1. Discussion
COVID-19 is a newly emerging disease that started in 2019 and spread worldwide to become a pandemic disease in 2020. Typically, the disease affects the respiratory system, and patients suffering from COVID 19 present with fever, cough, and shortness of breath. Nevertheless, affected patients may be asymptomatic or may present due to diseases in other systems or organs, like the nervous system, the heart, or the eye. 1 , 2 , 3
An acute ST-elevation myocardial infarction occurs due to the occlusion of one or more coronary arteries, causing transmural myocardial ischemia and resulting in myocardial injury or necrosis. Chest pain is the most common symptom of acute myocardial infarction. Other symptoms include shortness of breath, sweating, nausea or vomiting, and fainting. Moreover, some patients may be totally asymptomatic. Multiple risk factors were identified for myocardial infarction such as active smoking, hypertension, and diabetes. Patients with ST-elevation myocardial infarction (STEMI) should undergo percutaneous coronary intervention (PCI). If the PCI is not possible or not available, fibrinolytic therapy should be initiated. Myocardial infarction is associated with multiple complications such as pericarditis, ventricular free wall rupture, and different types of arrhythmia.
It is likely that COVID-19, directly and indirectly, affects the cardiovascular system and the heart in particular. Potential cardiovascular injury mechanisms have been identified and include direct myocardial injury from hemodynamic derangement or hypoxemia, inflammatory myocarditis, stress cardiomyopathy, microvascular dysfunction, thrombosis due to hypercoagulability, or systemic inflammation (cytokine storm) that can destabilize coronary artery plaques. In patients with COVID-19, the clinical manifestations of acute coronary artery disease are likely similar to those without the virus. Patients with symptomatic COVID-19 who present with acute STEMI appear to have a worse prognosis than those without COVID-19. 4 , 5
2. Visual case discussion
A 53-year-old patient was referred to the emergency department (ED) from a Covid-19 facility due to elevated blood pressure. The patient is a known case of hypertension who missed his medications for the last two days. He tested positive for the SARS-CoV-2 virus three days before presenting to the ED. The patient's blood pressure upon referral was 191/101 mmHg. In the ED, the patient was completely asymptomatic with no active complaints. The patient's vital signs showed a blood pressure of 170/93 mmHg; a heart rate of 119 beats per minute; a respiratory rate of 18 breaths per minute; a temperature of 37 C; and an oxygen saturation of 99% on room air. Thus, the patient's blood pressure medication was restarted. The patient's blood tests, and computerized chest tomography (CT) were unremarkable.
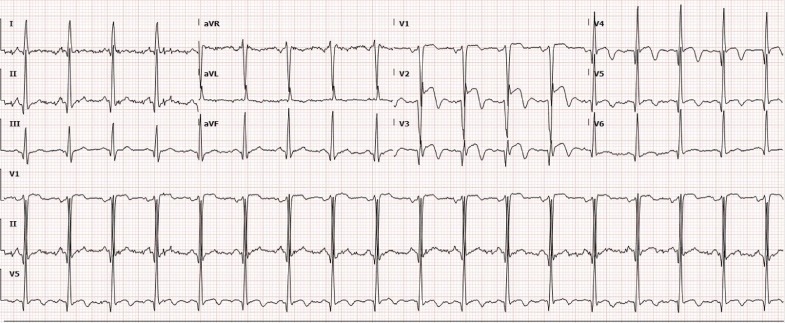
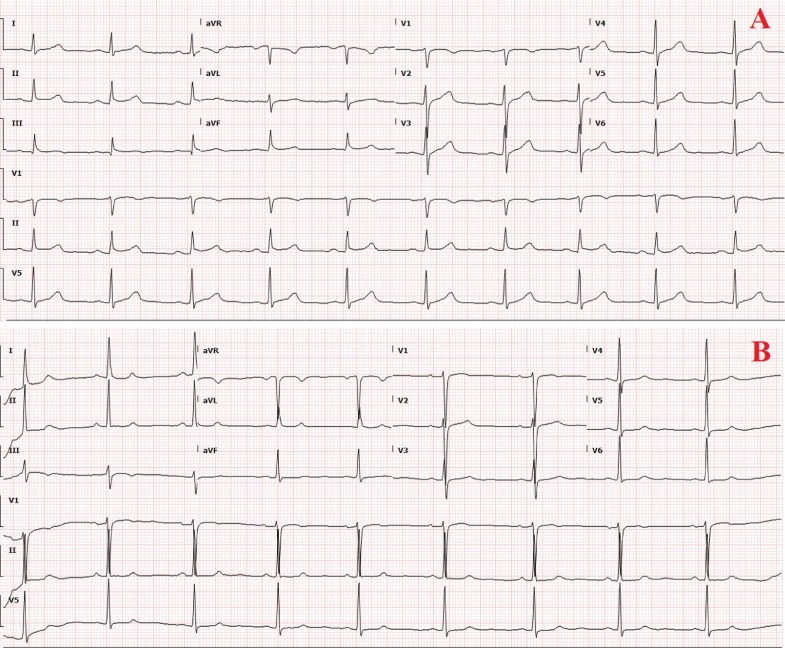
Nevertheless, the patient's electrocardiography (ECG) showed an ST-segment elevation in leads V1 – V4 and T inversion in chest leads (Fig. 1 ). The high sensitivity troponin T was standard 10.16 (<15 ng/L). Therefore, the interventional cardiologist was consulted, who suggest admitting the patient for observation and serial troponin as the patient was asymptomatic with normal serum troponin and his ECG changes are mostly due to elevated blood pressure. Serial troponin tests came back normal. His-repeated ECGs one hour and six hours later showed normal sinus rhythm with no ST-T changes (Fig. 2 A&B). Additionally, echocardiography revealed normal left ventricular function and no regional wall motion abnormality. Consequently, the patient was discharged to the field hospital.
Fig. 1.
ECG showed sinus tachycardia with ST segment elevation in leads V1–V3 with T inversion in chest leads.
Fig. 2.
ECG showed (A) a normal sinus rhythm with (B) signs of left ventricular hypertrophy.
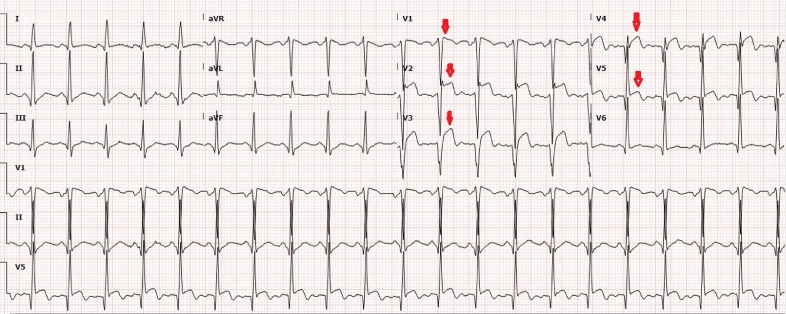
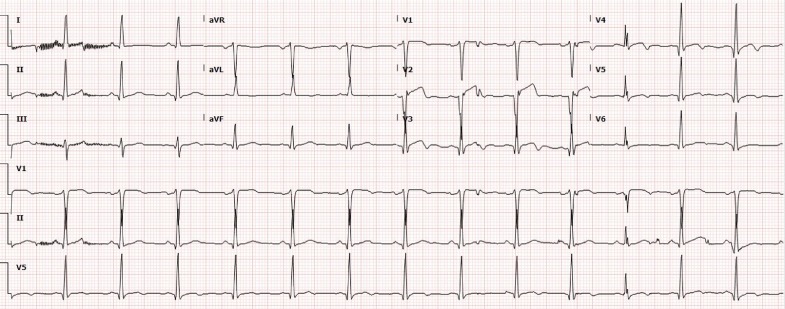
One day later, the patient was referred from the field hospital due to exertional chest discomfort and ECG changes. The ECG showed sinus tachycardia and ST-segment elevation in leads V1 – V5 (Fig. 3 ). The patient's vital signs revealed a blood pressure of 145/75 mmHg; a heart rate of 116 beats per minute; a respiratory rate of 22 breaths per minute; a temperature of 37 C; and an oxygen saturation of 99% on room air. ST-elevation myocardial infarction (STEMI) protocol was initiated, the interventional cardiologist was consulted, and the patient was shifted to another facility for urgent percutaneous coronary angiography (PCI). The coronary angiography showed two-vessel (left anterior descending artery and left circumflex artery) and left main stem disease. The patient was returned to the emergency and then admitted to the intensive care unit for monitoring. His-ECG post the cardiac catheterization showed regression of ST-segment elevation and the appearance of T wave inversion (Fig. 4 ). The patient was treated with dual antiplatelet, low molecular weight heparin, statin, and other supportive treatments. The patient improved and was observed in a telemetry bed. He remained asymptomatic until he became COVID-19 free. His-ECG before discharge showed the appearance of a Q wave in the anterior leads (Fig. 5 ); therefore, the patient was referred to another facility for coronary angiography bypass surgery.
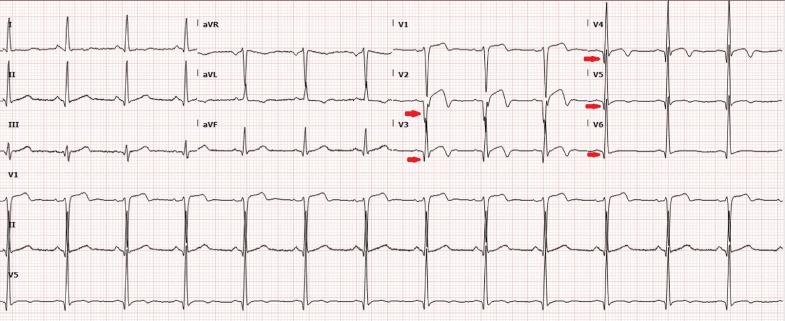
Fig. 3.
ECG showed sinus tachycardia and ST-segment elevation in leads V1 – V5 (down arrows).
Fig. 4.
ECG revealed sinus rhythm and regression of ST-segment elevation with the appearance of T wave inversion in leads V3-V5.
Fig. 5.
ECG showed sinus rhythm with the appearance of Q wave in chest leads (right arrows) in ddtion to the T waves inversion.
3. Questions and answers
Question 1
Please choose one option:
What is the acceptable standard door-to-balloon time for a STEMI patient in a PCI-capable facility?
-
1-
64 min.
-
2-
75 min.
-
3-
90 min.
-
4-
110 min.
-
5-
140 min.
The correct answer is (3- 90 min)
Explanation:
A door-to-balloon time of fewer than 90 min is the goal of a PCI-capable facility. It is one of the core measures of the Joint Commission on Accreditation of Healthcare Organizations. This is the time between the patient's arrival to the emergency department and the culprit lesion crossing by a guidewire in the cardiac Cath lab. Teamwork between EMS, emergency department physicians, and interventional cardiologists sets the groundwork for optimal door-to-balloon times (Level 1). 4
Question 2
True/ False Question:
Acute mitral regurgitation is considered one of the life-threatening mechanical complications of myocardial infarction?
-
1-
True.
-
2-
False.
The correct answer is (1- True)
Explanation: There are 3 life-threatening mechanical complications of myocardial infarction: ventricular free wall rupture, interventricular septum rupture, and acute mitral regurgitation. Acute mitral regurgitation following a myocardial infarction is most commonly due to ischemic papillary muscle displacement, left ventricular dilatation, or rupture of the papillary muscle of chordae. In ST-elevation myocardial infarction, the degree of mitral regurgitation is usually severe and associated with a 30-day survival of 24%. 4
Declaration of Competing Interest
We have no conflicts of interest to disclose.
References
- 1.Eid M.M., Zubaidi A.A. Cerebral venous thrombosis in a young patient with COVID-19. Vis J Emerg Med. 2021 doi: 10.1016/j.visj.2021. May 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eid M.M., Al Khalaf B.N. Conjunctivitis as initial presenting symptom in a COVID-19 patient. Vis J Emerg Med. 2021;23 doi: 10.1016/j.visj.2021.100997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eid M.M. COVID-19 patient with symptomatic bradycardia. Vis J Emerg Med. 2021;22 doi: 10.1016/j.visj.2020.100920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akbar H., Foth C., Kahloon R.A., et al. StatPearls [Internet] StatPearls Publishing; Treasure Island (FL): 2021. Acute ST Elevation myocardial infarction. [Updated 2020 Aug. 8]https://www.ncbi.nlm.nih.gov/books/NBK532281/ Jan-. Available from: [PubMed] [Google Scholar]
- 5.Pinto D., Windecker S., Saperia G. UpToDate. Uptodate.com. https://www.uptodate.com/contents/covid-19-myocardial-infarction-and-other-coronary-artery-disease-issues. Published 2021. Accessed April 2, 2021.