Abstract
The purpose of the study was to examine trends in COVID-19 cases, related deaths, and staffing shortages in nursing homes (NH) by rural and urban status from May 2020 to Feb 2021. Generalized linear mixed models with state-fixed effects were used to estimate the interaction effect of study period and rural/urban status on having at least: one COVID-19 case, one related death, and/or at least one week of staffing shortage using the NH COVID-19 data spanning the 40-week period. The findings revealed shortages in staff, particularly direct care providers, were greatly accelerated in rural NHs as the pandemic wore on over time. Conversely, staffing shortages in urban NHs were relatively stable despite the fluctuating COVID-19 cases over the same time period. The findings highlight the need of identifying effective strategies that prevent rural NHs from encountering staffing deficits in response to long-lasting natural disasters such as the COVID-19 pandemic.
Keywords: COVID-19; Rural and urban status; Staffing, and nursing home
Introduction
The COVID-19 pandemic inflicted unprecedented hardship on US nursing homes (NHs) including high COVID-19 infections and mortality rates among residents, as well as disruption in day-to-day operations.1, 2 - 3 Although the impacts were myriad, early reports noted pandemic-related shortages in staffing and on-hand supplies, which may have exacerbated the ability of NHs to respond to the event itself, in addition to magnifying persistent pre-existent staffing-related challenges.4, 5, 6 - 7
The negative impacts of the COVID-19 pandemic may be even more pronounced in disadvantaged or low quality NHs such as those located in rural areas of the US given their unique challenges in meeting resident care needs.7 , 8 For example, staffing shortages and frequent turnover among other infrastructural and operational challenges were well-documented in rural NHs prior to the pandemic when compared to urban NHs.9 Furthermore, rural populations are older on average than those in urban areas, with complex-health conditions and higher rates of disability.10 This may not only make them potentially more susceptible to COVID-19 infections, but also make infectious outbreaks harder to contain, and thus more likely to weaken the rural healthcare system resilience over time.
To date, only a few studies have investigated geographic location in relation to COVID-19 impact on NHs,6 , 7 , 11 , 12 with inconclusive findings. Two studies examined the role of geographical location using data collected in May, 2020, from a subset of states in US.11 , 12 Both studies found that NHs located in urban locations were associated with an increased probability of having at least one COVID-19 case or a higher likelihood of more COVID-19 cases. Another study found that metropolitan status of NHs was not related to staffing shortages during COVID-19 pandemic.6 Conversely, a similarly conducted study reported higher rates of staffing shortages clustered in parts of the South and Midwest where the proportion of rural areas is relatively higher than in other US locations.7 Moreover, despite the potential importance of these findings, these results may not fully reflect changes that were developed over the course of the year because most of these studies were conducted in real time using only a few weeks of COVID-19 data collected in early days of the pandemic. In response, we sought to examine how COVID-19 infections, related deaths, and staffing shortages changed over time in NHs by rural/urban status using compiled Centers for Medicare and Medicaid Services (CMS) NH Compare COVID-19 data spanning a continuous 40-week period.
Methods
Study design, data source, and sample
This cross-sectional time-series study used large healthcare administrative datasets publicly available from CMS, Health Resources and Services Administration (HRSA), and NY Times websites. These include CMS NH COVID-19 compiled data from 5/25/2020 to 2/28/2021 containing information about COVID-19 cases, related deaths, and four types of staffing shortages; NH provider information files for facility characteristics; and the latest available NH Payroll-Based Journal data (4/1-6/30, 2020) for staffing level information from CMS. After linking files by facility identifiers, these data were merged with Area Health Resource Files (AHRF) from HRSA, 2019-202013 to permit specification of regional characteristics. Data were also linked with NY Times coronavirus case data14 (accessed in March, 2021) to identify county-level COVID-19 cases using county zip codes.
We initially identified 15,393 NHs that submitted at least one weekly report of COVID-19 cases, related deaths, and four types of staffing shortages between 5/25/2020 and 2/28/2021. Reports from 254 NHs were excluded due to failure to pass the data quality assurance check imposed by CMS.15 Next, we divided the cumulative 40-week reports into four groups by 10-week intervals in order to derive more stable estimates. The breakdown for the total number of NHs reporting at least one report each time period was as follows: 14,901 NHs submitted at least one weekly report during Period 1 (5/25/2020-8/2/2020); 14,889 NHs reported during Period 2 (8/3/2020-10/11/20); 14,872 NHs reported during Period 3 (10/12/20-12/20/20), and 14,853 NHs reported during Period 4 (12/23/20-2/28/21), resulting in a total of 59,515 aggregated reports across all reporting periods and representing data from 15,139 unique NHs.
Measures
The following facility-level dependent variables were specified: having at least one COVID-19 case, at least one COVID-related death, and at least one reported week of staffing shortages in a given period. For our purpose, study period served as the primary independent variable and was grouped into four 10-week intervals (Periods 1-4) as previously described. Rural/urban status also served as a key variable of study interest and was defined using the Rural-Urban continuum available from AHRF. Other regional characteristics included market-level provider availability captured as the number of registered nurses (RNs), licensed practical nurses (LPNs), and certified nursing assistants (CNAs) per 100,000 population aged 65+, by county. We also calculated a variable that captured a single week of county-level COVID-19 cases per 100,000 population immediately prior to each period of the NH data, under the assumption that COVID-19-related cases in NHs reflect broader area infection rates.
Additional covariates were included to adjust for facility operating differences. Facility size was measured as the number of beds and categorized into three groups: ≤49, 50-149, and 150+ beds. Other organizational characteristics included ownership (profit, not-for-profit, or government affiliation), overall five-star quality rating, hospital-affiliation status, chain-affiliation status, the percentage of resident stays reimbursed by Medicare and Medicaid, and case-mix. As a measure of facility case-mix, we used the expected hours of care provided per resident day available from the CMS NH Compare provider information file.
Statistical analyses
SAS version 9.4 and STATA version 13 were used for data merging and analyses. First, bivariate statistics were used to describe facility and regional characteristics of NHs by rural/urban status. Then, we plotted the proportion of NHs that reported at least one COVID-19 case, at least one related death, and staffing shortages by rural/urban status to visualize the weekly trends in those variables in rural vs urban NHs. For the main analyses, we estimated the likelihood of having at least one COVID-19 case, one COVID-related death, or at least one reported week of staffing shortages in rural NHs compared to that in urban NHs over four time periods. Generalized linear mixed models were used to account for repeated measures of outcomes from individual NHs over time and state-clustering effects after adjusting for facility and regional characteristics. We also tested the interaction effect between study period and rural/urban status to examine if the changes over time in rural NHs are significantly different from the ones in urban NHs.
Results
Characteristics of rural/urban NHs
Approximately 4,228 NHs (28%) were located in rural regions of the US (Table 1 ). Rural NHs tended to be smaller and more often affiliated with a hospital or owned by non-profit/government organizations in comparison with their urban counterparts (n=10,911). Baseline RN, LPN, and CNA HPRDs in rural NHs, which was measured right before COVID-19 related staffing shortage data were collected, were each significantly lower than those in urban NHs (p<0.001). The market-level direct care and medical provider availabilities were also lower in rural areas (p<0.001), except for a higher number of LPNs in 100,000 population (66.07 vs 32.84, p<0.001). In comparison with rural NHs, urban NHs had higher case-mix measured as expected HPRD (3.28 vs 3.15, p<0.001), as well as higher Medicare (22.99% vs 19.18%, p<0.001) and Medicaid (12.21% vs 9.50%, p<0.001) census rates.
Table 1.
Characteristics of US nursing homes (NHs) by rural and urban areas (n=15,139)1
| Rural NHs (n=4,228) | Urban NHs (n=10,911) | p-value | ||||||
|---|---|---|---|---|---|---|---|---|
| Facility characteristics | ||||||||
| Facility size (n, %) | <0.001 | |||||||
| Small (bed no.<50) | 1,050 | 19.23 | 2,461 | 26.21 | ||||
| Medium (bed no. ≥50 and <150) | 3,909 | 71.59 | 5,088 | 54.20 | ||||
| Large (bed no.≥150) | 501 | 9.18 | 1,839 | 19.59 | ||||
| Ownership (n, %) | <0.001 | |||||||
| Profit | 3,353 | 66.59 | 5,393 | 71.19 | ||||
| Government affiliated | 450 | 8.94 | 333 | 4.40 | ||||
| Non-profit | 1,232 | 24.47 | 1,850 | 24.42 | ||||
| Hospital affiliation (n, %) | <0.001 | |||||||
| Yes | 297 | 5.9 | 228 | 3.01 | ||||
| No | 4,737 | 94.1 | 7,340 | 96.99 | ||||
| Chain affiliation (n, %) | 0.11 | |||||||
| Yes | 2,990 | 59.41 | 4,387 | 57.98 | ||||
| No | 2,043 | 40.59 | 3,179 | 42.02 | ||||
| Percent of residents covered by Medicaid (mean, SD2) | 49.03 | 19.18 | 47.04 | 22.99 | <0.001 | |||
| Percent of residents covered by Medicare (mean, SD) | 10.63 | 9.50 | 13.71 | 12.21 | <0.001 | |||
| Overall quality rating (mean, SD) | 3.21 | 1.39 | 3.30 | 1.42 | 0.11 | |||
| Expected staffing (case-mix)* (mean, SD) | 3.15 | 0.26 | 3.28 | 0.31 | <0.001 | |||
| Staffing level | ||||||||
| Registered nurse (RN) HPRD3 | 0.45 | 0.41 | 0.54 | 0.50 | <0.001 | |||
| Licensed practical nurse (LPN) HPRD | 0.77 | 0.36 | 0.89 | 0.39 | <0.001 | |||
| Certified nursing assistant (CNA) HPRD | 2.14 | 0.58 | 2.25 | 0.62 | <0.001 | |||
| Regional characteristics | ||||||||
| Number of aides per 100,000 population (mean, SD) | 165.31 | 196.84 | 182.72 | 136.79 | <0.001 | |||
| Number of LPNs per 100,000 population (mean, SD) | 66.07 | 74.09 | 32.84 | 39.97 | <0.001 | |||
| Number of RNs per 100,000 population (mean, SD) | 504.60 | 427.77 | 634.84 | 415.01 | <0.001 | |||
| Number of APPs4 per 100,000 population (mean, SD) | 175.04 | 123.73 | 213.35 | 112.99 | <0.001 | |||
| Number of MDs5 per 100,000 population (mean, SD) | 171.25 | 193.69 | 372.06 | 224.98 | <0.001 | |||
Note. 1. Data sources: Nursing Home Compare COVID-19 data from Centers for Medicare and Medicaid Services, 2020-2021, Area of Health Resource File from HRSA, and New York Times COVID-19 county level data accessed in 3/21/2021; 2. SD means standard deviation, 3. HPRD means hours per resident day; 4. APP means advanced practice provider; 5. MD means medical doctor; p<0.05 in bold face
Trends in COVID-19 cases, related deaths, and staffing shortages by rural/urban status
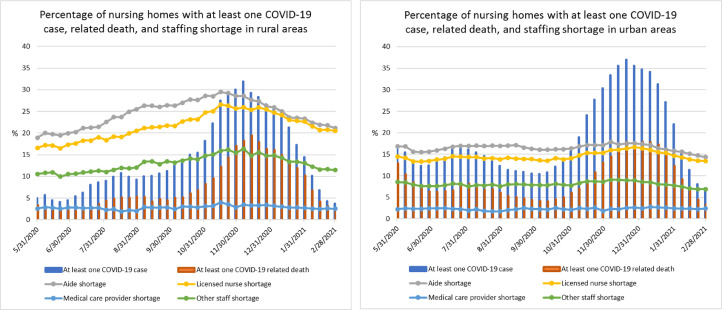
The proportion of rural NHs reporting staffing shortages was higher than that of urban NHs, with a gradual increase until mid-November 2020 and a decrease afterwards, corresponding with trends in the proportion of NHs with at least one COVID-19 case. Conversely, staffing shortages in urban NHs were lower than those in rural NHs and were relatively stable over time, despite the fluctuating COVID-19 cases over the same period. The proportion of NHs reporting medical provider shortages was less than 5 % in both rural and urban areas. This was consistently lower and did not change much over time in comparison to reported shortages in aides, licensed nurses, and other staff (Fig. 1 ).
Fig. 1.
Trends in nursing homes with at least one COVID-19 case, at least one related death, and staffing shortages weekly reported from 5/25/2020 to 2/28/2021 (Nursing Home COVID-19 data from Centers for Medicare and Medicaid Services, n=15,139)
Results from the adjusted model suggest that the odds of having at least one COVID-19 case were significantly lower among rurally located NHs (AOR=0.43, 95% CI=0.39, 0.47). Likewise, among rural NHs, having at least one COVID-related death (AOR=0.45, 95% CI=0.40, 0.51), and at least one week of nurse aide shortages (AOR=0.77, 95% CI=0.66, 0.91) were significantly lower in comparison to otherwise similar NHs located in urban areas (Table 2 ). However, when the interaction effect between study period and rural/urban status was examined in the same model, there was a significantly higher likelihood of having at least one COVID-19 case, related death, and shortages in aides, licensed nurses, and other staff in later periods than in Period 1 in rural NHs, compared to urban NHs. Not surprisingly, NHs with at least one COVID-19 case had significantly higher odds of having all four types of staff shortages during the pandemic. There was no difference in odds of having medical provider shortages across the periods in rural NHs compared to urban NHs.
Table 2.
Factors affecting COVID-19 cases, related deaths, and staffing shortages in US nursing homes between 5/25/2020 and 2/28/2021 1
| At least one COVID-19 case |
At least one COVID-19 related death |
Shortage of aides during at least one week |
Shortage of licensed nurses during at least one week |
Shortage of medical providers during at least one week |
Shortage of other staff during at least one week |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AOR2 | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | ||
| Rural/urban status (reference=urban) | |||||||||||||
| Rural area | 0.43 | (0.39, 0.47) | 0.45 | (0.40, 0.51) | 0.77 | (0.66, 0.91) | 0.89 | (0.75, 1.04) | 1.10 | (0.95, 1.28) | 0.90 | (0.78, 1.05) | |
| Period (reference=Period 1)3 | |||||||||||||
| Period 2 | 0.72 | (0.67, 0.77) | 0.57 | (0.53, 0.63) | 0.88 | (0.80, 0.98) | 0.88 | (0.80, 0.97) | 0.94 | (0.83, 1.05) | 0.92 | (0.83, 1.01) | |
| Period 3 | 2.84 | (2.63, 3.07) | 0.85 | (0.79, 0.93) | 0.82 | (0.74, 0.90) | 0.94 | (0.85, 1.04) | 1.03 | (0.92, 1.16) | 0.96 | (0.86, 1.06) | |
| Period 4 | 2.29 | (2.12, 2.47) | 1.33 | (1.23, 1.45) | 0.69 | (0.62, 0.76) | 0.85 | (0.77, 0.94) | 1.74 | (0.96, 1.20) | 0.79 | (0.71, 0.88) | |
| Period*rural/urban status | |||||||||||||
| Period 2*rural | 2.45 | (2.18, 2.75) | 2.07 | (1.77, 2.41) | 1.56 | (1.34, 1.82) | 1.33 | (1.14, 1.55) | 0.98 | (0.82, 1.17) | 1.23 | (1.05, 1.43) | |
| Period 3*rural | 3.04 | (2.68, 3.44) | 3.10 | (2.69, 3.57) | 1.94 | (1.66, 2.26) | 1.53 | (1.32, 1.79) | 1.07 | (0.90, 1.27) | 1.43 | (1.23, 1.66) | |
| Period 4*rural | 1.74 | (1.54, 1.96) | 2.23 | (1.93, 2.57) | 1.36 | (1.17, 1.59) | 1.19 | (1.02, 1.39) | 0.85 | (0.71, 1.01) | 1.22 | (1.04, 1.42) | |
| At least one COVID-19 case in a given period | . | . | 14.79 | (13.82, 15.83) | 1.92 | (1.84, 2.11) | 2.02 | (1.89, 2.16) | 1.25 | (1.16, 1.34) | 1.61 | (1.50, 1.72) | |
| Facility size (reference=small) | |||||||||||||
| Medium | 2.42 | (2.22, 2.64) | 1.55 | (1.40, 1.74) | 0.74 | (0.61, 0.91) | 0.83 | (0.68, 1.01) | 1.04 | (0.88, 1.22) | 0.92 | (0.77, 1.10) | |
| Large | 5.06 | (4.57, 5.62) | 2.21 | (1.94, 2.50) | 0.68 | (0.53, 0.86) | 0.77 | (0.61, 0.97) | 1.00 | (0.83, 1.22) | 0.80 | (0.65, 0.99) | |
| Profit status (reference=profit) | |||||||||||||
| Non-profit | 0.99 | (0.94, 1.06) | 1.06 | (1.00, 1.15) | 1.15 | (0.99, 1.33) | 1.02 | (0.89, 1.17) | 1.01 | (0.90, 1,13) | 1.02 | (0.90, 1.16) | |
| Government-affiliated | 0.93 | (0.84, 1.04) | 1.00 | (0.89, 1.13) | 1.21 | (0.95, 1.33) | 1.18 | (0.93, 1.49) | 1.02 | (0.85, 1.24) | 1.09 | (0.88, 1.34) | |
| Hospital affiliation (reference=non-hospital based) | |||||||||||||
| Hospital-based | 0.81 | (0.71, 0.93) | 0.79 | (0.67, 0.93) | 1.19 | (0.86, 1.64) | 1.20 | (0.88, 1.65) | 0.98 | (0.76, 1.26) | 0.93 | (0.70, 1.23) | |
| Chain affiliation (reference=non-chain affiliated) | |||||||||||||
| Chain affiliated | 1.11 | (1.05, 1.17) | 0.99 | (0.93, 1.04) | 0.67 | (0.60, 0.75) | 0.71 | (0.64, 0.80) | 0.91 | (0.83, 0.99) | 0.80 | (0.72, 0.88) | |
| Expected staffing (case-mix). | 1.31. | (1.18, 1.44) | 1.07 | (0.95, 1.20) | 0.49 | (0.38, 0.63) | 0.45 | (0.35, 0.53) | 0.66 | (0.54, 0.80) | 0.46 | (0.37, 0.57) | |
| Percent of residents under Medicare. | 1.00 | (1.00, 1.01) | 1.00 | (0.99, 1.00) | 0.98 | (0.98, 0.99) | 0.99 | (0.98, 0.99) | 0.99 | (0.99, 1.00) | 0.99 | (0.99, 0.99) | |
| Percent of residents under Medicaid. | 0.99 | (0.99, 1.00) | 1.00 | (0.99, 1.00) | 1.00 | (1.00, 1.01) | 1.00 | (0.99, 1.00) | 1.00 | (0.99, 1.00) | 1.00 | (0.99, 1.00) | |
| Overall five star rating. | 0.98 | (0.97, 1.00) | 1.00 | (0.98, 1.02) | 0.83 | (0.80, 0.87) | 0.81 | (0.78, 0.84) | 0.91 | (0.88, 0.94) | 0.87 | (0.84, 1.34) | |
| RN HPRD4. | 0.83 | (0.77, 0.89) | 0.84 | (0.77, 0.91) | 0.81 | (0.68, 0.96) | 0.78 | (0.66, 0.93) | 1.02 | (0.90, 1.16) | 1.01 | (0.87, 1.17) | |
| LPN HPRD. | 1.08 | (0.99, 1.17) | 0.88 | (0.80, 0.96) | 0.87 | (0.72, 1.06) | 0.82 | (0.68, 0.99) | 1.02 | (0.88, 1.19) | 0.97 | (0.82, 1.15) | |
| CNA HPRD. | 1.05 | (0.99, 1.10) | 0.97 | (0.91, 1.02) | 0.86 | (0.77, 0.97) | 0.98 | (0.87, 1.10) | 1.05 | (0.96, 1.15) | 0.91 | (0.82, 1.01) | |
Note. 1. Data source: Nursing Home Compare COVID-19 data from Centers for Medicare and Medicaid services, 2020-2021, Area of Health Resource File from HRSA, and New York Times COVID-19 county level data accessed in 3/21/2021; 2. AOR means adjusted odds ratio; Lagged variables, regional workforce variables were additionally adjusted; 3. Period 1 covers Period 2 covers 8/3/2020-10/11/2020, Period 3 covers 10/12/2020-12/20/2020, and Period 4 covers 12/21/2020-2/28/2021; 4. The reporting period for the staffing level data was 4/1-6/30/2020 and HPRD means hours per resident day.
Discussion
Using CMS NH COVID-19 data compiled weekly from May, 2020 to February, 2021, we examined trends in the proportion of NHs having at least: one COVID-19 case, one related death, and/or at least one week of having reported shortages in four types of staffing in rural NHs compared to urban NHs. Interestingly, rurality itself was not negatively associated with COVID-19 infections, related deaths, or staffing shortages in NHs in adjusted estimates combining all four time-periods, with only a minimal difference in staffing shortages between rural and urban NHs at the beginning of the study period. This finding is consistent with some of the earlier NH COVID-19 outbreak morbidity, mortality, and NH staffing related data.6 , 11 , 12 However, when we examined fluctuation in staffing over time, greater change in staffing shortages were observed, particularly in direct care staffing levels among rural NHs, which suggested staffing shortages were greatly accelerated in comparison with facilities located in urban areas. Plausibly, our findings suggest that rural NH human resource infrastructure capacity was less able to endure the prolonged caregiving intensity, which far exceeded normal demands, as the impact of the COVID-19 pandemic wore on and extended beyond one year. Pre-existing human and material resource deficits persistent in rural NHs, including inadequate pre-pandemic staffing-levels;16 lower BSN educated RN staffing,17 , 18 and the need for well-trained rural nursing personnel19 , 20 may have exacerbated staffing shortages over time and in response to increasing workload related to COVID-19 infections.
Another possible reason related to accelerated staffing shortages in rural NHs during the pandemic was absence of family or friend support in NHs caused by COVID-19 community lock-out. A previous study reported that family visitors to rural NHs were more likely to provide direct care help and see staff as sharing similar goals, compared to urban family members who played more of purely third-party staff “watchdog” role and were less likely to see themselves as part of the care team.21 Presumably, this absent family support in rural NHs during the lock-out had a more significant impact on COVID-19 related NH workload leading to staff work overload, stress and turnover. In other words, as the strain of the pandemic wore on, the impact was felt more acutely among staff in rural NHs as replacement staff were scarcer and the contribution of family members to resident care was prohibited.
A majority of research and media reports about COVID-19 has focused on urban areas due to their high COVID-19 caseloads.22 Yet, findings from this study suggest that the higher volume of COVID-19 infections in urban facilities did not contribute much to the urban NH workforce shortages during the pandemic. Undoubtedly, urban NHs also must have experienced increased pandemic work-related stress, work-overload, and even higher turnover rates as COVID-19 was spreading in urban long-term care communities. These challenges, however, may have been mitigated by various available local resources, including a better ability to train and equip existing staff for the outbreak management, to relieve over-burdened staff, or to find replacements when necessary.
The findings indicated that the market-level direct care provider availability in urban areas was significantly higher than that in rural areas prior to COVID-19 potentially making it easier for urban NHs to find replacement staffing. Conversely, rural areas had lower overall market-level provider availability except for higher LPN availability. The higher LPN availability in rural areas would have increased a chance for rural NHs to hire additional LPNs in order to substitute shortages in direct care providers. However, the higher LPN staffing level without adequate RN or CNA staffing has been frequently linked to negative resident care outcomes in previous studies.18 , 23 Thus, findings from this study suggest a complex interaction between market forces across the rural-urban divide and the availability of replacement staffing during the pandemic.
Inadequate NH staffing levels may lead to poor infection control,4 higher confirmed COVID-19 cases,12 , 24 and weakened NH capacity to provide essential ongoing care not directly related to COVID-19.18 , 25 Our study findings that pre-pandemic staffing levels were negatively associated with NH's self-reported staffing shortages during the course of the pandemic re-emphasize the pressing need to address pre-existing rural-urban disparities in working conditions and workforce capacity in rural areas. Rural NHs should be more proactive and strategic about attracting direct care providers by providing competitive compensation, benefits, or incentives such as reduced training costs or loan repayment. In addition, increasing the opportunities for continuing education and availability of afterschool programs and daycare may ease the concerns from prospective employees and their families when they consider moving to rural areas.26 , 27 Changing policies that remove state and federal level barriers to professional practice (e.g., restricted scope of practice) also can ensure that all levels of professionals practice to the full extent of their training and educational preparation.26 , 27 These strategies could help optimize the use of healthcare professionals in rural NHs.
Consistent with previous studies,4 , 6 there was no major change in the degree of medical provider shortages among rural-urban NHs over the study period. Disparities in medical care accessibility due to physician shortage in rural communities have been well-documented,28 yet no significant difference in physician shortages was observed between rural and urban NHs during the pandemic. Plausibly, increased use of telemedicine visits attenuated the impact of the pandemic on medical provider accessiblity29 in both rural and urban areas. The recent regulatory change surrounding telemedicine services (e.g., reimbursement waiver or relaxation of HIPPA by Medicare)30 will most likely continue to encourage telemedicine use in NHs, and thus, potentially alleviate medical provider shortages.
Potential study limitations should be acknowledged when interpreting findings. First, NHs that did not pass the data quality check were excluded from study, and thus, findings may not be generalizable to these facilities. Second, the nature of the self-reported NH data, coupled with recent reports of understated COVID-19 related deaths in New York and perhaps, elsewhere, may have biased study results. Future studies should explore actual (versus self-reported) NH pandemic era staffing level differences by rural/urban status to confirm our findings.
Conclusions
The COVID-19 pandemic added a significant burden in meeting the needs of rural NH residents, exacerbating limited healthcare resources which were already strained and vulnerable prior to the COVID-19 pandemic. Pandemic-related policies should more focus on alleviating geographic disparities in NH human resources during the pandemic. To do so, further research is needed to identify effective strategies to augment workforce to better prepare rural NHs for long-lasting natural disasters as witnessed following the COVID-19 pandemic. For example, workforce redeployment or additional enhanced staff training and continuing education for outbreak management is a must to ensuring rapid, effective, and efficient response to infectious outbreaks while reducing subsequent work-related stressors.
Declaration of Competing Interest
None
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Ouslander JG, Grabowski DC. COVID-19 in nursing homes: Calming the perfect storm. J Am Geriatr Soc. 2020;68(10):2153–2162. doi: 10.1111/jgs.16784. [DOI] [PubMed] [Google Scholar]
- 2.Barnett ML, Hu L, Martin T, Grabowski DC. Mortality, admissions, and patient census at SNFs in 3 US cities during the COVID-19 pandemic. JAMA - J Am Med Assoc. 2020;324(5):507–509. doi: 10.1001/jama.2020.11642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foundation Kaiser Family. In: Kaiser Family Foundation, editor. Vol. 24. KFF; 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/factors-associated-with-covid-19-cases-and-deaths-in-long-term-care-facilities-findings-from-a-literature-review/ (Factors Associated With COVID-19 Cases and Deaths in Long-Term Care Facilities: Findings from a Literature Review | KFF). [Google Scholar]
- 4.Harrington C, Ross L, Chapman S, Halifax E, Spurlock B, Bakerjian D. Nurse staffing and Coronavirus infections in California nursing homes. Policy, Polit Nurs Pract. 2020;21(3):174–186. doi: 10.1177/1527154420938707. [DOI] [PubMed] [Google Scholar]
- 5.Gibson DM, Greene J. State actions and shortages of personal protective equipment and staff in U.S. nursing homes. J Am Geriatr Soc. 2020;68(12):2721–2726. doi: 10.1111/jgs.16883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu H, Intrator O, Bowblis JR. Shortages of staff in nursing homes during the COVID-19 pandemic: What are the driving factors? J Am Med Dir Assoc. 2020;21(10):1371–1377. doi: 10.1016/j.jamda.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGarry BE, Grabowski DC, Barnett ML. Severe staffing and personal protective equipment shortages faced by nursing homes during the covid-19 pandemic. Health Aff. 2020;39(10):1812–1821. doi: 10.1377/hlthaff.2020.01269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peters DJ. Community susceptibility and resiliency to COVID-19 across the rural-urban continuum in the United States. J Rural Heal. 2020;36(3):446–456. doi: 10.1111/jrh.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adams SL. Influences of turnover, retention, and job embeddedness in the nursing workforce literature. Online J Rural Nurs Heal Care. 2016;16(2):168–195. doi: 10.14574/ojrnhc.v16i2.405. [DOI] [Google Scholar]
- 10.Henning-Smith C, Cross D, Rahman A. Challenges to admitting residents: Perspectives from rural nursing home administrators and staff. Inq J Heal Care Organ Provision, Financ. 2021 doi: 10.1177/00469580211005191. https://journals-sagepub-com.proxy-tu.researchport.umd.edu/doi/pdf/10.1177/00469580211005191 2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen MK, Chevalier J, Long E. Nursing Home Staff Networks and COVID-19. Cambridge, MA; 2020. 10.3386/w27608 [DOI] [PMC free article] [PubMed]
- 12.Abrams HR, Loomer L, Gandhi A, Grabowski DC. Characteristics of U.S. nursing homes with COVID-19 cases. J Am Geriatr Soc. 2020;68(8):1653–1656. doi: 10.1111/jgs.16661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Department of Health and Human Services; 2021. Health Resources and Services Administration. Area Health Resources Files.https://data.hrsa.gov/topics/health-workforce/ahrf [Google Scholar]
- 14.New York Times. GitHub - nytimes/covid-19-data: An ongoing repository of data on coronavirus cases and deaths in the U.S. https://github.com/nytimes/covid-19-data. Accessed March 5, 2021.
- 15.COVID-19 Nursing Home Data | Data. CMS.gov. 2021;16 https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg/ [Google Scholar]
- 16.Bowblis JR, Meng H, Hyer K. The urban-rural disparity in nursing home quality indicators: The case of facility-acquired contractures. Health Serv Res. 2013;48(1):47–69. doi: 10.1111/j.1475-6773.2012.01431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baernholdt M, Hinton ID, Yan G, Xin W, Cramer E, Dunton N. Fall rates in urban and rural nursing units does location matter? J Nurs Care Qual. 2018;33(4):326–333. doi: 10.1097/NCQ.0000000000000319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang BK, Carter MW, Trinkoff AM, Nelson HW. Nurse staffing and skill mix patterns in relation to resident care outcomes in US nursing homes. J Am Med Dir Assoc. 2021;22(5):1081–1087. doi: 10.1016/j.jamda.2020.09.009. e1. [DOI] [PubMed] [Google Scholar]
- 19.Fahs P.S., Rouhana N. Policy and politics in nursing and health care. 8th. Saunders; Philadelphia: 2020. Rural Health Care: Workforce Challenges and Opportunities; pp. 437–446. [Google Scholar]
- 20.Probst JC, Baek JD, Laditka SB. Characteristics and recruitment paths of certified nursing assistants in rural and urban nursing homes. J Rural Heal. 2009;25(3):267–275. doi: 10.1111/j.1748-0361.2009.00229.x. [DOI] [PubMed] [Google Scholar]
- 21.Gessert CE, Elliott BA, Peden-McAlpine C. Family decision-making for nursing home residents with dementia: Rural-urban differences. J Rural Heal. 2006;22(1):1–8. doi: 10.1111/j.1748-0361.2006.00013.x. [DOI] [PubMed] [Google Scholar]
- 22.Aron Jamie, A, Bulteel Alexander, J. B., Clayman Kelsey, A, et al. Strategies for responding to the COVID-19 pandemic in a rural health system in New York state. Health Care. 2021;9(2):100508. doi: 10.1016/j.hjdsi.2020.100508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Corazzini KN, Anderson RA, Mueller C, Thorpe JM, McConnell ES. Licensed practical nurse scope of practice and quality of nursing home care. Nurs Res. 2013;62(5):315–324. doi: 10.1097/NNR.0b013e31829eba00. [DOI] [PubMed] [Google Scholar]
- 24.Gorges RJ, Konetzka RT. Staffing levels and COVID-19 cases and outbreaks in U.S. nursing homes. J Am Geriatr Soc. 2020;68(11):2462–2466. doi: 10.1111/jgs.16787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boscart VM, Sidani S, Poss J, et al. The associations between staffing hours and quality of care indicators in long-term care. BMC Health Serv Res. 2018;18(1) doi: 10.1186/s12913-018-3552-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rural Health Information Hub . Rural Health Information Hub; 2021. Recruitment and retention for rural health facilities overview.https://www.ruralhealthinfo.org/topics/rural-health-recruitment-retention [Google Scholar]
- 27.HRSA . US Department of Health and Human Services; 2021. Training needs to prepare the healthcare workforce for rural practice.https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/graduate-medical-edu/publications/cogme-rural-health.pdf Retreived from. [Google Scholar]
- 28.Gemelas JC. Post-ACA trends in the US primary care physician shortage with index of relative rurality. J Rural Heal. 2020 doi: 10.1111/jrh.12506. [DOI] [PubMed] [Google Scholar]
- 29.Alexander GL, Powell KR, Deroche CB. An evaluation of telehealth expansion in U.S. nursing homes. J Am Med Inform Assoc. 2021;28(2):342–348. doi: 10.1093/jamia/ocaa253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karlovitch S. Telehealth technology is underused in nursing homes despite pandemic. Contemporary Clinic; 2021. https://www.contemporaryclinic.com/view/telehealth-technology-is-underused-in-nursing-homes-despite-pandemic [Google Scholar]