Summary
Frailty prevention is a cornerstone for the extension of healthy life expectancy. It is a multi-dimensional construct that includes physical, mental, and social aspects. Frailty is reversible and can be attenuated by intervention; therefore, its early detection is important in primary and community care. The mainstream of disability prevention in Japan, which comprises the Japanese and local governments as well as healthcare workers, was a high-risk approach until 2014. Given the revision on Japan's long-term care insurance law, current ageing health policies have shifted to more population centric approach. Implements group activities called "Kayoi-no-ba" has been valued in Japan as disability prevention initiative. The Kihon Checklist - a 25-item questionnaire - has been broadly used by health experts and researchers to assess frailty in Japan. However, a new 15-item questionnaire has been newly developed to identify frailty and other health-related problems in older people of 75 years and above. This will enable providing the necessary support to frail individuals at any healthcare facility in local communities. The increase in frailty prevalence in older people has been concern during the COVID-19 pandemic. Home-based physical exercise programs are expected to be effective for frailty prevention. Utilization of information and communication technologies, social network services, and video calls has attracted attention for being effective tools to facilitate communication for older people during the pandemic. Further, life course approaches are needed to clarify the midlife risk of frailty development in later life.
Keywords: COVID-19, Kayoi-no-ba, HEPOP, community, social connection, ICT
Introduction
The number of elderly people worldwide is increasing rapidly, and the rate of this increase is fastest in Japan. While the average life expectancy is increasing year by year, improvements in healthy life expectancy have only tracked these in parallel (1) (Figure 1). The Japanese government has set a target of extending healthy life expectancy by three or more years by 2040 (2). To close the gap between the average life expectancy and healthy life expectancy, it is necessary for society as a whole to act against frailty.
Figure 1.
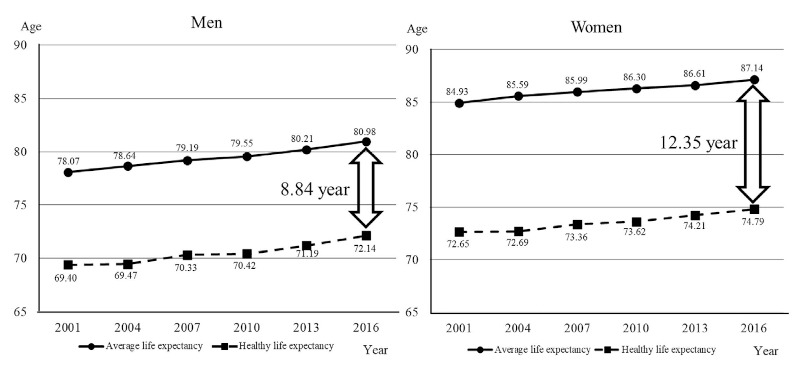
Chronological change of average life expectancy and healthy life expectancy. Average life expectancy is increasing year by year, but healthy life expectancy is only improving in parallel. Data source: Cabinet Office Japan. Annual Report on the Ageing Society 2019 (1).
In this article, we briefly review the definition and assessment of frailty and discuss how it can best be managed during the COVID-19 pandemic in Japan.
Definition of frailty
The word "frailty" has been attracting attention as a keyword in geriatric medicine and public health since the end of the 20th century (3). As a generic term, "frailty" is the noun form of frail, which means "easily broken or destroyed" or "physically weak." As a term in geriatric medicine and gerontology, experts involved in the Frailty Consensus Conference defined frailty in 2013 as follows (4): "A medical syndrome with multiple causes and contributors that is characterized by diminished strength, endurance, and reduced physiologic function that increases an individual's vulnerability for developing increased dependency and/or death". Similarly, the Japan Geriatrics Society defined frailty in 2014 as "a state of increased vulnerability to disability caused by various functional and/or intrinsic capacity deterioration due to aging" (5).
Among experts, the consensus is that frailty is reversible or attenuated by interventions; thus, early detection is important in primary and community care by health workers (6). Frailty is also characterized by multiple dimensions, namely, physical, mental, and social aspects, which are associated with each other and determine an individual's frailty status.
No standardized definition of frailty has been yet established (4), making it impossible to measure its prevalence, which is therefore uncertain. A systematic review of 21 studies including 61,500 older community residents revealed a wide variance in the prevalence of frailty among studies (range 4.0-59.1%) and estimated the overall weighted prevalence as 11% (7). Frailty was generally found to be higher in women than in men, and it becomes more prevalent with age (7-9). Being a member of an ethnic minority group or having low socioeconomic status are considered risk factors for frailty (8,9).
There are two major models that have been widely used to operationalize the concept of physical frailty. One is the phenotype model proposed by Fried et al. (10), which suggested considering the presence of five symptoms to identify frailty in individuals: weight loss, exhaustion, weakness, slowness, and reduced physical activity. The criteria they developed for the Cardiovascular Health Study (CHS) has been widely used as the standard of physical frailty. Additionally, the deficit model proposed by Rockwood and Mitnitski accumulates the number of impairments and conditions to create frailty index (11).
With aging, muscle strength weakens, and this induces fatigue. Thus, older persons feeling excessive fatigue tend to avoid physical activity and stay home, which results in a further decline of muscle strength, energy expenditure, and appetite, thereby leading to weight and further muscle loss, that is, a frailty cycle (10). Fatigue and physical inactivity may cause sleep disturbance, depression, and social isolation, which accelerate the loss of appetite and vitality. There is no doubt that social disconnectedness, loneliness, and depression are associated with each other, and each increases the risk of physical frailty (12). However, there has been much debate about how to capture mental and social aspects of frailty (13).
Assessment of frailty
There have been a number of tools created to evaluate frailty. In their review article, Dent et al. listed 16 commonly used frailty instruments (14). It is important to choose an appropriate assessment tool for different types of patients (15). The validity of the instruments may vary by the setting and purpose, such as primary care facilities, hospitals, long-term care facilities, or local community facilities, where frailty prevention strategies have primarily been conducted by public health nurses.
As the standard criteria to diagnose frailty in Japan, the Japanese version of the CHS frailty index criteria (J-CHS criteria) was proposed based on the evidence of Japanese older adults (Table 1, J-CHS criteria) (16). According to the J-CHS criteria, prevalence of frailty among community dwellers ≥ 65 years ranged from 2.0% to 21.5% in Japan (16). Age-stratified meta-analyses showed the pooled prevalence of frailty defined by CHS criteria in Japan was 8.1% for women and 7.6% for men (17).
Table 1. The J-CHS Criteria.
| Shrinking | Have you lost 2 kg or more in the past 6 months? | Yes = 1, No = 0 |
| Low activity | 1) Do you engage in moderate levels of physical exercise or sports aimed at health? | "No" to both questions = 1 |
| 2) Do you engage in low levels of physical exercise aimed at health? | ||
| Exhaustion | In the past 2 weeks have you felt tired without a reason? | Yes = 1, No = 0 |
| Weakness | Grip strength | |
| Men: < 26 kg, Women: < 18 kg | ||
| Slowness | Gait speed | |
| < 1.0 m/s |
Note: Frailty, prefrailty, and robustness are defined by having 3-5, 1-2, and 0 components, respectively (13).
The J-CHS criteria include grip strength and gait speed, which requires actual measurement. Therefore, a more convenient tool is desired for broader application in public health practices. The Kihon Checklist (KCL) is a self-administrative questionnaire comprising 25 items (18), which was originally developed to select the targets for disability prevention by the Japanese Ministry of Health, Labour and Welfare (MHLW). It comprises seven domains, namely, instrumental ability of daily living, physical function, nutritional status, oral function, social isolation, cognitive function, and mental health. Its reliability and validity as a frailty screening tool against the CHS criteria has been demonstrated among outpatients (19). The validity of KCL as a predictive index of the need for long-term care and mortality among community-dwelling older people has also been confirmed (20). Furthermore, it has been translated into English, Spanish, Portuguese, and Simplified Chinese and has been widely used worldwide (21).
Recently, a new 15-item self-administrative questionnaire was developed and proposed by MHLW to assess health-related problems for older people, 75 years or above (22,23). It includes questions inquiring about general health perception; life satisfaction; and physical, cognitive, mental, social, and oral frailty. Detailed properties of the new frail questionnaire are under investigation. The recently developed Questionnaire for Medical Checkup of Old-Old (QMCOO) is designed to identify frail older persons in all healthcare settings, including at health checkups and in primary care clinics (Table 2) (23). This approach is expected to help frail patients find support that they need in their communities.
Table 2. Questionnaire for medical checkup of the old-old (QMCOO) (23) .
| No. | Questions | Answer |
|---|---|---|
| 1 | How is your health? | ① Excellent ② Good ③ Fair ④ Poor ⑤ Very poor |
| 2 | Are you satisfied with your daily life? | ① Satisfied ② Moderately satisfied ③ Moderately dissatisfied ④ Dissatisfied |
| 3 | Do you eat three times a day? | ① Yes ② No |
| 4 | Do you have any difficulties eating tough foods, compared to 6 months ago? | ① Yes ② No |
| 5 | Have you choked on your tea or soup recently? | ① Yes ② No |
| 6 | Have you lost 2 kg or more in the past 6 months? | ① Yes ② No |
| 7 | Do you think you walk slower than before? | ① Yes ② No |
| 8 | Have you experienced a fall in the past year? | ① Yes ② No |
| 9 | Do you go for a walk for your health at least once a week? | ① Yes ② No |
| 10 | Do your family or friends point out your memory loss? (e.g., "You ask the same question over and over again.") | ① Yes ② No |
| 11 | Do you find yourself not knowing today's date? | ① Yes ② No |
| 12 | Do you smoke? | ① Yes ② No ③ I quit |
| 13 | Do you go out at least once a week? | ① Yes ② No |
| 14 | Do you keep up regular communication with your family and friends? | ① Yes ② No |
| 15 | When you are not feeling well, do you have anyone you can talk to? | ① Yes ② No |
Management of frailty
Although the importance of the management of frailty is recognized globally, effective strategies have not been established yet (14). Physical activity, diet, and social participation are possibly the key components of an effective intervention because physical inactivity, malnutrition, and social isolation are considered as modifiable risk factors of frailty (14).
"Kayoi-no-ba" is a mutual focal point where locally living older residents can work on health promotion through physical exercise, hobbies or other activities, supported by local activists, while the whole activities and the process are supported by local government. The word for word translation of "Kaoyoi" is "commuting" and "ba" is "a place" in English. However, "ba" in this context implies a focal point where people with mutual interests are drawn to gather. As an intervening measure of frailty/disability prevention, "Kayoi-no-ba" generated greater public interests and is taken place across local communities in Japan. A large epidemiological study including 375,400 older adults aged 65 years or older living in a total of 81 regions (the Japan Gerontological Evaluation Study, JAGES, (24)) demonstrated that every social activity per hundred older people was significantly associated with an 11% reduction of the likelihood of frailty (odds ratio = 0.89; 95% credible interval = 0.81, 0.99) (25).
The mainstream of long-term care prevention in Japan used to be a high-risk approach, that is, efforts were made to identify and support individuals whose ability to perform activities of daily living was declining. Because of the revision to the Long-Term Care Insurance Law in 2014, the policy was shifted to more population-centric approach. "Kayoi-no-ba" came to the forefront regarding the measures for frailty and disability prevention. Both the number of "Kayoi-no-ba" and the prevalence of participants have kept increasing. According to a government report, there were 106,766 places and 5.7% of the community-dwelling older people participated in "Kayoi-no-ba" in 2018 (26). In 2019, the government announced an 8% increase to the participation rate of "Kayoi-no-ba" by 2025 as a numerical target of an initiative to prevent dementia.
From April 2020, "Integration of long-term care prevention and health services for the elderly" has been promoted by the MHLW. In this initiative, health professionals-such as public health nurses, registered dieticians, dental hygienists, physical therapists, occupational therapists, and speech therapists - are expected to actively get involved with "Kayoi-no-ba" by providing health consultation and education to the participants. They are also expected to evaluate participants' health condition and identify frail persons by using QMCOO, the new 15-item questionnaire for frailty assessment (23) to direct them toward the necessary support and medical services.
In the implementation of integrated disability prevention and healthcare services for older people, one of the major tasks is utilizing the database of national health insurance (Kokumin Hoken Database, KDB) to organize and analyze the health issues of local communities. Local municipalities are responsible for the provision of healthcare services to the residents. KDB is linked to the databases for long-term care services, so that it enables provision of all information regarding medical and long-term care for each older person.
Health professionals who visit "Kayoi-no-ba" can evaluate the health condition of older individuals by using QMCOO, along with information on health checkups, medical care, and long-term care extracted from the KDB system. Then, they would advise the older person based on the available data and introduce them to appropriate healthcare services. Furthermore, by recording individuals' participation in "Kayoi-no-ba" in the KDB data, it is possible to evaluate the effectiveness of the "Kayoi-no-ba" as a frailty prevention strategy in the targeted area. From now on, by monitoring the effectiveness of "Kayoi-no-ba," it is expected to further improve the quality of the "Kayoi-no-ba" program in accordance with the plan-do-check-act cycle of local community-based integrated care system (27).
The COVID-19 pandemic and frailty
COVID-19, which began in Wuhan, China, started spreading throughout the world sometime in late 2019. The WHO declared it as a pandemic on March 11, 2020.
Figure 2 shows the daily number of reported COVID-19 cases in Japan during the period of January 16, 2020 and April 12, 2021 (28). In Japan, the first cases were reported on January 16, 2020, and hit its first peak in mid-April, with the number of new cases reaching 720 a day. From early April to May, a state of emergency was declared; movie theaters and department stores were closed, and people were asked to refrain from going out. The number of infected people rose again, reaching a second peak of 1,604 at the beginning of August. It began to increase in early November with a peak of 7,844 on January 8. A fourth wave came in early April, 2021, and the number of cases including new variants continues to increase even now (April 19, 2021).
Figure 2.
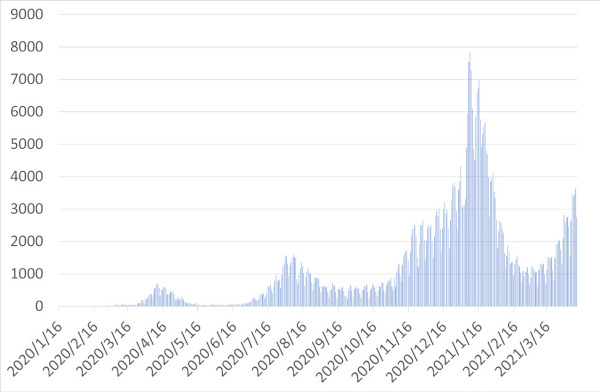
Number of daily confirmed cases of COVID-19 tested by PCR in Japan. During the period of January 16, 2020 and April 12, 2021. Data source: Ministry of Health, Labour and Welfare, Open data (28).
One of the characteristics of COVID-19 is that older people are more likely to become seriously ill. In the first wave, older people were the major victims of the COVID-19 pandemic (Figure 3) (29). Most seniors refrained from going out for fear of infection and stayed home.
Figure 3.
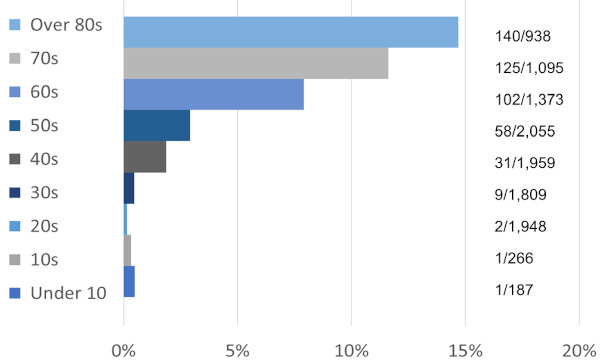
Prevalence of severe cases among confirmed cases of COVID-19 during the first wave of COVID-19 pandemic in Japan. Older people were more likely to become seriously ill from suffering from COVID-19 during the period of January 16 and April 22, 2020, in the first wave of COVID-19 pandemic. Data source: Ministry of Health, Labour and Welfare, The case of coronavirus, April 23, 2020 (29).
It is obvious that restraint from going out will accelerate the frailty cycle in older people. The impact of the COVID-19 pandemic on the development of frailty has only been beginning to emerge. Thus, we need to consider what can and should be done for better management of frailty during the pandemic (30,31).
Prevention of frailty under the COVID-19 pandemic: NCGG-HEPOP
At time of writing (mid-April 2021), it is unpredictable when the COVID-19 pandemic will come to an end. For older adults, staying at home for fear of infection is considered to be a risk in terms of the development of frailty. Thus, efforts to prevent frailty along with infection control are needed (32,33).
Presently, efforts for frailty prevention during the COVID-19 pandemic are being made. The National Center of Geriatrics and Gerontology (NCGG) has developed a guide for home-based activities for frailty prevention and made it available on the web (34) (https://www.ncgg.go.jp/hospital/english/hepop/). The guide for Home Exercise Program for Older People (HEPOP) introduces six packages, including physical exercises, eating methods, and cognitive training, that older individuals can practice at home according to their individual abilities or needs in an easy-to-understand manner. The packages include balance improvement, physical strengthening, inactivity prevention, cognitive, feeding and swallowing improvement, and nutrition improvement.
Those who would like to start HEPOP, the home exercise program, can use the flowchart to determine which package is the most appropriate (Figure 4). As the appropriateness of the package may change depending on the patient's physical and mental status, it is recommended to reassess once a month or whenever any change is perceived. Before starting an exercise or activity, it is recommended to check the "precautions and methods of use" and "exercise intensity" to select the most appropriate exercise or activity for each individual's needs.
Figure 4.
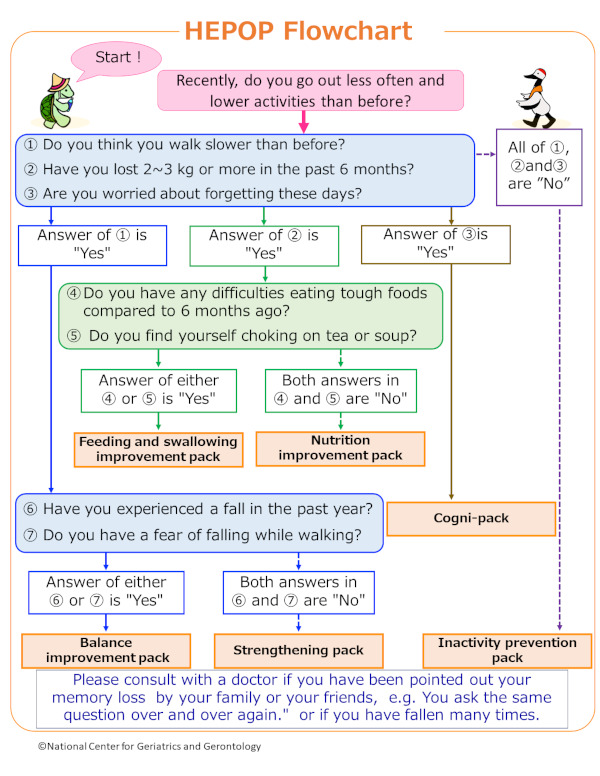
HEPOP flowchart. Reproduced from (34) by permission of National Center for Geriatrics and Gerontology. Those who would like to start HEPOP, the home exercise program, can use the flowchart to determine which program package is the most appropriate for them. The questionnaire items are derived from Kihon Checklist (18) and QMCOO (23).
The balance improvement package is for frail or pre-frail individuals who have fear of falling to improve their muscle strength and balancing ability. The physical strengthening package is for those who perceive slowness in their walking speed, and it is designed to improve and maintain physical functions and strength. The inactivity prevention package is designed to help robust older people to maintain their physical functions. All three packages include stretching, balance, muscle training, and whole-body exercises. These combine various exercises and require 40 to 60 minutes per day depending on the self-condition (20 to 60 minutes for the balance improvement package). The cogni-package is for those who are afraid of cognitive decline. It includes several tasks combining "exercise" with "cognition," which we call "cognicise" (35): dual-task training, conducting cognitive tasks such as word games, performing fast simple numerical calculations, and playing a simple memory span game while performing aerobic exercises. The feeding and swallowing improvement package is for those who have lost more than 2 to 3 kg of weight during the past six months and feel difficulties in eating and/or swallowing and who want to be provided with basic information about oral frailty (36) and exercises to maintain oral and swallowing function. The nutrition improvement package is for those who lost weight without oral frailty and is designed to provide information about malnutrition and advice to improve their diet.
HEPOP is applicable to all older people with stable physical condition and no serious pain, including inpatients on discharge, outpatients, and older people living in the community. Implementation, adoption, and effectiveness of HEPOP are under investigation.
Social connection under the COVID-19 pandemic
The COVID-19 pandemic forces older people to avoid physical contact with others, which increases psychological distress and reduces sources of support, thus leading them to frailty or more severe consequences. To maintain social connection during the COVID-19 pandemic is the most difficult part of frailty prevention, especially for older people living alone. While phone calls and postal letters are common conventional communication tools, e-mails have become popular. Use of social network services and video calls has attracted attention as effective tools during the pandemic to facilitate communication for older people (33). According to reports from the Ministry of Internal Affairs and Communications (37), 90.5% of 60-year-olds, 74.2% of 70-year-olds, and 57.5% of 80-year-olds were using internet in 2019. Although the evidence regarding the effectiveness of video call in the reduction of loneliness in older adults are still limited (38), intervention utilizing information and communication technologies (ICT) has been promoted. Note that ICT is not always beneficial for all people (39), and promoting ICT may increase inequality in terms of access and usage because not everyone can afford to buy ICT tools or have enough time and skills to keep up with the latest information as well as reach out to various support services. Those who are disadvantaged could be left far behind in this information age. Thus, it is crucial to provide sufficient support for older people to use ICT such as mobile phones or computers as well as other options.
Future implication
Recently, Taniguchi et al. examined 2,675 Japanese people aged 65-90 years prospectively and identified four distinct trajectory patterns (40). According to their report, 36.3% had very high functional capacity at the age of 65 and maintained higher functional capacity even after 85 years of age. In contrast, 6.1% had low functional capacity at the age of 65 already and kept losing their functional capacity year by year. The rest shared the same level of functional capacity at the age of 65 years; however, 40.1% maintained the level until 85 years of age and 17.4% saw a decrease. Their study implies that most of those who would be frail in the future may have been already determined at the age of 65. This is consistent with the findings of the Whitehall II study by Brunner et al. that health behaviors and biomedical risk factors measured at 50 years of age and above explained more than one-third of socioeconomic inequalities in frailty (41).
It is essential to detect frail individual among older persons to provide them with the necessary support. It is also important to intervene with middle-aged people to limit future frailty. More life course studies are needed to clarify the modifiable risk factors concerning frailty.
Conclusion
There is an urgent need to establish an effective frailty prevention strategy for use during the COVID-19 pandemic. A newly developed 15-item questionnaire and home-based physical exercise programs are expected to promote frailty management in Japan. Life course approaches are also needed to clarify the midlife risk for frailty development in later life.
Acknowledgements
We thank Dr. Noriko Cable for valuable advice on the description about "Kayoi-no-ba" and Dr. Mikako Yasuoka for drawing the figure.
Funding:
This work was supported by the Health and Labour Sciences Research Grants (number 20AA2006), JSPS KAKENHI Grant (number JP20H03954), the Research Funding for Longevity Sciences from National Center for Geriatrics and Gerontology, Japan (19- 51), and the Japan Health Research Promotion Bureau Research Fund (2020-B-09).
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- 1.Cabinet Office Japan. Annual Report on the Ageing Society 2019 ‒ Trends of living of the elderly. https://www8.cao.go.jp/kourei/english/annualreport/2019/pdf/2019.pdf (accessed December 1, 2020) .
- 2.Ministry of Health, Labour and Welfare. Report from the expert meeting regarding health expectancy 2019. https://www.mhlw.go.jp/content/10904750/000495323.pdf (accessed December 1, 2020). (in Japanese).
- 3.Rockwood K, Fox RA, Stolee P, Robertson D, Beattie BL. Frailty in elderly people: An evolving concept. CMAJ. 1994; 150:489-495. [PMC free article] [PubMed] [Google Scholar]
- 4.Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: A call to action. J Am Med Dir Assoc. 2013; 14:392-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Society TJG. Statement on the frailty from the Japan Geriatrics Society 2014. http://www.jpn-geriat-soc.or.jp/info/topics/pdf/20140513_01_01.pdf (accessed December 1, 2020). (in Japanese).
- 6.Rodríguez-Mañas L, Féart C, Mann G, et al. Searching for an operational definition of frailty: A Delphi method based consensus statement: The frailty operative definition-consensus conference project. J Gerontol A Biol Sci Med Sci. 2013; 68:62-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: A systematic review. J Am Geriatr Soc. 2012; 60:1487-1492. [DOI] [PubMed] [Google Scholar]
- 8.Bandeen-Roche K, Seplaki CL, Huang J, Buta B, Kalyani RR, Varadhan R, Xue QL, Walston JD, Kasper JD. Frailty in older adults: A nationally representative profile in the United States. J Gerontol A Biol Sci Med Sci. 2015; 70:1427-1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoogendijk EO, van Hout HP, Heymans MW, van der Horst HE, Frijters DH, van Groenou MI, Deeg DJ, Huisman M. Explaining the association between educational level and frailty in older adults: Results from a 13-year longitudinal study in the Netherlands. Ann Epidemiol. 2014; 24:538-544. [DOI] [PubMed] [Google Scholar]
- 10.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001; 56:M146-M156. [DOI] [PubMed] [Google Scholar]
- 11.Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007; 62:722-727. [DOI] [PubMed] [Google Scholar]
- 12.Gale CR, Westbury L, Cooper C. Social isolation and loneliness as risk factors for the progression of frailty: The english longitudinal study of ageing. Age Ageing. 2018; 47:392-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bunt S, Steverink N, Olthof J, van der Schans CP, Hobbelen JSM. Social frailty in older adults: A scoping review. Eur J Ageing. 2017; 14:323-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: Opportunities, challenges, and future directions. The Lancet. 2019; 394:1376-1386. [DOI] [PubMed] [Google Scholar]
- 15.Rockwood K, Theou O, Mitnitski A. What are frailty instruments for? Age Ageing. 2015; 44:545-547. [DOI] [PubMed] [Google Scholar]
- 16.Satake S, Shimada H, Yamada M, Kim H, Yoshida H, Gondo Y, Matsubayashi K, Matsushita E, Kuzuya M, Kozaki K, Sugimoto K. Prevalence of frailty among community-dwellers and outpatients in Japan as defined by the Japanese version of the Cardiovascular Health Study criteria. Geriatr Gerontol Int. 2017; 17:2629-2634. [DOI] [PubMed] [Google Scholar]
- 17.Kojima G, Iliffe S, Taniguchi Y, Shimada H, Rakugi H, Walters K. Prevalence of frailty in Japan: A systematic review and meta-analysis. J Epidemiol. 2017; 27:347-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arai H, Satake S. English translation of the Kihon Checklist. Geriatr Gerontol Int. 2015; 15:518-519. [DOI] [PubMed] [Google Scholar]
- 19.Satake S, Senda K, Hong YJ, Miura H, Endo H, Sakurai T, Kondo I, Toba K. Validity of the Kihon Checklist for assessing frailty status. Geriatr Gerontol Int. 2016; 16:709-715. [DOI] [PubMed] [Google Scholar]
- 20.Satake S, Shimokata H, Senda K, Kondo I, Toba K. Validity of total Kihon checklist score for predicting the incidence of 3-year dependency and mortality in a community-dwelling older population. J Am Med Dir Assoc. 2017; 18:552. e1-e6 [DOI] [PubMed] [Google Scholar]
- 21.Sewo Sampaio PY, Sampaio RA, Yamada M, Arai H. Systematic review of the Kihon Checklist: Is it a reliable assessment of frailty? Geriatr Gerontol Int. 2016; 16:893-902. [DOI] [PubMed] [Google Scholar]
- 22.Ministry of Health, Labour and Welfare. Explanation and n o tes o f the q u e s t ionnai r e f o r med i cal checkup of the old-old. https://www.mhlw.go.jp/content/12401000/000557576.pdf (accessed December 1, 2020). (in Japanese).
- 23.Satake S, Arai H. Questionnaire for medical checkup of old-old (QMCOO). Geriatr Gerontol Int. 2020; 20:991-992. [DOI] [PubMed] [Google Scholar]
- 24.Kondo K, Rosenberg M, World Health O. Advancing universal health coverage through knowledge translation for healthy ageing: Lessons learnt from the Japan gerontological evaluation study. Geneva: World Health Organization. 2018. [Google Scholar]
- 25.Sato K, Ikeda T, Watanabe R, Kondo N, Kawachi I, Kondo K. Intensity of community-based programs by long-term care insurers and the likelihood of frailty: Multilevel analysis of older Japanese adults. Soc Sci Med. 2020; 245:112701. [DOI] [PubMed] [Google Scholar]
- 26.Ministry of Health, Labour and Welfare. Report of the long-term care prevention and daily life support service 2018. https://www.mhlw.go.jp/content/12300000/000570876.pdf (accessed December 1, 2020). (in Japanese).
- 27.Ministry of Health, Labour and Welfare. Establishing 'the Community-based Integrated Care System' 2017. https://www.mhlw.go.jp/english/policy/care-welfare/care-welfare-elderly/dl/establish_e.pdf (accessed December 1, 2020).
- 28.Ministry of Health, Labour and Welfare. Open data/ number of positive cases. https://www.mhlw.go.jp/stf/covid-19/open-data_english.html (accessed April 1, 2021).
- 29.Ministry of Health, Labour and Welfare. The case of the coronavirus, April 23, 2020, Updates on COVID-19 in Japan. https://www.mhlw.go.jp/content/10900000/000624432.pdf (accessed April 1, 2021).
- 30.Nestola T, Orlandini L, Beard JR, Cesari M. COVID-19 and intrinsic capacity. J Nutr Health Aging. 2020; 24:692-695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Richardson SJ, Carroll CB, Close J, Gordon AL, O'Brien J, Quinn TJ, Rochester L, Sayer AA, Shenkin SD, van der Velde N, Woo J. Research with older people in a world with COVID-19: Identification of current and future priorities, challenges and opportunities. Age Ageing. 2020; 49:901-906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Valenzuela PL, Santos-Lozano A, Lista S, Serra-Rexach JA, Emanuele E, Lucia A. Coronavirus lockdown: Forced inactivity for the oldest old? J Am Med Dir Assoc. 2020; 21:988-989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen K. Use of gerontechnology to assist older adults to cope with the COVID-19 pandemic. J Am Med Dir Assoc. 2020; 21:983-984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Center for Geriatrics and Gerontology. NCGG Home Exercise Program for Older People (NCGG-HEPOP) 2020. https://www.ncgg.go.jp/hospital/english/hepop/index.html (accessed April 1, 2021).
- 35.Shimada H, Makizako H, Doi T, Park H, Tsutsumimoto K, Verghese J, Suzuki T. Effects of combined physical and cognitive exercises on cognition and mobility in patients with mild cognitive impairment: A randomized clinical trial. J Am Med Dir Assoc. 2018; 19:584-591. [DOI] [PubMed] [Google Scholar]
- 36.Watanabe Y, Okada K, Kondo M, Matsushita T, Nakazawa S, Yamazaki Y. Oral health for achieving longevity. Geriatr Gerontol Int. 2020; 20:526-538. [DOI] [PubMed] [Google Scholar]
- 37.Ministry of Internal Affairs and Communications. Participation rate in internet use by age 2021. https://www.soumu.go.jp/main_content/000689454.pdf (accessed December 1, 2020). (in Japanese).
- 38.Noone C, McSharry J, Smalle M, Burns A, Dwan K, Devane D, Morrissey EC. Video calls for reducing social isolation and loneliness in older people: A rapid review. Cochrane Database Syst Rev. 2020; 5:CD013632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hewitt J, Pennington A, Smith A, Gething S, Price M, White J, Dewar R, Carter B. A multi-centre, UK-based, non-inferiority randomised controlled trial of 4 follow-up assessment methods in stroke survivors. BMC Medicine. 2019; 17:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taniguchi Y, Kitamura A, Nofuji Y, Ishizaki T, Seino S, Yokoyama Y, Shinozaki T, Murayama H, Mitsutake S, Amano H, Nishi M. Association of trajectories of higher-level functional capacity with mortality and medical and long-term care costs among community-dwelling older Japanese. J Gerontol A Biol Sci Med Sci. 2019; 74:211-218. [DOI] [PubMed] [Google Scholar]
- 41.Brunner EJ, Shipley MJ, Ahmadi-Abhari S, Hernandez CV, Abell JG, Singh-Manoux A, Kawachi I, Kivimaki M. Midlife contributors to socioeconomic differences in frailty during later life: A prospective cohort study. Lancet Public Health. 2018; 3:e313-e322. [DOI] [PMC free article] [PubMed] [Google Scholar]


