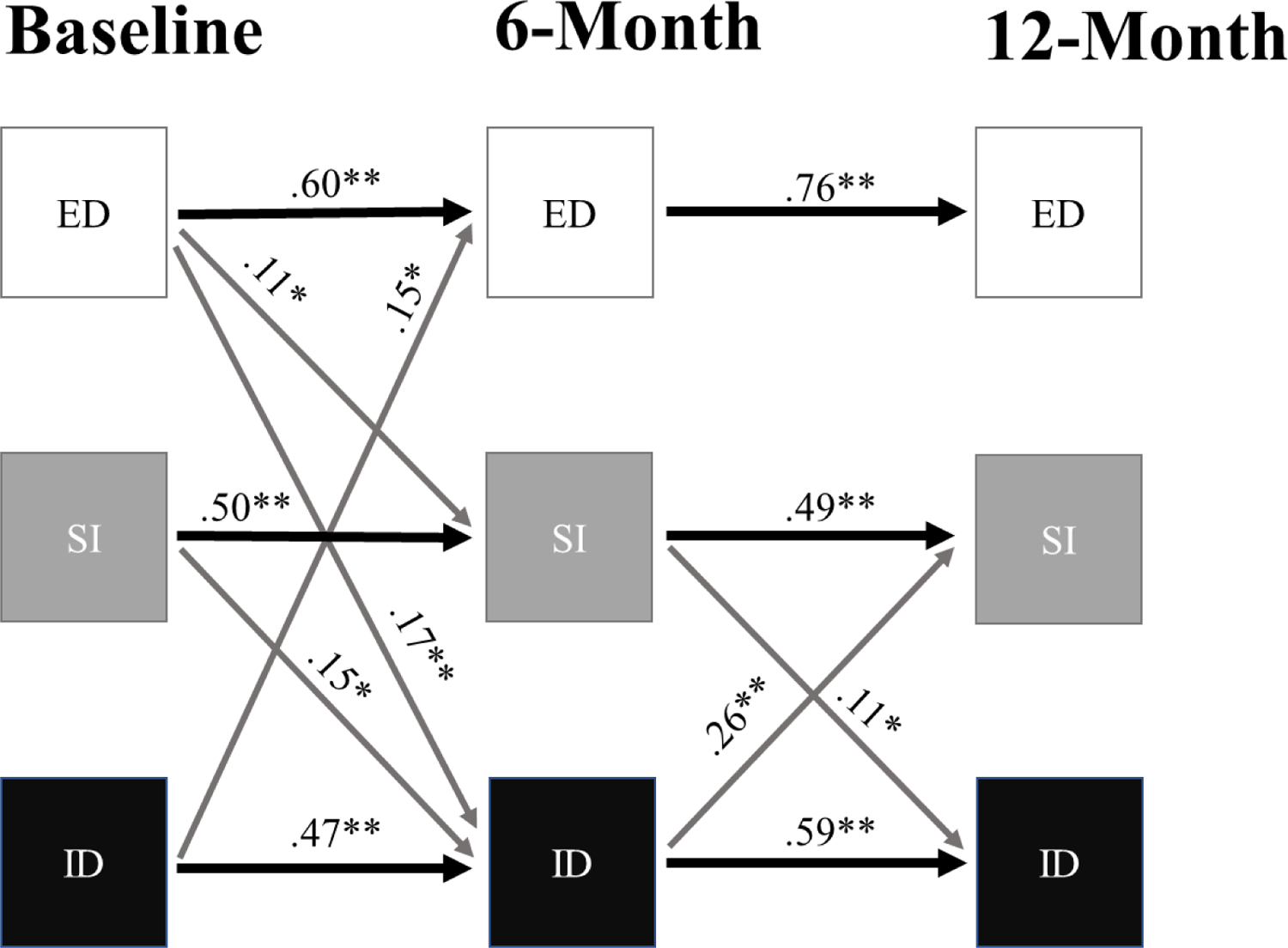
Note. * p<.05; ** p < .01; black lines = significant autoregressive paths; gray lines = significant cross-lagged paths; ED = Eating disorder symptoms SI = suicidal ideation; ID = Interoceptive deficits; although not illustrated for ease of interpretation, variables were permitted to covary at each time point.
Table 2.
Values and interpretations of effect sizes for the model pathways when controlling for the other variables at the same time point
| Pathway | f 2 | Relative size |
|---|---|---|
| Time 1 ID → Time 2 ED | 0.02 | Small |
| Time 1 ID → Time 2 ID | 0.15 | Medium |
| Time 1 SI → Time 2 ID | 0.02 | Small |
| Time 1 ED → Time 2 ED | 0.32 | Medium |
| Time 1 ID → Time 2 ED | 0.02 | Small |
| Time 1 SI → Time 2 ED | 0.00 | None |
| Time 1 ED → Time 2 SI | 0.02 | Small |
| Time 1 ID → Time 2 SI | 0.01 | None |
| Time 1 SI → Time 2 SI | 0.15 | Small |
| Time 2 ED → Time 3 ID | 0.01 | None |
| Time 2 ID → Time 3 ID | 0.23 | Medium |
| Time 2 SI → Time 3 ID | 0.02 | Small |
| Time 2 ED → Time 3 ED | 0.46 | Large |
| Time 2 ID → Time 3 ED | 0.00 | None |
| Time 2 SI → Time 3 ED | 0.00 | None |
| Time 2 ED → Time 3 SI | 0.01 | None |
| Time 2 ID → Time 3 SI | 0.03 | Small |
| Time 2 SI → Time 3 SI | 0.11 | Small |
Note. SI = suicidal ideation; ID = interoceptive deficits; ED = eating disorder composite variable
Results
Hypothesis 1: ED Symptoms, Interoceptive Deficits and Suicidal Ideation will relate to each other at each Time Point
Correlations between variables at each time point ranged in strength from .31–.80 and were all statistically significant (see Table 1).
Hypothesis 2: ED Symptoms and Suicidal Ideation will predict each other at each Time Point
The second aim was to investigate the directionality of the longitudinal relations between suicidal ideation and ED symptoms. To test this hypothesis and our third hypothesis, we ran an autoregressive cross-lagged model to analyze how suicidal ideation, interoceptive deficits, and ED symptomatology affect each other over the course of the 12-month study period (see Figure 1). Our CFI value was above .95 (CFI = .96) and the SRMR value was below .05 (SRMR = .04) while RMSEA = .08; these estimates indicate our model fit ranged from acceptable to excellent.
Partially supporting our hypothesis, we found a significant cross-lagged path from baseline ED symptoms predicting suicidal ideation severity at 6-month follow-up, when controlling for baseline suicidal ideation (B = 0.11, S.E. = .05, p = .04). We did not see an instance of suicidal ideation predicting ED symptoms across time points.
Hypothesis 3: Interoceptive Deficits will predict ED Symptoms and Suicidal Ideation at each Time Point
We found partial support for our hypothesis. Specially, we found that baseline interoceptive deficits significantly predicted 6-month follow-up ED symptoms, when controlling for baseline ED symptoms (B = 0.15, S.E. = .07, p = .03). Additionally, we found 6-month follow-up interoceptive deficits significantly predicted 12-month follow-up suicidal ideation symptoms, when controlling for suicidal ideation at time of 6-month follow-up (B = 0.26, S.E. = .07, p < .01).
Discussion
While EDs and suicidality are robustly associated with each other, longitudinal research examining the relationship between EDs and suicidal ideation is limited. Given that prior research has identified interoceptive deficits as a risk factor for EDs and suicidal ideation, the current study examined how interoceptive deficits, ED symptoms, and suicidal ideation related to each other at six-month intervals over the course of a year within a sample of adolescent students. Supporting our first hypothesis, ED symptoms, suicidal ideation, and interoceptive deficits remained correlated with each other at each time point over the duration of the study. This finding, along with previous research that has also found a robust association between these variables (Forrest et al., 2015; Jenkinson et al., 2018; Rogers et al., 2018), underscores the importance of assessing ED symptoms and interoceptive deficits in those endorsing thoughts about suicide and vice versa. Unfortunately, these practices are not routinely occurring in clinical settings. For instance, research found that providers who worked with ED patients screened for suicidal thoughts and behaviors in less than 50% of all cases (Peebles et al., 2010).
Our results only partially supported our second hypothesis; while we found an instance where ED symptoms predicted suicidal ideation at the following time point, we did not find that suicidal ideation predicted ED symptoms. Thus, we were unable to replicate some previous work that found that suicidal ideation predicted ED symptoms in a sample of adult ED patients (Ortiz & Smith, 2020). Given this prior work was conducted using adults that were diagnosed with EDs, it appears that the relationship between ED and suicidal ideation may differ in a community sample of adolescents. However, our findings do align with meta-analytic results that indicate EDs predict other forms of suicidality (i.e. suicide attempts), albeit weakly (Smith et al., 2018b). Given that suicidal ideation is a risk factor for future suicidal behavior (Franklin et al., 2017), these results further support the literature that engaging in ED behaviors may increase risk for all forms of suicidality (i.e., suicidal ideation, attempts, and death). Research has shown that one-third of adolescents with suicide ideation will transition to making a plan and/or a suicide attempt, and 60% of those who transition to an attempt will do so in the first year after onset of suicidal thoughts (Glenn & Nock, 2014; Nock et al., 2013). Thus, it is important to continue exploring which factors may contribute to this increase risk for suicidal ideation and/or suicide attempts. However, given that our model did not include suicide attempts as a variable, these conclusions should be considered and interpreted with appropriate caution. In addition, we only found that ED symptoms at baseline predicted suicidal ideation at the 6-month follow-up. This pattern was not observed between ED symptoms at 6-months and suicidal ideation at 12-months. Given the lack of consistency observed in this relationship, these results should be interpreted with caution and further study of longitudinal relationship between ED symptoms and suicidal ideation is warranted. As Ortiz and Smith (2020) found this relationship to be present between one week follow-ups, future work may benefit from examining the longitudinal relationship across varying length follow-ups.
Our third hypothesis tested whether interoceptive deficits predicted suicidal ideation and ED symptoms at the following time point. We found two significant pathways in our model in support of this. First, baseline interoceptive deficits predicted ED symptoms at the following time point. This finding supports the notion that difficulty interpreting bodily signals, such as hunger and satiety cues, and/or deficits in identifying one’s emotional state, increases the risk for engaging in disordered eating behaviors (Jenkinson et al., 2018). Future work should determine which facets of interoceptive deficits may lead to greater disordered eating risk. For example, Brown et al. (2018), found that individuals with more severe ED symptoms were more distracted from uncomfortable bodily sensations, had a lesser ability to regulate distress caused by uncomfortable bodily sensations, and trusted their bodies less. Second, we found interoceptive deficits at 6-month follow-up predicted suicidal ideation at 12-month follow-up. Taking these results together along with previous findings, it appears that interoceptive deficits are a significant predictor of maladaptive thoughts and behaviors in adolescence, as well as in adulthood (e.g. Jenkinson et al., 2018).
It is also noteworthy that several hypothesized pathways within our model were not significant or differed from predictions. Instead of finding a bidirectional relationship between ED symptoms and suicidal ideation, we instead found a bidirectional relationship between interoceptive deficits and ED symptoms between baseline and 6-month follow-up, as well as a bidirectional relationship between interoceptive deficits and suicidal ideation between the 6- and 12-month follow-up time points. As previously discussed, these bidirectional pathways may demonstrate a cyclical relationship between interoceptive deficits and ED symptoms and suicidal ideation. It is well-established that interoceptive deficits increase risk for ED symptoms and suicidal ideation by removing a barrier to engaging in harmful and painful behaviors (Ainley & Tsakiris, 2013; Brausch & Muehlenkamp, 2014; Muehlenkamp, 2012), but less work has examined how ED symptoms and suicidal ideation may negatively impact interoception. Some research has shown that prolonged engagement in ED symptoms reduces one’s ability to notice and accurately identify interoceptive signals (Kerr et al., 2016). Cardiac interoception (i.e., the ability to accurately and precisely discern cardiac sensations) has been shown to react negatively to experimentally induced stress (Shulz et al., 2013). As suicidal thoughts are inherently stressful, they may increase stress and thereby reduce one’s interoceptive awareness. Therefore, greater interoceptive deficits brought on by ED symptoms and suicidal ideation may further increase risk for these behaviors in the future. Taken together, these findings illustrate a very dynamic relationship between interoceptive deficits, disordered eating, and suicidal ideation; given how interconnected these variables appear to be, intervening upon one of these conditions may also reduce the other conditions (Preyde et al., 2016). Indeed, Price and colleagues (2019) found interoceptive awareness training through Mindful Awareness in Body-oriented Therapy reduced depressive symptoms and maladaptive behaviors related substance use. Thus, it may be that a similar approach could also directly or indirectly lower disordered eating behaviors.
Relatedly, it is also important to consider why several of our predicted pathways were non-significant. One possibility is that symptom variables were too strongly related to each other across time points to leave enough predictive power for the other symptom variables. Indeed, our ED variables did become more strongly correlated across time, which may help explain why ED symptoms at 6-month follow-up was the only variable that predicted ED symptoms at 12-month follow-up. This increase in association during the course of our study may indicate that some symptoms reinforce each other over time. Another possibility is that other variables may better explain the relation between these variables. Future work should consider including measures of emotion dysregulation or negative affect into future models as prior work has found these to relate to suicidal ideation, EDs, and interoceptive deficits (e.g., Muehlenkamp et al., 2012; Preyde et al., 2016; Price et al., 2019).
Overall, this study has important clinical implications. First, interoceptive deficits were found to be a risk factor for both suicidal ideation and ED symptoms. This indicates that interoceptive deficits may be an important target in prevention and treatment programs (Fischer et al., 2017; Smith et al., in prep). This notion is further supported given that prior work has found interoceptive deficits to be a risk factor in adults who experience suicidality or have been diagnosed with an ED (e.g., Duffy et al., in press). Targeting interoception through treatment and prevention in early adolescence, prior to the average age of onset for ED symptoms and suicidal ideation (Mustelin et al., 2016; Rueter & Kwon, 2005; Stice et al., 1998), may prevent the emergence of some of these maladaptive behaviors. School-based mental health interventions including mindfulness skills (Linehan, 2014) may be effective at teaching adolescent individuals how to be better attuned with their internal processes to help improve eating behaviors and emotion regulation. Results also highlight the need to evaluate adolescents for suicidal ideation and ED symptoms regularly beginning in early adolescence as these behaviors can become more difficult treat without early intervention.
Strengths, Limitations, and Future Directions
The present findings should be interpreted in conjunction with the study’s strengths and limitations. With respect to strengths, this study applied longitudinal methodology to a relatively large sample and had shorter follow-up points compared to previous research (e.g. Crow et al., 2008a; Rodríguez-Cano et al., 2006). This study also benefitted from the use of a continuous measure of suicidal ideation as compared to a dichotomous variable that has been used in previous studies (e.g., Bodell et al., 2018). The use of a continuous variable allowed us to examine ED symptoms and interoceptive deficits in relation to suicidal ideation severity as opposed to simply evaluating if ideation had occurred for the participants.
Despite these strengths, the current study had several limitations. Although this study was the first to examine the cross-lagged paths between ED symptoms, suicidal ideation, and interoceptive deficits in adolescents, we did not test how specific ED symptoms may relate to interoceptive deficits and suicidal ideation. The sample was also fairly homogenous in terms of race, ethnicity, and sexual orientation. Thus, our results may not generalize to non-White populations or sexual minorities as these populations often report higher rates of ED symptoms and suicidal ideation (Calzo et al., 2017; Chu et al., 2010; Rodgers et al., 2018). Additionally, we used a community sample of individuals who were not diagnosed with an ED. Although the use of a community sample provides a picture of how ED symptoms, interoceptive deficits, and suicidal ideation may influence one another in the general population, this study should be replicated within a sample of individuals diagnosed with EDs. Lastly, our measure of interoceptive deficits included physiological items more relevant to ED symptoms than general psychopathology, such as I get confused as to whether or not I am hungry and did not include other dimensions of interoception that may be important in the development and maintenance of suicidal ideation (e.g., body trust, worrying about physiological sensations; Garner, 2004; Rogers et al., 2018). Future work may benefit from using a scale that assesses multiple facets of interoceptive awareness such as the Multidimensional Assessment of Interoceptive Awareness (Mehling et al., 2018).
Along with the previously mentioned suggestions for future studies, below we highlight additional directions for research. First, future work should consider including other theoretically-derived constructs. For example, interoceptive deficits are associated with fearlessness about death, a construct theorized by the IPTS to be essential for an individual to move from suicidal thought to behavior (Dodd et al., 2017). Furthermore, perceived burdensomeness may also be important to include as a mediator in future models as is an established contributor to suicidal desire as outlined by the IPTS (Joiner, 2005). Furthermore, Trujillo and colleagues (2019) found perceived burdensomeness predicted ED symptoms over an 8-week period. Second, using shorter follow-up time points, such as through daily ecological momentary assessments, may provide greater insight into these relationships as ED symptoms and suicidal ideation are known to fluctuate over days and weeks (Bryan & Rudd, 2016; Smyth et al., 2007).
In sum, our results indicate that interoceptive deficits can predict and be predicted by ED symptoms and suicidal ideation. Further, our work suggests that ED symptoms can predict the severity of suicidal ideation within adolescents. Clinically, these results highlight the need for early and regular assessment of suicidal ideation and ED symptoms in adolescents and underscore the need for targeted interventions by improving interoception.
Highlights.
Interoceptive deficits predicted eating disorder symptoms at follow-up
Interoceptive deficits predicted suicidal ideation at follow-up
Eating disorder symptoms predicted suicidal ideation at follow-up
Interoceptive deficits mediated the eating disorder to suicidal ideation pathway
Funding:
This project was supported by the National Institute of General Medical Sciences of the National Institutes of Health under award number P20GM103436. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Shelby N. Ortiz reports support from the National Science Foundation Graduate Research Fellowship Program during the conduct of the study. Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the National Science Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: None.
References
- Ainley V Tsakiris M (2013). Body conscious? Interoceptive awareness, measured by heartbeat perception, is negatively correlated with self-objectification. PLoS ONE, 8, e55568. 10.1371/journal.pone.0055568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anestis MD, & Joiner TE (2011). Examining the role of emotion in suicidality: Negative urgency as an amplifier of the relationship between components of the interpersonal–psychological theory of suicidal behavior and lifetime number of suicide attempts. Journal of Affective Disorders, 129, 261–269. 10.1016/j.jad.2010.08.006 [DOI] [PubMed] [Google Scholar]
- Anestis MD, Selby EA, Fink EL, & Joiner TE (2007). The multifaceted role of distress tolerance in dysregulated eating behaviors. International Journal of Eating Disorders, 40, 718–726. 10.1002/eat.20471 [DOI] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. 10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Berg KC, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA, & Peterson CB (2015). Negative affect prior to and following overeating-only, loss of control eating-only, and binge eating episodes in obese adults. International Journal of Eating Disorders, 48, 641–653. 10.1002/eat.22401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodell LP, Cheng Y, & Wildes JE (2018). Psychological impairment as a predictor of suicide ideation in individuals with anorexia nervosa. Suicide and Life-Threatening Behavior, 49, 520–528. 10.1111/sltb.12459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boomsma A, & Hoogland JJ (2001). The robustness of LISREL modeling revisited. Structural equation models: Present and future. A Festschrift in Honor of Karl Jöreskog, 2, 139–168. [Google Scholar]
- Brausch AM, & Muehlenkamp JJ (2014). Experience of the body. In Claes L & Muehlenkamp JJ (Eds.), Non-suicidal self-injury in eating disorders: Advancements in etiology and treatment. Springer. 10.1007/978-3-642-40107-7_14 [DOI] [Google Scholar]
- Brookings JB, Jackson DL, & Garner DM (in press). A bifactor and item response theory analysis of the Eating Disorder Inventory-3. Journal of Psychopathology and Behavioral Assessment. 10.1007/s10862-020-09827-2 [DOI]
- Brown TA, Berner LA, Jones MD, Reilly EE, Cusack A, Anderson LK, Kaye WH, & Wierenga CE (2018). Psychometric evaluation and norms for the Multidimensional Assessment of Interceptive Awareness (MAIA) in a clinical eating disorders sample. European Eating Disorders Review, 25, 411–416. 10.1002/erv.2532 [DOI] [PubMed] [Google Scholar]
- Browne MW, & Cudeck R (1993). Alternative ways of assessing model fit. Sage Focus Editions, 154, 136–136. 10.1177/0049124192021002005 [DOI] [Google Scholar]
- Bryan CJ, & Rudd MD (2016). The importance of temporal dynamics in the transition from suicidal thought to behavior. Clinical Psychology: Science and Practice, 23, 21–25. 10.1111/cpsp.12135 [DOI] [Google Scholar]
- Bunderla T, & Kumperščak HG (2015). Altered pain perception in self-injurious behavior and the association of psychological elements with pain perception measures: A systematic review. Psychiatria Danubina, 27, 346–354. [PubMed] [Google Scholar]
- Calzo JP, Blashill AJ, Brown TA, Argenal RL (2017). Eating disorders and disordered weight and shape control behaviors in sexual minority populations. Current Psychiatry Reports, 19, 49. 10.1007/s11920-017-0801-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu JP, Goldblum P, Floyd R, & Bongar B (2010). The cultural theory and model of suicide. Applied and Preventive Psychology, 14, 25–40. 10.1016/j.appsy.2011.11.001 [DOI] [Google Scholar]
- Clausen L, Rosenvinge JH, Friborg O, & Rokkedal K (2011). Validating the Eating Disorder Inventory-3 (EDI-3): A comparison between 561 female eating disorders patients and 878 females from the general population. Journal of Psychopathology and Behavioral Assessement, 33, 101–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig AD (2002). How do you feel? Interoception: The sense of the physiological condition of the body. Nature Reviews: Neuroscience, 10, 59–70. 10.1038/nrn894 [DOI] [PubMed] [Google Scholar]
- Critchley HD, & Garfinkel SN (2017). Interoception and emotion. Current Opinion in Psychology, 17, 7–14. [DOI] [PubMed] [Google Scholar]
- Crow S, Eisenberg ME, Story M, & Neumark-Sztainer D (2008a). Are body dissatisfaction, eating disturbance and body mass index predictors of suicidal behavior in adolescents? A longitudinal study. Journal of Consulting and Clinical Psychology, 76, 887–892. 10.1037/a0012783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crow S, Eisenberg ME, Story M, & Neumark-Sztainer D (2008b). Suicidal behavior in adolescents: Relationships to weight status, weight control behaviors, and body dissatisfaction. International Journal of Eating Disorders, 41, 82–87. 10.1002/eat.20466 [DOI] [PubMed] [Google Scholar]
- Deville DC, Kuplicki R, Stewart JL, Tulsa 1000 Investigators, Paulus MP, & Khalsa SS (2020). Diminished responses to bodily threat and blunted interoception in suicide attempters. eLife, 9, e51593. 10.7554/eLife.51593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhingra K, Boduszek D, & O’Connor RC (2015). Differentiating suicide attempters from suicide ideators using the integrated motivational-volitional model of suicidal behavior. Journal of Affective Disorders, 186, 211–218. 10.1016/j.jad.2015.07.007 [DOI] [PubMed] [Google Scholar]
- Dodd DR, Smith AR, Forrest LN Witte TK, Bodell L, Bartlett M, Siegfried N, Goodwin N (2017). Interoceptive deficits, nonsuicidal self-injury, and suicide attempts among women with eating disorders. Suicide and Life-Threatening Behavior, 48, 438–448. 10.1111/sltb.12383 [DOI] [PubMed] [Google Scholar]
- Duffy ME, Lieberman A, Siegfried N, Henretty JR, Bass G, Cox SA, & Joiner TE (2020). Body trust, agitation, and suicidal ideation in a clinical eating disorder sample. International Journal of Eating Disorders, 53, 1746–1750. 10.1002/eat.23352 [DOI] [PubMed] [Google Scholar]
- Duffy ME, Rogers ML, Gallyer AJ, & Joiner TE (in press). Body trust and agitation: Pathways to suicidal thoughts and behaviors. Archives of Suicide Research. 10.1080/13811118.2019.1592039 [DOI] [PubMed]
- Eichen DM, Kass AE, Fitzsimmons-Craft EE, Gibbs E, Trockel M Taylor CB, & Wilfley DE (2016). Non-suicidal self-injury and suicidal ideation in relation to eating and general psychopathology among college-age women. Psychiatry Research, 235, 77–82. 10.1016/j.psychres.2015.11.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, & Beglin SJ (1994). Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders, 16, 363–370. [DOI] [PubMed] [Google Scholar]
- Fischer D, Messner M, & Pollatos O (2017). Improvement of interoceptive processes after an 8-week body scan intervention. Frontiers in Human Neuroscience, 11, 452. 10.3389/fnhum.2017.00452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest LN, Smith AR, White RD, & Joiner TE (2015). (Dis)connected: An examination of interoception in individuals with suicidality. Journal of Abnormal Psychology, 124, 754–763. 10.1037/abn0000074 [DOI] [PubMed] [Google Scholar]
- Forrest LN, Zuromski KL, Dodd DR, & Smith AR (2017). Suicidality in adolescents and adults with binge-eating disorder: Results from the national comorbidity survey replication and adolescent supplement. International Journal of Eating Disorders, 50, 40–49. 10.1002/eat.22582 [DOI] [PubMed] [Google Scholar]
- Fox KR, Wang SB, Boccagno C, Haynos AF, Kleiman E, & Hooley JM (2019). Comparing self-harming intentions underlying eating disordered behaviors and NSSI: Evidence that distinctions are less clear than assumed. International Journal of Eating Disorders, 52, 564–575. 10.1002/eat.23041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franko DL, & Keel PK (2006). Suicidality in eating disorders: Occurrence, correlates, and clinical implications. Clinical Psychology Review, 26, 769–782. 10.1016/j.cpr.2006.04.001 [DOI] [PubMed] [Google Scholar]
- Garner DM (2004). The eating disorder inventory-3: Professional manual. Psychological Assessment Resources Inc. [Google Scholar]
- Hoogland JJ, & Boomsma A (1998). Robustness studies in covariance structure modeling: An overview and a meta-analysis. Sociological Methods & Research, 26, 329–367. 10.1177/0049124198026003003 [DOI] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jenkinson PM, Taylor L, & Laws KR (2018). Self-reported interoceptive deficits in eating disorders: A meta-analysis of studies using the eating disorder inventory. Journal of Psychosomatic Research, 110, 38–45. 10.1016/j.jpsychores.2018.04.005 [DOI] [PubMed] [Google Scholar]
- Joiner TE (2005). Why people die by suicide. Harvard University Press. [Google Scholar]
- Kerr KL, Moseman SE, Avery JA, Bodurka J, Zucker NL, & Simmons WK (2016). Altered insula activity during visceral interoception in weight-restored patients with anorexia nervosa. Neuropsychopharmacology, 41, 521–528. 10.1038/npp.2015.174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalsa SS, Craske MG, Li W, Vangala S, Strober M, & Feusner JD (2015). Altered interoceptive awareness in anorexia nervosa: Effects of meal anticipation, consumption and bodily arousal. International Journal of Eating Disorders, 48, 889–897. 10.1002/eat.22387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, & Kim H (2009). Body-image dissatisfaction as a predictor of suicidal ideation among Korean boys and girls in different stages of adolescence: A two-year longitudinal study. Journal of Adolescent Health, 45, 47–54. 10.1016/j.jadohealth.2008.11.017 [DOI] [PubMed] [Google Scholar]
- Kok BE, & Singer T (2017). Phenomenological fingerprints of four meditations: Differential state changes in affect, mind-wandering, meta-cognition, and interoception before and after daily practice across 9 months of training. Mindfulness, 8, 218–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan M (2014). DBT Skills training manual. New York: Guilford Publications. [Google Scholar]
- Mehling WE, Acree M, Stewart A, Silas J, & Jones A (2018). The multidimensional assessment of interoceptive awareness, version 2 (MAIA-2). PLoS ONE, 13, e0208034. 10.1371/journal.pone.0208034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merwin RM, Zucker NL, Lacy JL, & Elliot CA (2010). Interoceptive awareness in eating disorders: Distinguishing lack of clarity from non-acceptance of internal experience. Cognition and Emotion, 24, 892–902. 10.1080/02699930902985845 [DOI] [Google Scholar]
- Muehlenkamp JJ (2012). Body regard in nonsuicidal self-injury: Theoretical explanations and treatment directions. Journal of Cognitive Psychotherapy, 26, 331–347. 10.1891/0889-8391.26.4.331 [DOI] [Google Scholar]
- Muehlenkamp JJ, Peat CM, Claes L, & Smits D (2012). Self‐injury and disordered eating: Expressing emotion dysregulation through the body. Suicide and Life‐Threatening Behavior, 42, 416–425. 10.1111/j.1943-278X.2012.00100.x [DOI] [PubMed] [Google Scholar]
- Muthén LK & Muthén BO (1998–2012). Mplus user’s guide: Statistical analysis with latent variables (7th ed.). Muthén & Muthén. [Google Scholar]
- Mustelin L, Silén Y, Raevuori A, Hoek HW, Kaprio J, & Keski-Rahkonen A (2016). The DSM-5 diagnostic criteria for anorexia nervosa may change its population prevalence and prognostic value. Journal of Psychiatric Research, 77, 85–91. 10.1016/j.jpsychires.2016.03.003 [DOI] [PubMed] [Google Scholar]
- Obeid N, Norris ML, Valois DD, Buchholz A, Goldfield GS, Hadjiyannakis S, Henderson KA, Flament M, Hammond NG, Dunn J, & Spettigue W (2020). Bingeing, purging, and suicidal ideation in clinical and non-clinical samples of youth. Eating Disorders, 28, 289–307. 10.1080/10640266.2019.1642033 [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Levinson C, & Calebs B (2018). A network analysis of eating disorder symptoms and characteristics in an inpatient sample. Psychiatry Research, 262, 270–281. 10.1016/j.psychres.2018.02.027 [DOI] [PubMed] [Google Scholar]
- Ortiz SN, & Smith AR (2020). A longitudinal examination of the relationship between eating disorder symptoms and suicidal ideation. International Journal of Eating Disorders, 53, 69–78. 10.1002/eat.23162 [DOI] [PubMed] [Google Scholar]
- Paxton SJ, & Diggens J (1997). Avoidance coping, binge eating, and depression: An examination of the escape theory of binge eating. International Journal of Eating Disorders, 22, 83–87. [DOI] [PubMed] [Google Scholar]
- Peebles R, Wilson JL, & Lock JD (2011). Self-injury in adolescents with eating disorders: Correlates and provider bias. Journal of Adolescent Health, 48, 310–313. 10.1016/j.jadohealth.2010.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollatos O, Kurz A, Albrecht J, Schreder T, Kleeman AM, Schöpf V, Kopietz R, Wiesemann M, & Schandry R (2008). Reduced perception of bodily signals in anorexia nervosa. Eating Behaviors, 9, 381–388. 10.1016/j.eatbeh.2008.02.001 [DOI] [PubMed] [Google Scholar]
- Preyde M, Watson J, Remers S, & Stuart R (2016). Emotional dysregulation, interoceptive deficits, and treatment outcomes in patients with eating disorders. Social Work in Mental Health, 14, 227–244. 10.1080/15332985.2014.990076 [DOI] [Google Scholar]
- Price CJ, Thompson EA, Crowell SE, Pike K, Cheng SC, Parent S, & Hooven C (2019). Immediate effects of interoceptive awareness training through Mindful Awareness in Body-oriented Therapy (MABT) for women in substance use disorder treatment. Substance Abuse, 40, 102–115. 10.1080/08897077.2018.1488335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds WM (1987). Suicidal ideation questionnaire-Junior. Psychological Assessment Resources. [Google Scholar]
- Rodgers RF, Berry R, & Franko DL (2018). Eating disorders in ethnic minorities: An update. Current Psychiatry Reports, 20, 90. 10.1007/s11920-018-0938-3 [DOI] [PubMed] [Google Scholar]
- Rodríguez-Cano T, Beato-Fernández L, & Llario AB (2006). Body dissatisfaction as a predictor of self-reported suicide attempts in adolescents: A Spanish community prospective study. Journal of Adolescent Health, 38, 684–688. 10.1016/j.jadohealth.2005.08.003 [DOI] [PubMed] [Google Scholar]
- Rogers ML, Hagan CR, & Joiner TE (2018). Examination of interoception along the suicidality continuum. Journal of Clinical Psychology, 74, 1004–1016. 10.1002/jclp.22564 [DOI] [PubMed] [Google Scholar]
- Rueter MA, & Kwon H (2005). Developmental trends in adolescent suicidal ideation. Journal of Research on Adolescence, 15, 205–222. 10.1111/j.1532-7795.2005.00092.x [DOI] [Google Scholar]
- Schulz A, Lass-Hennemann J, Sütterlin S Schächinger H, Vögele C (2013). Cold pressor stress induces opposite effects on cardioceptive accuracy dependent on assessment paradigm. Biological Psychology, 93(1), 167–174. 10.1016/j.biopsycho.2013.01.007 [DOI] [PubMed] [Google Scholar]
- Smith AR, Dodd DR, Ortiz SN, Forrest LN, & Witte TK (2019a). Interoceptive deficits differentiate suicide groups and associate with self-injurious thoughts and behaviors in a military sample. Suicide and Life-Threatening Behavior, 50, 472–489. 10.1111/sltb.12603 [DOI] [PubMed] [Google Scholar]
- Smith AR, Forrest LN, Perkins NM, Kinkel-Ram S, Bernstein M, & Witte TK (in prep). Reconnecting to internal sensation and experiences: Development of an online intervention to improve interoception and results from a pilot feasibility study. [DOI] [PubMed]
- Smith AR, Forrest LN, & Velkoff EA (2018a). Out of touch: Interoceptive deficits are elevated in suicide attempters with eating disorders. Eating Disorders, 26, 52–65. 10.1080/10640266.2018.1418243 [DOI] [PubMed] [Google Scholar]
- Smith AR, Ortiz SN, Forrest LN, Velkoff EA, & Dodd DR (2018b). Which comes first? An examination of associations and shared risk factors for eating disorders and suicidality. Current Psychiatry Reports, 20, 77. 10.1007/s11920-018-0931-x [DOI] [PubMed] [Google Scholar]
- Smith AR, Velkoff EA, Ribeiro JD, & Franklin JC (2019b). Are eating disorders and related symptoms risk factors for suicidal thoughts and behaviors? A meta-analysis. Suicide and Life-Threatening Behavior, 49, 221–239. 10.1111/sltb.12427 [DOI] [PubMed] [Google Scholar]
- Smyth JM, Heron KE, Sliwinski MJ, Wonderlich SA, Crosby RD, Mitchel JE, & Engel SG (2007). Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology, 75, 629–638. 10.1037/0022-006X.75.4.629 [DOI] [PubMed] [Google Scholar]
- Soper DS (2020). A-priori Sample Size Calculator for Structural Equation Models [Software]. Available from https://www.danielsoper.com/statcalc
- Stice E, Killen JD, Hayward C, & Taylor CB (1998). Age of onset for binge eating and purging during late adolescence: A 4-year survival analysis. Journal of Abnormal Psychology, 107, 671–675. 10.1037/0021-843X.107.4.671 [DOI] [PubMed] [Google Scholar]
- Strigo IA, Matthews SC, Simmons AN, Oberndorfer T, Klabunde LE, & Kate WH (2013). Altered insula activation during pain anticipation in individuals recovered from anorexia nervosa: Evidence of interoceptive dysregulation. International Journal of Eating Disorders, 46, 23–33. 10.1002/eat.22045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trujillo A, Forrest LN, Claypool HM, & Smith AR (2019). Assessing longitudinal relationships among thwarted belongingness, perceived burdensomeness, and eating disorder symptoms. Suicide and Life-Threatening Behavior, 49, 1609–1620. 10.1111/sltb.12541 [DOI] [PubMed] [Google Scholar]
- Tylka TL (2006). Development and psychometric properties of a measure of intuitive eating. Journal of Counseling Psychology, 53, 226–240. 10.1037/0022-0167.53.2.226 [DOI] [Google Scholar]
- Wildes JE, Ringham RM, & Marcus MD (2010). Emotion avoidance in patients with anorexia nervosa: Initial test of a functional model. International Journal of Eating Disorders, 43, 398–404. 10.1002/eat.20730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittkamp MF, Bertsch K, Vögele C & Schulz A (2018). A latent state-trait analysis of interoceptive accuracy. Psychophysiology, 55, e13055. 10.1111/psyp.13055 [DOI] [PubMed] [Google Scholar]
- Zamariola G, Frost N, Oost AV, Corneille O, Luminet O (2019). Relationship between interoception and emotion regulation: New evidence from mixed methods. Journal of Affective Disorders, 246, 480–485. 10.1016/j.jad.2018.12.101 [DOI] [PubMed] [Google Scholar]


