Abstract
Background
On March 17, 2020 the Association of American Medical Colleges recommended dismissal of medical students from clinical settings due to the COVID-19 pandemic. Third-year (M3) and fourth-year (M4) medical students were at home, M4s were interested in teaching, and residents and faculty had fewer clinical responsibilities due to elective surgery cancellations. To continue M3 access to education, we created a virtual surgery elective (VSE) that aimed to broaden students’ exposure to, and elicit interest in, general surgery (GS).
Methods
Faculty, surgical residents, and M4s collaborated to create a 2-wk VSE focusing on self-directed learning and direct interactions with surgery faculty. Each day was dedicated to a specific pathology commonly encountered in GS. A variety of teaching methods were employed including self-directed readings and videos, M4 peer lectures, case-based learning and operative video review with surgery faculty, and weekly surgical conferences. A VSE skills lab was also conducted to teach basic suturing and knot-tying. All lectures and skills labs were via Zoom videoconference (Zoom Video Communications Inc). A post-course anonymous survey sent to all participants assessed changes in their understanding of GS and their interest in GS and surgery overall.
Results
Fourteen M3s participated in this elective over two consecutive iterations. The survey response rate was 79%. Ninety-one percent of students believed the course met its learning objectives “well” or “very well.” Prior to the course, 27% reported a “good understanding” and 0% a “very good” understanding of GS. Post-course, 100% reported a “good” or “very good” understanding of GS, a statistically significant increase (P = 0.0003). Eighty-two percent reported increased interest in GS and 64% reported an increase in pursuing GS as a career.
Conclusions
As proof of concept, this online course successfully demonstrated virtual medical student education can increase student understanding of GS topics, increase interest in GS, and increase interest in careers in surgery. To broaden student exposure to GS, we plan to integrate archived portions of this course into the regular third-year surgery clerkship and these can also be used to introduce GS in the preclinical years.
Keywords: General surgery, COVID-19 response, Surgical education, Medical students, Non-clinical elective, Virtual learning, Distance learning, Undergraduate medical education
Introduction
The COVID-19 pandemic fundamentally disrupted businesses, schools, and lives around the world in a variety of unprecedented ways. In addition to stay-at-home orders from government and public health authorities, on March 17, 2020, the Association of American Medical Colleges issued guidelines, which were subsequently revised on April 14.1 , 2 These set forth strong recommendations that “medical students not be involved in any direct patient care activities” in the majority of clinical settings. Thus, while first-year (M1) and second-year (M2) medical students found themselves attending lectures online, third-year (M3) and fourth-year (M4) students were unable to participate in clinical activities for many weeks. The goal of this project was to sustain medical education via a virtual elective in general surgery (GS), something not offered previously at our institution.
The M3 surgery clerkship is particularly complex in that students must transition from classroom to active learners in a clinical environment, learn basic skills, acclimate to the operating room (OR), and refine their diagnostic and patient-care abilities in the context of a surgical practice. Pre-clinical medical students often have limited exposure to surgery and difficulty establishing education goals, making this transition even more difficult.3 , 4 Preparation before the surgery clerkship begins results in increased student satisfaction with their M3 experience.5, 6, 7 Further, as recent projections show a significant shortage of surgeons to meet growing demand, there is a need for increasing interest and recruitment into GS and surgical subspecialties.8
We created a virtual elective that would allow for direct teaching between faculty members, residents and students while maintaining time for physicians’ clinical responsibilities. We aimed to show students a large breadth of GS, which they might otherwise not see, not only during COVID-19, but during the limitations of service assignment on a regularly conducted clerkship. Our 2-wk elective was targeted to M3s and M4s who had completed the pre-clinical years. During our institution's 8-wk surgical clerkship, there are ample metrics to assess students' knowledge and learning including multiple-choice exams, oral exams, and clinician evaluations. Given that none of the students had yet completed the typical surgical clerkship, in this elective, we sought to provide exposure and preparation to succeed in the clerkship. Students were expected to have basic knowledge about the presentation, anatomy, and pathophysiology of the diseases to be discussed in the course based on their completed human anatomy and organ system-based pre-clinical courses.
Methods
A team of faculty, surgical residents, and medical students created a 2-wk online non-clinical elective that introduced students to the field of GS. The primary goal was to broaden students’ exposure to and elicit interest in GS.
Goals
Daily topics were selected (Table 1 ) to support the overall educational goals:
-
1.
Evaluation of the acutely presenting surgical patient.
-
2.
Evaluation of surgical patients in an ambulatory setting.
-
3.
Understanding the pathophysiology and management of common surgical conditions.
-
4.
Practical elements of perioperative patient management.
-
5.
Comprehensive care of the injured patient.
Table 1.
Topic schedule.
| Week 1 | Week 2 | |
|---|---|---|
| Monday | General Principles of Surgery | Inguinal Hernia |
| Tuesday | Biliary Disease | Ventral Hernia |
| Wednesday | Appendicitis & Diverticular Disease | Anti-Reflux Surgery & Hiatal Hernia |
| Thursday | Bowel Obstruction | Bariatric Surgery |
| Friday | Trauma | Perioperative Management |
Teaching methods
Multiple learning techniques were used to achieve these goals. Each day's assigned topic was selected by a committee of surgery residents and faculty with an aim to choose topics that were broad, common in general surgery, foundational to understanding this field and areas of teaching faculty expertise. Students began each day with self-directed readings about the anatomy, embryology, pathophysiology, presentation, and management relating to the day's topic. To ensure the reading was at an appropriate level for students, readings were sourced by residents and M4 students from surgical textbooks available from commercial online subscription services. (AccessSurgery, McGraw-Hill, New York, NY and ClinicalKey, Elsevier, Inc, Amsterdam, NL). Specific textbooks were chosen whose intended audience was medical students,9, 10, 11 a mix of medical students and surgical trainees,12 and – to challenge students – more advanced textbooks focused on trainees.13, 14, 15 These readings were supplemented with videos demonstrating the corresponding surgical intervention, sourced from the same subscription services as well as curated from a repository of de-identified operative videos maintained by faculty in the Department of Surgery. To supplement self-directed reading and videos, M4s led morning peer lectures on the day's topic (e.g., appendicitis, biliary disease, small bowel obstruction, Table 1). These lectures were reviewed, edited, and approved by the surgical faculty for accuracy and reliability. Lessons covered the relevant anatomy, typical presentation, appropriate management, and potential complications of the surgical condition.
The self-directed readings and peer lectures prepared students for group discussions in the afternoon with faculty and senior residents. Students demonstrated and reinforced what they had learned earlier in the day by answering questions, discussing radiographic findings, and working through patient cases. The faculty then led students through the operative videos highlighting methods for accessing the abdomen, fascial planes, relevant anatomy, and critical steps of the procedure.
Ancillary activities supported the daily core modules, and these were also presented remotely. The first day of the 2-wk cycle also featured a surgical skills lab taught by senior residents and faculty. The lab focused on basic techniques for suturing (simple interrupted stitch with instrument tie and running subcuticular stitch) and knot tying (one-handed and two-handed surgical knots). Each student was provided with a kit of materials to support the surgical skills lab (Table 2 ). Students attended weekly GS morbidity & mortality conference and weekly surgery grand rounds.
Table 2.
Suture lab kit contents.
| Student-supplied | Instruments | Consumables | Durables |
|---|---|---|---|
| Smartphone | Needle driver | 3-0 silk ties | Plastic suture boards |
| Laptop or tablet (optional) | Suture scissor | 3-0 braided suture | Silicone suture pad |
| Forceps | Nitrile gloves | Miniature smartphone tripod |
Collaboration platforms, data source and informatics
All lectures, skills labs, and conferences were conducted using secure videoconferencing using a multi-platform application (Zoom Video Communications Inc, San Jose, CA). Selected sessions were recorded and posted for further review by participants and possible use later during the regular surgery clerkship. A dedicated web-based document repository designed and deployed using an off-the-shelf collaboration platform (SharePoint Online, Microsoft Corporation, Redmond, WA) was used to store and distribute learning resources.
At the end of the elective an anonymous survey was sent to all participants via an online form (Google Forms, Google LLC, Mountain View, CA). This survey was created by fourth year medical students and utilized across multiple other electives running simultaneously within the Department of Surgery. Due to time constraints, this survey was unable to be validated prior to use. Students were asked some basic demographic information and their opinion on how well the learning objectives were met. Students were also asked to indicate how much they understood the field of GS before and after the course, their interest pre- and post-course in a career in GS or in surgery overall. Responses were scored on a four-point Likert scale. Finally, students were encouraged to submit a free-text response to describe aspects of the course that went well and areas for improvement.
Study population
M3s and M4s at Emory University School of Medicine were invited to enroll in the elective during cessation of clinical rotations for COVID-19. The course was completed twice consecutively in early 2020 (20 April – 1 May and 4 May – 15 May) for a total of two student cohorts.
Statistical analysis
Most of the survey data was represented with percentages to describe the distribution of categorical variables (how the course changed understanding of and interest in GS and in a surgical career more broadly). A student's paired t-test was used to detect statistical significance between how understanding of the field of GS changed before and after the course. A two-sided P value of ≤0.05 determined statistical significance. Calculations were performed in Excel version 16.39 (Microsoft Corporation, Redmond, WA).
This study was approved as exempt by the Emory University Institutional Review Board.
Results
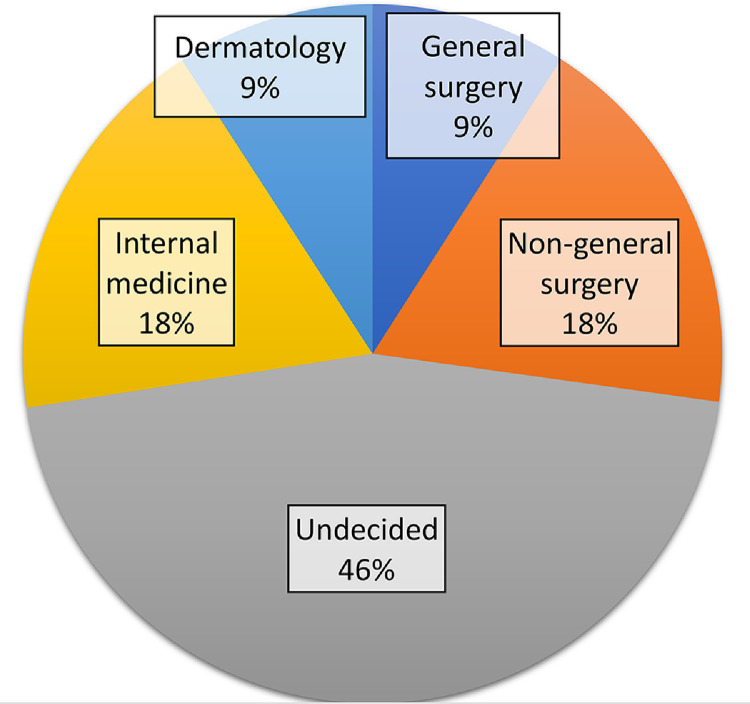
Fourteen medical students participated in this course: eight students in the first course and six students in the second. Eleven students (79%) completed the post-course survey. None of the students had completed their regular M3 surgery clerkship and all students reported feeling comfortable or very comfortable using videoconferencing. In terms of future career, 45% (n = 5) of students were undecided, 18% (n = 2) intended to pursue a surgical specialty other than GS, 9% (n = 1) intended to pursue GS, and the remaining two students were interested in internal medicine and dermatology (Fig. 1 ).
Fig. 1.
Distribution of pre-course student career interest.
On completion of the VSE, 91% of students believed the course had met its learning objectives “very well” or “well” (Fig. 2 ). Before taking this elective and compared to their peers’ understanding of GS, only 27% (n = 3) reported a “good understanding,” and no students a “very good understanding” of GS. After the course, 100% of students reported a “good” or “very good” understanding (Table 3 ), a statistically significant difference (P = 0.0003).
Fig. 2.
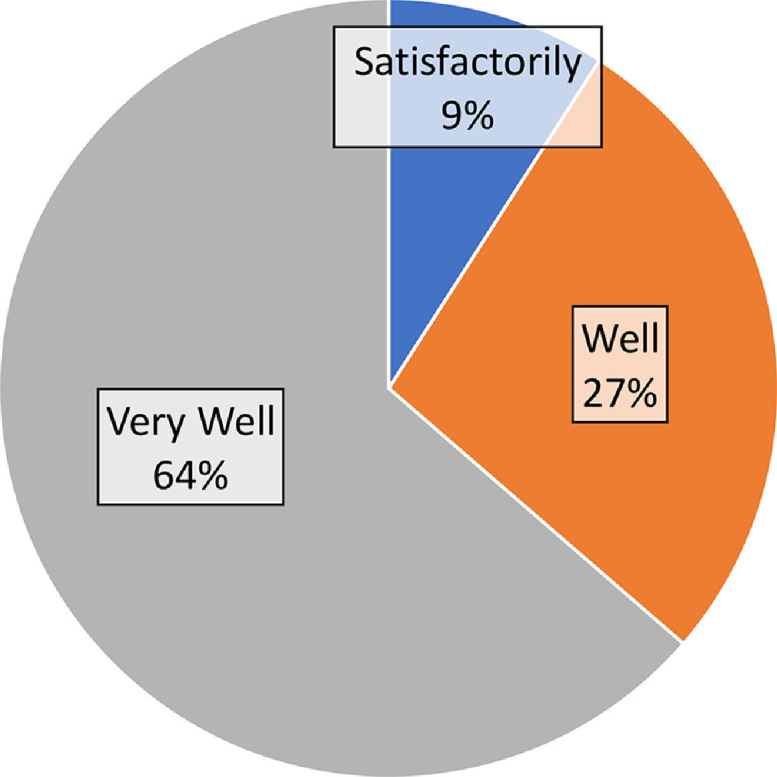
Student rating of how the virtual surgical elective met its learning objectives.
Table 3.
Student rating of understanding of the field of general surgery pre-course and post-course.
| Pre-course | Post-course | |
|---|---|---|
| Poor | 36% | 0% |
| Fair | 36% | 0% |
| Good | 27% | 91% |
| Very good | 0% | 9% |
With respect to career planning, seven (63%) students reported being “interested” or “very interested” in GS (Table 4 ) prior to the course. Upon completion of the course, one student reported “decreased interest,” three (27%) reported “no change,” and the remaining seven (64%) reported “increased” interest (Table 5 ). When surveyed on their interest in pursuing any field of surgery, 63% of students reported themselves “interested” or “very interested” prior to the course (Table 4). After completing the VSE, no student reported decreased interest, 55% (n = 6) reported “no change” in interest, and 45% (n = 5) reported “increased” or “greatly increased” interest in pursuing a career in any surgical field (Table 5).
Table 4.
Pre-course interest in any surgical field and general surgery.
| Any surgery | General surgery | |
|---|---|---|
| Uninterested | 18% | 27% |
| Indifferent | 18% | 9% |
| Interested | 18% | 36% |
| Very interested | 45% | 27% |
Table 5.
Post-course interest change in any surgical field and general surgery.
| Any surgery | General surgery | |
|---|---|---|
| Decreased interest | 0% | 9% |
| No change | 55% | 27% |
| Increased interested | 36% | 64% |
| Greatly increased interested | 9% | 0% |
Students enjoyed the faculty-lead sessions with a combination of lecture, operative video, and discussion of patient cases. Interactive engagement, comprehensive discussion including surgical indication, pre-operative care, and operative goals, and a Socratic style of teaching were appreciated by students as well as the faculty's “meeting us where we are.” Finally, students enjoyed the peer lectures led by fourth year medical students as they provided a “low-pressure setting” for learning.
The most frequently mentioned area for improvement was regarding self-directed reading. Students found that the volume of assigned reading was inconsistent and at times too great. Finally, students were interested in additional skills labs, more peer-led lectures, and fewer days discussing hernias.
Discussion
In March 2020, the American College of Surgeons formed a committee to “explore ways of innovating and improving surgical education in the aftermath of COVID-19" and closed their recommendations with “the pandemic has allowed us to explore ways in which virtual technology brings us closer together as a community.”16Various accommodations have been described in the literature supporting undergraduate medical education in the context of the pandemic17, 18, 19 and virtual interventions have been highlighted as a compelling adaptation.20 At our institution, a collaboration of M4s, surgical residents, faculty, and department administration was able to plan and quickly implement this novel type of undergraduate medical education. In addition to providing supplementary educational content, the VSE provided unique opportunities to increase specific understanding of and interest in surgical practice in general and GS in particular. We believe this effort has implications in surgical education beyond those of COVID-19.
Nearly all of the students surveyed (91%) felt the course met its learning objectives “well” or “very well” and self-reported understanding of GS increased significantly. Participating students represented a diverse cross-section of our student body and only 27% were interested in surgery prior to the course. In considering any field of surgery, no student reported a decrease in interest and nearly half reported either an “increased” or “greatly increased” interest after the course. In addition, 64% reported an “increase” in interest in GS specifically.
Our results suggest an elective can increase interest in a specialty and impact career planning. This has several implications for medical education, the first being in the recruitment of students and specialty choice. With projections reporting a shortfall of as many as 23,400 surgeons by 2032, opportunities to increase exposure and interest may be of growing importance in order to recruit students and meet increasing demand.8 As an elective course to complement required clerkships, we viewed our course more as one of those opportunities to invigorate potential future surgeons, life-long learners, and work to fill the shortfall rather than further testing the knowledge of students in traditional manners.
Although our VSE represents a limited alternative to a clinical rotation on a GS service at a teaching hospital, several elements stand out in our implementation. Teaching methods that were particularly successful included faculty-led sessions using a Socratic style of teaching, operative videos focusing on fascial planes and relevant anatomy, and case presentations. Students appreciated the “low-stakes” peer lectures in the morning before meeting with faculty. Moving forward, we feel that surgical education beyond COVID-19 must transition more towards these various teaching methods. Peer lectures may be a practical replacement for faculty-presented didactic lectures and consequently ease scheduling conflicts. This in turn may allow expert clinicians, faculty, and residents to maintain greater focus on clinical reasoning, case scenarios, and technical skill acquisition. The operative videos were well-received and another valuable opportunity to apply our elective efforts further. The narration and discussion along with the video will provide students on the clerkship with more unique individualized pre-operation preparatory or post-operation supplementary learning materials.
The virtual suture skills labs developed in this course were an innovative way to teach surgical skills. The students expressed not only increased understanding in techniques but also a desire for more skills labs. The ability to do this remotely allows more exposure and opportunities for suture skill-building, an area of surgical education many students often feel weak, unprepared, and wish for more time in. We hope to implement these virtual labs into surgical clerkships to not only allow more practice outside of the OR but also free up flexibility in scheduling such opportunities.
Due to shifting COVID-19 restrictions in place at our institution, only two iterations of the course could be implemented before students returned to the clinical services. Future refinements of this elective would include reducing self-directed reading to ensure appropriate content level and equal amount is consistently assigned each day, more peer-led lectures and surgical skills labs, combining inguinal and ventral hernia content into a single session. Additional topics could include common surgical disease in thoracic, vascular, or colorectal surgery including esophageal and lung cancer, aortic and peripheral artery disease, or colorectal malignancies. The future curriculum's topical areas would include a balance of common general surgery topics as well as some surgical pathologies of the surgical subspecialties.
Limitations of this observational study include the small population of self-selected students enrolled at a single institution. Additionally, because of the circumstances under which the elective was created and run, there was no official control group consisting of students who took the elective with no prior interest in surgery. The students’ baseline interest in the field and in a career in general surgery prior to taking the elective served as the study's point of comparison for how well the course increased surgical interest. Statistical inferences and persistence of interest would therefore require replication in a larger and/or unselected cohort. However, as proof of concept, the VSE has demonstrated several useful and replicable elements regarding virtual instruction in GS. The core content appears compatible with online instruction and this approach may be useful in the future to prepare preclinical students and/or orient students new to the surgery clerkship. Unexpectedly, we also found that the collaboration between the M4s, residents, and faculty brought the surgery education community at Emory closer. The methods described here could be applied to future online courses, offered in conjunction with in-person clinical learning and should be studied for its possible application in other areas of medical education.
Acknowledgments
Acknowledgment
The authors have no external funding sources to disclose; this research was supported by the Department of Surgery and the Emory University School of Medicine. In-kind donations of supplies were provided under an educational grant by Ethicon, Inc (Johnson & Johnson Medical Devices, Somerville, NJ, Grant ID #362503) and W.L. Gore & Associates, Inc (Newark, DE) for suture and suture boards respectively.
Disclosure
The authors have no significant personal or financial relationships to disclose that might influence the materials or conclusions presented here.
Authors’ Contributions
Mr. Grady participated in the conception and design, the analysis, and interpretation of data as well as drafting and critical revision of the manuscript for important intellectual content. Ms. Gallo participated in the conception and design, the analysis, and interpretation of data as well as drafting and critical revision of the manuscript for important intellectual content. Ms. Lin participated in the conception and design, the analysis, and interpretation of data as well as drafting and critical revision of the manuscript for important intellectual content. Mr. Magod participated in the conception and design, the analysis, and interpretation of data as well as drafting and critical revision of the manuscript for important intellectual content. Dr. Coulthard participated in the conception and design, the analysis, and interpretation of data as well as drafting and critical revision of the manuscript for important intellectual content. Dr. Flink participated in the conception and design, the analysis, and interpretation of data as well as drafting and critical revision of the manuscript for important intellectual content. Dr. Knauer participated the conception and design, analysis, and interpretation of data as well as drafting and critical revision of the manuscript for important intellectual content. Dr. Winer participated in the conception and design, the analysis, and interpretation of data as well as drafting and critical revision of the manuscript for important intellectual content. Dr. Papandria participated in the conception and design, the analysis, and interpretation of data as well as drafting and critical revision of the manuscript for important intellectual content. Dr. Pettitt participated in the conception and design, acquisition, analysis, and interpretation of data as well as drafting and critical revision of the manuscript for important intellectual content.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jss.2021.08.020.
Appendix. Supplementary Materials
References
- 1.Prescott JE. AAMC; 2020. Important Guidance for Medical Students on Clinical Rotations During the Coronavirus (COVID-19) Outbreak.https://www.aamc.org/news-insights/press-releases/important-guidance-medical-students-clinical-rotations-during-coronavirus-covid-19-outbreak |. PublishedAccessed June 30, 2020. [Google Scholar]
- 2.Whelan A, Prescott JE, Young G, Catanese VM, McKinney R. Guidance on medical students’ participation in direct patient contact activities. https://www.aamc.org/media/42776/download. Published 2020. Accessed June 30, 2020.
- 3.Lyons-Warren AM, Kirby JP, Larsen DP. Student views on the role of self-regulated learning in a surgery clerkship. J Surg Res. 2016;206:273–279. doi: 10.1016/j.jss.2016.08.022. [DOI] [PubMed] [Google Scholar]
- 4.McKinley SK, Kochis M, Cooper CM, et al. Medical students’ perceptions and motivations prior to their surgery clerkship. Am J Surg. 2019;218:424–429. doi: 10.1016/j.amjsurg.2019.01.010. [DOI] [PubMed] [Google Scholar]
- 5.Patel MS, Khalsa B, Rama A, et al. Early intervention to promote medical student interest in surgery and the surgical subspecialties. J Surg Educ. 2013;70:81–86. doi: 10.1016/j.jsurg.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Li JZ, Chan SCY, Au M, et al. Review of a medical student-run surgery lecture series and skills lab curriculum. Can J Surg. 2014;57:152–154. doi: 10.1503/cjs.002913. Canadian Medical Association. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miller S, Shipper E, Hasty B, et al. Introductory surgical skills course: technical training and preparation for the surgical environment. MedEdPORTAL J Teach Learn Resour. 2018;14:10775. doi: 10.15766/mep_2374-8265.10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dall T, Reynolds R, Jones K, Chakrabarti R, Iacobucci W. The Complexities of Physician Supply and Demand. Washington, DC; 2019. https://www.aamc.org/system/files/2020-06/stratcomm-aamc-physician-workforce-projections-june-2020.pdf. Accessed December 7, 2020.
- 9.de Virgilio C, Frank PN, Grigorian A, editors. Surgery. Springer New York; New York, NY: 2015. [DOI] [Google Scholar]
- 10.Campbell AR, Toy EC, Liu TH, editors. Case Files Surgery. 4th ed. McGraw Hill Medical; New York: 2012. [Google Scholar]
- 11.Doherty GM, editor. Current Diagnosis & Treatment: Surgery. 15e ed. McGraw-Hill; New York: 2020. https://www.accesssurgery.mhmedical.com/content.aspx?bookid=2859. [Google Scholar]
- 12.Brunicardi FC, Andersen DK, Billiar TR, et al., editors. Schwartz's Principles of Surgery. 11e ed. McGraw-Hill; New York: 2019. https://accesssurgery.mhmedical.com/content.aspx?bookid=2576, Accessed June 14, 2020. [Google Scholar]
- 13.Maingot R, Zinner M, Ashley SW, Hines OJ, editors. Maingot's Abdominal Operations. 13e ed. McGraw-Hill; New York: 2019. https://accesssurgery.mhmedical.com/content.aspx?bookid=2546, Accessed June 14, 2020. [Google Scholar]
- 14.Townsend CM, Beauchamp RD, Evers BM, Mattox KL. 20th ed. Elsevier; Philadelphia: 2016. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. https://www.clinicalkey.com/#!/browse/book/3-s2.0-C20130186151, Accessed June 14, 2020. [Google Scholar]
- 15.Moore EE, Feliciano DV., Mattox KL, editors. Trauma. 8e ed. McGraw-Hill; New York: 2017. https://accesssurgery.mhmedical.com/content.aspx?bookid=2057, Accessed June 14, 2020. [Google Scholar]
- 16.American College of Surgeons. ACS Academy of Master Surgeon Educators Committee addresses challenges and opportunities in surgical training during COVID-19. ACS Bulletin Brief - Education. https://www.facs.org/publications/bulletin-brief/051920/education. Published May 19, 2020. Accessed June 14, 2020.
- 17.Prigoff J, Hunter M, Nowygrod R. Medical Student Assessment in the time of COVID-19. J Surg Educ. 2020 doi: 10.1016/j.jsurg.2020.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sandhaus Y, Kushnir T, Ashkenazi S. Electronic distance learning of pre-clinical studies during the COVID-19 pandemic: a preliminary study of medical student responses and potential future impact. Isr Med Assoc J. 2020;8:423–427. http://www.ncbi.nlm.nih.gov/pubmed/32812716 Accessed August 24, 2020. [PubMed] [Google Scholar]
- 19.Looi JCL, Bonner D, Maguire P, et al. Flattening the curve of COVID-19 for medical education in psychiatry and addiction medicine. Australas Psychiatry. 2020 doi: 10.1177/1039856220946647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tabatabai S. COVID-19 impact and virtual medical education. J Adv Med Educ Prof. 2020;8:140–143. doi: 10.30476/jamp.2020.86070.1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.